Abstract
Disorders of consciousness (DoC) is a state where consciousness has been affected by severe damage to the brain, including acute or prolonged DoC (pDoC). The pDoC means that the loss of consciousness lasts for more than 28 days, with the first cause being cerebral trauma, followed by stroke and hypoxic encephalopathy. pDoC is classified into vegetative state (VS) and minimally conscious state (MCS) according to the level of residual consciousness. VS refers to a state in which basic brainstem reflexes and sleep-wakefulness cycles are preserved, with spontaneous or stimulated eye-opening, but with no consciousness. MCS refers to the presence of clear signs of consciousness with discontinuity and fluctuation in patients after severe brain injury. It is more difficult for patients in VS to recover consciousness, while MCS patients have good recovery potential. New clinical and imaging data suggest that some pDoC patients may still benefit from therapeutic interventions several years after the onset of the disease. Most studies aimed at improving the level of consciousness and functional recovery of patients are open trials or case reports about behavior or brain imaging. The results of a few randomized controlled trials, especially on noninvasive neurostimulation treatments, have been published. It suggests that new therapies such as neurostimulation are valuable for the treatment of DoC, while the stimulation method and parameters still need further testing and validation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Disorders of consciousness (DoC) is a state where consciousness has been affected by severe damage to the brain, including acute or prolonged DoC (pDoC). The pDoC means that the loss of consciousness lasts for more than 28 days, with the first cause being cerebral trauma, followed by stroke and hypoxic encephalopathy. pDoC is classified into vegetative state (VS) and minimally conscious state (MCS) according to the level of residual consciousness. VS refers to a state in which basic brainstem reflexes and sleep-wakefulness cycles are preserved, with spontaneous or stimulated eye-opening, but with no consciousness. MCS refers to the presence of clear signs of consciousness with discontinuity and fluctuation in patients after severe brain injury, and MCS− refers to the clinical presence of visual object tracking, pain stimulation localization, and directed voluntary movements, but the inability to complete the activities as required. MCS+ is a state in which patients can move eyes, open or close eyes, and stably move limbs as required while fail in functional communication with others or intentionally using objects. It is more difficult for patients in VS to recover consciousness, while MCS patients have good recovery potential (Giacino et al. 2018). The key of pDoC patient assessment is to determine the consciousness level of patients by identifying whether the response to stimulation is reflexive or comes from active behavior with partial perceptual involvement. The JFK Coma Recovery Scale-Revised (CRS-R) is the standard clinical scale for the examination and assessment of pDoC (Giacino et al. 2004). The CRS-R and the Glasgow Outcome Scale-Extended (GOS-E) are the primary prognostic evaluation tools for DoC (Group of Disorders of Consciousness and Conscious-promotion, Professional Committee of Neurorepair of Chinese Medical Doctor Association 2021).
The treatment option for DoC matters. New clinical and imaging data suggest that some pDoC patients may still benefit from therapeutic interventions several years after the onset of the disease. Most studies aimed at improving the level of consciousness and functional recovery of patients are open trials or case reports about behavior or brain imaging. The results of a few randomized controlled trials, especially on noninvasive neurostimulation treatments, have been published. It suggests that new therapies such as neurostimulation are valuable for the treatment of DoC, while the stimulation method and parameters still need further testing and validation (Bourdillon et al. 2019).
As patients are unable to express themselves, DoC treatment should follow the four basic principles of medical ethics: autonomy, non-maleficence, beneficence, and justice. The recommendation on treatment abandonment in the early stage of injury (within 28 days) needs to be made with great caution, and the treatment strategy after the stabilization period should take the state of consciousness, physical condition, pre-morbid wishes, and family opinions of the patients into account. When attempting new clinical interventions, adequate supportive evidence and relevant study reports, sound study protocols and risk control measures should be provided, and ethical approval should be provided. Families should be adequately informed of the evidence, limitations, potential risks, and harms of treatments. Patients in the prolonged phase need to be systematically evaluated in an experienced center, and the patient’s family should be informed of the patient’s prognosis and the need for a long-term assisted care plan in case of permanent disability, if possible (Kondziella et al. 2020).
