Abstract
Liposarcoma (LPS) is the most common soft tissue sarcoma and accounts for approximately 20 % of all adult sarcomas. Current treatment modalities (surgery, chemotherapy, and radiotherapy) all have limitations; therefore, molecularly driven studies are needed to improve the identification and increased understanding of genetic and epigenetic deregulations in LPS if we are to successfully target specific tumorigenic drivers. It can be anticipated that such biology-driven therapeutics will improve treatments by selectively deleting cancer cells while sparing normal tissues. This review will focus on several therapeutically actionable molecular markers identified in well-differentiated LPS and dedifferentiated LPS, highlighting their potential clinical applicability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Soft tissue sarcomas (STSs) are a rare (<1 % tumors in adults) heterogeneous group of diseases arising from mesenchymal cells. In the United States, there are an estimated 11,930 new cases of STS and 4870 deaths annually [1]. Liposarcoma (LPS) is the most common STS, accounting for 24 % of extremity and 45 % of retroperitoneal occurrences [2]. LPS is a heterogeneous group of malignant adipocytic tumors that are morphologically classified into four subtypes: (1) well differentiated, (2) dedifferentiated, (3) myxoid, and (4) pleomorphic [2, 3]. Depending on the specific subtype and location, liposarcomas can recur in over 80 % of cases, and mortality rates that range from 1 to 90 % highlight the importance of accurate classification [4, 5].
WD and DDLPS embody the most common liposarcoma histologies observed clinically and are the focus of this review. These two subtypes have both common and unique features that contribute to their clinical behavior. Identifying the molecular underpinnings of LPS is a critical step in understanding the biology of LPS. Recent developments in genomic approaches have provided critical information regarding genetic aberrations driving tumorigenesis, histological characterization, and identification of new biomarkers potentially useful for targeted drug therapies in patients.
Clinical presentation
WDLPS accounts for approximately 40–45 % of all LPS and is characterized as a low-grade tumor with a high local recurrence rate of 60 % at 5 year follow-up [6, 7]. The majority of WDLPS arises in the retroperitoneum; however, it can be found in the deep soft tissue of the thigh, paratesticular area, and the mediastinum [8, 9]. The location of this tumor is an important prognostic factor as tumors found in the retroperitoneum are more capable of recurrence compared with the extremities (>40 % compared with <2 %; respectively) [2, 8, 10]. Importantly, in as many as 40 % of recurrent lesions within the retroperitoneum, WDLPS manifests a dedifferentiated component [8–11].
In 1979, Evans first described the histopathological features of dedifferentiated regions that were observed in recurrent, initially well-differentiated liposarcomas [12]. DDLPS is categorized as an intermediate—to high-grade lesion and may arise as a primary, or “de novo” lesion (90 % of cases) or as recurrence of a prior WDLPS (10 % of cases, i.e., secondary DDLPS) [7, 13–15]. Similar to WD, DDLPS commonly originates in the retroperitoneum and exhibit high local recurrence [13, 16]. Clinically, DDLPS is much more aggressive than WDLPS with a metastatic rate of approximately 15–20 % and a dismal 30 % 5-year overall survival (OS) compared with 90 % OS for WD [2, 7, 9, 11, 13, 17].
The WD/DDLPS dichotomy
Morphologically, these tumors are remarkably different in other regards as well. WDLPS is composed of malignant adipocytes and spindle cells showing fibroblastic/myofibroblastic differentiation with aberrantly enlarged and hyperchromatic nuclei (Fig. 1a, b) On gross examination, these tumors show solid, highly cellular, non-lipomatous dedifferentiation areas abruptly demarcated from the often multi-nodular and yellow mass that constitutes the well-differentiated portion of the tumor (Fig. 1c) [2, 13, 17–20]. In most cases, DDLPS is no longer recognizably adipocytic; however, lipogenic features similar to those seen in pleomorphic liposarcoma have been observed [21, 22].
Well-differentiated and dedifferentiated liposarcoma. a Hematoxylin and eosin stain of WDLPS (magnification ×200). Image shows a lipomatous tumor with broad and cellular septa containing hyperchromatic cells. b Hyperchromasia of the atypical cells, consistent with atypical lipomatous tumor/well-differentiated liposarcoma (magnification ×400). c Hematoxylin and eosin stain of DDLPS (magnification ×200). Image demonstrates the biphasic malignant neoplasm composed of a high-grade spindle cell sarcoma separated from a well-differentiated fatty tumor by a fibrous capsule. The inset on the lower left shows scattered single hyperchromatic cells within the fatty tumor consistent with the WDLPS component of DDLPS. d Positive MDM2 gene amplification by fluorescence in situ hybridization observed in both WD and DDLPS
These morphological and clinical observations give rise to an unexplained conundrum; WD/DDLPS has a common origin and entail a process of progressive evolution from WD to DDLPS or do they ascend from two different cellular populations, representing two distinct malignancies cohabitating in the same anatomic locus? To address these possibilities, profiling studies seeking to identify the unique drivers of each subtype have been performed.
