Abstract
As sequencing technology and information of the genomic causes for cancer development expand, multi-gene panel testing for hereditary cancer is increasing in clinical practice. In this chapter, we reviewed the application of multi-gene panel with pre-/post- testing considerations and summarized genetic counseling based on panel testing results in clinical field. In addition, we introduce multi-gene panel for hereditary cancer developed in Seoul National University Hospital.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Hereditary/familial breast cancer
- Breast cancer susceptibility
- Multigene panel testing
- Next-generation sequencing
- High penetrance gene
- Genetic counseling
- BRCA1/2 gene mutation
As sequencing technology advances and next-generation sequencing increases with cost effectiveness, the application of assaying large panels of genes, called “multigene panel” or “panel testing”, for hereditary cancer risk assessment is becoming commonplace in clinical practice. Gene panel testing simultaneously analyzes a set of genes associated with a specific family cancer phenotype or syndrome of cancer. Gene panel included low to moderate penetrance genes like as PALB2, ATM, CHEK2, NBN, NF1, RAD50, and so on as well as high penetrance mutations in BRCA1/2, TP53, PTEN, STK11, and CDH1, even though the clinical meaning of these genes is not yet completely defined. (Fig. 24.1).
Genetic architecture of relative cancer risk and allele frequency. This figure depicts finding of rare, high-penetrance variants, such as pathogenic mutations in BRCA1/BRCA2 genes associated with hereditary breast and ovarian cancer, moderate-penetrance variants, and low-penetrance alleles identified in genome-wide association studies
In the early stage of the widespread use with NGS-based multigene panel, Stephen E. Lincoln et al. [1] estimated reliability of the multigene panel testing. They compared between traditional (previously received clinical testing in several genes including BRCA 1/2) and NGS-based multigene panel testing with 29-gene for hereditary breast and ovarian cancer genes in more than 1000 patients. They showed that NGS can achieve high-analytic sensitivity and specificity in comparison with traditional genetic testing methods, even for some technically challenging (e.g., CNVs and large indels) classes of genetic variation that make up a significant fraction of the pathogenic variants in HBOC. Interpretation concordance for BRCA1 and BRCA2 was also high, demonstrating that broadly available resources combined with recent guidelines can produce results similar to those of an established laboratory using a large proprietary database. Furthermore, half (372 of 750) of the variants were in genes other than BRCA1 or BRCA2, and most (607 of 750) of these variants were reported by the previous tests, providing the most unbiased view of sensitivity for the NGS panel (607 of 607 Z 100%; 95% CI, 100% e99.59%). Thus, they concluded gene panels can be a viable replacement for traditional tests in appropriate circumstances. The additional pathogenic variants uncovered by panel testing appeared clinically relevant, albeit with the caveat of identifying many additional VUSs. Another group of research, Nimmi S. Kapoor et al. [2], presented similar result about validation of multigene panel. Multigene panel testing comparing traditional test detected pathogenic BRCA1/2 mutations at equivalent rates (4.0 vs. 3.6%, p = 0.86) with increasing proportion of the VUS. An additional 3.9% (n = 13) in nonBRCA pathogenic mutations and 13.4% (n = 45) had nonBRCA VUSs identified in patients who underwent panel testing. The most common nonBRCA mutations were in PALB2, CHEK2, and ATM gene. They recommended multigene panel testing for the patients at risk for hereditary breast cancer as a safe, more beneficial, and efficient modality.
