Abstract
The goal of treating acute Kawasaki disease (KD) is to treat inflammation and reduce cardiovascular sequelae by reducing the inflammation of the coronary arteries. We reviewed the clinical studies that focused on the efficacy of medications used for KD. Intravenous immunoglobulin (IVIG) is the standard treatments for KD. Some studies have the use of adjunctive corticosteroids in selective patients with KD. Corticosteroids were found to lower the progression of aneurysms in patients with Z scores ≥2.5. The efficacies of corticosteroids in KD remain controversial. Biologics, including etanercept and infliximab, have also been reported to exert benefits in patients with coronary artery abnormalities. Clinical trials with larger sample sizes are warranted to examine the efficacy of medications and clarify the role of acetylsalicylic acid in traditional treatments in KD.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Coronary artery aneurysm
- Corticosteroids
- Intravenous immunoglobulin
- Kawasaki disease
- Vasculitis
- Treatment
Intravenous Immunoglobulin
The American Heart Association (AHA) proposed the guidelines for the diagnosis and management of Kawasaki disease (KD) in 2004 based on the evidence including the summary provided by the meta-analysis published in the Cochrane in 2003 and the guideline was updated in 2017 [1,2,3]. Intravenous immunoglobulin (IVIG) is pooled from serum IgG. High-dose IVIG was applied in the therapy of KD in Japan in 1984 [4]. Then, Newburger et al. conducted a multicenter, randomized controlled trial study (RCT) confirmed that a single high dose IVIG can, indeed, reduce the coronary-artery abnormalities to <5% in then the USA [5]. Since then, KD is considered a nonfatal disease with good prognosis. There are many ways to use IVIG at the beginning, covering IVIG 400 mg/kg daily, for 5 days, or for 3–4 days, IVIG 1 g/kg for 1 or 2 days, IVIG 200 mg/kg per day for 5 consecutive days, IVIG 50–100 mg/kg for 5 days, or IVIG 2 g/kg [3]. Statistical analysis points out that prevalence of coronary artery abnormalities in KD is highly dependent on IVIG dose [3, 6]. The 2004 and 2017 treatment guidelines recommend IVIG 2 g/kg as a single infusion, usually given over 10–12 h [1, 2]. IVIG should be administered within 7 days of fever, and give it as soon as possible after the diagnosis of KD before developing histological arteritis. In a cohort study in Japan from 2011 to 2012, among 20,933 KD patients, patients with IVIG administered after 7 days of fever were prone to developing coronary artery dilations compared to those with IVIG before 7 days (odds ratio: 1.66) [7]. IVIG started ≦4 days of symptoms did not reduce the formation of coronary artery dilations. KD is considered a self-limited disease because the patient will go away from fever without treatment [8]. In a retrospective study, among 293 KD patients who had a fever for 5–10 days, the risk of coronary aneurysms after 1 month was significantly higher in 37 patients without IVIG treatment than that of patients who received IVIG (18.9% vs. 5.1%) [8]. Especially in patients younger than 1 year old and with elevated white blood cells, they were a high-risk group for coronary aneurysms. A retrospective study in Japan found that among 968 patients with KD, 71 patients had initial spontaneous defervescence within 7 days. If there was no abnormal coronary artery findings and persistent inflammation, the prognosis was relatively benign [9]. The current treatment recommendations are KD patients including those with spontaneous defervescence need IVIG treatment. However, we need further research to distinguish between high-risk groups and low-risk groups that do not require IVIG treatment for patients with spontaneous defervescence.
The high dose of IVIG has the effect of regulating immunity by lowering the high-affinity receptor FcγRI and ameliorating the inflammation of KD. At the same time, it also reduces the expression of FcγRII and other low-affinity receptors [10, 11]. IVIG also avoids autoimmunity caused by the combination of autoantibodies and Fcγ receptors [12]. The role of IVIG also includes enhancing the activity of regulatory T cells, inhibiting the production of antibodies and inflammation, and balancing type 1/type 2 inflammations [13,14,15,16]. The monoclonal antibodies against IgG Fc-dependent pathways have been undergoing clinical studies one after another [12, 17].
Serious adverse effects after treatment with IVIG are quite rare [18]. In 2017, Ibrahim et al. presented a patient with KD who developed transfusion-related acute lung injury after immunoglobulin infusion [19]. The patient’s condition resolved with supportive care. Kemmotsu et al. conducted a retrospective analysis, 10-year period study in KD patients treated with high dose IVIG. They observed that acute treatment with high dose IVIG was related to aseptic meningitis in 4 out of 384 patients [20]. Mention of immediate reaction after infusion, one small-sample, cross-sectional study on high dose IVIG treatment reported one child developed skin rash in the 11 pediatric patients with KD [21]. A case series conducted at a tertiary care pediatric hospital identified five KD patients with severe anemia requiring transfusion with incidence of 0.36% [22].
