Abstract
Abdominal wall endometriosis, a rare extrapelvic disease, normally is related to obstetric or gynecologic surgery; however, focused ultrasound surgery may be an alternative with a lower incidence of adverse events. Contrast-enhanced ultrasonography and magnetic resonance imaging were used to assess and observe abdominal wall endometriosis before and after focused ultrasound ablation. The therapeutic techniques, focused ultrasound parameters, and treatment outcomes are revealed, and the treatment outcomes with follow-up are shown and discussed. Cesarean scar pregnancy, which is the gestational sac implanted in a cesarean section scar, has a high risk of severe hemorrhage and uterine perforation after curettage. The therapeutic strategies, focused ultrasound parameters, and treatment outcomes are revealed to ablate the lesion without or with subsequent curettage.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- MRI
- Contrast-enhanced ultrasonography
- High-intensity focused ultrasound
- Ablation
- Abdominal wall endometriosis
- Cesarean scar pregnancy
- Curettage
Since 1997, the first patient with a malignant bone tumor was successfully treated with extracorporeal high-intensity focused ultrasound (HIFU) in the world; the focused ultrasound ablation has been used to treat liver cancer, pancreatic cancer, breast cancer, renal cancer, and other malignant tumors. As the treatment technology of uterine fibroids and adenomyosis has become more and more mature, Focused ultrasound ablation surgery (FUAS) application in gynecology has exhibited greater advantages. In recent years, it has also attracted the attention of some experts and clinicians in the application of pregnancy-related diseases, such as abdominal endometriosis and cesarean scar pregnancy. This chapter describes the clinical application of focused ultrasound for treating abdominal endometriosis and cesarean section scar pregnancy.
6.1 Focused Ultrasound Ablation for Abdominal Wall Endometriosis
6.1.1 Case 1
6.1.1.1 Case Description
The female patient was 28 years old. She had periodic abdominal pain for more than 3 years. The abdominal pain started one year after a cesarean section, and it occurred during menstruation and was relieved after menstruation. A mass was found in the abdominal wall for 5 months. Because of the progressive abdominal wall pain, treatment was required.
6.1.1.2 Pre-Treatment Assessment
MRI sagittal scan showed mixed high and low signals on T2WI suggestive of abdominal wall endometriosis, with a range of about 39 mm ×31 mm × 13 mm, T1WI contrast-enhanced T1WI showed abundant blood supply of the lesion, and the arrow in the figure showed abdominal wall endometriosis lesions (Fig. 6.1).
6.1.1.3 Treatment Techniques
-
1.
Focused ultrasound parameters. Average acoustic power: 125 W, sonication time: 381 s, duration of treatment: 76 min, total energy: 47,625 J.
-
2.
Focused ultrasound ablation techniques. The ablation range was 0.5–1.0 cm around the lesion. For patients with abdominal wall thickness less than 3 cm, focused ultrasound ablation should be chosen carefully.
6.1.1.4 Post-Treatment Assessment
MRI follow-up at 5 months after treatment. After 5 months of treatment, the abdominal wall endometriosis lesions were significantly reduced and absorbed (1.2 m × 0.7 cm). The arrow in the figure showed the abdominal wall had reduced endometriosis lesions (Fig. 6.2).
6.1.1.5 Discussion
-
The patient was a typical case of abdominal wall endometriosis and was unwilling to choose the traditional surgical treatment. After focused ultrasound ablation, the abdominal wall pain disappeared completely. Five months after the ablation treatment, MRI showed significantly reduced lesions.
-
In this case, the lesion was deep and close to the parietal peritoneum, and the risk of focused ultrasound ablation was high. During the treatment, attention should be paid to distending the bladder and covering the lesion with the bladder to prevent intestinal tissue damage by ultrasound ablation. If there is a bladder behind the lesion, the focus point should be placed 1 cm away from the abdominal peritoneum and avoid urinary retention after treatment.
6.1.2 Case 2
6.1.2.1 Case Description
The female patient was 38 years old. She had menstrual abdominal pain for more than 2 years. After the focused ultrasound ablation treatment, abdominal pain was relieved.
6.1.2.2 Pre-Treatment Assessment
MRI sagittal scan showed abdominal wall endometriosis with mixed high and low signals on T2WI measuring 32 mm × 45 mm × 32 mm. Contrast-enhanced T1WI showed that the lesion had an abundant blood supply (Fig. 6.3). Color Doppler ultrasound showed blood perfusion in the lesion (Fig. 6.4a).