1 Noninvasive Neurostimulation Technique
1.1 Repetitive Transcranial Magnetic Stimulation
Stimulation Principle
Repetitive transcranial magnetic stimulation (rTMS) is based on the principle of electromagnetic induction to create an electric field in the brain, which induces neural depolarization to achieve the effect of modulating the excitability of the cortex. Primary motor cortex (M1) stimulation may enhance the excitability of the motor cortex, and the stimulation to dorsolateral prefrontal cortex (DLPFC) may induce stronger connectivity between the prefrontal cortex and the thalamus (Thibaut et al. 2019).
Stimulation Protocols
There is no consensus on the parameters of rTMS for pDoC. It is recommended to apply rTMS at 5–20 Hz with an intensity of 90–100% motor threshold to DLPFC, parieto-occipital junction, or motor area M1 for a course of 1–20 days, with 300–1500 pulses in total (O’Neal et al. 2021). Multiple treatment courses may also be considered based on the recovery characteristics of the disease. It may be implemented as early as possible after the primary condition is stabilized and the cerebral edema has resolved. It is not recommended for patients with unstable lesions in the target area, a history of epilepsy, skull defects at the treatment site, or metal implants in the body.
Clinical Application
A single-blind, uncontrolled study conducted in China applied 20 times rTMS at 10 Hz to DLPFC (11 min per stimulation) in 16 patients with DoC (3–35 months post-injury) (Xia et al. 2017). All 5 MCS patients and 4/11 VS patients showed an improvement in the total score of CRS-R, and the improvement was more significant in MCS patients. The prefrontal lobe may be a better target for stimulation than the motor cortex. Several randomized controlled trials (RCT) tests of high-frequency rTMS to the M1 region of DoC patients have been completed and have found that rTMS affects cerebral blood flow and subsequent electroencephalogram (EEG) power spectrum in MCS patients (He et al. 2018; Liu et al. 2018). Although none of the current studies on RCT of rTMS have shown significant effects at the group level, there are many parameters (e.g., stimulation type, frequency, or duration) that can be optimized to improve its efficacy.
1.2 Transcranial Direct Current Stimulation
Stimulation Principle
To modulate the excitability and connectivity of the cortex with weak direct current; the cumulative effect of long-course transcranial direct current stimulation (tDCS) modulation can reshape the consciousness network (Xia et al. 2018). The prefrontal cortex can be a target for stimulation because it is extensively connected to the striatum. The connectivity between thalamus and cortex can be strengthened by stimulating the striatum and disinhibiting the thalamus. MCS is more likely to benefit from treatment (Barra et al. 2022).
Treatment Protocols
There is no unified standard regarding the stimulation site, time, parameters, and treatment course of tDCS for pDoC patients up to now. The recommended stimulation site is DLPFC or posterior parietal cortex, at 10–20 min per stimulation and 1–2 mA for 10–20 days. It should be applied with caution in patients with a history of epilepsy or intracranial metal implants.
Clinical Application
A double-blind randomized controlled trial tested the effects of tDCS on the prefrontal lobe (i.e., continuous stimulation to the left DLPFC at 2 mA for 20 min) in 55 patients with acute and prolonged DoC (1 week–26 years after injury). At the group level, behavioral improvements (as measured by the CRS-R) were observed in MCS patients, but not in VS patients. At the individual level, 13/30 MCS (43%) showed improvements associated with tDCS (i.e., recovery of clinical signs of awareness not observed prior to tDCS or during sham treatment). Importantly, no patients reported side effects associated with tDCS (Thibaut et al. 2014).
