Abstract
Osteoarthritis secondary to developmental dysplasia of the hip (DDH) is a common orthopedic condition [1]. DDH is a congenital disorder in infants and children. Early detection and nonoperative management have been shown to be effective in preventing secondary osteoarthritis [2]. The incidence of osteoarthritis (OA) secondary to DDH shows considerable geographic and ethnic variation [3]. Regardless of whether or not patients have undergone nonoperative treatment in their early childhood, patients often develop hip pain when they reach a certain age. The anatomical and biomechanical alterations of the acetabulum, femur, and pelvis in DDH predispose to the development of hip OA [4]. A radiological evaluation will demonstrate hip joint degeneration and bony abnormalities. Some patients show subluxation or complete dislocation of the hip joint. These patients are usually relatively young, mostly 40–60 years old, with some being only between in their twenties. Thus, their lifestyle is comparably active, posing high requirements on function, and they need a good survival of the implant. So, they are in need of surgical treatment to either improve their joint function or to achieve normal joint function and mobility in the first place, so as to pursue a normal life and work.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
-
1.
Epidemiology and classification of developmental dysplasia of the Hip.
-
2.
Typical anatomical deformities of acetabulum and femur in DDH.
-
3.
Preoperative plan and surgical technique for I-II DDH.
1 Introduction
Osteoarthritis secondary to developmental dysplasia of the hip (DDH) is a common orthopedic condition [1]. DDH is a congenital disorder in infants and children. Early detection and nonoperative management have been shown to be effective in preventing secondary osteoarthritis [2]. The incidence of osteoarthritis (OA) secondary to DDH shows considerable geographic and ethnic variation [3]. Regardless of whether or not patients have undergone nonoperative treatment in their early childhood, patients often develop hip pain when they reach a certain age. The anatomical and biomechanical alterations of the acetabulum, femur, and pelvis in DDH predispose to the development of hip OA [4]. A radiological evaluation will demonstrate hip joint degeneration and bony abnormalities. Some patients show subluxation or complete dislocation of the hip joint. These patients are usually relatively young, mostly 40–60 years old, with some being only between in their twenties. Thus, their lifestyle is comparably active, posing high requirements on function, and they need a good survival of the implant. So, they are in need of surgical treatment to either improve their joint function or to achieve normal joint function and mobility in the first place, so as to pursue a normal life and work.
The principles of total hip arthroplasty (THA) in DDH are the same as those of THAs for other OA causes: The normal biomechanics of the hip should be restored as much as possible. At the same time, the various anatomical abnormalities often increase the difficulty of the operation. It is critical to evaluate these abnormalities meticulously before surgery. This generally entails a careful examination of the clinical manifestations and the findings on medical imaging, including radiography and computed tomography (CT). Surgeons require comprehensive clinical experience and a thorough understanding of hip anatomy and surgical techniques. Only the integration of knowledge with highly developed surgical skills permits performing high-quality THA in DDH patients.
2 Typical Deformities
The acetabulum and femur of DDH patients are abnormal. The true acetabulum is characterized by insufficient depth, a thin anterior wall, reduced bone mass, and also bone defects. The true acetabulum may be shallow and have full contact with the femoral head, partly in contact with a false acetabulum, or extremely small, shallow, and triangular, showing a complete loss of congruency with the femoral head [5]. Anteriorly, bone stock is limited, often with segmental wall defects. The bone stock is usually rearranged posteriorly [6], and the femoral head is only insufficiently covered by the acetabulum [7]. Commonly, compensatory hyperplasia, thickening, and hypertrophy of the labrum and joint capsule are found. Depending on the length of a patient’s history, osteophytes will have formed around the acetabulum, while the bone defects will be aggravated as a result of long-standing weight bearing on the acetabulum [8]. It is critical to estimate the difficulty of the operation preoperatively and select the most appropriate way to reconstruct the rotation center of the hip joint. Femoral hypoplasia with loss of the metaphyseal flare is often present, with a narrow and straight intramedullary canal [9]. Many patients have marked femoral anteversion and torsion and a short neck, with a coxa valga and lower offset than these of a normal femur [6, 10]. The CT manifestations in patients with dysplasia of the hip include a shallow acetabulum, poor matching between the acetabulum and femoral head, a thin anterior wall, and superior lateral defects (Fig. 13.1). The preoperative CT is helpful to evaluate the degree of bone defects, regardless of whether the anterior wall and posterior wall are intact or not, and the bone stock of the acetabular floor. In patients with a long history of the disease, severe degeneration, and hyperplasia, numerous osteophytes around the acetabulum may have formed (Fig. 13.2). These need to be removed during THA, paying attention not to damage the normal residual structures of the hip joint. Removal of osteophytes can release the capsule and reduce the impact on the hip joint after the operation. Most of the time, osteophytes are removed after the acetabular prosthesis is placed (Fig. 13.3).