6.1.2.3 Treatment Techniques
-
1.
Focused ultrasound parameters. Average acoustic power: 119 W, sonication time: 891 s, duration of treatment: 115 min, total energy: 106,030 J.
-
2.
Focused ultrasound ablation techniques. During the operation, the bladder was distended to the appropriate size to push the bowels away from behind the lesion to establish a safe acoustic pathway. Check the skin of the abdominal wall regularly to prevent skin scald or burn.
6.1.2.4 Post-Treatment Assessment
No obvious blood perfusion was found in the lesions by color Doppler ultrasound immediately after treatment (Fig. 6.4b).
6.1.2.5 Discussion
-
This patient is a typical case of abdominal wall endometriosis. The lesion diameter is large (about 4.5 cm), so choosing the over-range ablation during the treatment would be better. It must be noted that the ablation is 0.5 cm outside the junction of the normal tissue and the lesion. To avoid the influence of abdominal wall movement on the treatment, we should pay attention to controlling the pain reaction of patients and inform them to cooperate with the ablation.
6.1.3 Case 3
6.1.3.1 Case Description
The female patient was 27 years old. She had periodic abdominal pain for more than 4 years and a mass at the abdominal wall for 2 years.
6.1.3.2 Pre-Treatment Assessment
Sagittal MRI scan showed abdominal wall endometriosis with mixed high and low signals on T2WI, measuring 34 mm × 58 mm × 16 mm. Contrast-enhanced T1WI revealed that the lesion had an abundant blood supply (Fig. 6.5). Color Doppler ultrasound showed blood perfusion in the lesion (Fig. 6.6a).
6.1.3.3 Treatment Techniques
-
1.
Focused ultrasound parameters. Average acoustic power: 197 W, sonication time: 800 s, duration of treatment: 129 min, total energy: 157,600 J.
-
2.
Focused ultrasound ablation techniques. The location of the lesion was low in the abdominal wall, and the uterus was behind it. The uterus could block the bowels to establish a safe acoustic pathway. The treatment can be carried out close to the deep layer of the lesion.
6.1.3.4 Post-Treatment Assessment
The lesion did not have obvious blood perfusion immediately after treatment (Fig. 6.6b). The abdominal wall pain was relieved after follow-up.
6.1.3.5 Discussion
-
If patients have large lesions, use long treatment time and high power. Treatment should pay attention to the pain response of patients.
-
It is suggested that the treatment intensity should be gradually increased from low to high power. The acoustic power should start to increase after the effect of sedation and analgesia is satisfied. The treatment intensity should be maintained at 1:3 (1s sonication: 3s cooling interval).
6.1.4 Case 4
6.1.4.1 Case Description
The female patient was 33 years old and had left sub-abdominal pain during the menstrual period for more than one year. A nodule (around 2 cm in diameter) could be subcutaneously palpated near but not at the original cesarean scar in the left lower abdomen and it became larger with time. Abdominal wall endometriosis was diagnosed to refer to focused ultrasound ablation treatment. Three months after ultrasound ablation, the pain disappeared, and the nodule became smaller.
6.1.4.2 Pre-Treatment Assessment
MRI T2WI showed mini-cystic hyperintensity mixed with slightly high signals within the lesion (20 mm × 28 mm × 35mm) involving the rectus abdominis (Fig. 6.7a, black arrow), and heterogeneous enhancement was observed on the contrast-enhanced T1WI before treatment (Fig. 6.7b, c).
The lesion was located at the deep musculus layer of left side from the cesarean section scar, which did not influence the near-field of focused ultrasound.
6.1.4.3 Treatment Techniques
-
1.
Focused ultrasound parameters. Average acoustic power: 100 W, sonication time: 1100 s, duration of treatment: 45 min, total energy: 110,000 J.
-
2.
Focused ultrasound ablation techniques. The strategy with low acoustic power and longer sonication time would be employed because of the lesions involving the rectus abdominis. Each energy exposure lasted for 1 s and ceased for 2–3 s for cooling.
6.1.4.4 Post-Treatment Assessment
MRI evaluation after treatment: The treated lesion showed isointensity with a small portion of high signal (white arrow, tiny bleeding) on the T1WI image (Fig. 6.7d) and contrast-enhanced T1WI demonstrated the whole lesion of endometriosis was completely ablated within the swollen rectus abdominis (Fig. 6.7e, f).
6.1.4.5 Discussion
-
This patient had an intrauterine metal device (IUD) that interfered with MR imaging, but it did not influence the display of abdominal wall endometriosis. So, there is no need for the patient to remove the IUD.
