Abstract
The vital role of structurally and functionally stable vasculature in engineered tissues is well-established in regenerative medicine. Large-volume, natural, and synthetic tissue constructs require a high degree of perfusion and nutrient diffusion to meet the physiological demands of the encapsulated cells. Additionally, cancer tissue models fabricated using various scaffolds and matrices also need to incorporate tumor-mimetic abnormal vasculature to study the influence of angiogenesis on tumor growth, progression, and anti-cancer drug delivery. In this chapter, prominent hydrogel-based matrices that have been developed for vascular tissue engineering as well as modeling of the tumor vasculature and angiogenesis are discussed. Various microenvironmental considerations (including biophysical and biochemical characteristics of the matrix) required for emulating vascular regeneration as well as tumor angiogenesis are described. A wide range of hydrogel-based models (including natural, synthetic and hybrid materials) and associated biofabrication strategies (spanning molecular design to macroscale materials processing) for creating vascularized scaffolds are elaborated. Overall, this chapter provides an overview to the reader on creation of engineered scaffolds for implementation in tissue vascularization and repair and in disease models for future applications in drug testing.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
8.1 Introduction
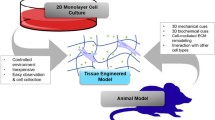
In recent decades, there has been an increasing demand for large-volume tissue-engineered organs and synthetic biomaterial-based constructs for use in regenerative medicine applications. One of the fundamental requirements of such organs or constructs is the presence of stable and functional vascular network which can provide the required supply of oxygen and nutrients as well as metabolic waste clearance in a continuous and consistent manner. The proper function of the vascular network is essential in maintaining long-term cell viability, and overall structure and function in a wide range of organ- and tissue-mimics (Auger et al. 2013).
However, generation of such vascular networks has been beset with several challenges. A wide range of biomaterials have been employed so far for synthetic vascularized tissues and more are under development. Also, vascular cells used for tissue engineering applications are obtained from a wide variety of sources, making it difficult to control and compare experimental conditions for further translation and replication. Given the strict requirements of vascular cells in terms of matrix microenvironment conducive to vascular network formation, it is important to match the right biomaterial properties and culture conditions with the vascular cell types used for specific applications (Novosel et al. 2011; Chang and Niklason 2017).
In addition to tissue engineering applications, in vitro modeling of various diseases and pathologies has also gained prominence. Particularly, modeling of cancer has been an attractive research problem, owing to the ability to recapitulate the native tumor microenvironment (TME) using various biomaterial-based approaches (Pradhan et al. 2016). One of the most influential components of the TME is the tumor-associated endothelial cells (TECs), which constitute the leaky and tortuous tumor vasculature adjacent to growing tumors. TECs actively participate in tumor angiogenesis and promote tumor growth, progression, and metastasis via a wide range of mechanisms (Dudley 2012). When creating in vitro tumor models, it is important to incorporate TECs along with cancer cells, so that the wide diversity of intercellular and cell-matrix crosstalk can be accurately captured in in vitro engineered systems. These vascularized tumor models can provide high-quality predictive information regarding candidate drug efficacy and accelerate the anti-cancer drug screening process.
In recent years, numerous biomaterials (including natural, synthetic, and semi-synthetic hydrogels) have been implemented for the generation of vascularized matrices and scaffolds for both regenerative medicine and disease modeling applications (Chang and Niklason 2017). Hydrogels are an attractive material of choice owing to their versatility, user programmability, ease of fabrication, availability of wide range of biochemical and mechanical properties that fits diverse requirements of various physiological and pathological tissues. Hydrogels have been used for both two-dimensional (2D) and three-dimensional (3D) culture of vascular cells by modifying the matrix properties to suit vascular growth, morphogenesis, and function. Additionally, hydrogels have also been used to model the processes of vasculogenesis (formation of blood vessels de novo) and angiogenesis (formation of new blood vessels from pre-existing ones) within 3D matrices (Rouwkema and Khademhosseini 2016). An important advantage of using hydrogel matrices for vascular studies is the ability to monitor and control the process of vascular morphogenesis in a dynamic, user-controllable fashion simply by altering the material properties in a spatiotemporal manner. These matrices can also be used to obtain vascular networks from a wide variety of cell sources (including human induced pluripotent stem cells, patient-derived adipose stromal cells, and others). By controlling the matrix properties, including adhesivity, porosity, stiffness, alignment, and matrix compliance, the evolution of the vascular networks can be controlled to obtain patent, perfusable, and stable branched microchannels that closely human capillary networks (Nerem and Seliktar 2001; Stegemann et al. 2007). Overall, hydrogels have an important role to play in modeling vascular morphogenesis and function to mimic various physiological and diseased states.
In this chapter, an overview of the microenvironmental considerations for recreating vascular networks for regenerative medicine and tissue engineering applications is provided. Further, special considerations of the TME that are required to mimic tumor angiogenesis are described. Multiple hydrogel-based strategies employed for these applications, especially modifications of biochemical and biophysical properties in hydrogel matrices that induce vascular differentiation, morphogenesis, and stabilization, are also described. Various biofabrication strategies (ranging from chemical and molecular modifications to large-scale volumetric matrix modifications) that have been implemented to mimic the vasculogenesis and angiogenesis processes are described at length. Finally, the current challenges pertaining to tissue vascularization and modeling of vascularized tumors are analyzed and perspectives for future studies are discussed. We anticipate the readers to obtain a fundamental understanding of the basic requirements to recreate vascular networks for various applications, various material-based strategies and biofabrication technologies available to recreate these networks, and finally apply these principles to further translate these biomaterial-based vascularization techniques towards clinical implementation.
8.2 Microenvironmental Considerations for Vascular Regeneration
In order to design engineered vascular networks using hydrogel-based scaffolds, it is necessary to understand the basic vascular structure found across various parts of the human body as well as the surrounding tissue niches and associated microenvironments served by these networks. A typical large blood vessel consists of three layers: the innermost layer, tunica intima; the middle layer, tunica media; and the outermost layer, tunica adventitia.
Tunica intima is composed of a monolayer of endothelial cells (ECs), whose cellular, molecular, and genetic characteristics vary from organ to organ. The monolayer is surrounded by a thin and protein-rich basement membrane (BM) primarily composed of collagen type IV and laminin which forms the endothelium. The endothelium forms a selective but permeable barrier between the blood and the surrounding tissues, primarily through the tight intercellular junction and adhesion molecules between the ECs (e.g., VE-Cadherin, CD31, CD144 amongst others). A healthy and stable endothelium maintains vascular homeostasis by regulating vascular tone, blood pressure, inflammation, and angiogenesis by secretion of multiple cytokines and signaling molecules, and permeability to nutrients, oxygen, and metabolites (James and Allen 2018; Charbonier et al. 2019; Pradhan et al. 2020). All vascularized tissue-engineered models must incorporate ECs as they are an indispensable component of blood vessels. Additionally, organ-specific recapitulation of engineered tissues requires incorporation of organ-specific ECs (Marcu et al. 2018). For example, in case of liver regeneration, recreating hepatic sinusoids requires fabrication of a fenestrated endothelium made of liver sinusoid endothelial cells (LSECs), while in case of retinal tissue regeneration, choroidal ECs are required to form the perfusable network underlying the retinal pigment epithelial (RPE) cells.
The tunica media is composed of pericytes or smooth muscle cells (SMCs) that surround the endothelium and are held together by a supportive layer of ECM proteins primarily composed of collagen type I and elastin. The medial layer provides structural support to the endothelium and maintain vascular quiescence, stability, and integrity. Disruption of the medial layer is often associated with increased vascular sprouting and angiogenesis, particularly in cases of wound healing and tumor growth. The tight wrapping of pericytes around microvascular networks is particularly critical for selectively permeable vascular barriers in the body, for example, the blood-brain barrier (BBB) that closely regulates the exchange of nutrients, metabolites, and toxins in the brain niche. Considering the physical forces involved with flow of blood, nutrients, and culture media within the endothelium, the SMCs in the medial layer are particularly responsible for vasoconstriction and vasodilation, especially in the larger blood vessels (James and Allen 2018; Charbonier et al. 2019; Pradhan et al. 2020). Although many tissue-engineered vascularized constructs operate solely on encapsulated ECs, incorporation of SMCs, pericytes, or differentiated stromal/stem cells along with ECs has been shown to increase microvascular network stability, patency, and permeability. However, similar to ECs, the proper selection of organ-specific perivascular cells is also important, especially when fabricating organ-specific vascular networks.
The tunica adventitia is composed of a heterogenous population of cells including fibroblasts, myofibroblasts, macrophages, mesenchymal stem/stromal cells (MSCs) amongst others surrounded by a thicker ECM layer composed of collagen types I and III and elastin. Similar to the medial layer, the adventitial layer, provides additional mechanical stability to large blood vessels and regulates vasomodulation in response to fluidic pressures within the endothelium. Disruption of the tunica adventitia can lead to serious vascular damage and may require greater involvement of external microenvironmental factors (immune cell infiltration, inflammation, and deposition of ECM proteins) as a regenerative strategy for vascular restabilization and repair (James and Allen 2018; Charbonier et al. 2019; Pradhan et al. 2020). Majority of tissue-engineered constructs primarily recapitulate microvascular networks and hence incorporation of mural cells comprising the adventitia is generally overlooked. However, several studies have explored the incorporation of fibroblasts, MSCs and even SMCs to stabilize rudimentary vascular networks. In addition to maintaining cell-cell contact with ECs, these stromal cells also secrete a multitude of pro-angiogenic and/or pro-vasculogenic factors which help regulate the growth, spreading, and quiescence of underlying ECs in a context-dependent manner. Regulating the biophysical and biochemical interactions of these stromal cells with ECs is key to maintaining stable vasculature in engineered tissues (Fig. 8.1).
Morphological differences between normal and tumor vascular networks. Normal vasculature is characterized by an initial cell plexus that is regulated by cell-cell and cell matrix interactions and appropriate mechanical signaling processes that help form ordered networks with structurally and functionally stable lumens. Tumor vasculature owing to recruitment of multiple cell types and imbalance of various signaling factors results in a disordered, tortuous, and leaky network. Images of blood vessels from intravital microscopy and corresponding skeletonized images demonstrate the differences between the organization and structure of the vascular networks. Adapted with permission from (Jain 2003)
In addition to different cell types constituting the vasculature, it is important to consider the role of the ECM surrounding the cells as well as various hemodynamic variables which exert physical forces on both the cellular and acellular components in the vascular niche. The composition and microarchitecture of the ECM present in the basement membrane (BM) and the surrounding ECM vary with location in the body, age of the individual, physiological state, and other broader environmental factors. Particularly, in younger individuals, the basement membrane is composed of collagen IV which progressively gets replaced with collagen I with aging. Similarly, the production of elastin is also reduced drastically with age, thereby making blood vessels much stiffer, inability to modulate vascular tone, more prone to inflammation, and susceptible to damage under milder physical forces. The porosity and mechanical compliance of the BM and the permeability of the endothelium (resulting from the tight EC junctions) are also dependent upon the proteomic composition. With increasing collagen I deposition due to vascular aging and misalignment in deposited fibrillar proteins, the BM can become more porous and the EC junctions can weaken over time to lose their phenotypic plasticity. This can cause the vascular endothelium to become leaky and more permeable (James and Allen 2018; Charbonier et al. 2019; Pradhan et al. 2020). Hence, when designing synthetic scaffolds for vascularized tissue, it is important to maintain the appropriate stiffness, matrix compliance, porosity, and fibrillar alignment so that rudimentary blood vessel segments can interconnect with each other into an integrated fluidic network that has uniform coverage of the entire scaffold or matrix.