1.3 Other Neurostimulation Therapies
Transcutaneous auricular vagal nerve stimulation (taVNS) increases cerebral blood flow, enhances brain electrical activity, affects the secretion of neurotransmitters, and increases wakefulness and awareness levels. taVNS may be applied early to the right side with a current of 10–20 mA and a frequency of 40–70 Hz at 1 time/day or 30 min–8 h per stimulation for 7–30 days. taVNS enters the nucleus tractus solitaries of the brainstem through the auricular branch of the vagus nerve and joins the ascending reticular activating system to participate in the modulation of the consciousness loop (Briand et al. 2020). There are no studies with large sample sizes, and the mostly recommended stimulation sites include the margin middle of bilateral auricular concha (AT2.3.4i) and the acupuncture points on brainstem (AT3.4i) (Yu et al. 2021). Stimulation with an intensity of 6 mA is applied continuously at 20 min per time, with 10 days per course. In addition, there are a few case reports on treating early post-traumatic disorders of consciousness and improving the language comprehension and spatio-temporal orientation of patients with low-intensity focused ultrasound pulsations (Cain et al. 2022).
2 Implantable Device Stimulation Technique
Implantable neuromodulation therapy for DoC has been studied for nearly 50 years. Several clinical studies have shown that it can significantly improve consciousness and behavior. However, due to the complexity and diversity of injury mechanisms and conditions in disorders of consciousness, systematic studies with large sample size are lacking. As there are many defects in terms of key scientific issues such as case screening, implementation, program control paradigm, and efficacy evaluation of nerve electrical stimulation for arousal, it has not become a definite therapy method. Therefore, neuromodulation surgery for pDoC should be taken as a complementary tool to conventional therapy. Before surgical evaluation, patients should be recommended to receive conventional rehabilitation and arousal treatment preferentially. The results of the evaluation should be fully explained to the family prior to surgery, and the possible efficacies should be clearly communicated. Recommended indications for surgery: (1) Patients with sudden onset of DoC and consistent with the diagnosis of MCS; (2) The duration of disease must be more than 3 months, with no progressive improvement or deterioration of consciousness for more than 4 consecutive weeks; for traumatic injuries, it is recommended to extend the surgery to be 6 months after the injury with no improvement of consciousness for 8 consecutive weeks; (3) Patients do not have serious complications or contraindications to surgery (Functional Neurosurgery Group of the Chinese Neurosurgery Medical Association, Professional Committee of Neurorepair of Chinese Medical Doctor Association, Chinese Society of Consciousness and Disorders of Consciousness 2019).
2.1 Deep Brain Stimulation
Treatment Principle
The implantation target of deep brain stimulation (DBS) for improving the state of consciousness in DoC patients is mainly at the centrothalamic region with the center median-parafascicular complex (CM-pf) as the core, which aims to improve the low neural activity level after brain injury and enhance wakefulness and consciousness based on the central loop mechanism of consciousness by stimulating the key nodes of the loop bilaterally in centrothalamus and activating the consciousness-related neural network of patients. If the connectivity within this large network or between the thalamus and this network is disrupted, DBS is unlikely to significantly affect this network via the thalamus. Traumatic lesions are often numerous but scattered, thus allowing the presence of more neural connections. Therefore, DBS may be more effective in traumatized patients.
The central thalamus, a key integration center for consciousness generation and maintenance, can induce incremental recruiting, augmenting response (Ward 2011), and amplitude modulation of EEG after receiving sustained low-frequency stimulation, thus activating and enhancing consciousness-related brain network activity (Schiff et al. 2007). Therefore, DBS is applied to compensate for the activity of centrothalamic neurons and thus restore cognitive functions based on these networks (e.g., attention, memory, language, and executive functions), and finally improve the level of consciousness (Baker et al. 2016). Animal studies have shown similar results. DBS can also repair neural cells and effectively control the progression of the disease. As for the neural remodeling that may be involved in the sustained effects of treatment, further observations and studies are needed.
