Abstract
Dysregulation of angiogenesis is a phenomenon observed in several disorders such as diabetic foot, critical limb ischemia and myocardial infarction. Mesenchymal stromal cells (MSCs) possess angiogenic potential and have recently emerged as a powerful tool for cell therapy to promote angiogenesis. Although bone marrow-derived MSCs are the primary cell of choice, obtaining them has become a challenge. The placenta has become a popular alternative as it is a highly vascular organ, easily available and ethically more favorable with a rich supply of MSCs. Comparatively, placenta-derived MSCs (PMSCs) are clinically promising due to their proliferative, migratory, clonogenic and immunomodulatory properties. PMSCs release a plethora of cytokines and chemokines key to angiogenic signaling and facilitate the possibility of delivering PMSC-derived exosomes as a targeted therapy to promote angiogenesis. However, there still remains the challenge of heterogeneity in the isolated populations, questions on the maternal or fetal origin of these cells and the diversity in previously reported isolation and culture conditions. Nonetheless, the growing rate of clinical trials using PMSCs clearly indicates a shift in favor of PMSCs. The overall aim of the review is to highlight the importance of this rather poorly understood cell type and emphasize the need for further investigations into their angiogenic potential as an alternative source for therapeutic angiogenesis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Clinical demand for angiogenesis
Angiogenesis is the process of formation of new blood vessels from pre-existing vasculature and is observed throughout the lifetime of an individual. Beginning with the earlier studies of Judah Folkman, a great interest developed over the years in understanding the regulation of angiogenesis as a key therapeutic tool [1,2,3]. While inhibition of angiogenesis is therapeutic for cancer, rheumatoid arthritis, etc., the enhancement of angiogenesis is a prerequisite, in a long list of disorders characterized by the lack of proper vascular development as seen in heart and brain ischemia, myocardial infarction, limb ischemia, diabetic wounds, pre-eclampsia and so on. Furthermore, age-related decline in vascular endothelial growth factor (VEGF), a key regulator of angiogenic signaling, could also lead to several complications [4]. Therefore, unlike what was thought of earlier, it has become very evident that angiogenesis and angiogenic factors play an important role in several clinical disorders.
Around two decades ago, a new term was coined called ‘Therapeutic Angiogenesis’, defined as the means to stimulate angiogenesis for clinically relevant outcomes. This concept was further developed as a result of several experimental studies providing compelling evidence that certain factors like specific growth factors, oxygen regulation, pharmaceutical agents, bioactive matrices and other tissue-engineered products could be used to enhance the angiogenic potential at the sites of injury [5, 6]. Currently, researchers are turning toward cell-based therapies and specifically the use of mesenchymal stromal cells (MSCs) as an alternative tool for ‘natural systems of tissue repair’ [7]. Among several sources of MSCs, the placenta is now being considered a possible option. This review focuses on understanding the relevance of using placenta-derived MSCs (PMSCs) as a possible alternative cell source for therapeutic angiogenesis, the characteristics that set them apart, the means of enhancing their angiogenic potential and the main challenges that surround the use of these cells.
Placental mesenchymal stromal cells
It was A. J. Friedenstein and his colleagues, back in the early 1970s, who were the first to report on the significance of MSCs, which are multipotent, self-renewing and undifferentiated cells [8]. Although bone marrow-derived MSCs (BMMSCs) are considered a gold standard among other MSCs, the difficulty in obtaining BMMSCs has forced scientists to a hunt for new and versatile sources. MSCs from several sources have angiogenic potential [9, 10]. Indeed, MSCs from several sources have attracted a lot of attention in the clinical setting as a sought after cell-based therapy for acute diseases [11]. Among them, the placenta is gaining a lot of attention as an alternative source of MSCs, owing to its abundance and ease of availability. The placenta is a transient feto-maternal organ, disposed off after delivery and involves no invasive procedures, making it ethically a more favorable source. A large recovery of PMSCs from a small tissue chunk has been also reported [12, 13]. It is also noteworthy that unlike most human tissue, the placenta is known to have lower levels of DNA methylation, making it more compatible with the human genome [14]. Moreover, as the placenta is a highly vascular organ, it is logical to assume that MSCs isolated from them should possess more angiogenic properties [15, 16]. This assumption is further supported by studies that show a direct contribution of the mesenchymal cells in the placenta to the formation of the early progenitors of hemangiogenic cells, rather than the fetal blood cells. Hemangiogenic cells form the first vessels in the placenta, providing further evidence of the putative role of PMSCs in angiogenesis [17].
Sources of PMSCs
The placenta is a disk-like structure with a diameter of 16–20 cm, thickness of 2–3 cm and weight an average of 500 g [12]. The placenta as a materno-fetal organ consists of both fetal and maternal parts (Fig. 1). The fetal parts include the chorionic plate (the fetal side of the placenta covered by the amnion), the amnion (covering the chorionic plate) and the umbilical cord (consists of two arteries and vein immersed in the Wharton’s jelly surrounded by the amniotic epithelium). The fetal membranes, the amniotic membrane (transparent, smooth, avascular and single-layered membrane composed of epithelium and mesenchyme) and chorionic membranes (composed of fibroblasts and trophoblast cells) further extend from the edges of the placenta and surround the fetus embedded in the amniotic fluid. The chorionic villi originate from the chorionic plate into the cotyledons. On the other hand, the maternal part is primarily formed of the decidua basalis [18]. The basal plate region of the decidua basalis protrudes into the chorionic villi region forming approximately 15–20 separations called the placental septa. The placental septa in turn partitions the parenchyma in the chorionic villi region into the cotyledons [12].
PMSCs have been used as a general term in referring to cells isolated from different sites of the placenta. Cells have been isolated from the decidua basalis (DBMSCs) [19], the chorionic membrane (CMMSCs) [20], the chorionic villi (CVMSCs) [21], chorionic cotyledons or intervillous space (CIVMSCs) [22, 23], chorionic plate (CPMSCs) [24], the chorionic trophoblastic cells [25], the amniotic membrane (AMMSCs) [26] and the amniotic fluid (AFMSCs) [27]. Since all these cells are from direct parts or extensions of the placenta, researchers sometimes refer to them generally as PMSCs, making it difficult to identify which specific cells have been used. Moreover, we only have a limited understanding of PMSCs from different sites of the placenta and only a few comparative studies have been performed to date [28]. We have tried to include all variants of direct isolations from the placenta, referring to specific types wherever available.
The PMSCs are often isolated via explant or enzymatic methods. In short, for the explant method, tissue from the respective source is dissected and washed with ice-cold phosphate-buffered saline to remove excess blood. The tissue chunks are minced and allowed to settle on culture dishes and the plates are then incubated with mesenchymal stem cell propagation media, in a humidified chamber with 5% CO2 at 37 °C [29]. For the enzymatic method, the tissue was similarly minced and enzymatically treated with trypsin, while other protocols prefer an overnight collagenase treatment. After this, the isolated cells are seeded onto culture plates and maintained in the same way as that of the explant culture [30, 31].