Among the hemodynamic factors influencing vascular regeneration, the most important are fluid shear stress, circumferential strain, cyclic stretch, and fluid pressure. Considering the pulsatile nature of blood flow (originating in the heart and propagating to the capillaries) and the wide range of shear stress values existing across the spectrum of blood vessels, it is necessary to study the effect of these factors in the context of vascular regeneration. Physiological levels of shear stress are necessary to maintain vascular patency, EC junction adhesion strength, and an overall healthy endothelium. In addition, the fluid pressure level and a consistent level of pulsatile flow should also be maintained to ensure physiological levels of circumferential strain and cyclic stretch. The biophysical forces acting on the endothelium also ensures optimum secretion of pro-vasculogenic biochemical signaling to ensure proper endothelial structure and function (James and Allen 2018; Charbonier et al. 2019; Pradhan et al. 2020). Some of these factors include vascular endothelial growth factor (VEGF), basic fibroblast derived factor (bFGF), angiopoietin-2 (Ang2), platelet derived growth factor BB (PDGF-BB) and others. When designing vascularized scaffolds, it is important to incorporate these hemodynamic factors on 2D substrates or within the 3D volumes, which shape the initial spreading and connectivity of ECs and ensure proper tubulogenesis and lumenogenesis to form vascular networks.
In addition to soluble factor signaling, local oxygen concentration is one of the key determinants of vascularization. Hypoxic microenvironments promote upregulation in expression of key pro-angiogenic genes including hypoxia-inducible factor-1α (HIF-1α), vascular endothelial growth factor-A (VEGFA), and others. This leads to promotion of angiogenic sprouting, vessel branching, and rapid vascularization (Krock et al. 2011). This principle has often been used for wound healing and reparative angiogenesis. On the flip side, this process is also hijacked by diseased cells, including cancer, to promote excess and undesired vessel formation, which leads to further complications. Physiological oxygen concentration helps in maintaining stable microvascular networks. Hence, the local oxygen concentration must be carefully monitored and dynamically controlled to ensure that rudimentary vascular segments undergoing anastomosis are gradually stabilized and form patent and long-lasting microvascular networks.
Overall, when fabricating designer-scaffolds for vascularization and tissue regeneration, the initial matrix microenvironmental conditions must be made amenable not only to the functional cells of interest but also the organ-specific vascular cells that would eventually form the vasculature. This includes control of cellular components (ratio of different cell types, density of cells in the matrix volume, inclusion of supportive mural cells, etc.), culture conditions (composition of media, growth factors, hormones, etc.), extracellular components (ECM composition, stiffness, adhesivity, porosity, alignment, etc.), hemodynamic forces (shear stress, interstitial fluid pressure, diffusion, matrix perfusability, cyclic load, etc.), amongst others.
8.3 Microenvironmental Considerations for Tumor Angiogenesis
The tumor microenvironment is a unique and complex milieu of a wide range of cellular, extracellular, and biochemical factors that work in an intertwined fashion to promote the growth and invasion of the central tumor mass. A growing tumor mass generally consists of an outer proliferating cell layer, a middle quiescent layer, and an inner necrotic core of cells densely packed with each other. Due to limitations in oxygen diffusion through this densely packed mass, majority of cancer cells undergo hypoxia and secrete pro-angiogenic factors to promote tumor angiogenesis from surrounding healthy vasculature (Harris 2002).
However, tumor angiogenesis leads to rapid angiogenic sprouting, without sufficient time for recruitment of supportive mural cells for vessel stabilization. Hence, the resulting vascular network is disorganized, tortuous, immature, and hyperpermeable. Although normal blood vessels have unidirectional flow, tumor blood vessel exhibit chaotic loops and irregular branches, leading to disrupted and bidirectional flow. The discontinuous endothelial lining and poor EC junctions lead to leaky vessels and deposition of vascular components in the extravascular space. At the cellular level, TECs are significantly different in their genetic and molecular characteristics from normal ECs, which also lead to differences at the hierarchical tissue level (Dudley 2012) (Fig. 8.1).
Designing this complex pathological state within tissue-engineered constructs is both crucial and challenging at the same time. 3D models of vascularized tumors are important testbeds for screening the efficacy of candidate drugs and therapeutic agents. Tumor cells cultured alone and those in co-culture with endothelial cells (or even better, tumor-associated endothelial cells, TECs) have been shown to have distinct response profiles to drugs. The presence of supportive vascular or stromal cells in the TME also confers additional chemoresistance to tumor cells and enables survival and future relapse. Hence, it is important to incorporate vascular cells and/or stromal cells to accurately recapitulate the native microenvironmental conditions of tumors. In that regard, employing hydrogels as ECM-mimics is an advantageous strategy owing to the ability to independently tune the biochemical and mechanical properties to suit multiple cell types and modularly assemble them into integrated complex synthetic tissues for co-culture studies. For example, it is known that the tumor ECM is stiffer than adjacent normal ECM due to altered secretion and deposition of matrix proteins. Hence, hydrogels with higher stiffness can be used to culture tumor cells or tumor spheroids to form a central 3D tumor mass. Adjacent to this mass, hydrogels encapsulating endothelial cells in a softer matrix can be used for co-culturing with cancer cells. The combined hydrogel assembly can be used as an integrated vascularized tumor-mimic for drug-testing applications.
Recapitulating the complex architecture of tumor microvasculature is technologically challenging owing to various factors. Obtaining TECs from reliable and consistent sources is not guaranteed and isolation of TECs is also associated with inter-patient variability. Encapsulation of ECs in co-culture with cancer cells within 3D hydrogel matrices is one common strategy employed in many studies. However, the ability of the ECs to reassemble into tumor vessel-like networks depends completely on the culture and matrix conditions and the ability of tumor cells to secrete pro-angiogenic factors. This variability has led to some engineering innovations where tumor vessel-like microchannels are prefabricated within 3D hydrogel volumes or within microfluidic devices and later seeded with ECs which assume the morphology and structure of these microchannels (Michna et al. 2018). Although most studies use normal endothelial cells like human umbilical vein endothelial cells (HUVECs) for cancer co-culture studies, the use of tumor-specific ECs or patient-derived ECs is also gaining prominence.
In general, hydrogel-based vascularized tumor models provide a reasonable approach for modeling the complexity of native tumors and can be designed from a bottom-up approach to match the characteristics of the complex milieu. Considering the wide range of intra-tumor and inter-tumor heterogeneity, it is necessary to standardize the practice of fabricating vascularized tumors, especially for discovery of targets against tumor angiogenesis and the development of anti-angiogenic drugs. Alternate strategies for normalization of tumor blood vessels are also being explored for more efficient delivery of drugs and therapeutics that can reach the tumor mass effectively.
8.4 Hydrogel-Based Models for Vascular Regeneration and Tumor Angiogenesis
As discussed earlier, hydrogels provide a diverse and dynamic set of matrix microenvironmental conditions to mimic native ECM that can promote vascular growth, long-term maintenance, integration with host vasculature for tissue engineering, and regenerative medicine applications. By tuning the chemical building blocks of polymer chains, constitutive functional groups, and the degree of crosslinking, higher order macromolecular properties of hydrogel-based scaffolds (including viscoelasticity, adhesivity, hydrophilicity, surface charge, porosity, and topology) can be controlled and can be optimized for various types of vascular cells. Traditionally, ECs are seeded on 2D bioactive hydrogel substrates to assess for their vasculogenic potential by quantifying cell spread, proliferation, tubule formation, and expression of prominent vasculogenic markers (CD31, VE-Cadherin, VEGFA, etc.). In some cases, 2.5D cultures are established where ECs seeded on the top surface of a hydrogel scaffold can transmigrate through the underlying porous network and infiltrate deeper regions of the scaffold. However, to accurately mimic native physiological vascular morphogenesis, it is necessary to establish 3D cultures of hydrogel-encapsulated cells. Single ECs when encapsulated within permissive hydrogel matrices at specific cell densities can interconnect with each other through filopodial protrusions and elongated cell bodies to form rudimentary vascular networks. These rudimentary networks can be stabilized by surrounding mural cells (e.g., pericytes, fibroblasts, MSCs) until they anastomose into integrated vascular lumens (Peters et al. 2016).
Hydrogels employed for vascular applications can be broadly grouped into natural, synthetic and hybrid materials. Natural ones (e.g., Matrigel, collagen, fibrin, gelatin, alginate and agarose) are obtained from animal or plant sources and have long been used for both in vitro modeling and in vivo vascular regeneration studies. Synthetic hydrogels (e.g., poly(ethylene glycol) (PEG), poly(lactic-co-glycolic acid), poly(caprolactone)) are obtained through chemical synthesis. Hybrid hydrogels (e.g., gelatin methacryloyl, methacrylated hyaluronic acid, methacrylated dextran, PEGylated proteins) are obtained by synthetically modifying natural components to improve their suitability for vascular applications.
Compared to natural hydrogels, synthetic polymers allow better control over their chemistry (by functionalization with polysaccharides, proteins, or peptides) and structure to fabricate highly tailored 3D scaffolds (in terms of mechanical properties, biofunctions and degradability) for vascular regeneration and tumor angiogenesis. Moreover, since these polymers are chemically synthesized, the problem of availability and batch-to-batch variability is almost negligible, thus promoting highly reproducible scaffold properties. Inherent inertness of most synthetic polymers guarantees unintentional immune responses when implanted as vascular grafts even for long-term regeneration. Some of natural (Table 8.1), synthetic, and hybrid (Table 8.2) scaffolds are described in detail below.
8.4.1 Matrigel
Matrigel, isolated from Engelbreth-Holm-Swarm (EHS) mouse sarcoma and rich in laminin, collagen IV and other growth factors, is a popular choice amongst biologists as a reconstituted basement membrane for 3D cellular studies. Owing to its tumorigenic source, Matrigel contains a wide range of pro-angiogenic growth factors and proteomic components which makes it ideal for angiogenesis assays (i.e., assess the potential of vascular cells to form tubulogenic networks, vascular sprouts). Moreover, these assays are increasingly being integrated with other technologies to build more complex angiogenesis evaluation methods, particularly for high-throughput, reliable, and effective readouts (Akhtar et al. 2002; Kleinman and Martin 2005; Khoo et al. 2011) (Fig. 8.2a). Matrigel has also been shown to enhance the rate of epithelialization and wound healing and promotes the retention of keratinocytes in deep wounds, although its clinical translation is questionable. Matrigel owing to its ability to support tumor growth can be used for co-culture studies of cancer cells with ECs. It is routinely used for in vivo implantation of tumors and in invasion assays. However, it is inherently limited in its material properties due to its animal origin. The heterogeneity in its chemical composition and the inability to control rigidity of gels across different batches makes it difficult to reproduce results across large study sets. This has led to the gradual development of synthetic materials as an alternative to Matrigel (Aisenbrey and Murphy 2020).
Representative examples of natural hydrogels enabling vascularization and angiogenesis. (a) GFP-labelled HUVECs co-cultured with ADSCs in Matrigel/rat tail collagen I hydrogels after 14 days of culture in serum-free media demonstrate stable, lumenized, and patent microvascular networks as evidenced by fluorescent dextran perfusion. Adapted from (Andrée et al. 2019). (b) HUVECs (red) and pericytes (green) co-cultured within fibrin gels undergo angiogenic sprouting towards a biochemical gradient within a microfluidic chip as imaged on day 3 (left) and day 6 (right). Pericytes gradually wrap around endothelial lumens to stabilize the neovessels and form patent lumens. Scale bar: 100 μm. Adapted from (Kim et al. 2015)
Similar to Matrigel, various decellularized ECM (dECM) have also been prepared from various animal (porcine, bovine, etc.) and human sources that have been implemented for vascular tissue engineering (Hackethal et al. 2021). dECM contains a multitude of native growth factors, hormones, and other bound signaling factors necessary for optimal vascular morphogenesis and have been successfully implemented in various regenerative studies. However, the heterogeneity in composition coupled with unreliability of source material makes it challenging to implement it extensively at a clinical scale.