In support to the first theory, genomic profiling has identified common molecular aberrations in WD/DDLPS. Supernumerary ring and/or giant rod chromosomes containing amplified segments from the 12q13–15 region are observed in both WD and DDLPS [2, 23]. This alteration can be utilized for pathological diagnosis using comparative genomic hybridization to detect DNA sequence copy number changes, thereby distinguishing WD and DDLPS from benign lipomas [24] (Fig. 1d). Additional molecular studies have identified common molecular underpinnings in LPS [25]. In both WD and DDLPS, murine double minute type 2 (MDM2) is the most frequently amplified gene (100 % of DDLPS cases), followed closely by cyclin-dependent kinase 4 (CDK4; amplified in >90 % of cases) [2, 26]. It has been proposed that co-amplification of MDM2 and CDK4, which both reside within the 12q13–15 amplicon, are potentially the initiating “driving” factor in these tumors [26–29]. As a result, extensive studies targeting the MDM2 and CDK4 oncogenes as an anti-LPS therapy have been conducted.
To further explain the potential WD/DDLPS disease progression, Shimoji et al. investigated the heterogeneity of LPS tumors, seeking to identify more aggressive cellular populations. Using cDNA microarray analysis, they observed that the WDLPS component of a DDLPS lesion clustered independently from that of a pure WDLPS tumor, suggesting that perhaps, only a subset of WDLPS is capable of progressing to DDLPS [30].
Although similar to WD, DDLPS has an overall more complex genetic profile, which may contribute to its more aggressive phenotype. In support of this second theory, studies considering the differences between WD and DDLPS as separate entities have been performed. Matushansky et al. demonstrated the genomic resemblance of liposarcoma histologies to the various differentiation stages of mesenchymal stem cells to mature adipose tissue, reporting that DDLPS and WDLPS potentially arise from different stages of development [31].
Molecular targets and therapeutic implications
Despite the two conflicting theories of disease origin, the question is still unresolved about which additional molecular alterations may account for the very different behavior and prognosis of WD vs DD LPS. Several studies have focused on the underlying mechanisms driving these two distinct LPS subtypes and their therapeutic implications. To date, surgery remains the cornerstone of potentially curative treatment for both WD and DDLPS [32]. However, in either disease, the majority of patients will manifest local recurrence and require additional therapeutic management [7]. The poor response to systemic chemotherapy emphasizes the necessity to therapeutically target molecular aberrations as possible new strategies for WD/DDLPS patients and, hence, the effort at identification of actionable targets and biology-driven therapies in this disease.
MDM2 amplification leads to the ubiquitination and degradation of tumor suppressor p53 (TP53); as a result, p53-reactivation via MDM2 inhibition may comprise an ideal target for DDLPS therapy. Recent work performed in our laboratory exploited this possibility by utilizing a small-molecule MDM2 inhibitor, SAR405838 (Sanofi-Aventis) to disrupt this specific protein–protein interaction [33]. This approach restored the p53 pathway, inducing cell cycle arrest and ultimately apoptosis. SAR405838 was compared with Nutlin-3a and MI-219, which are other small molecules that target MDM2. These preclinical results highlight the contribution of the MDM2-p53 axis in DDLPS tumorigenesis and the potential utilization of SAR405838 as a therapeutic option for patients suffering from this disease.
CDK4, the second most observed molecular irregularity in WD and DDLPS, has also been implicated as a therapeutic target. Inhibition of CDK4 with NVP-LEE011 (LEE011; Novartis) decreases cell proliferation via G1/G0 arrest, due to the reduction of phosphorylation on retinoblastoma (pRb) [34]. Although continuous exposure to LEE011 eventually led to reentry into the cell cycle, a repeat exposure to this drug reinstated the cell cycle arrest and halted in proliferation. This points to the ability of cancer cells to mount a dynamic mechanism that can overcome drug sensitivity, and also suggests the importance of dosage scheduling and the applicability of dual-target strategy to elicit a cytotoxic synergy as an additional relevant option.
