Abstract
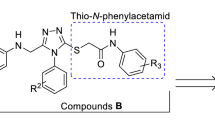
A series of 5,6-bisaryl-1,2,4-triazine-3-thiol-substituted derivatives were synthesized by condensation of 1,2-diketones and thiosemicarbazide under microwave irradiations and subsequent alkylation of thiol group by chloromethylpyridinium chloride. Evaluation of anticonvulsant activity of compounds was performed by maximal electroshock and pentylenetetrazole-induced seizures tests. In order to evaluate their neuroprotective potential, the ability of compounds to inhibit soybean 15-lipoxygenase was also assessed. Further molecular modeling and docking study on Na+ channel and GABAA receptor was performed to elucidate their mechanisms of action and necessary interactions in the active site. Compounds 2c and 2d with bis(4-bromophenyl) and pyridyl substituents showed highest protection up to 70 and 80 % in PTZ and MES-induced seizures, respectively, compared to the control group. Molecular docking study revealed their possible antiseizure mechanism of action through GABAA receptor, and in silico assessment of their BBB permeability indicated them as CNS active agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epilepsy affects approximately 1 % (50 million people) of the world’s population, and one in 10 people will suffer a seizure in their lifetime. Epilepsy is as common as breast cancer in America and takes many lives. Although administration of available antiepileptic drugs (AEDs) in patients successfully controls seizures in 50 % of patients developing partial seizures and 60–70 % of those developing generalized seizures, remaining are not responsive to the conventionally available AEDs. Moreover, the efficacy of many AEDs is limited by the dose-dependent toxicities and adverse drug reactions such as minimal brain impairment, megaloblastic anemia to death from aplastic anemia, or hepatic failure. Thus, there is a substantial need for further development of safer agents and novel mechanistic approaches in the treatment of epilepsy (Landmark, 2007); (Siddiqui and Ahsan, 2010).
However, oxidative injury may play a role in the initiation and progression of epilepsy, and therapies targeted at reducing oxidative stress may ameliorate tissue damage and favorably alter the clinical course of the disease (Devi et al., 2008).
Several in vivo evidences of oxidative stress were found in animal models of epilepsy. Accordingly, antioxidant therapies with the aim of reducing oxidative injury have received remarkable attention in the treatment of epilepsy (Acharya et al., 2008).
According to this fact, anticonvulsant agents with neuroprotective properties have received considerable attention in the treatment of epilepsy. Several studies reported that neurodegeneration is the major neurobiological abnormality in epileptic brain (Naegele, 2007). Since epileptic seizure and neurodegeneration are very similar in some aspects of their basic pathophysiology therefore, some anticonvulsive agents are equally effective neuroprotectives (Stanislaw et al., 2007).
Previous studies on oxidative stress model in neuronal cells have revealed a role for the lipoxygenases (LOX), lipid oxidizing enzymes, to produce neuronal damage. 15-LOX is one of the key inflammatory mediators in neurodegenerative disease because it is stimulated by reactive oxygen species (ROS). Activation of 15-LOX tends to generate lipid hydroperoxides (15-HPETE) that help to amplify oxidative stress (Loscalzo, 2008).
Increased level of 15-LOX has been found in early stages of Alzheimer disease in human and in experimental model of stroke in mice (Van Leyen et al., 2006; Pratico et al., 2004). Therefore, inhibition of 15-LOX may protect a variety of neuronal cell types, and 15-LOX inhibitors could be potential neuroprotective agents.
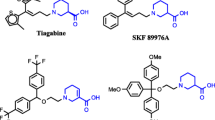
Several heterocycle-containing compounds have been reported to have considerable antiepileptic activities. 1,2,4-triazine is among the usually occurred heterocyclic nuclei possessing the wide range of biological applications such as anticonvulsant (Irannejad et al., 2014), antiparkinsonism (Congreve et al., 2012), and potent neuroprotective (Irannejad et al., 2010) activities. Among these biological activities, 1,2,4-triazine derivatives have been a promising scaffold which is mainly used in the novel anticonvulsant drugs such as lamotrigine (Fig. 1). Lamotrigine shares similar mode of action on neuronal sodium channel as phenytoin.
