Abstract
Objectives
To review existing cardiovascular risk models applicable to South Asian populations.
Methods
A systematic review of the literature using a combination of search terms for “South Asian”, “cardiovascular”, “risk”/“score” and existing risk models for inclusion. South Asian was defined as those residing in or with ancestry belonging to the Indian subcontinent.
Results
The literature search including MEDLINE and EMBASE identified 7560 papers. After full-text review, 4 papers met the inclusion criteria. Only 1 reported formal measures of model performance. In that study, both a modified Framingham model and QRISK2 showed similar good discrimination with AUROCs of 0.73–0.77 with calibration also reasonable in men (0.71–0.93) but poor in women (0.43–0.52).
Conclusions
Considering the number of South Asians and prevalence of cardiovascular disease, very few studies have reported performance of risk scores in South Asian populations. Furthermore, it was difficult to make comparisons, as many did not provide measures of discrimination, accuracy and calibration. There is a need for further research to evaluate risk models in South Asians, and ideally derive and validate cardiovascular risk models within South Asian populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite advances in diagnosis, treatment and prevention of cardiovascular disease (CVD) in recent decades, CVD still remains the single largest cause of non-communicable disease death worldwide (WHO 2014). Individuals who are of South Asian descent make up one in five of the world’s population and are at particular risk of CVD (Turin et al. 2013). Compared to Caucasian populations, South Asians have an increased prevalence of established risk factors, such as hyperlipidaemia, smoking and limited physical activity, at younger ages (Joshi et al. 2007; Misra and Khurana 2011; Prasad et al. 2011); are younger on admission with ischaemic stroke and have poorer 30-day survival (Gunarathne et al. 2008); have an increased risk of 30-day mortality from re-infarction or heart failure; and those with type-2 diabetes mellitus are affected by cardiovascular events 7.4 years before their Caucasian counterparts (Bellary et al. 2010).
The incidence and prevalence of CVD are also continuing to increase in South Asian populations. Over the last 20 years, the prevalence of coronary heart disease has increased twofold in India alone (Turin et al. 2013) and the associated global CVD adult burden in developing countries and increasing costs of hospitalisation on local workforces (Srivastava and Mohanty 2013) are reasons for concern (Prasad et al. 2011).
Attempts to reduce this excess morbidity and mortality include collective approaches targeting the wider underlying risk factors in an attempt to shift the entire population distribution of CVD risk, and approaches that focus on identification of individuals at high risk. A key part of the latter approach is the use of risk models that enable estimation of an individual’s risk of developing CVD. These have the potential to help clinicians with decisions regarding treatment, facilitate an informed discussion between clinician and patient, and may also motivate individuals to improve their health-related behaviours. They also provide an opportunity to prioritise individuals with the highest CVD risk and so allocate resources more efficiently.
A number of risk models capable of identifying those at high risk of CVD exist, however most have been developed in Caucasian populations and, given the role of population ethnicity and region in modifying cardiovascular risk (Beswick and Brindle 2006), it is not clear which is currently the most appropriate for people of South Asian descent. The aim of this research was to systematically review and compare existing cardiovascular risk models validated in adult South Asian populations to inform the choice of risk model in these populations.
Methods
Search strategy
An electronic literature search of MEDLINE, EMBASE (Excerpta Medica dataBASE), HMIC (Health Management Information Consortium), AMED (Allied and Complementary Medicine Database) and PsychINFO from January 2000 to April 2014 was performed using a combination of medical subject heading (MESH) terms and free text incorporating “South Asian”, “cardiovascular”, “risk”/“score” and specific risk models for inclusion (see Supplementary material for complete search strategy). The search was restricted to human studies. Duplicates were removed and the references of each included paper were screened manually for additional studies.
Study selection
Studies were included if they fulfilled all the following criteria: (1) a primary research paper published in a peer-reviewed journal; (2) contain details of a cardiovascular risk model; (3) apply a cardiovascular risk model to one or more subgroups of a South Asian population where South Asian is defined as originating from the Indian subcontinent—India, Pakistan, Bangladesh, Nepal, Bhutan, Sri Lanka; (4) include persons greater than and including the age of 18; (5) include a defined end-point such as 5-year all-cause mortality or overall lifetime cardiovascular risk. Studies focussing on sole ethnic groups that did not fall under the bracket of “South Asian” and studies with participants with a history of CVD or using cardiovascular risks models to estimate disease prevalence or incidence were excluded. Abstracts presented at conferences were also excluded.