The contribution to tumorigenesis and disease progression from additional oncogenes residing in the 12q amplicon (HMGA2, FRS2, STAT6, and so on) has been an on-going investigation of many researchers [28, 35, 36]. This delineated chromosomal amplification exemplifies the genomic complexity and heterogeneity in LPS. In addition, genomic amplifications in 1p32, 1q21–24, and/or 6q23 (which reside the oncogenes JUN, ASK1, and MAP3K5, respectively) are observed frequently in DDLPS and may contribute to the more aggressive and stem-like phenotype that could contribute to worse prognosis [37–41]. Added targets that reside outside the 12q13–15 amplicon, such as c-JUN and ASK1, have also been investigated [40]. Both proteins act downstream on peroxisome proliferator-activated receptor gamma (PPAR-γ), suggesting a key role in adipocyte differentiation into DD or WD [38, 39, 42]. Together, these results demonstrate that high expression of c-JUN may play a role in the loss of early stage adipogenesis, and consequently, its inhibition may offer therapeutic implication in DDLPS.
Tyrosine kinase receptors have been utilized as key targets for molecular based therapies due to their direct impact on signaling pathways. Aberrant activation of the Met pathway has been implicated in multiple tumor types, including sarcoma [43–47], and combination treatment with standard chemotherapy has been demonstrated to be effective against proliferation in multiple myeloma [48]. In LPS, increased Met pathway activation has been observed [49]. Ectopic expression of the only known activating Met ligand, hepatocyte growth factor (HGF) results in increased proliferation and motility in DDLPS cells, while Met inhibition impairs the growth of DDLPS cell lines in vivo [50]. Thus, the Met pathway may be a potential therapeutic target for DDLPS treatment.
Taken together, identification of molecular aberrations potentially driving LPS tumor establishment and progression has demonstrated clinical application; however, there is still much to be learned. For example, the degree of MDM2 amplification is variable, and identifying a specific threshold may identify a subset of patients who benefit better from specific therapeutic combinations [51]. This study stratified DDLPS cell lines by their relative degree of MDM2 amplification and found that doxorubicin was more effective in the lower expressing MDM2 subset, while small molecule MDM2 inhibitors were more potent when MDM2 was expressed at higher levels. This study exemplifies the need to carefully evaluate the contribution of a molecular event and also illustrates the limitations of such molecular studies, i.e., even the most frequently studied LPS molecular aberration (MDM2) requires better characterization if it is to serve as a meaningful predictive and prognostic marker in LPS.
miRNAs contribution to liposarcoma progression
Recently, not only genes and proteins, but also miRNAs have been shown to be useful in understanding the WDLPS/DDLPS dilemma and to gain insight into the basis of liposarcoma progression. miRNAs are short (circa 22 nucleotides in length) non-coding RNAs (ncRNAs) that regulate gene expression by binding to specific mRNA targets and promoting their degradation and/or translational inhibition. A central role in LPS has been shown for miR-143; miR-143, which is abundant in normal adipose tissue, was found to be underexpressed in WDLPS, and its expression decreased further as the tumor progressed to DDLPS. Restoring miR-143 expression in DDLPS cells inhibited proliferation and induced apoptosis by targeting the gene network that includes: B-cell lymphoma 2 (BCL2), DNA Topoisomerase II (TOP2A), protein regulator of cytokinesis 1 (PRC1), and polo-like kinase 1 (PLK1) [52].
miR-145 and miR-451 have been also proposed to have important role in LPS as they can act as tumor suppressors in adipose tissue; overexpression of mR-145 and miR-451 in LPS cell lines decreases cellular proliferation rate, impairs cell cycle progression, and induces apoptosis [53]. In 2013, an interesting work by Lee et al. revealed the contribution of miR-26a-2 to LPS tumorigenesis, identifying a new target gene of miR-26a-2, regulator of chromosome condensation and BTB domain-containing protein 1 (RCBTB1). RCBTB1 is located at 13q12.3–q14.3, a region responsible for loss of heterozygosity in LPS. As a regulator of the DNA damage/repair pathway and apoptosis, inhibition of RCBTB1 by overexpression of miR-26a-2 rendered LPS cells more resistant to apoptotic stress [54].
The important function of miR-155 and β-catenin signaling in progression of WDLPS/DDLPS was established by Zhang et al. They found that miR-155 is highly expressed in human WD/DDLPS and contributes to the tumorigenic phenotype of these malignancies through the regulation of casein kinase 1α (CK1α), which results in the activation of the β-catenin pathway. β-catenin and its downstream effector cyclin D1 were found to be overexpressed in all human DDLPS cell lines compared with pre-adipocytes and adipocytes and were also shown to induce DDLPS cell proliferation and cell cycle progression [55].