-
Rarely the endometriosis lesion was not at cesarean incision, which is beneficial to ultrasound thermal ablation. Even so, the lower acoustic power still needs to be used.
-
When the endometriosis lesion involves abdominal muscles, it is recommended to expand the scope of surgery resection to prevent recurrence appropriately, but the risk might increase. Under such circumstances, non-invasive focused ultrasound ablation would be an alternative therapy.
6.1.5 Case 5
6.1.5.1 Case Description
The female patient, 28 years old, had periodic abdominal pain for more than one year, which started one year after a cesarean section. The pain occurred during menstruation and became severe. A sub-abdominal mass (around 50 mm × 80 mm) was found in the cesarean scar over 1 year, and no medication was effective.
6.1.5.2 Pre-Treatment Assessment
MRI scan showed the endometriosis lesion of cystic hyperintensity mainly mixed with low signals in the muscle of the subabdominal wall on T2WI, measuring about 35 mm × 58 mm × 75 mm (Fig. 6.8a). Contrast-enhanced T1WI revealed that the lesion had a moderately homogenous enhancement (Fig. 6.8b).
6.1.5.3 Treatment Techniques
-
1.
Focused ultrasound parameters: Average acoustic power: 89 W, sonication time: 3200 s, duration of treatment: 150 min, total energy: 284,800 J.
-
2.
Focused ultrasound ablation techniques: The lesion was located in the sub-abdominal wall adjacent to small bowels. The bladder was to be distended to separate them, avoiding the thermal injury to bowels (Fig. 6.8b, white arrow) since the energy deposit in the far-field of sound focus should be considered.
6.1.5.4 Post-Treatment Assessment
MRI evaluation after treatment: The lesion was completely ablated with a larger range than the original one. The peripheral enhancement around the non-perfused area was observed (Fig. 6.8c).
MRI follow-up at 3 months after treatment. The treated lesion significantly decreased on the contrast-enhanced T1-weighted image without recurrence after focused ultrasound ablation, and the pseudoenhancement around the lesion disappeared (Fig. 6.8d).
6.1.5.5 Discussion
-
The endometriosis was large in the abdominal muscle with fussy boundaries. It is difficult to completely remove the whole lesion by traditional surgery, and the probability of postoperative recurrence is high.
-
The lesion invades the rectus abdominis, and the surgical resection of the lesion would cause muscle loss resulting in an abdominal incisional hernia.
-
The fully distended bladder should be used to establish a safe acoustic pathway, avoiding the injury of the intestinal during the focused ultrasound ablation procedure because the lesion was located in the deeper layer of the abdominal wall.
-
Focused ultrasound ablation treatment can preserve the integrity of the abdominal wall and avoid the complications and sequelae of surgical resection.
6.2 Focused Ultrasound Ablation for Cesarean Scar Pregnancy
6.2.1 Case 1
6.2.1.1 Case Description
The female patient was 25 years old. She was hospitalized for 13 days due to vaginal bleeding after a drug-induced abortion. B-ultrasound showed mixed echo mass and abundant blood flow signal in the previous cesarean incision of uterus. The risk of curettage was high, so focused ultrasound ablation was proposed. After focused ultrasound ablation, MRI follow-up showed no abnormal vaginal bleeding, and hCG decreased gradually.
6.2.1.2 Pre-Treatment Assessment
MRI sagittal scan showed the lesions of cesarean scar pregnancy with mixed high and low signals on T2WI, and the implanted scar was deep into the serosal layer of uterus (Fig. 6.9a, b). The lesion measured about 35 mm × 30 mm × 28 mm. Contrast-enhanced T1WI showed abundant blood supply (Fig. 6.9c, d)
6.2.1.3 Treatment Techniques
-
1.
Focused ultrasound parameters. Average acoustic power: 400 W, sonication time: 1085 s, duration of time: 210 min, total energy: 434,000 J.
-
2.
Focused ultrasound ablation techniques. During the treatment the pregnancy tissue should be ablated. The focused ultrasound ablation can ablate the blood vessels less than 2 mm in diameter, but it is unnecessary to ablate the large blood vessels around the lesions. After the pregnancy tissue is ablated, the blood vessels can atrophy by themselves. The focus point should be more than 1.0 cm away from the serosal layer during the treatment to avoid energy diffusion to the myometrium and bladder injury.
6.2.1.4 Post-Treatment Assessment
MRI follow-up at 3 months after treatment: After treatment, MRI showed no obvious pregnancy tissue in the cesarean scar, which was completely ablated and discharged (Fig. 6.10).