Acetylsalicylic Acid
Before IVIG therapy has been established as the standard treatment for KD and the invention of cardiac ultrasound, acetylsalicylic acid was once believed to reduce the mortality of KD due to its effect on thrombotic occlusion of a coronary artery [23]. High-dose acetylsalicylic acid was applied from 80 to 100 mg/kg/day in the USA to 30–50 mg/kg/day in Japan, poses anti-inflammatory effect by blocking arachidonic acid producing prostaglandin E2, and converted to low-dose acetylsalicylic acid 3–5 mg/kg/day which had antiplatelet function by blocking cyclooxygenase producing thromboxane A2 48 h after defervescence for 6–8 weeks [24]. KD patients with coronary artery abnormalities are recommended to be treated until the cardiac ultrasound is normal and the inflammation index is completely improved.
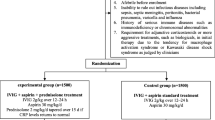
Despite the lack of evidence provided by RCT, in contrast, traditional high-dose acetylsalicylic acid was considered to have no significant therapeutic effect in a 10-year retrospective study with 260 KD children [24, 25]. But it is still necessary to understand the preventive effect of low-dose aspirin on coronary artery lesions [26]. Kuo et al. designed a multi-center, randomized controlled, evaluator-blinded trial to compare the difference of coronary artery lesions between the two groups (IVIG alone vs. IVIG plus high-dose acetylsalicylic acid at acute stage) 1 month later [27].
Kuo et al. found that high-dose acetylsalicylic acid was associated with anemia [28]. The previous study involving 609 KD patients in Taiwan showed high dose acetylsalicylic acid posed no appreciable benefit in preventing the IVIG treatment failure, the formation of coronary artery lesions, or shortening the length of hospital stay. The use of acetylsalicylic acid is most prone to side effects of the digestive system (5.3% among 910 KD patients) in a retrospective study with large sample size [29]. Bleeding in the upper and lower gastrointestinal tract and abnormal liver function have been reported, and symptoms of abdominal discomfort may appear under the treatment of acetylsalicylic acid [30].
Adjuvant Therapy: Corticosteroids
Before knowing which way to treat KD, corticosteroids alone in the treatment of acute KD increased the incidence of coronary artery lesions (CAL) [23]. However, the current goal of precision medicine is to use adjuvant therapy for patients who are predicted to respond poorly to IVIG treatment. Two meta-analyses (one is limited to RCT and the other is not limited to) try to distinguish the effect of corticosteroids in KD [31, 32]. In selected high-risk patients with KD, initial combination with corticosteroids can reduce coronary artery abnormalities [33]. A 35-year retrospective analysis in the USA found that adjuvant therapy can effectively increase the CAL regression rate [34]. When 121 children diagnosed KD with a Z score ≥2.5 and <10, treatment plus corticosteroids or infliximab compared with IVIG alone can reduce the deterioration of coronary artery abnormalities [35]. Newburger and colleagues investigated the efficacy of initial methylprednisolone pulse therapy (30 mg/kg) combined with following IVIG in nonselective KD patients. This RCT found coadministration of methylprednisolone and IVIG cannot decrease the risk of coronary artery abnormalities [36].
Studies have investigated the use of initial adjunctive prednisolone with respect to its treatment effect in patients with severe KD in Japan. However, the results of these trials are conflicting.
Kobayashi and colleagues conducted an RCT called RAISE study and evaluated the efficacy of adjunctive initial prednisolone in selected high-risk KD patients evaluated by Kobayashi score [37]. They found that the effect of additional prednisolone was significant for coronary artery abnormalities (4/125 patients in combination group vs. 28/123 patients in standard group, p < 0.0001). Analysis of large-scale data from nationwide epidemiologic KD surveys which cannot identified the severity score found significantly decreased risk (estimated risk ratio 0.53) of coronary artery abnormality (74/1593 in combination treatment group with corticosteroids added to initial standard treatment vs. 140/1593 in IVIG group) and the requirement of retreatment for treatment failure (estimated risk ratio 0.65; 225/1593 in combination treatment group with corticosteroids added to initial standard treatment vs. 234/1593 in controls) [38, 39]. However, a Post RAISE study with a multicenter, prospective cohort design did not find different coronary outcomes between patients predicted IVIG resistance using Kobayashi score treated with combination treatment consisting of prednisolone and IVIG and placebo group [40].
Because the design of risk score varies from race to race, it also affects the clinical use of corticosteroids and related research [38, 41]. Since the therapeutic effect is equivalent to secondary IVIG, corticosteroids are also considered an option for refractory KD [42, 43].