Computed tomography in developmental dysplasia of the hip. (a) This CT shows a shallow acetabulum, poor matching between the acetabulum and femoral head, a thin anterior wall, and a superior lateral defect. (b) femoral head dislocate from acetabulum. (c, d) femoral anteversion is abnormal. (e) CT findings in severe cases showing extensive osteophyte growth around the acetabulum, femoral head dislocate from acetabulum
3 Classification
Many classifications of DDH have been proposed. The most popular are the Hartofilakidis and Crowe classifications. The Crowe classification [11] divides DDH into four types according to the degree of dislocation of the femoral head from the true acetabulum (Fig. 13.4). The teardrop and the inner edge of the femoral head and neck are reference points in this classification, and the height of the femoral head is the reference height.
-
Type I is a subluxation of less than 50% of the vertical diameter of the femoral head;
-
Type II is a 50–75% subluxation of vertical diameter of the femoral head;
-
Type III is a 75–100% subluxation of vertical diameter of the femoral head;
-
Type IV is a more than 100% subluxation of the femoral head.
The disadvantage of this quantitative classification is that it focuses on the degree of displacement of the femoral head and does not consider the anatomical abnormalities of the acetabulum. It requires a pelvic radiograph, presents some difficulties in defining the landmarks, and does not explain the underlying pathology. Furthermore, it is not very helpful in preoperative planning.
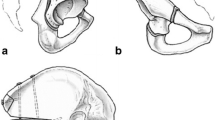
The Hartofilakidis classification [12] is more practical than the Crowe classification. As a qualitative classification, it explains the underlying pathology and anatomic variations. It distinguishes three types (Fig. 13.5):
-
Type A: Dysplasia, the femoral head is located within the true acetabulum;
-
Type B: Low dislocation, the femoral head is located within the false acetabulum. The lower lip of the acetabulum adjoins or overlaps the upper lip of the true acetabulum;
-
Type C: High dislocation, the femoral head has migrated posteriorly and superiorly and has no contact with the true or false acetabulum. This type can be further divided into two distinct subtypes, based on the presence (C1) or absence (C2) of a false acetabulum [13]. Revision rates are higher in C2 than C1 [14]. The femur in C2 has a smaller neck-shaft angle, higher migration index, shorter femoral neck, and higher position of the greater trochanter [15].
4 Surgical Planning
Surgeons should use standard anteroposterior and lateral radiographs for templating [16]. Most of the time, the mean mediolateral diaphyseal diameter of the femoral canal is smaller than the anteroposterior in all DDH types. Therefore, small and even smallest diameter implants (e.g. 38 mm) are needed. CT with 3D reconstruction is performed to evaluate any wall deficiencies, the socket size, and bone stock of the true acetabulum. Furthermore, the anteroposterior acetabular diameter is crucial in cup size selection [17]. Leg-length discrepancy and decreased acetabular anteversion compared with normal population correlate with advanced disease [18]. Templating is performed to choose the type and size of the implant, and the success of DDH reconstruction will depend on the correct choice of the implant. However, intraoperative findings may change implant requirements. Preferably, the acetabular component which has a hemispherical porous shell with multiple holes for screw fixation is used. Even if seldom needed, augments, buttress, and equipment for structure bone grafts should be prepared preoperatively.
A variety of femoral components should be available to address both routine and complex cases. Since increased anteversion is a common finding even in mild DDH (I, II), modular implants that allow rotational adjustment are useful. Modular stems such as those in the S-ROM® Modular Hip System (DePuy Synthes, Raynham, MA, US) are well suited for DDH. The S-ROM® is a cementless modular cylindrical prosthesis system. The titanium alloy stem is polished distally with splines around a coronal slot to reduce stem stiffness. Additionally, there are proximal standard and calcar height and offset options. It offers porous-coated or hydroxyapatite-coated sleeves designed to convert hoop and shear stresses to compressive forces at the sleeve-bone interface. Cerclage cables, femoral plates, and screws should be available in case they are needed. Biant et al. reported the average 10-year clinical and radiographic results of 28 hips with Crowe III or IV DDH and a technically difficult primary hip arthroplasty using the cementless modular S-ROM® stem [19]. None of the S-ROM® stems had been revised or were loose at the latest follow-up.