To add further complexity to this picture, it has been shown that extracellular vesicles, such as exosomes, macrovesicles, and apoptotic bodies, contain miRNAs with LPS-relevant functions [56]. It is now well established that transfer of genetic information in the form of RNA exists and that this form of transfer between cells is functional relevant by causing gene silencing in recipient cells. This newly discovered manner of genetic exchange between cells opens a new possibility of how adjacent cells within an organ may communicate and how miRNAs can affect a cell type or a tissue remote from where it is produced [57]. Increasing evidence suggests that this form of communication occurs in various processes and in pathological situations, including tumor development. In particular, extracellular miRNAs could be important regulators of tumor microenvironment [58]. This field of research is still growing, and our group is focusing on how exosomal miRNAs associated with LPS could perhaps enhance liposarcomagenesis and dedifferentiation by delivering tumor-promoting miRNAs to adjacent and distant recipient cells, hopefully lending new insight into our understanding of the growth, and malignant behavior of liposarcoma.
Biomarker potential in WD/DDLPS
Early biomarker cancer detection remains a major challenge in malignant disease but holds the promise of resulting in more favorable disease outcomes. In WD/DDLPS, in particular, new biomarkers could help to diagnose recurrence (and dedifferentiation) prior to the currently available radiologic detectability time points. Unfortunately, early predictive/prospective biomarker signatures are not yet developed for those patients, many of whom will ultimately dedifferentiate, and are, therefore, at especially high mortality risk.
To understand the role of biomarkers in clinical research, it is important to recall that the term “biomarker” was defined by the National Institutes of Health as “a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention” or “any substance, structure, or process, that can be measured in the body or its products and influence or predict the incidence and outcome of disease” [59].
Prognostic markers have been associated with overall survival in soft tissue sarcoma, e.g., tumor size and depth, site, grade, and resection margins. Recently, hemoglobin, alkali phosphatase, and C-reactive protein were found to predict the patient outcome, as well as serum creatinine and albumin in liposarcoma [60, 61].
Understanding the relationship between measurable biological processes and clinical outcomes is vital to expand treatment for disease; therefore, several important questions to be considered include whether or not a biomarker expression correlates with tumor diagnosis and prognosis independent of the treatment received, and also whether or not a biomarker can predict a treatment effect if such effects are different for biomarker-positive vs biomarker-negative patients [62].
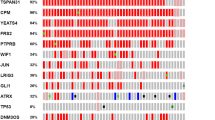
The assessment of multiple miRNA expression levels (also referred to as miRNA signatures) can accurately predict prognosis in a variety of cancers, and miRNAs expression patterns may be uniquely differing between cancer and normal tissues [63]. For example, miRNAs profiling in liposarcoma has been shown to discriminate WD and DDLPS from normal adipose tissue [64–67] and also to distinguish WDLPS from DDLPS [52, 67, 68].
A comprehensive miRNA expression database for a variety of human sarcoma types was generated by Sarver–Subramanian: the sarcoma microRNA expression database (S-MED) (http://www.oncomir.umn.edu/). These studies do not always report common and consistent results; discrepancies and differences reported in miRNAs signature can be due not only to the intratumoral heterogeneity that is the major cause for misinterpretation in most molecular test [69], but also because of the different subtypes of liposarcoma that may be considered together or separately and in comparison with normal fat, lipoma, or other liposarcoma subtypes.
miRNAs have become more attractive as biomarker given their easily retrievable presence in plasma and other body fluids, such as urine, saliva, and so on. From their first discovery in body fluids, multiple studies in a wide range of malignancies have shown unique miRNA biomarkers in the plasma or serum of cancer patients, potentially making them useful for routine clinical diagnosis.
MicroRNAs are considered to enter body fluids via three major mechanisms: (1) passive release from damaged tissue, (2) active secretion in cell-borne membrane vesicles (exosomes, microvesicles, and apoptotic bodies), (3) active secretion in macromolecular complexes associated with Argonaute (Ago) proteins (among other still unidentified proteins) and high-density lipoprotein (HDL) particles [70]. The biological relevance of blood-borne microRNAs is largely unknown, but such entities might be regarded as analogous to circulating hormones implicated in cell-to-cell communication within the tumor, and affecting the immune responses, facilitating angiogenesis, tumor invasion, and even metastatic propagation [71, 72]. However, the possibility that patient-derived serum or plasma miRNAs might serve as novel biomarkers for monitoring stage and diagnosis of sarcomas has not yet been extensively considered especially in WD/DDLPS [73–75].
In light of this reality, our group is putting much effort in identifying miRNAs as potential biomarkers in the peripheral blood of WD/DDLPS patients. Our preliminary observations demonstrate a typical circulating miRNA signature in WD/DDLPS patients that may be able to discriminate between healthy individual and patients with WD/DDLPS and also serve as biomarkers of drug resistance, which could help optimize individual treatment options (manuscript in preparation).