8.4.2 Collagen and Gelatin
Collagen (primarily type I) and its hydrolytic product, gelatin, have been widely used for vascular tissue engineering applications and for in vitro cancer studies, owing to its ease of isolation and abundance in animal tissues (Fig. 8.2a). When thermally/physically crosslinked, collagen and gelatin assume a fibrillar architecture, whose microstructural properties (including fiber alignment, thickness, stiffness, and density) can be controlled by modulating concentration, temperature, and pH, thereby resulting in gels with widely varying bulk properties (McGuigan and Sefton 2006; Celie et al. 2019; Morgan et al. 2019; Redd et al. 2019). Alignment of collagen/gelatin fibers is of particular interest as they promote contact-guidance dependent assembly and migration of cells encapsulated in 3D gels or topographical guidance on 2D substrates. ECs seeded in scaffolds of aligned, isotropic collagen fibers can form rapid and robust vascular networks compared to those in random, anisotropic collagen scaffolds. Collagen and gelatin hydrogels have also been used extensively for spheroid cultures to study 3D vascular sprouting and vascular morphogenesis assays.
In addition to physical crosslinking, collagen and gelatin can also be chemically or enzymatically crosslinked using various functional side groups on the macromolecular backbone to form more robust hydrogels. Although stiffness of these hydrogels can be increased with additional crosslinks, it is still lower than that observed in native tumor tissues, and they are susceptible to rapid degradation post implantation in vivo. Further, various matrix properties including stiffness, porosity, degradability, and adhesivity of collagen/gelatin are intimately coupled with each other, making it difficult to independently study the role of these parameters in vascular regeneration and tumor angiogenesis. In recent approaches, collagen and gelatin have also been modified with functional methacrylate groups that can be chemically crosslinked to form stiffer hydrogels (Yuan et al. 2021). The degree of methacrylation and polymer concentration determines the degree of crosslinking and the resulting macromolecular architecture of the hydrogels. Owing to the cheap and facile nature of handling collagen and gelatin, these are popular choices for both in vitro and in vivo vascular applications.
8.4.3 Fibrin
Fibrin hydrogels, obtained by thrombin-mediated cleavage and polymerization of blood-isolated fibrinogen protein, have often been used for various vascular regeneration as well as for in vitro mechanistic studies of vasculogenesis and angiogenesis (Fig. 8.2b). Owing to its good hemocompatibility, ability to bind to large number of blood proteins, and rapid crosslinking properties, fibrin is an attractive material of choice, particularly for wound healing and tissue sealing applications. In addition to endothelial cells, fibrin is conducive to other supportive cell types, including MSCs, SMCs, pericytes, adipose-derived stromal cells (ADSCs), that help form integrated and stable vascular networks in three-dimensional constructs. Fibrin hydrogels are also commonly used for vascular sprouting assays to assess the vasculogenic potential of isolated cell types (Nehls et al. 1994; Nehls and Drenckhahn 1995; Nakatsu et al. 2003).
The fibrillar microarchitecture of fibrin hydrogels allows directional migration and rapid interlinking of encapsulated vascular cells and rudimentary tubules. However, fibrin hydrogels, owing to their high in vivo degradation rates, result in rapid generation of new capillaries that are unstable, tortuous, and highly branched. High fibril density is also detrimental to the vascular sprouting process. Implantation and long-term studies using fibrin can be conducted by modulating the fibrin microarchitecture or by mixing with other materials (collagen, gelatin, alginate, etc.) to form integrated and multi-crosslinked constructs. Depending upon the polymerization mechanism and dynamics (pH, temperature, additional crosslinkers like transglutaminase, etc.), the mechanical and architectural properties of the fibrillar network can be modified in various ways (Juliar et al. 2018). This enables users to adjust the bulk stiffness, stability, and biodegradability of fibrin gels at the macro-scale as well as modulate cellular-level responses and morphology at the micro-scale. These abilities make fibrin an attractive material of choice for vasculogenic and angiogenic applications.
8.4.4 Alginate and Agarose
Alginate and agarose, linear polysaccharide-based co-polymers obtained from seaweed, have been extensively used as a cheap source of vascular-compatible biomaterials for several in vitro and in vivo applications. Alginate is composed of β-(1–4)-linked d-mannuronic acid (M) and β-(1–4)-linked l-guluronic acid (G) units, while agarose is composed of α-(1-3) linked d-galactose and β-(1-4) linked 3,6-anhydro-l-galactopyranose. Sodium alginate, when treated with calcium ions, gets chelated rapidly to form calcium alginate hydrogels via ionic crosslinking. Agarose when dissolved in water and heated cools back to form hydrogels via thermal gelation. Alginate and agarose do not have any inherent cell-adhesive ligands; hence vasculo-mimetic ligands need to be incorporated separately when preparing scaffolds of these materials. Some of these ligands include the ubiquitous RGD peptide motif and the protease-sensitive VEGF receptor binding peptide GPQGIAGKLTWQELYQLKYKGI amongst others (Barrs et al. 2021; Teixeira et al. 2021). Additionally, alginate and agarose can also be combined with other materials like gelatin, fibrin, and others to form hybrid hydrogels with improved mechanical and biochemical properties (Kinoshita et al. 2016).
Some major advantages of alginate hydrogels include the ability to modulate its degree of crosslinking and stiffness by regulating the concentration of Ca2+ ions, high degree of stability and relatively lower rate of biodegradation, 2D and 3D printability and injectability (due to it viscoelastic nature), amongst others. In certain applications, faster degradation of alginate matrices is desirable which can be attained by loading alginate lyase (in a dose-dependent manner) along with encapsulated cells (Campbell et al. 2018; Antunes et al. 2021). The ability to closely modulate the mechanical properties and 3D architecture of alginate also enables it to be used for creating modular scaffolds and create hierarchically structured patterns for more complex 3D vascular designs. Calcium alginate can also be degraded using ethylenediaminetetraacetic acid (EDTA), and this strategy can be exploited to form sacrificial scaffolds and templated 3D structures for various vascular applications.
8.4.5 Other Natural Materials
A few other emerging natural materials implemented for vascular tissue engineering and modeling of tumor angiogenesis include silk, chitosan, hyaluronic acid, and other GAG-based hydrogels. Although they are biocompatible and have low immunogenicity, the vasculo-mimetic potential is variable and often depends on the source of the material, molecular characteristics, and biochemical composition. Silk is primarily obtained from the cocoons of silkworms (mulberry or non-mulberry in origin). Silk fibroin is a promising protein-based biomaterial that has high hemocompatibility, excellent mechanical strength, and the ability to be molded into various shapes and sizes from nano-scale to centimeter-scale constructs (Blanco-Fernandez et al. 2021; Gupta and Mandal 2021). Silk fibroin has both amorphous and crystalline regions which transition from α-helix and random coil structure to β-sheets during isolation and processing. Additionally, sericin protein found in silk also acts as a glue to bind fibroin protein fibrils. Although sericin has been used to a lesser extent, it is primarily fibroin protein which is predominant for vascular applications (e.g., tissue-engineered vascular grafts, TEVGs) (Zamani et al. 2017; van Uden et al. 2019). Silk fibroin scaffolds or nanoparticles loaded with VEGF or heparin have been used extensively to enhance angiogenic repair in combination with various vascular cell types (ECs, SMC, ADSCs, and others) (Zamani et al. 2017; Zhang et al. 2018). The stiffness of silk-based hydrogels can be controlled by tuning initial polymer concentration, by combining with other natural or synthetic materials, or by inducing additional crosslinking of the tyrosine groups using horseradish peroxidase (HRP)/H2O2. In general, silk biomaterial is still in its nascent stages in terms of being applied for vascular tissue engineering (Gupta and Mandal 2021).
Chitosan, a linear polysaccharide, composed of repeating units of d-glucosamine and N-acetyl-d-glucosamine linked by β-(1,4) glycosidic bonds has often been used with other biomaterials to enhance vascularization and angiogenesis in the context of wound healing, fabrication of small diameter vascular grafts, and tissue engineered blood vessels. Chitosan has hydrophilic groups and is biocompatible and biodegradable with minimal immunogenicity. Additionally, it can be blended with a wide variety of natural and synthetic materials to improve mechanical properties, surface properties, in vivo stability, and vasculogenic potential of engineered constructs (Islam et al. 2020). Further, the processability of chitosan into various scale-spanning structures like nano/microparticles, flat layers, scaffolds and matrices, tubes and fibers helps in creating a wide range of desired vascular constructs (Deng et al. 2010; Badhe et al. 2017; Wang et al. 2020). Interestingly, chitosan has also been used to inhibit tumor angiogenesis through blocking of the VEGF signaling pathway as well as a drug carrier for several compounds that inhibit tumor angiogenesis and thereby tumor growth (Li et al. 2019b; Yadav et al. 2020).
Hyaluronic acid (HA), a linear glycosaminoglycan (GAG) polysaccharide, composed of d-glucuronic acid and N-acetyl-d-glucosamine linked by β-(1,4) glycosidic bonds is another popular choice for vascular tissue engineering. Although HA does not have any integrin binding sites, it has receptors for CD44 and receptor for HA-mediated motility (RHAMM). However, for encapsulation or culture of ECs, it is often necessary to incorporate vasculo-mimetic factors that engage directly for improved vascular signaling and morphogenesis. These factors include the RGD peptide sequence for improved cell adhesion, VEGF-mimetic peptide sequence, and conjugation with heparin/thiolated heparin for improved vasculogenesis. In addition, inclusion of MMP-sensitive peptide sequences and dynamic induction of hypoxia within hydrogels also helps improve vascularization (Shen et al. 2014; Lu et al. 2019; Natividad-Diaz et al. 2019). In previous studies, HA has also been chemically modified with other materials including collagen, chitosan, and poly(ε-caprolactone) (PCL) to create improved scaffolds for vascularization (Vignesh et al. 2018; Kang et al. 2019; Li et al. 2019a). While using HA, it is necessary to optimize the molecular weight of the polymer chains and viscoelasticity of the resulting scaffold, as these play important roles in determining spreading, adhesion, and vascular morphogenesis of ECs.
8.4.6 Poly(ethylene Glycol)
Poly(ethylene glycol) (PEG) is a synthetic linear or multi-arm polymer that serves as a “blank slate” on which various biochemical modifications can be made to make it suitable for vascular applications. Although PEG by itself does not have any bioactive sites required for cell adhesion or degradation, it can be modified by chemical conjugation with various cell-binding and proteolytically degradable peptide sequences, ECM proteins, growth factors, and hormones to produce bioactive and bioresponsive scaffolds (Moore and West 2019). Multi-arm PEG chains provide the added advantage of covalently conjugating multiple bioactive moieties in the same macromolecular network. PEG-chains end-modified with diacrylate (DA) or dimethacrylate (DMA) groups can be covalently crosslinked via UV- or visible light-based photoinitiators or via click-based chemistries to form scaffolds and hydrogels (Zieris et al. 2010; Chwalek et al. 2015; Taubenberger et al. 2016). Further, by controlling the molecular weight, initial polymer concentration, and crosslinker concentration, the overall stiffness, porosity, and other microarchitectural features of PEG-based scaffolds can be tuned for the required cell type used. PEGDA hydrogels with RGD- and MMP-degradable peptide sequences have been used for vascular regeneration, in vitro, in vivo, and in PDMS-based microfluidic models to form patent lumen-like vessels that provide diffusive and convective mass transport to adjacent tissue space (Suresh and West 2020) (Fig. 8.3a). PEGDA hydrogels can also be modified by conjugation with photo-degradable peptide sequences that can be selectively degraded using light of specific wavelengths (or a laser source) to create patterned and user-guided vascular channels (Kloxin et al. 2009). Co-culture of human umbilical vein endothelial cells (HUVEC) and human vascular pericytes (HVP) with lung adenocarcinoma cells within a two-layered PEG-peptide based hydrogels demonstrated that proximity to vascular cells helped promote higher tumor growth in large, disorganized clusters (Roudsari et al. 2016). Overall, PEG-based scaffolds provide immense potential and opportunities for researchers to elucidate specific microenvironmental factors regulating vascular regeneration and tumor angiogenesis (Bray et al. 2015; Taubenberger et al. 2016).