Why PMSCs? A comparative note
MSCs isolated from different sources have specific differentiation potentials. We have presented a comparative understanding of different MSCs to PMSCs, based on properties that regulate angiogenesis.
Anatomical location MSCs are known to reside in several tissues and it is well documented that the niche in which they reside is a key regulator of the properties of that particular kind of stem cell [32]. Being a highly vascular structure, the placenta is exposed to enhanced levels of angiogenic signals that need to be maintained throughout the gestational period in response to fetal demands [33]. The placenta thus provides a suitable niche for pro-angiogenic signals. Moreover, researchers have shown that PMSCs reside primarily in the vascular niche of the placenta [15]. The highly vascular niche, suggests a higher potency of PMSCs for angiogenesis. The placenta is also a rich source of other cells such as hematopoietic stem cells [34].
Source of fetal stem cells While ethical concerns restrict the use of embryonic stem cells, the use of fetal stem cells has been considered as a possible option. Fetal stem cells have been proven to be more primitive and more potent than their adult counterparts, making the use of fetal cells more effective in clinical applications [35]. The placenta is fittingly a rich source of fetal stem cells, an intermediate state between the adult stem cells and the embryonic stem cells.
Proliferative ability and migratory ability PMSCs have been shown to be more robust and proliferative and have more long-term growth ability when compared to their BMMSCs counterparts [30, 36, 37]. Several of their regulatory pathways have also been explored [38]. For instance, BMSCs have a greater migratory capacity when compared to PMSCs [39], indicating that the BMMSCs can cross the endothelial blood vessel barrier more efficiently than the PMSCs [21]. Nonetheless, co-cultures of PMSCs, but not BMMSCs, with endothelial cells (ECs) induce migration of the ECs [40].
Differentiation potential Among the differentiation lineages, AMMSCs and CPMSCs have higher osteogenic and chondrogenic potential, but not adipogenic when compared to BMMSCs [20]. On the other hand, CPMSCs were more adipogenic, but not osteogenic when compared to the Wharton’s jelly-derived MSCs (WJMSCs) counterparts [24]. Whether these differences in their basic differentiation potential would influence the angiogenic differentiation of these cells has not yet been established.
Immunomodulatory properties of MSCs One of the most striking features of MSCs is their immunomodulatory ability: a unique way of escaping and modulating the immune system [41]. Adult MSCs may express intermediate levels of HLA major histocompatibility complex (MHC) class I proteins, but lack MHC class II proteins on their cell surface [41]. Like other MSCs, PMSCs also have limited expression of HLA-A, B, C, making them less immunogenic and thus suitable for transplantation. A comparative study concluded that PMSCs have an advantage over several other MSCs including the BMMSCs [42], due in part to their immunomodulatory properties [43]. Stimulation of BMMSCs, umbilical cord MSCs (UCMSCs), and adipose-derived MSCs (ADMSCs) with interferon-γ (IFN-γ) resulted in an upregulated expression of MHC class II, while even a 3 day stimulation only showed a minimal expression in PMSCs [19]. This further supports earlier reports that PMSCs are more immunomodulatory compared to UCMSCs [42]. PMSCs regulate macrophage differentiation from an inflammatory M1 state to an anti-inflammatory M2 stage [44, 45]. The PMSCs also express (HLA)-G, which mediates inhibition of T cell proliferation [46]. A comparative study between conditioned media of cord blood-derived MSCs (CBMSCs) and PMSCs on mononuclear cells and dendritic cells demonstrated a significantly pronounced reduction in T cell proliferation by PMSCs [42], due in part to transforming growth factor-beta and interleukin [47] or mediated by indoleamine-pyrrole 2,3-dioxygenase [48]. Although not much is known of the PMSC interaction with B cells, there are reports that state the prevention of early apoptosis of B cells. PMSCs also mediate immunosuppressive effects on NK cells [49]. Another key step during an inflammatory stimulation is the activation of the endothelium—involving the enhanced proliferation and upregulation of adhesion and inflammatory markers by the endothelium. DBMSCs, have a protective role under inflammatory conditions by reversing the effect of H2O2 on ECs [50]. Another group similarly demonstrated that T cell-mediated reprogramming of macrophages led to enhanced angiogenesis in mice with hind limb ischemia [44]. These studies are perhaps indicative of the fact that immunomodulation is one of the means by which PMSCs regulate angiogenesis [51].
Clonogenic ability of PMSCs The ability of a cell to form colonies may also be considered as a reflection of the ability of the cell to grow in a density-intensive fashion and is regarded as a mark of a genuine stromal cell [52]. A comparative study of CBMSCs demonstrated an increased formation of colonies by PMSCs when compared to CBMSCs isolated from the same tissue. This may also be reflective of the higher expansion ability of PMSCs [42].
Collectively, although the PMSCs are not highly migratory in nature, their anatomical location, proliferative ability, clonogenic ability and their high degree of immunomodulatory properties, make them ideal candidates for cell-based therapy. Moreover, a comparative study on the cytokine levels indicated a compatible level of VEGF and basic fibroblast growth factor (bFGF) secretion in PMSCs and human umbilical vein endothelial cells (HUVECs) when compared to UCMSCs and even BMMSCs [53] and a higher endothelial differentiation ability of CVMSCs than that of BMMSCs [54]. However, there is a need to optimize the ideal isolation and culture conditions such that bona fide fetal MSCs are grown.
Angiogenic ability of placental mesenchymal stromal cells
MSCs are now an accepted tool for therapy in case of dysfunctional angiogenesis [55] and PMSCs are gaining a lot of interest as a suitable cell source [56, 57]. The placenta is a vascular tissue, and it is therefore probable that MSCs isolated from the placenta may prove to be more potent for therapeutic angiogenesis. Apart from its general properties, their secretion of angiogenic factors, migration and secretion of matrix metalloproteinases to mediate the migration and capillary tube formation further suggest their suitability for therapeutic angiogenesis (Fig. 2).
Placental mesenchymal stromal cells and angiogenesis. Pictorial outline describing the different sources and properties of placenta-derived mesenchymal stromal cells (PMSCs). PMSCs can be primed to enhance their angiogenic potential. The cells or their secretome can be applied to promote angiogenesis
PMSC cell-mediated angiogenesis
PMSCs as a cell-based system for therapeutic angiogenesis is promising [58,59,60] (Table 1).