One reviewer (DG) performed the search and screened the articles to exclude those that were clearly not relevant to assessment of cardiovascular risk at title and abstract level, whilst a second reviewer (JUS) independently assessed 5 % of articles excluded at this stage. Both reviewers independently examined all full texts where an article could not be rejected purely at title and abstract level. Those articles that did not fulfil inclusion criteria by both reviewers were excluded. Any discrepancies around whether articles fulfilled inclusion criteria were discussed at consensus meetings.
Data extraction and synthesis
Data were extracted independently by both researchers using a standardised form to decrease recording bias. The form included details on: (1) the risk model itself, including availability on the internet and risk model variables included; (2) model development, including study location, study years, study design, model development method, variables included in the model and model performance in the study population such as discrimination, calibration, accuracy where applicable; (3) external validation of the model on a study population, including study location, study years, study design, and model performance in the study population such as discrimination, calibration, accuracy where applicable.
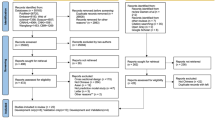
Results
After removing duplicate records, the search isolated 7560 articles. 7486 were excluded at title and abstract level with a further 70 records excluded after full-text assessment (Fig. 1). Full concordance was reached between researchers during screening and a large proportion of articles were excluded because they had used risk scores only to estimate prevalence or incidence of CVD or were conference abstracts. A small number were also excluded because they were specific to patients with thyroid carcinoma or renal transplantation and so not applicable to the general population, the model was used to predict in-hospital mortality or the article was not available online or from the British Library. Further reference list searching and wider reading did not identify any extra papers that warranted inclusion in addition to the wider search results. Only 4 papers (Guha et al. 2004; Jaquet et al. 2008; Bellary et al. 2010; Tillin et al. 2014) fulfilled the inclusion criteria. Details of the design and methods of these four studies are shown in Table 1. Two are based in the UK, one in Guadeloupe and one in India. Two included only patients with diabetes (Bellary et al. 2010; Jaquet et al. 2008) and all used different outcome measures: Guha et al. included only acute coronary syndrome; Tillin et al. included angina, stroke and TIA in addition to myocardial infection and coronary heart disease; Bellary et al. and Jaquet et al. included all fatal and non-fatal cardiovascular events. Whilst the aim in all 4 was to assess the performance of CVD risk models in South Asian populations, the design of the studies also differed with Guha et al. using a case–control design with patients recruited in secondary care and the other three using a cohort design with follow-up of between 2 and 10 years.
Between them, the four studies included details on the performance of four cardiovascular risk models in adult South Asian populations. These are summarised in Table 2 along with the main results from each study. They include the Framingham model developed from 5573 participants in the USA between 1968 and 1975 (Anderson et al. 1991), a modified version of the Framingham model (NICE 2008), the UKPDS developed in the UK between 1977 and 1991 in patients with known type 2 diabetes (Stevens et al. 2001) and QRISK2 developed from the electronic primary health care records of 2,290,000 patients registered with GPs in the UK (Hippisley-Cox et al. 2008). All 4 include a set of 4 common risk factors (age, gender, smoking history, systolic blood pressure). The Framingham model includes an additional 5 risk factors (diastolic blood pressure, total cholesterol, HDL cholesterol, left ventricular hypertrophy, diabetes), the UKPDS an additional 3 (total: HDL cholesterol ratio, HbA1C and ethnicity) and QRISK2 11 extra factors, including both variables related to biological disease development and others, such as social deprivation, that may be markers of other determinants of disease in general (total: HDL cholesterol ratio, antihypertensive use, essential hypertension, chronic kidney disease, body mass index, social deprivation, family history of ischaemic heart disease in first-degree relative aged below 60 years, ethnicity, type 2 diabetes, rheumatoid arthritis, and atrial fibrillation). In total, 20 different factors were used across the 4 different risk models with the UKPDS using 7 factors and the modified Framingham and Framingham 10-year models were composed of 9 components, whilst the QRISK2 was made up using 15 factors. All are available online with the exception of the modified Framingham risk model which requires multiplication of the online Framingham score by a factor of 1.4 for men.
