Abstract
Objectives
Long-term social costs associated with underground uranium mining are largely unknown. This study estimated health costs of Native American and white (Hispanic and non-Hispanic origin) uranium miners in the US Public Health Service Colorado Plateau cohort study.
Methods
Elevated uranium miner person-years of life lost (PYLL) were calculated from the most recent study of the Colorado Plateau cohort over 1960–2005. Nine causes of death categories were included. Costs to society of miner PYLL were monetized using the value of a statistical life-year approach.
Results
Costs over 1960–2005 totaled $2 billion USD [95% CI: $1.8, $2.2], or $2.9 million per elevated miner death. This corresponds to $43.1 million [95%: $38.7, $48.7] in annual costs. Lung cancer was the most costly cause of death at $1.4 billion [95%: $1.3, $1.5]. Absolute health costs were largest for white miners, but Native Americans had larger costs per elevated death. Annual excess mortality over 1960–2005 averaged 366.4 per 100,000 miners; 404.6 (white) and 201.5 per 100,000 (Native American).
Conclusions
This research advances our understanding of uranium extraction legacy impacts, particularly among indigenous populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Uranium miners face significant health risks. Elevated rates of cancer and respiratory diseases (e.g., chronic obstructive pulmonary disease (COPD), silicosis, pulmonary fibrosis, etc.) are often observed among miners exposed to radon in underground uranium mines (Rage et al. 2015; Tirmarche et al. 2012; Boice et al. 2008; Samet et al. 1991; Archer et al. 1976). Cohort studies of uranium miners working underground between 1940 and 1960 find that health impacts can persist for decades after last radon exposure, (Duan et al. 2015; Al-Zoughool and Krewski 2009) through as recently as 2005 for miners working on the Colorado Plateau in the 1950s; 45+ years since first being examined (Schubauer-Berigan et al. 2009).
Excess risk of mortality in uranium mining imposes considerable long-term health impacts on society, in addition to emotional and physical burdens on families and communities. However, the mortality health costs to society among this population remains largely unknown. Understanding the legacy, health economic impacts of uranium extraction is important for at least three reasons. First, nuclear power is seen as a sustainable source of low-carbon energy that is expected to play an increasingly important role as the international community implements the recent 21st session of the United Nations Conference of the Parties (COP21) climate change agreement (IAEA 2015). Increased use of nuclear energy will lead to renewed interest in global uranium mining. Second, assessments of uranium extraction lack quantifiable data on uranium miner health costs (e.g., National Research Council 2012; Chmura Economics & Analytics 2011), limiting their usefulness in the policymaking process. Lack of information on monetary health costs of uranium preclude unit-per-unit comparisons to the benefits that uranium provides (e.g., jobs, tax revenue, etc.). Finally, on-going calls to strengthen the current US National Institute for Occupational Safety and Health (NIOSH) mining radon exposure standard (NIOSH 1987) would benefit from a more complete understanding of the economic impacts to society of exposure-related uranium mortality.
To address this gap in the literature, this study investigates the health economic costs associated with underground uranium mining in the Colorado Plateau, USA, the oldest and largest uranium mining district in the US-spanning parts of Colorado, Utah, Arizona, and New Mexico. In the 1950s and 1960s, the US Public Health Service (USPHS) conducted a uranium miner cohort study to investigate the risk of lung cancer and other diseases associated with exposure to radon—a naturally occurring radioactive daughter element of uranium (Lundin et al. 1971). This was partly in response to warnings from industrial hygienists in the 1950s that poor ventilation in underground mines was leading to high-levels of radon exposure (Ringholz 1989) and concerns among USPHS personnel of evidence coming out of Europe showing a link between radon and lung cancer (NIOSH 1987; Lundin et al. 1971; Donaldson 1969). Among miners in this cohort, elevated mortality risks for lung cancer, non-malignant respiratory diseases, stomach cancer, multiple myeloma, lymphohematopoietic cancers, and workplace injuries have been observed across multiple studies of white (Hispanic and non-Hispanic white) and Native American miners (Schubauer-Berigan et al. 2009; Roscoe 1997; Roscoe et al. 1995; Waxweiler et al. 1981; Archer et al. 1976; Lundin et al. 1971). To-date, no health costs analysis has been published for the Colorado Plateau study group.
