Abstract
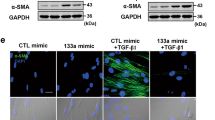
Idiopathic Pulmonary Fibrosis (IPF) is a progressively fatal and incurable disease characterized by the loss of alveolar structures, increased epithelial–mesenchymal transition (EMT), and aberrant tissue repair. In this study, we investigated the role of Nuclear Factor I-B (NFIB), a transcription factor critical for lung development and maturation, in IPF. Using both human lung tissue samples from patients with IPF, and a mouse model of lung fibrosis induced by bleomycin, we showed that there was a significant reduction of NFIB both in the lungs of patients and mice with IPF. Furthermore, our in vitro experiments using cultured human lung cells demonstrated that the loss of NFIB was associated with the induction of EMT by transforming growth factor beta (TGF-β). Knockdown of NFIB promoted EMT, while overexpression of NFIB suppressed EMT and attenuated the severity of bleomycin-induced lung fibrosis in mice. Mechanistically, we identified post-translational regulation of NFIB by miR-326, a miRNA with anti-fibrotic effects that is diminished in IPF. Specifically, we showed that miR-326 stabilized and increased the expression of NFIB through its 3'UTR target sites for Human antigen R (HuR). Moreover, treatment of mice with either NFIB plasmid or miR-326 reversed airway collagen deposition and fibrosis. In conclusion, our study emphasizes the critical role of NFIB in lung development and maturation, and its reduction in IPF leading to EMT and loss of alveolar structures. Our study highlights the potential of miR-326 as a therapeutic intervention for IPF.
Graphical abstract
The schema shows the role of NFIB in maintaining the normal epithelial cell characteristics in the lungs and how its reduction leads to a shift towards mesenchymal cell-like features and pulmonary fibrosis. A In normal lungs, NFIB is expressed abundantly in the epithelial cells, which helps in maintaining their shape, cell polarity and adhesion molecules. However, when the lungs are exposed to factors that induce pulmonary fibrosis, such as bleomycin, or TGF-β, the epithelial cells undergo epithelial to mesenchymal transition (EMT), which leads to a decrease in NFIB. B The mesenchymal cells that arise from EMT appear as spindle-shaped with loss of cell junctions, increased cell migration, loss of polarity and expression of markers associated with mesenchymal cells/fibroblasts. C We designed a therapeutic approach that involves exogenous administration of NFIB in the form of overexpression plasmid or microRNA-326. This therapeutic approach decreases the mesenchymal cell phenotype and restores the epithelial cell phenotype, thus preventing the development or progression of pulmonary fibrosis.






Similar content being viewed by others
Data availability
The datasets generated during the current study are available from the corresponding author upon reasonable request.
References
Pardo A, Selman M, Kaminski N (2008) Approaching the degradome in idiopathic pulmonary fibrosis. Int J Biochem Cell Biol 40(6–7):1141–1155
Todd NW, Luzina IG, Atamas SP (2012) Molecular and cellular mechanisms of pulmonary fibrosis. Fibrogenes Tissue Repair 5(1):1
Shi W, Xu J, Warburton D (2009) Development, repair and fibrosis: What is common and why it matters series. Respirology 14(5):656–665
Selman M, Pardo A (2001) Idiopathic pulmonary fibrosis: an epithelial/fibroblastic cross-talk disorder. Respir Res 3:1–8
Willis BC, DuBois RM, Borok Z (2006) Epithelial origin of myofibroblasts during fibrosis in the lung. Proc Am Thorac Soc 3(4):377–382