Recently, we synthesized and evaluated anticonvulsant activity of some 1,2,4-triazine-substituted derivatives (Fig. 1). Among the compounds tested, we found out the prominent anticonvulsant activity of 3-((pyridin-4-ylmethyl)thio)-5,6-di-p-tolyl-1,2,4-triazine as a lead compound in both maximal electroshock (MES) and pentylenetetrazole (PTZ)-induced seizures tests (Irannejad et al., 2014). Motivated by these observations and in continuation of our previous ongoing research studies on novel neuroprotectives and anticonvulsants, we synthesized some new 5,6-bisaryl-1,2,4-triazine-3-thiol derivatives (Fig. 2) and evaluated their anticonvulsant and 15-LOX inhibition activities. Evaluation of anticonvulsant activity was performed by two conventional and well-established methods, MES and PTZ-induced seizures tests. Neurotoxicity of synthesized compounds was assessed by rota-rod test, and the ability of compounds to inhibit soybean 15-LOX was also evaluated. To find out their possible anticonvulsant mechanism of action, molecular docking was performed on the two main targets of conventional antiseizure drugs, Na + channel and GABAA receptor.
Materials and methods
Chemistry
Chemical reagents and solvents were purchased from Sigma-Aldrich or Merck. NMR spectra were recorded in DMSO-d 6 on a Brucker DRX400 MHz instrument. TMS was used as an internal standard in reporting chemical shifts (δ). Mass spectra were obtained with Agilent 7890A spectrometer. Progress of reaction and purity of compounds were monitored on TLC silica gel F254 plates. The microwave irradiation was carried out using MicroSYNTH Laboratory System (MILESTONE S.r.l) in Teflon closed vessel at 300 W power.
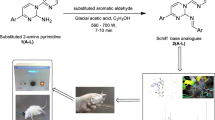
General procedure for preparation of 3 and 1a,b
Preparation of 5,6-bisaryl-1,2,4-triazine-3-thiol derivatives was performed by a rapid, simple, and green procedure reported previously by us (Scheme 1). In general, a few drops of concentrated hydrochloric acid were added to a mixture of the appropriate 1,2-diketone (1 eq) and thiosemicarbazide (1.2 eq) in an appropriate ratio of water and ethanol and then the mixture was irradiated under microwave conditions for 10 min at 120 °C (300 W). At the end of this time, the precipitated solid was filtered and washed with water several times to give the desired product (Irannejad et al., 2014).
General procedure for preparation of compound 2a–d and 4a,b
To a stirred solution of compound 3 or 1a,b (1.7 mmol) in 20 ml of ethanol, sodium hydroxide solution (170 mg in 5 ml of water) and appropriate chloromethylpyridinium chloride (2 mmol) were added, and the resulting mixture was stirred at room temperature for 3 h. At the end of this time, it was concentrated under vacuum and neutralized with HCl 1 N, and the resulting aqueous phase was extracted with chloroform, dried with sodium sulfate. Upon concentrating the organic phase under vacuum, the resulting material was purified by column chromatography (silica gel, mesh 230–400) eluting with dichloromethane–methanol (9:1) (Irannejad et al., 2014).
5,6-Bis(4-fluorophenyl)-3-(pyridin-3-ylmethylthio)-1,2,4-triazine (2a)
M.p.: 188–190 °C; IR (KBr): 3125, 2870, 1667 (C=N), 1560 (N=N). 1H NMR (400 MHz, DMSO-d 6) δ: 3.73 (s, 2H, SCH2), 7.18 (d, J = 7.24 Hz, 2H, phenyl), 7.22 (d, J = 7.28 Hz, 2H, phenyl), 7.32 (dd, J = 6.76 Hz, 4.36 Hz, 2H, phenyl), 7.43 (dd, J = 6.8 Hz, 4.36 Hz, 2H, phenyl), 7.70 (d, J = 6.12 Hz, 1H, pyridine), 8.44 (d, J = 3.6 Hz, 1H, pyridine), 8.47 (s, 1H, pyridine). 13C NMR (100 MHz, DMSO-d 6) δ: 32.31, 115.10 (d, J = 6.24 Hz), 115.27 (d, J = 6.24 Hz), 123.49, 131.12 (d, J = 6.79 Hz), 131.96 (d, J = 6.79 Hz), 132.30, 136.30, 141.50, 148.05, 149.71, 154.32, 161.20, 162.38, 163.15, 164.36, 165.33. Anal. Calcd for C21H14F2N4S: C, 64.27; H, 3.60; N, 14.28. Found: C, 64.41; H, 3.53; N, 14.39.