We perform an economic cost analysis to quantify the non-market costs to society of premature mortality due to occupational hazard (Mishan and Quah 2007). This approach has been applied twice before to study miners. Jones (2014) found $2.5 billion in excess mortality costs for uranium miners in Grants, New Mexico, USA over 1955–2005. For coal miners in Appalachia, Hendryx and Ahern (2009) estimated $50 billion in excess mortality health costs over 1979–2005. We investigate excess mortality health costs of miners in the Colorado Plateau cohort study over 1960–2005 using the most recent extant follow-up study of the miner cohort (Schubauer-Berigan et al. 2009).
Methods
The Colorado Plateau study group
The Colorado Plateau cohort study was established by the USPHS in 1950 to study the health effects of uranium miners’ exposure to radon (Lundin et al. 1971). The cohort consisted of 3347 white and 779 non-white (primarily Native American) male uranium miners (Lundin et al. 1971). Miners came from thousands of uranium mines scattered across remote regions of the Colorado Plateau. Between 1950 and 1954, recruitment of miners was sporadic and has been described as “hit or miss”, but after 1954 a systematic epidemiological study of the miners was initiated (Advisory Committee on Human Radiation Experiments 1995). Miners were voluntarily recruited by on-site USPHS personnel to take part in medical screenings and were asked to provide smoking, medical, and occupational histories (Roscoe 1997; Roscoe et al. 1989). By the late 1950s, participation rates in the study were approximately 90% (Roscoe 1997). To be included in the cohort, miners must have completed at least 1 month underground uranium mining by January 1, 1964 and volunteered for at least one medical examination between January 1, 1950 and December 31, 1959 (Roscoe 1997; Roscoe et al. 1989).
Data
Mortality data
Mortality data for uranium miners in the Colorado Plateau cohort comes from the most recent published follow-up analysis, by Schubauer-Berigan et al. in (2009). Mortality follow-up from January 1, 1960 to December 31, 2005 was performed by linking individual workers to the National Death Index and the Social Security Administration’s mortality file. Deaths and person-years were classified into 119 cause of death categories and were stratified on age, race, calendar year, cumulative radon exposure, and smoking category. Cumulative radon exposure was calculated from the dates on which each miner’s uranium mine exposure to radon reached a given exposure level (Schubauer-Berigan et al. 2009). Mine exposure levels were estimated using actual measurements, interpolation, or geographic area estimation (Lundin et al. 1971). Standardized mortality ratios (SMRs) were estimated as the ratio of observed to expected deaths (Schubauer-Berigan et al. 2009).
Using the reported results in Schubauer-Berigan et al. (2009), we independently calculated the number of elevated deaths (i.e., observed minus expected) for cause of death categories with statistically significant SMRs at the 5% significance level. Data were stratified by race—white and Native American. Table 1 summarizes the mortality risk data used in the present analysis. In our data, we observe that the largest mortality risk is observed for silicosis where miners died at rates 2320% (Native American) to 4150% (whites) higher than expected. Rates of lung cancer are significantly elevated in the data set—218% above expectation for Native Americans and 396% above expectation for whites. Cause of death due to pulmonary fibrosis (SMR = 3.95, white; SMR = 8.70, Native American) and tuberculosis (SMR = 3.44, white; SMR = 2.40, Native American) are additionally elevated for both white and Native American miners. Whites suffer from higher rates of lymphohematopoietic cancers (SMR = 1.38) and acute glomerulonephritis and acute renal failure (SMR = 3.17). Native American miners have elevated risk of stomach cancer (SMR = 1.92).
Economic cost data
A regularly used approach to valuing mortality risk reductions is based on observations of market choices that involve tradeoffs between wages and occupational risk (Aldy and Viscusi 2008). The relevant metric is society’s willingness to pay for a risk reduction benefit. For example, in a hypothetical survey of 100,000 workers, each worker might be asked their willingness to pay for a 1-in-100,000 decrease in their risk of occupationally related mortality during the next year. If their average willingness to pay is $50 for this change, then the so-called value of a statistical life or VSL in this population would be ($50) × (100,000) = $5 million. By proportionally relating the VSL to life expectancy at age of death, we obtain the value of a statistical life-year or VSLY (Robinson 2007). VSLY is a per year value based on remaining life expectancy. This is not the value of a human life or the value of saving a life. Instead, it is the amount that a population of interest would be willing to pay for marginal change in the likelihood of death.
