Abstract
Objective and design
Alzheimer’s disease (AD) is associated with amyloid plaques (Aβ) and hyperphosphorylated tau protein tangles in the brain. We investigated the possible neuroprotective role of flavocoxid, a dual inhibitor of cyclooxygenases-1/2 (COX-1/2) and 5-Lipoxygenase (5-LOX), in triple-transgenic (3xTg-AD) mice.
Subjects
Mice were 3 months at the beginning of the study.
Treatment
Animals received once daily for 3-month saline solution or flavocoxid (20 mg/kg/ip).
Methods
Morris water maze was used to assess learning and memory. Histology was performed to evidence Aβ plaques and neuronal loss, while inflammatory proteins were determined by western blot analysis.
Results
Saline-treated 3xTg-AD mice showed an impairment in spatial learning and memory (assessed at 6 months of age), and increased expression of inflammatory and apoptotic molecules. Treatment of 3xTg-AD mice with flavocoxid reduced: (1) learning and memory loss; (2) the increased eicosanoid production and the phosphorylation level of amyloid precursor protein (APP-pThr668), Aβ 1–42, p-tau (pThr181), pERK, and the activation of the NLRP3 inflammasome; (3) Aβ plaques; and (4) neuronal loss, compared to saline-treated animals.
Conclusions
Pharmacological blockade of both COX-1/2 and 5-LOX was able to counteract the progression of AD by targeting pathophysiological mechanisms up- and downstream of Aβ and tau.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) is a major cause of disability and mortality if not effectively treated [1–3]. In the cortex and hippocampus of AD brains, two members of the α-secretase complex presenilin-1 (PS1) and presenilin-2 (PS2), together with the β-secretases, process the amyloid precursor protein (APP) to generate deposits of extracellular β-amyloid (Aβ plaques). Another characteristic lesion is represented by intraneuronal tau neurofibrillary tangles composed of hyperphosphorylated tau protein. Plaques and tangles promote the onset of synaptic dysfunction, rapidly followed by neurodegeneration, neuronal loss, and cognitive impairment [2–6]. An established role is known to be played by oxidative and nitrosative stress, with a consequent inflammatory response, leading to the production of cytokines and eicosanoids [6–9]. The cycloxygenase enzymes COX-1 and COX-2, together with the lipoxygenase 5-LOX, are known to be involved in numerous inflammatory activities and in normal neuronal functions. COX-2 expressed by hippocampal and cortical neurons and COX-1, found in microglia, regulates neuroplasticity producing prostaglandins [10]. Furthermore, 5-LOX appears to regulate amyloid-beta levels in the brain by influencing gamma-secretase [11].
Numerous epidemiological reports and animal studies showed that nonsteroidal anti-inflammatory drugs (NSAIDs), the most widely used anti-inflammatory agents, provided a proof of concept on the anti-inflammatory approach to disease modification [12]. Brain inflammation is characterized by the activation of glial cells and the consequent release of pro-inflammatory cytokines and chemokines, especially in the hippocampus [13]. The β-amyloid plaques also stimulates the production of inactive interleuchin-1β (IL-1β), further activated by the NLRP3 inflammasome, a multimeric complex activated by damage-associated molecular patterns (DAMPs) [14, 15]. As recently demonstrated in a genetic model of AD animals, β-amyloid accumulation acts as a DAMP activating the NLRP3 and its downstream cascade that includes caspase-1 cleavage and cytochrome c release from mitochondria [13, 15]. Flavonoids, as a class, are known to reduce reactive oxygen species and some of them have also the ability to inhibit NFkB transcriptional activity; thus, it has been hypothesized that they have the potential of blunting NLRP3 synthesis and activation [16]. Flavocoxid, a mixture of purified baicalin and catechin, exerts its anti-inflammatory properties inhibiting the peroxidase activity of the COX enzymes, rather than their cyclooxygenase activity, common target of the NSAIDs [17]. In addition, flavocoxid has inhibitory activities towards cytoplasmic phospholipase A2 (cPLA2) and 5-LOX along with a strong and broad antioxidant activity, modulating, in turn, inducible gene expression. An anti-apoptotic effect may also be produced by flavocoxid inhibiting NF-κB-induced inflammation in terms of cytokine, COX-2 and 5-LOX expression, as well as through suppression of the p38 and JNK-1 inflammatory pathways [18].
In this paper, we tested the neuroprotective effect of the dual COX/5-LOX inhibitor, flavocoxid, in a well-known mouse transgenic model of AD (3xTg-AD).