Treatment Protocols
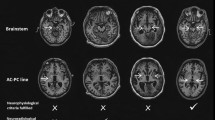
The basic surgical principles and methods are the same as those of other DBS procedures. Patients with severe destruction of intracranial structures or significant brain atrophy are not suitable for DBS. After general anesthesia, the stimulation is usually applied to the centromedian nucleus-parafascicular nucleus of the thalamus (CM-pf). The anatomical coordinates are X = 7–9 mm, Y = 8 mm (after the midpoint of anterior commissure—posterior commissure line), and Z = 0–3 mm. The planning of the electrode implantation path needs to avoid the lateral ventricles. The application of anesthetic or strong sedative drugs that affect cellular activity should be stopped after drilling to obtain satisfactory microelectrode records. According to preliminary observations, the discharge of CM-pf is significantly weaker than that of single cell in the adjacent nucleus mass, while studies with a large sample size are still required for verification. Implanted electrodes with long-pitch contacts are recommended. DBS is mainly unipolar, and the stimulation parameters of the program set should be set as follows: frequency: 25–100 Hz, wave width: 100–240 μs, voltage: 1.0–4.0 V. Cyclic stimulation mode is adopted, with daytime stimulation and nighttime power-off, to correspond to the normal wakefulness-sleep cycle (Functional Neurosurgery Group of the Chinese Neurosurgery Medical Association, Professional Committee of Neurorepair of Chinese Medical Doctor Association, Chinese Society of Consciousness and Disorders of Consciousness 2019).
Clinical Application
Clinical studies can be generally divided into three phases: (1) Early studies confirmed that DBS has an enhancing effect on the arousal system. Early animal studies found a relationship between the midbrain reticular formation and the arousal level, and stimulation caused an EEG desynchronization manifestation similar to the wakefulness state. In 1968, McLardy first applied DBS to the left medial interlaminar nucleus and midbrain reticular formation of a 19-year-old patient in a vegetative state 8 months after cerebral trauma (McLardy et al. 1968). Other subsequent studies took the intralaminar nucleus and the nucleus of medulla oblongata as DBS targets. Due to the limitations of the times, these studies all applied short-term stimulation lasting a few weeks, finding no clear evidence that the stimulation targets were structurally compatible with the arousal system. However, it was noted by all of these studies that stimulation could enhance behavioral response and lead to EEG desynchronization. (2) Finding targets and indications compliant with the physiological basis. In the 1980s, a multi-center study jointly conducted by France, Japan, and the United States was conducted on a cohort of 25 patients in a vegetative state with a course over 3 months, where DBS was applied to the parafascicular nucleus and the centromedian nucleus of the thalamus. 13 cases showed significant improvement in the level of consciousness after 1–3 weeks of treatment. Tsubokawa et al. evaluated eight patients in a vegetative state with a course of 2–3 months, three of which showed behavioral improvement (response to commands and phonation/verbal expression) and one showed partial behavioral improvement (resumption of oral feeding and expression of emotions) (Tsubokawa et al. 1990). In 2010, Yamamoto et al. evaluated 21 patients in VS, 8 of which awakened (38.1%) (Yamamoto et al. 2010). In 2013, Yamamoto et al. reported DBS or spinal cord stimulation for 36 patients in VS and MCS again, with 15 patients in the DBS group (15/26) regaining consciousness. Some other investigators also reported similar improvements (Yamamoto et al. 2013). This suggests that electrical neurostimulation can significantly improve the consciousness of patients. (3) Individualized DBS treatment protocols consistent with physiological mechanisms. In 2007, Nature reported a study published by Schiff et al. that was highly informative in determining the efficacy of DBS. A case report of a patient in minimally conscious state 6 years after trauma, treated with DBS to the intralaminar nucleus of thalamus, demonstrated significant improvement of symptoms after neurostimulator implantation. This was manifested by the comprehensible verbal expression and the correct use of objects that occurred in the early parameter titration phase, followed by compliance activity, voluntary limb movements and oral feeding, and in particular, the restoration of functional communication with others. Continuous DBS produced sustained effects on behavior, and behavioral improvements were maintained even during the DBS off period (Schiff et al. 2007). Animal studies have shown similar results. As for the neural remodeling that may be involved in the sustained effects of treatment, further observations and studies are needed.
2.2 Spinal Cord Stimulation
Treatment Principle
Spinal cord stimulation (SCS) is performed by surgically placing stimulation electrodes in the middle epidural region at C2–C4 level of the cervical cord. The electrical stimulation travels up the high cervical spinal cord to the brainstem and reaches the cerebral cortex through the ascending reticular activating system and the subthalamic activating system so that (1) the impulse stimulation at the initiation site of conscious impulses enhances the activity of conscious impulses, improves the state of nerve conduction and increases EEG activity via the pathway of ascending reticular activating system-thalamus-cortex (Della Pepa et al. 2013). (2) Modulation of sympathetic ganglion activity in the neck enhances CBF and improves cerebral metabolism. (3) It can increase the release of excitatory transmitters in the loop as well as the neurotransmitters (e.g., catecholamines, dopamine, and norepinephrine), and activate partial proteinase to enhance the modulation of biological signals.