Estimates of VSLY abound in the economics literature (Kniesner et al. 2012; Murphy and Topel 2006; Viscusi and Aldy 2003). Many federal agencies, including the Food and Drug Administration (FDA), US Department of Transportation (US DOT), US Environmental Protection Agency (US EPA), and the Office of Management and Budget (OMB) use the VSLY to determine whether the value of an associated risk reduction brought about by regulation exceeds the value of resources diverted. Use of the VSLY is widely accepted in policymaking (Robinson 2007).
The VSLY used in the present analysis is $213,000 per year of life lost. To obtain this value, we inflation adjusted to 2015 dollars the VSLY of $150,000 in 1999 dollars recommended for use in health cost analyses based on a synthesis of more than 2 dozen studies of risk/reward tradeoffs among employed populations, including miners (Tolley et al. 1994). Inflation adjustment was done using the annual US Consumer Price Index for urban consumers. This VSLY (accounting for differences in inflation) has been used to calculate mortality health costs of uranium mining in New Mexico (Jones 2014) and the life-saving benefits of tobacco settlements (Cutler et al. 2002). While defensible, this VSLY is arguably a conservative lower-bound among estimates in the economics literature, which range as high as $480,000 for individuals of similar age as uranium miners at time of death (Aldy and Viscusi 2008). We believe that utilizing a conservative VSLY estimate is prudent given ongoing debates on valuing mortality risk reductions (US EPA 2010; Aldy and Viscusi 2008; Robinson 2007).
Analysis
Mortality health costs associated with Colorado Plateau uranium mining were calculated from person-years of life lost or PYLL. PYLL is defined as the difference in years between when a miner actually died due to a given disease and when they would have died, in expectation, given their sex, age, and race, multiplied by the total number of miners dying from that disease (Howlader et al. 2016).
Years of life lost (YLL) were estimated as the difference between the average miner’s life expectancy at the age and year of death and their actual age of death. For example, a male Native American miner dying at age 66 in the year 1992 would have a YLL of 13.9 based on an average life expectancy of 79.9. Life expectancy data were obtained by sex and race from the US Centers for Disease Control and Prevention life tables (National Center for Health Statistics 1990, 1992).
Numbers of elevated deaths over 1960–2005 for nine statistically significant cause of death SMRs as identified in the most recent mortality follow-up of Colorado Plateau miners (Schubauer-Berigan et al. 2009)—lung cancer, stomach cancer, lymphohematopoietic cancers, multiple myeloma, COPD, silicosis, pulmonary fibrosis, tuberculosis, and acute glomerulonephritis and acute renal failure (see Table 1)—were multiplied by YLL for the median miner. This product produces PYLL, which is interpreted as an aggregate measure of the person-years that uranium miners in the Colorado Plateau cohort prematurely lost due to occupationally related radon exposure. PYLL calculations were performed separately by group.
Mortality health costs were determined as the product of VSLY and PYLL, following Jones (2014), and are in units of inflation-adjusted 2015 US dollars (USD). The resulting USD figure reflects the unintended costs to society of premature uranium miner mortality across nine health endpoints between 1960 and 2005.
Cause of death categories investigated in the main effects analysis were those where a priori relationship is thought to exist between radon progeny and certain diseases, as explained in Schubauer-Berigan et al. (2009) for Colorado Plateau miners. PYLL and mortality health costs for cause of death categories with significant SMRs not of a priori interest were additionally calculated (see Electronic Supplementary Material).
Results
Uranium miners in the Colorado Plateau cohort had a median age of death of 67.5 (whites) and 66 (Native Americans). Median life expectancy at age and year of death ranged from 79.9 years (Native Americans) to 81.3 years (whites). Years of life lost (YLL) for the median miner were 13.3 (whites) and 13.9 (Native Americans). For additional information on miner characteristics (e.g., birth year, smoker, cumulative radon exposure, etc.) see Table 1 in Schubauer-Berigan et al. (2009).
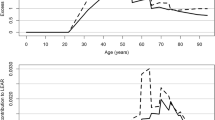
A total of 697.2 elevated deaths occurred—625 whites and 72.2 Native Americans—out of a total of 2964 observed deaths in the cohort of 3358 white and 779 Native American men. Excess mortality averaged 16,852.8 per 100,000 miners over 1960–2005 (white: 18,612.3 per 100,000; Native American: 9,268.3 per 100,000) or 366.4 per 100,000 miners annually (white: 404.6 per 100,000; Native American: 201.5 per 100,000).