Adjuvant Therapy: Biologics
Tumor necrosis factor α (TNFα) is a well-known biomarker for KD. TNFα mediates endothelial cell activation and is involved in the CAL development [44]. Due to the breakthrough development of monoclonal antibodies, strong specificity can avoid systemic immunosuppression and other associated comorbidities [45]. Among the 16 refractory KD patients, 13 patients under infliximab were found to resolve their fever in a small series in 2005 [46]. A phase 3 RCT enrolled 196 patients and demonstrated no additional benefit of treatment resistance for the addition of infliximab, biologics as the format of chimeric murine/human IgG1, produced by hybridoma, to primary treatment in acute KD [47]. However, a meta-analysis for five RCTs with 494 participants reported anti-TNFα has beneficial effects on treatment resistance [48]. The reduced transcripts of peptidase inhibitor-3, matrix metalloproteinase-8, chemokine receptor-2, and pentraxin-3 related to IVIG resistance after infliximab treatment support the use of infliximab in KD patients with IVIG resistance [49].
Another anti-TNF synthetic biologic, etanercept, binds only soluble TNF. A double-blind multicenter controlled trial on unselected KD patients who were treated with primary adjuvant etanercept demonstrated benefit in IVIG resistance in patients >1 year. It also has favorable effects on ameliorating coronary artery dilation in patients with baseline abnormalities (Z score > 2.5, n = 22 in etanercept group compared with n = 24 in placebo group p = 0.03) [50].
Adjuvant Treatments: Cyclosporin
Cyclosporin is a calcineurin inhibitor and then suppressed the activation of T cells by negative regulation of nuclear factor of activated T cells (NFAT) pathway, following signal transmission with functional polymorphism of Inositol 1,4,5-trisphosphate 3-kinase C (ITPKC) associated with the susceptibility and aneurysm formation in KD patients [51]. The high-risk ITPKC genotype involved in treatment failure is associated with the higher baseline and activated intracellular calcium and inflammatory biomarkers including IL-1β [52]. A phase 3 RCT collected 175 participants with Kobayashi risk score scale ≧5 points [53]. Combined primary therapy with IVIG and ciclosporin resulted in significantly lower incidence of CAL than IVIG group (12 [14%] of 86 patients; 27 [31%] of 87 patients; p = 0.010) [54].
Adjuvant Treatments: Clarithromycin
Immunological and epidemiological evidence strongly suggests characteristics of infectious disease for KD [55, 56]. Mycoplasma pneumoniae is the secondary bacterial etiology of pediatric pneumonia in Taiwan and may have association with KD and cardiac outcome [57, 58]. A retrospective Korean survey found 37 cases in 152 tested KD patients showed positive mycoplasma antibodies [59]. Current research cannot confirm that Mycoplasma pneumoniae is a possible trigger of KD or just a mere coincidental association [60].
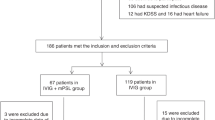
Clarithromycin is a 14-membered ring macrolide with anti-inflammatory activity for respiratory tract infections in children [61]. In a phase 2 RCT involving nonselective patients with KD, IVIG plus clarithromycin showed the efficacy of improving relapse rate of patients (5/40 patients in additional clarithromycin group versus 12/39 patients in control group, p = 0.046) [61].
Second-Line Therapy of Refractory Kawasaki Disease
Refractory KD or IVIG resistance was defined as KD patients with fever ≥36 h and <7 days after the completion of their first IVIG treatment [1]. Ten to 20% of KD patients do not respond to gold standard treatment and have an increased risk of cardiovascular sequelae. Currently, there is no consensus regarding optimal adjunctive primary and second-line therapeutics for KD, especially in high-risk patients and patients with complications. Most patients still receive secondary IVIG treatment among more than 300 patients [43]. A meta-analysis identified no significant difference in the effect of intravenous pulse methylprednisolone, infliximab, or secondary IVIG on CAL [42]. Caution is still required in the use of intravenous pulse methylprednisolone due to the higher fever recurrence, higher rehospitalization rate and the higher CAL found in long-term follow-up in the methylprednisolone group [62, 63]. Infliximab’s ability to reduce fever is even better than secondary IVIG [43]. The ongoing multicenter phase 3 RCT compares the therapeutic effects of infliximab and secondary IVIG on refractory KD [64]. The IL (interleukin)-1 pathway plays a significant role in KD pathogenesis. In the experimental mouse model of KD, it was found that both IL-1α and IL-1β can cause myocarditis and the formation of aneurysm, which can be improved by anti-inflammatory drugs anakinra [52, 65]. In a phase 2, open-label study involving 16 patients with IVIG-resistant KD, anakinra, IL-1 inhibitors, showed clinical efficacy [66]. Only one patient stopped treatment because of swelling at the injection site. Highly invasive treatment of plasma exchange increases the risk of treatment. Plasma exchange is a therapeutic option (Class IIb; Level of Evidence C) reserved for patients failed to all other choices for refractory KD [1].