Materials and methods
Animals
Male triple-transgenic 3xTg-AD mice and their wild-type littermates (The Jackson Laboratories, Bar Harbor, ME) were used in this study. The 3xTg-AD carry human transgenes APPSwe, PS1M146V, and tauP301L (encoding mutant human APP, PS1, and tau protein, respectively), thus mimicking human AD features [4, 5]. At the beginning of the treatment, mice were 3 months, and were kept in the standard environmental conditions with food in pellets and tap water ad libitum for 2 weeks before starting the experiment. Housing conditions and experimental procedures were in strict accordance with the “Guide for the Care and Use of Laboratory Animals” (National Institutes of Health [NIH] publication, 8th edition, 2011) and the European Community regulations on the use and care of animals for scientific purposes (CEE Council 89/609; Italian D.L. 22-1-92 No. 116), and were approved by the Committee on Animal Health and Care of Modena and Reggio Emilia University (#05/201,411). At the end of the study, sacrifice was performed under general anaesthesia with sodium pentobarbital (50 mg/kg/i.p; Sigma–Aldrich, Milan, Italy).
Drugs and dose selection
Flavocoxid, a kind gift of Primus Pharmaceuticals Inc. (Scottsdale, AZ), was dissolved in 30% DMSO and saline solution (stock solution), and given i.p. (20 mg/kg/i.p., once daily for 3 months) when mice were 3 months. Control animals (3xTg-AD and wild-type mice) received the vehicle used for flavocoxid by the same route. The dose of flavocoxid was chosen on the basis of our previous studies demonstrating its ability to block the COX1-2/5-LOX pathway [17–21].
To assess whether flavocoxid, and in particular its components, might cross the blood–brain barrier, we performed an in situ permeability measurement, as previously described for other flavonoids [22]. Briefly hemiperfusion was performed in anaesthetized wild-type mice (n = 6) cannulating the right common carotid artery, while the right external carotid artery was ligated near to its bifurcation, and the heart was stopped by cutting the left ventricle. Perfusion was started immediately, using warm (37 °C) Ringer’s solution containing flavocoxid (20 mg/kg), and at the end of perfusion, the brain was quickly removed for analysis. The cortex and the hippocampus were dissected and homogenized, the lysate was left overnight with 0.2 U/mL of β-glucuronidase, and 2 U/mL of sulfatase and the day after baicalin and catechin concentrations were assayed with a custom Europium-labelled Time-Resolved Fluoro-ImmunoAssay.
Assessment of spatial learning and memory
We used the Morris Water-Maze test with minor modifications, as previously described [4, 23–26] to measure the ability to learn, to remember, and to go to a place defined only by its position relative to distal extramaze cues. Mice used in the present study were 3–6 months, that is an age characterized by mild cognitive decline and the development of AD pathological hallmarks [27, 28]. In a sound-proof room, a rounded white pool (100 cm large and 55 cm dept) was filled with water (27 °C ± 1 °C) made opaque with milk powder. Mice (12 per group) were trained to find the location of a platform hidden 1 cm below the water level. The four cardinal points were defined by means of different geometrical figures. Latency to escape onto the hidden platform was recorded for each training day. Each mouse performed four daily trials, for 5 days consecutively, starting randomly from a different cardinal point. If the animal failed to locate the platform within 60 s, escape latency was considered equal to 60 s (so daily maximum total escape latency was 240 s). The Morris Water Test was performed during the last week of treatments when mice were 6 months. The mice were subjected to a 5-day training sequence, to assay learning (first session, learning), followed 3 days later by a second 1-day training to assay memory (second session, memory). To assess memory retention, a probe trial (without the platform) was also carried out the day after the memory session. Animals were allowed to search the platform for 60 s, and the time spent in the target quadrant was used to assess the retention of memory.
Isolation of cytoplasmic and nuclear proteins and Western blot analysis
The whole hippocampus was dissected from six animals per group (within 90 min after the end of the last behavioral test), and after extraction protein samples (30 μg lane) were electrophoretically separated and transferred to PVDF membranes. The membranes were blocked in 5% milk and incubated overnight at 4 °C with the following primary antibodies: phospho (p)-tau Thr181, total Tau, p-APP Thr668, total APP, Aβ (1–42 specific), pERK1/2, total ERK1/2 (all from Cell Signaling, Charlottesville, VA), BAX, Bcl-2, Bcl-xL (Bio-Vision, Inc., Milpitas, CA), and NLRP3 (Abcam, Cambridge, UK). The day after, the membranes were incubated with a specific secondary antibody peroxidase-conjugated for 1 h at room temperature. To prove equal loading, the stripped blots were incubated with an anti-β-actin antibody (Cell Signaling). The membranes were analyzed by the enhanced chemiluminescence (ECL plus) system. The protein signals were quantified by scanning densitometry using a bio-image analysis system (Bio-Profil, Celbio, Italy) and expressed as relative integrated intensity compared with controls tested in the same batch.