The Framingham 10-year risk model was used in 3 papers (Guha et al. 2004; Jaquet et al. 2008; Bellary et al. 2010). Guha et al. (2004) used a case–control design to compare the 10-year Framingham risk model in patients presenting with acute coronary syndrome (ACS) and controls with no history of CVD and a normal ECG. They then divided both cases and controls into those with and without diabetes and based on the calculated 10-year risk, grouped them into high risk (>20 %), moderately high risk (10–20 %) and low risk (<10 %). They found a statistically significant difference in the mean projected risk between cases and controls without diabetes (mean 10-year risk 14.15 for cases and 8.61 for controls, p < 0.01), but no difference amongst those with diabetes (mean 10-year risk 11.37 for cases and 10.41 for controls, p = NS). Although the distribution of risk was higher in those who developed ACS, use of the Framingham 10-year risk score prior to developing ACS would have underestimated CVD risk: only 20 % of those without diabetes and 14 % of those with diabetes would have been identified as high risk and 41 and 53 % would have been classified as low risk, respectively.
Jaquet et al. (2008) used data from a Guadeloupian retrospective cohort study to compare the Framingham 10-year risk model and metabolic syndrome as potential predictors of fatal or non-fatal coronary heart disease, ischaemic or haemorrhagic stroke or peripheral vascular disease in 148 Indian patients with impaired glucose tolerance or type-2 diabetes. Using Cox proportional hazards modelling, they found that higher Framingham risk scores at baseline were associated with cardiovascular events at 9-year follow-up but this effect was greater for scores ≥10 % than ≥20 % (hazard ratio 4.78 (95 % CI 1.65–13.5) for a risk score ≥10 %, and 2.94 (95 % CI 1.42–6.06) for a risk score ≥20 %).
The third study to use the Framingham risk model was Bellary et al. (2010) who used data from the United Kingdom Asian Diabetes Study (UKADS) cohort (Bellary et al. 2008) to compare the Framingham 10-year risk and UKPDS 10-year risk in 1140 British South Asians and 317 Caucasians with established type-2 diabetes over a 2-year period. For both Framingham and UKPDS risk models they observed a trend for increased CVD events with increasing risk score in the South Asian group. However, despite similar predicted CVD risk in the South Asian and Caucasian groups (Framingham 10-year females: 7.3 vs 6.5, males: 11.7 vs 11.7; UKPDS 10-year females: 10.8 vs 10.1, males 21.9 vs 22.6), over the 2-year period there were substantially more cardiovascular events in the South Asian group (26.10 per 1000 person-years for South Asians vs 19.29 for Caucasians) suggesting that both models underestimated risk in the South Asian group.
The fourth study by Tillin et al. (2014) compared the performance of a modified Framingham 10-year model (derived by multiplying the Framingham risk by 1.4 for South Asian men and recommended by the NICE guidelines in 2008 (NICE 2008)) and QRISK2 10-year score in a tri-ethnic cohort including 1317 South Asians with 10-year CVD event follow-up. They chose the same end-points as for QRISK2 (first myocardial infarction, angina, CHD, stroke, transient ischaemic attack) for assessment of both QRISK2 and the modified Framingham 10-year model which was initially developed with only CHD as an end-point which would be expected to favour performance of the QRISK2. They also did not have data on presence or absence of rheumatoid arthritis, chronic kidney disease or atrial fibrillation at baseline and only had data on family history of CHD for survivors at 20-year follow-up and left ventricular hypertrophy in a subset and so assumed null values for these variables when calculating the risk scores. Despite these limitations, it is the only study to provide statistical measures of model performance. For South Asians, there was little difference in the discriminatory performance of the two models with both having moderate discrimination and better in females than males: the modified Framingham model had an area under receiver operator curve (AUROC) of 0.73 for males and 0.77 for females and QRISK2 an AUROC of 0.73 for males, 0.75 for females; and the R 2 statistic was also similar for the modified Framingham score (males 26.6 %, females 37.6 %) and QRISK2 model (males 26.3 %, females 36.4 %). Both under-predicted risk with the modified Framingham model better calibrated in men compared to the QRISK2 (predicted: observed (95 % CI) modified Framingham 0.93 (0.88–0.96) vs QRISK2 0.71 (0.64–0.78)) and QRISK 2 better in women (predicted: observed QRISK2 0.52 (0.32–0.72) vs modified Framingham 0.43 (0.25–0.63)). Overall performance, as measured by the Brier M statistic, was moderate and almost identical for both models with values of 0.14 and 0.10 for South Asian males and females, respectively.