Differentiation into vascular-like cells
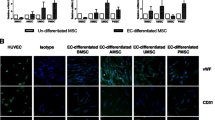
Capillary tube formation is a method employed to determine the cell’s ability to differentiate into tube-like structures or stimulate capillary tube formation in ECs, and is used to measure in vitro angiogenic potential of cells. Cells are often observed for tube formation on Matrigel (growth factor reduced) surfaces and further quantified for the number of branch points, nodes, junctions, etc. [61]. Several studies have shown that PMSCs are capable of forming tubes in vitro (Fig. 3) on Matrigel without any additional cellular support. However, expression of markers such as von Willebrand factor (vWF) [62] was not seen either in CVMSCs or AMMSCs, suggesting a possible resistance toward differentiation into mature endothelial cells. However, a few studies indicate that post-induction, PMSCs were shown to acquire endothelial morphology and expressed vWF [53]. Interestingly, co-culturing of ECs with CVMSCs resulted in enhanced capillary tube formation, where PMSCs were seen to incorporate into the ECs in vitro [16]. CVMSCs also cross talk with ECs that expressed platelet-derived growth factor receptor-β (PDGF-BB receptor-β) via PDGF-BB signaling, which resulted in signal transducer and activator of transcription 3 (STAT3) activation of PMSCs and thus advanced formation of the vascular network [60] (Fig. 4). Moreover, following transplantation of labeled PMSCs, the cells were able to associate and incorporate into the mural layer of mouse placental vasculature and also expressed smooth muscle cell markers. Similarly, transplantation of green fluorescent protein (GFP)-labeled PMSCs revealed dual staining of GFP with αSMA and vWF in frozen sections of the muscle [53]. This signifies a synergistic role of PMSCs along with ECs and the possibility of direct differentiation of PMSCs into vascular cells that further highlights the engraftment potential of these cells.
Possible mechanism of placental mesenchymal stromal cells contributing to angiogenesis. Possible mechanism behind the role of PMSCs mediating angiogenesis via direct de-differentiation or through its paracrine effects on effector cells such as the smooth muscle cells, endothelial cells and the pericytes in forming mature vessels
In addition, PMSCs were seen to activate pericytes, which are contractile cells that wrap around blood vessels to provide contractility. A certain percentage of PMSCs exhibit pericyte-like phenotype, suggesting that PMSCs can give rise to progenitor cells that are responsible for the maintenance and repair of vessels, thereby contributing to stabilizing capillary tubes [15]. Furthermore, PMSCs can also differentiate into smooth muscle cells which aid in remodeling and stabilizing the vasculature [16]. The in vitro differentiation ability of PMSCs was dependent on the matrix on which it was coated with collagen I, collagen IV and laminin, showing improved differentiation into smooth muscle cells [16].
The question as to how exactly PMSCs modulate angiogenesis is still unclear—do PMSCs themselves differentiate into endothelial-like cells or is it more of an exocrine effect regulating the endogenous niche cells to mediate angiogenesis? Although there is need for more clarity on whether PMSCs themselves differentiate into mature endothelial cells, their paracrine influence on other cells types is certain.
PMSC secretome-mediated angiogenesis
Secretion of pro-angiogenic factors
MSCs are known to secrete a plethora of bioactive molecules that can enhance cell survival and are immunosuppressive, immunomodulatory and angiogenic [63]. PMSCs co-cultured with endothelial progenitor cells (EPCs) enhanced the angiogenic potential of the EPCs via PDGF and NOTCH signaling [60]. Conditioned media (CM) collected from PMSC cultures have significant pro-angiogenic effects on EPCs and HUVECs [57]. Interestingly, a comparative study revealed MSCs derived from blood vessels (CVMSCs) were able to stimulate angiogenesis of ECs to a greater extent than MSCs from avascular sources (AMMSCs) [62], highlighting the importance of determining the components of the CM from different cell sources (Table 1).
Among the angiogenic factors, PMSCs express VEGF (302 ± 25.79 pg/mL) [60], bFGF (50 ± 30.72 pg/mL) [60], angiogenin, IL-6, IL-8, HGF, IGFBP2, IGFBP3 and IGFBP6 [57, 62]. The possible mechanisms of angiogenesis reported include activation of pAkt and p38MAPK/pSTAT3 that activate VEGF secretion [64]; PDGF-BB (vascular maturation and recruitment of smooth muscle cells and pericytes) [16] that enhance the angiogenic potential of endothelial cells by upregulating angiogenic markers such as Tie2 and Ang2 [57] and the role of stromal cell (PMSCs)-derived Slit2 expressed by PMSCs in enhancing endothelial tube formation via Roundabout (Robo) receptors present on endothelial cells [22] (Fig. 4).
CM of PMSCs have other properties that improve transplantation. Cell viability is enhanced coupled with reduced oxidative stress, when CM of PMSCs are deployed along with the cryopreservation mix. The priming of cells with the PMSC-derived CM improves the transplantation ability of cells when compared to CBMSC-derived CM [65]. There are several studies supporting the concept that tissue repair is likely to be an atrophic effect mediated by the secretion of factors, rather than the differentiation of the cells themselves [66, 67].
Role of exosomes
Current research is now shifting gears and looking at more specific components of the CM, most notably the exosomes. These are extracellular vesicles, much smaller than the microvesicles (> 200 nm), ranging from 50 to 200 nm in diameter, processed through several endocytic steps before being released and are known to be involved in several functions [68, 69]. Exosomes contain proteins or RNA and can be prepared from CM of MSCs by ultracentrifugation [57]. PMSC-derived exosomes (PMSC-exos) are known to influence osteogenic and adipogenic differentiation by upregulating OCT4 and NANOG in dermal fibroblasts [70]. They enhance tube formation and migration of endothelial cells [57]. Incorporation of labeled exosomes into the endothelial cells demonstrated the involvement of exosomes in mediating these changes.
Possible exosomal mechanisms include transfer of miRNAs into the endothelial cells that subsequently promote angiogenesis [71] and may be responsible for up to 60% of the angiogenic potential of the CM [57]. miRNAs are 20–24 nt-long non-coding RNAs that mediate a sequence-specific degradation of mRNA [72]. Most of the placenta-specific miRNAs are derived from the chromosome 14 and chromosome 19 miRNA clusters (C14MC/C19MC) [73], which are the largest gene clusters of human miRNAs [74]. Several studies have implicated the role of miRNAs in angiogenesis, miR-17-92 cluster (tumor angiogenesis), miR-27b [75], bLet7-f [75], miR210 and mir-130a. However, specific miRNAs from PMSC-exos targeting endothelial cell function and angiogenesis are yet to be identified. There are, however, reports indicating the role of miRNA125a (adipose-derived exosome) in repressing the angiogenic inhibitor delta-like 4 (DLL4) in endothelial cells and thereby promoting angiogenesis [76]. Although several studies use CBMSCs [77], there are fewer studies reported with PMSCs and therefore a more detailed analysis needs to be done on the potential role of placenta-specific miRNAs. Moreover, as exosomes are not static but highly diverse [69], the relevance of the niche of cells and the protocols used are also being intensively investigated. However, further studies are needed to validate this, but if proven these studies may open up new avenues for the use of cell-free therapy [78].
There is a lot of attention on cell-free or secretome-based therapy with the prospect that the native endogenous cells could be triggered to respond to an injury [79]. However, in most degenerative diseases such as diabetes and among patients undergoing chemo/radiotherapy, the MSC niche is compromised [80]. There have also been reports of age-related decline in the quantity and quality of endogenous MSCs [81]. Under such circumstances, the use of cells over that of CM may become the preferred choice of therapy, thereby making the selection of cell or cell-free based therapy a more case-dependent choice.