5,6-Bis(4-fluorophenyl)-3-(pyridin-4-ylmethylthio)-1,2,4-triazine (2b)
M.p.: 172–174 °C; IR (KBr): 3,122, 2,884, 1,665 (C=N), 1,569 (N=N). 1H NMR (400 MHz, DMSO-d 6) δ: 3.78 (s, 2H, SCH2), 7.11 (t, J = 7.5 Hz, 2H, Ar), 7.14 (t, J = 7.5 Hz, 2H, Ar), 7.56 (dd, J = 6.8 Hz, 4.5 Hz, 2H, Ar), 7.59 (dd, J = 6.8 Hz, 4.5 Hz, 2H, Ar), 7.82 (d, J = 4.7 Hz, 2H, pyridine), 8.44 (d, J = 4.8 Hz, 2H, pyridine). 13C NMR (100 MHz, DMSO-d 6) δ: 34.33, 117.45 (d, J = 6.29 Hz), 117.56 (d, J = 6.29 Hz), 122.42, 133.57 (d, J = 6.75 Hz), 134.12 (d, J = 6.75 Hz), 134.77, 136.16, 137.29, 142.46, 147.28, 149.63, 157.51, 160.53, 162.07. Anal. Calcd for C21H14F2N4S: C, 64.27; H, 3.60; N, 14.28. Found: C, 64.32; H, 3.48; N, 14.12.
5,6-Bis(4-bromophenyl)-3-(pyridin-3-ylmethylthio)-1,2,4-triazine (2c)
M.p.: 212–214 °C; IR (KBr): 3,093, 2,897, 1,680 (C=N), 1,564 (N=N). 1H NMR (400 MHz, DMSO-d 6) δ: 3.72 (s, 2H, SCH2), 7.22 (d, J = 6.72 Hz, 2H, phenyl), 7.31 (d, J = 6.72 Hz, 2H, phenyl), 7.51 (t, J = 6.34 Hz, 1H, pyridine), 7.55 (d, J = 6.68 Hz, 2H, phenyl), 7.59 (d, J = 6.84 Hz, 2H, phenyl), 7.70 (d, J = 6.08 Hz, 1H, pyridine), 8.44 (d, J = 2.84 Hz 1H, pyridine), 8.47 (s, 1H, pyridine). 13C NMR (100 MHz, DMSO-d 6) δ: 32.32, 122.26, 123.50, 124.57, 130.24, 130.92, 131.18, 131.24, 131.37, 133.90, 134.99, 136.30, 141.35, 148.04, 149.71, 154.53, 165.06. Anal. Calcd for C21H14Br2N4S: C, 49.05; H, 2.74; N, 10.90. Found: C, 49.28; H, 2.68; N, 10.54 s.
5,6-Bis(4-bromophenyl)-3-(pyridin-4-ylmethylthio)-1,2,4-triazine (2d)
M.p.: 209–211 °C; IR (KBr): 3,104, 2,833, 1,684 (C=N), 1,562 (N=N). 1H NMR (400 MHz, DMSO-d 6) δ: 4.6 (s, 2H, SCH2), 7.40 (d, J = 6.72 Hz, 2H, phenyl), 7.42 (d, J = 6.72 Hz, 2H, phenyl), 7.63 (d, J = 6.72 Hz, 4H, phenyl), 7.51 (d, J = 4.72 Hz, 2H, pyridine), 8.51 (d, J = 4.8 Hz, 2H, pyridine). 13C NMR (100 MHz, DMSO-d 6) δ: 32.66, 123.17, 123.98, 124.85, 131.38, 131.53, 131.74, 133.92, 134.16, 146.70, 149.61, 153.37, 154.89, 169.24. Anal. Calcd for C21H14Br2N4S: C, 49.05; H, 2.74; N, 10.90. Found: C, 49.23; H, 2.64; N, 10.69.