Treatment Protocols
General anesthesia is generally performed in the prone or lateral position. Keep the neck in anterior flexion and incise it along the midline. Take out the C5 spinous process and the vertebral plate and fully loosen the C2–4 epidural space along the midline with a special dilator before delivering the surgical electrodes upward to the middle of the epidural region at the C2–4 level. Connect the wire and implantable pulse generator (IPG). Bipolar stimulation is commonly used for postoperative programmed SCS, with a stimulation frequency of 5–70 Hz for the program group. It is recommended to use 70 Hz as the preferred stimulation frequency, with a pulse width of 100–240 μs and a voltage of 1.0–5.0 V. The mode of cyclic stimulation is adopted, with daytime stimulation and nighttime power-off, to correspond to the normal wakefulness-sleep cycle (Functional Neurosurgery Group of the Chinese Neurosurgery Medical Association, Professional Committee of Neurorepair of Chinese Medical Doctor Association, Chinese Society of Consciousness and Disorders of Consciousness 2019).
Clinical Application
Komai first reported SCS for VS in the early 1980s (Kanno et al. 1989), after which Kanno and Momose et al. evaluated changes in cerebral glucose metabolism and cerebral blood flow in patients with DoC after SCS and confirmed that the local cerebral glucose metabolic rate and cerebral blood flow increased significantly before and after stimulation. They found that consciousness was restored in 56 (43%) of 130 cases of VS patients. In 2012, Yamamoto performed SCS on 10 MCS patients, 7 of whom showed significant improvement in consciousness (Yamamoto et al. 2013), Yamamoto et al. reported SCS for 10 patients in MCS again, with 5 of them restoring consciousness. The efficacy of SCS is now considered definite, with an overall response rate of 20–40% (Mattogno et al. 2017), while the arousal rate and effectiveness of VS for post-traumatic brain injury are even higher. It was first reported in China by Wang Peidong et al. in 2001 that 6 patients in VS received SCS treatment, 2 of whom were awakened. In 2019, Xia Xiaoyu and He Jianghong reported 110 patients with DoC treated with electrical neurostimulation, and the rate of arousal was about 30% (Xia et al. 2019).
2.3 Other Stimulation Modes
There are only few case reports on the arousal by cortical electrical stimulation, vagus nerve stimulation (VNS), and baclofen pump implantation, with unclear efficacy. For example, it was reported that implanted VNS was adopted in an uncontrolled case study on a VS patient with 15 years of onset. The patient improved from VS to MCS and showed enhanced brain connectivity (i.e., increased activity in the frontoparietal-occipital and basal ganglia regions) (Corazzol et al. 2017). As with all uncontrolled studies, this case report needed to be treated with caution. Nevertheless, it suggested the possibility of this approach for patients with DoC.
2.4 Major Complications of the Procedure and the Corresponding Management
2.4.1 Deviation in the Position of Electrodes
The actual position of DBS electrodes implanted may deviate from the intraoperative plan due to brain atrophy and deformation, cerebral ventriculomegaly, and intraoperative brain shift. Therefore, except for patients with severe brain atrophy and deformation who are not considered for DBS surgery, the procedure of DBS electrode implantation in patients with indications needs to be carefully checked and operated. In addition to the use of surgical planning system and electronic brain nucleus spectrum to improve localization accuracy, it is recommended to select stimulation electrodes with contacts separated by a long distance to cover as many nuclei of the central thalamus as possible, providing sufficient space for postoperative program control and adjustment. For SCS, preoperative X-ray positioning must be performed to ensure accurate implantation of electrodes, which should be placed in the midline of the spinal cord as much as possible to avoid discomfort on one side caused by low stimulation intensity that may otherwise affect the setting of program control parameters.