Conclusion
WD and DDLPS embody the most common liposarcoma histology. These two subtypes have both common and unique features, and the clinical outcome are very different: long-term survival is common in WDLPS, whereas DDLPS is markedly more aggressive and has metastatic possibilities. This WD/DDLPS dichotomy is not yet completely understood.
Unique in solid tumor oncology, the WD/DDLPS dichotomy in morphology, clinical behavior, molecular biology, and prognosis unequivocally identifies the need for biomarkers that enable earlier detection of clinical differences relevant to therapeutic intervention. Such efforts, already underway, hold the promise of new therapies and earlier detection of WD/DDLPS recurrences or progression, a critical effort if we are to improve outcomes for patients burdened by the specter of this very unfavorable malignant condition.
References
American Cancer Society (2015) Cancer facts & figures 2015. American Cancer Society, Atlanta
Fletcher CDM, Bridge J, Hogendoorn P et al (2013) World Health Organization Classification of tumours pathology and genetics of tumours of soft tissue and bone, 4th edn. IARC Press, Lyon
Doyle LA (2014) Sarcoma classification: an update based on the 2013 World Health Organization Classification of tumors of soft tissue and bone. Cancer 120:1763–1774. doi:10.1002/cncr.28657
Dalal KM, Kattan MW, Antonescu CR et al (2006) Subtype specific prognostic nomogram for patients with primary liposarcoma of the retroperitoneum, extremity, or trunk. Ann Surg 244:381–391. doi:10.1097/01.sla.0000234795.98607.00
Bonvalot S, Rivoire M, Castaing M et al (2009) Primary retroperitoneal sarcomas: a multivariate analysis of surgical factors associated with local control. J Clin Oncol 27:31–37. doi:10.1200/JCO.2008.18.0802
Dei Tos AP (2000) Liposarcoma: new entities and evolving concepts. Ann Diagn Pathol 4:252–266. doi:10.1053/adpa.2000.8133
Lahat G, Anaya DA, Wang X et al (2008) Resectable well-differentiated versus dedifferentiated liposarcomas: two different diseases possibly requiring different treatment approaches. Ann Surg Oncol 15:1585–1593. doi:10.1245/s10434-007-9805-x
Azumi N, Curtis J, Kempson RL, Hendrickson MR (1987) Atypical and malignant neoplasms showing lipomatous differentiation. A study of 111 cases. Am J Surg Pathol 11:161–183
Keung EZ, Hornick JL, Bertagnolli MM et al (2014) Predictors of outcomes in patients with primary retroperitoneal dedifferentiated liposarcoma undergoing surgery. J Am Coll Surg 218:206–217. doi:10.1016/j.jamcollsurg.2013.10.009
Fabre-Guillevin E, Coindre J-M, de Saint Aubain Somerhausen N et al (2006) Retroperitoneal liposarcomas: follow-up analysis of dedifferentiation after clinicopathologic reexamination of 86 liposarcomas and malignant fibrous histiocytomas. Cancer 106:2725–2733
Singer S, Antonescu CR, Riedel E, Brennan MF (2003) Histologic subtype and margin of resection predict pattern of recurrence and survival for retroperitoneal liposarcoma. Ann Surg 238:358–70. doi:10.1097/01.sla.0000086542.11899.38 (Discussion 370–371)
Evans HL (1979) Liposarcoma: a study of 55 cases with a reassessment of its classification. Am J Surg Pathol 3:507–523
Ghadimi MP, Al-Zaid T, Madewell J et al (2011) Diagnosis, management, and outcome of patients with dedifferentiated liposarcoma systemic metastasis. Ann Surg Oncol 18:3762–3770. doi:10.1245/s10434-011-1794-0
Evans HL, Khurana KK, Kemp BL, Ayala AG (1994) Heterologous elements in the dedifferentiated component of dedifferentiated liposarcoma. Am J Surg Pathol 18:1150–1157
Henricks WH, Chu YC, Goldblum JR, Weiss SW (1997) Dedifferentiated liposarcoma: a clinicopathological analysis of 155 cases with a proposal for an expanded definition of dedifferentiation. Am J Surg Pathol 21:271–281
Tseng WW, Madewell JE, Wei W et al (2014) Locoregional disease patterns in well-differentiated and dedifferentiated retroperitoneal liposarcoma: implications for the extent of resection? Ann Surg Oncol 21:2136–2143. doi:10.1245/s10434-014-3643-4