References
McCrindle BW, Rowley AH, Newburger JW, Burns JC, Bolger AF, Gewitz M, Baker AL, Jackson MA, Takahashi M, Shah PB, Kobayashi T, Wu MH, Saji TT, Pahl E. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017;135(17):e927–99. https://doi.org/10.1161/cir.0000000000000484.
Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, Shulman ST, Bolger AF, Ferrieri P, Baltimore RS, Wilson WR, Baddour LM, Levison ME, Pallasch TJ, Falace DA, Taubert KA. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Circulation. 2004;110(17):2747–71. https://doi.org/10.1161/01.CIR.0000145143.19711.78.
Oates-Whitehead RM, Baumer JH, Haines L, Love S, Maconochie IK, Gupta A, Roman K, Dua JS, Flynn I. Intravenous immunoglobulin for the treatment of Kawasaki disease in children. Cochrane Database Syst Rev. 2003;(4):CD004000. https://doi.org/10.1002/14651858.Cd004000.
Furusho K, Sato K, Soeda T, Matsumoto H, Okabe T, Hirota T, Kawada S. High-dose intravenous gammaglobulin for Kawasaki disease. Lancet (London, England). 1983;2(8363):1359. https://doi.org/10.1016/s0140-6736(83)91109-1.
Newburger JW, Takahashi M, Burns JC, Beiser AS, Chung KJ, Duffy CE, Glode MP, Mason WH, Reddy V, Sanders SP, et al. The treatment of Kawasaki syndrome with intravenous gamma globulin. N Engl J Med. 1986;315(6):341–7. https://doi.org/10.1056/nejm198608073150601.
Terai M, Shulman ST. Prevalence of coronary artery abnormalities in Kawasaki disease is highly dependent on gamma globulin dose but independent of salicylate dose. J Pediatr. 1997;131(6):888–93. https://doi.org/10.1016/S0022-3476(97)70038-6.
Kuwabara M, Yashiro M, Ae R, Yanagawa H, Nakamura Y. The effects of early intravenous immunoglobulin therapy for Kawasaki disease: the 22nd nationwide survey in Japan. Int J Cardiol. 2018;269:334–8. https://doi.org/10.1016/j.ijcard.2018.07.092.
Hu YC, Liu HM, Lin MT, Chen CA, Chiu SN, Lu CW, Chang LY, Wang JK, Wu MH. Outcomes of Kawasaki disease children with spontaneous defervescence within 10 days. Front Pediatr. 2019;7:158. https://doi.org/10.3389/fped.2019.00158.
Takahashi T, Sakakibara H, Morikawa Y, Miura M. Development of coronary artery lesions in indolent kawasaki disease following initial spontaneous defervescence: a retrospective cohort study. Pediatr Rheumatol. 2015;13(1):44. https://doi.org/10.1186/s12969-015-0042-8.
Chang LS, Lo MH, Li SC, Yang MY, Hsieh KS, Kuo HC. The effect of FcγRIIA and FcγRIIB on coronary artery lesion formation and intravenous immunoglobulin treatment responses in children with Kawasaki disease. Oncotarget. 2017;8(2):2044–52. https://doi.org/10.18632/oncotarget.13489.
Chang LS, Ming-Huey Guo M, Lo MH, Kuo HC. Identification of increased expression of activating Fc receptors and novel findings regarding distinct IgE and IgM receptors in Kawasaki disease. Pediatr Res. 2021;89(1):191–7. https://doi.org/10.1038/s41390-019-0707-y.
Shock A, Humphreys D, Nimmerjahn F. Dissecting the mechanism of action of intravenous immunoglobulin in human autoimmune disease: lessons from therapeutic modalities targeting Fcγ receptors. J Allergy Clin Immunol. 2020;146(3):492–500. https://doi.org/10.1016/j.jaci.2020.06.036.
Wang CL, Wu YT, Lee CJ, Liu HC, Huang LT, Yang KD. Decreased nitric oxide production after intravenous immunoglobulin treatment in patients with Kawasaki disease. J Pediatr. 2002;141(4):560–5. https://doi.org/10.1067/mpd.2002.127505.
Wang CL, Wu YT, Liu CA, Lin MW, Lee CJ, Huang LT, Yang KD. Expression of CD40 ligand on CD4+ T-cells and platelets correlated to the coronary artery lesion and disease progress in Kawasaki disease. Pediatrics. 2003;111(2):E140–7. https://doi.org/10.1542/peds.111.2.e140.
Kuo HC, Wang CL, Liang CD, Yu HR, Chen HH, Wang L, Yang KD. Persistent monocytosis after intravenous immunoglobulin therapy correlated with the development of coronary artery lesions in patients with Kawasaki disease. J Microbiol Immunol Infect. 2007;40(5):395–400.