Discussion
Despite the increasing use of cardiovascular risk models and recognition of the impact of ethnicity on CVD risk, this systematic review identified only 4 studies that assessed the performance of risk models in South Asian populations. All showed that an increased risk score was associated with increased CVD events, and 3 of the 4 risk models underestimated risk in South Asian populations. Only 1 reported formal measures of model performance. In that study (Tillin et al. 2014), both a modified Framingham model and QRISK2 showed similar good discrimination with AUROCs of 0.73–0.77 with calibration also reasonable in men (0.71–0.93) but poor in women (0.43–0.52).
Strengths and limitations
The main strength of this study is the systematic approach and use of different search engines, including EMBASE and MEDLINE, as well as manual screening of the reference lists of included articles. However, there is an element of publication bias that is intrinsic to the literature limiting available analysable data sets, so we cannot exclude the possibility that there are other studies that we did not identify.
The main weaknesses relate to the volume and quality of the published data. The results of the widespread search found only 4 studies using 4 risk models. All used different outcome measures, only 1 reported statistical measures for performance, and only the Framingham model was assessed in more than one study so the conclusions that can be drawn from the extracted data are limited. Additionally, the populations included in the studies are of limited generalisability: two included only participants with type 2 diabetes and one only those presenting to one secondary care hospital. Although unlikely to have a large effect, the only study to include performance measures (Tillin et al. 2014) also had missing data for several of the component risk factors for each model. Furthermore, of the studies included, only two specified the subgroups of South Asians within their study (Jaquet et al. 2008; Tillin et al. 2014), whilst the other two described the included population as only ‘South Asian’ (Bellary et al. 2010) or ‘Indian’ (Guha et al. 2004). This makes interpreting and applying the results to specific subgroups more difficult. Finally, there was a lack of reporting of consistent measures of discrimination, calibration and accuracy making a comparison between risk models difficult.
Implications for clinicians and policy makers
Despite these limitations, the findings from this review are of relevance to the large number of clinicians worldwide that use CVD risk information with South Asian patients regularly in their practice, and policy makers involved in designing and implementing strategies for the prevention of CVD. Given the widespread use of CVD risk models and the increasing South Asian population (UN 2014), it is surprising and concerning that there is such limited data on the performance of these models in South Asian populations. Only 4 risk models have been tested and performance data are only available for 2. Increased risk scores in all 4 models are associated with increased CVD events, but, where reported, all underestimate risk. This underestimation is perhaps not surprising for the Framingham risk model as it was developed in a cohort of white Caucasian individuals from the late 1960s onwards (Anderson et al. 1991) and, along with other risk models, is commonly believed to underestimate CVD risk when applied to 1990s and 2000s South Asian populations (Kanjilal et al. 2008; Bansal et al. 2009; Perumal et al. 2012; Khanna et al. 2013) and when compared to expected mortality rates amongst South Asians (Cappuccio et al. 2002; Quirke et al. 2003; Aarabi and Jackson 2005; Bhopal et al. 2005; Brindle et al. 2006; Wells et al. 2007; Kumar et al. 2009; Perumal et al. 2012). QRISK2, however, was derived using a large South Asian population (n = 17,102) (Hippisley-Cox et al. 2008) and so would be expected to take account of differences in intrinsic CVD risk amongst South Asians. Nevertheless, the performance of QRISK2 and the modified Framingham model in South Asian populations are not dissimilar from those in white Caucasians or other ethnic groups: in the study by Tillin et al. (2014), the AUROC and R 2 statistic for both risk models were higher in South Asians than Europeans or African Caribbeans or all ethnicities combined for both men and women. The notable difference is in South Asian females where both QRISK2 and the modified Framingham model underestimate risk substantially more than for other ethnic groups (predicted: observed 0.52 (95 % CI 0.34–0.72) for QRISK2 and 0.43 (95 % CI 0.25–0.63) for modified Framingham compared to 0.73 (0.57–0.88) and 0.74 (0.57–0.88), respectively, in Europeans), and the QRISK2 high-risk classification would miss approximately two-thirds of events. This may be explained by the absence of any incident cases in South Asian women in the Framingham model development population (compared to 241 in white Caucasian women) and the small number of incident cases in South Asian women in the QRISK2 derivation dataset relative to those in the White ethnic group (413 compared to 40,278). This underestimation is important though for clinicians to recognise as women often do not present with typical symptoms before or during a cardiovascular event (McSweeney et al. 2003, 2010) and alternative strategies may be required to identify high-risk South Asian women.
