Abstract
Breast cancer (BC) is the major cause of death in women worldwide. It is a global issue with nearly 2.3 million patients diagnosed with BC and 0.685 million deaths in 2020 which greatly affects human resources as well as healthcare costs. Besides the development of systemic therapies, radiotherapy (RT) provides long life expectancy and high survival rates in breast cancer patients. With the advent of current radiotherapy planning systems, irradiation of breast cancer has undergone a drastic change. Historically, conventional fractionation techniques using tangential field protocol were considered a benchmark in RT for breast cancer. During the past 15 years, advances in treatment techniques, specifically, RT allows subsequent decline in treatment-related complications. The transition from two-dimensional to three-dimensional treatment planning has drastically decreased long-term cardiac toxicity. Herewith, it is prudent that treatment using radiations is carried out with utmost efficiency. This chapter provides practical as well as theoretical insight into the advances in radiotherapy techniques that are recently used in clinical practice. Besides three-dimensional RT planning, Intensity Modulated Radiotherapy (IMRT), Volumetric Modulated Arc Therapy (VMAT), and proton therapy are other modern treatment options. The other attractive approach which has resulted in shortened treatment duration is the hypofractionated RT technique. In addition, Accelerated Partial Breast Irradiation (APBI) and Deep Inspiration Breath Hold (DIBH) are also reasonable options for low-risk patients and maximal heart protection, respectively. Advanced techniques focus on cardiac sparing or deep breath-hold approaches which provide maximum safety and a decrease in long-term cardiac toxicity. This chapter will provide an up-to-date guide and resource for radiation oncologists, clinicians, and fellows seeking to learn and practice breast cancer radiotherapy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Radiotherapy
- Breast cancer
- Hypofractionated radiotherapy
- Deep Inspiration Breath-Hold Radiotherapy
- Cardiac toxicity
1 Positioning and Immobilization Techniques
Adjuvant RT, which is the fusion of irradiation of breast and breast-conserving therapy (BCT), has become state-of-the-art therapeutic option for BC. Breast irradiation not only contributes to improved outcomes in patients but also reduces the fatality rate. Radiotherapy (RT) of breast cancer can be variable and difficult based on the patient’s anatomy, i.e., axilla depth and concavity of chest wall. The first step is to perform CT simulation for scheduling conformal RT or IMRT using heart-sparing techniques like heart blocking or breathe hold, particularly for patients with left breast cancer (BC). Treatment fields are a combination of the whole breast, axillary fields, internal mammary artery, and supraclavicular. The predominant goal of breast radiotherapy fields is to keep away from hot and cold dose areas among adjoining fields while decreasing radiation dose to healthy surrounding tissues, i.e., heart and lungs. Treatment fields have to be adjusted according to the anatomy of the breast, which because of its irregular surface can originate inhomogeneity in dose. Also, a setup must be designed which can easily be reproduced.
Most patients receiving radiotherapy post breast-conserving therapy (BCT) are treated in the supine position, which is considered as topmost natural position for women. It has advantages such as accuracy, comfort, repeatable positioning, and optimum surgical access to the chest wall. During this position, the mammary gland extends over the chest wall, particularly in heavy-breasted women. Consequently, irradiation of the heart and lungs is unavoidable and the area of skin fold expands. Therefore, radiation-induced toxicity is inexorable (Yu et al. 2018).
Usually, a prone position is recommended for patients with large sagging breasts to reduce late and acute toxicities. The development of modern CT planning techniques has made this position reproducible. The prone technique is advocated not only for patients with large breasts but in most BC patients as it largely reduces the lung and heart within the field (Griem et al. 2003; Cross et al. 1989). However, there are conflicting data on healthy tissue efficiency reduction. Modern RT techniques have eased the exploration of the hypofractionation scheme with the associated boost to the tumor bed in the prone position (Huppert et al. 2011). Initially, a prone position is suggested for heavy-breasted women. Later, reports of decreased doses to lung and heart resulted in the utilization of prone breast irradiation for patients with or without heavy breasts. At the same time, refinements in RT techniques and the advent of DIBH methods, that moves the heart away from the radiation field, result in a significant decrease in radiation doses to OARs even with supine position (Haffty 2018).
According to Würschmidt et al. (2014), the ancillary dose to the LAD (left anterior descending) arterial blood vessel, once the left breast was irradiated in a prone position, was 33.5 Gy versus 25.6 Gy in a sitting position. In comparison, Kirby et al. (2010) also predicted prone position to decrease the heart doses to about 64% of 30 patients treated with whole breast irradiation (WBI) and 24 percentage of the same number of patients treated with partial breast irradiation (PBI) with median reduction is 29.3 Gy, along with decreasing ipsilateral lung (mean) in the whole breast and 61 of 65 PBI cases, and chest wall V (50 Gy) in all WBI cases. According to Varga et al. (2009) randomized clinical trial, the displacement range was greater in this position. In the prone position, the main concern is setup errors and reproducibility in contrast to the standard supine position. Setup errors were lower for supine positioning as compared to prone positioning in such a way: systematic errors: 3.1–4.3 mm (prone) (p = 0.02) and 1.3–1.9 mm (supine) and random errors: 3.8–5.4 mm (prone) (p = 0.02) and 2.6–3.2 mm (supine). Even patient treatment time and comfort scores were compared. Reported clinical target volume and planning target volume margins were determined to be smaller for the supine position (10 mm) than for the prone position (12–16 mm) (Kirby et al. 2011).