Thway K, Jones RL, Noujaim J et al (2016) Dedifferentiated Liposarcoma: updates on morphology, genetics, and therapeutic strategies. Adv Anat Pathol 23:30–40. doi:10.1097/PAP.0000000000000101
Evans HL (1979) Liposarcoma a study of 55 cases with a reassessment of its classification. Am J Surg Pathol 3(6):507–523
Henricks WH, Chu YC, Goldblum JR, Weiss SW (1997) Dedifferentiated Liposarcoma: a clinicopathological analysis of 155 cases with a proposal for an expanded definition of dedifferentiation. Am J Clin Pathol 21:271–281
Evans HL, Khurana KK, Kemp BL, Ayala AG (1994) Heterologous elements in the dedifferentiated components of dedifferentiated liposarcoma. Am J Clin Pathol 18:1077–1182
Mariño-Enríquez A, Fletcher CDM, Dal Cin P, Hornick JL (2010) Dedifferentiated liposarcoma with “homologous” lipoblastic (pleomorphic liposarcoma-like) differentiation: clinicopathologic and molecular analysis of a series suggesting revised diagnostic criteria. Am J Surg Pathol 34:1122–1131. doi:10.1097/PAS.0b013e3181e5dc49
Boland JM, Weiss SW, Oliveira AM et al (2010) Liposarcomas with mixed well-differentiated and pleomorphic features: a clinicopathologic study of 12 cases. Am J Surg Pathol 34:837–843. doi:10.1097/PAS.0b013e3181dbf2f7
Mandahl N, Höglund M, Mertens F et al (1994) Cytogenetic aberrations in 188 benign and borderline adipose tissue tumors. Genes Chromosomes Cancer 9:207–215
Szymanska J, Virolainen M, Tarkkanen M et al (1997) Overrepresentation of 1q21–23 and 12q13–21 in lipoma-like liposarcomas but not in benign lipomas: a comparative genomic hybridization study. Cancer Genet Cytogenet 99:14–18
Crago AM, Singer S (2011) Clinical and molecular approaches to well differentiated and dedifferentiated liposarcoma. Curr Opin Oncol 23:373–378. doi:10.1097/CCO.0b013e32834796e6
Italiano A, Bianchini L, Gjernes E et al (2009) Clinical and biological significance of CDK4 amplification in well-differentiated and dedifferentiated liposarcomas. Clin Cancer Res 15:5696–5703. doi:10.1158/1078-0432.CCR-08-3185
Pilotti S, Della Torre G, Lavarino C et al (1998) Molecular abnormalities in liposarcoma: role of MDM2 and CDK4-containing amplicons at 12q13–22. J Pathol 185:188–190. doi:10.1002/(SICI)1096-9896(199806)185:2<188:AID-PATH53>3.0.CO;2-2
Dei Tos AP, Doglioni C, Piccinin S et al (2000) Coordinated expression and amplification of the MDM2, CDK4, and HMGI-C genes in atypical lipomatous tumours. J Pathol 190:531–536
Segura-Sánchez J, González-Cámpora R, Pareja-Megia MJ et al (2006) Chromosome-12 copy number alterations and MDM2, CDK4 and TP53 expression in soft tissue liposarcoma. Anticancer Res 26:4937–4942
Shimoji T, Kanda H, Kitagawa T et al (2004) Clinico-molecular study of dedifferentiation in well-differentiated liposarcoma. Biochem Biophys Res Commun 314:1133–1140
Matushansky I, Hernando E, Socci ND et al (2008) A developmental model of sarcomagenesis defines a differentiation-based classification for liposarcomas. Am J Pathol 172:1069–1080. doi:10.2353/ajpath.2008.070284
Kollár A, Benson C (2014) Current management options for liposarcoma and challenges for the future. Expert Rev Anticancer Ther 14:297–306. doi:10.1586/14737140.2014.869173
Bill KLJ, Garnett J, Meaux I et al (2016) SAR405838: a novel and potent inhibitor of the MDM2:p53 axis for the treatment of dedifferentiated liposarcoma. Clin Cancer Res 22:1150–1160. doi:10.1158/1078-0432.CCR-15-1522
Zhang Y-X, Sicinska E, Czaplinski JT et al (2014) Antiproliferative Effects of CDK4/6 inhibition in CDK4-amplified human liposarcoma in vitro and in vivo. Mol Cancer Ther 13:2184–2193. doi:10.1158/1535-7163.MCT-14-0387
Sandberg AA (2004) Updates on the cytogenetics and molecular genetics of bone and soft tissue tumors: liposarcoma. Cancer Genet Cytogenet 155:1–24. doi:10.1016/j.cancergencyto.2004.08.005
Wang X, Asmann YW, Erickson-johnson MR et al (2011) High-resolution genomic mapping reveals consistent amplification of the fibroblast growth factor receptor substrate 2 gene in well-differentiated and dedifferentiated liposarcoma. Genes Chromosomes Cancer 858:849–858. doi:10.1002/gcc