PYLL were 2475.3 person-years per 1000 white miners and 1288.1 person-years per 1000 Native American miners, totaling 3763.4 person-years per 1000 miners across both groups (Table 2). Lung cancer PYLL are largest across both groups, constituting approximately 67% of observed person-years lost in the miner cohort. For whites, cause of death due to COPD was the second largest category of PYLL (403.3 person-years per 1000), while for Native Americans pulmonary fibrosis (157.9 person-years per 1000) was the second largest source of person-years lost. PYLL were lowest for silicosis among Native American miners (102.7 person-years per 1000) and lowest for acute glomerulonephritis and acute renal failure among white miners (16.3 person-years per 10,000). On average, 81.8 person-years per 1000 miners were lost annually (white: 53.8 person-years; Native American: 28.0 person-years per 1000).
Mortality health costs associated with miner PYLL vary considerably by cause of death (Table 2). Lung cancer mortality has created $1.4 billion in health costs ($1.24 billion for whites; $127.9 million for Native Americans) among Colorado Plateau study miners over 1960–2005. The corresponding 95% confidence intervals (CI) are $1.2–$1.39 billion (whites) and $110.4–$140.7 million (Native Americans). Mortality costs associated with other causes of death range from $11.6 million (acute glomerulonephritis and acute renal failure) to $288.5 million (COPD). Total mortality health costs for whites were $1.8 billion [95% CI: $1.6–$2.0 billion] and $213.7 million for Native Americans [95% CI: $159.7–$243.9 million]: a percentage difference in costs of 157%. For both groups combined, costs total approximately $2 billion [95% CI: $1.8–$2.2 billion], or $2.9 million per elevated miner death. This corresponds to an average of $43.1 million in annual health costs over 1960–2005.
Discussion
The paper investigates mortality health costs of 4137 uranium miners in the USPHS Colorado Plateau study cohort over 1960–2005. Previously published estimates of elevated mortality risk in the cohort were appropriately combined with the value of a statistical life-year (VSLY) to independently estimate occupationally related health costs for this group.
The present study expands upon the only previous uranium health cost analysis (Jones 2014) in the following ways. First, the study area is significantly expanded to be representative of miners working in the Colorado Plateau, the largest uranium producing region in the US. Second, health costs for over a dozen new cause of death categories are estimated for the first time, consistent with recent research on Colorado Plateau miners (Schubauer-Berigan et al. 2009). Third, Native American uranium miners are included, an addition to previously studied white miners. Finally, we take as our study group the US Public Health Service (USPHS) Colorado Plateau prospective cohort study, a highly influential long-term study of uranium miners in the western US.
Consistent with the extant research on underground uranium mining (Duan et al. 2015), we find that lung cancer is the most significant health effect among both white and Native American Colorado Plateau miners. We show for the first time that lung cancer accounts for over 67% of estimated total health costs associated with mining, or 70% of total costs among whites and 60% of total costs among Native Americans.
Native American miners had 6.9% larger per excess death mortality health costs than white miners. Among Native Americans, health costs were $3 million per elevated death compared to $2.8 million per elevated death for whites. This is because white miners had fewer average YLL than Native American miners. This provides the first suggestive evidence that the economic costs of lost Native American uranium miners is larger than whites on a per death basis.
Native American miners faced fewer occupationally related diseases than whites. Out of the nine cause of death categories investigated, elevated mortality risk was insignificant for four categories among Native Americans (lymphohematopoietic cancers, multiple myeloma, COPD, and acute glomerulonephritis and acute renal failure), compared to only one category (stomach cancer) for whites. Consequently, mortality health costs for Native Americans are driven by a narrower range of diseases and illnesses. When we compare total health costs across whites and Native Americans for only those causes of death that were elevated in both groups (i.e., lung cancer, silicosis, pulmonary fibrosis, and tuberculosis), we find that total health costs are $1.4 billion (whites) and $195.3 million (Native Americans): a difference in costs of 151%, compared to the previously presented 157% difference when all elevated causes of death were included and not just those that overlapped.
Our results suggest that the social costs of uranium mining in the Colorado Plateau fell disproportionally on Native American underground miners. The vast majority of these miners were Navajos (Roscoe et al. 1995), which is a group of Native Americans who have a long and controversial history with uranium mining (Brugge and Goble 2002). Future mining operations on the Colorado Plateau (or elsewhere) might benefit from considerations of uranium’s disproportionate impacts on indigenous populations.