Representative examples of synthetic/hybrid hydrogels used for vascular tissue engineering. (a) EPCs and HUVECs (red) co-cultured with SMCs (green) within PEG-based hydrogels with adhesive RGDS and MMP-sensitive peptide sequences after 14 days of culture form stable microvascular networks. Scale bar: 200 μm. Cells are stained for VE-Cadherin (green/red), connexin-32 gap junction (cyan), and nuclei (blue) (central panel) and endothelial nitric oxide synthase (eNOS, cyan) (bottom panel). Scale bar: 100 μm. Adapted from (Peters et al. 2016). (b) ECFCs (red) co-encapsulated with MSCs within GelMA hydrogels at varying cell densities as imaged on day 7 of culture forming rudimentary microvascular networks with hollow patent lumens. Scale bar: 100 μm (left), 20 μm (bottom right). Adapted from (Chen et al. 2012)
8.4.7 Poly(lactic-co-Glycolic Acid) and Poly(caprolactone)
Poly(lactic-co-glycolic acid) (PLGA), a co-polymer of lactic acid and glycolic acid, has been used a cheap alternative for various vascular tissue engineering applications due to its biocompatibility and biodegradability (Pan and Ding 2012). The rate of PLGA biodegradation (via hydrolytic cleavage of the ester bonds) can be controlled by tuning the relative ratios of the monomers used to form the PLGA scaffold. Although hydrophilic, PLGA by itself does not have any cell-adhesive ligands necessary for vascular cell attachment. Hence, it is often combined with other natural polymers (e.g., collagen, fibrin, silk) or specific peptide sequences (e.g., RGD) to promote cell adhesion and spreading (Shin et al. 2017). PLGA is often molded into microspheres and nanoparticles for controlled released of vascular growth factors (e.g., VEGF, BMP-2) that promote vascular regeneration and wound healing (Golub et al. 2010). PLGA can also be molded into electrospun scaffolds with tunable microarchitectural properties (e.g., fiber thickness, alignment, porosity), and in conjunction with other cell-adhesive materials, be used to make small-diameter vascular grafts and porous scaffolds (Han et al. 2011). Incorporation of growth factor loaded-PLGA microspheres within larger scaffolds also helps in recruitment of ECs seeded on the scaffold surface, thereby mimicking angiogenic growth in 3D microenvironments.
Similar to PLGA, poly(ε-caprolactone) (PCL) is another biodegradable polyester that is employed as small diameter vascular grafts and bioactive scaffolds for vascular regeneration. By combining with other materials, including fibrin, collagen, silk, chitosan, PLA, PVA, and others, controlled release of vascular growth factors, and by fabricating into molded structures, including electrospun fibers, multi-layered scaffolds, PCL can be used for a wide variety of applications involving vasculogenesis and angiogenesis (Fuchs et al. 2009; Singh et al. 2011; Gniesmer et al. 2019).
8.4.8 Hybrid Hydrogels
In order to overcome the limitations of natural and synthetic matrices, hybrid hydrogels have been developed comprising multiple natural and synthetic components that provide a wider range of bioactive cues to encapsulated ECs, thereby promoting vasculogenic and angiogenic processes. Since natural materials are mechanically weak and susceptible to rapid degradation in vivo, and synthetic materials lack the wide range of biochemical cues necessary for vascular functionalization, it is beneficial to develop hybrid materials that incorporate the “best of both worlds” and thereby provide optimized and tunable microenvironments necessary for vascular growth and development.
Some of these include protein-based materials (gelatin, collagen, silk, Matrigel, and others) that are functionalized with synthetic side/end-groups to provide additional cross-link sites that increase the overall mechanical strength of the fabricated scaffolds (Fig. 8.3b). Proteins can also be blended with synthetic polymers to improve mechanical properties of hybrid hydrogels provided there is no molecular level phase separation between different macromolecules. Protein-mimetic or protein-derived peptide sequences (e.g., collagen-mimetic peptide, VEGF-mimetic peptide, and self-assembling peptides) can be incorporated into polymer-based hydrogels to provide additional biochemical or biophysical signaling cues required for ECs (Jia and Kiick 2009; Singh et al. 2013; Klotz et al. 2019; Kim et al. 2020).
In addition to proteins, carbohydrate polymers including dextran, alginate, and hyaluronic acid can also be functionalized with synthetic groups to improve structural and functional properties of scaffolds. Methacrylate groups covalently coupled to hyaluronic acid and dextran have been used to create methacrylated HA (MeHA) and methacrylated dextran (DexMA), respectively, (Möller et al. 2007; Jin et al. 2010; Liu and Chan-Park 2010; Eke et al. 2017; Lu et al. 2022). In these polymers, choosing the optimum molecular weight and degree of crosslink is critical to ensuring success in vascularization strategies. Too high molecular weight polymer chains can increase the matrix viscoelasticity through chain entanglements that may hinder vascular migration, network formation, and vessel branching. Too low molecular weight polymer chains may cause inflammatory responses and dysfunctional behavior in encapsulated or seeded cells. Similarly, degree of crosslink determines the matrix porosity, stiffness, and overall permissivity towards vascular growth and spreading. MeHa and DexMA can be used in ratiometric combinations with gelatin to form interpenetrating polymer networks (IPNs) that promote vascularization.
Overall, a wide range of polymeric biomaterials are available for tissue revascularization and for modeling tumor angiogenesis. Although various materials-chemistry based methods have been developed to create improved scaffolds, novel innovations are under way to improve hemocompatibility of scaffolds and matrices, create stable and long-lasting vasculature, incorporate tissue-specific vascular and stromal cells, and to fabricate functionally consistent vascularized constructs. In addition, hydrogel-based scaffolds for modeling of tumor angiogenesis have also been developed in an effort to understand cancer-vascular crosstalk, disrupt tumor angiogenic signaling and thereby prevent vascular growth.
8.5 Biofabrication Strategies for Vasculogenesis and Angiogenesis
Developing in vitro vascular models requires not only the selection of the appropriate biomaterial but also the optimization of various fabrication and processing techniques that integrate the cells and the biomaterial to create structurally and functionally stable vascularized constructs. In this regard, various chemical, mechanical, and optical processing techniques have been developed including self-assembly, bioprinting, micromolding, photolithography, and laser-based techniques, amongst others (Bajaj et al. 2014; Moroni et al. 2018; Pradhan et al. 2020). These techniques are either additive or subtractive in nature. Additive techniques (3D bioprinting, stereolithography, electrospinning, etc.) include step-by-step controlled addition of cell/biomaterial mixture to the growing mass of the final construct that is regulated by photo/thermal/chemical crosslinking. Additive techniques are useful for creating well-designed scaffolds in a high-throughput fashion with good degree of repeatability. Subtractive techniques (laser-based degradation, sacrificial micromolding, etc.) include subjecting a bulk scaffold to optical/chemical treatment that removes controlled volume of material from the scaffold leaving behind a network of porous structures that can be readily occupied by vascular cells to form the vasculature. This approach helps attain finer resolution vascular networks compared to additive bulk processing techniques, but its throughput is much less.
Depending on the end-application, the user must optimize between speed/fabrication throughput, resolution, and complexity of the vascular structure, and reproducibility of the vascularized structures. In some tissue engineering applications (e.g., tissue vascularization and wound healing), fabrication speed and time are more critical than resolution. However, in other applications involving disease modeling and mechanistic studies (e.g., tumor angiogenesis, vascular dysfunction), resolution, architectural complexity, and repeatability are more important. Some of these techniques are discussed in more detail below (Table 8.3).
8.5.1 Self-Assembly
The technique of self-assembly primarily involves 3D encapsulation of vascular cells within hydrogel-based scaffolds and reliance on cellular migration and morphogenesis to form 3D interconnected vascular networks (Blinder et al. 2016) (Fig. 8.4a). Alternatively, cells seeded on top of a 3D scaffold can also migrate inwards into the material to form vascular protrusions and neo-vessel like formations, reminiscent of angiogenic growth. In this approach, both the material micro- and macro-scale properties as well as the cellular features (cell density, migration potential, etc.) are important considerations to achieve optimum vascularization. Higher cell density leads to faster interconnections between encapsulated cells and better anastomoses between the neovessels. As the cells tunnel through the matrix to connect with their neighboring cells, the matrix compliance and permissiveness determine the efficiency of the process. If the matrix is nanoporous or poorly degradable, it is challenging for encapsulated vascular cells to form lumenized networks, and they eventually regress and die. Since this technique is highly dependent on the migration potential of the cells and is stochastic in nature, several strategies have been developed to improve and accelerate the self-assembly process.
Representative biofabrication techniques for construction of vascularized tissues. (a) Schematic of the dynamic vascular self-assembly process of HUVECs and HNDFs in a fibrin gel loaded in macroporous PLLA/PLGA scaffold over 7 days in culture. Adapted from (Blinder et al. 2016). (b) Schematic of the coaxial extrusion bioprinting of perfusable patent 3D vascular structures and HUVECs stained for characteristic markers (CD31: red; VE-Cadherin: green; nuclei: blue) demonstrating patent lumen and sprouting microvessels after 7 days. Scale bar: 100 μm. Adapted with permission from (Gao et al. 2018). (c) Electrospun PCL scaffolds of controlled spacing coated with fibronectin and seeded with HUVECs and fibroblasts and stacked with cell-accumulation technology to create thick vascularized constructs with contact-guidance patterned oriented vascular networks. Scale bar: 200 μm. Adapted with permission from (Bertlein et al. 2018)
The most facile strategy to alter matrix microarchitecture is to control the degree of crosslinking either by controlling polymer concentration, crosslinker concentration, or changing pH/temperature during crosslinking process to tune the scaffold porosity, fiber density, fiber thickness, pore size, etc. (Cross et al. 2010; McCoy et al. 2018). Matrix porosity can also be altered by employing techniques like gas foaming, salt leaching, lyophilization or sacrificial molding (Harris et al. 1998; Ford et al. 2006). Gas foaming involves fabrication of scaffolds under high pressure with non-reactive gases (e.g., carbon dioxide), which is released at the end to leave behind macroporous hydrogel scaffolds that permit cell spreading and migration. Salt leaching involves soluble porogens (e.g., sodium chloride) that are added along with the polymer precursor at specific concentration. After completion of crosslinking, the porogens leach out into the surrounding buffer leaving behind voids and pores in the scaffold. Freeze-drying/lyophilization of polymer scaffolds is also used to create highly porous constructs. Alternately, thermo-sensitive polymers (e.g., gelatin, dextran) can also be incorporated within scaffolds in the form of microspheres or other intricate structures, which can later melt and dissolve away leaving behind templated pores and channels within the crosslinked polymer scaffolds. In recent developments, macroporous scaffolds have been achieved through annealing polymeric microspheres of various sizes to form larger scaffolds so that seeded cells can migrate through the void spaces between the microspheres and connect with neighboring cells (Griffin et al. 2015). The size of the microspheres determines the void fraction and porosity of the overall scaffold, while the stiffness and surface adhesivity of the microspheres determine the level of cell-matrix engagement through the void volumes.