3-(Pyridin-3-ylmethylthio)-5,6-di(thiophen-2-yl)-1,2,4-triazine (4a)
M.p.: 175 °C; IR (KBr): 3,086, 2,852, 1,671 (C=N), 1,523 (N=N). 1H NMR (400 MHz, DMSO-d 6) δ (ppm): 3.62 (s, 2H, SCH2), 7.02 (d, J = 3.2 Hz, 1H, Ar), 7.14 (t, J = 3.6 Hz, 1H, Ar), 7.24 (t, J = 3.6 Hz, 1H, Ar), 7.34 (d, J = 3.3 Hz, 1H, Ar), 7.57 (d, J = 4.0 Hz, 1H, Ar), 7.87 (d, J = 4.0 Hz, 1H, Ar), 7.51 (t, J = 4.5 Hz, 1H, pyridine), 7.81 (d, J = 4.0 Hz, 1H, pyridine), 8.31 (s, 1H, pyridine), 8.43 (d, J = 4.5 Hz, 1H, pyridine). 13C NMR (100 MHz, DMSO-d 6) δ: 36.82, 125.93, 127.69, 128.45, 129.11, 129.27, 132.51, 132.59, 133.20, 134.62, 136.38, 138.63, 147.07, 148.03, 149.08, 150.51, 168.54. Anal. Calcd for C17H12N4S3: C, 55.41; H, 3.28; N, 15.20. Found: C, 55.69; H, 3.16; N, 15.49.
3-(Pyridin-4-ylmethylthio)-5,6-di(thiophen-2-yl)-1,2,4-triazine (4b)
M.p.: 178–180 °C; IR (KBr): 3,091, 2,899, 1,681 (C=N), 1,556 (N=N). 1H NMR (400 MHz, DMSO-d 6) δ (ppm): 3.68 (s, 2H, SCH2), 6.96 (d, J = 3.0 Hz, 1H, Ar), 7.08 (t, J = 3.96 Hz, 1H, Ar), 7.18 (t, J = 4.08 Hz, 1H, Ar), 7.30 (d, J = 2.48 Hz, 1H, Ar), 7.80 (d, J = 4.16 Hz, 1H, Ar), 7.95 (d, J = 4.16 Hz, 1H, Ar), 7.37 (d, J = 4.6 Hz, 2H, pyridine), 8.49 (d, J = 4.6 Hz, 2H, pyridine). 13C NMR (100 MHz, DMSO-d 6) δ: 38.48, 126.82, 127.43, 128.06, 129.22, 129.31, 131.58, 132.49, 134.82, 135.25, 145.67, 147.71, 148.73, 148.86, 166.72. Anal. Calcd for C17H12N4S3: C, 55.41; H, 3.28; N, 15.20. Found: C, 55.53; H, 3.41; N, 15.38.
Docking study
The homology model of the Diazepam bound GABAA receptor developed by Richter et al. (2012) and lamotrigine bound Na+ channel by Lipkind and Fozzard (2010) was retrieved from the supplementary material of their published paper.
Protein structure was prepared with Pymol 1.6.0 (The PyMOL Molecular Graphics System, Schrödinger, LLC). HyperChem v.8, with AM1 force field was used to generate the lowest energy conformations. Docking study has been performed with AutoDock 4.2 software, using AutoDock Tools (ADT) in MGLTools 1.5.6. For the protein and the ligand, Kollman and Gasteiger charges were computed, respectively. The Lamarckian genetic algorithm (LGA) was used as a search engine. AutoGrid 4.2 was utilized for defining active site, and the grid size was set to 20 × 20 × 20 points with a grid spacing of 1.0 on the center of the X-ray ligand in the crystal structure complex. The other parameters were as follows:
Maximum number of energy evaluations: 2,500,000, independent GA runs: 20, maximum number of LGA operations: 27,000, population size: 150, crossover: 0.80, mutation: 0.02, elitism: 1.
Pharmacology
In vivo seizure test was performed on male NMRI mice weighting 20–30 g (Pasteur Institute, Tehran, Iran). Mice were kept in animal facility at controlled temperature (22 ± 2 °C) with 12–12 h light–dark cycle and free access to food and water. The behavioral experiments were done between 9 a.m. and 4 p.m. Each mouse was used only once in all experiments. Solutions were prepared in a vehicle consisted of polyethyleneglycol (PEG) 30 % v/v in distilled water and were administered at the dose of 100 mg/kg to mice. All compounds (or vehicle in control group) were administered through intraperitoneal (i.p.) injection 30 min before performing seizure test. Procedures involving animals were conducted in accordance with the Shahid Beheshti University Guidelines for Care and Use of Laboratory Animals.
