Abstract
Like B cells, T cells can be immortalized through hybridization with lymphoma cells, a technique that has been particularly useful in the study of the T cell receptors (TCR) for antigen. In T cell hybridizations, the AKR mouse strain-derived thymus lymphoma BW5147 is by far the most popular fusion line. However, the full potential of this technology had to await inactivation of the productively rearranged TCR-α and -β genes in the lymphoma. BWα-β-, the TCR-gene deficient variant of the original lymphoma, which has become the fusion line of choice for αβ T cells, is now available with numerous modifications, enabling the investigation of many aspects of TCR-mediated responses and TCR-structure. Unexpectedly, inactivating BW’s functional TCR-α gene also rendered the lymphoma more permissive for the expression of TCR-γδ, facilitating the study of γδ T cells, their TCRs, and their TCR-mediated reactivity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Making B Cells Immortal Through Hybridization
B and T cell antigen receptors (BCR, TCR) are expressed by individual lymphocytes, selected out of mixed cell populations to survive and mature in vivo, and potentially respond as clones to antigenic stimulation (Burnet 1959). The study of such cells and their antigen receptors in the laboratory usually requires amplification at the cellular or molecular levels. Historically, cells were maintained in vitro and clonally expanded through ever more refined tissue culture methods, but this remained something of an art, not always readily achieved. The discovery in the 1970s that certain properties of normal lymphocytes, including their expressed antigen receptors and specificities, can be preserved through hybridization with immortal lymphoma cells, removed much of this limitation.
Köhler and Milstein (1975), who were later recognized for their groundbreaking work with the Nobel Prize in Medicine, reported the first successful hybridizations of B cells secreting antibodies having the desired specificity (Köhler and Milstein 1975, 1976). The technique was soon refined by establishing as fusion partners B cell tumors unable to produce their own antibodies so that B cell hybridomas generated with them exclusively produced antibodies derived from the normal B cell (Kearney et al. 1979; Shulman et al. 1978). The availability of antigen-specific monoclonal antibodies revolutionized biological and medical research and enabled the development of monoclonal antibody-based drugs.
T Cell Hybridomas
After the first report describing B cell hybridomas, the potential of using hybridization in a similar manner for immortalizing antigen-specific T cells was obvious, and T cell hybridization was attempted almost immediately. Among T lymphomas that proved to be suitable for generating murine T cell hybridomas were the EL-4 line, derived from a carcinogen-induced lymphoma in a C57BL/6 mouse (Gorer and Kaliss 1959), the L5178 line that originated from a leukemic DBA/2 mouse (Kao and Puck 1969), and the BW5147 line, which had been derived from a thymus lymphoma in an AKR/J mouse by Hyman and Stallings (1974), and had been rendered drug-sensitive so as to be unable to survive in hypoxanthine/aminopterin/thymidine (HAT)-medium. Other T cell tumors were also tested for use in T cell hybridizations, including several human leukemia-derived cell lines (Ozaki 1998). However, hybridization of human T cells did not become a widely used technique, in part perhaps because normal human T cells can be more easily cloned and maintained in vitro than mouse T cells.
In 1977, the first papers appeared demonstrating the feasibility of generating T cell hybridomas (Goldsby et al. 1977; Hammerling 1977; Köhler et al. 1977). The following three years saw reports of several “functional” hybridomas, including those producing what appeared to be specific immune-suppressive factors (Kapp et al. 1980; Kontiainen et al. 1978; Taniguchi and Miller 1978; Taussig et al. 1979), as well as “allogeneic effect factor” (Katz et al. 1980), and a factor “with helper activity specific to the synthetic polypeptide (T,G)-A-L and bears surface determinants of the immunoglobulin heavy chain variable region” (Eshar et al. 1980). The team of Kappler and Marrack, relying on BW5147 cells, which had emerged as the preferred fusion partner for mouse T cell hybridization (Eshar et al. 1980; Hammerling 1977; Kapp et al. 1980; Kontiainen et al. 1978), polyethylene glycol as fusogen, and HAT-selection, also reported a T cell hybridoma during this period (Harwell et al. 1980). This hybridoma (FS6-14.13), which had been derived from concanavalin A (Con A)-stimulated T cells of a B6D2F1 mouse, produced upon stimulation with Con A a non-specific T cell growth factor supporting the cytokine-dependent HT-2 cell line (Watson 1979). The inducible factor was identified as interleukin (IL)-2 (Harwell et al. 1980).