Determination of eicosanoids and IL-1β in mouse brain lysates
The inflammatory eicosanoids prostaglandin E2 (PGE-2) and leukotriene B(4) (LTB-4) were measured in cerebral cortex lysates (deriving from the brains used for western blot n = 6) with a specific enzyme-linked immunosorbent assay (ELISA) kit. Brain cortex lysates were centrifuged at 15,000 rpm, and supernatants were assayed for PGE-2 (Cusabio Biotech, Wuhan, People’s Republic of China) and LTB4 (Bioassay Technology Laboratory, Shanghai, P.R., China) following the manufacturer’s instructions, and results were expressed as pg/ml. Interleukin-1β (IL-1β) was measured from the same lysates with a specific kit (Abcam, Cambridge, UK), following the manufacture’s instructions, and results were compared to a standard curve and expressed as pg/ml.
Histology
At the end of the probe test, the remaining six mice per group underwent transcardial perfusion with ice-cold 4% paraformaldehyde (phosphate-buffered), then brains were removed and processed for histological examination, as previously described [4]. Hippocampus and isocortex morphology was studied in 7-µm-thick paraffin-embedded sections, hematoxylin–eosin stained; the extent of Aβ plaques was assessed after ethanol-Congo red/Weigert hematoxylin staining. Morphological analyses were performed using an Axiophot photomicroscope (Carl Zeiss GmbH, Jena, Germany) connected to a DS-5M digital camera (Nikon Instruments, Tokio, Japan), under ordinary and polarized light. Digital images of extracellular Aβ deposits (Aβ plaques) were collected, on the whole slide stained by Congo red, in five seriated sections per animal taken every 100 μm starting −1 mm (frontal isocortex) and +2 mm (hippocampus) from bregma zero coordinates. Histomorphometry was performed using an image system (analySIS, Soft Imaging System GmbH, Münster, Germany).
Statistical analysis
All data were detected blind to the treatment and are shown as means ± SD. Values were analyzed by means of two-way repeated measures ANOVA (behavioral data) or one-way ANOVA (all other data) followed by the Student–Newman–Keuls’ test. A value of p < 0.05 was considered significant. Graphs were drawn using the GraphPad Prism software version 5.0 for Windows (GraphPad Software Inc., La Jolla, CA, USA).
Results
Flavocoxid improved cognitive function and brain damage in 3xTg-AD mice
The concentration of Flavocoxid components determined in brain lysates following perfusion, demonstrated that the achieved levels were similar to that reported as effective in cell models of AD [29, 30], specifically catechin levels were 18.6 ± 5.1 µMol and baicalin levels were 12.2 ± 3.4 µMol. The results clearly indicated the presence of both flavonoids in brain lysates.
3xTg-AD mice treated with saline showed impaired ability (as compared with wild-type mice) in place finding both during the first and second sessions (assay of learning and memory, respectively; Fig. 1a, b). On the contrary, 3xTg-AD animals treated with flavocoxid at the dose of 20 mg/kg demonstrated a significant improvement in learning (since the third day) and memory performances after 3-month treatments compared with 3xTg-AD animals treated with saline (Fig. 1a, b). In the probe test for the assay of memory retention, flavocoxid-treated 3xTg-AD animals spent more time than saline-treated animals, demonstrating a significant improvement in learning (Fig. 1c).
Flavocoxid improves learning and memory in3xTg-AD mice. Graphs indicate mean values ± SD of (a, b) latency to escape onto the hidden platform (Morris water-maze test, n = 12 mice per group); and values ± SD of (c) indicate the time spent on the target zone (probe test). Mice (age 3 months) were treated with flavocixid (20 mg/kg i.p.) or saline once daily for 3 months. The first session (a) started the last week of the treatments (6 months), and the second session (b) took place 3 days after the end of the first session. The probe test (c) was performed 24 h after the second session. WT wild-type mice, 3xTg 3xTg-AD saline-treated mice, Flavo flavocoxid. *p < 0.01 vs 3xTg-AD treated with saline
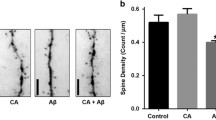
The histological analysis revealed a substantial extracellular amyloid deposit in the hippocampus of saline-treated 3xTg-AD mice (Fig. 2b, e, f). Flavocoxid treatment interferes on the process of amyloid plaques formation, with a reduction in amyloid deposit, compared with saline-treated 3xTg-AD animals (Fig. 2b, c, e, f, g).