Co-encapsulation of supporting vascular cell types like fibroblasts, MSCs, and pericytes along with ECs also helps accelerate and stabilize the vascular network formation, as these mural cells provide the initial tunneled paths within the matrix which is followed by the ECs to form lumenized networks (Peters et al. 2016). In case of modeling tumor angiogenesis, the most common strategy is to provide a gradient of biochemical or biophysical cues that enables ECs to form sprouting vasculature through chemotaxis or durotaxis, respectively (Kim et al. 2015). The biochemical gradient can be induced through various growth or angiogenic factors that are either encoded within the matrix or through simple diffusion. Biophysical cues can be incorporated through strain-assisted stretching and alignment of fibrillar components of the matrix/scaffold which enables encapsulated cells to directionally migrate along the aligned fibers and form aligned vascular networks (McCoy et al. 2018). Overall, multiple biochemical, biophysical, and meso-scale materials processing techniques have greatly improved the vascularization potential and performance of scaffolds towards guided self-assembly of vascular networks.
8.5.2 Bioprinting
Three-dimensional (3D) bioprinting has emerged as one of the most popular choices for high-throughput, repeatable, and reliable techniques for the fabrication of vascularized constructs. Although various types of 3D bioprinting (e.g., ink-jet/droplet, valve-jet) have been developed, the most prominent technique is extrusion-based bioprinting/bioplotting which involves controlled dispensing of cell-polymer mixture in a 3D volume which is then crosslinked to form an integrated scaffold (Fig. 8.4b). Most major vascularization applications have adopted extrusion-printing owing to its ability to fabricate at high speed, high resolution, low cell damage and toxicity, ability to print intricate and complex patterns, and suitability with a wide range of bioinks. Considering that tissue engineered vascularized scaffolds are usually millimeter- to centimeter-scale thick, this approach ensures that highest efficiency in terms of speed and resolution achievable.
The bioink used for extrusion-printing needs to be carefully selected and optimized for the cell type as well as for the printing process itself (Ouyang et al. 2017). The viscosity of the hydrogel precursor to be used as the bioink, its temperature-sensitivity, and the shear forces experienced by the cells during extrusion through the nozzle need to be carefully monitored to optimize the process. If the bioink is thermally-crosslinked, the dispensing rate needs to be controlled to allow sufficient time for the extruded material to crosslink before further material can be added on top of it to create hierarchical structures. This approach can slow down the overall throughput; hence, researchers have explored other avenues, including shear-thinning, self-healing hydrogels, or rapidly photocrosslinkable hydrogels as potential bioinks. MeHA hydrogels with adamantane and β-cyclodextrin groups which employ the guest-host bonding chemistry and which can be further photocrosslinked using UV light have been used as a potential bioink (Ouyang et al. 2016, 2017). The bioinks used can either be pre-photocrosslinked and dispensed to maintain patency of the structure, or photocrosslinked during the dispensing process itself to ensure structural integrity with the fabricated scaffold. The dispensing mechanism can itself be fluidically controlled to obtain various morphologies of the extruded material including linearly uniform fibers, core-shell fibers, and hollow core fibers.
In recent developments, the bioprinting process can be achieved by extruding the bioink within a gel-like support medium composed of granular particles (e.g., gelatin, Carbopol) (Bhattacharjee et al. 2015; Hinton et al. 2015). As the nozzle-head moves through the support bath and extrudes the bioink, the local region is temporarily fluidized and holds the extruded material in place after the nozzle moves away. After the entire structure is printed in 3D, the support bath is dissolved or melted to extract the 3D printed material. This process enables creation of relatively high resolution and hierarchically complex vascular patterns in 3D volumes. In an inverse approach, sacrificial bioinks (composed of water-soluble dextran, etc.) can be printed into 3D vascular-mimetic templates, which can then be encapsulated within polymeric hydrogel scaffolds and the dextran template is dissolved away to leave behind a vascular channel-based network (Miller et al. 2012). Thus, multiple approaches to 3D bioprinting have been developed to create more defined, patterned, and user-guided large-scale vascularized constructs for various tissue engineering applications.
8.5.3 Electrospinning
Similar to extrusion-bioprinting, electrospinning is another technique that is used to produce nano- to micron-scale polymer fibers that are integrated to form larger porous scaffolds. However, these fibers are produced via application of an electric field which can be tuned to vary the dimensions of the fibers formed. The polymer biomaterial chosen for this technique needs to be electrically conductive (e.g., PCL, PVA amongst others), have low surface tension and sufficiently high viscosity to be spun into fibers. The polymer melt or polymer-solvent solution is subjected to an electrical field within a nozzle, which when it overcomes the surface tension of the liquid, generates a stream of liquid jet. The dried liquid jet is collected in the form of fibers on a rotating mandrel to obtain electrospun mats. Both the polymer solution properties as well as the operating parameters can be tuned to obtain fibers of various thickness and alignment degree.
Highly aligned electrospun scaffolds help in directional migration of seeded vascular cells and improve network connectivity (Ahn et al. 2015; Bertlein et al. 2018) (Fig. 8.4c). The inter-fiber spacing should be tuned in a way to allow optimized matrix porosity, cellular migration and motility, and overall matrix stiffness to ensure accelerated vascularization. The overall stiffness of electrospun scaffolds arises from the stiffness of individual fibers (determined by initial polymer concentration and molecular weight) and the relative density, thickness, and alignment of fibers in the scaffold. Thicker fibrils enable higher matrix stiffness but reduced porosity, while thinner fibrils allow higher porosity and contact-guidance based cellular migration. Consequently, this technique is particularly suited to study the role of contact-guidance based endothelial migration and spreading. In studies of tumor angiogenesis, where surrounding ECs exploit the biophysical matrix cues to preferentially grow and migrate towards the central tumor mass, electrospun scaffolds of varying fiber thickness, spacing, stiffness and alignment can help elucidate the mechanisms of such contact guidance-based migration. Overall, electrospinning is one of the key techniques that can exploit the cell-matrix biophysical engagement and thereby enable studies of vascular migration and broader tissue vascularization.
8.5.4 Micromolding
Traditional soft lithography approaches including micromolding have been used extensively as a facile technique for making large- to small-scale vascular channels within large biomaterial scaffolds. The most common material used for this purpose is poly(dimethyl siloxane) (PDMS) which can be poured and molded into a wide variety of shapes and sizes on negative masters and thermally cured to obtain positive molds. These PDMS molds can then be used as templates by encapsulating them within biomaterial/hydrogel scaffold of choice and physical removal of the mold to obtain vessel-like structures of the desired template (Jiménez-Torres et al. 2016). PDMS is widely preferred due to its moldability, flexibility, facile handling and low cytotoxicity post removal from the hydrogel scaffold. However, other materials, including metal wires, viscoelastic fluids, ice, and others, can also be used as templating agents to obtain vascular networks of choice (Chrobak et al. 2006; de Graaf et al. 2019; Wang et al. 2019). This technique is limited by some inherent challenges like resolution (inability to obtain micron-scale small features), large number of handling steps involved, and inability to obtain hierarchically complex structures, although some advances have been made in these respects for obtaining vascularized constructs. However, once the workflow has been optimized based on process parameters, this technique can be scaled up easily and enable highly reproducible scaffolds with in-laden vascular channels. Hence, it is also a popular choice for making organ-on-chip or microfluidics-based devices which are used extensively for a wide range of in vitro vascular studies.
8.5.5 Photolithography and Laser-Based Techniques
Photolithography-based techniques depend on the manipulation of light as it is projected on a 3D volume of biomaterial/hydrogel precursor to obtain desired features in the final fabricated scaffold. Photolithography enables fabrication of highly complex patterns with high resolutions and relatively high speeds by controlling the light path as it traverses the polymer mixture to photocrosslink into solid scaffolds. Depending on the mode of operation, it can be classified into mask-based photolithography, stereolithography, and laser-based lithography. Mask-based photolithography involves placing photomasks of defined features in the light path and selectively allowing light to expose certain areas/volumes of the polymer precursor to crosslink it (Aubin et al. 2010; Kazemzadeh-Narbat et al. 2017). Although facile, it is limited in terms of resolution and complexity of the vascular patterns achievable at increasing depths as the projected light gets diffused while traversing through the 3D volume. The use of photoabsorbers in the polymer precursor can mitigate the optical dispersal to a certain extent. Inversely, using an optical diffuser helps achieve feature height gradation that improves the resolution of the complex vascular patterns.
Stereolithography, also called maskless photolithography, involves manipulation of projected light using an array of mirrors (digital mirror device, DMD) that can be guided and controlled through a computer-aided design (CAD) software. This approach allows digital light projection in a dynamic fashion in a layer-by-layer fashion where each thin section of the polymer precursor volume is crosslinked by bringing it into focus with the projected light. Once crosslinking is complete, the next layer is brought into focus with an altered projected light path and the process continues until the entire scaffold is fabricated to its last layer. This approach provides the advantages of building higher resolution features one layer at a time to create intricate, complex, and tortuous vascular patterns with a high degree of spatiotemporal control. By optimizing the type and chemistry of the photocrosslinkers used, relatively high speeds can be achieved to obtain centimeter-scale vascularized constructs (Zhang and Larsen 2017; Zhu et al. 2017; Grigoryan et al. 2019).
Laser-based photolithography depends on the ability of coherent light beam of specific wavelength and power to penetrate a given 3D volume of a polymer precursor and initiate photocrosslinking to form fabricated scaffolds with highly defined and localized patterns (Aizawa et al. 2010). The spatial coherence of the laser beam, obtained through nano- to femto-scale pulses, combined with a two-photon (2P) microscopy platform enables delivery of light energy to specific points in a 3D volume with high degree of lateral and axial resolution and this enables creation of image-guided patterned hydrogels for highly specific and repeatable applications. The polymer precursor chosen for the application can be made to be responsive at specific wavelengths either through chemical modification of the backbone or via appropriate photocrosslinkers. Vascular patterns obtained from 2D/3D scans of in vivo/patient samples can be digitally processed and recreated to obtain in vitro laser-guided patterns in 3D hydrogel volumes with high fidelity (Culver et al. 2012). Although highly precise structures can be achieved through the technique, it is limited in terms of speed and throughput owing to the 3D scanning rates of the laser and microscopy system. Hence, scale-up of this technique to large areas/volumes is currently limited and the fabricated scaffolds are primarily used for mechanistic studies of vasculogenesis and tumor angiogenesis.
Alternate to additive methods, laser-based techniques can be used for subtractive fabrication of hydrogels scaffolds as well. A large-volume, prefabricated hydrogel scaffold can be degraded in a user-defined, image-guided manner to form interconnected and highly precise vascular network with high degree of fidelity to the original vascular pattern. This can be achieved by optimizing the fluence, power, and pulse duration of the laser source combined with 2P-microscopy to generate microchannels through laser-induced photocavitation of water molecules present within the polymer scaffold (Brandenberg and Lutolf 2016; Heintz et al. 2016). Another approach is to use polymers with encoded photocleavable moieties that can undergo chemical scission under exposure to lasers of specific wavelength (Arakawa et al. 2017). This approach vastly improves the speed of the fabrication process as the scission and photocavitation occur at much faster rates compared to the scanning speed of the laser and microscopy stage itself. Thermally crosslinked hydrogels can also be laser-degraded by incorporation of heat-absorbing gold nanorods/nanoparticles which can locally melt the polymer macromolecules upon laser excitation and heating (Hribar et al. 2015).