Although investigations into suppressor factors and “allogeneic effect factor” eventually were abandoned, T cell hybridomas became very popular when Kappler et al. (1981) demonstrated that these hybridomas could, just like normal T cells, display clonal antigen and MHC specificities. Desirous to preserve inducible IL-2 production, which they saw with the Con A-responsive FS6-14.13 cells but not with BW5147 cells, Kappler et al. (1981) turned FS6-14.13 into a new fusion line. They selected an azaguanine-resistant (HAT-sensitive) variant of their hybridoma, FS6-14.13.AG2, and then hybridized it (instead of BW5147) with T cell blasts from chicken ovalbumin (cOVA)-immunized B10.A (H-2a) mice. One of the resulting hybrid-hybridomas, AO-40 (A for H-2a and O for ovalbumin), produced IL-2 in response to antigen stimulation, cOVA plus irradiated B10.A spleen cells. Though FS6-14.13.AG2 ultimately proved unnecessary, because the BW5147 fusion line itself usually supports IL-2 production in TCR-bearing hybridomas generated with it, the AO-40 hybridoma proved interesting. In contrast to total lymph node T cells from the cOVA-immunized mice, which showed a broader reactivity pattern and responded to chicken, duck and turkey OVA, the AO-40-subclone AO-40 clone was specific for cOVA. Testing the MHC-specificity of AO-40 with cOVA and irradiated antigen-presenting cells (APCs) derived from a panel of H-2-congenic and recombinant mice, Kappler et al. (1981) deduced that AO-40 cells recognized cOVA in the context of the I-region from H-2 k, and mapped the relevant I region gene(s) to I-Ak (B10.A mice express I-Ak, I-Bk, I-Jk and I-Ek as part of their H-2a MHC haplotype). With this, they had shown that MHCII-restricted antigen-specificities of individual T helper cells could be preserved and defined, with T cell hybridomas.
Still using FS6-14.13 as fusion line, Kappler et al. (1981) also prepared hybridomas with apo beef cytochrome c/H-2d-specific T cells and mapped the H-2 fine-specificity of one such hybridoma (DC-1.18.3) to I-Ad. Furthermore, they generated hybridomas with T cells from keyhole limpet hemocyanin (KLH)-immunized DBA/2 mice, and fused them to azaguanine-selected (HAT-sensitive) AO-40 cells to produce AODK (D for H-2d, K for KLH) hybridomas, which represented a combination of BW5147 and three normal T cell parents, and showed that two subclones (AODK-10.4 and AODK-1.16), both of which responded specifically to KLH in the presence of B10.D2 APCs (H-2d), had different H-2I region fine-specificities. At that time, the dual specificity of T cells—for antigen and MHC—was still an open question. Therefore, Kappler et al. (1981) next endeavored to generate hybridomas having two functional antigen/I-region specificities in the same cell. To this end, they fused HAT-sensitized AO-40.10 cells, themselves already specific for cOVA/H-2a, to normal T cell blasts of different antigen/H-2 specificities, and tested the resulting hybrids (again a combination of BW5147 and three normal T cell parents) for their ability to recognize pairs of antigens (cOVA, KLH or HGG) and H-2 types (H-2a, H-2f or H-2d). Individual hybrids responded to a given antigen only in combination with H-2 types of the mice originally immunized with this antigen, an experimental outcome supporting the notion of dual recognition via a single TCR, and inconsistent with the current competing models of independent antigen and H-2 recognition by different receptors.
The paper by Kappler et al. (1981) beautifully illustrates the usefulness of T cell hybridomas for the study of T cell specificity. Published in 1981, still before any structural information about the TCR was known, it shaped expectations about the nature of the molecular interaction between TCR with both antigen and MHC and thus provided much needed guidance for the studies that followed.