Flavocoxid reduces amyloid deposits—representative histological pictures (ethanol-Congo red/weigert hematoxylin staining; field width = 205 μm) of the hippocampus (n = 6), at ordinary (a–c) and polarized (d–f) light, in WT (a, d) saline (b, e) and flavocoxid (c, f) treated 3xTg-AD mice. Alpha-amyloid deposit (orange–brown, under polarized light), less present in the flavocoxid-treated 3xTg-AD mice (c, f) as compared with saline-treated one (b, e), located on or near hippocampus neurons mainly of CA3 and CA4 fields. Graph (g) indicates mean values ± SD of amyloid deposit/mm2. *p < 0.001 vs WT; # p < 0.005 vs 3xTg-AD treated with saline. WT wild-type mice, 3xTg 3xTg-AD saline-treated mice, Flavo flavocoxid
Flavocoxid decreased eicosanoid production in brain of 3xTg-AD mice
Flavocoxid is known to inhibit COX-2 and 5-LOX enzymes, thus to prove that flavocoxid was able to cross the blood–brain barrier and act on these enzymes; we evaluated the concentration of their main products, PGE-2 and LTB-4, respectively, in brain lysates at the end of the study. Wild-type animals showed, as expected, very low levels of both eicosanoids. PGE-2 and LTB-4 levels were dramatically increased in saline-treated 3xTg-AD mice, compared to wild type. Treatment with flavocoxid was able to markedly reduce PGE-2 and LTB-4, demonstrating that both flavonoid components were able to cross the barrier and exert their beneficial actions (Fig. 3a, b).
Flavocoxid blunts eicosanoids and sterile inflammation. PGE-2 (a), LTB-4 (b), NLRP3 (c), and IL-1β (d) in brain lysates from 3xTg-AD mice treated with saline or flavocoxid. The representative western blot analysis is presented with the β-actin as loading control. Representative bands have been cropped from the same films. Graph indicate mean values ± SD (n = 6). WT wild-type mice, 3xTg 3xTg-AD saline-treated mice; Flavo flavocoxid. *p < 0.001 vs WT; # p < 0.005 vs 3xTg-AD treated with saline
Flavocoxid reduced the activation of NLRP3 and IL-1β production
The pro-inflammatory protein IL-1β is primarly activated by “sterile” inflammation, as in the case of AD via the inflammasome NLRP3 pathway, and as a matter of fact, we detected higher levels of IL-1β and NLRP3 in cortex of 3xTg-AD mice, compared to wild-type animals (Fig. 3c, d). Flavocoxid administration was able to reduce the increased activation of the inflammasome and of its downstream product, IL-1β (Fig. 3c, d).
Flavocoxid reduced level/phosphorylation state of amyloid/tau cascade proteins
The amyloid/tau cascade was also investigated in the hippocampus by western blot analysis, at the end of the study. The saline-treated 3xTg-AD mice showed a marked expression of phosphorylated APP (Thr668) and Tau (Thr181). In addition, an overexpression of Aβ was detected in these animals (Fig. 4a–c). On the contrary, in flavocoxid-treated 3xTg-AD mice, the phosphorylation/expression level of the amyloid/tau cascade proteins was markedly decreased, demonstrating a positive effect on the main molecular hallmarks of AD (Fig. 4a–c).
Flavocoxid reduces AD proteins—phospo-APP, β-amyloid, and p-tau representative western blot analysis presented with the β-actin as loading control. Representative bands have been cropped from the same films. Graph indicates mean values ± SD (n = 6). WT wild-type mice; 3xTg 3xTg-AD saline-treated mice; Flavo flavocoxid. *p < 0.001 vs WT; # p < 0.005 vs 3xTg-AD treated with saline
Flavocoxid reduced inflammatory and apoptotic markers in 3xTg-AD mice
In AD, an important role is played also by the mitogen-activated protein kinases (MAPK) pERK 1/2. Western blot analysis for activated pERK 1/2 showed an increased expression in saline-treated 3xTg-AD mice, compared to wild-type animals (Fig. 5a). In 3xTg-AD mice treated with flavocoxid, there was a significant reduction of pERK 1/2 activation (Fig. 5a), compared to 3xTg-AD control mice.