Recently, many researchers from various countries have released large-scale result about hereditary cancer risk and multigene panel testing. Fergus J. Couch et al. [3] evaluated the associations between nonBRCA1/2 predisposition genes and breast cancer in over than 65,000 patients. They showed there are a total of 10.2% frequency of pathogenic variants in 21 panel genes including BRCA1, BRCA2, syndromic breast cancer genes (CDH1, PTEN, and TP53), and high or moderate penetrance genes (ATM, BARD1, CHEK2, PALB2, and RAD51D) and 6.2% frequency of women with breast cancer after exclusion of BRCA1 and BRCA2. This study established several panel genes as high- and moderate-risk breast cancer; most commonly mutated nonBRCA1/2 genes among white women with breast cancer were CHEK2 (1.73%), ATM (1.06%), and PALB2 (0.87%) and provided estimates of breast cancer risk associated with pathogenic variants in these genes with relative risk from high (OR 7.46 in PALB2) to moderate (OR 3.07, 2.78, and 2.16 in RAD 51D, ATM, and CHEK2, respectively). In another study conducted by Saundra S. Buys et al. [4], the authors analyzed about 35,000 women with 25-gene panel testing and stratified to high risk for hereditary cancer who met NCCN guideline for HBOC testing regarding age at diagnosis and family history of ovary/pancreas cancer or not. Among the women who met NCCN testing criteria, 9.6% (316 of 32,993) had a deleterious mutation, compared with 5.9% (143 of 2416) of those who did not meet NCCN criteria. Nearly one-half of the pathogenic variants (PV) identified during testing were in the BRCA1 (24.0%) and BRCA2 (24.4%) genes. An additional 40.9% of the PVs were in other genes associated with breast cancer, including CHEK2 (11.7%), ATM (9.7%), and PALB2 (9.3%). Other genes on the panel accounted for 10.7% of mutations, including those associated with Lynch syndrome (7.0%).
As the application of multigene panel expands beyond breast cancer, the result on the outcomes of testing to identify inherited risks for colorectal, endometrial, gastric, pancreatic, prostate, and melanoma cancers as well as breast and ovary cancer was reported [5]. In this study, multigene hereditary cancer testing detected >1 pathogenic variants (PVs) in 6.7% of individuals and they showed up to 50% of all clinically significant findings would have been missed by single-syndrome testing.
Now, several companies offer panel tests composed of various cancer susceptibility genes, and it is commercially available to use in clinical practice with the purpose of personalized management for whom had a genetic predisposition to hereditary cancer. Clinicians or even individual oneself who wants the test can choose genetic test services among companies, list of genes, and number of gene-set range from single to dozens of genes. The companies provided the information online including available gene list-associated familial cancer type, clinical meaning of each gene, indications of the test based on individual’s risk, cautions of the test, and process to the genetic test for both the medical staff and patients/patients’ family members.
There are some issues in multigene panel testing: (1) lack of evidence for clinical application in several genes especially moderate-penetrant genes, which had limited data on the degree of cancer risk and failed to provide guidelines on risk management for carriers of pathogenic variants, (2) not all genes included on available multigene panel are clinically actionable, and (3) increased likelihood of finding variants of unknown significance (VUS). Many reports, previously mentioned, established the finding of a number of VUS with multigene panel testing in large cohort, and it ranged from about 10–70%. Thomas Paul Slavin et al. [6] reported only 6.2% of pathogenic variants in high-risk genes included in the panels (BRCA1, BRCA2, MSH6, PMS2, TP53, APC, and CDH1). Instead, they identified variants of uncertain significance (VUS) in 42%. They insisted that adequate pretest counseling is more important in anticipation of higher percentages of positive, unexpected, and ambiguous test results including VUSs. Test result ambiguity can be limited by the use of phenotype-specific panels. Furthermore, for pathogenic variants in low and moderate risk genes, the researchers said adequate risk modeling based on the patient’s personal and family history of cancer can be better than gene-specific risk. They stressed further research efforts will be needed to better classify variants and reduce clinical ambiguity of multigene panels.
Most important issue among these is clinical validity; the decision to test with multigene panel is focused on identifying a mutation known to be clinically actionable, that is, whether the management of an individual with a risk for hereditary cancer is altered based on the presence or absence of a mutation. Additionally, it needs to determine with discretion which group with a specific condition would get the crucial benefit from the application of multigene panel. LeifW. Ellisen et al. in Massachusetts General Hospital Cancer Center [7] designed interesting research to define the potential clinical effect of multigene panel testing for HBOC in a clinically representative cohort. They evaluated the likelihood of (1) a posttest management change and (2) an indication for additional familial testing, considering gene-specific consensus management guidelines, gene-associated cancer risks, and personal and family history. Among mutation-positive patients, about half (33 [52%] of 63) considered additional disease-specific screening and/or prevention measures beyond those based on personal and family history alone. Furthermore, additional familial testing would be considered for those with first-degree relatives (42 [72%] of 58; 95% CI, 59.8–82.2%) based on potential management changes for mutation-positive relatives. They concluded multigene testing is more likely to alter near-term cancer risk assessment and management recommendations for mutation-affected individuals.