Shimizu C, Jain S, Davila S, Hibberd ML, Lin KO, Molkara D, Frazer JR, Sun S, Baker AL, Newburger JW, Rowley AH, Shulman ST, Burgner D, Breunis WB, Kuijpers TW, Wright VJ, Levin M, Eleftherohorinou H, Coin L, Popper SJ, Relman DA, Fury W, Lin C, Mellis S, Tremoulet AH, Burns JC. Transforming growth factor-beta signaling pathway in patients with Kawasaki disease. Circ Cardiovasc Genet. 2011;4(1):16–25. https://doi.org/10.1161/circgenetics.110.940858.
Fitzpatrick EA, Wang J, Strome SE. Engineering of Fc multimers as a protein therapy for autoimmune disease. Front Immunol. 2020;11:496. https://doi.org/10.3389/fimmu.2020.00496.
Guo Y, Tian X, Wang X, Xiao Z. Adverse effects of immunoglobulin therapy. Front Immunol. 2018;9:1299. https://doi.org/10.3389/fimmu.2018.01299.
Ibrahim J, Al Amri A, Ghatasheh G. Transfusion-related acute lung injury after immunoglobulin infusion for Kawasaki disease: a case report and literature review. Glob Pediatr Health. 2017;4:2333794x17746545. https://doi.org/10.1177/2333794x17746545.
Kemmotsu Y, Nakayama T, Matsuura H, Saji T. Clinical characteristics of aseptic meningitis induced by intravenous immunoglobulin in patients with Kawasaki disease. Pediatr Rheumatol Online J. 2011;9:28. https://doi.org/10.1186/1546-0096-9-28.
Kaba S, Keskindemirci G, Aydogmus C, Siraneci R, Erol Cipe F. Immediate adverse reactions to intravenous immunoglobulin in children: a single center experience. Eur Ann Allergy Clin Immunol. 2017;49(1):11–4.
Luban NL, Wong EC, Henrich Lobo R, Pary P, Duke S. Intravenous immunoglobulin-related hemolysis in patients treated for Kawasaki disease. Transfusion. 2015;55(Suppl 2):S90–4. https://doi.org/10.1111/trf.13089.
Kato H, Koike S, Yokoyama T. Kawasaki disease: effect of treatment on coronary artery involvement. Pediatrics. 1979;63(2):175–9.
Chang LS, Hsu YW, Lu CC, Lo MH, Hsieh KS, Li SC, Chang WC, Kuo HC. CYP2E1 gene polymorphisms related to the formation of coronary artery lesions in Kawasaki disease. Pediatr Infect Dis J. 2017;36(11):1039–43. https://doi.org/10.1097/inf.0000000000001657.
Platt B, Belarski E, Manaloor J, Ofner S, Carroll AE, John CC, Wood JB. Comparison of risk of recrudescent fever in children with Kawasaki disease treated with intravenous immunoglobulin and low-dose vs high-dose aspirin. JAMA Netw Open. 2020;3(1):e1918565. https://doi.org/10.1001/jamanetworkopen.2019.18565.
Chiang MH, Liu HE, Wang JL. Low-dose or no aspirin administration in acute-phase Kawasaki disease: a meta-analysis and systematic review. Arch Dis Child. 2021;106(7):662–8. https://doi.org/10.1136/archdischild-2019-318245.
Kuo HC, Guo MMH, Lo MH, Hsieh KS, Huang YH. Effectiveness of intravenous immunoglobulin alone and intravenous immunoglobulin combined with high-dose aspirin in the acute stage of Kawasaki disease: study protocol for a randomized controlled trial. BMC Pediatr. 2018;18(1):200. https://doi.org/10.1186/s12887-018-1180-1.
Kuo HC, Lo MH, Hsieh KS, Guo MM, Huang YH. High-dose aspirin is associated with anemia and does not confer benefit to disease outcomes in Kawasaki disease. PLoS One. 2015;10(12):e0144603. https://doi.org/10.1371/journal.pone.0144603.
Huang X, Huang P, Zhang L, Xie X, Xia S, Gong F, Yuan J, Jin L. Is aspirin necessary in the acute phase of Kawasaki disease? J Paediatr Child Health. 2018;54(6):661–4. https://doi.org/10.1111/jpc.13816.
Zheng X, Yue P, Liu L, Tang C, Ma F, Zhang Y, Wang C, Duan H, Zhou K, Hua Y, Wu G, Li Y. Efficacy between low and high dose aspirin for the initial treatment of Kawasaki disease: current evidence based on a meta-analysis. PLoS One. 2019;14(5):e0217274. https://doi.org/10.1371/journal.pone.0217274.
Wardle AJ, Connolly GM, Seager MJ, Tulloh RM. Corticosteroids for the treatment of Kawasaki disease in children. Cochrane Database Syst Rev. 2017;(1):Cd011188. https://doi.org/10.1002/14651858.CD011188.pub2.