Flavocoxid reduces inflammation and apoptosis—pERK, BAX, Bcl-2, and Bcl-xL representative western blot analysis presented with the β-actin as loading control. Representative bands have been cropped from the same films. Graph indicate mean values ± SD (n = 6). WT wild-type mice; 3xTg 3xTg-AD saline-treated mice; Flavo flavocoxid. *p < 0.001 vs WT; # p < 0.005 vs 3xTg treated with saline
The apoptotic BAX and the anti-apoptotic Bcl-2 and Bcl-xL were also investigated, demonstrating an increased expression of BAX and a concomitantly reduction of Bcl-2 and Bcl-xL in saline-treated 3xTg-AD mice, compared to wild-type animals (Fig. 5b–d). Flavocoxid-treated animals revealed a reduced activation of BAX and restored Bcl-2 and Bcl-xL levels (Fig. 5b–d), compared to 3xTg-AD control mice.
Discussion
Recent findings suggest that the AD is the results of a sterile inflammatory process that is triggered by extracellular Aβ plaques and phospho-Tau tangles, which are recognized by microglia and are responsible for its activation [14].
Here, we first demonstrate that a baicalin/catechin formulation, flavocoxid, is able to suppress this inflammation through the NLRP3 inflammasome pathway thus reducing p-Tau and Abeta deposition and preserving the brain from functional and morphological impairment [15]. Flavocoxid acts mainly interfering with COX-2 and 5-LOX activity as previously demonstrated [17], but as other flavonoid compounds, it blocks also the activation of transcription factors as NFκB [18, 19] with an elevated safety profile, at least in mice [21]. The ability of reducing inflammasome activation was never tested before, and besides, it has been hypothesized that flavonoids might have this ability; to date, this was never reported in AD. Reduced NLRP3 activity was also confirmed by the dramatically reduced production of the pro-inflammatory cytokine IL-1β, released mainly during sterile inflammation and with a prominent role in AD [31]. Besides sterile inflammation, amyloid deposits trigger also the production of oxygen radicals [4] and the consequent activation of Mitogen-activated protein kinase (MAPKs), as ERK 1/2, recently involved in brain damage of 3xTg-AD animals [32]. Thus, we evaluated the MAPK in brain lysates observing a prominent expression in AD animals that was mostly reduced following flavocoxid treatment, confirming the positive effect of this compound on several inflammatory pathways. The combined effect of the two flavonoids is greater than the isolated molecules, as shown in a previous paper [19]. As a consequence of NF-κB modulation, flavocoxid reduces COX-2, 5-LOX, iNOS, and TNFα production, and it also blunts the formation of COX-2, 5-LOX, and iNOS metabolites, as PGE2, LTB4, and nitrates. These effects provide a rationale for the use of a dual inhibitor in acute and chronic inflammatory conditions.
The main anti-inflammatory action of flavocoxid is to inhibit the enzymatic activity of COX1/2 and 5-LOX and in turn the eicosanoid production at the site of injury. In the brains of 3xTg-AD animals, we found elevated levels of PGE-2 and LTB-4 that were dramatically blunted by flavocoxid treatment. These results prove not only the ability of the two components of the flavonoid mixture (baicalin and catechin) to cross the blood–brain barrier, but also to preserve their pharmacological function also at brain level, a fundamental characteristic for translational implications. In addition, in normal mice, we demonstrated that baicalin and catechin can be found following hemiperfusion at concentrations already reported as effective in cell models of AD [29, 30]. Although we used a different administration route in our experiment (intraperitoneal), it is possible to hypothesize that a similar amount of baicalin and cathechin was present at brain level. It has been speculated that anti-inflammatory agents might alter the conformation of Aβ peptides reducing neuroinflammation and degeneration, at least in vitro [33]. It was also shown that aspirin reverses the β-sheet conformation of the aggregated Aβ25–35, Aβ-40, and Aβ-42 peptides [34], in addition an improved memory function was inversely related to PGE2 levels [35]. These data support our findings on the inhibition of COX by a non selective inhibitor, flavocoxid, that has been able to reduce Aβ (1–42) accumulation in hippocampus, and the phosphorylation of APP at Thr668. This also suggests that neuroinflammation particularly mediated by COX activity may interfere with the synaptic process that appears in learning and memory ability. On the other hand, a recent paper by Chakrabarty et al. [36] points out to an involvement of IL-4, a well-known anti-inflammatory interleukin, in the accumulation of Aβ in APP transgenic mice, but no data are available in 3xTg mice.