Multigene testing may play a role in individuals with negative result in a single or just two genes but whose personal or familial history reveals suggestive of an inherited susceptibility or developed multiple phenotypes in a family. With all this in mind, the new NCCN committee suggested that multigene panel testing is offered in the context of professional genetic expertise with elaborate pre- and posttest counseling [8].
As the risk of cancer in carriers identified genetic mutations are stratified to several factors, the genetic expertise must evaluate the risk of inherited cancer based on individuals’ needs and concerns as well as cancer history of the detailed personal/family/relatives. Based on reliable risk assessment compounding history and genetic results, the expert should provide appropriate guidelines to the carrier with information of lifetime cancer risks, adequate screening test, and risk-reducing procedure. Though a major dilemma regarding multigene testing is that there are limited evidence and a lack of clear guidelines, several countries suggested similar guidelines for managing the care of individuals with predisposition to hereditary cancer (NCCN; United States, NICE; United Kingdom; GC-HBOC–; Germany, eviQ Cancer Treatments Online; Australia, and so on).
As a result, since identification of abnormality in BRCA1/2 genes has made contribution to the care of hereditary cancer patients and their families, further progress in our understanding of the genetic factors with cancer phenotype still continues. But the penetrance and phenotype of mutations are different among individuals, that is, there are not sufficient data about association between cancer development and detection of a pathogenic mutation. In addition, a negative result from genetic testing even in a large number of genes does not mean an individual has no risk of cancer. It is also another challenge to share information with the patients as well as the interpretation adequately of the result on germline mutations. Furthermore, gene testing can give rise to psychosocial consequences of all individuals and their families and may also have effect on social community. As the genetic test expands, the role of experts is more important; the integrated approach of clinicians and genetic counselors is indispensable. They should carefully access to better clarify counseling and management for the patient and family. The adequate prediction of the risk for hereditary cancer through enough risk assessment process and consideration of the patients’ need and concern with regarding the impact on patients and their families of the gene test result should be preceded in pretest counseling. In addition, in the analysis and transmission of the meaning of gene results, they should strive to provide comprehensive conclusions about the risk of cancer development considering the patient’s personal and family history and educate tailored risk-reducing guidelines.
1 Development and Application of Multigene Panel for Hereditary Cancer in SNUH
All of this section was currently published in Cancer Research Treatment (copyright by Korean Cancer Association) [9]. This is an Open-Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
1.1 Introduction
Though many commercial multiple-gene panels provide genetic information for hereditary cancer risk assessment, there is insufficient information on differences among ethnicities in cancer-susceptible germline mutations, and the assessment of germline mutations in all ethnic groups with clinical data is mandatory especially in Korea and Asia. We applied multiple-gene panel testing to 64 cancer-susceptibility genes to examine the frequency of mutations and to assess the clinical value of NGS-based multiple-gene panel testing in Korean breast cancer patients with clinical features of hereditary breast and ovarian cancer syndrome (HBOC). (Table 24.1).
1.2 Materials and Methods
The study population included 496 breast cancer patients with the following features of HBOC: (1) diagnosed with breast cancer and another primary cancer; (2) a family history that included at least two cases of breast cancer in first- or second-degree relatives; (3) bilateral breast cancer; or (4) breast cancer diagnosis before the age of 40 years. Of the patients, 349 patients were admitted to Seoul National University Hospital, Korea, and 147 patients were admitted to National Cancer Center, Korea, between 2002 and 2017. The medical records were reviewed and personal and family histories and pathologic data of cancer were recorded. Genomic DNA was extracted from the participants’ peripheral blood samples. Our panel included 64 hereditary cancer predisposing genes (ALK, APC, ATM, ATR, BAP1, BARD1, BLM, BMPR1A, BRCA1, BRCA2, BRIP1, CDH1, CDK4, CDKN2A, CHEK2, EPCAM, FAM175A, FANCA, FANCB, FANCC, FANCD2, FANCE, FANCF, FANCG, FANCI, FANCL, FH, FLCN, GSTP1, HOXB13, KRAS, LIG4, MEN1, MET, MLH1, MRE11A, MSH2, MSH6, MUTYH, NAT, NBN, NF1, PALB2, PALLD, PMS2, PRKAR1A, PRSS1, PTEN, RAD50, RAD51, RAD51C, RAD51D, RB1, RET, SDHB, SDHC, SDHD, SLX4, SMAD4, SPINK1, STK11, TP53, VHL, and XRCC2).