It soon became clear that the detour via hybridoma-fusion-lines was not required since hybridomas generated by direct fusion of BW5147 and normal T cells responded to antigen plus MHC by producing IL-2 (Kappler et al. 1982; White et al. 1983). The Kappler and Marrack research group continued their work with T cell hybridomas for several purposes: to investigate T cell functions (Roehm et al. 1984), to generate antibodies specific for the TCR (Haskins et al. 1984; Marrack et al. 1983b; White et al. 1983), and eventually to isolate (Haskins et al. 1983; Marrack et al. 1983b) and molecularly characterize the elusive TCR molecule itself (Kappler et al. 1983a, b; Marrack et al. 1983a). Other uses for T cell hybridomas soon also became apparent. One of us (WB) joined the Kappler and Marrack group in 1984, to prepare hybridoma—“swarms” generated by a random fusion of normal T cells from non-immunized mice, so as to analyze mixed T cell populations at both the clonal and the population levels, towards the study of T cell development. Indeed, hybridomas with normal thymocytes were readily produced, and an examination of thymocyte hybridomas derived from fetal thymi at successive ontogenetic stages (fetal liver, thymus e14–17 and adult) revealed a distinct developmental pattern of TCR-β gene rearrangements, despite considerable variation between individual thymocytes (Born et al. 1985). We used the same technique to investigate and compare TCR-γ and even IgH gene rearrangements in developing thymocytes and established correlations in developmental timing between the gene rearrangements at these loci (Born et al. 1986, 1988). However, “randomly” generated hybridomas are not necessarily representative of mixed cell populations, and what renders a normal T cell or thymocyte to fuse was not clear then and, to our knowledge, remains unclear to the present date. Hence, data generated in this way need to be validated by comparison with normal cells.
TCR-Loss Variants of BW5147
The thymus lymphoma BW5147 (Hyman and Stallings 1974) still was the preferred and most widely used fusion line for the generation of T cell hybridomas. But after the TCR was discovered, and the genes that encode it had been sequenced, it became clear that BW5147 had the qualities of a Trojan horse. Albeit surface TCR-negative, this lymphoma nevertheless did contain its own functionally rearranged TCR-α and -β genes (Chien et al. 1984; Hedrick et al. 1984). While it did not express its TCR due to mutations in invariant proteins of the CD3 complex, which, as we know now, are required for TCR assembly and surface expression (Bolliger and Johansson 1999), intact CD3 genes from the normal T cell partner in hybridomas generated with BW5147 could complement this deficiency and support TCR expression. In fact, T cell hybridomas generated with BW5147 and a single T cell parent potentially expressed up to four different TCRs: the heterodimeric TCR derived from the normal cell partner and that from BW, plus two possible mixed heterodimers. Although it was improbable that the (still unknown) antigen specificity of the BW TCR would obscure selected antigen specificities of the normal T cells that were hybridized, since TCRs commonly show a tendency to cross-react on at least some allogeneic MHC molecules, it seemed quite probable that the lymphoma-derived TCR could confer a response to an allogeneic MHC-epitope, and thereby confound the allo-MHC specificity of the normal T cell partner. Indeed, T cell hybridomas generated with BW5147 were found to respond at an higher than expected frequency to cells bearing I-Ab, and analysis of chromosome loss variants of one famous T cell hybridoma (DO-11.10), specific for cOVA/I-Ad, cOVA/I-Ab, and for I-Ab alone, showed that the reactivity of this hybridoma with I-Ab, in fact, depended on the presence of the BW5147-derived TCR-α chain (Blackman et al. 1986).
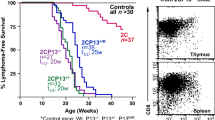
Thus, as with B cells a decade earlier (Kearney et al. 1979; Shulman et al. 1978), a fusion line for T cells incapable of expressing its own antigen receptor genes was needed. Such cells were not directly available, and because BW5147 had in the past worked better than other T cell-fusion lines, attempting to generate a TCR-deficient version of BW5147 seemed reasonable. Unencumbered by experience and thus perhaps overly optimistic, one of us (WB) thought that this might be accomplished by random mutagenesis, aided by the fact that due to allelic exclusion, functionally rearranged TCR genes are usually present only on one allele, in contrast to most other genes. Among cloned survivors of high dose γ-irradiation lethal for the majority of BW5147 cells, we were, in fact, able to isolate two clones, which no longer expressed Vα1.1, the Vα gene of the BW TCR. Only one of these, later simply named BWalpha- (BWα-) (Fig. 1), gave rise to stable hybridomas. Interestingly, during the test-hybridizations, we found that BWα-, unlike BW5147, was permissive for expression not only of the αβ TCR but also of the γδ TCR (Born et al. 1987). This lucky break allowed us to generate with randomly fused day 16 fetal mouse thymocytes a small collection γδ TCR+ hybridomas, to purify the γδ hetero-dimer of one of them, and to sequence the γ and δ protein chains (Born et al. 1987). Peptide sequences derived from the γ protein matched those of the earlier described γ genes (Hayday et al. 1985), and the sequences obtained from the δ protein established that the candidate for a “TCR δ-gene”, reported by Chien et al. (1987) earlier the same year, indeed encoded TCR-δ. Thus, as proposed by two research groups in the year before (Bank et al. 1986; Brenner et al. 1986), the cell-surface-expressed γδ molecule discovered by Brenner, Bank and colleagues indeed represented a second hetero-dimeric TCR, encoded by genes distinct from those of the αβ TCR (Born et al. 1987).
