Abstract
Chronic cough in children is usually defined as a cough lasting ≥4 weeks. When managing children with chronic cough, most clinical practice guidelines recommend a similar systematic approach, in which it is crucial to find out specific cough pointers that suggest underlying diseases of cough through focused history, physical examination, and tests that can be easily performed in an outpatient setting. Additional investigations depend on the provisional diagnosis after initial evaluation and the clinical course of cough. Nonspecific cough can be managed with reassurance, watchful waiting, and reevaluation, whereas specific cough should be managed with etiology-based treatment. If empirical treatments are trialed due to parental concerns and/or diagnostic purpose under provisional diagnosis of asthma (isolated dry cough) or protracted bacterial bronchitis (isolated wet cough), a reassessment is recommended in predefined time frame (e.g., 2–4 weeks). If the cough has not improved substantially by this time, other causes should be considered.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Introduction
Cough is the most common reason for parents to seek medical advices for their children [1]. Most acute cough is associated with viral upper respiratory tract infections (URTIs). However, cough can be very distressing to watch if it persists and/or interferes with daily activities, including child and parents’ sleep. In addition, cough may present as a symptom of serious underlying pulmonary or extrapulmonary diseases. Therefore, attention should be paid to persistent cough, and, in some cases, active investigations for underlying etiology may be necessary.
While the physiology of the respiratory systems may be similar across age groups, there are also distinct differences in airway, respiratory muscle and chest wall structure, lung mechanics, and respiratory control between children and adults [2, 3]. Therefore, it is not surprising that adult diagnostic and therapeutic approaches should not be applied to children.
However, it is often difficult to diagnose and treat children with chronic cough due to lack of solid data and parents’ concerns. Therefore, to determine whether to initiate additional investigations or empirical treatments accordingly, a systematic approach to find out clues suggesting underlying disease is necessary, in consideration of the patient’s age and medical resources.
Definition of Chronic Cough in Children
There is no consensus on the duration of cough which defines chronic cough in children, whereas cough lasting ≥8 weeks is commonly used to define chronic cough in adults. However, chronic cough in children aged ≤14 years is usually defined as a cough lasting ≥4 weeks based upon expert consensus [4]. The rationale behind the decision is that most acute URTIs in children resolve within this time frame [5, 6].
Meanwhile, British Thoracic Society (BTS) guideline suggests the same definition as adults based on the observation that acute cough due to URTIs could last more than 3 weeks in about 10% of children and could last up to several months in some children who showed repeated cough receptor hypersensitivity after respiratory viral infection [7]. However, the guideline still encourages careful individualized management, including warnings that investigation before 8 weeks is warranted if the child shows any signs of chronic lung disease or when the cough becomes worse. Indeed, 17.6% of children with chronic cough had a serious underlying disease (bronchiectasis, aspiration, or cystic fibrosis) in a multicenter study using a standardized cough management pathway [8]. Therefore, most guidelines including the American College Chest Physicians (ACCP) guideline define chronic cough in children as a cough lasting ≥4 weeks [9,10,11,12]. Although this approach may potentially lead to unnecessary investigations, it calls for earlier attention on child with prolonged cough to prevent possible damage caused by delayed diagnosis and treatment. However, these guidelines also recommend “watchful waiting” for patients without any specific symptom and/or sign suggesting underlying diseases.
It still remains unclear what age should be used to stratify into child and adult in applying the definition of and approach for chronic cough. Although there are many differences in underlying etiologies, outcome measures, and feasible investigatory tests between children and adults, none of the guidelines provide a robust evidence regarding the cutoff age of such stratification. However, it is reasonable to use adult guidelines for adolescents 15 years and older since the causes of chronic cough in this age group are fairly similar to those in adults [3, 13, 14].
Common Causes of Chronic Cough in Children
Although asthma, upper airway cough syndrome (UACS), and gastroesophageal reflux disease (GERD) are known to be major cough-triggering conditions in adults with chronic cough [15], common causes in children are reportedly variable, due to the heterogeneity in study design, chronic cough definition, age range of study populations, practice settings, or cough epidemiology across regions. Although there are few prospective studies based on a standardized management protocol, recent multicenter studies suggested that the most common causes of chronic cough in children are asthma, protracted bacterial bronchitis (PBB), UACS, and nonspecific cough (that resolves spontaneously or is likely post-infectious cough) [8, 16].