Pentylenetetrazole (PTZ)-induced seizure test
Thirty minutes after intraperitoneal injection (at a volume of 10 ml/kg) of synthesized compounds or vehicle (PEG 30 % v/v in distilled water), animals were subject to PTZ-induced seizure test. The threshold for clonic seizures was determined by infusion of a 1 % solution of PTZ in distilled water through the tail vein of unrestricted freely moving mouse at a constant rate of 0.25 ml/min with an infusion pump (model 53140, Stoelting, USA). The required dose of PTZ (in mg/kg) that caused generalized clonic seizure with loss of righting reflex was considered as the threshold for the clonic seizure (Naderi et al., 2011).
Maximal electroshock (MES)-induced seizure test
Electroshock was induced by generating an alternating current (intensity 40 mA, pulse duration 0.2 s, frequency 50 Hz, pulse width 0.5 ms) through ear clip electrodes by a stimulator (Borj Sanat, Iran). In order to improve electrode conduction, electrodes were moistened by saline before attaching to the ear of mouse. The end-point for the occurrence of seizure was the observation of hind-limb tonic extension (HLTE) in mice (Woodbury and Davenport, 1952); (Woodbury and Swinyard, 1952). To select proper current intensity for electroconvulsions, 5 groups of mice consisting of five animals per group were challenged with electroshocks of various intensities (25, 30, 35, 40, and 45 mA) that yield seizure in minimum of 20 % and maximum of 100 % of animals in a current-dependent manner. After plotting a current intensity-seizure curve, the CS97 (40 mA), which was a current intensity that produced HLTE in 97 % of animals, was determined according to log-Probit method by Litchfield and Wilcoxon (1949) and was applied in all electroshock experiments. Data were shown as percent protection, which is the percentage of animals in each group that did not have HLTE after receiving electroshock.
Rota-rod test
To evaluate the effect of compounds on motor coordination, rota-rod test was conducted before seizure test. The animals were placed on rods (rotating at the speed of 10 rounds per minute). Failure to keep staying on the rotating rod for a period of 90 s was considered as drug-induced motor impairment.
Statistical analysis
Statistical analysis was done using GraphPad Prism 5.0 (GraphPad Software Inc., CA, USA). In PTZ test, the results were shown as mean ± SEM. One-way analysis of variance (ANOVA) followed by Dunnett’s post-test was used to compare various groups with the control group. In MES test, data were analyzed using Fisher’s exact test. p values less than 0.05 were considered as statistically significant.
15-Lipoxygenase inhibition assay
LOX inhibitory activity of target compounds was studied by a spectrophotometric assay. The tested compounds were dissolved in DMSO (1 ml) and phosphate buffer (9 ml, 0.1 M, pH 8). This stock solution was added to test solution containing enzyme (final concentration: 167 U/ml) and phosphate buffer (pH 8) to achieve concentrations in range of 10−3–10−6 M. After incubation of test solution for 4 min, substrate (linoleic acid, final concentration: 134 µM) was added, and change in the absorbance was measured for 60 s at 234 nm. The enzyme solution was kept in ice, and controls were measured at intervals throughout the experimental periods to ensure that the enzyme activity was constant (Assadieskandar et al., 2012).
Results and discussion
Antiseizure effects of compounds in PTZ and MES-induced seizure test in mice
Protective effect of new compounds against convulsion was evaluated in MES and PTZ-induced seizures in mice. The required dose of PTZ to induce seizure, 30 min after the intraperitoneal administration of drugs, through continuous i.v. infusion for each compound is shown in Table 1. One-way ANOVA revealed a significant change in the dose of PTZ required for seizure induction between different groups [F(7,41) = 2.567; p = 0.027]. Further analysis using Dunnett’s test revealed a significant increase in PTZ dose for seizure induction in mice pretreated with compound 2c (70 mg/kg, p < 0.05) compared with the control group. Compound 2c bearing bromine atom at para position of phenyl rings and 3-pyridylmethylthio side chain had the highest protective effect in PTZ-induced seizure test among all compounds. The required dose of PTZ to induce seizure in control group was 45 mg/kg and in group receiving the reference drug lamotrigine was 82 mg/kg. Compound 4b was in the second order of protective effect and required 66 mg/kg of PTZ to induce seizure. The other compounds had less anticonvulsive effect especially compounds 3 and 1a,b without the pyridylmethyl side chain on thiol group.

