Abstract
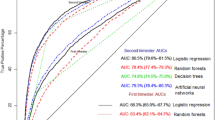
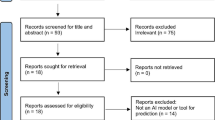
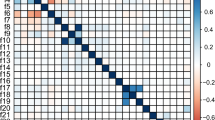
The objective of this systematic review is to analyze the application of machine learning for the prediction of pregnancy complications through an extensive review of published literature. The data sources for this research are scientific journals listed in prominent databases such as PubMed and Scopus. The findings of this research suggest that machine learning has been effectively employed in predicting pregnancy complications in multiple studies. Decision tree, random forest, logistic regression, and neural network are among the various machine learning algorithms that were utilized in this investigation. However, there are limitations to using machine learning technology in predicting pregnancy complications, such as reliance on the quality of data and a lack of transparency in the prediction process. This study provides a comprehensive understanding of the application of machine learning in predicting pregnancy complications and establishes a firm basis for further research in this area.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Padilla CR, Shamshirsaz A (2022) Critical care in obstetrics. Best Pract Res Clin Anaesthesiol 36:209–225
WHO (2017) Recommendations on newborn health: approved by the WHO Guidelines Review Committee WHO, 1–28
World Health Organization (2020) Maternal mortality evidence brief, 1–4
Leonard SA, Main EK, Lyell DJ (2022) Obstetric comorbidity scores and disparities in severe maternal morbidity across marginalized groups. Am J Obstet Gynecol MFM 4
Diana S, Wahyuni CU, Prasetyo B (2020) Maternal complications and risk factors for mortality. J Public health Res 9:1842
Mehari MA, Maeruf H, Robles CC, Woldemariam S, Adhena T, Mulugeta M, Haftu A, Hagose H, Kumsa H (2020) Advanced maternal age pregnancy and its adverse obstetrical and perinatal outcomes in Ayder comprehensive specialized hospital, Northern Ethiopia, 2017: a comparative cross-sectional study. BMC Pregnancy Childbirth 20:1–10
Bhandari TR (2013) Maternal and child health situation in South East Asia. Nepal J Obstet Gynaecol 7:5–10
Sadovsky Y, Mesiano S, Burton GJ, Lampl M, Murray JC, Freathy RM, Mahadevan-Jansen A, Moffett A (2020) Advancing human health in the decade ahead: pregnancy as a key window for discovery: A Burroughs Wellcome Fund Pregnancy Think Tank. Am J Obstet Gynecol 223:312–321
Bertini A, Salas R, Chabert S, Sobrevia L, Pardo F (2022) Using machine learning to predict complications in pregnancy: a systematic review. Front Bioeng Biotechnol 9
Feduniw S, Golik D, Kajdy A, Pruc M, Modzelewski J (2022) Application of artificial ıntelligence in screening for adverse perinatal outcomes—a systematic review. Healthc 10
Attwaters M (2022) Detecting pregnancy complications from blood. Nat Rev Genet 23:136
Pietsch M, Ho A, Bardanzellu A, Zeidan AMA, Chappell LC, Hajnal JV, Rutherford M, Hutter J (2021) APPLAUSE: automatic prediction of PLAcental health via U-net segmentation and statistical evaluation. Med Image Anal 72
Schmidt LJ, Rieger O, Neznansky M, Hackelöer M, Dröge LA, Henrich W, Higgins D, Verlohren S (2022) A machine-learning-based algorithm improves prediction of preeclampsia-associated adverse outcomes. Am J Obstet Gynecol 227(77):e1-77.e30
Espinosa C, Becker M, Marić I, Wong RJ, Shaw GM, Gaudilliere B, Aghaeepour N, Stevenson DK (2021) Data-driven modeling of pregnancy-related complications. Trends Mol Med 27:762–776
Zheng D, Hao X, Khan M, Wang L, Li F, Xiang N, Kang F, Hamalainen T, Cong F, Song K, Qiao C (2022) Comparison of machine learning and logistic regression as predictive models for adverse maternal and neonatal outcomes of preeclampsia: a retrospective study. Front Cardiovasc Med 9
Cecula P (2021) Artificial intelligence: the current state of affairs for AI in pregnancy and labour. J Gynecol Obstet Hum Reprod 50