Asthma
Variable airflow obstruction in asthma leads to typical symptoms such as wheezing, dyspnea, and cough. Asthma is rarely a cause of “isolated” cough in children; therefore, the evaluation for chronic cough in children should include careful medical history about other suggestive findings of asthma, and, if possible, spirometry and assessment of response to bronchodilators and bronchial challenge test [17, 18].
However, typical symptoms of asthma may not be present initially, and cough can be the sole symptom, called as “cough variant asthma (CVA)” [19]. CVA may present as a nonspecific chronic cough in children. Thus, the possibility of asthma should be considered even in a child with chronic cough presenting no other apparent asthma symptoms. The cough associated with asthma is typically dry, but a wet cough alone cannot exclude asthma since other diseases or infections may coexist.
Protracted Bacterial Bronchitis
PBB is one of the most common causes of chronic wet cough, especially in preschool children [20, 21]. It accounted for approximately 40% of children under 18 years referred with chronic cough in a prospective multicenter study [8]. PBB may therefore be more common than previously thought [8, 20]. Although much skepticism regarding the existence of PBB has been raised, this disorder is now widely accepted and incorporated into most cough guidelines [22,23,24]. However, PBB has remained largely unrecognized and is often misdiagnosed as asthma.
Although the original diagnostic criteria for PBB included positive bronchoalveolar lavage (BAL) fluid cultures for respiratory bacterial pathogens, it was changed to more pragmatic one since performing BAL using a bronchoscopy on every child with a chronic wet cough is impractical. Now, PBB is usually diagnosed by a chronic wet cough (>4 weeks) without any symptoms or signs of an alternative cause and responds to 2–4 week course of appropriate antibiotics [10, 25]. Chest radiographs are often normal or reveal only minor abnormalities such as peribronchial wall thickening. Pulmonary function tests are also usually normal. PPB is frequently associated with airway malacia [25]. H. influenzae, S. pneumoniae, and M. catarrhalis are the most common pathogens isolated in the BAL fluid culture from children with PBB. Most widely used first-line empiric antibiotic is oral amoxicillin-clavulanate, which is active against beta-lactamase-producing strains based on a randomized controlled study [26, 27].
Timely diagnosis has been emphasized due to the potential risk that PBB may progress to chronic suppurative lung disease or bronchiectasis. However, each case should be carefully assessed to exclude alternative causes of chronic cough since the proposed diagnostic criteria of PBB may lead to overdiagnosis and unnecessary prescription of antibiotics.
The optimal duration of treatment of PBB is still unknown. The ACCP and European Respiratory Society (ERS) guidelines recommend 2-week course of antibiotics followed by 2 weeks if cough does not resolve, while the BTS guidelines recommend an initial course of 4–6 weeks [7, 9, 10]. If the wet cough has not improved substantially by this time, other causes should be considered. Chest CT scan is needed in the case of chronic productive or wet cough unresponsive to 4 weeks of antibiotics, recurrent (>3 times per year) PBB, and other key symptoms of bronchiectasis (e.g., hemoptysis, persistent pneumonia, or chest pain) [22].
Nonspecific Cough That Resolves Without Specific Treatment (or Post-infectious Cough)
Post-infectious cough is mostly self-limiting and usually resolves with time. Although the specific pathogen causing the post-infectious cough in most cases remains unidentified, respiratory viruses (particularly respiratory syncytial virus, influenza, parainfluenza, and adenovirus), Mycoplasma pneumoniae, Chlamydia pneumoniae, and Bordetella pertussis may be the pathogens that may potentially lead to chronic cough [28,29,30,31]. Although the pathogenesis of the post-infectious cough is not fully understood, prolonged and excessive stimulation from extensive disruption of epithelial integrity and exposure of sensory nerve endings in the airway lining are considered to contribute to the development of post-infectious cough [31]. Cough receptors and peripheral and central neural circuits are also involved in post-infectious cough [32, 33].
Respiratory viruses are supposed to be the most common pathogens related with post-infectious cough and can be managed with reassurance. Substantial number of children with chronic cough had a serologic evidence of recent pertussis infection despite full immunization, but the classic features of pertussis infection (repetitive paroxysmal coughing episodes, inspiratory whoop, and posttussive vomiting) may not be seen in infants and older children [34]. Thus, post-pertussis cough should be considered in children with chronic cough regardless of immunization status. M. pneumoniae is also a common cause of post-infectious cough, and although C. pneumoniae is less common than M. pneumoniae, symptoms may be more severe. Post-infectious cough is often difficult to distinguish from PBB, and this may complicate therapeutic decisions.