Overall, several novel biofabrication technologies, coupled with biochemical and biophysical modifications of biomaterials/hydrogels, have been developed to construct vascularized scaffolds for a wide range of applications. Based on the end need, various operational parameters including speed, resolution, scalability of the fabrication processes need to be optimized. Although some techniques like self-assembly and 3D bioprinting produce scaffolds with high degree of scalability and throughput which may be suitable for in vivo implantation, the process is stochastic and may vary between different materials and different cell types. On the other hand, laser-based techniques produce highly precise vascularized scaffolds that may not be scalable but can be used for mechanistic investigation of disease progression, including mechanisms of tumor angiogenesis.
8.6 Conclusions
Hydrogels, owing to their versatility, moldability, ease of handling and processing, and relatively low cost, have become a popular choice of biomaterial for a wide range of vascular tissue engineering applications. Their biocompatibility with multiple vascular cell types and hemocompatibility with existing vasculature enables their translation towards regenerative medicine. In recent times, there has been an increasing need to create vascularized thick tissues with high degree of patency, structural and functional stability as well as architectural complexity. Although various biofabrication techniques have been developed to address this need, further improvements are necessary to match the required resolution while maintaining efficient fabrication speed at scale. In addition to cardiovascular system, the synthetic generation and modeling of the lymphatic system has gained attention due to critical role of lymphatics in interstitial fluid clearance and dynamic transport. It is hoped that with the continued discovery of new biomaterials, as well as novel advances in biophysical and biochemical modifications to existing ones, a wider repertoire of biomaterials will be available for individualized and specific applications.
The domain of tumor angiogenesis has also received impetus with the implementation of hydrogel-based vascularized scaffolds. Particularly, with the development of lab-on-a-chip/organ-on-a-chip devices, it has become possible to integrate hydrogel-based scaffolds with microfluidic systems to study mechanisms of cancer cell-endothelial cell crosstalk and investigate angiogenic growth of tumors. By tuning hydrogel properties, the cellular functional and morphological responses that mediate tumor angiogenesis can be studied, and the results gained thereof can be even extended towards other angiogenic processes in the body. These integrated systems can pave the way for testing pre-clinical efficiency of candidate anti-angiogenic drugs and provide valuable data that would be too expensive to obtain from animal models. In the future, these hydrogel-based tissue mimics are expected to be widely implemented for various biomedical applications.
Abbreviations
- 2D:
-
Two-dimensional
- 2P:
-
Two-photon
- 3D:
-
Three-dimensional
- ADSC:
-
Adipose-derived stromal cell
- Ang2:
-
Angiopoietin-2
- BBB:
-
Blood-brain barrier
- bFGF:
-
Basic fibroblast derived factor
- BM:
-
Basement membrane
- BMP-2:
-
Bone morphogenetic protein-2
- CAD:
-
Computer-aided design
- DA:
-
Diacrylate
- DexMA:
-
Methacrylated dextran
- DMA:
-
Dimethacrylate
- DMD:
-
Digital mirror device
- ECFC:
-
Endothelial colony forming cell
- ECM:
-
Extracellular matrix
- ECs:
-
Endothelial cells
- EDTA:
-
Ethylenediaminetetraacetic acid
- FN:
-
Fibronectin
- GAG:
-
Glycosaminoglycan
- HA:
-
Hyaluronic acid
- HIF-1α:
-
Hypoxia-inducible factor-1α
- HRP:
-
Horseradish peroxidase
- HUVEC:
-
Human umbilical vein endothelial cell
- HVP:
-
Human vascular pericyte
- IPN:
-
Interpenetrating polymer network
- LSEC:
-
Liver sinusoid endothelial cell
- MeHA:
-
Methacrylated hyaluronic acid
- MMP:
-
Matrix metalloproteinase
- MSC:
-
Mesenchymal stem/stromal cell
- NHDF/HNDF:
-
Normal human dermal fibroblasts
- PCL:
-
Poly(ε-caprolactone)
- PDGF-BB:
-
Platelet derived growth factor BB
- PDMS:
-
Poly(dimethylsiloxane)
- PEG:
-
Poly(ethylene glycol)
- PEGDA:
-
Poly(ethylene glycol diacrylate)
- PLGA:
-
Poly(lactic-co-glycolic acid)
- PVA:
-
Polyvinyl alcohol
- RGD:
-
Arginine-glycine-aspartate
- RHAMM:
-
Receptor for HA-mediated motility
- RPE:
-
Retinal pigment epithelial
- SMC:
-
Smooth muscle cell
- TEC:
-
Tumor-(associated) endothelial cell
- TEVG:
-
Tissue-engineered vascular grafts
- TME:
-
Tumor microenvironment
- VE-Cadherin:
-
Vascular endothelial cadherin
- VEGF:
-
Vascular endothelial growth factor
References
Ahn H et al (2015) Engineered small diameter vascular grafts by combining cell sheet engineering and electrospinning technology. Acta Biomater 16:14–22. https://doi.org/10.1016/j.actbio.2015.01.030
Aisenbrey EA, Murphy WL (2020) Synthetic alternatives to Matrigel. Nat Rev Mater 5(7):539–551. https://doi.org/10.1038/s41578-020-0199-8
Aizawa Y, Wylie R, Shoichet M (2010) Endothelial cell guidance in 3D patterned scaffolds. Adv Mater 22(43):4831–4835. https://doi.org/10.1002/adma.201001855
Akhtar N, Dickerson EB, Auerbach R (2002) The sponge/Matrigel angiogenesis assay. Angiogenesis 5(1–2):75–80. https://doi.org/10.1023/a:1021507031486
Andrée B et al (2019) Formation of three-dimensional tubular endothelial cell networks under defined serum-free cell culture conditions in human collagen hydrogels. Sci Rep 9(1):5437. https://doi.org/10.1038/s41598-019-41985-6
Antunes M et al (2021) Development of alginate-based hydrogels for blood vessel engineering. Mater Sci Eng C 134:112588. https://doi.org/10.1016/j.msec.2021.112588
Arakawa CK et al (2017) Multicellular vascularized engineered tissues through user-programmable biomaterial photodegradation. Adv Mater 29(37):1703156. https://doi.org/10.1002/adma.201703156
Athirasala A et al (2017) A novel strategy to engineer pre-vascularized full-length dental pulp-like tissue constructs. Sci Rep 7(1):3323. https://doi.org/10.1038/s41598-017-02532-3
Aubin H et al (2010) Directed 3D cell alignment and elongation in microengineered hydrogels. Biomaterials 31(27):6941–6951. https://doi.org/10.1016/j.biomaterials.2010.05.056
Auger FA, Gibot L, Lacroix D (2013) The pivotal role of vascularization in tissue engineering. Annu Rev Biomed Eng 15(1):177–200. https://doi.org/10.1146/annurev-bioeng-071812-152428
Badhe RV et al (2017) A composite chitosan-gelatin bi-layered, biomimetic macroporous scaffold for blood vessel tissue engineering. Carbohydr Polym 157:1215–1225. https://doi.org/10.1016/j.carbpol.2016.09.095
Bajaj P et al (2014) 3D biofabrication strategies for tissue engineering and regenerative medicine. Annu Rev Biomed Eng 16(1):247–276. https://doi.org/10.1146/annurev-bioeng-071813-105155
Barrs RW et al (2021) Engineering a chemically defined hydrogel bioink for direct bioprinting of microvasculature. Biomacromolecules 22(2):275–288. https://doi.org/10.1021/acs.biomac.0c00947
Bertlein S et al (2018) Development of endothelial cell networks in 3D tissues by combination of melt electrospinning writing with cell-accumulation technology. Small 14(2):1701521. https://doi.org/10.1002/smll.201701521
Bhattacharjee T et al (2015) Writing in the granular gel medium. Sci Adv 1(8):e1500655. https://doi.org/10.1126/sciadv.1500655
Blanco-Fernandez B et al (2021) Proteinaceous hydrogels for bioengineering advanced 3D tumor models. Adv Sci 8(4):2003129. https://doi.org/10.1002/advs.202003129
Blinder YJ et al (2016) Vasculogenic dynamics in 3D engineered tissue constructs. Sci Rep 5(1):17840. https://doi.org/10.1038/srep17840
Brandenberg N, Lutolf MP (2016) In situ patterning of microfluidic networks in 3D cell-laden hydrogels. Adv Mater 28(34):7450–7456. https://doi.org/10.1002/adma.201601099
Bray LJ et al (2015) Multi-parametric hydrogels support 3D in vitro bioengineered microenvironment models of tumour angiogenesis. Biomaterials 53:609–620. https://doi.org/10.1016/j.biomaterials.2015.02.124
Campbell KT, Stilhano RS, Silva EA (2018) Enzymatically degradable alginate hydrogel systems to deliver endothelial progenitor cells for potential revasculature applications. Biomaterials 179:109–121. https://doi.org/10.1016/j.biomaterials.2018.06.038
Celie K-B et al (2019) Microstructured hydrogel scaffolds containing differential density interfaces promote rapid cellular invasion and vascularization. Acta Biomater 91:144–158. https://doi.org/10.1016/j.actbio.2019.04.027
Chang WG, Niklason LE (2017) A short discourse on vascular tissue engineering. NPJ Regen Med 2(1):1–8. https://doi.org/10.1038/s41536-017-0011-6
Charbonier FW, Zamani M, Huang NF (2019) Endothelial cell mechanotransduction in the dynamic vascular environment. Adv Biosyst 3(2):1800252. https://doi.org/10.1002/adbi.201800252
Chen Y-C et al (2012) Functional human vascular network generated in photocrosslinkable gelatin methacrylate hydrogels. Adv Funct Mater 22(10):2027–2039. https://doi.org/10.1002/adfm.201101662
Chiu LLY et al (2012) Perfusable branching microvessel bed for vascularization of engineered tissues. Proc Natl Acad Sci 109(50):E3414–E3423. https://doi.org/10.1073/pnas.1210580109
Chrobak KM, Potter DR, Tien J (2006) Formation of perfused, functional microvascular tubes in vitro. Microvasc Res 71(3):185–196. https://doi.org/10.1016/j.mvr.2006.02.005
Chwalek K et al (2015) Glycosaminoglycan-based hydrogels to modulate heterocellular communication in in vitro angiogenesis models. Sci Rep 4(1):4414. https://doi.org/10.1038/srep04414
Cross VL et al (2010) Dense type I collagen matrices that support cellular remodeling and microfabrication for studies of tumor angiogenesis and vasculogenesis in vitro. Biomaterials 31(33):8596–8607. https://doi.org/10.1016/j.biomaterials.2010.07.072
Culver JC et al (2012) Three-dimensional biomimetic patterning in hydrogels to guide cellular organization. Adv Mater 24(17):2344–2348. https://doi.org/10.1002/adma.201200395
de Graaf MNS et al (2019) Scalable microphysiological system to model three-dimensional blood vessels. APL Bioeng 3(2):026105. https://doi.org/10.1063/1.5090986
Deng C et al (2010) A collagen–chitosan hydrogel for endothelial differentiation and angiogenesis. Tissue Eng A 16(10):3099–3109. https://doi.org/10.1089/ten.tea.2009.0504