The results of MES-induced seizure test are also shown in Table 1. Control group (receiving PEG 30 % in water) did not show any protective effect against MES-induced seizures, while group receiving the reference drug lamotrigine revealed 100 % protection. Among compounds tested, compound 2d with bromine atom at phenyl rings had the highest protective effect up to 80 % with p value less than 0.01. Compounds 4a, 2c, and 2b could protect animals up to 71, 60, and 58 %, respectively (p value <0.01). Similar to PTZ-induced seizure test, compounds 3 and 1a,b without the pyridylmethyl side chain on thiol group had the least protective effect against MES-induced seizures. Obtained results clearly indicated that the pyridylmethyl side chain is necessary for optimal anticonvulsive effect, and a lipophilic group such as bromine atom at para positions of phenyl rings could improve the protective effect of compounds. The results of rota-rod test revealed no drug-induced motor impairment at the administered dose of 100 mg/kg (data not shown).
The results of anticonvulsant evaluation of compounds revealed that presence of a lipophilic atom such as bromine at para position of phenyl rings could improve the antiseizure ability of compounds 2c and 2d. Presence of thiophene ring instead of 4-bromophenyl moiety has also increased the anticonvulsant property in compound 4a due to its lipophilic character. Similar results were obtained in our previous study on 1,2,4-triazine-substituted derivatives in which lipophilic substituents such as chloro atom and methyl group at para position of phenyl ring showed higher anticonvulsant action (Irannejad et al., 2014). Presence of a suitable substitution at thiol group is necessary for optimum antiseizure property. According to our previous study on new antiepileptic compounds, 3-pyridylmethyl or 4-pyridylmethyl groups could increase antiepileptic character of compounds and are preferred over methyl group or non-substituted compounds at thiol groups (compounds 1a,b and 3). Investigation of structure–activity relationship of 5,6-diaryl-1,2,4-triazine derivatives as new anticonvulsant compounds has shown that incorporation of groups capable of constituting polar interactions such as hydrogen bonds (in this case, nitrogen atom of pyridine ring) can substantially increase the anticonvulsant effect.
Molecular docking study
In order to find out their possible mechanism of anticonvulsion, molecular docking was performed on the two main targets of conventional anticonvulsant drugs, Na+ channel and GABAA receptor. Compound 2d was chosen for this purpose due to its high anticonvulsive property.
Na+ channel is a multisubunit complex. Channel’s pore and especially the principal drug-binding site are composed of α-subunit with approximately 2,000 amino acids. Four highly homologous domains (I–IV) make the α-subunit, and each domain is composed of six presumably transmembrane α-helical segments (S1–S6), assembled in a clockwise pattern around the central pore. This pore has a large outer vestibule, formed by the four extracellular P loop segments. These P loops fold back into the membrane to make a shallow funnel so that in deeper part becomes narrow and makes the selectivity filter with 4 × 6 Å size.
The large outer vestibule of this pore was used as binding site for docking of anticonvulsant drugs. After docking calculation, compound 2d was located in the middle of sodium channel and could occlude the inner pore as shown in Fig. 3. Binding mode of compound 2d showed that 4-bromophenyl moieties of this compound are interacting with Phe91 and Leu88 of IIS6 and IIIS6 and Phe84 and Val88 in IVS6 through hydrophobic and π–π interactions. Pyridyl ring has twisted toward Val87, Val88, and Tyr91 of IVS6 and Phe84 from IS6 and constitutes van der waals interactions mainly by its aromatic π electrons. Finally, triazine ring is hydrogen bonded to Asn88 side chain in IS6. The estimated free energy of binding to sodium channel was −6.38 kcal/mol.
GABAA receptor is one of the main targets for anticonvulsive drugs such as benzodiazepines. The majority of GABAA receptors are composed of α, β, and γ-subunits. The benzodiazepine-binding site of these receptors is located extra-cellularly at α1–γ2 interface. Molecular docking was performed on the benzodiazepine-binding site of GABAA receptor.
Binding mode of compound 2d is visualized in Fig. 4. As shown, one 4-bromophenyl part of ligand is interacted with Tyr159 and His101 at α1-subunit, while the other 4-bromophenyl group is in contact with α1-Val202 and Phe77 at δ2-subunit. Triazine ring has π–π stacking with α1-Tyr209, and the protonated nitrogen atom of pyridine ring at physiological pH is ionic bonded to δ2-Arg132. The free energy of binding was estimated to be −11.74 kcal/mol, in benzodiazepine-binding site in GABAA receptor. The higher free energy of binding for compound 2d in GABAA receptor than Na+ channel may propose its possible mechanism of anticonvulsant action through binding to benzodiazepine-binding site on GABAA receptor. On the other hand, compound 2d and its congeners (compounds 2a–d and 4a,b) possibly bind to the benzodiazepine-binding site on GABAA receptor to exert their antiseizure action as revealed by the binding free energy calculation. However, other important anticonvulsant targets such as glutamate receptors and calcium channels are not evaluated here, but it remains to be cleared in our next study.