Selman M, Pardo A, Kaminski N (2008) Idiopathic pulmonary fibrosis: Aberrant recapitulation of developmental programs? PLoS Med 5(3):0373–0380
Hsu YC, Osinski J, Campbell CE, Litwack ED, Wang D, Liu S et al (2011) Mesenchymal nuclear factor I B regulates cell proliferation and epithelial differentiation during lung maturation. Dev Biol 354(2):242–252
Steele-Perkins G, Plachez C, Butz KG, Yang G, Bachurski CJ, Kinsman SL et al (2005) The transcription factor gene Nfib is essential for both lung maturation and brain development. Mol Cell Biol 25(2):685–698
Becker-Santos DD, Lonergan KM, Gronostajski RM, Lam WL (2017) Nuclear factor I/B: a master regulator of cell differentiation with paradoxical roles in cancer. EBioMedicine 22:2–9
Bartel DP (2004) MicroRNAs: genomics, biogenesis, mechanism, and function. Cell 116(2):281–297
Das S, Kumar M, Negi V, Pattnaik B, Prakash YS, Agrawal A et al (2014) MicroRNA-326 regulates profibrotic functions of transforming growth factor-β in pulmonary fibrosis. Am J Respir Cell Mol Biol 50(5):882–892
Ning J, Zhang H, Yang H (2018) MicroRNA-326 inhibits endometrial fibrosis by regulating TGF-ß1/Smad3 pathway in intrauterine adhesions. Mol Med Rep 18(2):2286–2292
Wang Y, Zhang R, Zhang J, Liu F (2018) MicroRNA-326-3p ameliorates high glucose and ox-LDL-IC- induced fibrotic injury in renal mesangial cells by targeting FcγRIII. Nephrology 23(11):1031–1038
Liu M, Wu H, Liu Y, Tan Y, Wang S, Xie S et al (2021) MiR-326 mediates malignant biological behaviors of lung adenocarcinoma by targeting ZEB1. Sci Prog 104(2):1–15
Zhang H, Yan HL, Li XY, Guo YN (2020) TNFSF14, a novel target of miR-326, facilitates airway remodeling in airway smooth muscle cells via inducing extracellular matrix protein deposition and proliferation. Kaohsiung J Med Sci 36(7):508–514
Xu T, Yan W, Wu Q, Xu Q, Yuan J, Li Y et al (2019) MiR-326 inhibits inflammation and promotes autophagy in silica-induced pulmonary Fibrosis through targeting TNFSF14 and PTBP1. Chem Res Toxicol 32(11):2192–2203
Lin LN, Zhang QM, Ge YY, Luo B, Xie XX (2021) A review of miR-326 and female related diseases. Acta Histochem Cytochem 54(3):79–86
Tu J, Wu F, Chen L, Zheng L, Yang Y, Ying X et al (2021) Long non-coding RNA PCAT6 Induces M2 polarization of macrophages in cholangiocarcinoma via modulating miR-326 and RhoA-ROCK signaling pathway. Front Oncol 10:1–12
Gieseck RL, Wilson MS, Wynn TA (2018) Type 2 immunity in tissue repair and fibrosis. Nat Rev Immunol 18(1):62–76
Thomas A, Wynn KMV (2016) Macrophages in tissue repair, regeneration, and fibrosis Thomas. Immunity 44(3):450–462
Pan YJ, Wan J, Wang C-B (2019) MiR-326: promising biomarker for cancer. Cancer Manag Res. 11:10411–10418
Ghaemi Z, Soltani BM, Mowla SJ (2019) MicroRNA-326 functions as a tumor suppressor in breast cancer by targeting ErbB/PI3K signaling pathway. Front Oncol 9:1–12
Zhang J, He H, Wang K, Xie Y, Yang Z, Qie M et al (2020) miR-326 inhibits the cell proliferation and cancer stem cell-like property of cervical cancer in vitro and oncogenesis in vivo via targeting TCF4. Ann Transl Med 8(24):1638–1638
Barré B, Vigneron A, Coqueret O (2005) The STAT3 transcription factor is a target for the Myc and riboblastoma proteins on the Cdc25A promoter. J Biol Chem 280(16):15673–15681
Amaya ML, Inguva A, Pei S, Jones C, Krug A, Ye H et al (2022) The STAT3-MYC axis promotes survival of leukemia stem cells by regulating SLC1A5 and oxidative phosphorylation. Blood 139(4):584–596