Ding Z et al (2019) Injectable silk nanofiber hydrogels for sustained release of small-molecule drugs and vascularization. ACS Biomater Sci Eng 5(8):4077–4088. https://doi.org/10.1021/acsbiomaterials.9b00621
DiVito KA et al (2017) Microfabricated blood vessels undergo neoangiogenesis. Biomaterials 138:142–152. https://doi.org/10.1016/j.biomaterials.2017.05.012
Dudley AC (2012) Tumor endothelial cells. Cold Spring Harb Perspect Med 2(3):a006536–a006536. https://doi.org/10.1101/cshperspect.a006536
Eke G et al (2017) Development of a UV crosslinked biodegradable hydrogel containing adipose derived stem cells to promote vascularization for skin wounds and tissue engineering. Biomaterials 129:188–198. https://doi.org/10.1016/j.biomaterials.2017.03.021
Ford MC et al (2006) A macroporous hydrogel for the coculture of neural progenitor and endothelial cells to form functional vascular networks in vivo. Proc Natl Acad Sci 103(8):2512–2517. https://doi.org/10.1073/pnas.0506020102
Fuchs S et al (2009) Contribution of outgrowth endothelial cells from human peripheral blood on in vivo vascularization of bone tissue engineered constructs based on starch polycaprolactone scaffolds. Biomaterials 30(4):526–534. https://doi.org/10.1016/j.biomaterials.2008.09.058
Gaebel R et al (2011) Patterning human stem cells and endothelial cells with laser printing for cardiac regeneration. Biomaterials 32(35):9218–9230. https://doi.org/10.1016/j.biomaterials.2011.08.071
Gao G et al (2018) Coaxial cell printing of freestanding, perfusable, and functional in vitro vascular models for recapitulation of native vascular endothelium pathophysiology. Adv Healthc Mater 7(23):1801102. https://doi.org/10.1002/adhm.201801102
Gniesmer S et al (2019) In vivo analysis of vascularization and biocompatibility of electrospun polycaprolactone fibre mats in the rat femur chamber. J Tissue Eng Regen Med 13(7):1190–1202. https://doi.org/10.1002/term.2868
Golub JS et al (2010) Sustained VEGF delivery via PLGA nanoparticles promotes vascular growth. Am J Physiol Heart Circ Physiol 298(6):H1959–H1965. https://doi.org/10.1152/ajpheart.00199.2009
Griffin DR et al (2015) Accelerated wound healing by injectable microporous gel scaffolds assembled from annealed building blocks. Nat Mater 14(7):737–744. https://doi.org/10.1038/nmat4294
Grigoryan B et al (2019) Multivascular networks and functional intravascular topologies within biocompatible hydrogels. Science 364(6439):458–464. https://doi.org/10.1126/science.aav9750
Guo H-F et al (2017) A simply prepared small-diameter artificial blood vessel that promotes in situ endothelialization. Acta Biomater 54:107–116. https://doi.org/10.1016/j.actbio.2017.02.038
Gupta P, Mandal BB (2021) Silk biomaterials for vascular tissue engineering applications. Acta Biomater 134:79–106. https://doi.org/10.1016/j.actbio.2021.08.004
Hackethal J et al (2021) Novel human placenta-based extract for vascularization strategies in tissue engineering. Tissue Eng Part C Methods 27(11):616–632. https://doi.org/10.1089/ten.tec.2021.0173
Han J et al (2011) Co-electrospun blends of PLGA, gelatin, and elastin as potential nonthrombogenic scaffolds for vascular tissue engineering. Biomacromolecules 12(2):399–408. https://doi.org/10.1021/bm101149r
Harris AL (2002) Hypoxia—a key regulatory factor in tumour growth. Nat Rev Cancer 2(1):38–47. https://doi.org/10.1038/nrc704
Harris LD, Kim BS, Mooney DJ (1998) Open pore biodegradable matrices formed with gas foaming. J Biomed Mater Res 42(3):396–402
Heintz KA et al (2016) Fabrication of 3D biomimetic microfluidic networks in hydrogels. Adv Healthc Mater 5(17):2153–2160. https://doi.org/10.1002/adhm.201600351
Highley CB, Rodell CB, Burdick JA (2015) Direct 3D printing of shear-thinning hydrogels into self-healing hydrogels. Adv Mater 27(34):5075–5079. https://doi.org/10.1002/adma.201501234
Hinton TJ et al (2015) Three-dimensional printing of complex biological structures by freeform reversible embedding of suspended hydrogels. Sci Adv 1(9):e1500758. https://doi.org/10.1126/sciadv.1500758
Hribar KC et al (2015) Three-dimensional direct cell patterning in collagen hydrogels with near-infrared femtosecond laser. Sci Rep 5(1):17203. https://doi.org/10.1038/srep17203
Ishihara M et al (2003) Controlled release of fibroblast growth factors and heparin from photocrosslinked chitosan hydrogels and subsequent effect on in vivo vascularization. J Biomed Mater Res A 64A(3):551–559. https://doi.org/10.1002/jbm.a.10427
Islam MM et al (2020) Chitosan based bioactive materials in tissue engineering applications—a review. Bioact Mater 5(1):164–183. https://doi.org/10.1016/j.bioactmat.2020.01.012
Jain RK (2003) Molecular regulation of vessel maturation. Nat Med 9(6):685–693. https://doi.org/10.1038/nm0603-685
James BD, Allen JB (2018) Vascular endothelial cell behavior in complex mechanical microenvironments. ACS Biomater Sci Eng 4(11):3818–3842. https://doi.org/10.1021/acsbiomaterials.8b00628
Jia X, Kiick KL (2009) Hybrid multicomponent hydrogels for tissue engineering: hybrid multicomponent hydrogels for tissue engineering. Macromol Biosci 9(2):140–156. https://doi.org/10.1002/mabi.200800284
Jiménez-Torres JA et al (2016) LumeNEXT: a practical method to pattern luminal structures in ECM gels. Adv Healthc Mater 5(2):198–204. https://doi.org/10.1002/adhm.201500608
Jin R et al (2010) Enzymatically-crosslinked injectable hydrogels based on biomimetic dextran-hyaluronic acid conjugates for cartilage tissue engineering. Biomaterials 31(11):3103–3113. https://doi.org/10.1016/j.biomaterials.2010.01.013
Juliar BA et al (2018) Sprouting angiogenesis induces significant mechanical heterogeneities and ECM stiffening across length scales in fibrin hydrogels. Biomaterials 162:99–108. https://doi.org/10.1016/j.biomaterials.2018.02.012
Kampmann A et al (2013) Additive effect of mesenchymal stem cells and VEGF to vascularization of PLGA scaffolds. Microvasc Res 90:71–79. https://doi.org/10.1016/j.mvr.2013.07.006
Kang L et al (2019) Hyaluronic acid oligosaccharide-modified collagen nanofibers as vascular tissue-engineered scaffold for promoting endothelial cell proliferation. Carbohydr Polym 223:115106. https://doi.org/10.1016/j.carbpol.2019.115106
Kayabolen A et al (2017) Native extracellular matrix/fibroin hydrogels for adipose tissue engineering with enhanced vascularization. Biomed Mater 12(3):035007. https://doi.org/10.1088/1748-605X/aa6a63
Kazemzadeh-Narbat M et al (2017) Engineering photocrosslinkable bicomponent hydrogel constructs for creating 3D vascularized bone. Adv Healthc Mater 6(10):1601122. https://doi.org/10.1002/adhm.201601122
Khoo CP, Micklem K, Watt SM (2011) A comparison of methods for quantifying angiogenesis in the Matrigel assay in vitro, https://home.liebertpub.com/tec. Mary Ann Liebert, Inc. 140 Huguenot Street, 3rd Floor New Rochelle, NY 10801 USA. https://doi.org/10.1089/ten.tec.2011.0150
Kim J et al (2015) Engineering of a biomimetic pericyte-covered 3D microvascular network. PLoS One 10(7):e0133880. https://doi.org/10.1371/journal.pone.0133880
Kim S, Pan C-C, Yang YP (2020) Development of a dual hydrogel model system for vascularization. Macromol Biosci 20(10):2000204. https://doi.org/10.1002/mabi.202000204
Kinoshita K et al (2016) Fabrication of multilayered vascular tissues using microfluidic agarose hydrogel platforms. Biotechnol J 11(11):1415–1423. https://doi.org/10.1002/biot.201600083
Kleinman HK, Martin GR (2005) Matrigel: basement membrane matrix with biological activity. Semin Cancer Biol 15(5):378–386. https://doi.org/10.1016/j.semcancer.2005.05.004
Klotz BJ et al (2019) A versatile biosynthetic hydrogel platform for engineering of tissue analogues. Adv Healthc Mater 8(19):1900979. https://doi.org/10.1002/adhm.201900979
Kloxin AM et al (2009) Photodegradable hydrogels for dynamic tuning of physical and chemical properties. Science 324(5923):59–63. https://doi.org/10.1126/science.1169494
Krock BL, Skuli N, Simon MC (2011) Hypoxia-induced angiogenesis. Genes Cancer 2(12):1117–1133. https://doi.org/10.1177/1947601911423654
Laschke MW et al (2008) Improvement of vascularization of PLGA scaffolds by inosculation of in situ-preformed functional blood vessels with the host microvasculature. Ann Surg 248(6):939–948. https://doi.org/10.1097/SLA.0b013e31818fa52f
Levenberg S et al (2005) Engineering vascularized skeletal muscle tissue. Nat Biotechnol 23(7):879–884. https://doi.org/10.1038/nbt1109
Li X et al (1994) Vascular smooth muscle cells grown on Matrigel. A model of the contractile phenotype with decreased activation of mitogen-activated protein kinase. J Biol Chem 269(30):19653–19658
Li X et al (2019a) Nanofiber-hydrogel composite–mediated angiogenesis for soft tissue reconstruction. Sci Transl Med 11(490):eaau6210. https://doi.org/10.1126/scitranslmed.aau6210
Li Y et al (2019b) Chitosan sulfate inhibits angiogenesis via blocking the VEGF/VEGFR2 pathway and suppresses tumor growth in vivo. Biomater Sci 7(4):1584–1597. https://doi.org/10.1039/C8BM01337C
Liu Y, Chan-Park MB (2010) A biomimetic hydrogel based on methacrylated dextran-graft-lysine and gelatin for 3D smooth muscle cell culture. Biomaterials 31(6):1158–1170. https://doi.org/10.1016/j.biomaterials.2009.10.040
Lu J et al (2019) Enhanced angiogenesis by the hyaluronic acid hydrogels immobilized with a VEGF mimetic peptide in a traumatic brain injury model in rats. Regen Biomater 6(6):325–334. https://doi.org/10.1093/rb/rbz027
Lu D et al (2022) Macroporous methacrylated hyaluronic acid hydrogel with different pore sizes for in vitro and in vivo evaluation of vascularization. Biomed Mater 17(2):025006. https://doi.org/10.1088/1748-605X/ac494b
Marcu R et al (2018) Human organ-specific endothelial cell heterogeneity. iScience 4:20–35. https://doi.org/10.1016/j.isci.2018.05.003
McCoy MG et al (2018) Collagen fiber orientation regulates 3D vascular network formation and alignment. ACS Biomater Sci Eng 4(8):2967–2976. https://doi.org/10.1021/acsbiomaterials.8b00384
McGuigan AP, Sefton MV (2006) Vascularized organoid engineered by modular assembly enables blood perfusion. Proc Natl Acad Sci 103(31):11461–11466. https://doi.org/10.1073/pnas.0602740103
McGuigan AP, Sefton MV (2007) Modular tissue engineering: fabrication of a gelatin-based construct. J Tissue Eng Regen Med 1(2):136–145. https://doi.org/10.1002/term.14
Michna R et al (2018) Vascularized microfluidic platforms to mimic the tumor microenvironment. Biotechnol Bioeng 115(11):2793–2806. https://doi.org/10.1002/bit.26778