Chen S, Dong Y, Kiuchi MG, Wang J, Li R, Ling Z, Zhou T, Wang Z, Martinek M, Purerfellner H, Liu S, Krucoff MW. Coronary artery complication in Kawasaki disease and the importance of early intervention: a systematic review and meta-analysis. JAMA Pediatr. 2016;170(12):1156–63. https://doi.org/10.1001/jamapediatrics.2016.2055.
Chang LS, Kuo HC. The role of corticosteroids in the treatment of Kawasaki disease. Expert Rev Anti-Infect Ther. 2020;18(2):155–64. https://doi.org/10.1080/14787210.2020.1713752.
Friedman KG, Gauvreau K, Hamaoka-Okamoto A, Tang A, Berry E, Tremoulet AH, Mahavadi VS, Baker A, de Ferranti SD, Fulton DR, Burns JC, Newburger JW. Coronary artery aneurysms in Kawasaki disease: risk factors for progressive disease and adverse cardiac events in the US population. J Am Heart Assoc. 2016;5(9):e003289. https://doi.org/10.1161/jaha.116.003289.
Dionne A, Burns JC, Dahdah N, Tremoulet AH, Gauvreau K, de Ferranti SD, Baker AL, Son MB, Gould P, Fournier A, Newburger JW, Friedman KG. Treatment intensification in patients with Kawasaki disease and coronary aneurysm at diagnosis. Pediatrics. 2019;143(6):e20183341. https://doi.org/10.1542/peds.2018-3341.
Newburger JW, Sleeper LA, McCrindle BW, Minich LL, Gersony W, Vetter VL, Atz AM, Li JS, Takahashi M, Baker AL, Colan SD, Mitchell PD, Klein GL, Sundel RP. Randomized trial of pulsed corticosteroid therapy for primary treatment of Kawasaki disease. N Engl J Med. 2007;356(7):663–75. https://doi.org/10.1056/NEJMoa061235.
Kobayashi T, Saji T, Otani T, Takeuchi K, Nakamura T, Arakawa H, Kato T, Hara T, Hamaoka K, Ogawa S, Miura M, Nomura Y, Fuse S, Ichida F, Seki M, Fukazawa R, Ogawa C, Furuno K, Tokunaga H, Takatsuki S, Hara S, Morikawa A. Efficacy of immunoglobulin plus prednisolone for prevention of coronary artery abnormalities in severe Kawasaki disease (RAISE study): a randomised, open-label, blinded-endpoints trial. Lancet (London, England). 2012;379(9826):1613–20. https://doi.org/10.1016/s0140-6736(11)61930-2.
Ae R, Abrams JY, Maddox RA, Schonberger LB, Nakamura Y, Kuwabara M, Makino N, Matsubara Y, Kosami K, Sasahara T, Belay ED. Corticosteroids added to initial intravenous immunoglobulin treatment for the prevention of coronary artery abnormalities in high-risk patients with Kawasaki disease. J Am Heart Assoc. 2020;9(17):e015308. https://doi.org/10.1161/jaha.119.015308.
Burns JC. Revisiting once again steroids for the treatment of acute Kawasaki disease. J Am Heart Assoc. 2020;9(17):e018300. https://doi.org/10.1161/jaha.120.018300.
Miyata K, Kaneko T, Morikawa Y, Sakakibara H, Matsushima T, Misawa M, Takahashi T, Nakazawa M, Tamame T, Tsuchihashi T, Yamashita Y, Obonai T, Chiga M, Hori N, Komiyama O, Yamagishi H, Miura M. Efficacy and safety of intravenous immunoglobulin plus prednisolone therapy in patients with Kawasaki disease (Post RAISE): a multicentre, prospective cohort study. Lancet Child Adolesc Health. 2018;2(12):855–62. https://doi.org/10.1016/s2352-4642(18)30293-1.
Son MBF, Gauvreau K, Tremoulet AH, Lo M, Baker AL, de Ferranti S, Dedeoglu F, Sundel RP, Friedman KG, Burns JC, Newburger JW. Risk model development and validation for prediction of coronary artery aneurysms in Kawasaki disease in a North American population. J Am Heart Assoc. 2019;8(11):e011319. https://doi.org/10.1161/jaha.118.011319.
Chan H, Chi H, You H, Wang M, Zhang G, Yang H, Li Q. Indirect-comparison meta-analysis of treatment options for patients with refractory Kawasaki disease. BMC Pediatr. 2019;19(1):158. https://doi.org/10.1186/s12887-019-1504-9.
Crayne CB, Mitchell C, Beukelman T. Comparison of second-line therapy in IVIg-refractory Kawasaki disease: a systematic review. Pediatr Rheumatol Online J. 2019;17(1):77. https://doi.org/10.1186/s12969-019-0380-z.