Overall, the results suggest that mortality health costs to society of the Colorado Plateau study uranium miners are $2 billion, or $2.9 million per elevated miner death, on average. We estimate from the US Bureau of Mines, Minerals Yearbook (US Bureau of Mines 1950–1960) that 11,786 uranium miners worked on the Colorado Plateau over 1950–1960 and had >1 month work experience when the cohort study was being populated [see Jones (2014) for more on estimation techniques of uranium miner populations]. Assuming that the 4137 miners in the cohort study were an average representation of the 11,786 uranium miners on the Colorado Plateau, then a total of 1992 elevated miner deaths would be expected between 1960 and 2005. Based on our cost estimate of $2.9 million per elevated death in this study, it follows that mortality health costs across all Plateau miners working in the 1950s or 1960s would total $5.8 billion, or $125.6 million per year over 1960–2005. Given that an estimated 137 million pounds of uranium oxide were produced in the US over 1950–1960 (US 2012), we conclude that for every pound of uranium oxide produced, $42.34/lb. of long-term mortality health costs were created. This is an important key insight provided by this study and compares to an average contract price of uranium oxide of $86.49/lb. over 1950–1960.
This is only the second study of uranium miner mortality health costs. Our results are conservative in comparison to the other study by Jones (2014), which estimated costs of $4.4 million per elevated lung cancer death in New Mexico, USA. The difference in results appears to be driven by heterogeneity in average YLL. New Mexico miners had almost double the average YLL compared to Colorado Plateau miners. This may be a function of the fact that New Mexico miners worked underground 8 years longer, on average, than Plateau study miners, increasing their mortality risk (Roscoe 1997; Samet et al. 1989). However, New Mexico miners generally had lower radon exposures than other miners (Samet et al. 1991), suggestive that duration underground may only be capturing some of the observed difference in cost estimates across the two studies. We leave it to future work to explore this issue.
There are several limitations of this study. First, there is evidence of a submultiplicative interaction between smoking and radon-induced lung cancer (Tomasek 2013; Schubauer-Berigan et al. 2009). It is possible that smoking might be a strong confounder of the previously published mortality risks used in this study. This concern has been consistently raised and evaluated in the radon literature—see Duan et al. (2015) for a meta-analysis. The evidence strongly suggests that the relationship between radon exposure and risk of lung cancer does not significantly vary based on smoking habits among occupationally exposed populations (Duan et al. 2015; Tomasek 2013; Siemiatycki et al. 1988; Samet et al. 1984). Thus, mortality health costs estimated in this study are unlikely to be significantly affected. Second, it is unclear if the Colorado Plateau cohort is representative of other uranium miners working in the western US. Roscoe (1997) reports that while uranium miners’ participation rates in the USPHS medical interviews were lower before 1954, the 1957 and 1960 surveys captured 90% of the miners in the areas visited. Selection bias might exist if the mines selected for visit by the USPHS systematically differed from others in the region. Cost results could suffer from upward (downward) bias if selected mines employed miners with greater (lesser) radon exposure than the average Colorado Plateau miner. Third, the cost estimates presented here represent the lower-bound of total health costs associated with Colorado Plateau miners. Healthcare costs borne by individual miners, their families, or taxpayers (through government subsidized health insurance) were not included in the study. These costs are not always trivial. Lifetime medical treatment costs for lung cancer, for example, average $236,000 per diagnosed patient (Mariotto et al. 2011). Inclusion of healthcare costs in miner health cost studies is a potential area for future research.
Conclusions
Globally, there is renewed interest in uranium as a source of low-carbon, renewable energy due to climate change concerns, as well as international and bi-lateral climate agreements (e.g., COP21, US-China Joint Announcement on Climate Change, etc.). For example, in the Colorado Plateau several new uranium mines and one processing mill are currently under development, including one mine adjacent to the Grand Canyon National Park and another in New Mexico that if built would be the largest uranium mine in the US (US EIA 2015; Hartranft 2013, May 19).
The human health costs of past uranium mining are not trivial. The main finding of this work is that past Colorado Plateau mining resulted in $43.1 million in annual health costs among a cohort of 3358 white and 779 Native American men over 1960–2005, equivalent to $10,418 per miner per year. Health costs were largest per excess death among Native American miners. These result are likely a lower-bound on the full range of health costs of uranium mining since they do not include uncertain medical costs. These findings are relevant factors to consider when setting national and even global nuclear policy, given growing international literature on uranium’s non-monetary and monetary societal costs.