Matsumura I, Tanaka H, Kanakura Y (2003) E2F1 and c-Myc in cell growth and death. Cell Cycle 2(4):333–338
Dang CV (1999) c-Myc target genes involved in cell growth, apoptosis, and metabolism. Mol Cell Biol 19(1):1–11
Kalluri R, Neilson EG (2003) Epithelial-mesenchymal transition and its implications for fibrosis. J Clin Invest 112(12):1776–1784
Zhang S, Fan Y, Qin L, Fang X, Zhang C, Yue J et al (2021) IL-1β augments TGF-β inducing epithelial-mesenchymal transition of epithelial cells and associates with poor pulmonary function improvement in neutrophilic asthmatics. Respir Res 22(1):1–15
Sgalla G, Iovene B, Calvello M, Ori M, Varone F, Richeldi L (2018) Idiopathic pulmonary fibrosis: pathogenesis and management. Respir Res 19(1):1–18
Rock JR, Barkauskas CE, Cronce MJ, Xue Y, Harris JR, Liang J et al (2011) Multiple stromal populations contribute to pulmonary fibrosis without evidence for epithelial to mesenchymal transition. Proc Natl Acad Sci U S A 108(52):E1475–E1483
Stone RC, Pastar I, Ojeh N, Chen V, Liu S, Garzon KI, Tomic-Canic M (2016) Epithelial-mesenchymal transition in tissue repair and fibrosis. Cell Tissue Res 365(3):495–506
Salton F, Volpe MC, Confalonieri M (2019) Epithelial-mesenchymal transition in the pathogenesis of idiopathic pulmonary fibrosis. Med 55(4):1–8
Salton F, Ruaro B, Confalonieri P, Confalonieri M (2020) Epithelial–mesenchymal transition: a major pathogenic driver in idiopathic pulmonary fibrosis? Med 56(11):1–4
Borzone G, Moreno R, Urrea R, Meneses M, Oyarzún M, Lisboa C (2001) Bleomycin-induced chronic lung damage does not resemble human idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 163(7):1648–1653
Pongracz JE, Stockley RA (2006) Wnt signalling in lung development and diseases. Respir Res 7:1–10
Ortiz-zapater E, Signes-costa J, Montero P, Roger I (2022) Lung fibrosis and fibrosis in the lungs: is it all about myofibroblasts? Biomedicines 10(6):1–20
Cheng R, Gao S, Hu W, Liu Y, Cao Y (2021) Nuclear factor I/B mediates epithelial-mesenchymal transition in human melanoma cells through ZEB1. Oncol Lett 21(2):1–11
Hill CS, Treisman R (1995) Transcriptional regulation by extracellular signals: mechanisms and specificity. Cell 80(2):199–211
Li P, Spolski R, Liao W, Leonard WJ (2014) Complex interactions of transcription factors in mediating cytokine biology in T cells. Immunol Rev 261(1):141–156
Lawrence T (2009) The nuclear factor NF-kappaB pathway in inflammation. Cold Spring Harb Perspect Biol 1(6):a001651
Gao G, Hausmann S, Flores NM, Benitez AM, Shen J, Yang X et al (2023) The NFIB/CARM1 partnership is a driver in preclinical models of small cell lung cancer. Nat Commun 14(1):363
Cai M, Wang Z, Zhang J, Zhou H, Jin L, Bai R et al (2015) Adam17, a target of Mir-326, promotes Emt-induced cells invasion in lung adenocarcinoma. Cell Physiol Biochem 36(3):1175–1185
Ahuja D, Goyal A, Ray PS (2016) Interplay between RNA-binding protein HuR and microRNA-125b regulates p53 mRNA translation in response to genotoxic stress. RNA Biol 13(11):1152–1165
Gubin MM, Calaluce R, Davis JW, Magee JD, Strouse CS, Shaw DP et al (2010) Overexpression of the RNA binding protein HuR impairs tumor growth in triple negative breast cancer associated with deficient angiogenesis. Cell Cycle 9(16):3357–3366
Wu X, Xu L (2022) The RNA-binding protein HuR in human cancer: a friend or foe? Adv Drug Deliv Rev 184:1–26
Trivlidis J, Aloufi N, Al-Habeeb F, Nair P, Azuelos I, Eidelman DH et al (2021) HuR drives lung fibroblast differentiation but not metabolic reprogramming in response to TGF-β and hypoxia. Respir Res 22(1):1–19