Induction of PMSCs to enhance angiogenesis
Although several outcomes under laboratory conditions are promising, actual pre-clinical experimentation has not been as successful. Angiogenesis is a complex process and requires the interplay of multiple factors [82]. Hence, researchers are trying to understand how the angiogenic potential of PMSCs can be made more effective. There is growing evidence that the differentiation of MSCs can be altered by varying their environment [83]. Scientists are now looking at priming cells with factors or physical environment suitable for enhancing their angiogenic potential to ensure success in cell therapy [84].
As placental development takes place under hypoxic conditions (rather normal conditions for placenta cells), one area of focus is in considering the culture of cells under more physiologically relevant oxygen conditions [34]. The placenta has been documented to have a PO2 of 20 mmHg in the first trimester [85]. Studies now indicate that hypoxic priming of PMSCs may enhance their angiogenic potential [23]. In this context, Xu et al. demonstrated how hypoxia mediated phosphorylation of JAK/STAT3 signaling-promoted angiogenesis in trophoblast cells [86]. Conversely, hypoxia decreased angiogenesis via Notch 1 signaling [87]. Another surprising study revealed that in differentiated syncytiotrophoblast, HIF2α downregulated placental growth factor (PlGF) secretion [88], which is a key molecule in angiogenesis. It is clear from the available literature that the oxygen concentration is indeed relevant not only for in vitro culture of cells, but also in regulating how cells trigger angiogenesis in vivo. Nonetheless, more validation is required to establish this process in full. Several molecular interventions, such as compounds to increase the expression of CXCR4 [stromal cell-derived factor-(SDF-)1 receptor], to enhance the migratory ability of MSCs [80], priming with endothelial growth medium [89], erythropoietin [90] and even pharmacological agents such as polyunsaturated fatty acids [91, 92] have been proposed. Alternatively, application of differentiated vasculogenic progeny to endothelial-like cells from PMSCs contributed to enhancing blood vessel formation in an integrin (α5β1)-dependent manner [38].
It’s is therefore clear that PMSCs have an ability to form tubes in vitro and increased capillary formation in vivo. They can also induce other niche cells such as the ECs, pericytes and smooth muscle cells to contribute to angiogenesis via paracrine factors. The more recent studies using exosomes further confirm that both cellular and secretome-based applications are possible from PMSCs.
Applications
Pregnancy-related disorders
Severe dysfunctional vasculature is seen in many pregnancy-related disorders such as pre-eclampsia and gestational diabetes [93]. As pregnancy disorders are often related to trophoblastic abnormalities and since PMSCs are present in the placenta through term, there is increasing interest in considering PMSCs isolated from such placentae as tools to study the respective disorder [94]. Evidence of incorporation of transplanted PMSCs (human) in the vessel walls of mouse placenta further confirms the involvement of PMSCs along with endothelial cells during placentation [16]. Few relevant examples include studies that demonstrate that MSCs from the placenta of gestationally diabetic mothers are hampered in their glucose uptake and display premature aging and altered angiogenesis, while MSCs from obese mothers have greater adipogenesis [95, 96].
Angiogenic potential
Several in vivo studies show promising results of usage of PMSCs in mice models, particularly in limb ischemia models. PMSCs possibly by direct differentiation and incorporation [16, 60] or via cytokine release [91] mediated an increase in the number of blood vessels and blood flow, enhanced vessel density and perfusion at the ischemic site [97, 98] in a very dose- and site-specific manner [56].
Anti-angiogenic potential
Conversely, co-culturing of CVMSCs along with breast cancer cells resulted in a significant reduction in proliferation, migration and tube formation ability of HUVEC cells [99]. Exosomes of MSCs suppress angiogenesis via downregulation of VEGFA [100], while PMSCs suppress peritoneal tumorigenesis [101]. AMMSCs, when injected into retinopathy mouse models, were able to suppress proliferation and prevent neovascularization via upregulation of TGF-β1 [102]. This can partly be explained by the upregulation of miRNAs such as miR-136 [103] under pathology conditions that mediate inhibition of capillary formation. Therefore, it is important to note that PMSCs modulate angiogenesis in a very contextual manner.
Clinical trials
The first clinical trial to use culture-expanded MSCs was performed at the Ireland Cancer Center of University Hospitals of Cleveland [104] using bone marrow-derived MSCs in a phase I trial. Several studies have since been completed and the results are promising (http://www.clinicaltrials.gov/). Studies on the use of PMSCs for other complications such as pulmonary fibrosis (NCT01385644) and Peyronie’s disease (NCT02395029) have been completed. The first of its kind company to harvest PMSCs as a therapeutic product is the Pluristem Therapeutics Inc., Israel, which validated the possibility of an ‘off-the-shelf supply of therapeutic cells’ isolated from the placenta. Their work initially suggested that intramuscular administration of PMSCs in a hind limb ischemia BALB/c mouse model resulted in reduced endothelial damage and enhanced limb function [105]. Further clinical trials using PMSCs, administered via intramuscular injections, for critical limb ischemia and peripheral vascular disease range from phase I to phase III and the results seem encouraging (Table 1).
Other applications include the role of PMSCs as feeder layer for the culture of hematopoietic stem cells—HSCs [106]. The results from the use of PMSCs have been so promising that researchers are now even suggesting the establishment of placental cell biobanks [34].
Challenges
There is a lot of heterogeneity in the techniques adopted for PMSC isolation and consequently a lot of variation in the results, hence the need for proper determination of isolation techniques and means of characterization of the isolated cells. In addition, CVMSCs that were VCAM-1(+) were more promising for in vivo administration in ischemic mice models [107], further emphasizing the identification of key cells within the pool of isolated PMSCs.
Are PMSCs fetal cells? According to the First International Workshop on Placenta Derived Stem Cells, it is mandated that isolated cells be verified as of fetal origin with less than 1% contamination with maternal cells [12]. Although it is assumed that cells isolated from pre-natal sources are ideally fetal, there is very little documentation available among published literature on whether cells isolated from the placenta are indeed fetal. An interesting study reported the presence of fetal cells isolated from the amniotic membrane and maternal cells from the chorionic membrane [20]. Such uncertainty over the origin of cells can lead to variations in published results [108]. Indeed, reports that maternal cells overpopulate a culture of cells isolated from fetal villi clearly suggests that the mere choice of site of isolation would not guarantee the origin of the cells [109]. Researchers are now pointing out that even the protocol used for isolation [110] or the media used in expansion [109] is relevant in obtaining and maintaining pure fetal cells. Another important factor that could add to the differences is the maternal age [111], although it is not clear how this would influence fetal cells! This necessitates the need to standardize isolation protocols to obtain fetal cells and definitely a need to validate the cell cultures prior to experimentation.