Upper Airway Cough Syndrome
UACS, formerly termed as posterior nasal drip (PND) syndrome, includes a variety of disorders such as allergic rhinitis, non-allergic rhinitis, rhinosinusitis, and adenoiditis if associated with cough. The diagnosis of UACS in children is often made clinically based on symptoms, physical examination, and a response to therapy with antihistamines. The reported proportion of UACS varies widely (3–38%) in children with chronic cough depending on diagnostic algorithms [13, 20, 35]. It also seems to be age-dependent. A low proportion was reported when the age of study population was young and ENT examination and allergy tests were not included in the diagnostic workup. However, whether PND is the cause of chronic cough in children is controversial and the pathophysiologic mechanism is still debated [36, 37].
Gastroesophageal Reflux Disease
Although it remains controversial whether GERD is common cause of chronic cough in children, chronic cough may be a presentation of GERD. There is also evidence suggesting a role for non-acid reflux in triggering chronic cough [38,39,40,41]. However, GERD is not commonly identified as the cause of “isolated” chronic cough in children (i.e., absence of gastrointestinal GERD symptoms) [9]. Thus, only for children with chronic cough who have gastrointestinal GERD symptoms, it is recommended investigations and treatment for GERD following pediatric GERD guidelines.
Tic Cough (Habit Cough) and Somatic Cough Disorder (Psychogenic Cough)
Tic cough describes a dry repetitive “tic-like” cough. It is usually not very disruptive and has habitual features similar to a vocal tic [42]. Meanwhile, somatic cough disorder shows bizarre honking cough. It is very disruptive to daily life and brings some secondary gain to the child. These coughs become worse in front of the caregivers or medical staffs and often disappear during sleep or engrossment. The coughs are very loud, but the patients themselves are often indifferent (la belle indifference). Although typical clinical characteristics are usually evident, a diagnosis can be made after other possible causes have been excluded. Non-pharmacological trials of hypnosis or suggestion therapy or combinations of reassurance, counseling, or referral to a psychiatrist are suggested in tic cough and somatic cough disorder in children [42, 43].
Other Causes of Chronic Cough in Children
Possible other causes of chronic cough in children are listed in Table 9.1. As the causes of chronic cough in children are so diverse across pulmonary and extrapulmonary diseases, this list outlines only some of the relatively common encounters. The child’s age can help narrow the list of possible causes. Asthma, UACS, and GERD, reported as the most common causes of chronic cough in adults and adolescents, are not much common in preschool children. Instead, PBB, post-infectious cough, and bronchiectasis may account for most of the causes in this age group [20]. Therefore, the sequence of evaluation is guided by the age and accompanying symptoms/signs of each child.
Clinical Approach (Fig. 9.1)
Chronic cough in children may be representative of a simple, self-limiting cough or a serious underlying disease. In this regard, chronic cough has been classified into specific and nonspecific cough. Specific cough refers to a chronic cough that suggests a specific underlying disease and needs further investigations to confirm a diagnosis. Whereas, nonspecific cough refers to a chronic cough that does not suggest identifiable cause after a reasonable evaluation. To distinguish these two types of cough, it is crucial to find out clues that suggest underlying diseases through focused history, physical examination, and tests that can be easily performed in an outpatient setting (chest radiography or pulmonary function tests). However, specific cough may not be easily distinguished from nonspecific cough after initial evaluation. Thus, children with a nonspecific chronic cough should be reevaluated until cough is spontaneously resolved or a specific cause is identified.
When managing children with chronic cough, most guidelines recommend a similar systematic approach, which was shown to significantly improve clinical outcomes in a multicenter randomized trial [4]. Remaining uncertainties about this approach are whether the management algorithm should depend on the duration or severity of chronic cough and the cutoff age for child-specific guideline to be applied.
Clinical History and Physical Examination
Many children experience recurrent acute cough which parents will not readily distinguish from chronic cough. So, first of all, it is necessary to confirm whether the patient’s cough is truly chronic. Then, the history and physical examination focuses on identifying symptoms or signs suggestive of a specific cause of cough (specific cough pointers; Table 9.1).