Haluska FG, Huebner K, Isobe M et al (1988) Localization of the human JUN protooncogene to chromosome region 1p31-32. Proc Natl Acad Sci USA 85:2215–2218
Mariani O, Brennetot C, Coindre J-M et al (2007) JUN oncogene amplification and overexpression block adipocytic differentiation in highly aggressive sarcomas. Cancer Cell 11:361–374. doi:10.1016/j.ccr.2007.02.007
Snyder EL, Sandstrom DJ, Law K et al (2009) c-Jun amplification and overexpression are oncogenic in liposarcoma but not always sufficient to inhibit the adipocytic differentiation programme. J Pathol 218:292–300. doi:10.1002/path.2564
Chibon F, Mariani O, Derré J et al (2004) ASK1 (MAP3K5) as a potential therapeutic target in malignant fibrous histiocytomas with 12q14–q15 and 6q23 amplifications. Genes Chromosomes Cancer 40:32–37. doi:10.1002/gcc.20012
Schmidt H, Bartel F, Kappler M et al (2005) Gains of 13q are correlated with a poor prognosis in liposarcoma. Mod Pathol 18:638–644. doi:10.1038/modpathol.3800326
Wisdom R, Johnson RS, Moore C (1999) c-Jun regulates cell cycle progression and apoptosis by distinct mechanisms. EMBO J 18:188–197. doi:10.1093/emboj/18.1.188
Cortner J, Vande Woude GF, Rong S (1995) The Met-HGF/SF autocrine signaling mechanism is involved in sarcomagenesis. EXS 74:89–121
Rong S, Jeffers M, Resau JH et al (1993) Met Expression and sarcoma tumorigenicity. Cancer Res 53:5355–5360
Ferracini R, Olivero M, Di Renzo MF et al (1996) Retrogenic expression of the MET proto-oncogene correlates with the invasive phenotype of human rhabdomyosarcomas. Oncogene 12:1697–1705
Rao UN, Sonmez-Alpan E, Michalopoulos GK (1997) Hepatocyte growth factor and c-MET in benign and malignant peripheral nerve sheath tumors. Hum Pathol 28:1066–1070
Torres KE, Zhu Q-S, Bill K et al (2011) Activated MET is a molecular prognosticator and potential therapeutic target for malignant peripheral nerve sheath tumors. Clin Cancer Res 17:3943–3955. doi:10.1158/1078-0432.CCR-11-0193
Que W, Chen J (2011) Knockdown of c-Met inhibits cell proliferation and invasion and increases chemosensitivity to doxorubicin in human multiple myeloma U266 cells in vitro. Mol Med Rep 4:343–349. doi:10.3892/mmr.2011.426
Peng T, Zhang P, Liu J et al (2011) An experimental model for the study of well-differentiated and dedifferentiated liposarcoma; deregulation of targetable tyrosine kinase receptors. Lab Invest 91:392–403. doi:10.1038/labinvest.2010.185
Bill KLJ, Garnett J, Ma X et al (2015) The hepatocyte growth factor receptor as a potential therapeutic target for dedifferentiated liposarcoma. Lab Investig 95:951–961. doi:10.1038/labinvest.2015.62
Bill KLJ, Pollock RE, Chen J (2015) Sensitivity to doxorubicin and MDM2 inhibitors correlate with MDM2 levels in dedifferentiated liposarcoma (abstract). In: 20th Annual meeting Connective Tissue Oncology Society
Ugras S, Brill E, Jacobsen A et al (2011) Small RNA sequencing and functional characterization reveals microRNA-143 tumor suppressor activity in liposarcoma. Cancer Res 71:5659–5669. doi:10.1158/0008-5472
Gits CMM, Van Kuijk PF, Jonkers MBE et al (2014) MicroRNA expression profiles distinguish liposarcoma subtypes and implicate miR-145 and miR-451 as tumor suppressors. Int J Cancer 135:348–361. doi:10.1002/ijc.28694
Lee DH, Amanat S, Goff C et al (2013) Overexpression of miR-26a-2 in human liposarcoma is correlated with poor patient survival. Oncogenesis 2:e47. doi:10.1038/oncsis.2013.10
Zhang P, Bill K, Liu J et al (2012) MiR-155 is a liposarcoma oncogene that targets casein kinase-1α and enhances β-catenin signaling. Cancer Res 72:1751–1762. doi:10.1158/0008-5472.CAN-11-3027
Valadi H, Ekström K, Bossios A et al (2007) Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat Cell Biol 9:654–659. doi:10.1038/ncb1596
Kinet V, Halkein J, Dirkx E, De Windt LJ (2013) Cardiovascular extracellular microRNAs: emerging diagnostic markers and mechanisms of cell-to-cell RNA communication. Front Genet 4:214. doi:10.3389/fgene.2013.00214