For mutation analysis, 64 gene-containing DNA fragments were enriched by solution-based hybridization capture followed by sequencing with an Illumina NextSeq platform (Illumina, San Diego, CA, USA) with the 150-bp paired end read module. The target region included all coding exons. Capture probes were generated by Celemics, Inc. (Seoul, Korea). The hybridization capture procedure was also performed according to the manufacturer’s standard protocol. Genomic DNA was sheared via sonication. Biotynilated RNA oligonucleotide probes were hybridized with sheared DNA. Captured fragments were removed from solution via streptavidin-coated magnetic beads and subsequently eluted. The enriched fragment library was then subjected to polymerase chain reaction (PCR) amplification using primers specific to the linked Illumina adaptors. Resulting libraries were quantified via Agilent 2200 TapeStation before proceeding to Illumina NextSeq platform. All samples were pooled into a single lane on a flow cell and sequenced together. Raw FASTQ files were filtered using Trimmomatic (Version 0.33) and aligned with the genome of reference (GRCh37/hg19) using Burrows-Wheeler Aligner (Version 0.7.10). PCR duplicates, overrepresented sequences, and low-quality reads were removed. Realignments of insertions and deletions were performed using GATK. Reads with mapping quality of 0 were filtered out. If a read was able to be mapped at two different places with an identical percentage, the mapping quality equaled zero. Otherwise, the read was mapped to the most identical region. Variant calling was performed using Samtools (Version 1.1) and Varscan (Version 2.4.0).
Variants were described according to the nomenclature recommendations of the Human Genome Variation Society (http://www.hgvs.org/mutnomen) and classified according to the following American College of Medical Genetics and Genomics recommendations: pathogenic (P), likely pathogenic (LP), variants of unknown significance (VUS), likely benign, and benign/polymorphism [7]. We used online databases, including the Human Gene Mutation Database, the Single Nucleotide Polymorphism Database, the 1000 Genome project, ClinVar, the Sorting Intolerant From Tolerant, Polymorphism Phenotyping-2, and the Korean Reference Genome Database, for in silico prediction of identified variants. Variants classified as P or LP were considered deleterious mutations.
1.3 Results
1.3.1 Study Population
The clinical characteristics of the patients are shown in Table 24.2. The median age at diagnosis of cancer was 48 years (range, 19–80 years). In these patients, 390 patients (78.6%) had stage I or II disease. More than half of the patients (N = 250, 50.4%) had another primary cancer, including ovarian cancer, stomach cancer, colon cancer, lung cancer, or other malignancy. In all, 169 patients (34.1%) reported that they had two or more first- or second-degree relatives with breast cancer. Fifty-seven patients (11.5%) had synchronous or metachronous bilateral breast cancer, and 84 patients (16.9%) were diagnosed with breast cancer at an age younger than 40 years. Sixty-four patients had two or more risk factors for HBOC (e.g., bilateral breast cancer and breast cancer diagnosis <40 years old).
1.3.2 Frequency of Deleterious Mutations
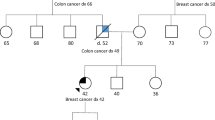
A total of 95 (19.2%) among all 496 patients were found to have deleterious germline mutations of cancer-susceptibility genes. The proportions of risk factors, including breast cancer with another primary cancer, family history of breast cancer, and bilateral breast cancer were also not different between the groups with or without deleterious mutations. However, the proportion of patients with deleterious mutations were higher in patients who were diagnosed with breast cancer at younger than 40 years old than patients with another risk factors (P = 0.022). Furthermore, having two or more risk factors for HBOC was also associated with a higher rate of deleterious mutations (P = 0.001). Table 24.3 and Fig. 24.2 summarize 48 deleterious mutations found in 95 patients.