Chaudhary H, Nameirakpam J, Kumrah R, Pandiarajan V, Suri D, Rawat A, Singh S. Biomarkers for Kawasaki disease: clinical utility and the challenges ahead. Front Pediatr. 2019;7:242. https://doi.org/10.3389/fped.2019.00242.
Lu RM, Hwang YC, Liu IJ, Lee CC, Tsai HZ, Li HJ, Wu HC. Development of therapeutic antibodies for the treatment of diseases. J Biomed Sci. 2020;27(1):1. https://doi.org/10.1186/s12929-019-0592-z.
Burns JC, Mason WH, Hauger SB, Janai H, Bastian JF, Wohrley JD, Balfour I, Shen CA, Michel ED, Shulman ST, Melish ME. Infliximab treatment for refractory Kawasaki syndrome. J Pediatr. 2005;146(5):662–7. https://doi.org/10.1016/j.jpeds.2004.12.022.
Tremoulet AH, Jain S, Jaggi P, Jimenez-Fernandez S, Pancheri JM, Sun X, Kanegaye JT, Kovalchin JP, Printz BF, Ramilo O, Burns JC. Infliximab for intensification of primary therapy for Kawasaki disease: a phase 3 randomised, double-blind, placebo-controlled trial. Lancet. 2014;383(9930):1731–8. https://doi.org/10.1016/S0140-6736(13)62298-9.
Yamaji N, da Silva Lopes K, Shoda T, Ishitsuka K, Kobayashi T, Ota E, Mori R. TNF-α blockers for the treatment of Kawasaki disease in children. Cochrane Database Syst Rev. 2019;8(8):Cd012448. https://doi.org/10.1002/14651858.CD012448.pub2.
Ogihara Y, Ogata S, Nomoto K, Ebato T, Sato K, Kokubo K, Kobayashi H, Ishii M. Transcriptional regulation by infliximab therapy in Kawasaki disease patients with immunoglobulin resistance. Pediatr Res. 2014;76(3):287–93. https://doi.org/10.1038/pr.2014.92.
Portman MA, Dahdah NS, Slee A, Olson AK, Choueiter NF, Soriano BD, Buddhe S, Altman CA. Etanercept with IVIg for acute Kawasaki disease: a randomized controlled trial. Pediatrics. 2019;143(6):e20183675. https://doi.org/10.1542/peds.2018-3675.
Kuo HC, Yang KD, Juo SH, Liang CD, Chen WC, Wang YS, Lee CH, Hsi E, Yu HR, Woon PY, Lin IC, Huang CF, Hwang DY, Lee CP, Lin LY, Chang WP, Chang WC. ITPKC single nucleotide polymorphism associated with the Kawasaki disease in a Taiwanese population. PLoS One. 2011;6(4):e17370. https://doi.org/10.1371/journal.pone.0017370.
Dusser P, Koné-Paut I. IL-1 inhibition may have an important role in treating refractory Kawasaki disease. Front Pharmacol. 2017;8:163. https://doi.org/10.3389/fphar.2017.00163.
Aoyagi R, Hamada H, Sato Y, Suzuki H, Onouchi Y, Ebata R, Nagashima K, Terauchi M, Terai M, Hanaoka H, Hata A. Study protocol for a phase III multicentre, randomised, open-label, blinded-end point trial to evaluate the efficacy and safety of immunoglobulin plus cyclosporin A in patients with severe Kawasaki disease (KAICA Trial). BMJ Open. 2015;5(12):e009562. https://doi.org/10.1136/bmjopen-2015-009562.
Erratum: Efficacy of primary treatment with immunoglobulin plus ciclosporin for prevention of coronary artery abnormalities in patients with Kawasaki disease predicted to be at increased risk of non-response to intravenous immunoglobulin (KAICA): a randomised controlled, open-label, blinded-endpoints, phase 3 trial (Lancet. 2019;393(10176):1128–37. PII: S0140673618320038. DOI: https://doi.org/10.1016/S0140-6736(18)32003-8). Lancet. 2019;393(10180):1504. https://doi.org/10.1016/S0140-6736(19)30810-4.
Kuo HC, Pan CT, Huang YH, Huang FC, Lin YS, Li SC, Huang LH. Global investigation of immune repertoire suggests Kawasaki disease has infectious cause. Circ J. 2019;83(10):2070–8. https://doi.org/10.1253/circj.CJ-19-0206.
Huang YH, Lin KM, Ho SC, Yan JH, Lo MH, Kuo HC. Increased incidence of Kawasaki disease in Taiwan in recent years: a 15 years nationwide population-based cohort study. Front Pediatr. 2019;7:121. https://doi.org/10.3389/fped.2019.00121.