2.4.2 Incision and Skin Breakage
Patients with DoC are generally malnourished and therefore at high risk for skin breakage. Breakage at the IPG implantation site is often caused by postoperative skin pulling because the capsular bag is excessively small and shallow. When an incision split occurs, it should be cleared early, and the capsular bag should be enlarged and deepened. The incision should be sutured without tension. The subcutaneous effusion under IPG is uncommon, and most of the effusion can be self-absorbed under local pressure.
2.4.3 Stimulation-Related Convulsion or Epilepsy Seizure
If the SCS electrode deviates from the midline, stimulation is very likely to lead to convulsion and discomfort on one limb of the patient, resulting in the forced reduction of stimulation intensity or even the abandonment of stimulation contact, which ultimately affects the surgical outcome. Neuromodulation has the potential to induce epileptic seizures, which are not uncommon in post-DoC stimulation. When the stimulation parameters are not set properly or the intensity is too high, it can lead to EEG hyperactivity or even epilepsy seizure in patients, mostly generalized seizures. Once it occurs, stimulation should be stopped immediately. If there is no seizure in the following 1–2 weeks, the stimulation intensity can be adjusted downward and then turned on, and the intensity can be adjusted to the appropriate level if there is no abnormality in the subsequent observation.
Although neuromodulation surgery has become one of the major research hotspots and directions for the treatment of DoC, studies on surgical treatment are limited by the limited understanding of DoC, actual modulation ability, and clinical experience. In addition, there are many bottlenecks and difficulties in the selection of patients, determination of treatment target sites, setting of program control parameters and scientific verification of efficacy. Therefore, it should be performed cautiously and scientifically before becoming a common clinical practice, and its clinical efficacy and adverse events should be recorded in detail.
References
Baker JL, Ryou JW, Wei XF et al (2016) Robust modulation of arousal regulation, performance, and frontostriatal activity through central thalamic deep brain stimulation in healthy nonhuman primates. J Neurophysiol 116:2383–2404
Barra A, Rosenfelder M, Mortaheb S et al (2022) Transcranial pulsed-current stimulation versus transcranial direct current stimulation in patients with disorders of consciousness: a pilot, sham-controlled cross-over double-blind study. Brain Sci 12:429
Bourdillon P, Hermann B, Sitt JD et al (2019) Electromagnetic brain stimulation in patients with disorders of consciousness. Front Neurosci 13:223
Briand M-M, Gosseries O, Staumont B et al (2020) Transcutaneous auricular vagal nerve stimulation and disorders of consciousness: a hypothesis for mechanisms of action. Front Neurol 11:933
Cain JA, Spivak NM, Coetzee JP et al (2022) Ultrasonic deep brain neuromodulation in acute disorders of consciousness: a proof-of-concept. Brain Sci 12:428
Corazzol M, Lio G, Lefevre A et al (2017) Restoring consciousness with vagus nerve stimulation. Curr Biol 27:R994–R996
Della Pepa GM, Fukaya C, La Rocca G et al (2013) Neuromodulation of vegetative state through spinal cord stimulation: where are we now and where are we going? Stereotact Funct Neurosurg 91:275–287
Functional Neurosurgery Group of the Chinese Neurosurgery Medical Association, Professional Committee of Neurorepair of Chinese Medical Doctor Association, Chinese Society of Consciousness and Disorders of Consciousness (2019) Neurosurgery treatment of chronic disorders of consciousness Chinese Expert Consensus. Chin J Neurosurg 35:5
Giacino JT, Kalmar K, Whyte J (2004) The JFK Coma Recovery Scale-Revised: measurement characteristics and diagnostic utility. Arch Phys Med Rehabil 85:2020–2029
Giacino JT, Katz DI, Schiff ND et al (2018) Practice guideline update recommendations summary: Disorders of consciousness: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology; the American Congress of Rehabilitation Medicine; and the National Institute on Disability, Independent Living, and Rehabilitation Research. Neurology 91:450–460