Cemented prostheses fare less well in DDH. Stans et al. [20] reported the results of a cemented prosthesis in 70 Crowe type III hips in patients with secondary OA after an average of 16 years postoperatively, showing aseptic loosening of 40% of the femoral stems. Eleven stems had been revised, including four because of an infection and two following component fractures. Klapach et al. [21] reported on the long-term follow-up of cemented THA in 65 hips with Crowe II, III, and IV DDH.
5 Surgical Technique
Surgeons performing THA in DDH need to have sufficient experience, not only to correctly determine the location of the true acetabulum but also to master the technical demands of the reconstruction. The preoperative imaging examination allows evaluating the bone stock and the intactness of the anterior and posterior wall of the acetabulum. If the bone stock of the inner wall of the acetabulum is sufficient and the anterior wall is intact, the operation is relatively easy. If the inner wall of the acetabulum is thin and the anterior wall is weak or has defects, the operation becomes difficult. In this case, the key is to protect the anterior wall during reaming. A small cup has to be used and reaming should not go beyond a distance of approximately 2–3 mm from the inner cortex to leave sufficient bone stock for potential future revision surgery. Surgeons should aim to achieve 75–80% coverage of the cup.
The principles of reconstruction in DDH are:
-
1.
Aiming to reconstruct the acetabulum in the correct position and avoid moving the rotation center cranially. It is critical to determine the ideal rotation center, which can be measured on preoperative radiographs as follows: If the contralateral hip is normal, the position of its acetabular center determines the height of the center of the reconstructed hip. If both sides are abnormal, the ideal rotation center can be found by drawing Ranawat’s triangle.
-
2.
Aiming to maximize the contact area between the prosthesis and the host bone to facilitate bone ingrowth and obtain stable and reliable long-term fixation.
-
3.
Using the largest cup possible, which can increase the liner thickness, increase the diameter of the femoral head, and reduce the dislocation rate.
It should be underlined that the position of the acetabular fossa should be determined first, and thereafter a small reamer can be used to expose the bottom of the acetabular fossa. Following that, surgeons should gradually enlarge the size of the cup to find the most appropriate size.
The following three reconstruction methods are recommended in Crowe type I–II DDH:
-
1.
Deepening of the acetabulum. In patients with sufficient acetabular bone stock, this method is mostly used and saves time. After identification of the true acetabulum position, it is important to expose the entire circumference of the acetabulum and the transverse acetabular ligaments. In DDH patients, the ligaments are generally a certain mark of acetabulum. The inner wall of the acetabulum is reamed with a small reamer, for example, 38 mm. The depth of reaming is determined by the inner wall of the acetabulum, which corresponds to the lateral edge of the teardrop on the radiograph. If the depth is insufficient, it is likely to lateralize the cup and result in inadequate coverage. In general, the anterior wall is very thin but relatively hard in Crowe type I–II. If the anterior and posterior walls cannot provide sufficient support to stabilize the cup, the acetabulum may be too shallow. In that case, reaming can be performed to deepen it appropriately, even if at the cost of slightly penetrating the inner wall. In complex cases, fluoroscopy can be used intraoperatively to support the surgeon’s judgment. Once the stability of the anterior and posterior wall has been secured, the bone fragments harvested during reaming can be implanted into the acetabular floor, and screws may assist fixation of the prosthesis (Fig. 13.6).
-
2.
If the above method cannot obtain stable conditions, an inner wall osteotomy may be performed. Surgeons use the osteotome to cut a circle of about half the diameter of the inner wall and then carefully advance the central bone block into the pelvis while still keeping contact between the bone block and the acetabulum. This allows to deepen the acetabulum, preserve the bone stock of the inner wall, and obtain stable fixation (Fig. 13.7).
-
3.
If the acetabular bone stock measured on the preoperative images is insufficient, defects are severe, and acetabular coverage is poor, autologous femoral head grafting or an appropriate type of metal augments can be used to supplement the superolateral defects (Fig. 13.8).
The femoral side reconstruction of the dysplastic hip is equally important. In this case, the offset of the femoral head can be reconstructed by using a conventional prosthesis, carefully avoiding a leg-length discrepancy. The femoral anteversion is calculated on preoperative imaging and confirmed intraoperatively. Usually, a CT measurement is used for the preliminary calculation (Fig. 13.9). If the anteversion is too large, it needs to be adjusted by using a modular prosthesis. It should be noted that the femoral anteversion calculated using CT preoperatively can be used as a reference but sometimes is not consistent with the actual anteversion measured during the operation. The reasons may be measurement errors, inaccuracy in CT, or an improper decubitus position during scanning. If the femoral anteversion is considerably increased, for example, >30°, a modular prosthesis should be used to adjust the anteversion, such as the S-ROM® prosthesis. However, in Crowe I–II, a monoblock prosthesis is usually sufficient to perform THA.