Age and circumstance at onset of cough can help identify the cause. Neonatal onset, especially within a few days or weeks of birth, can be associated with congenital malformations of airway such as tracheobronchomalacia or tracheoesophageal fistula, so an immediate diagnostic process should be followed to reveal the underlying disease. In toddlers, sudden onset or onset after choking episode while playing or eating should raise suspicion of a foreign body aspiration. Sometimes, the characteristics of cough may be easily recognizable in the clinical history, which can provide diagnostic clues to underlying etiology. This is diagnostically less useful in adults [44]. Severe paroxysmal cough accompanied by vomiting or inspiratory “whoop” suggests an infection with pertussis or parapertussis. Chronic paroxysmal cough triggered by exercise and/or cold air is often seen in patients with asthma. Barking or loud brassy cough suggests lesions of proximal airway such as airway malacia or foreign body inhalation. Staccato cough in young infants suggests chlamydia infection, and honking cough that disappears during sleep or engrossment in something suggests a tic cough (habit cough) or somatic cough disorder (psychogenic cough). A chronic productive cough (wet cough) suggests suppurative process such as infection, bronchiectasis, cystic fibrosis, or immune deficiency, whereas dry cough suggests airway irritation, inflammation, or a non-airway cause of the cough.
Past medical history including perinatal period and family history relevant to chronic cough should be taken. History about cough-triggering factors can also provide helpful information. Environmental exposure to allergens (e.g., pollen, pets, dust) or irritants (e.g., active or passive smoking, environmental pollutants) that may cause cough should be evaluated.
Medications also should be reviewed carefully. Any current medications that can induce cough (e.g., angiotensin-converting enzyme (ACE) inhibitors) and a response to prior therapy may yield diagnostic clues.
All children with chronic cough need close physical examination, including overall health, growth, development, and nutritional state. As with medical history, physical examination should focus on identifying any signs suggesting underlying etiologies. If possible, listening to the patient’s spontaneous cough can help to identify the characteristics of cough. Since other organs besides the lungs can be an origin of chronic cough, it is necessary to have a full physical examination, including an otorhinolaryngological examination as well as a chest examination.
Initial Diagnostic Tests
Chest Radiography
Although a definitive diagnosis is rarely made on the radiographic findings alone, chest radiography should be obtained as a part of initial workup. It can provide important information about the overall condition of the lungs and the need for additional diagnostic tests. However, a normal chest radiograph cannot exclude the possibility of underlying pulmonary diseases as a cause of cough, including bronchiectasis, airway abnormality, and interstitial lung disease. Therefore, additional imaging studies such as chest CT scan may be necessary if certain pulmonary diseases are suspected in medical history and physical examination.
Pulmonary Function Tests
Spirometry provides an important overview for lung volume and airway caliber, so, if available, it is recommended in children over 5–6 years who can cooperate. An obstructive pattern in the spirometry indicates obstructive lung diseases such as asthma and emphysema, while a restrictive pattern reflects restrictive lung diseases such as interstitial lung disease, pulmonary fibrosis, and neuromuscular disease. Bronchodilator responsiveness or bronchial challenge tests (direct or indirect) can help to diagnose asthma. However, a normal spirometry does not fully exclude these conditions.
Classification into Specific and Nonspecific Cough
After the patient’s chronic cough has been classified into a specific and a nonspecific cough with an initial evaluation, the specific cough should be further investigated to diagnose the suspected specific disease and then managed with etiology-based treatment. In the case of nonspecific cough, reassurance and “watchful waiting” can be a reasonable option because it usually resolves over time without any specific treatment. However, some patients with specific or nonspecific cough may require an empirical treatment for diagnostic purpose. Parental expectations and concerns should be considered when determining whether to initiate empirical treatments.
Empirical Treatments in Children with Chronic Isolated Cough (Cough Without Any Other Specific Cough Pointer)
When empirical treatments are trialed, the placebo or “period effects” should be considered since the spontaneous resolution of cough over time is common [45]. To avoid lasting unnecessary treatments, reassessment of the patients is emphasized in 2–4 weeks that is usual time to response for most medications [9].