We then subjected BWα- to irradiation again, and one of the cloned survivors, later named BWalpha-beta- (BWα-β-), no longer expressed Vβ1.1, the Vβ gene of the BW5147 TCR. Southern blots and DNA-sequencing confirmed deletion mutations for both genes (White et al. 1989). The double TCR-loss mutant, BWα-β- (Fig. 1), which finally allowed the direct generation of T cell hybridomas that exclusively express the TCR of the normal T cell fusion partner, was immediately pressed into use by others and us (Happ et al. 1989; O'Brien et al. 1989), well before its formal publication. The paper by White et al. (1989), which describes the genesis of BWα- and BWα-β-, also includes molecular details of the gene-loss mutations, and it provides direct evidence that the expressed TCR-α chain of BW5147 imparts both I-Ab and I-Eb allo-specificities on TCRs of which it is a component.
Derivatives of BWα-β-
By the end of 1989, BWα-β- had become the T cell fusion line of choice, similarly to the Ig-deficient B cell fusion lines a decade earlier. Still, inherent properties of this cell line and its parent, BW5147, both of which express CD4 but not CD8, imposed certain limitations on T cell hybridization. For example, hybridomas generated with BWα-β- or BW5147 rarely express CD8, and if so, only transiently, which could impair the functionality of CD8-dependent T cells, limiting its use to CD4+ MHCII-restricted and non-conventional αβ T cells as well as a majority of γδ T cells. Carbone et al. (1988b) found that BW5147 actively suppresses CD8 expression in T cell hybridomas by re-methylating the CD8 gene locus, which is de-methylated in CD8+ T cells, on the chromosomes of the normal T cell partners. Because CD4+ murine T cells also contain de-methylated CD8 genes (Carbone et al. 1988a), perhaps the thymus lymphoma BW5147 represents a stage in thymocyte maturation prior to “double positive” thymocytes. To address this limitation, Burgert et al. (1989) transfected a CD8α cDNA construct into the BWα-β- fusion line. Fortunately, the BWα-β- cells proved incapable of suppressing CD8α when expressed from this construct, and the transfected cells expressed CD8α on their surface. One high-level CD8α-expressing clone, referred to in their paper as BWLyt2-4, proved to be a suitable fusion line (Fig. 1), capable of supporting the generation of CD8 + MHCI-restricted T cell hybridomas (Burgert et al. 1989).
Upon stimulation via the TCR, hybridomas generated with BW5147 or BWα-β- tend to produce IL-2 (as well as other factors), and this feature can be used to measure average antigen responses of these cells using cytokine ELISA or more indirect biological assays. However, these assays are not suitable for the detection of antigen responses by individual cells. Therefore, Sanderson and Shastri (1994) established a single cell reporter assay based on the observation that the nuclear factor of activated T cells (NFAT) enhancer element of the IL-2 gene can regulate expression of the Escherichia coli lacZ reporter gene in activated T cells. To introduce this feature into T cell hybridomas, they then transfected BWα-β- and BWα-β-CD8α+ (BWLyt2-4) cells with an inducible NFAT-lacZ gene construct to generate two new fusion partners (Fig. 1), referred to in their paper as BWZ.36 (i.e. BWα-β-NFAT-lacZ) and BWZ.36 CD8α (i.e. BWα-β-CD8α+NFAT-lacZ) (Sanderson and Shastri 1994). They found that measuring ligand-induced T cell activation by the lacZ assay was simpler, faster and cheaper by comparison with conventional IL-2 assays. More importantly, with the lacZ-based IL-2-reporter lines, they were able to detect activation of individual hybridoma cells (Sanderson and Shastri 1994). Taking advantage of this feature, we further explored a previously observed characteristic of γδ T cell hybridomas, which responded to peptide antigens in the absence of APCs (O'Brien et al. 1992), unlike peptide-specific αβ T cells. Using an insulin-peptide-specific γδ T cell hybridoma generated with the IL-2 reporter fusion line, we observed that isolated single cells responded to the insulin peptide, indicating that no cell–cell interactions are required in this response (Zhang et al. 2010). In this regard, the γδ TCR-dependent response to the insulin peptide resembles B cell-reactivity more than conventional T cell-reactivity. A B cell-like mode of antigen recognition for γδ T cells had been already proposed by Rock et al. (1994), based on a structural analysis and comparison of γδ and αβ TCRs, and BCRs.