To date, the current approved therapy relies on activation of anti-glutamatergic and cholinergic mechanisms, but symptom improvement is modest and transient [1, 3]. The alarming increase in AD incidence, due to the augmented number of aged populations, raises the socio-economic burden of this disease [37], determining the need for more effective pharmacological approaches. This paper provides evidence for a rational use of flavocoxid to reduce the specific hallmark of AD, specifically the increased content of Aβ fragment 1–42 and tau hyperphosphorylation. These changes at molecular level were also evident at morphological analysis that revealed a reduced deposit of amyloid in brains of flavocoxid-treated animals, especially in the CA3 area of the hippocampus, responsible for memory and learning abilities. Indeed, the 3xTg mice treated with flavocoxid demonstrated a reduced impairment in memory and learning, collecting better performances in the Morris test with improved memory retention, compared to saline-treated animals.
It is well recognized that the accumulation of amyloid-β and hyperphosphorylated tau protein impairs neuronal survival; in either cases, the common trigger might be represented by an altered lysosomial degradation of APP in the AD brain [38], which eventually causes cell death. Accordingly, the apoptosis regulators Bcl2 and BAX were colocalized in 45% of cells of Alzheimer patients compared to the 30% of aged subjects, suggesting an important role for these molecules in the disease [39]. In the brain of saline-treated 3xTg-AD mice, we observed a significant increase in BAX expression with a decrease in Bcl-2 and Bcl-xL that likely depict a pro-apoptotic status, and the administration of flavocoxid for 3 months determined a re-establishment of the apoptosis balance, confirmed also by morphological observation.
The intriguing results obtained with flavocoxid treatment in the 3xTg-AD mouse model is supported, at least in part, by epidemiological data indicating a reduced risk of developing AD in those patients that take COX-inhibitors [12]. However, the well-known side effects of these compounds reduce the appeal of such a treatment. Safety concerns have been raised recently suggesting that flavocoxid treatment causes liver injury but the biggest limitation of this case report is that the frequency and mechanism of this effect was not clear [18]. The report suggests that only in four female patients out of 877, the causality assessment suggested that in three patients, it is highly likely, and in one, it is only a possible cause. The product information sheet of Limbrel® also suggested that in that case, this medical food should always be administered with the supervision of a physician. In light of these considerations, the promising data obtained in this experimental model suggest a role for flavocoxid as therapeutic option for slowing the progression, or even treating AD.
References
Galimberti D, Ghezzi L, Scarpini E. Immunotherapy against amyloid pathology in Alzheimer’s disease. J Neurol Sci. 2013;333:50–4.
Ittner LM, Götz J. Amyloid-β and tau—a toxic pas de deux in Alzheimer’s disease. Nat Rev Neurosci. 2011;12:65–72.
Tayeb HO, Yang HD, Price BH, Tarazi FI. Pharmacotherapies for Alzheimer’s disease: beyond cholinesterase inhibitors. Pharmacol Ther. 2012;134:8–25.
Giuliani D, Bitto A, Galantucci M, Zaffe D, Ottani A, Irrera N, Neri L, Cavallini GM, Altavilla D, Botticelli AR, Squadrito F, Guarini S. Melanocortins protect against progression of Alzheimer’s disease in triple-transgenic mice by targeting multiple pathophysiological pathways. Neurobiol Aging. 2014;35:537–47.
Kumar S, Wirths O, Theil S, Gerth J, Bayer TA, Walter J. Early intraneuronal accumulation and increased aggregation of phosphorylated Abeta in a mouse model of Alzheimer’s disease. Acta Neuropathol. 2013;125:699–709.
Munoz L, Ammit AJ. Targeting p38 MAPK pathway for the treatment of Alzheimer’s disease. Neuropharmacology. 2010;58:561–8.
Banerjee R, Beal MF, Thomas B. Autophagy in neurodegenerative disorders: pathogenetic roles and therapeutic implications. Trends Neurosci. 2010;33:541–9.
Zipp F, Aktas O. The brain as a target of inflammation: common pathways link inflammatory and nurodegenerative diseases. Trends Neurosci. 2006;29:518–27.
Klegeris A, McGeer PL. Cyclooxygenase and 5-lipoxygenase inhibitors protect against mononuclear phagocyte neurotoxicity. Neurobiol Aging. 2002;23:787–94.
Yang H, Chen C. Cyclooxygenase-2 in synaptic signaling. Curr Pharm Des. 2008;14:1443–51.
Firuzi O, Zhuo J, Chinnici CM, Wisniewski T, Praticò D. 5-Lipoxygenase gene disruption reduces amyloid-beta pathology in a mouse model of Alzheimer’s disease. FASEB J. 2008;22:1169–78.
Pasinetti GM. From epidemiology to therapeutic trials with anti-inflammatory drugs in Alzheimer’s disease: the role of NSAIDs and cyclooxygenase in beta-amyloidosis and clinical dementia. J Alzheimers Dis. 2002;4:435–45.