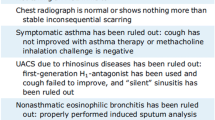
Chronic Isolated Dry Cough
Because of an imprecise definition of asthma and lack of available tests to confirm the diagnosis in young children, asthma cannot be easily excluded in young children whose cough is the only symptom. Thus, when the cough is dry and objective testing cannot be undertaken, empirical treatment with inhaled corticosteroids (ICS) under provisional diagnosis of asthma may be considered. However, before starting ICS therapy, a period of the empirical treatment (e.g., 2–4 weeks) and objective end points should be pre-determined. The use of high-dose ICS in this situation must be balanced against well-known potential adverse events including growth deceleration, adrenal suppression, and pulmonary infection. Asthma medication should not be continued unless the diagnosis of asthma can be made with confidence. In children who responded to ICS, an early relapse of cough after the cessation of ICS may be a clue for the diagnosis of asthma.
Chronic Isolated Wet Cough
Chronic wet cough is a specific cough pointer that needs further investigations to find out an underlying etiology. However, empirical antibiotics for 2–4 weeks can be trialed in isolated wet cough under a provisional diagnosis of PBB. Although treatment with amoxicillin-clavulanate is usually effective, antibiotic selection should be based upon regional sensitivity patterns. If chronic wet cough fails to respond to antibiotics, then further investigations (see additional tests below) are required to rule out other suppurative lung diseases.
Empirical treatments targeting GERD or UACS are not usually recommended in children with chronic isolated cough, unless they have specific symptoms or signs for the diagnosis. These two disorders are not common cause of isolated cough, and there is no convincing evidence supporting that these empirical treatments are effective in children with chronic isolated cough.
Additional Diagnostic Tests
Additional investigations depend on the provisional diagnosis after initial evaluation and the clinical course of cough with or whiteout treatments.
Chest CT Scan
Chest CT scan is useful for the diagnosis of pulmonary parenchymal or central airway disease. High-resolution computed tomography is considered as a standard diagnostic method for structural changes in the small airways because it is more sensitive than pulmonary function tests. However, chest CT scan should be selectively performed only for patients with other accompanying symptoms/signs suggestive of underlying pulmonary diseases in consideration of the risk associated with radiation.
Bronchoscopy
Sometimes, chronic cough itself can be an indication for bronchoscopy in children [46]. However, considering that bronchoscopy is an invasive test and medical conditions requiring bronchoscopy are relatively rare, it is desirable to first perform noninvasive tests for common diseases. In children with chronic cough, indications for bronchoscopy are (1) a suspicion of tumor or structural abnormality in the central airway, (2) suspected retained foreign body inhalation, (3) suspected bronchial tuberculosis, (4) localized changes on chest radiography, and (5) bronchoalveolar lavage for bacteriological examination.
Sputum Testing
In most children with chronic wet/productive cough, it is difficult to obtain the sputum necessary for the examination, but if possible, culture with susceptibility testing and viral PCR should be performed.
Allergy Testing
Allergy testing is usually not recommended in the assessment of every child with chronic cough. However, a skin prick test or serum-specific IgE test can help to diagnose asthma or allergic rhinitis in children with a family or personal history of allergies or with any symptoms or signs for respiratory allergic diseases.
Esophageal pH or Multichannel Intraluminal Impedance Monitoring
In selected children who have GERD symptoms (e.g., acid regurgitation, heartburn) with chronic cough, esophageal monitoring may be undertaken to determine if the cough episodes are associated with reflux events.
Fractional Exhaled Nitric Oxide
Fractional exhaled nitric oxide (FeNO) is a quantitative, noninvasive, and simple method for measuring airway inflammation that provides a complementary tool for diagnosing and monitoring asthma. FeNO levels have been shown to well reflect the degree of airway eosinophilic inflammation and to predict corticosteroid responsiveness in patients with respiratory symptoms [47, 48]. Thus, FeNO measurement may be particularly useful for younger patients and adults who find it difficult to perform the bronchial challenge test [49].
However, it should be noted that FeNO levels alone do not directly indicate a diagnosis of a specific disease. Many factors such as ethnicity, age, height, dietary intake, atopy, and tobacco smoke exposure can influence FeNO levels [50, 51]. Although ATS recommended FeNO levels >35 ppb in children aged ≤12 years and >50 ppb in children aged >12 years as cutoff to define presence of clinically important eosinophilic inflammation, there are still substantial discrepancies in the optimal cutoff value for defining abnormality among studies [52].