The IL-2 reporting T cell fusion lines established by Sanderson and Shastri (1994) require for the detection of lacZ activity a histochemistry that kills the responding cells. Activated labeled cells can be analyzed in bulk using a colorimetric assay, or individually by microscopy. However, to keep responding cells alive for further study, a different reporting system was needed. Consequently, a new fusion partner was derived from BWα-β-, carrying four copies of the minimal human IL-2 promoter, each containing three NFAT-binding sites inserted upstream of the EGFP coding sequence (BW NFAT-EGFP) (Kisielow et al. 2011; van Essen et al. 2009) (Fig. 1). This fusion line is able to confer green fluorescence to hybridomas activated via the TCR. Using the “green” fusion line, Kisielow et al. (2011) then generated hybridomas with thymocytes that had been activated with plate-bound anti-CD3ε and anti-CD28 monoclonal antibodies, and cultured in the presence of mouse IL-2, and were able to measure by flow cytometry responses of these hybridomas to different stimuli, by determining the percentage of GFP+ “green” cells. In a further modification, BWα-β- was transduced with an NFAT-slow fluorescent timer (sFT) construct (Fig. 1) (Kisielow et al. 2019). Over time, the inducible sFT reporter protein changes its fluorescence from blue to red, a feature that allows for distinguishing NFAT activation events based on the timing of their occurrence (Kisielow et al. 2019; Subach et al. 2009).
All of these BWα-β- derived fusion lines are eminently suitable for the study of T cell hybridomas and their TCR-dependent responses, but due to the inherent CD3-deficiency of BW5147, they do not serve for investigations using transfected or transduced TCR-constructs. Initially, this problem had been addressed by selecting TCR-loss variants of T cell hybridomas with BW5147 that could then be used to express and study extraneous TCR constructs. Thus, Letourneur and Malissen (1989) were able to isolate a TCR-α and -β-deficient variant of the hybridoma DO-11.10.7, 58α-β-, which they then used to express other TCRs. Interestingly, in their characterization of the TCR-loss variant 58α-β-, the same group also detected a BW5147-derived non-functional TCR-α gene, which is still present in BWα-β- but cannot give rise to a surface-expressed TCR-α protein. 58α-β- also supports the expression of the γδ TCR (Fu et al. 1994). A second hybridoma-derived TCR-loss variant, 5KC-73.8.20α-β- (White et al. 1993), has also been used for the expression and study of αβ and γδ TCRs (Zhang et al. 2010), and finally, a TCR-β gene-deficient subclone of the T cell hybridoma DS23.27, clone DS23.27.4G.4 (4G4), like BWα-β- generated by radiation mutagenesis, and initially used for studying of the influence of TCR-β on allo-reactivity (DiGiusto and Palmer 1994), is now available. All of these (BW-derived) TCR-deficient hybridomas served their purpose well but they came with “baggage”: Their additional chromosomes, which can account for genetic instability with hybridomas, also may cause instability in gene-transfected/transduced cell lines. In addition, these cells express MHC molecules from genetically different parents, which adds some complexity. This problem has been solved by directly transducing BWα-β- with a multi-cistronic retroviral vector encoding all murine CD3 subunits plus GFP (Fig. 1) (Dunst et al. 2020; Holst et al. 2008). This manipulation created a more stable BW5147-derived cell line with the ability to functionally express extraneous TCRs. Dually transduced BWα-β- cells expressing both the slow fluorescent timer and CD3 (BW-sFT-CD3) (Fig. 1) were recently used successfully to solve the long-standing problem of “spontaneous” reactivity in hybridomas expressing TCR-Vγ1 and a limited set of TCR-Vδs (Happ et al. 1989; O'Brien et al. 1989). Here, Dunst et al. (2020) found that cells transduced with the relevant TCR genes actually respond to negatively charged surfaces present in tissue culture vessels. Their observation fits perfectly with observations of broad reactivity of certain γδ T cells with multiple unrelated poly-anionic ligands (Born et al. 1999, 2013), and a concept of non-conventional binding interactions between these ligands and TCR-Vγ1+ γδ TCRs (Born et al. 2013; Dunst et al. 2020).