When choosing which model to use, clinicians should be aware that both QRISK2 and a modified Framingham model have been externally tested in South Asian populations and both have similar modest discrimination and overall performance but underestimate risk, particularly in South Asian women. The choice of which to use can therefore be guided by access, availability of risk factors, and local preferences. Both QRISK2 and the Framingham model are freely accessible on the internet but, whilst QRISK2 includes an option for ‘South Asian’, when using the Framingham model in South Asians clinicians would need to multiply the calculated risk by 1.4 for men before interpreting it. This is not difficult but adds a further step into risk calculation and limits the use of the Framingham model to screen electronic records. QRISK2 includes 15 variables compared to the 9 in the Framingham score. Age, gender, systolic BP, total cholesterol, HDL, smoking status and diabetes are risk factors common to both scores with the Framingham model additionally including left ventricular hypertrophy and QRISK2 body mass index, family history, social deprivation, antihypertensive treatment, ethnicity, hypertension, rheumatoid arthritis, chronic kidney disease and atrial fibrillation. Some of these additional variables in the QRISK2 model may not be readily known, however, in the validation study (Tillin et al. 2014), data were also not available for rheumatoid arthritis, chronic kidney disease, atrial fibrillation or left ventricular hypertrophy and family history data was missing for many participants so this may have limited consequences. Both are also recommended in current guidelines but these differ between countries with the UK National Institute for Health and Clinical Excellence (NICE) currently recommending QRISK2 (NICE 2015) and the American College of Cardiology suggesting the Framingham risk model or SCORE guidelines (Conroy et al. 2003) based on validation in Afro-Caribbeans (Goff et al. 2014).
Unanswered questions and future research
Whilst this review provides a summary of published studies reporting the performance of CVD risk models in South Asian populations, it also highlights the lack of evidence in this area. Given the increasing incidence of CVD and reliance on risk prediction tools for treatment decisions, there is the need for further research in this area. This includes both wider validation of existing risk models, such as ETHRISK which is another modified version of the Framingham risk model designed to take account of ethnicity (Brindle et al. 2006), and the development of new models incorporating ethnicity to reduce the intrinsic difficulties when applying a risk model developed in one ethnicity to a different ethnicity in a different location and point in time. This work will also need to address the difficulties involved in developing risk models for South Asians where the umbrella term ‘South Asian’ includes persons with different levels of acculturation, different migration patterns and different ethnic subgroups, both within and outside the Indian subcontinent.
In the past, this has been limited by the lack of studies including South Asian populations but with the development of large cohorts such as the Emerging Risk Factors Collaboration (Danesh et al. 2007; Thompson et al. 2010) and UK Biobank (Elliott and Peakman 2008; Kaptoge et al. 2012) and the increasing availability of electronic medical record databases, it should now be possible to validate existing models and develop new ones. Only once we have an accurate risk model for South Asian populations, will we be able to maximise the potential benefits of a calibrated CVD risk assessment and directed primary preventive strategies for this group who make up 1 in 5 of the ever-expanding world population.