Treatment of Chronic Cough in Children
Making the correct diagnosis and then managing the underlying etiology is the key to treatment of chronic cough in children. There is little evidence supporting the benefit of treatments without a clear diagnosis. It is also important to ensure that children with chronic cough are not exposed to tobacco smoking and other pollutants.
Nonspecific cough can be managed with reassurance, watchful waiting, and reevaluation. If an empirical treatment is trialed, a regular re-assessment for the treatment response and diagnosis is recommended with a predefined time frame. Further investigations with specialist referral are warranted if cough has not resolved with therapeutic trials or specific cough pointers have emerged. Specific cough should be managed with etiology-based treatment except empirical antibiotics in chronic isolated wet cough under provisional diagnosis of PBB. Management of each specific etiology is beyond the scope of this chapter and should follow the specific guidelines for each disease.
Summary
Chronic cough in children is usually defined as a cough lasting ≥4 weeks. Although the most common causes of chronic cough in children are reportedly variable, asthma, PBB, UACS, and nonspecific cough are suggested as common causes. When managing children with chronic cough, most guidelines recommend a similar systematic approach, which was shown to significantly improve clinical outcomes. In this regard, chronic cough has been classified into specific and nonspecific cough. To distinguish these two types of cough, it is crucial to find out clues that suggest underlying diseases through focused history, physical examination, and tests that can be easily performed in an outpatient setting. Additional investigations depend on the provisional diagnosis after initial evaluation and the clinical course of cough. Nonspecific cough can be managed with reassurance, watchful waiting, and reevaluation, whereas specific cough should be managed with etiology-based treatment. If empirical treatments are trialed due to parental concerns and/or diagnostic purpose under provisional diagnosis of asthma (isolated dry cough) or PBB (isolated wet cough), a reassessment is recommended in predefined time frame (e.g., 2–4 weeks). If the cough has not improved substantially by this time, other causes should be considered.
References
Irwin RS. Introduction to the diagnosis and management of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 Suppl):25S–7S.
Chang AB. Cough: are children really different to adults? Cough. 2005;1:7.
Kantar A, Seminara M. Why chronic cough in children is different. Pulm Pharmacol Ther. 2019;56:51–5.
Chang AB, Oppenheimer JJ, Weinberger M, Weir K, Rubin BK, Irwin RS. Use of management pathways or algorithms in children with chronic cough: systematic reviews. Chest. 2016;149(1):106–19.
Hay AD, Wilson AD. The natural history of acute cough in children aged 0 to 4 years in primary care: a systematic review. Br J Gen Pract. 2002;52(478):401–9.
Hay AD, Wilson A, Fahey T, Peters TJ. The duration of acute cough in pre-school children presenting to primary care: a prospective cohort study. Fam Pract. 2003;20(6):696–705.
Shields MD, Bush A, Everard ML, McKenzie S, Primhak R, British Thoracic Society Cough Guideline G. BTS guidelines: recommendations for the assessment and management of cough in children. Thorax. 2008;63 Suppl 3:iii1–iii15.
Chang AB, Robertson CF, Van Asperen PP, Glasgow NJ, Mellis CM, Masters IB, et al. A multicenter study on chronic cough in children: burden and etiologies based on a standardized management pathway. Chest. 2012;142(4):943–50.
Chang AB, Oppenheimer JJ, Irwin RS, Panel CEC. Managing chronic cough as a symptom in children and management algorithms: CHEST Guideline and Expert Panel Report. Chest. 2020;
Morice AH, Millqvist E, Bieksiene K, Birring SS, Dicpinigaitis P, Domingo Ribas C, et al. ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur Respir J. 2020;55(1)
Gibson PG, Chang AB, Glasgow NJ, Holmes PW, Katelaris P, Kemp AS, et al. CICADA: Cough in Children and Adults: Diagnosis and Assessment. Australian cough guidelines summary statement. Med J Aust. 2010;192(5):265–71.
Song DJ, Song WJ, Kwon JW, Kim GW, Kim MA, Kim MY, et al. KAAACI evidence-based clinical practice guidelines for chronic cough in adults and children in Korea. Allergy Asthma Immunol Res. 2018;10(6):591–613.
Asilsoy S, Bayram E, Agin H, Apa H, Can D, Gulle S, et al. Evaluation of chronic cough in children. Chest. 2008;134(6):1122–8.