In vitro 15-LOX inhibition assay
As discussed earlier in this section, 15-lipoxygenase (15-LOX) is a key enzyme in initiation of oxidative stress in neurodegenerative diseases. Thus, inhibition of 15-LOX by synthesized 1,2,4-triazine-substituted derivatives was assessed, and the results are shown in Table 2. All compounds showed mild to moderate inhibition of 15-LOX at about 100 µM, while quercetin as a reference drug inhibited the 15-LOX at 18 µM. Compound 2c with highest anticonvulsive property in PTZ test could inhibit 15-LOX at 89 µM which was again the best one among compounds. There was not a significant difference in potency among compounds against 15-LOX, and the IC50 values were ranging from 89 to 119 µM due to their high structural similarity protective effect of compounds against MES and PTZ-induced seizures along with their moderate inhibition of 15-LOX may provide synergistic effect in prevention of neurodegenerative diseases progression and to introduce new generation of anticonvulsant agents.
Prediction of blood–brain barrier permeability
Blood–brain barrier (BBB) permeability is one of the most important challenges in the pharmacology of CNS active drugs. The extent of CNS penetration has limited usage of many drugs whose target is located in the central nervous system and high percentage of CNS-acting drugs fail to pass the clinical trials annually due to the CNS penetration failure. This drawback has imposed high expenses at pharmaceutical and drug development companies nowadays. Therefore, evaluating the capability of new compounds to pass the BBB by in silico methods would be inevitable and helpful.
Several “rules of thumb” have been developed for prediction of passive BBB permeability. Compounds are more likely to penetrate the BBB if the following criteria meet. (1) Molecular weight (MW) less than 400–500 Da. (2) LogD (logarithm of distribution coefficient) between −1 and 4. (3) Number of total hydrogen bonds (nHB) less than 10. (4) Polar surface area (TPSA) less than 90 Å2. Increasing the number of rules which are not obeyed by one compound decreases the possibility of its BBB permeability (Waterbeemd et al., 1998).
The calculated physiochemical parameters for compounds 2a–d and 4a,b are shown in Table 3 along with their predicted values of logBB (logarithm of brain/plasma concentration) and CNS activity by ACD/Lab. As shown, values of MW are almost in the defined range (<500 Da), but with a minor and negligible increase for compounds 2c and 2d, but predicted logD values for these two compounds (5.96 and 5.94, respectively) are located a bit far from the maximum allowed value of 4. As seen in this table, number of total hydrogen bonds for all compounds is less than 10. However, some predicted values such as logD of compounds 2c,d and TPSA for 4a,b fall a bit out of the range, but it does not mean that these compounds have lack of CNS activity and only may reduce their extent of passage through BBB. Moreover, this fact was further confirmed by the predicted values of logBB and CNS activity. Finally, considering the pred. logBB values of compounds 2a–d and 4a,b reported in Table 3, all of them were predicted to be CNS active.
Conclusion
Development of novel anticonvulsive drugs has become a challenge of the new century. Available anticonvulsive drugs are not effective and responsive in most cases. Therefore, introduction of novel and multitargeted anticonvulsive agents offers new opportunity to overcome convulsions. In this study, some new 1,2,4-triazine derivatives were evaluated as dual anticonvulsive and 15-lipoxygenase inhibitors. Molecular docking study revealed their possible antiseizure mechanism of action through GABAA receptor. Finally, in silico assessment of their BBB permeability indicated them as CNS active agents. Future studies of these novel neuroprotective inhibitors of 15-LOX may provide new therapeutic opportunities to combat convulsion and neurodegenerative diseases.