Miller JS et al (2012) Rapid casting of patterned vascular networks for perfusable engineered three-dimensional tissues. Nat Mater 11(9):768–774. https://doi.org/10.1038/nmat3357
Millik SC et al (2019) 3D printed coaxial nozzles for the extrusion of hydrogel tubes toward modeling vascular endothelium. Biofabrication 11(4):045009. https://doi.org/10.1088/1758-5090/ab2b4d
Möller S et al (2007) Dextran and hyaluronan methacrylate based hydrogels as matrices for soft tissue reconstruction. Biomol Eng 24(5):496–504. https://doi.org/10.1016/j.bioeng.2007.08.014
Moon JJ et al (2010) Biomimetic hydrogels with pro-angiogenic properties. Biomaterials 31(14):3840–3847. https://doi.org/10.1016/j.biomaterials.2010.01.104
Moore EM, West JL (2019) Bioactive poly(ethylene glycol) acrylate hydrogels for regenerative engineering. Regen Eng Transl Med 5(2):167–179. https://doi.org/10.1007/s40883-018-0074-y
Morgan JT et al (2019) Fabrication of centimeter-scale and geometrically arbitrary vascular networks using in vitro self-assembly. Biomaterials 189:37–47. https://doi.org/10.1016/j.biomaterials.2018.10.021
Moroni L et al (2018) Biofabrication: a guide to technology and terminology. Trends Biotechnol 36(4):384–402. https://doi.org/10.1016/j.tibtech.2017.10.015
Muller S et al (2019) Human adipose stromal-vascular fraction self-organizes to form vascularized adipose tissue in 3D cultures. Sci Rep 9(1):7250. https://doi.org/10.1038/s41598-019-43624-6
Nakatsu MN et al (2003) Angiogenic sprouting and capillary lumen formation modeled by human umbilical vein endothelial cells (HUVEC) in fibrin gels: the role of fibroblasts and Angiopoietin-1☆. Microvasc Res 66(2):102–112. https://doi.org/10.1016/S0026-2862(03)00045-1
Natividad-Diaz SL et al (2019) A combined hiPSC-derived endothelial cell and in vitro microfluidic platform for assessing biomaterial-based angiogenesis. Biomaterials 194:73–83. https://doi.org/10.1016/j.biomaterials.2018.11.032
Nehls V, Drenckhahn D (1995) A novel, microcarrier-based in vitro assay for rapid and reliable quantification of three-dimensional cell migration and angiogenesis. Microvasc Res 50(3):311–322. https://doi.org/10.1006/mvre.1995.1061
Nehls V, Schuchardt E, Drenckhahn D (1994) The effect of fibroblasts, vascular smooth muscle cells, and pericytes on sprout formation of endothelial cells in a fibrin gel angiogenesis system. Microvasc Res 48(3):349–363. https://doi.org/10.1006/mvre.1994.1061
Nerem RM, Seliktar D (2001) Vascular tissue engineering. Annu Rev Biomed Eng 3(1):225–243. https://doi.org/10.1146/annurev.bioeng.3.1.225
Novosel EC, Kleinhans C, Kluger PJ (2011) Vascularization is the key challenge in tissue engineering. Adv Drug Deliv Rev 63(4–5):300–311. https://doi.org/10.1016/j.addr.2011.03.004
Ouyang L et al (2016) 3D printing of shear-thinning hyaluronic acid hydrogels with secondary cross-linking. ACS Biomater Sci Eng 2(10):1743–1751. https://doi.org/10.1021/acsbiomaterials.6b00158
Ouyang L et al (2017) A generalizable strategy for the 3D bioprinting of hydrogels from nonviscous photo-crosslinkable inks. Adv Mater 29(8):1604983. https://doi.org/10.1002/adma.201604983
Pan Z, Ding J (2012) Poly(lactide-co-glycolide) porous scaffolds for tissue engineering and regenerative medicine. Interface Focus 2(3):366–377. https://doi.org/10.1098/rsfs.2011.0123
Peters EB et al (2016) Poly(ethylene glycol) hydrogel scaffolds containing cell-adhesive and protease-sensitive peptides support microvessel formation by endothelial progenitor cells. Cell Mol Bioeng 9(1):38–54. https://doi.org/10.1007/s12195-015-0423-6
Pradhan S et al (2016) Polymeric biomaterials for in vitro cancer tissue engineering and drug testing applications. Tissue Eng Part B Rev 22(6):470–484. https://doi.org/10.1089/ten.teb.2015.0567
Pradhan S et al (2020) Biofabrication strategies and engineered in vitro systems for vascular mechanobiology. Adv Healthc Mater 9(8):1901255. https://doi.org/10.1002/adhm.201901255
Redd MA et al (2019) Patterned human microvascular grafts enable rapid vascularization and increase perfusion in infarcted rat hearts. Nat Commun 10(1):584. https://doi.org/10.1038/s41467-019-08388-7
Roudsari LC et al (2016) A 3D poly(ethylene glycol)-based tumor angiogenesis model to study the influence of vascular cells on lung tumor cell behavior. Sci Rep 6(1):32726. https://doi.org/10.1038/srep32726
Rouwkema J, Khademhosseini A (2016) Vascularization and angiogenesis in tissue engineering: beyond creating static networks. Trends Biotechnol 34(9):733–745. https://doi.org/10.1016/j.tibtech.2016.03.002
Sacchi V et al (2014) Long-lasting fibrin matrices ensure stable and functional angiogenesis by highly tunable, sustained delivery of recombinant VEGF164. Proc Natl Acad Sci 111(19):6952–6957. https://doi.org/10.1073/pnas.1404605111
Shen Y-I et al (2014) Hyaluronic acid hydrogel stiffness and oxygen tension affect cancer cell fate and endothelial sprouting. Biomater Sci 2(5):655. https://doi.org/10.1039/c3bm60274e
Shin YC et al (2017) RGD peptide and graphene oxide co-functionalized PLGA nanofiber scaffolds for vascular tissue engineering. Regen Biomater 4(3):159–166. https://doi.org/10.1093/rb/rbx001
Singh S, Wu BM, Dunn JCY (2011) Accelerating vascularization in polycaprolactone scaffolds by endothelial progenitor cells. Tissue Eng A 17(13–14):1819–1830. https://doi.org/10.1089/ten.tea.2010.0708
Singh RK, Seliktar D, Putnam AJ (2013) Capillary morphogenesis in PEG-collagen hydrogels. Biomaterials 34(37):9331–9340. https://doi.org/10.1016/j.biomaterials.2013.08.016
Slater JH et al (2011) Fabrication of multifaceted micropatterned surfaces with laser scanning lithography. Adv Funct Mater 21(15):2876–2888. https://doi.org/10.1002/adfm.201100297
Stegemann JP, Kaszuba SN, Rowe SL (2007) Review: advances in vascular tissue engineering using protein-based biomaterials. Tissue Eng 13(11):2601–2613. https://doi.org/10.1089/ten.2007.0196
Sun W et al (2016) Co-culture of outgrowth endothelial cells with human mesenchymal stem cells in silk fibroin hydrogels promotes angiogenesis. Biomed Mater 11(3):035009. https://doi.org/10.1088/1748-6041/11/3/035009
Suresh V, West JL (2020) 3D culture facilitates VEGF-stimulated endothelial differentiation of adipose-derived stem cells. Ann Biomed Eng 48(3):1034–1044. https://doi.org/10.1007/s10439-019-02297-y
Taubenberger AV et al (2016) 3D extracellular matrix interactions modulate tumour cell growth, invasion and angiogenesis in engineered tumour microenvironments. Acta Biomater 36:73–85. https://doi.org/10.1016/j.actbio.2016.03.017
Teixeira FC et al (2021) Engineering a vascularized 3D hybrid system to model tumor-stroma interactions in breast cancer. Front Bioeng Biotechnol 9:647031. https://doi.org/10.3389/fbioe.2021.647031
van Uden S et al (2019) A novel hybrid silk-fibroin/polyurethane three-layered vascular graft: towards in situ tissue-engineered vascular accesses for haemodialysis. Biomed Mater 14(2):025007. https://doi.org/10.1088/1748-605X/aafc96
Vignesh S et al (2018) Injectable deferoxamine nanoparticles loaded chitosan-hyaluronic acid coacervate hydrogel for therapeutic angiogenesis. Colloids Surf B: Biointerfaces 161:129–138. https://doi.org/10.1016/j.colsurfb.2017.10.033
Wang R et al (2019) Freestanding hierarchical vascular structures engineered from ice. Biomaterials 192:334–345. https://doi.org/10.1016/j.biomaterials.2018.11.011
Wang Y et al (2020) A chitosan modified asymmetric small-diameter vascular graft with anti-thrombotic and anti-bacterial functions for vascular tissue engineering. J Mater Chem B 8(3):568–577. https://doi.org/10.1039/C9TB01755K
Yadav AS et al (2020) RGD functionalized chitosan nanoparticle mediated targeted delivery of raloxifene selectively suppresses angiogenesis and tumor growth in breast cancer. Nanoscale 12(19):10664–10684. https://doi.org/10.1039/C9NR10673A
Yuan Z et al (2021) Injectable GelMA cryogel microspheres for modularized cell delivery and potential vascularized bone regeneration. Small 17(11):2006596. https://doi.org/10.1002/smll.202006596
Zamani M et al (2017) A biomimetic heparinized composite silk-based vascular scaffold with sustained antithrombogenicity. Sci Rep 7(1):4455. https://doi.org/10.1038/s41598-017-04510-1
Zhang R, Larsen NB (2017) Stereolithographic hydrogel printing of 3D culture chips with biofunctionalized complex 3D perfusion networks. Lab Chip 17(24):4273–4282. https://doi.org/10.1039/C7LC00926G
Zhang D et al (2018) The enhanced angiogenesis effect of VEGF-silk fibroin nanospheres-BAMG scaffold composited with adipose derived stem cells in a rabbit model. RSC Adv 8(27):15158–15165. https://doi.org/10.1039/C7RA11610A
Zheng Y et al (2012) In vitro microvessels for the study of angiogenesis and thrombosis. Proc Natl Acad Sci 109(24):9342–9347. https://doi.org/10.1073/pnas.1201240109
Zhu W et al (2017) Direct 3D bioprinting of prevascularized tissue constructs with complex microarchitecture. Biomaterials 124:106–115. https://doi.org/10.1016/j.biomaterials.2017.01.042
Zieris A et al (2010) FGF-2 and VEGF functionalization of starPEG–heparin hydrogels to modulate biomolecular and physical cues of angiogenesis. Biomaterials 31(31):7985–7994. https://doi.org/10.1016/j.biomaterials.2010.07.021
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Ethics declarations
This work was supported by funding from DBT Ramalingaswami Fellowship (BT/RLF/Re-entry/16/2019) (SP), DST-SERB Startup Research Grant (SRG/2020/000343) (SP), IITM Exploratory Research Project (BT1920893RFER008955) (SP), IITM Seed Grant (BT1920587NFIG008955 and BT2021084NFSC008955) (SP), Prime Minister’s Research Fellowship (PMRF) (AB), and UGC Junior Research Fellowship (IPP).
Conflict of Interest
Shantanu Pradhan is the co-founder, director, and holds equity in ISMO Biophotonics Pvt. Ltd. registered in Chennai, India.
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Bist, S., Banerjee, A., Patra, I.P., Jayaprakash, S.R., Sureka, R., Pradhan, S. (2023). Hydrogel-Based Tissue-Mimics for Vascular Regeneration and Tumor Angiogenesis. In: Chakravorty, N., Shukla, P.C. (eds) Regenerative Medicine. Springer, Singapore. https://doi.org/10.1007/978-981-19-6008-6_8
Download citation
DOI: https://doi.org/10.1007/978-981-19-6008-6_8
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-6007-9
Online ISBN: 978-981-19-6008-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)