Abstract
Pelvic floor dysfunction (PFD) is a general term for a variety of clinical disorders, including urinary incontinence (UI), pelvic organ prolapsed (POP) (Fig. 49.1), fecal dysfunction, lower urinary tract sensory and emptying abnormalities, sexual dysfunction, and some chronic pelvic pain syndromes. More than 15% of multiparous women are affected by the disease. The risk factors for PFD include vaginal delivery, multiparity, hysterectomy, advanced age, and chronic obstructive pulmonary disease, among which vaginal delivery and advanced age are the most correlated risk factors [1]. With increasing life expectancy, the negative effect of PFD on the health care system in terms of cost, productivity, and quality of life is critical. The clinical evaluation of PFD is mainly performed by using the POP quantification system, which demonstrated low sensitivity and specificity for the diagnosis of complex alterations [2]. The accuracy of clinical diagnosis directly affects the formulation of surgical plan, which is also one of the important reasons for associated surgical failure and high recurrence rates. Traditional techniques for PFD include assessment of the bladder and levator ani muscle (Fig. 49.2) by transvaginal ultrasonography (US), urodynamic test, and vesicovaginal defecography. During the past decade, three-dimensional (3D) and four-dimensional (4D) translabial ultrasonography and magnetic resonance imaging (MRI) have been used to accurately assess pelvic floor anatomy and function, enabling evaluation of all three pelvic compartments simultaneously. MRI has excellent soft tissue and time resolution and can evaluate the organs, muscles, and ligaments in the pelvic cavity in multiplanar without ionizing radiation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Pelvic floor dysfunction (PFD) is a general term for a variety of clinical disorders, including urinary incontinence (UI), pelvic organ prolapsed (POP) (Fig. 49.1), fecal dysfunction, lower urinary tract sensory and emptying abnormalities, sexual dysfunction, and some chronic pelvic pain syndromes. More than 15% of multiparous women are affected by the disease. The risk factors for PFD include vaginal delivery, multiparity, hysterectomy, advanced age, and chronic obstructive pulmonary disease, among which vaginal delivery and advanced age are the most correlated risk factors [1]. With increasing life expectancy, the negative effect of PFD on the health care system in terms of cost, productivity, and quality of life is critical. The clinical evaluation of PFD is mainly performed by using the POP quantification system, which demonstrated low sensitivity and specificity for the diagnosis of complex alterations [2]. The accuracy of clinical diagnosis directly affects the formulation of surgical plan, which is also one of the important reasons for associated surgical failure and high recurrence rates. Traditional techniques for PFD include assessment of the bladder and levator ani muscle (Fig. 49.2) by transvaginal ultrasonography (US), urodynamic test, and vesicovaginal defecography. During the past decade, three-dimensional (3D) and four-dimensional (4D) translabial ultrasonography and magnetic resonance imaging (MRI) have been used to accurately assess pelvic floor anatomy and function, enabling evaluation of all three pelvic compartments simultaneously. MRI has excellent soft tissue and time resolution and can evaluate the organs, muscles, and ligaments in the pelvic cavity in multiplanar without ionizing radiation.
Multiplanar MRI images of a female patient with pelvic organ prolapse (POP). (a) Midline sagittal section of a female patient at rest, this section should encompass the pubic symphysis, bladder neck, vagina, rectum, and coccyx. “PCL” line is the line from the lower border of the pubic symphysis to the last coccygeal joint, representing the level of the entire pelvic floor. Letter “B” in figures represents the lowest point of bladder neck (white arrow); letter “C” in figures represents the most inferior and anterior point of the cervix (white arrowhead); letter “R” in figures stands for anorectal junction (black framed arrowhead). The anorectal angle is within the normal range (asterisk). (b) Coronal T2WI obtained at rest of a 60-year-old female patient with POP. The iliococcygeus muscle and pubococcygeus muscle (black arrow) can be seen lost its horizontal configuration. (c) Sagittal T2WI HASTE obtained during straining. The vortices of urine in the bladder are caused by maximal straining of patient. The lowest point “B” of the bladder and the lowest point “C” of the anterior lip of the cervix changed obviously relative to the PCL. The anorectal angle becomes more obtuse during squeezing (asterisk). (d) Sagittal T2WI HASTE obtained during squeezing. The anorectal joint is higher and the angle becomes more acute than that in a. (e) Deformation of the vaginal fornix (asterisk)
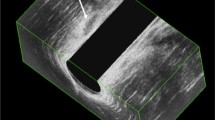
Imaging anatomy of levator ani muscle. (a) Coronal T2WI obtained at rest of a 52-year-old healthy woman. The bilateral iliococcygeus muscle and pubococcygeus muscle can be seen clearly (black long arrow), which having a horizontal orientation. The “U” shape of the puborectalis muscle with detachment of the right aspect of it can be seen in an axial T2WI (b). (c) Midsagittal T2WI. The levator plane is seen posterior to the rectum and anterior to the coccyx (white arrowhead)
1 Imaging Analysis
The pelvic floor is a dynamically balanced three-dimensional structure. The pelvic floor is divided into three major compartments: (1) anterior: urinary bladder, urethra, and urethral support system; (2) middle: vagina (anterior and posterior wall) and uterocervical support; and (3) posterior: rectum and support structure. The main support structures are the endopelvic fascia and ligaments, the pelvic diaphragm, and the urogenital diaphragm from cranial to caudal. The support structures of the pelvic floor consist of a complex interaction among the bones, muscles, ligaments, and organs. The pathological features of PFD generally affect the interrelated network of them and result in structural damage and dysfunction in three pelvic compartments [3].