Conclusion
The story of BW5147, an AKR mouse strain-derived thymus lymphoma, which became—mainly in the form of its TCR-gene-deficient derivative, BWα-β-, the most widely used tumor cell partner for the generation of T cell hybridomas, has been ripe with fascinating discoveries and the occasional pitfalls. Most likely, the story is not over yet as new modifications of this fusion-line continue to increase experimental options and potential applications.
References
Bank I, DePinHo RA, Brenner MB et al (1986) A functional T3 molecule associated with a novel heterodimer on the surface of immature human thymocytes. Nature 322:179–181
Blackman M, Yague J, Kubo R et al (1986) The T cell recpertoire may be biased in favor of MHC recognition. Cell 47:349–357
Bolliger L, Johansson B (1999) Identification and functional characterization of the zeta-chain dimerization motif for TCR surface expression. J Immunol 163:3867–3876
Born W, Yague J, Palmer E et al (1985) Rearrangement of T-cell receptor b-chain genes during T-cell development. Proc Natl Acad Sci USA 82:2925–2929
Born W, Rathbun G, Tucker P et al (1986) Synchronized rearrangement of T-cell γ and β chain genes in fetal thymocyte development. Science 234:479–482
Born W, Miles C, White J et al (1987) Peptide sequences of T-cell receptor δ and γ chains are identical to predicted X and γ proteins. Nature 330:572–574
Born W, White J, Kappler J et al (1988) Rearrangement of IgH genes in normal thymocyte development. J Immunol 140:3228–3232
Born W, Cady C, Jones-Carson J et al (1999) Immunoregulatory functions of gammadelta T cells. Adv Immunol 71:77–144
Born WK, Kemal Aydintug M, O'Brien R (2013) Diversity of gammadelta T-cell antigens. Cell Mol Immunol 10:13–20
Brenner MB, McLean J, Dialynas DP et al (1986) Identification of a putative second T-cell receptor. Nature 322:145–149
Burgert HG, White J, Weltzien HU et al (1989) Reactivity of VB17A+ CD8+ T cell hybrids: analysis using a new CD8+ T cell fusion partner. J Exp Med 170:1887–1904
Burnet FM (1959) The clonal selection theory of acquired immunity. Cambridge University Press, London
Carbone AM, Marrack P, Kappler JW (1988a) De-methylation of the CD8 gene in CD4+ murine T cells suggests that CD4+ cells develop from CD8+ precursors. Science 242:1174–1176
Carbone AM, Marrack P, Kappler JW (1988b) Remethylation at sites 5″ of the murine Lyt-2 gene in association withshutdown of Lyt-2 expression. J Immunol 141:1369–1375
Chien Y, Becker DM, Lindsten T et al (1984) A third type of murine T-cell receptor gene. Nature 312:31–35
Chien YH, Iwashima M, Kaplan K et al (1987) A new T-cell receptor gene located within the alpha locus and expressed early in T-cell differentiation. Nature 327:677–682
DiGiusto DL, Palmer E (1994) An analysis of sequence variation in the beta chain framework and complementary determining regions of an allo-reactive T cell receptor. Mol Immunol 31:693–699
Dunst J, Glaros V, Englmaier L et al (2020) Recognition of synthetic polyanionic ligands underlies “spontaneous” reactivity of Vgamma1gammadeltaTCRs. J Leukoc Biol. https://doi.org/10.1002/JLB.2MA1219-392R
Eshar Z, Apte RN, Lowy I et al (1980) T-cell hybridoma bearing heavy chain variable region determinants producing (T,G)-A-L-specific helper factor. Nature 286:270–272
Fu YX, Vollmer M, Kalataradi H et al (1994) Structural requirements for peptides that stimulate a subset of γδ T cells. J Immunol 152:1578–1588
Goldsby RA, Osborne BA, Simpson E et al (1977) Hybrid cell lines with T-cell characteristics. Nature 267:707–708
Gorer PA, Kaliss N (1959) The effect of isoantibodies in vivo on three different transplantable neoplasms in mice. Cancer Res 19:824–830
Hammerling GJ (1977) T lymphocyte tissue culture lines produced by cell hybridization. Eur J Immunol 7:743–746