Guarnieri AR, Anthony SR, Gozdiff A, Green LC, Fleifil SM, Slone S, Nieman ML, Alam P, Benoit JB, Owens AP, Kanisicak O, Michael T (2021) Adipocyte-specific deletion of HuR induces spontaneous cardiac hypertrophy and fibrosis. Am J Physiol Hear Circ Physiol. 321(1):H228–H241
Subramanian P, Gargani S, Palladini A, Chatzimike M, Grzybek M, Peitzsch M et al (2022) The RNA binding protein human antigen R is a gatekeeper of liver homeostasis. Hepatology 75(4):881–897
Ahmad T, Kumar M, Mabalirajan U, Pattnaik B, Aggarwal S, Singh R et al (2012) Hypoxia response in asthma: differential modulation on inflammation and epithelial injury. Am J Respir Cell Mol Biol 47(1):1–10
Acknowledgements
The authors would like to thank Dr. Kritika Khanna, Dr. Naveen K Bhatraju, Dr. Manish Kumar, Dr. Dhurjyoti Saha, and Dr. Prashant Bajpai from CSIR-IGIB, India for their valuable assistance in this study. We also acknowledge the microscopy facility of the Council for Scientific and Industrial Research Institute of Genomics and Integrative Biology (CSIR-IGIB) for their support in confocal microscopy.
Funding
This work was supported by grants from the Council of Scientific and Industrial Research (CSIR), India (MLP5502, BSC 0116, GAP0069 and MLP 1201); Swarnajayanti Fellowship (Anurag Agrawal), Department of Science and Technology (DST), India, and Wellcome Trust India Alliance Senior Fellowship (Anurag Agrawal), GAP0084 (Balaram Ghosh). Dr. Tanveer Ahmad acknowledges funding support from the core research grant of the Science and Engineering Research Board (CRG/2020/002294) and the extramural grant of the Indian Council of Medical Research (ICMR) (GIA/2019/000274/PRCGIA (Ver-1)).
Author information
Authors and Affiliations
Contributions
BP, TA, BG and AA: conceptualized and established the hypotheses, designed the study; BP: executed the experiments; performed data acquisition, analysis, and interpretation; BP, TA and AA: drafted the manuscript; critically revised the manuscript, and performed statistical analysis. KD, AG, and BP, VN and RC: were involved in mice experiments, data acquisition, and analysis; performed histology and imaging; assisted critical revision of the manuscript; and provided technical support. MF, AA, MS, SA: critically revised the manuscript, and performed statistical analysis. YSP: provided human lung samples from patients with IPF and non-fibrotic control subjects and was involved in critical revision of the manuscript. RG was involved in critical revision of the manuscript. TA, BG and AA: provided the financial support.
Corresponding authors
Ethics declarations
Conflict interest
The authors declare that they have no competing interests pertaining to this work.
Ethics approval and consent to participate
The study design was approved by the Institutional Animal Ethics Committee (IAEC) for using mice models. The collection of human tissue samples was performed only after obtaining approval from the Mayo Clinic Institutional Review Board, which ensures that research studies involving human subjects are conducted in an ethical and safe manner.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pattnaik, B., Negi, V., Chaudhuri, R. et al. MiR-326-mediated overexpression of NFIB offsets TGF-β induced epithelial to mesenchymal transition and reverses lung fibrosis. Cell. Mol. Life Sci. 80, 357 (2023). https://doi.org/10.1007/s00018-023-05005-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00018-023-05005-1