MRI protocols of PFD consist of static sequences and dynamic sequences. Dynamic MRI examination is performed while the patient is squeezing, straining, and defecation. The findings seen on high-resolution T2-weighted images obtained at rest are helpful for anatomic evaluation. This mainly include puborectalis muscle, pubococcygeus muscle, iliac coccygeus muscle, levator plate, etc. The assessment should be focused on: (1) the structural and signal intensity, symmetry, and thickness of bilateral puborectalis muscle, pubococcygeus muscle, and iliac coccygeus muscle; (2) the levator plate tends to be vertical and is no longer roughly parallel to the upper half of the vagina; and (3) vagina loses its “H” shape on axial images [4].
Steady state (e.g., FISP, GRASS, FFE, PSIF, SSFP, T2-FFE) or balanced state free precession sequences (e.g., True-FISP, FIESTA, B-FFE) in sagittal plane is recommended for dynamic sequences (squeezing and straining) and evacuation sequence [5]. Interpretation of pelvic floor MRI requires a standardized approach. At present, pubococcygeal line (PCL) is the most widely accepted reference line. It extends from the inferior border of the pubic symphysis to the last coccygeal joint in the midsagittal plane, represents the level of the pelvic floor. Before MRI examination, approximately 180 mL of warm ultrasound gel is injected into the vagina and rectum in our institution to better display the organ reference point. In the anterior compartment of the pelvis, the reference point is the most inferior aspect of bladder base. In the middle compartment of the pelvis, the reference point is the most anterior and inferior aspect of the cervix or the vaginal posterior apex in patients who have undergone a hysterectomy. In the posterior compartment of the pelvis, the reference point is the anterior aspect of anorectal junction. The vertical distance from each reference point to PCL should be measured. In women with a normal pelvic floor anatomy, these organ reference points are located at or above the PCL level. Even in the case of maximum abdominal pressure, the range of variation not more than 1 cm below the PCL is considered normal. The severity of pelvic floor organ prolapse can be graded according to “Rule of three”: prolapse of an organ below the PCL by 3 cm or less is mild, between 3 cm and 6 cm is moderate, and more than 6 cm is severe [6, 7]. The change of the anorectal angle was observed, while the patient is resting and squeezing. This angle is drawn between the longitudinal axis of the anal canal and the posterior rectal wall. It normally measures 108°–127° at rest and varies between 15° and 20° during contraction or defecation. Failure of the anorectal angle to open (become more obtuse) during defecation and prolonged and incomplete evacuation of the rectal gel (less than two-third gel evacuated in more than 30 s) are suggestive of spastic pelvic floor syndrome.
The anterior compartment organ prolapse mainly includes cystocele (Fig. 49.3) and urethral hypermobility (Fig. 49.4). Cystocele is defined as greater than 1 cm descent of the posterior bladder wall or bladder neck below the PCL. The grading standard follows “Rule of three.” Clinically, eversion of the vaginal mucosa can be seen, and severe cystocele may cover up urethral hypermobility and impair bladder voiding. In healthy women, the urethral axis maintains vertical orientation. In patients with urethral hypermobility, there is a more drastic horizontal clockwise rotation greater than 30° during strain/evacuation, which can lead to stress urinary incontinence [8]. Moderate to severe bladder prolapse is usually associated. It is secondary to loss of periurethral and paraurethral support. Urethral hypermobility and funneling are associated with stress-induced urinary incontinence and can lead to urinary tract infections.
Cystocele. Sagittal HASTE image obtained during straining of a 55-year-old woman with cystocele. The “PCL” line is drawn from the inferior border of the pubic symphysis to the last coccygeal joint. Sagittal T2WI image showed the lowest point of the bladder (B), the vaginal vault (C), and the anorectal junction (R) all located below the PCL. The distance of Bb was 4.5 cm
Urethral hypermobility and urethral funneling. (a, b) Sagittal HASTE images obtained during straining of a 70-year-old woman and 65-year-old woman with cystocele, respectively. (a) Rotation of the urethral axis, even beyond the horizontal position. (b) Dilation of the proximal urethral lumen and apparent shortening of the urethra
The middle compartment organ prolapse mainly includes uterine prolapse (Fig. 49.5) or vaginal vault prolapse and peritoneocele. Uterine or vaginal vault prolapse is measured perpendicularly from the most anterior and inferior aspect of the cervix or the vaginal posterior apex to the PCL. Grading of the prolapse is severity according to “Rule of three.” In healthy women, the pouch of Douglas is normally located at the level of the posterior vagina fornix. Peritoneocele can be diagnosed when peritoneal fat and small bowel loop appeared between rectum and vagina, and the position of small bowel loop was lower than PCL. These hernias are named according to their content (peritoneal fat, small bowel loop, or sigmoid colon). On dynamic MRI, peritoneocele manifests at the end of the evacuation phase after emptying of the bladder and rectum [3].