Group of Disorders of Consciousness and Conscious-Promotion, Professional Committee of Neurorepair of Chinese Medical Doctor Association (2021) Diagnoses and treatments of prolonged disorders of consciousness: an experts consensus. Chin J Neuromed 19:977–982
He F, Wu M, Meng F et al (2018) Effects of 20 Hz repetitive transcranial magnetic stimulation on disorders of consciousness: a resting-state electroencephalography study. Neural Plast 2018:5036184
Kanno T, Kamel Y, Yokoyama T et al (1989) Effects of dorsal column spinal cord stimulation (DCS) on reversibility of neuronal function-experience of treatment for vegetative states. Pac Clin Electrophysiol 12:733–738
Kondziella D, Bender A, Diserens K et al (2020) European Academy of Neurology guideline on the diagnosis of coma and other disorders of consciousness. Eur J Neurol 27:741–756
Liu X, Meng F, Gao J et al (2018) Behavioral and resting state functional connectivity effects of high frequency rTMS on disorders of consciousness: a Sham-controlled study. Front Neurol 9:982
Mattogno PP, Barbagallo G, Iacopino G et al (2017) Recovery from chronic diseases of consciousness: state of the art in neuromodulation for persistent vegetative state and minimally conscious state, vol 124. Springer International Publishing, Cham, pp 19–25
McLardy T, Ervin F, Mark V et al (1968) Attempted inset-electrodes-arousal from traumatic coma: neuropathological findings. Trans Am Neurol Assoc 93:25–30
O’Neal CM, Schroeder LN, Wells AA et al (2021) Patient outcomes in disorders of consciousness following transcranial magnetic stimulation: a systematic review and meta-analysis of individual patient data. Front Neurol 12:694970
Schiff ND, Giacino JT, Kalmar K et al (2007) Behavioural improvements with thalamic stimulation after severe traumatic brain injury. Nature 448:600–603
Thibaut A, Bruno M-A, Ledoux D et al (2014) tDCS in patients with disorders of consciousness: Sham-controlled randomized double-blind study. Neurology 82:1112–1118
Thibaut A, Schiff N, Giacino J et al (2019) Therapeutic interventions in patients with prolonged disorders of consciousness. Lancet Neurol 18:600–614
Tsubokawa T, Yamamoto T, Katayama Y et al (1990) Deep-brain stimulation in a persistent vegetative state: follow-up results and criteria for selection of candidates. Brain Injury 4:315–327
Ward LM (2011) The thalamic dynamic core theory of conscious experience. Conscious Cogn 20:464–486
Xia X, Bai Y, Zhou Y et al (2017) Effects of 10 Hz repetitive transcranial magnetic stimulation of the left dorsolateral prefrontal cortex in disorders of consciousness. Front Neurol 8:182
Xia X, Yang Y, Guo Y et al (2018) Current status of neuromodulatory therapies for disorders of consciousness. Neurosci Bull 34:615–625
Xia XY, Yang Y, Dang YY et al (2019) Therapeutic effect of spinal cord stimulation on chronic disorders of consciousness after brain injury: a report of 110 cases. Chin J Neurosurg 35:5
Yamamoto T, Katayama Y, Kobayashi K et al (2010) Deep brain stimulation for the treatment of vegetative state: DBS for the treatment of VS. Eur J Neurosci 32:1145–1151
Yamamoto T, Katayama Y, Obuchi T et al (2013) Deep brain stimulation and spinal cord stimulation for vegetative state and minimally conscious state. World Neurosurg 80:S30.e1–S30.e9
Yu Y, Yang Y, Gan S et al (2021) Cerebral hemodynamic correlates of transcutaneous auricular vagal nerve stimulation in consciousness restoration: an open-label pilot study. Front Neurol 12:684791
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
He, J., Dang, Y. (2023). Disorders of Consciousness. In: Wang, Y. (eds) Therapeutics of Neural Stimulation for Neurological Disorders. Springer, Singapore. https://doi.org/10.1007/978-981-99-4538-2_27
Download citation
DOI: https://doi.org/10.1007/978-981-99-4538-2_27
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-99-4537-5
Online ISBN: 978-981-99-4538-2
eBook Packages: MedicineMedicine (R0)