Measurement of femoral anteversion on computed tomography prior to total hip arthroplasty in developmental dysplasia of the hip in Crowe type I–II. The line of the posterior edge of the femoral condyle was used as a reference to measure the relative Angle of the femoral neck relative to the level of the posterior edge of the femoral condyle
References
Gustke K. The dysplastic hip: not for the shallow surgeon. Bone Joint J. 2013;95-B(11 Suppl A):31–6.
Mulpuri K, Song KM. AAOS clinical practice guideline: detection and nonoperative management of pediatric developmental dysplasia of the hip in infants up to six months of age. J Am Acad Orthop Surg. 2015;23(3):206–7.
Kumar JN, et al. Medium-term outcome of total hip replacement for dysplastic hips in Singapore. J Orthop Surg (Hong Kong). 2010;18(3):296–302.
Greber EM, et al. Challenges in total hip arthroplasty in the setting of developmental dysplasia of the hip. J Arthroplast. 2017;32(9s):S38–44.
Hartofilakidis G, et al. Congenital hip disease in adults. Classification of acetabular deficiencies and operative treatment with acetabuloplasty combined with total hip arthroplasty. J Bone Joint Surg Am. 1996;78(5):683–92.
Argenson JN, et al. Anatomy of the dysplastic hip and consequences for total hip arthroplasty. Clin Orthop Relat Res. 2007;465:40–5.
Steppacher SD, et al. Femoral morphology differs between deficient and excessive acetabular coverage. Clin Orthop Relat Res. 2008;466(4):782–90.
Li PL, Ganz R. Morphologic features of congenital acetabular dysplasia: one in six is retroverted. Clin Orthop Relat Res. 2003;416(416):245–53.
Yasgur DJ, et al. Subtrochanteric femoral shortening osteotomy in total hip arthroplasty for high-riding developmental dislocation of the hip. J Arthroplast. 1997;12(8):880–8.
Noble PC, et al. Three-dimensional shape of the dysplastic femur: implications for THR. Clin Orthop Relat Res. 2003;417(417):27–40.
Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979;61(1):15–23.
Hartofilakidis G, Stamos K, Ioannidis TT. Low friction arthroplasty for old untreated congenital dislocation of the hip. J Bone Joint Surg Br. 1988;70(2):182–6.
Hartofilakidis G, Yiannakopoulos CK, Babis GC. The morphologic variations of low and high hip dislocation. Clin Orthop Relat Res. 2008;466(4):820–4.
Hartofilakidis G, et al. Results of total hip arthroplasty differ in subtypes of high dislocation. Clin Orthop Relat Res. 2013;471(9):2972–9.
Wang Z, et al. Three-dimensional femoral morphology in Hartofilakidis type C developmental dysplastic hips and the implications for total hip arthroplasty. Int Orthop. 2020;44(10):1935–42.
Mulcahy H, Chew FS. Current concepts of hip arthroplasty for radiologists: part 2, revisions and complications. AJR Am J Roentgenol. 2012;199(3):570–80.
Sakellariou VI, et al. Reconstruction of the acetabulum in developmental dysplasia of the hip in total hip replacement. Arch Bone Jt Surg. 2014;2(3):130–6.
Bernasek TL, et al. Total hip arthroplasty requiring subtrochanteric osteotomy for developmental hip dysplasia: 5- to 14-year results. J Arthroplast. 2007;22(6 Suppl 2):145–50.
Biant LC, et al. Primary total hip arthroplasty in severe developmental dysplasia of the hip. Ten-year results using a cementless modular stem. J Arthroplast. 2009;24(1):27–32.
Stans AA, et al. Results of total hip arthroplasty for Crowe type III developmental hip dysplasia. Clin Orthop Relat Res. 1998;348(348):149–57.
Klapach AS, et al. Total hip arthroplasty with cement and without acetabular bone graft for severe hip dysplasia. A concise follow-up, at a minimum of twenty years, of a previous report. J Bone Joint Surg Am. 2005;87(2):280–5.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Science Press
About this chapter
Cite this chapter
Ji, S., Tang, J. (2022). Total Hip Arthroplasty for Developmental Dysplasia of the Hip. Part 1: Crowe I–II. In: Zhou, Y., Tang, J., Shao, H. (eds) Principles of Primary Total Hip Arthroplasty. Springer, Singapore. https://doi.org/10.1007/978-981-19-3606-7_13
Download citation
DOI: https://doi.org/10.1007/978-981-19-3606-7_13
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-3605-0
Online ISBN: 978-981-19-3606-7
eBook Packages: MedicineMedicine (R0)