Heneka MT, Kummer MP, Stutz A, Delekate A, Schwartz S, Vieira-Saecker A, Griep A, Axt D, Remus A, Tzeng TC, Gelpi E, Halle A, Korte M, Latz E, Golenbock DT. NLRP3 is activated in Alzheimer’s disease and contributes to pathology in APP/PS1 mice. Nature. 2013;493:674–8.
Tan MS, Yu JT, Jiang T, Zhu XC, Tan L. The NLRP3 inflammasome in Alzheimer’s disease. Mol Neurobiol. 2013;48:875–82.
Ghosh S, Wu MD, Shaftel SS, Kyrkanides S, LaFerla FM, Olschowka JA, O’Banion MK. Sustained interleukin-1β overexpression exacerbates tau pathology despite reduced amyloid burden in an Alzheimer’s mouse model. J Neurosci. 2013;33:5053–64.
Sorbara MT, Girardin SE. Mitochondrial ROS fuel the inflammasome. Cell Res. 2011;21:558–60.
Burnett BP, Bitto A, Altavilla D, Squadrito F, Levy RM, Pillai L. Flavocoxid inhibits phospholipase A2, peroxidase moieties of the cyclooxygenases (COX), and 5-lipoxygenase, modifies COX-2 gene expression, and acts as an antioxidant. Mediators Inflamm. 2011;2011:385780.
Bitto A, Squadrito F, Irrera N, Pizzino G, Pallio G, Mecchio A, Galfo F, Altavilla D. Flavocoxid, a nutraceutical approach to blunt inflammatory conditions. Mediators Inflam. 2014;2014:790851.
Bitto A, Minutoli L, David A, Irrera N, Rinaldi M, Venuti FS, Squadrito F, Altavilla D. Flavocoxid, a dual inhibitor of COX-2 and 5-LOX of natural origin, attenuates the inflammatory response and protects mice from sepsis. Crit Care. 2012;16:32.
Burnett BP, Jia Q, Zhao Y, Levy RM. A medicinal extract of Scutellaria baicalensis and Acacia catechu acts as a dual inhibitor of cyclooxygenase and 5-lipoxygenase to reduce inflammation. J Med Food. 2007;10:442–51.
Minutoli L, Marini H, Rinaldi M, Bitto A, Irrera N, Pizzino G, Pallio G, Calò M, Adamo EB, Trichilo V, Interdonato M, Galfo F, Squadrito F, Altavilla D. A dual inhibitor of cyclooxygenase and 5-lipoxygenase protects against kainic Acid-induced brain injury. Neuromolecular Med. 2015;17:192–201.
Youdim KA, Qaiser MZ, Begley DJ, Rice-Evans CA, Abbott NJ. Flavonoid permeability across an in situ model of the blood-brain barrier. Free Radic Biol Med. 2004;36:592–604.
Giuliani D, Mioni C, Altavilla D, Leone S, Bazzani C, Minutoli L, Bitto A, Cainazzo MM, Marini H, Zaffe D, Botticelli AR, Pizzala R, Savio M, Necchi D, Schiöth HB, Bertolini A, Squadrito F, Guarini S. Both early and delayed treatment with melanocortin 4 receptor-stimulating melanocortins produces neuroprotection in cerebral ischemia. Endocrinology. 2006;147:1126–35.
Giuliani D, Neri L, Canalini F, Calevro A, Ottani A, Vandini E, Sena P, Zaffe D, Guarini S. NDP-α-MSH induces intense neurogenesis and cognitive recovery in Alzheimer transgenic mice through activation of melanocortin MC4 receptors. Mol Cell Neurosci. 2015;67:13–21.
Giuliani D, Ottani A, Minutoli L, Stefano VD, Galantucci M, Bitto A, Zaffe D, Altavilla D, Botticelli AR, Squadrito F, Guarini S. Functional recovery after delayed treatment of ischemic stroke with melanocortins is associated with overexpression of the activity-dependent gene Zif268. Brain Behav Immun. 2009;23:844–50.
Sabogal-Guáqueta AM, Muñoz-Manco JI, Ramírez-Pineda JR, Lamprea-Rodriguez M, Osorio E, Cardona-Gómez GP. The flavonoid quercetin ameliorates Alzheimer’s disease pathology and protects cognitive and emotional function in aged triple transgenic Alzheimer’s disease model mice. Neuropharmacology. 2015;93:134–45.