Khoshoo V, Edell D, Mohnot S, Haydel R Jr, Saturno E, Kobernick A. Associated factors in children with chronic cough. Chest. 2009;136(3):811–5.
Irwin RS, Corrao WM, Pratter MR. Chronic persistent cough in the adult: the spectrum and frequency of causes and successful outcome of specific therapy. Am Rev Respir Dis. 1981;123(4 Pt 1):413–7.
O’Grady KF, Grimwood K, Torzillo PJ, Rablin S, Lovie-Toon Y, Kaus M, et al. Effectiveness of a chronic cough management algorithm at the transitional stage from acute to chronic cough in children: a multicenter, nested, single-blind, randomised controlled trial. Lancet Child Adolesc Health. 2019;3(12):889–98.
Chang AB, Asher MI. A review of cough in children. J Asthma. 2001;38(4):299–309.
James DR, Lyttle MD. British guideline on the management of asthma: SIGN Clinical Guideline 141, 2014. Arch Dis Child Educ Pract Ed. 2016;101(6):319–22.
Hannaway PJ, Hopper GD. Cough variant asthma in children. JAMA. 1982;247(2):206–8.
Marchant JM, Masters IB, Taylor SM, Cox NC, Seymour GJ, Chang AB. Evaluation and outcome of young children with chronic cough. Chest. 2006;129(5):1132–41.
Donnelly D, Critchlow A, Everard ML. Outcomes in children treated for persistent bacterial bronchitis. Thorax. 2007;62(1):80–4.
Chang AB, Bush A, Grimwood K. Bronchiectasis in children: diagnosis and treatment. Lancet. 2018;392(10150):866–79.
Verhagen LM, de Groot R. Recurrent, protracted and persistent lower respiratory tract infection: A neglected clinical entity. J Infect. 2015;71(Suppl 1):S106–11.
Das S, Sockrider M. Protracted bacterial bronchitis (PBB) in children. Am J Respir Crit Care Med. 2018;198(6):P11–P2.
Chang AB, Upham JW, Masters IB, Redding GR, Gibson PG, Marchant JM, et al. Protracted bacterial bronchitis: the last decade and the road ahead. Pediatr Pulmonol. 2016;51(3):225–42.
Marchant J, Masters IB, Champion A, Petsky H, Chang AB. Randomised controlled trial of amoxycillin clavulanate in children with chronic wet cough. Thorax. 2012;67(8):689–93.
Marchant JM, Petsky HL, Morris PS, Chang AB. Antibiotics for prolonged wet cough in children. Cochrane Database Syst Rev. 2018;7:CD004822.
Hallander HO, Gnarpe J, Gnarpe H, Olin P. Bordetella pertussis, Bordetella parapertussis, Mycoplasma pneumoniae, Chlamydia pneumoniae and persistent cough in children. Scand J Infect Dis. 1999;31(3):281–6.
Kamei RK. Chronic cough in children. Pediatr Clin North Am. 1991;38(3):593–605.
Wirsing von Konig CH, Rott H, Bogaerts H, Schmitt HJ. A serologic study of organisms possibly associated with pertussis-like coughing. Pediatr Infect Dis J. 1998;17(7):645–9.
Braman SS. Postinfectious cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 Suppl):138S–46S.
Atkinson SK, Sadofsky LR, Morice AH. How does rhinovirus cause the common cold cough? BMJ Open Respir Res. 2016;3(1):e000118.
Omar S, Clarke R, Abdullah H, Brady C, Corry J, Winter H, et al. Respiratory virus infection up-regulates TRPV1, TRPA1 and ASICS3 receptors on airway cells. PLoS One. 2017;12(2):e0171681.
Harnden A, Grant C, Harrison T, Perera R, Brueggemann AB, Mayon-White R, et al. Whooping cough in school age children with persistent cough: prospective cohort study in primary care. BMJ. 2006;333(7560):174–7.
Usta Guc B, Asilsoy S, Durmaz C. The assessment and management of chronic cough in children according to the British Thoracic Society guidelines: descriptive, prospective, clinical trial. Clin Respir J. 2014;8(3):330–7.
Kemp A. Does post-nasal drip cause cough in childhood? Paediatr Respir Rev. 2006;7(1):31–5.
O’Hara J, Jones NS. “Post-nasal drip syndrome”: most patients with purulent nasal secretions do not complain of chronic cough. Rhinology. 2006;44(4):270–3.