Conclusions
In summary, PMSCs are readily obtainable, ethically favored and can be isolated with ease and high cell yields. Their mesenchymal characteristics are similar to that of the gold standard BMMSCs and are highly immunomodulatory. The cells and their secretome can promote angiogenesis by modulating the niche cells (Fig. 2). Although a few clinical trials have shown promise, PMSCs are far less understood and explored compared to their BMMSC counterparts. Nevertheless, while further studies are required to better understand the potential of these cells, the existing literature clearly indicates the potential of PMSCs as an ideal cell source for therapeutic angiogenesis.
References
Sherwood LM, Parris EE, Folkman J (1971) Tumor angiogenesis: therapeutic implications. N Engl J Med 285(21):1182–1186
Cao Y, Langer R (2008) A review of Judah Folkman’s remarkable achievements in biomedicine. Proc Natl Acad Sci 105(36):13203–13205
Risau W (1997) Mechanisms of angiogenesis. Nature 386(6626):671–674
Yin G, Liu W, An P, Li P, Ding I, Planelles V et al (2002) Endostatin gene transfer inhibits joint angiogenesis and pannus formation in inflammatory arthritis. Mol Ther 5(5):547–554
Zhang H, van Olden C, Sweeney D, Martin-Rendon E (2014) Blood vessel repair and regeneration in the ischaemic heart. Open Heart 1(1):e000016
Laurenzana A, Fibbi G, Chillà A, Margheri G, Del Rosso T, Rovida E et al (2015) Lipid rafts: integrated platforms for vascular organization offering therapeutic opportunities. Cell Mol Life Sci 72(8):1537–1557
Schipani E, Kronenberg HM (2008) Adult mesenchymal stem cells. In: StemBook [Internet]. Cambridge (MA): Harvard Stem Cell Institute. https://doi.org/10.3824/stembook.1.38.1. https://www.ncbi.nlm.nih.gov/books/NBK27056/
Weissman IL, Anderson DJ, Gage F (2001) Stem and progenitor cells: origins, phenotypes, lineage commitments, and transdifferentiations. Annu Rev Cell Dev Biol 17(1):387–403
Alviano F, Fossati V, Marchionni C, Arpinati M, Bonsi L, Franchina M et al (2007) Term Amniotic membrane is a high throughput source for multipotent Mesenchymal Stem Cells with the ability to differentiate into endothelial cells in vitro. BMC Dev Biol 21(7):11
Rae PC, Kelly RD, Egginton S, St John JC (2011) Angiogenic potential of endothelial progenitor cells and embryonic stem cells. Vasc Cell 3(1):11
Lim R (2017) Concise review: fetal membranes in regenerative medicine: new tricks from an old dog?: fetal membranes in regenerative medicine. Stem Cells Transl Med 6(9):1767–1776
Parolini O, Alviano F, Bagnara GP, Bilic G, Bühring H-J, Evangelista M et al (2008) Concise review: isolation and characterization of cells from human term placenta: outcome of the first international workshop on placenta derived stem cells. Stem Cells 26(2):300–311
in’t Anker PS, Scherjon SA, Kleijburg-van der Keur C, de Groot-Swings GMJS, Claas FHJ, Fibbe WE et al (2004) Isolation of mesenchymal stem cells of fetal or maternal origin from human placenta. Stem Cells 22(7):1338–1345
Schroeder DI, Blair JD, Lott P, Yu HOK, Hong D, Crary F et al (2013) The human placenta methylome. Proc Natl Acad Sci 110(15):6037–6042
Castrechini NM, Murthi P, Gude NM, Erwich JJHM, Gronthos S, Zannettino A et al (2010) Mesenchymal stem cells in human placental chorionic villi reside in a vascular Niche. Placenta 31(3):203–212
Chen C-Y, Liu S-H, Chen C-Y, Chen P-C, Chen C-P (2015) Human placenta-derived multipotent mesenchymal stromal cells involved in placental angiogenesis via the PDGF-BB and STAT3 pathways1. Biol Reprod 1(103):1–10
Demir R, Kaufmann P, Castellucci M, Erbengi T, Kotowski A (1989) Fetal vasculogenesis and angiogenesis in human placental villi. Acta Anat (Basel) 136(3):190–203
Pogozhykh O, Prokopyuk V, Figueiredo C, Pogozhykh D (2018) Placenta and placental derivatives in regenerative therapies: experimental studies, history, and prospects. Stem Cells Int 2018:1–14
Abumaree MH, Abomaray FM, Alshabibi MA, AlAskar AS, Kalionis B (2017) Immunomodulatory properties of human placental mesenchymal stem/stromal cells. Placenta 59:87–95
Jaramillo-Ferrada PA, Wolvetang EJ, Cooper-White JJ (2012) Differential mesengenic potential and expression of stem cell-fate modulators in mesenchymal stromal cells from human-term placenta and bone marrow. J Cell Physiol 227(9):3234–3242
Makhoul G, Chiu RCJ, Cecere R (2013) Placental mesenchymal stem cells: a unique source for cellular cardiomyoplasty. Ann Thorac Surg 95(5):1827–1833
Chen C-Y, Tsai C-H, Chen C-Y, Wu Y-H, Chen C-P (2016) Human placental multipotent mesenchymal stromal cells modulate placenta angiogenesis through Slit2-Robo signaling. Cell Adhes Migr 10(1–2):66–76
Mathew SA, Chandravanshi B, Bhonde R (2017) Hypoxia primed placental mesenchymal stem cells for wound healing. Life Sci 182:85–92
Kim MJ, Shin KS, Jeon JH, Lee DR, Shim SH, Kim JK et al (2011) Human chorionic-plate-derived mesenchymal stem cells and Wharton’s jelly-derived mesenchymal stem cells: a comparative analysis of their potential as placenta-derived stem cells. Cell Tissue Res 346(1):53–64
Knöfler M, Haider S, Saleh L, Pollheimer J, Gamage TKJB, James J (2019) Human placenta and trophoblast development: key molecular mechanisms and model systems. Cell Mol Life Sci. https://doi.org/10.1007/s00018-019-03104-6
Tamagawa T, Ishiwata I, Saito S (2004) Establishment and characterization of a pluripotent stem cell line derived from human amniotic membranes and initiation of germ layers in vitro. Hum Cell 17(3):125–130
Moraghebi R, Kirkeby A, Chaves P, Rönn RE, Sitnicka E, Parmar M et al (2017) Term amniotic fluid: an unexploited reserve of mesenchymal stromal cells for reprogramming and potential cell therapy applications. Stem Cell Res Ther. https://doi.org/10.1186/s13287-017-0582-6
Gonzalez AC, Costa TF, Andrade Z, Medrado ARAP (2016) Wound healing—a literature review. Anais Brasileiros de Dermatologia 91(5):614–620