Uterine prolapse. A 46-year-old woman with uterine prolapse. The sagittal T2WI image (a) obtained at rest showed the lowest point of bladder base (letter “B”) and cervix (letter “C”) located above the PCL, while the anorectal junction (letter “R”) located below it. The T2WI HASTE image obtained during straining (b) showed all the point B, C, R located below PCL obviously. Bb, Cc, Rr represent their vertical distances to PCL, respectively. Rectocele also could be seen in (b). The Y line represents the expected margin of the normal anorectal wall. The X line represents the depth of wall protrusion beyond the expected margin of the normal anorectal wall
The middle compartment organ prolapse mainly includes rectocele (Fig. 49.6) and intussusception (Fig. 49.7). The most common measurement of rectocele on MRI is the depth of wall protrusion beyond the expected margin of the normal anorectal wall. It usually occurs in the anterior wall of the rectum and occasionally involves the posterior and lateral walls. When the outpouching of the rectal wall is less than 2 cm, the rectocele is termed mild, while 2–4 cm is termed moderate, and greater than 4 cm is severe. Mild rectocele is more common, with a range of ≤3 cm, and these are considered clinically significant only when symptoms develop [9]. Intussusception and rectal prolapse are an invagination of the rectal wall and can be internal or external. The distance of parietal inversion from the anal verge can be classified as intrarectal, intra-anal, or extra-anal. MR defecography has the potential advantage of clearly distinguishing between rectal mucosal intussusception and rectal full-thickness intussusception [10]. An intussusception is commonly only visible at the end of defecation phase, when the gel is evacuated [11].
Dynamic MRI is a helpful diagnostic tool for patients with multicompartmental pelvic floor abnormalities, or for those with prior surgical repairs. It has unique advantage over traditional examinations. Dynamic MR imaging of the pelvic floor is valuable for selecting candidates for surgical treatment and for indicating the most appropriate surgical approach. A standardized MR imaging and reporting of PFD is crucial to enhance effective communication between the radiologist and the clinician for the sake of patients’ benefit.
References
Mant J, Painter R, Vessey M. Epidemiology of genital prolapse: observations from the Oxford Family Planning Association Study. Br J Obstet Gynaecol. 1997;104(5):579–85.
Woodfield CA, Hampton BS, Sung V, Brody JM. Magnetic resonance imaging of pelvic organ prolapse: comparing pubococcygeal and midpubic lines with clinical staging. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(6):695–701.
Chamié LP, Ribeiro DMFR, Caiado AHM, Warmbrand G, Serafini PC. Translabial US and dynamic MR imaging of the pelvic floor: normal anatomy and dysfunction. Radiographics. 2018;38(1):287–308.
El Sayed RF. Magnetic resonance imaging of the female pelvic floor: anatomy overview, indications, and imaging protocols. Radiol Clin North Am. 2020;58(2):291–303.
El Sayed RF, Alt CD, Maccioni F, et al. Magnetic resonance imaging of pelvic floor dysfunction – joint recommendations of the ESUR and ESGAR pelvic floor working group. Eur Radiol. 2017;27:2067–85.
Garcia del Salto L, de Miguel CJ, Aguilera del Hoyo LF, et al. MR imaging-based assessment of the female pelvic floor. Radiographics. 2014;34(5):1417–39.
Colaiacomo MC, Masselli G, Polettini E, et al. Dynamic MR imaging of the pelvic floor: a pictorial review. Radiographics. 2009;29(3):e35.
Gupta AP, Pandya PR, Nguyen M-L, et al. Use of dynamic MRI of the pelvic floor in the assessment of anterior compartment disorders. Curr Urol Rep. 2018;19:112.
Alapati S, Jambhekar K. Dynamic magnetic resonance imaging of the pelvic floor. Semin Ultrasound CT MRI. 2017;38:188–99.
Mortele KJ, Fairhurst J. Dynamic MR defecography of the posterior compartment: indications, techniques and MRI features. Eur J Radiol. 2007;61(3):462–72.
MRI of the pelvic floor and MR defecography. Hodler J, et al. editors. Diseases of the abdomen and pelvis 2018–2021, IDKD Springer Series.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Liu, J. (2023). Pelvic Floor Dysfunction. In: Zhang, G. (eds) MRI of Gynaecological Diseases. Springer, Singapore. https://doi.org/10.1007/978-981-99-3644-1_49
Download citation
DOI: https://doi.org/10.1007/978-981-99-3644-1_49
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-99-3643-4
Online ISBN: 978-981-99-3644-1
eBook Packages: MedicineMedicine (R0)