Of these patients with deleterious mutations, 60 patients (63.2%) had BRCA1(31) and BRCA 2 (30) mutations. Patients _309 and _502 had 2 BRCA1 mutations, and patient HOPE_57 carried both BRCA1 and BRCA2 mutations. In addition, 38 patients (40.0%) had cancer-susceptibility gene mutations other than BRCA1/2: 35 patients (36.8%) had nonBRCA1/2 mutations and 3 patients had both a BRCA1/2 mutation and a nonBRCA1/2 mutation (Patient_14 had BRCA2 and SPINK1 mutations; Patient_33 had BRCA2, CDH1, and TP53 mutations; and patient_421 had BRCA1 and NBN mutations). Most of the deleterious mutations were found in CDH1 (N = 8, 8.4%), RAD51 (N = 7, 7.4%), SPINK1 (N = 6, 6.3%), TP53 (N = 5, 5.3%), and NBN (N = 3, 3.2%). The remaining patients had deleterious mutations in CHEK2, FANCA, MLH1 (N = 2 of each, 2.1%), BRIP1, MRE11A, MSH2, and MUTYH (N = 1 of each, 1.1%).
The proportion of deleterious mutations varied according to risk factors. The deleterious mutations were found in 39 of 250 patients (15.6%) who had breast cancer and another primary cancer, 38 of 169 patients (22.5%) who had a family history (≥2 relatives) of breast cancer, 16 of 57 patients (28.1%) who had bilateral breast cancer, and 29 of 84 patients (34.5%) who were diagnosed with breast cancer at younger than 40 years old (Fig. 24.3). Furthermore, the distributions of the cancer-susceptibility genes were different according to risk factors (Fig. 24.4). In breast cancer patients with another primary cancer, BRCA1/2 and nonBRCA1/2 mutations accounted for 52.3% and 47.7% of mutations, respectively. The nonBRCA1/2 mutations comprised CDH1 (11.4%), SPINK1 (9.1%), RAD51 (6.8%), and TP53 (6.8%) mutations. In breast cancer patients with a family history of breast cancer, 65.8% carried a BRCA1/2 mutation. In 34.2% of nonBRCA1/2 mutations, 7.9% had RAD51 and TP53 mutations and 5.3% had CDH1 and SPINK1 mutations. In bilateral breast cancer patients, 68.4% carried a BRCA1/2 mutation.
Among 31.6% who had nonBRCA1/2 mutations, CHEK2 (10.5%) was found frequently and 5.3% of patients had CDH1, TP53, NBN, and MRE11A mutations. In patients diagnosed with breast cancer at younger than 40 years old, 62.1% carried BRCA1/2 mutations and 37.9% carried nonBRCA1/2 mutations including RAD51, NBN, CHEK2, CDH1, TP53, PTEN, FANCA, and MRE11A mutations. In 64 hereditary cancer predisposing genes, we found deleterious mutations in 16 genes, including BRCA1/2. However, we did not find deleterious mutations in the remaining 48 genes.
1.3.3 Novel Deleterious Mutations
We detected two novel deleterious mutations that were not previously reported: c.3096_3111del (p. K1032Nfs) in BRCA2 and c.849T>A (p.Y283*) in MLH1. The p. K1032Nfs mutation in BRCA2 is identified in patient_468. This mutation encodes a truncated nonfunctional protein in the domain of the BRC repeats, interfering with cellular response to DNA damage (Fig. 24.5a). The p.Y283* mutation in MLH1 is identified in patient_378 and is also predicted to encode a nonfunctional protein, leading to the disruption of an important functional domain, such as the MutL C-terminal domain (Fig. 24.5b). The impact of both mutations was predicted deleterious mutations in in silico prediction.