Happ MP, Kubo RT, Palmer E et al (1989) Limited receptor repertoire in a mycobacteria-reactive subset of γδ T lymphocytes. Nature 342:696–698
Harwell L, Skidmore B, Marrack P et al (1980) Concanavalin A-inducible, interleukin-2-producing T cell hybridoma. J Exp Med 152:893–904
Haskins K, Kubo R, White J et al (1983) The major histocompatibility complex-restricted antigen receptor on T cells. I. Isolation with a monoclonal antibody. J Exp Med 157:1149–1169
Haskins K, Hannum C, White J et al (1984) The major histocompatibility complex-restricted antigen receptor on T cells. VI. An antibody to a receptor allotype. J Exp Med 160:452–471
Hayday AC, Saito H, Gillies SD et al (1985) Structure, organization, and somatic rearrangement of T cell gamma genes. Cell 40:259–269
Hedrick SM, Cohen DI, Nielsen EA et al (1984) Isolation of cDNA clones encoding T cell-specific membrane-associated proteins. Nature 308:149–153
Holst J, Wang H, Durick Eder K et al (2008) Scalable signaling mediated by T cell antigen receptor-CD3 ITAMs ensures effective negative selection and prevents autoimmunity. Nat Immunol 9:658–666
Hyman R, Stallings V (1974) Complementation patterns of Thy-1 variants and evidence that antigen loss variants “pre-exist” in the parental population. J Natl Cancer Inst 52:429–436
Kao FT, Puck TT (1969) Genetics of somatic mammalian cells. IX. Quantitation of mutagenesis by physical and chemical agents. J Cell Physiol 74:245–258
Kapp JA, Araneo BA, Clevinger BL (1980) Suppression of antibody and T cell proliferative responses to l-glutamic acid60-l-alanine30-l-tyrosine 10 by a specific monoclonal T cell factor. J Exp Med 152:235–240
Kappler JW, Skidmore B, White J et al (1981) Antigen-inducible, H-2-restricted, interleukin-2-producing T cell hybridomas. Lack of independent antigen and H-2 recognition. J Exp Med 153:1198–1214
Kappler J, White J, Wegmann D et al (1982) Antigen presentation by Ia+ B cell hybridomas to H-2 restricted T cell hybridomas. Proc Natl Acad Sci USA 79:3604–3607
Kappler J, Kubo R, Haskins K et al (1983a) The major histocompatibility complex-restricted antigen receptor on T cells in mouse and man: identification of constant and variable peptides. Cell 35:295–302
Kappler J, Kubo R, Haskins K et al (1983b) The mouse T cell receptor: comparison of MHC-restricted receptors on two T cell hybridomas. Cell 34:727–737
Katz DH, Bechtold TE, Altman A (1980) Construction of T cell hybridomas secreting allogeneic effect factor. J Exp Med 152:956–968
Kearney JF, Radbruch A, Liesegang B et al (1979) A new mouse myeloma cell line that has lost immunoglobulin expression but permits the construction of antibody-secreting hybrid cell lines. J Immunol 123:1548–1550
Kisielow J, Tortola L, Weber J et al (2011) Evidence for the divergence of innate and adaptive T-cell precursors before commtment to the alphabeta and gammadelta lineages. Blood 118:6591–6600
Kisielow J, Obermair FJ, Kopf M (2019) Deciphering CD4+ T cell specificity using novel MHC–TCR chimeric receptors. Nat Immunol 20:652–662
Köhler G, Milstein C (1975) Continuous cultures of fused cells secreting antibody of predefined specificity. Nature 256:495–497
Köhler G, Milstein C (1976) Derivation of specific antibody-producing tissue culture and tumor lines by cell fusion. Eur J Immunol 6:511–519
Köhler GI, Lefkovitz I, Elliott B et al (1977) Derivation of hybrids between a thymoma line and spleen cells activated in a mixed leucocyte reaction. Eur J Immunol 7:758–761
Kontiainen S, Simpson E, Bohrer E et al (1978) T-cell lines producing antigen-specific suppressor factor. Nature 274:477–480