Fabbri M, Paone A, Calore F et al (2012) MicroRNAs bind to Toll-like receptors to induce prometastatic inflammatory response. PNAS 109:2110–2116. doi:10.1073/pnas.1209414109/-/DCSupplemental.www.pnas.org/cgi/doi/10.1073/pnas.1209414109
Strimbu K, Tavel JA (2010) What are biomarkers? Curr Opin HIV AIDS 5:463–466. doi:10.1097/COH.0b013e32833ed177
Panotopoulos J, Posch F, Alici B et al (2015) Hemoglobin, alkalic phosphatase, and C-reactive protein predict the outcome in patients with liposarcoma. J Orthop Res 33:765–770. doi:10.1002/jor.22827
Panotopoulos J, Posch F, Funovics PT et al (2015) Elevated serum creatinine and low albumin are associated with poor outcomes in patients with liposarcoma. J Orthop Res. doi:10.1002/jor.23002
Ballman KV (2015) Biomarker: predictive or prognostic? doi:10.1200/JCO.2015.63.3651
Schwarzenbach H, Nishida N, Calin GA, Pantel K (2014) Clinical relevance of circulating cell-free microRNAs in cancer. Nat Rev Clin Oncol 11:145–156. doi:10.1038/nrclinonc.2014.5
Subramanian S, Lui WO, Lee CH et al (2008) MicroRNA expression signature of human sarcomas. Oncogene 27:2015–2026. doi:10.1038/sj.onc.1210836
Sarver AL, Phalak R, Thayanithy V, Subramanian S (2010) S-MED: sarcoma microRNA expression database. Lab Investig 90:753–761. doi:10.1038/labinvest.2010.53
Renner M, Czwan E, Hartmann W et al (2012) MicroRNA profiling of primary high-grade soft tissue sarcomas. Genes Chromosomes Cancer 51:982–996. doi:10.1002/gcc.21980
Zhou Y, Zhang Y, Huang Y et al (2014) Liposarcoma miRNA signatures identified from genome-wide miRNA expression profiling. Future Oncol 10:1373–1386. doi:10.2217/fon.14.90
Taylor BS, DeCarolis PL, Angeles CV et al (2011) Frequent alterations and epigenetic silencing of differentiation pathway genes in structurally rearranged liposarcomas. Cancer Discov 1:587–597. doi:10.1158/2159-8290.CD-11-0181
Pichler M, Calin GA (2015) MicroRNAs in cancer: from developmental genes in worms to their clinical application in patients. Br J Cancer 113:1–5. doi:10.1038/bjc.2015.253
Redis RS, Calin S, Yang Y et al (2012) Cell-to-cell miRNA transfer: from body homeostasis to therapy. Pharmacol Ther 136:169–174. doi:10.1016/j.pharmthera.2012.08.003
Taylor DD, Gercel-Taylor C (2013) The origin, function, and diagnostic potential of RNA within extracellular vesicles present in human biological fluids. Front Genet 4:1–12. doi:10.3389/fgene.2013.00142
Ma R, Jiang T, Kang X (2012) Circulating microRNAs in cancer: origin, function and application. J Exp Clin Cancer Res 31:38. doi:10.1186/1756-9966-31-38
Miyachi M, Tsuchiya K, Yoshida H et al (2010) Circulating muscle-specific microRNA, miR-206, as a potential diagnostic marker for rhabdomyosarcoma. Biochem Biophys Res Commun 400:89–93. doi:10.1016/j.bbrc.2010.08.015
Weng Y, Chen Y, Chen J et al (2013) Identification of serum microRNAs in genome-wide serum microRNA expression profiles as novel noninvasive biomarkers for malignant peripheral nerve sheath tumor diagnosis. Med Oncol 30:531–536. doi:10.1007/s12032-013-0531-x
Fricke A, Ullrich PV, Heinz J et al (2015) Identification of a blood-borne miRNA signature of synovial sarcoma. Mol Cancer 14:151. doi:10.1186/s12943-015-0424-z
Acknowledgments
The authors would like to acknowledge Dr. Julie Bridge from the Department of Pathology, University of Nebraska who graciously provided the Fluorescence In Situ Hybridization (FISH) image.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This review was supported by the NCI U54CA168512 to REP.
Additional information
K. L. J. Bill and L. Casadei have contributed equally.
Rights and permissions
About this article
Cite this article
Bill, K.L.J., Casadei, L., Prudner, B.C. et al. Liposarcoma: molecular targets and therapeutic implications. Cell. Mol. Life Sci. 73, 3711–3718 (2016). https://doi.org/10.1007/s00018-016-2266-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00018-016-2266-2