References
Advisory Committee on Human Radiation Experiments (1995) Final Report. US Government Printing Office, Washington, DC
Aldy JE, Viscusi WK (2008) Adjusting the value of a statistical life for age and cohort effects. Rev Econ Stat 90:573–581
Al-Zoughool M, Krewski D (2009) Health effects of radon: a review of the literature. Int J Radiat Biol 85:57–69
Archer VE, Gillam JD, Wagoner JK (1976) Respiratory disease mortality among uranium miners. Ann N Y Acad Sci 271:280–293
Boice JD, Cohen SS, Mumma MT, Chadda B, Blot WJ (2008) A cohort study of uranium millers and miners of Grants, New Mexico, 1979–2005. J Radiol Prot 28:303
Brugge D, Goble R (2002) The history of uranium mining and the navajo people. Am J Public Health 92:1410–1419
Chmura Economics & Analytics (2011) The Socioeconomic Impact of Uranium Mining and Milling in the Chatham Labor Shed, Virginia. Richmond, Virginia: Chmura Economics & Analytics. http://lis.virginia.gov/111/oth/Uranium.120611.pdf. Accessed 1 Feb 2016
Cutler DM, Gruber J, Hartman RS, Landrum MB, Newhouse JP, Rosenthal MB (2002) The economic impacts of the tobacco settlement. J Pol Anal Manage 21:1–19
Donaldson AW (1969) The epidemiology of lung cancer among uranium miners. Health Phys 16:563–569
Duan P, Quan C, Hu C, Zhang J, Xie F, Hu X et al (2015) Nonlinear dose–response relationship between radon exposure and the risk of lung cancer: evidence from a meta-analysis of published observational studies. Eur J Cancer Prev 24:267–277
Hartranft M (2013, May 19) Nation’s largest uranium mine planned for N.M. Albuquerque Journal. http://www.abqjournal.com/200845/news/nations-largest-uranium-mine-planned-for-nm.html. Accessed 1 Feb 2016
Hendryx M, Ahern MM (2009) Mortality in Appalachian coal mining regions: the value of statistical life lost. Public Health Rep 124:541–550
Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (2016) (eds). SEER cancer statistics review, 1975–2012, National Cancer Institute. Bethesda, MD. http://seer.cancer.gov/csr/1975_2012/. Accessed 1 Feb 2016
IAEA (2015) Climate Change and Nuclear Power 2015. Vienna, Austria: International Atomic Energy Agency. http://www-pub.iaea.org/MTCD/Publications/PDF/CCANP2015Web-78834554.pdf Accessed 1 Feb 2016
Jones BA (2014) What are the health costs of uranium mining? A case study of miners in Grants, New Mexico. Int J Occup Environ Health 20:289–300
Kniesner TJ, Viscusi WK, Woock C, Ziliak JP (2012) The value of a statistical life: Evidence from panel data. Rev Econ Statist 94:74–87
Lundin FE, Wagoner JK, Archer VE (1971) Radon daughter exposure and respiratory cancer quantitative and temporal aspects. NIOSH and NIEHS Joint Monograph No. 1. National Technical Information Service, Springfield
Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML (2011) Projections of the cost of cancer care in the United States: 2010–2020. J Natl Cancer Inst 103:117–128
Mishan E, Quah E (2007) Cost-benefit analysis, 5th edn. Routledge, New York
Murphy KM, Topel RH (2006) The value of health and longevity. J Polit Econ 114:871–904
National Center for Health Statistics (1990) United States Life Tables. Hyattsville, MD: Department of Health and Human Services Centers for Disease Control and Prevention
National Center for Health Statistics (1992) United States Life Tables. Hyattsville, MD: Department of Health and Human Services Centers for Disease Control and Prevention
National Research Council (2012) Uranium mining in virginia: scientific, technical, environmental, human health and safety, and regulatory aspects of uranium mining and processing in virginia. The National Academies Press, Washington DC. http://dls.virginia.gov/commissions/cec/files/NAS_study.pdf. Accessed 1 Feb 2016
NIOSH (1987) A Recommended Standard for Occupational Exposure to Radon Progeny in Underground Mines (DHHS (NIOSH) Publication No. 88–101). US Government Printing Office, Washington DC