Abumaree MH, Al Jumah MA, Kalionis B, Jawdat D, Al Khaldi A, AlTalabani AA et al (2013) Phenotypic and functional characterization of mesenchymal stem cells from chorionic villi of human term placenta. Stem Cell Rev Rep 9(1):16–31
Mathew SA, Rajendran S, Gupta PK, Bhonde R (2013) Modulation of physical environment makes placental mesenchymal stromal cells suitable for therapy. Cell Biol Int 37(11):1197–1204
Abomaray FM, Al Jumah MA, Alsaad KO, Jawdat D, Al Khaldi A, AlAskar AS et al (2016) Phenotypic and functional characterization of mesenchymal stem/multipotent stromal cells from Decidua Basalis of human term placenta. Stem Cells Int 2016:1–18
Ferraro F, Celso CL, Scadden D (2010) Adult stem cells and their niches. Adv Exp Med Biol 695:155–168
Pereira RD, De Long NE, Wang RC, Yazdi FT, Holloway AC, Raha S (2015) Angiogenesis in the placenta: the role of reactive oxygen species signaling. Biomed Res Int 2015:1–12
Antoniadou E, David AL (2016) Placental stem cells. Best Pract Res Clin Obstetr Gynaecol 31:13–29
Abdulrazzak H, Moschidou D, Jones G, Guillot PV (2010) Biological characteristics of stem cells from foetal, cord blood and extraembryonic tissues. J R Soc Interface 7(Suppl 6):S689–S706
Barlow S, Brooke G, Chatterjee K, Price G, Pelekanos R, Rossetti T et al (2008) Comparison of human placenta- and bone marrow-derived multipotent mesenchymal stem cells. Stem Cells Dev 17(6):1095–1108
Kusuma GD, Brennecke SP, O’Connor AJ, Kalionis B, Heath DE (2017) Decellularized extracellular matrices produced from immortal cell lines derived from different parts of the placenta support primary mesenchymal stem cell expansion. PLOS One 12(2):e0171488
Lee M-Y, Huang J-P, Chen Y-Y, Aplin JD, Wu Y-H, Chen C-Y et al (2009) Angiogenesis in differentiated placental multipotent mesenchymal stromal cells is dependent on integrin α5β1. PLoS One 4(10):e6913
Li G, Zhang X, Wang H, Wang X, Meng C, Chan C et al (2009) Comparative proteomic analysis of mesenchymal stem cells derived from human bone marrow, umbilical cord, and placenta: implication in the migration. Proteomics 9(1):20–30
Kamprom W, Kheolamai P, U-Pratya Y, Supokawej A, Wattanapanitch M, Laowtammathron C et al (2016) Endothelial progenitor cell migration-enhancing factors in the secretome of placental-derived mesenchymal stem cells. Stem Cells Int 2016:1–13
Le Blanc K, Ringdén O (2005) Immunobiology of human mesenchymal stem cells and future use in hematopoietic stem cell transplantation. Biol Blood Marrow Transpl 11(5):321–334
Talwadekar MD, Kale VP, Limaye LS (2015) Placenta-derived mesenchymal stem cells possess better immunoregulatory properties compared to their cord-derived counterparts—a paired sample study. Sci Rep 5:15784
Lee JM, Jung J, Lee H-J, Jeong SJ, Cho KJ, Hwang S-G et al (2012) Comparison of immunomodulatory effects of placenta mesenchymal stem cells with bone marrow and adipose mesenchymal stem cells. Int Immunopharmacol 13(2):219–224
He S, Gleason J, Fik-Rymarkiewicz E, DiFiglia A, Bharathan M, Morschauser A et al (2017) Human placenta-derived mesenchymal stromal-like cells enhance angiogenesis via T cell-dependent reprogramming of macrophage differentiation: PDA-002 enhances angiogenesis via immunomodulation. Stem Cells 35(6):1603–1613
Abumaree MH, Al Jumah MA, Kalionis B, Jawdat D, Al Khaldi A, Abomaray FM et al (2013) Human placental mesenchymal stem cells (pMSCs) play a role as immune suppressive cells by shifting macrophage differentiation from inflammatory M1 to anti-inflammatory M2 macrophages. Stem Cell Rev Rep 9:620–641
Choi JH, Jung J, Na K-H, Cho KJ, Yoon TK, Kim GJ (2014) Effect of mesenchymal stem cells and extracts derived from the placenta on trophoblast invasion and immune responses. Stem Cells Dev 23(2):132–145
Chang C-J, Yen M-L, Chen Y-C, Chien C-C, Huang H-I, Bai C-H et al (2006) Placenta-derived multipotent cells exhibit immunosuppressive properties that are enhanced in the presence of interferon-γ. Stem Cells 24(11):2466–2477
Jones BJ, Brooke G, Atkinson K, McTaggart SJ (2007) Immunosuppression by placental indoleamine 2,3-dioxygenase: a role for mesenchymal stem cells. Placenta 28(11–12):1174–1181
Selmani Z, Naji A, Zidi I, Favier B, Gaiffe E, Obert L et al (2008) Human leukocyte antigen-G5 secretion by human mesenchymal stem cells is required to suppress T lymphocyte and natural killer function and to induce CD4 CD25 FOXP3 regulatory T cells. Stem Cells 26:212–222
Alshabibi MA, Khatlani T, Abomaray FM, AlAskar AS, Kalionis B, Messaoudi SA et al (2018) Human decidua basalis mesenchymal stem/stromal cells protect endothelial cell functions from oxidative stress induced by hydrogen peroxide and monocytes. Stem Cell Res Ther. https://doi.org/10.1186/s13287-018-1021-z
Liao S, Zhang Y, Ting S, Zhen Z, Luo F, Zhu Z et al (2019) Potent immunomodulation and angiogenic effects of mesenchymal stem cells versus cardiomyocytes derived from pluripotent stem cells for treatment of heart failure. Stem Cell Res Ther 10(1):78
Bianco P, Robey PG, Simmons PJ (2008) Mesenchymal stem cells: revisiting history, concepts, and assays. Cell Stem Cell 2(4):313–319
Liang L, Li Z, Ma T, Han Z, Du W, Geng J et al (2017) Transplantation of human placenta-derived mesenchymal stem cells alleviates critical limb ischemia in diabetic nude rats. Cell Transpl 26(1):45–61
Meraviglia V, Vecellio M, Grasselli A, Baccarin M, Farsetti A, Capogrossi MC et al (2012) Human chorionic villus mesenchymal stromal cells reveal strong endothelial conversion properties. Differentiation 83(5):260–270
Watt SM, Gullo F, van der Garde M, Markeson D, Camicia R, Khoo CP et al (2013) The angiogenic properties of mesenchymal stem/stromal cells and their therapeutic potential. Br Med Bull 108(1):25–53
Zahavi-Goldstein E, Blumenfeld M, Fuchs-Telem D, Pinzur L, Rubin S, Aberman Z et al (2017) Placenta-derived PLX-PAD mesenchymal-like stromal cells are efficacious in rescuing blood flow in hind limb ischemia mouse model by a dose- and site-dependent mechanism of action. Cytotherapy. https://doi.org/10.1016/j.jcyt.2017.09.010