1.3.4 Frequency of VUS
A total of 333 missense mutations were identified in 64 genes. After in silico prediction by database and bioinformatics analysis to evaluate pathogenicity, most of the missense mutations were classified as benign or likely benign. Mutations with conflicting interpretations of pathogenicity but suspicion of being deleterious were classified as VUS. A total of 20 VUS were identified in 67 patients (13.5%) (Table 24.4). In 15 patients, deleterious mutation and VUS were found concurrently. The proportion of VUS differed among the risk factors for HBOC (Fig. 24.3). VUS was identified in 11.6% of breast cancer patients with another primary cancer, 14.8% of patients with a family history of breast cancer, 15.8% of bilateral breast cancer patients, and 17.0% of patients who were diagnosed with breast cancer younger than 40 years old. Additionally, 13 patients with VUS also had a concurrent deleterious mutation (patient_33, 66, 105, 115, 133, 182, 222, 233, 264, 280, 454, 468, and 501).
2 Conclusion
To the best of our knowledge, this is the largest study to include Korean breast cancer patients with clinical features of HBOC and examine the frequency and characteristics of germline mutations in BRCA1/2 and nonBRCA1/2 cancer-susceptibility genes.
We analyzed germline mutations from 496 breast cancer patients of Asian ethnicity with clinical features of HBOC using NGS-based multigene panel testing. Overall, 95 patients (19.2%) were found to carry 48 deleterious germline mutations in 16 cancer-susceptibility genes. The NGS-based multigene panel test improved the detection rates of deleterious mutations and provided a cost-effective cancer risk assessment compared with a gene-by-gene approach.
References
Lincoln SE, Kobayashi Y, Anderson MJ, Yang S, Desmond AJ, Mills MA, et al. A systematic comparison of traditional and multigene panel testing for hereditary breast and ovarian cancer genes in more than 1000 patients. J Mol Diagn. 2015;17(5):533–44.
Kapoor NS, Curcio LD, Blakemore CA, Bremner AK, McFarland RE, West JG, et al. Multigene panel testing detects equal rates of pathogenic BRCA1/2 mutations and has a higher diagnostic yield compared to limited BRCA1/2 analysis alone in patients at risk for hereditary breast cancer. Ann Surg Oncol. 2015;22(10):3282–8.
Couch FJ, Shimelis H, Hu C, Hart SN, Polley EC, Na J, et al. Associations between cancer predisposition testing panel genes and breast cancer. JAMA Oncol. 2017;3(9):1190–6.
Buys SS, Sandbach JF, Gammon A, Patel G, Kidd J, Brown KL, et al. A study of over 35,000 women with breast cancer tested with a 25-gene panel of hereditary cancer genes. Cancer. 2017;123(10):1721–30.
Rosenthal ET, Bernhisel R, Brown K, Kidd J, Manley S. Clinical testing with a panel of 25 genes associated with increased cancer risk results in a significant increase in clinically significant findings across a broad range of cancer histories. Cancer Genet. 2017;218:58–68.
Slavin TP, Niell-Swiller M, Solomon I, Nehoray B, Rybak C, Blazer KR, et al. Clinical application of multigene panels: challenges of next-generation counseling and cancer risk management. Front Oncol. 2015;5:208.
Desmond A, Kurian AW, Gabree M, Mills MA, Anderson MJ, Kobayashi Y, et al. Clinical actionability of multigene panel testing for hereditary breast and ovarian cancer risk assessment. JAMA Oncol. 2015;1(7):943–51.
Daly MB, Pilarski R, Berry M, Buys SS, Farmer M, Friedman S, et al. NCCN guidelines insights: genetic/familial high-risk assessment: breast and ovarian, version 2.2017. J Natl Compr Canc Netw. 2017;15(1):9–20.
Shin HC, Lee HB, Yoo TK, Lee ES, Kim RN, Park B, Yoon KA, Park C, Lee ES, Moon HG, Noh DY. Detection of germline mutations in breast cancer patients with clinical features of hereditary cancer syndrome using a multi-gene panel test. Cancer Res Treat. 2020;52(3):697–713.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Lee, ES., Kim, J., Han, W. (2021). Multigene Panel Testing for Hereditary Cancer and Genetic Counseling. In: Noh, DY., Han, W., Toi, M. (eds) Translational Research in Breast Cancer. Advances in Experimental Medicine and Biology, vol 1187. Springer, Singapore. https://doi.org/10.1007/978-981-32-9620-6_24
Download citation
DOI: https://doi.org/10.1007/978-981-32-9620-6_24
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-32-9619-0
Online ISBN: 978-981-32-9620-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)