Borrelli O, Marabotto C, Mancini V, Aloi M, Macri F, Falconieri P, et al. Role of gastroesophageal reflux in children with unexplained chronic cough. J Pediatr Gastroenterol Nutr. 2011;53(3):287–92.
Blondeau K, Mertens V, Dupont L, Pauwels A, Farre R, Malfroot A, et al. The relationship between gastroesophageal reflux and cough in children with chronic unexplained cough using combined impedance-pH-manometry recordings. Pediatr Pulmonol. 2011;46(3):286–94.
Ghezzi M, Guida E, Ullmann N, Sacco O, Mattioli G, Jasonni V, et al. Weakly acidic gastroesophageal refluxes are frequently triggers in young children with chronic cough. Pediatr Pulmonol. 2013;48(3):295–302.
Rosen R, Amirault J, Johnston N, Haver K, Khatwa U, Rubinstein E, et al. The utility of endoscopy and multichannel intraluminal impedance testing in children with cough and wheezing. Pediatr Pulmonol. 2014;49(11):1090–6.
Vertigan AE, Murad MH, Pringsheim T, Feinstein A, Chang AB, Newcombe PA, et al. Somatic cough syndrome (previously referred to as psychogenic cough) and tic cough (previously referred to as habit cough) in adults and children: CHEST Guideline and Expert Panel Report. Chest. 2015;148(1):24–31.
Haydour Q, Alahdab F, Farah M, Barrionuevo P, Vertigan AE, Newcombe PA, et al. Management and diagnosis of psychogenic cough, habit cough, and tic cough: a systematic review. Chest. 2014;146(2):355–72.
Mello CJ, Irwin RS, Curley FJ. Predictive values of the character, timing, and complications of chronic cough in diagnosing its cause. Arch Intern Med. 1996;156(9):997–1003.
Chang AB. Therapy for cough: where does it fall short? Expert Rev Respir Med. 2011;5(4):503–13.
Snijders D, Cattarozzi A, Panizzolo C, Zanardo V, Guariso G, Calabrese F, et al. Investigation of children with chronic nonspecific cough: any clinical benefit of bronchoscopy and bronchoalveolar lavage? Allergy Asthma Proc. 2007;28(4):462–7.
Song WJ, Kwon JW, Kim EJ, Lee SM, Kim SH, Lee SY, et al. Clinical application of exhaled nitric oxide measurements in a korean population. Allergy Asthma Immunol Res. 2015;7(1):3–13.
Lamon T, Didier A, Brouquieres D, Escamilla R, Dupuis M, Guibert N, et al. Exhaled nitric oxide in chronic cough: a good tool in a multi-step approach. Respir Med Res. 2019;76:4–9.
Song WJ, Kim HJ, Shim JS, Won HK, Kang SY, Sohn KH, et al. Diagnostic accuracy of fractional exhaled nitric oxide measurement in predicting cough-variant asthma and eosinophilic bronchitis in adults with chronic cough: a systematic review and meta-analysis. J Allergy Clin Immunol. 2017;140(3):701–9.
Buchvald F, Baraldi E, Carraro S, Gaston B, De Jongste J, Pijnenburg MW, et al. Measurements of exhaled nitric oxide in healthy subjects age 4 to 17 years. J Allergy Clin Immunol. 2005;115(6):1130–6.
Blake TL, Chang AB, Chatfield MD, Petsky HL, Rodwell LT, Brown MG, et al. Does ethnicity influence fractional exhaled nitric oxide in healthy individuals?: A systematic review. Chest. 2017;152(1):40–50.
Dweik RA, Boggs PB, Erzurum SC, Irvin CG, Leigh MW, Lundberg JO, et al. An official ATS clinical practice guideline: interpretation of exhaled nitric oxide levels (FENO) for clinical applications. Am J Respir Crit Care Med. 2011;184(5):602–15.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Song, D. (2021). Chronic Cough in Children. In: Cho, S.H., Song, WJ. (eds) Diagnosis and Treatment of Chronic Cough. Springer, Singapore. https://doi.org/10.1007/978-981-33-4029-9_9
Download citation
DOI: https://doi.org/10.1007/978-981-33-4029-9_9
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-33-4028-2
Online ISBN: 978-981-33-4029-9
eBook Packages: MedicineMedicine (R0)