References
Aarabi M, Jackson PR (2005) Predicting coronary risk in UK South Asians: an adjustment method for Framingham-based tools. Eur J Cardiovasc Prev Rehabil 12:46–51. doi:10.1097/01.hjr.0000159279.88814.aa
Anderson K, Odell P, Wilson P, Kannel W (1991) Cardiovascular disease risk profiles. Am Heart J 121:293–298. doi:10.1016/0002-8703(91)90861-B
Bansal M, Shrivastava S, Mehrotra R et al (2009) Low Framingham risk score despite high prevalence of metabolic syndrome in asymptomatic North-Indian population. J Assoc Physicians India 57:17–22
Bellary S, O’Hare JP, Raymond NT et al (2008) Enhanced diabetes care to patients of south Asian ethnic origin (the United Kingdom Asian Diabetes Study): a cluster randomised controlled trial. Lancet 371:1769–1776. doi:10.1016/S0140-6736(08)60764-3
Bellary S, O’Hare JP, Raymond NT et al (2010) Premature cardiovascular events and mortality in south Asians with type 2 diabetes in the United Kingdom Asian Diabetes Study—effect of ethnicity on risk. Curr Med Res Opin 26:1873–1879. doi:10.1185/03007995.2010.490468
Beswick A, Brindle P (2006) Risk scoring in the assessment of cardiovascular risk. Curr Opin Lipidol 17:375–386. doi:10.1097/01.mol.0000236362.56216.44
Bhopal R, Fischbacher C, Vartiainen E et al (2005) Predicted and observed cardiovascular disease in South Asians: application of FINRISK, Framingham and SCORE models to Newcastle Heart Project data. J Public Health (Oxf) 27:93–100. doi:10.1093/pubmed/fdh202
Brindle P, May M, Gill P et al (2006) Primary prevention of cardiovascular disease: a web-based risk score for seven British black and minority ethnic groups. Heart 92:1595–1602. doi:10.1136/hrt.2006.092346
Cappuccio FP, Oakeshott P, Strazzullo P, Kerry SM (2002) Application of Framingham risk estimates to ethnic minorities in United Kingdom and implications for primary prevention of heart disease in general practice: cross sectional population based study. BMJ 325:1271–1274. Erratum BMJ. 2003 327(7420):919. doi:10.1136/bmj.325.7375.1271
Conroy R, Pyörälä K, Fitzgerald A et al (2003) Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J 24:987–1003. doi:10.1016/S0195-668X(03)00114-3
Danesh J, Erqou S, Walker M, Thompson SG (2007) The Emerging Risk Factors Collaboration: analysis of individual data on lipid, inflammatory and other markers in over 1.1 million participants in 104 prospective studies of cardiovascular diseases. Eur J Epidemiol 22:839–869. doi:10.1007/s10654-007-9165-7
Elliott P, Peakman TC (2008) The UK Biobank sample handling and storage protocol for the collection, processing and archiving of human blood and urine. Int J Epidemiol 37:234–244. doi:10.1093/ije/dym276
Goff DC, Lloyd-Jones DM, Bennett G et al (2014) 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 63:2960–2984. doi:10.1016/j.jacc.2013.11.005
Guha S, Basu A, Pal S, et al (2004) Predictive efficacy of Framingham’s risk score in Indian scenario—a retrospective case-control study. J Indian Med Assoc 102:568, 570, 584 passim
Gunarathne A, Patel JV, Potluri R et al (2008) Secular trends in the cardiovascular risk profile and mortality of stroke admissions in an inner city, multiethnic population in the United Kingdom (1997–2005). J Hum Hypertens 22:18–23. doi:10.1038/sj.jhh.1002265
Hippisley-Cox J, Coupland C, Vinogradova Y et al (2008) Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ 336:1475–1482. doi:10.1136/bmj.39609.449676.25
Jaquet A, Deloumeaux J, Dumoulin M et al (2008) Metabolic syndrome and Framingham risk score for prediction of cardiovascular events in Caribbean Indian patients with blood glucose abnormalities. Diabetes Metab 34:177–181. doi:10.1016/j.diabet.2007.10.005
Joshi P, Islam S, Pais P et al (2007) Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA 297:286–294. doi:10.1001/jama.297.3.286
Kanjilal S, Rao VS, Mukherjee M et al (2008) Application of cardiovascular disease risk prediction models and the relevance of novel biomarkers to risk stratification in Asian Indians. Vasc Health Risk Manag 4:199–211. doi:10.2147/vhrm.2008.04.01.199
Kaptoge S, Di Angelantonio E, Pennells L et al (2012) C-reactive protein, fibrinogen, and cardiovascular disease prediction. N Engl J Med 367:1310–1320. doi:10.1056/NEJMoa1107477
Khanna R, Kapoor A, Kumar S et al (2013) Metabolic syndrome and Framingham Risk Score: observations from a coronary angiographic study in Indian patients. Indian J Med Res 137:295–301