Komaki M, Numata Y, Morioka C, Honda I, Tooi M, Yokoyama N et al (2017) Exosomes of human placenta-derived mesenchymal stem cells stimulate angiogenesis. Stem Cell Res Ther. https://doi.org/10.1186/s13287-017-0660-9
Restrepo Y, Merle M, Petry D, Michon J (1985) Empty perineurial tube graft used to repair a digital nerve: a first case report. Microsurgery 6(2):73–77
Clark D, Nakamura M, Miclau T, Marcucio R (2017) Effects of aging on fracture healing. Curr Osteoporos Rep 15:601. https://doi.org/10.1007/s11914-017-0413-9
Liang T, Zhu L, Gao W, Gong M, Ren J, Yao H et al (2017) Coculture of endothelial progenitor cells and mesenchymal stem cells enhanced their proliferation and angiogenesis through PDGF and Notch signaling. FEBS Open Bio 7(11):1722–1736
DeCicco-Skinner KL, Henry GH, Cataisson C, Tabib T, Gwilliam JC, Watson NJ et al (2014) Endothelial cell tube formation assay for the in vitro study of angiogenesis. J Vis Exp 91:51312. https://doi.org/10.3791/51312
König J, Weiss G, Rossi D, Wankhammer K, Reinisch A, Kinzer M et al (2015) Placental mesenchymal stromal cells derived from blood vessels or avascular tissues: what is the better choice to support endothelial cell function? Stem Cells Dev 24(1):115–131
Cuiffo BG, Karnoub AE (2012) Mesenchymal stem cells in tumor development: emerging roles and concepts. Cell Adhes Migr 6(3):220–230
Makhoul G, Jurakhan R, Jaiswal PK, Ridwan K, Li L, Selvasandran K et al (2016) Conditioned medium of H9c2 triggers VEGF dependent angiogenesis by activation of p38/pSTAT3 pathways in placenta derived stem cells for cardiac repair. Life Sci 153:213–221
Kadekar D, Rangole S, Kale V, Limaye L (2016) Conditioned medium from placental mesenchymal stem cells reduces oxidative stress during the cryopreservation of ex vivo expanded umbilical cord blood cells. PLOS One 11(10):e0165466
Prockop DJ (2007) “Stemness” does not explain the repair of many tissues by mesenchymal stem/multipotent stromal cells (MSCs). Clin Pharmacol Ther 82(3):241–243
Caplan AI (2007) Adult mesenchymal stem cells for tissue engineering versus regenerative medicine. J Cell Physiol 213(2):341–347
Yu B, Zhang X, Li X (2014) Exosomes derived from mesenchymal stem cells. Int J Mol Sci 15(3):4142–4157
Phinney DG, Pittenger MF (2017) Concise review: MSC-derived exosomes for cell-free therapy: MSC-derived exosomes. Stem Cells 35(4):851–858
Tooi M, Komaki M, Morioka C, Honda I, Iwasaki K, Yokoyama N et al (2016) Placenta mesenchymal stem cell derived exosomes confer plasticity on fibroblasts: a novel function of MSC-exosomes in vitro. J Cell Biochem 117(7):1658–1670
Gong M, Yu B, Wang J, Wang Y, Liu M, Paul C et al (2017) Mesenchymal stem cells release exosomes that transfer miRNAs to endothelial cells and promote angiogenesis. Oncotarget. https://doi.org/10.18632/oncotarget.16778
Hua Z, Lv Q, Ye W, Wong C-KA, Cai G, Gu D et al (2006) MiRNA-directed regulation of VEGF and other angiogenic factors under hypoxia. PLoS One 1(1):e116
Donker RB, Mouillet JF, Chu T, Hubel CA, Stolz DB, Morelli AE et al (2012) The expression profile of C19MC microRNAs in primary human trophoblast cells and exosomes. Mol Hum Reprod 18(8):417–424
Delorme-Axford E, Donker RB, Mouillet J-F, Chu T, Bayer A, Ouyang Y et al (2013) Human placental trophoblasts confer viral resistance to recipient cells. Proc Natl Acad Sci 110(29):12048–12053
Kuehbacher A, Urbich C, Dimmeler S (2008) Targeting microRNA expression to regulate angiogenesis. Trends Pharmacol Sci 29(1):12–15
Liang X, Zhang L, Wang S, Han Q, Zhao RC (2016) Exosomes secreted by mesenchymal stem cells promote endothelial cell angiogenesis by transferring miR-125a. J Cell Sci 129(11):2182–2189
Wang B, Jia H, Zhang B, Wang J, Ji C, Zhu X et al (2017) Pre-incubation with hucMSC-exosomes prevents cisplatin-induced nephrotoxicity by activating autophagy. Stem Cell Res Ther. https://doi.org/10.1186/s13287-016-0463-4
Vizoso F, Eiro N, Cid S, Schneider J, Perez-Fernandez R (2017) Mesenchymal stem cell secretome: toward cell-free therapeutic strategies in regenerative medicine. Int J Mol Sci 18(9):1852
Liang L (2019) Prenatal mesenchymal stem cell secretome and its clinical implication. In: Han ZC, Takahashi TA, Han Z, Li Z (eds) Perinatal stem cells. Springer, Singapore, pp 167–173. https://doi.org/10.1007/978-981-13-2703-2_13
Marquez-Curtis LA, Janowska-Wieczorek A (2013) Enhancing the migration ability of mesenchymal stromal cells by targeting the SDF-1/CXCR80 axis. Biomed Res Int 2013:1–15
Stolzing A, Jones E, McGonagle D, Scutt A (2008) Age-related changes in human bone marrow-derived mesenchymal stem cells: consequences for cell therapies. Mech Ageing Dev 129(3):163–173
Carmeliet P (2003) Angiogenesis in health and disease. Nat Med 9(6):653–660
McBeath R, Pirone DM, Nelson CM, Bhadriraju K, Chen CS (2004) Cell shape, cytoskeletal tension, and RhoA regulate stem cell lineage commitment. Dev Cell 6(4):483–495
Pacini S, Petrini I (2014) Are MSCs angiogenic cells? New insights on human nestin-positive bone marrow-derived multipotent cells. Front Cell Dev Biol 2:20
Charnock-Jones DS (2016) Placental hypoxia, endoplasmic reticulum stress and maternal endothelial sensitisation by sFLT1 in pre-eclampsia. J Reprod Immunol 114:81–85
Xu C, Li X, Guo P, Wang J (2017) Hypoxia-induced activation of JAK/STAT3 signaling pathway promotes trophoblast cell viability and angiogenesis in preeclampsia. Med Sci Monit 23:4909–4917
Li Y, Liu H, Cao L, Wu Y, Shi X, Qiao F et al (2017) Hypoxia downregulates the angiogenesis in human placenta via Notch1 signaling pathway. J Huazhong Univ Sci Technol [Medical Sciences] 37(4):541–546
Fujii T, Nagamatsu T, Morita K, Schust DJ, Iriyama T, Komatsu A et al (2017) Enhanced HIF2α expression during human trophoblast differentiation into syncytiotrophoblast suppresses transcription of placental growth factor. Sci Rep. https://doi.org/10.1038/s41598-017-12685-w