Hsiao K, Chapman P, Nilsen S, Eckman C, Harigaya Y, Younkin S, Yang F, Cole G. Correlative memory deficits, Abeta elevation, and amyloid plaques in transgenic mice. Science. 1996;274:99–102.
Lilja AM, Röjdner J, Mustafiz T, Thomé CM, Storelli E, Gonzalez D, Unger-Lithner C, Greig NH, Nordberg A, Marutle A. Age-dependent neuroplasticity mechanisms in Alzheimer Tg2576 mice following modulation of brain amyloid-β levels. PLoS One. 2013;8:e58752.
Fernandez JW, Rezai-Zadeh K, Obregon D, Tan J. EGCG functions through estrogen receptor-mediated activation of ADAM10 in the promotion of non-amyloidogenic processing of APP. FEBS Lett. 2010;584:4259–67.
Yin F, Liu J, Ji X, Wang Y, Zidichouski J, Zhang J. Baicalin prevents the production of hydrogen peroxide and oxidative stress induced by Aβ aggregation in SH-SY5Y cells. Neurosci Lett. 2011;492:76–9.
Ben Menachem-Zidon O, Menahem YB, Hur TB, Yirmiya R. Intra-hippocampal transplantation of neural precursor cells with transgenic over-expression of IL-1 receptor antagonist rescues memory and neurogenesis impairments in an Alzheimer’s disease model. Neuropsychopharmacology. 2014;39:401–14.
Feld M, Krawczyk MC, Sol Fustiñana M, Blake MG, Baratti CM, Romano A, Boccia MM. Decrease of ERK/MAPK overactivation in prefrontal cortex reverses early memory deficit in a mouse model of Alzheimer’s disease. J Alzheimers Dis. 2014;40:69–82.
Gasparini L, Ongini E, Wenk G. Non-steroidal anti-inflammatory drugs (NSAIDs) in Alzheimer’s disease: old and new mechanisms of action. J Neurochem. 2004;91:521–36.
Thomas T, Nadackal TG, Thomas K. Aspirin and non-steroidal anti-inflammatory drugs inhibit amyloid-beta aggregation. Neuroreport. 2001;12:3263–7.
Kotilinek LA, Westerman MA, Wang Q, Panizzon K, Lim GP, Simonyi A, Lesne S, Falinska A, Younkin LH, Younkin SG, Rowan M, Cleary J, Wallis RA, Sun GY, Cole G, Frautschy S, Anwyl R, Ashe KH. Cyclooxygenase-2 inhibition improves amyloid-beta-mediated suppression of memory and synaptic plasticity. Brain. 2008;131:651–64.
Chakrabarty P, Tianbai L, Herring A, Ceballos-Diaz C, Das P, Golde TE. Hippocampal expression of murine IL-4 results in exacerbation of amyloid deposition. Mol Neurodegener. 2012;7:36.
Gustavsson A, Svensson M, Jacobi F, Allgulander C, Alonso J, Beghi E, Dodel R, Ekman M, Faravelli C, Fratiglioni L, Gannon B, Jones DH, Jennum P, Jordanova A, Jönsson L, Karampampa K, Knapp M, Kobelt G, Kurth T, Lieb R, Linde M, Ljungcrantz C, Maercker A, Melin B, Moscarelli M, Musayev A, Norwood F, Preisig M, Pugliatti M, Rehm J, Salvador-Carulla L, Schlehofer B, Simon R, Steinhausen HC, Stovner LJ, Vallat JM, Van den Bergh P, van Os J, Vos P, Xu W, Wittchen HU, Jönsson B, Olesen J. Cost of disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21:718–79.
Caberlotto L, Nguyen TP. A systems biology investigation of neurodegenerative dementia reveals a pivotal role of autophagy. BMC Syst Biol. 2014;8:65.
Lu G, Kwong WH, Li Q, Wang X, Feng Z, Yew DT. Bcl2, bax, and nestin in the brains of patients with neurodegeneration and those of normal aging. J Mol Neurosci. 2005;27:167–74.
Acknowledgements
The work was supported by Departmental fundings. Flavocoxid was a kind gift of Primus Pharmaceuticals Inc., Scottsdale, AZ.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All applicable international, national, and institutional guidelines for the care and use of animals were followed. All procedures performed in studies involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted.
Additional information
Responsible Editor: Ji Zhang.
Rights and permissions
About this article
Cite this article
Bitto, A., Giuliani, D., Pallio, G. et al. Effects of COX1-2/5-LOX blockade in Alzheimer transgenic 3xTg-AD mice. Inflamm. Res. 66, 389–398 (2017). https://doi.org/10.1007/s00011-017-1022-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-017-1022-x