Kumar BN, Selmer R, Lindman AS et al (2009) Ethnic differences in SCORE cardiovascular risk in Oslo, Norway. Eur J Cardiovasc Prev Rehabil 16:229–234. doi:10.1097/HJR.0b013e3283294b07
McSweeney JC, Cody M, O’Sullivan P et al (2003) Women’s early warning symptoms of acute myocardial infarction. Circulation 108:2619–2623. doi:10.1161/01.CIR.0000097116.29625.7C
McSweeney JC, O’Sullivan P, Cleves MA et al (2010) Racial differences in women’s prodromal and acute myocardial infarction symptoms jean. Am J Crit Care 19:63–73. doi:10.1016/j.biotechadv.2011.08.021.Secreted
Misra A, Khurana L (2011) Obesity-related non-communicable diseases: South Asians vs White Caucasians. Int J Obes (Lond) 35:167–187. doi:10.1038/ijo.2010.135
NICE (2008) Lipid modification: Cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease. In: Natl. Inst. Heal. Clin. Excell. http://www.nice.org.uk/guidance/cg67/resources/guidance-lipid-modification-cardiovascular-risk-assessment-and-the-modification-of-blood-lipids-for-the-primary-and-secondary-prevention-of-cardiovascular-disease-pdf. Accessed 1 May 2015
NICE (2015) Lipid modification: cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease. In: National Institute for Health and Clinical Excellence. http://www.nice.org.uk/guidance/cg181/resources/guidance-lipid-modification-cardiovascular-risk-assessment-and-the-modification-of-blood-lipids-for-the-primary-and-secondary-prevention-of-cardiovascular-disease-pdf. Accessed 1 May 2015
Perumal L, Wells S, Ameratunga S et al (2012) Markedly different clustering of CVD risk factors in New Zealand Indian and European people but similar risk scores (PREDICT-14). Aust N Z J Public Health 36:141–144. doi:10.1111/j.1753-6405.2011.00808.x
Prasad DS, Kabir Z, Dash AK, Das Bhagabati C (2011) Childhood cardiovascular risk factors in South Asians: a cause of concern for adult cardiovascular disease epidemic. Ann Pediatr Cardiol 4:166–171. doi:10.4103/0974-2069.84663
Quirke TP, Gill PS, Mant JW, Allan TF (2003) The applicability of the Framingham coronary heart disease prediction function to black and minority ethnic groups in the UK. Heart 89:785–786. doi:10.1136/heart.89.7.785
Srivastava A, Mohanty SK (2013) Age and sex pattern of cardiovascular mortality, hospitalisation and associated cost in India. PLoS One 8:1–13. doi:10.1371/journal.pone.0062134
Stevens RJ, Kothari V, Adler AI, Stratton IM (2001) The UKPDS risk engine: a model for the risk of coronary heart disease in Type II diabetes (UKPDS 56). Clin Sci (Lond) 101:671–679. doi:10.1042/CS20000335
Thompson S, Kaptoge S, White I et al (2010) Statistical methods for the time-to-event analysis of individual participant data from multiple epidemiological studies. Int J Epidemiol 39:1345–1359. doi:10.1093/ije/dyq063
Tillin T, Hughes AD, Whincup P et al (2014) Ethnicity and prediction of cardiovascular disease: performance of QRISK2 and Framingham scores in a UK tri-ethnic prospective cohort study (SABRE–Southall And Brent REvisited). Heart 100:60–67. doi:10.1136/heartjnl-2013-304474
Turin TC, Shahana N, Wangchuk LZ et al (2013) Burden of cardio- and cerebro-vascular diseases and the conventional risk factors in South Asian population. Glob Heart 8:121–130. doi:10.1016/j.gheart.2012.01.001
UN (2014) Concise report on the world population situation in 2014. In: United Nations. http://www.un.org/en/development/desa/population/publications/pdf/trends/Concise. Report on the World Population Situation 2014/en.pdf. Accessed 4 Aug 2015
Wells S, Kerr A, Broad J et al (2007) The impact of New Zealand CVD risk chart adjustments for family history and ethnicity on eligibility for treatment (PREDICT CVD-5). N Z Med J 120:U2712
WHO (2014) Global status report on noncommunicable diseases 2014. In: World Health Organisation. http://apps.who.int/iris/bitstream/10665/148114/1/9789241564854_eng.pdf?ua=1. Accessed 1 May 2015
Acknowledgments
We thank Isla Kuhn, Reader Services Librarian at the University of Cambridge Medical Library, for her help with the structure and development of the systematic search strategy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
JUS is supported by a National Institute of Health Research (NIHR) Clinical Lectureship. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gopal, D.P., Usher-Smith, J.A. Cardiovascular risk models for South Asian populations: a systematic review. Int J Public Health 61, 525–534 (2016). https://doi.org/10.1007/s00038-015-0733-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00038-015-0733-4