Rage E, Caër-Lorho S, Drubay D, Ancelet S, Laroche P, Laurier D (2015) Mortality analyses in the updated French cohort of uranium miners (1946–2007). Int Arch Occup Environ Health 88:717–730
Ringholz RC (1989) Uranium Frenzy. W.W. Norton, New York
Robinson LA (2007) Policy monitor how US Government agencies value mortality risk reductions. Rev Environ Econ Policy 1:283–299
Roscoe RJ (1997) An update of mortality from all causes among white uranium miners from the Colorado Plateau Study Group. Am J Ind Med 31:211–222
Roscoe RJ, Steenland K, Halperin WE, Beaumont JJ, Waxweiler RJ (1989) Lung cancer mortality among nonsmoking uranium miners exposed to radon daughters. JAMA 262:629–633
Roscoe RJ, Deddens JA, Salvan A, Schnorr TM (1995) Mortality among Navajo uranium miners. Am J Public Health 85:535–540
Samet JM, Kutvirt DM, Waxweiler RJ, Key CR (1984) Uranium mining and lung cancer in Navajo men. N Engl J Med 310:1481–1484
Samet JM, Pathak DR, Morgan MV, Marbury MC, Key CR, Valdivia AA (1989) Radon progeny exposure and lung cancer risk in New Mexico U miners: a case-control study. Health Phys 56:415–421
Samet JM, Pathak DR, Morgan MV, Lubin JH, Valdivia AA, Key CR (1991) Lung cancer mortality and exposure to radon progeny in a cohort of New Mexico underground uranium miners. Health Phys 61:745–752
Schubauer-Berigan MK, Daniels RD, Pinkerton LE (2009) Radon exposure and mortality among white and American Indian uranium miners: an update of the Colorado Plateau cohort. Am J Epidemiol 169:718–730
Siemiatycki J, Wacholder S, Dewar R, Cardis E, Greenwood C, Richardson L (1988) Degree of confounding bias related to smoking, ethnic group, and socioeconomic status in estimates of the associations between occupation and cancer. J Occup Environ Med 30:617–625
Tirmarche M, Harrison J, Laurier D, Blanchardon E, Paquet F, Marsh J (2012) Risk of lung cancer from radon exposure: contribution of recently published studies of uranium miners. Ann ICRP 41:368–377
Tolley G, Kenkel D, Fabian R (1994) Valuing health for policy: an economic approach. University of Chicago Press, Chicago
Tomasek L (2013) Lung cancer risk from occupational and environmental radon and role of smoking in two Czech nested case-control studies. Int J Environ Res Public Health 10:963–979
US EPA (2010) Valuing mortality risk reductions for environmental policy: a white paper (Draft). US EPA National Center for Environmental Economics, Washington DC. http://yosemite.epa.gov/ee/epa/eerm.nsf/vwAN/EE-0563-1.pdf/$file/EE-0563-1.pdf. Accessed 1 Feb 2016
US EIA (2012) Annual Energy Review 2011 (DOE/EIA-0384(2011)). US Energy Information Administration, Washington, DC. https://www.eia.gov/totalenergy/data/annual/showtext.cfm?t=ptb0903. Accessed 1 Feb 2016
US EIA (2015) 2014 Domestic Uranium Production Report. US Energy Information Administration, Washington DC. http://www.eia.gov/uranium/production/annual/pdf/dupr.pdf. Accessed 1 Feb 2016
US Bureau of Mines (1950–1960) Minerals Yearbook. US Government Printing Office, Washington DC
Viscusi WK, Aldy JE (2003) The value of a statistical life: a critical review of market estimates throughout the world. J Risk Uncertain 27:5–76
Waxweiler RJ, Roscoe RJ, Archer VE, Thun MJ, Wagoner JK, Lundin FE (1981) Mortality follow-up through 1977 of the white underground uranium miners cohort examined by the United States Public Health Service. In Gomez, M. (ed.): Radiation Hazards in Mining. Society of Mining Engineers, AIME. Kingsport Press, Kingsport, Tennessee, pp 823–830
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Funding
This work was not supported by external or internal funding.
Conflict of interest
The authors have had no competing interests, financial interests, or benefits arising from this research.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jones, B.A. The social costs of uranium mining in the US Colorado Plateau cohort, 1960–2005. Int J Public Health 62, 471–478 (2017). https://doi.org/10.1007/s00038-017-0943-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00038-017-0943-z