Sarno L, Neola D, Carbone L, Saccone G, Carlea A, Miceli M, Iorio GG, Mappa I, Rizzo G, Girolamo RD, D’Antonio F, Guida M, Maruotti GM (2020) Use of artificial intelligence in obstetrics: not quite ready for prime time. Am J Obstet Gynecol MFM 5
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med
Zeng X, Zhang Y, Kwong JSW, Zhang C, Li S, Sun F, Niu Y, Du L (2015) The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med 8:2–10
Belaghi RA, Beyene J, McDonald SD (2021) Prediction of preterm birth in nulliparous women using logistic regression and machine learning. PLoS One 16
Hamilton EF, Dyachenko A, Ciampi A, Maurel K, Warrick A, Garite TJ (2018) Estimating risk of severe neonatal morbidity in preterm births under 32 weeks of gestation. J Matern Neonatal Med 7058
Lu X, Wang J, Cai J, Xing Z, Huang J (2022) Predıctıon of gestatıonal dıabetes and hypertensıon based on pregnancy examınatıon data. J Mech Med Biol 22
Malacova E, Tippaya S, Bailey HD, Chai K, Farrant BM, Gebremedhin AT, Leonard H, Marinovich ML (2020) Stillbirth risk prediction using machine learning for a large cohort of births from Western Australia, 1980–2015. Sci Rep 10
Meyer R, Hendin N, Zamir M, Mor N, Levin G, Sivan E (2020) Implementation of machine learning models for the prediction of vaginal birth after cesarean delivery. J Matern Neonatal Med, 1–7
Pini N, Lucchini M, Esposito G, Tagliaferri S (2021) A machine learning approach to monitor the emergence of late intrauterine growth restriction. Front Artifial Intell 4:1–11
Romeo V, Ricciardi C, Cuocolo R, Stanzione A, Verde F, Sarno L, Improta G, Paolo P, Armiento MD, Brunetti A, Maurea S, Machine learning analysis of MRI-derived texture features to predict placenta accreta spectrum in patients with placenta previa. Magn Reson Imag 64:71–76
Shazly SA, Hortu I, Shih J-C, Melekoglu R, Fan S, MEO, GGE. (MOGGE) Foundation-A. İntelligence (AI) (2022) Prediction of clinical outcomes in women with placenta accreta spectrum using machine learning models: an international multicenter study. J Matern Neonatal Med 35:6644–6653
Yoffe L, Polsky A, Gilam A, Raff C, Mecacci F, Ognibene A, Crispi F, Gratacós E (2019) Early diagnosis of gestational diabetes mellitus using circulating microRNAs. Eur J Endocrinol 181:565–577
Feduniw S, Sys D, Kwiatkowski S, Kajdy A (2020) Application of artificial intelligence in screening for adverse perinatal outcomes: a protocol for systematic review. Med (United States) 99:E23681
Cho H, Lee EH, Lee K-S, Heo JS (2022) Machine learning-based risk factor analysis of adverse birth outcomes in very low birth weight infants. Sci Rep 12
Rani S, Kumar M (2021) Prediction of the mortality rate and framework for remote monitoring of pregnant women based on IoT. Multimed Tools Appl 80:24555–24571
Belciug S (2022) Learning deep neural networks’ architectures using differential evolution. Case study: medical imaging processing. Comput Biol Med 146
Hang Y, Zhang Y, Lv Y, Yu W, Lin Y (2021) Electronic medical record based machine learning methods for adverse pregnancy outcome prediction. In: T, J, D, Q, Y, L, K, M (eds) 12th International conference on signal processing systems. SPIE, Key Laboratory of System Control and Information Processing, Ministry of Education, Shanghai Jiao Tong University, Shanghai, China
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this paper
Cite this paper
Lestari, D., Maulana, F.I., Persada, S.F., Adi, P.D.P. (2023). Machine Learning for Perinatal Complication Prediction: A Systematic Review. In: Ranganathan, G., Papakostas, G.A., Rocha, Á. (eds) Inventive Communication and Computational Technologies. ICICCT 2023. Lecture Notes in Networks and Systems, vol 757. Springer, Singapore. https://doi.org/10.1007/978-981-99-5166-6_53
Download citation
DOI: https://doi.org/10.1007/978-981-99-5166-6_53
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-99-5165-9
Online ISBN: 978-981-99-5166-6
eBook Packages: Intelligent Technologies and RoboticsIntelligent Technologies and Robotics (R0)