Chi H, Huang YC, Liu CC, Chang KY, Huang YC, Lin HC, Chang LY, Ho YH, Tsao KC, Mu JJ, Huang LM, Hsieh YC. Characteristics and etiology of hospitalized pediatric community-acquired pneumonia in Taiwan. J Formos Med Assoc. 2020;119(10):1490–9. https://doi.org/10.1016/j.jfma.2020.07.014.
Tang Y, Gao X, Shen J, Sun L, Yan W. Epidemiological and clinical characteristics of Kawasaki disease and factors associated with coronary artery abnormalities in east China: nine years experience. J Trop Pediatr. 2016;62(2):86–93. https://doi.org/10.1093/tropej/fmv077.
Park HR, Han MY, Yoon KL, Cha SH, Moon SK, Jung HW. Mycoplasma infection as a cause of persistent fever after intravenous immunoglobulin treatment of patients with Kawasaki disease: frequency and clinical impact. Infect Chemother. 2017;49(1):38–43. https://doi.org/10.3947/ic.2017.49.1.38.
Vitale EA, La Torre F, Calcagno G, Infricciori G, Fede C, Conti G, Chimenz R, Falcini F. Mycoplasma pneumoniae: a possible trigger of kawasaki disease or a mere coincidental association? Report of the first four Italian cases. Minerva Pediatr. 2010;62(6):605–7.
Nanishi E, Nishio H, Takada H, Yamamura K, Fukazawa M, Furuno K, Mizuno Y, Saigo K, Kadoya R, Ohbuchi N, Onoe Y, Yamashita H, Nakayama H, Hara T, Ohno T, Takahashi Y, Hatae K, Harada T, Shimose T, Kishimoto J, Ohga S, Hara T. Clarithromycin plus intravenous immunoglobulin therapy can reduce the relapse rate of Kawasaki disease: a phase 2, open-label, randomized control study. J Am Heart Assoc. 2017;6(7):e005370. https://doi.org/10.1161/jaha.116.005370.
Wang Z, Chen F, Wang Y, Li W, Xie X, Liu P, Zhang X, Zhang L, Huang P. Methylprednisolone pulse therapy or additional IVIG for patients with IVIG-resistant Kawasaki disease. J Immunol Res. 2020;2020:4175821. https://doi.org/10.1155/2020/4175821.
Furukawa T, Kishiro M, Akimoto K, Nagata S, Shimizu T, Yamashiro Y. Effects of steroid pulse therapy on immunoglobulin-resistant Kawasaki disease. Arch Dis Child. 2008;93(2):142–6. https://doi.org/10.1136/adc.2007.126144.
Roberts SC, Jain S, Tremoulet AH, Kim KK, Burns JC, Anand V, Anderson M, Ang J, Ansusinha E, Arditi M, Ashouri N, Bartlett A, Chatterjee A, DeBiasi R, Dekker C, DeZure C, Didion L, Dominguez S, El Feghaly R, Erdem G, Halasa N, Harahsheh A, Jackson MA, Jaggi P, Jain S, Jone PN, Kaushik N, Kurio G, Lillian A, Lloyd D, Manaloor J, McNelis A, Michalik DE, Newburger J, Newcomer C, Perkins T, Portman M, Romero J, Ronis T, Rowley A, Schneider K, Schuster J, Tejtel SKS, Sharma K, Simonsen K, Szmuszkovicz J, Truong D, Wood J, Yeh S. The Kawasaki Disease Comparative Effectiveness (KIDCARE) trial: a phase III, randomized trial of second intravenous immunoglobulin versus infliximab for resistant Kawasaki disease. Contemp Clin Trials. 2019;79:98–103. https://doi.org/10.1016/j.cct.2019.02.008.
Gorelik M, Lee Y, Abe M, Andrews T, Davis L, Patterson J, Chen S, Crother TR, Aune GJ, Noval Rivas M, Arditi M. IL-1 receptor antagonist, anakinra, prevents myocardial dysfunction in a mouse model of Kawasaki disease vasculitis and myocarditis. Clin Exp Immunol. 2019;198(1):101–10. https://doi.org/10.1111/cei.13314.
Koné-Paut I, Tellier S, Belot A, Brochard K, Guitton C, Marie I, Meinzer U, Cherqaoui B, Galeotti C, Boukhedouni N, Agostini H, Arditi M, Lambert V, Piedvache C. Phase II open label study of anakinra in intravenous immunoglobulin-resistant Kawasaki disease. Arthritis Rheumatol. 2021;73(1):151–61. https://doi.org/10.1002/art.41481.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Chang, LS. (2022). Treatment of Kawasaki Disease. In: Kuo, HC. (eds) Kawasaki Disease. Springer, Singapore. https://doi.org/10.1007/978-981-19-2944-1_4
Download citation
DOI: https://doi.org/10.1007/978-981-19-2944-1_4
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-2943-4
Online ISBN: 978-981-19-2944-1
eBook Packages: MedicineMedicine (R0)