6.2.1.5 Discussion
-
The lesion was implanted into the scar with abundant blood flow signals around. The curettage was prone to massive bleeding and uterine perforation, and the lesion was completely discharged after focused ultrasound ablation.
6.2.2 Case 2
6.2.2.1 Case Description
The female patient was 30 years old. She was hospitalized because of a small amount of vaginal bleeding for a day after having amenorrhea for 53 days. After focused ultrasound ablation, she had regular follow-ups, and her menstruation returned with no special symptoms.
6.2.2.2 Pre-Treatment Assessment
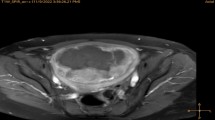
T2WI showed that the lower edge of the gestational sac of cesarean scar pregnancy was close to the scar, most of the gestational sac was in the uterine cavity, and the contrast-enhanced T1WI showed that the pregnancy tissue had an abundant blood supply (Fig. 6.11).
6.2.2.3 Treatment Techniques
-
1.
Focused ultrasound parameters: Average acoustic power: 400 W, sonication time: 750 s, duration of time: 73 min, total energy: 300,000 J.
-
2.
Focused ultrasound ablation techniques: High-intensity focused ultrasound (HIFU) was used to ablate the embryo and make the original heart tube beat disappear. The small blood vessels around the gestational sac, especially between the gestational sac and the anterior wall of the uterus, were destroyed. To avoid bladder injury, we should pay attention to keeping a distance from the serosal surface of the uterus.
6.2.2.4 Post-Treatment Assessment
-
Ultrasound imaging evaluation after treatment. The contrast-enhanced ultrasound showed that the pulsation of the cardiac tube disappeared, and the blood perfusion around the gestational sac decreased significantly. The curettage was performed 2 days after the operation, and the curettage process was smooth with less blood loss.
6.2.2.5 Discussion
-
The patient had an endophytic cesarean scar pregnancy. The lower edge was close to the scar. Most of the gestational sac was in the uterine cavity. There were abundant blood flow signals around it. Curettage was prone to massive bleeding. After focused ultrasound ablation, the curettage process and postoperative recovery were successful.
6.2.3 Case 3
6.2.3.1 Case Description
The female patient was 33 years old. She was hospitalized because of vaginal bleeding for 3 days after 47 days of amenorrhea. After focused ultrasound ablation, there were no special symptoms, and menstruation was recovered after 25 days.
6.2.3.2 Pre-Treatment Assessment
MRI T2WI showed that the gestational sac of cesarean scar pregnancy was completely located in the scar, protruding the serous layer outwards. It was considered an exogenous scar pregnancy. The contrast-enhanced T1WI showed that the lesion had an abundant blood supply (Fig. 6.12).
6.2.3.3 Treatment Techniques
-
1.
Focused ultrasound parameters: Average acoustic power: 400 W, sonication time: 500 s, duration of time: 74 min, total energy: 200,000 J.
-
2.
Focused ultrasound ablation techniques: High-intensity focused ultrasound (HIFU) was used to ablate the embryo, and the fetal heart tube pulsation had disappeared. The blood flow of the cesarean scar should be treated according to the thickness of the myometrium. If its thickness is less than 5 mm, it should be treated carefully to avoid perforation of the uterus during curettage.
6.2.3.4 Post-Treatment Assessment
-
After treatment, color Doppler ultrasound showed that the primitive heart tube pulsation disappeared. The curettage was performed 2 days after the ablation treatment, and the process of curettage was smooth with little blood loss.
6.2.3.5 Discussion
-
The gestational sac was completely located in the cesarean section scar. The gestational sac protruded through the serosal layer with a thin myometrial layer (only 2 mm). The focused ultrasound ablation should only treat the original heart tube pulsation and avoid overtreatment damaging the muscle layer and leading to scar perforation during curettage.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Zhu, X., Xu, Y., Xue, M., Wong, F. (2023). Focused Ultrasound Ablation for Other Gynecological Related Diseases. In: Xu, Y., Yang, L., Wong, F. (eds) Surgical Techniques of Focused Ultrasound Ablation in Benign Uterine Diseases. Springer, Singapore. https://doi.org/10.1007/978-981-19-7180-8_6
Download citation
DOI: https://doi.org/10.1007/978-981-19-7180-8_6
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-7179-2
Online ISBN: 978-981-19-7180-8
eBook Packages: MedicineMedicine (R0)