References
Acharya MM, Hattiangady B, Shetty AK (2008) Progress in neuroprotective strategies for preventing epilepsy. Prog Neurobiol 84:363–404
Assadieskandar A, Amini M, Salehi M, Sadeghian H, Alimardani M, Sakhteman A, Nadri H, Shafiee A (2012) Synthesis and SAR study of 4,5-diaryl-1H-imidazole-2(3H)-thione derivatives as potent 15-lipoxygenase inhibitors. Bioorg Med Chem 20:7160–7166
Congreve M, Andrews SP, Dore AS, Hollenstein K, Hurrel E, Langmead CJ, Mason JS, Ng IW, Tehan B, Zhukov A, Weir M, Marshall FH (2012) Discovery of 1,2,4-triazine derivatives as adenosine A2A antagonists using structure based drug design. J Med Chem 55:1898–1903
Devi PU, Manocha A, Vohora D (2008) Seizures, antiepileptics, antioxidants and oxidative stress: an insight for researchers. Expert Opin Pharmacother 9:3169–3177
Irannejad H, Amini M, Khodaghi F, Ansari N, Khoramian Tusi S, Sharifzadeh M, Shafiee A (2010) Synthesis and in vitro evaluation of novel 1,2,4-triazine derivatives as neuroprotective agents. Bioorg Med Chem 18:4224–4230
Irannejad H, Naderi N, Emami S, Foroumadi A, Qobadi Ghadikolaei R, Zafari T, Mazar-Atabaki A, Dadashpour S (2014) Microwave assisted synthesis and anticonvulsant activity of 5,6-bisaryl-1,2,4-triazine-3-thiol derivatives. Med Chem Res 23:2503–2514
Landmark CJ (2007) Targets for antiepileptic drugs in the synapse. Med Sci Monit 13:RA1–RA7
Lipkind GM, Fozzard HA (2010) Molecular model of anticonvulsant drug binding to the voltage-gated sodium channel inner pore. Mol Pharmacol 78:631–638
Litchfield J, Wilcoxon F (1949) A simplified method of evaluating dose-effect experiments. J Pharmacol Exp Ther 96:99–113
Loscalzo J (2008) Membrane redox state and apoptosis: death by peroxide. Cell Metab 8:182–183
Naderi N, Ahmad-Molaei L, Aziz Ahari F, Motamedi F (2011) Modulation of anticonvulsant effects of cannabinoid compounds by GABA-A receptor agonist in acute pentylenetetrazole model of seizure in rat. Neurochem Res 36:1520–1525
Naegele JR (2007) Neuroprotective strategies to avert seizure-induced neurodegeneration in epilepsy. Epilepsia 48:107–117
Pratico D, Zhukareva V, Yao Y, Uryu K, Funk CD, Lawson JA, Trojanowski JQ, Lee VM (2004) 12/15Lipoxygenase is increased in Alzheimer’s disease: possible involvement in brain oxidative stress. Am J Pathol 164:1655–1662
Richter L (2012) Diazepam-bound GABA receptor models identify new benzodiazepine binding-site ligands. Nat Chem Biol 8:455–464
Siddiqui N, Ahsan W (2010) Triazole incorporated thiazoles as a new class of anticonvulsants: design, synthesis and in vivo screening. Eur J Med Chem 45:1536–1543
Stanislaw C, Renata F, Barbara B, Kinga KB (2007) Neuroprotective effects of some newer and potential antiepileptic drugs. J Pre-Clin Clin Res 1:1–5
Van Leyen K, Kim HY, Lee SR, Jin G, Arai K, Lo EH (2006) Baicalein and 12/15-lipoxygenase in the ischemic brain. Stroke 37:3014–3018
Waterbeemd HV, Camenisch G, Folkers G, Chretien JR, Raevsky OA (1998) Estimation of blood-brain barrier crossing of drugs using molecular size and shape, and H-bonding descriptors. J Drug Target 6:151–165
Woodbury LA, Davenport VD (1952) Design and use of a new electroshock seizure apparatus, and analysis of factors altering seizure threshold and pattern. Arch Int Pharmacodyn Ther 92:97–107
Woodbury LA, Swinyard CA (1952) Stimulus parameters for electroshock seizures in rats. Am J Physiol 170:661–667
Acknowledgments
We gratefully acknowledge the financial support from the Research Council of Mazandaran University of Medical Sciences, Sari, Iran.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Irannejad, H., Nadri, H., Naderi, N. et al. Anticonvulsant activity of 1,2,4-triazine derivatives with pyridyl side chain: synthesis, biological, and computational study. Med Chem Res 24, 2505–2513 (2015). https://doi.org/10.1007/s00044-014-1315-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00044-014-1315-3