de Oliveira LF, Almeida TR, Ribeiro Machado MP, Cuba MB, Alves AC, da Silva MV et al (2015) Priming mesenchymal stem cells with endothelial growth medium boosts stem cell therapy for systemic arterial hypertension. Stem Cells Int 2015:1–12
Mizukami T, Iso Y, Sato C, Sasai M, Spees JL, Toyoda M et al (2016) Priming with erythropoietin enhances cell survival and angiogenic effect of mesenchymal stem cell implantation in rat limb ischemia. Regener Ther 4:1–8
Mathew SA, Bhonde RR (2018) Omega-3 polyunsaturated fatty acids promote angiogenesis in placenta derived mesenchymal stromal cells. Pharmacol Res 132:90–98
Wang J, Shi Y, Zhang L, Zhang F, Hu X, Zhang W et al (2014) Omega-3 polyunsaturated fatty acids enhance cerebral angiogenesis and provide long-term protection after stroke. Neurobiol Dis 68:91–103
Hitzerd E, Broekhuizen M, Neuman RI, Colafella KMM, Merkus D, Schoenmakers S et al (2019) Human placental vascular reactivity in health and disease: implications for the treatment of pre-eclampsia. Curr Pharm Des 25(5):505–527
Fuchi N, Miura K, Doi H, Li T-S, Masuzaki H (2017) Feasibility of placenta-derived mesenchymal stem cells as a tool for studying pregnancy-related disorders. Sci Rep 7:46220
Kim J, Piao Y, Pak YK, Chung D, Han YM, Hong JS et al (2015) Umbilical cord mesenchymal stromal cells affected by gestational diabetes mellitus display premature aging and mitochondrial dysfunction. Stem Cells Dev 24(5):575–586
Mathew SA, Bhonde R (2017) Mesenchymal stromal cells isolated from gestationally diabetic human placenta exhibit insulin resistance, decreased clonogenicity and angiogenesis. Placenta 59:1–8
Francki A, Labazzo K, He S, Baum EZ, Abbot SE, Herzberg U et al (2016) Angiogenic properties of human placenta-derived adherent cells and efficacy in hindlimb ischemia. J Vasc Surg 64(3):746–756
Xie N, Li Z, Adesanya TM, Guo W, Liu Y, Fu M et al (2016) Transplantation of placenta-derived mesenchymal stem cells enhances angiogenesis after ischemic limb injury in mice. J Cell Mol Med 20(1):29–37
Alshareeda AT, Rakha E, Alghwainem A, Alrfaei B, Alsowayan B, Albugami A et al (2018) The effect of human placental chorionic villi derived mesenchymal stem cell on triple-negative breast cancer hallmarks. PLOS One 13(11):e0207593
Lee J-K, Park S-R, Jung B-K, Jeon Y-K, Lee Y-S, Kim M-K et al (2013) Exosomes derived from mesenchymal stem cells suppress angiogenesis by down-regulating VEGF expression in breast cancer cells. PLoS One 8(12):e84256
Zhang D, Zheng L, Shi H, Chen X, Wan Y, Zhang H et al (2014) Suppression of peritoneal tumorigenesis by placenta-derived mesenchymal stem cells expressing endostatin on colorectal cancer. Int J Med Sci 11(9):870–879
Kim K-S, Park J-M, Kong T, Kim C, Bae S-H, Kim HW et al (2016) Retinal angiogenesis effects of TGF-β1 and paracrine factors secreted from human placental stem cells in response to a pathological environment. Cell Transpl 25(6):1145–1157
Ji L, Zhang L, Li Y, Guo L, Cao N, Bai Z et al (2017) MiR-136 contributes to pre-eclampsia through its effects on apoptosis and angiogenesis of mesenchymal stem cells. Placenta 50:102–109
Lazarus HM, Haynesworth SE, Gerson SL, Rosenthal NS, Caplan AI (1995) Ex vivo expansion and subsequent infusion of human bone marrow-derived stromal progenitor cells (mesenchymal progenitor cells): implications for therapeutic use. Bone Marrow Transpl 16(4):557–564
Prather WR, Toren A, Meiron M, Ofir R, Tschope C, Horwitz EM (2009) The role of placental-derived adherent stromal cell (PLX-PAD) in the treatment of critical limb ischemia. Cytotherapy 11(4):427–434
Kadekar D, Kale V, Limaye L (2015) Differential ability of MSCs isolated from placenta and cord as feeders for supporting ex vivo expansion of umbilical cord blood derived CD34 + cells. Stem Cell Res Ther 6:201
Du W, Li X, Chi Y, Ma F, Li Z, Yang S et al (2016) VCAM-1 + placenta chorionic villi-derived mesenchymal stem cells display potent pro-angiogenic activity. Stem Cell Res Ther 7:49
Heazlewood CF, Sherrell H, Ryan J, Atkinson K, Wells CA, Fisk NM (2014) High incidence of contaminating maternal cell overgrowth in human placental mesenchymal stem/stromal cell cultures: a systematic review: maternal contamination in placental MSCs: a review. Stem Cells Transl Med 3(11):1305–1311
Sardesai VS, Shafiee A, Fisk NM, Pelekanos RA (2017) Avoidance of maternal cell contamination and overgrowth in isolating fetal chorionic villi mesenchymal stem cells from human term placenta: determinants of pure feto-placental MSC isolation. Stem Cells Transl Med 6(4):1070–1084
Mathews S, Lakshmi Rao K, Suma Prasad K, Kanakavalli MK, Govardhana Reddy A, Avinash Raj T et al (2015) Propagation of pure fetal and maternal mesenchymal stromal cells from terminal chorionic villi of human term placenta. Sci Rep 5:10054
Alrefaei GI, Al-Karim S, Ayuob NN, Ali SS (2015) Does the maternal age affect the mesenchymal stem cell markers and gene expression in the human placenta? What is the evidence? Tissue Cell 47(4):406–419
Acknowledgements
The authors wish to thank the Vice-Chancellor and Registrar, Manipal Academy of Higher Education, India, for extending all the facilities needed to carry out the present work. We would also like to thank Dr. Gopal Pande, Dean SORM, for his continuous guidance and support and Mr. Febin Varghese for his contribution to the graphic work.
Author information
Authors and Affiliations
Contributions
Suja A. Mathew: conceived, designed and wrote the paper; Charuta Naik: collected the data and prepared the image; Paul A. Cahill: critical editing and writing of the paper; Ramesh Bhonde: designed and critical editing of the paper.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest in their study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mathew, S.A., Naik, C., Cahill, P.A. et al. Placental mesenchymal stromal cells as an alternative tool for therapeutic angiogenesis. Cell. Mol. Life Sci. 77, 253–265 (2020). https://doi.org/10.1007/s00018-019-03268-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00018-019-03268-1