Letourneur G, Malissen B (1989) Derivation of a T cell hybridoma variant deprived of functional T cell receptor α and β chain transcripts reveals a nonfunctional α-mRNA of BW5147 origin. Eur J Immunol 19:2269–2274
Marrack P, Hannum C, Harris M et al (1983a) Antigen-specific, major histocompatibility complex-restricted T cell receptors. Immunol Rev 76:131–145
Marrack P, Shimonkevitz R, Hannum C et al (1983b) The major histocompatibility complex-restricted antigen receptor on T cells. IV. An antiidiotypic antibody predicts both antigen and I-specificity. J Exp Med 158:1635–1646
O'Brien RL, Happ MP, Dallas A et al (1989) Stimulation of a major subset of lymphocytes expressing T cell receptor γδ by an antigen derived from Mycobacterium tuberculosis. Cell 57:667–674
O'Brien RL, Fu YX, Cranfill R et al (1992) Heat shock protein Hsp-60 reactive γδ cells: A large, diversified T lymphocyte subset with highly focused specificity. Proc Natl Acad Sci USA 89:4348–4352
Ozaki S (1998) Hybridomas, T cell. In: Delves P, Roitt I (eds) Encyclopedia of immunology, vol 2, 2nd edn. Academic Press, New York, pp 1152–1154
Rock EP, Sibbald PR, Davis MM et al (1994) CDR3 length in antigen-specific immune receptors. J Exp Med 179:323–328
Roehm N, Herron L, Cambier J et al (1984) The major histocompatibility complex-restricted antigen receptor on T cells: distribution on thymus and peripheral T cells. Cell 38:577–584
Sanderson S, Shastri N (1994) LacZ inducible, antigen/MHC-specific T cell hybrids. Int Immunol 6:369–376
Shulman MC, Wilde D, Köhler G (1978) A better cell line for making hybridomas secreting specific antibodies. Nature 276:269–270
Subach FV, Subach OM, Gundorov IS et al (2009) Monomeric fluorescent timers that chnage color from blue to red report on cellular trafficking. Nat Chem Biol 5:118–126
Taniguchi M, Miller JF (1978) Specific suppressive factors produced by hybridomas derived from the fusion of enriched suppressor T cell and a T lymphoma cell line. J Exp Med 148:373–382
Taussig MJ, Corvalan JR, Binns RM et al (1979) Production of an H-2-related suppressor factor by a hybrid T cell line. Nature 277:305–308
van Essen D, Engist B, Natoli G et al (2009) Two modes of transcriptional activation at native promoters by NF-kappaB p65. PLoS Biol 7:e73
Watson J (1979) Continuous proliferation of murine antigen-specific helper T lymphocytes in culture. J Exp Med 150:1510–1519
White J, Haskins KM, Marrack P et al (1983) Use of I region-restricted, antigen-specific T cell hybridomas to produce indiotypically specific anti-receptor antibodies. J Immunol 130:1033–1037
White J, Blackman M, Bill J et al (1989) Two better cell lines for making hybridomas expressing specific T cell receptors. J Immunol 143:1822–1825
White J, Pullen A, Choi K et al (1993) Antigen recognition properties of mutant Vbeta3+ T cell receptors are consistent with an imunoglobulin-like structure for the receptor. J Exp Med 177:119–125
Zhang L, Jin N, Nakayama M et al (2010) Gamma delta T cell receptors confer autonomous responsiveness to the insulin-peptide B:9–23. J Autoimmun 34:478–484
Acknowledgements
The authors would like to acknowledge the continued encouragement and support by Drs. Philippa Marrack and John Kappler.
Funding
None.
Author information
Authors and Affiliations
Contributions
The preparation of the manuscript was a joint effort by the authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest or competing interests.
Consent for publication
The authors declare their consent for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
White, J., O’Brien, R.L. & Born, W.K. BW5147 and Derivatives for the Study of T Cells and their Antigen Receptors. Arch. Immunol. Ther. Exp. 68, 15 (2020). https://doi.org/10.1007/s00005-020-00579-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00005-020-00579-1