Patients with large breasts are recommended to take up the lateral chronic leg position, which is a side-lying posture. Women undergoing breast irradiation have only been treated in this way by experienced centers since it is cumbersome to provide full coverage to the lymphatic region. More than 500 women have been dosed with 50 Gy of WBI using lateral decubitus position, which has been employed at the Curie Institute (Paris). Thin carbon fiber supports and special devices for patient positioning were designed specifically for this position. Suggested techniques have been indicated acceptable dose homogeneity for BC treatment volume, with a very small radiation dose to the underlying organs at risk (Campana et al. 2005). Despite the valid single-center outcomes, this position has not been extensively undertaken for everyday clinical practice.
Although there remain advocates for both prone and supine positions for breast irradiation depending on tumor location, breast anatomy, or other clinical considerations, in which one position may have benefited over another, patients are treated in both positions at most radiation centers. Choice of positioning preference may depend on differences in body habitus, training biases, physician preferences, and tumor size and shape. There is no proof that one positioning technique is superior to the other, but the main concern is that RT is effective and safe whether it is delivered in the supine position or prone position (Haffty 2018).
For the treatments of BC patients, special immobilization devices are designed which are widely used and are commonly available in routine. The well-known devices are recorded as alpha cradle, Vac-fix bag-Vacuum Cradle Bed, Board-Wing Butterfly Board, inclined plane, and breast boards. In the supine position, the simplest and most preferred arrangement has been made with the breast board in conjunction with an inclined plane having an armrest. The patient’s head should be facing to the opposite side, where the arms abduct (90°–120°) and rotated externally. On the stable board, the woman is lying on her back, and the breast board is angled to confirm the breastbone parallel to a table. According to clinical requirements, this angle could be modified, but larger angles can lead to an elevated radiation dose in the patient’s lungs demanding a supraclavicular field. The edge between the supraclavicular field and chest wall is commonly placed at the clavicular head bottom. Radiopaque wires have been exercised to describe breast borders and incisions (Griem et al. 2003). To minimize the dose to healthy surrounding organs, the use of a thermoplastic bra has also been explored. Results suggest that the use of thermoplastic bra provide shallower girder setting for the left-sided BC (medial with bra 288°–315° vs. without thermoplastic bra 302°–325°) and decreased radiation dose to lungs by 30.6% without any specific eligibility criteria for everyday clinical usage (Piroth et al. 2016).
2 Modern Planning and Delivery Techniques
BC is very common in females after cancer of the skin. Timely diagnosis, customized approach to therapy, and more understanding of the disease have all contributed to an increase in BC survival rates and continuous reduction in the number of fatalities associated with the disease.
It is one of the diseases for which the use of radiation for therapeutic purposes has progressed substantially over the last century, such as brachytherapy and EBRT. The use of advanced methods in EBRT has increased largely with time. As a result, the choice of radiation method is critical to cure the tumor and to reduce toxicities. The number of planning approaches have progressed over the past 20 years from 2D to 3D techniques, including IMRT, VMAT, and as well as proton therapy.
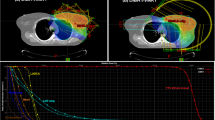
Modern radiotherapy techniques have reduced complications such as scarring of the tissues and long-term cardiac toxicity, while also improving loco-regional control rates, and coronary sparing with 4D-breath-hold techniques. The main purpose to use any appropriate therapy and planning is to deliver a high radiation dose to the tumor while reducing exposure to the surrounding healthy tissues or organs (such as the lung and heart) which are at risk. Figure 18.1 displays the complete process of treatment planning of BC.
2.1 Hypofractionation
In the middle of the 1980s, the hypofractionation (HF) approach has been familiarized and used in numerous departments of radiotherapy. Over the years, the HF approach was known by the number of statements. This term is defined as “fewer treatments” while conventionally 5–6 fractions are administered per week.
HF radiation therapy is the one in which total radiation dose is broken into large fractions and radiation doses are delivered often every day. Similar to conventional RT, the objective of HF is to destroy breast cancer cells, but through larger doses of radiation in fewer sessions. Its main advantage is to increase the dose of biological radiation to cancer without increasing the radiation dose to late responding healthy normal tissues. HF is the form of EBRT that releases X-ray beams of high-energy carefully targeted at the breast. Conventional radiations are supplied via the same machine, but with HF, tumors receive a higher radiation dose for each treatment session. So the course of RT is completed more rapidly using HF. When breast cancer patients experience a type of surgery that’s planned to keep as much of their breast tissue as possible, HF RT can also be used as follow-up therapy.
The two important benefits for employing the HF approach are:
First of all (Friberg and Ruden 2009), once megavolt machines have been familiarized, very deep tumors might be treated which increases demand for radiotherapy. No consistent increase in total treatment units was observed so it takes short time for treatment. With fewer fractions for each patient, additional patients might be treated over time. Secondly, HF can ease the problem for cancer patients that they don’t have to travel to the hospital every single day for treatment purpose.
With the passage of time, it was obvious that these treatment schedules might also harm patients. From the identified patients, radiation-induced injuries were noted, i.e., paralysis of the arm, edema of hand or arm, fractures in arms and thoracic skeleton, immobilization of shoulder, heart disease, respiratory distress, horner syndrome (due to damage to the sympathetic chain), and hoarseness. The main advantage is convenience because in fewer sessions’ patients can achieve full radiation treatment. Breast swelling (breast edema) as well as fatigue, skin itchiness, and skin irritation were less common among the women who received HF compared to other forms of RT techniques. Moreover, there is a reduced demand on equipment, time, and staff making HF a very resource-efficient approach while providing identical result for the patients. Gilbert Fletcher (1988) has defined the HF approach as: “The maximum time of patient treatment is consumed on arrangements, but the real-time for treatment is simply a part of total time, it has been reasonable to reduce the machine time by fewer large fractions.”
2.2 Whole Breast Irradiation
For the EBC, the standard of care has advanced from the modified-radical mastectomy (MRM) to breast conservation therapy (BCT), which consists of nodal basin evaluation, lumpectomy (partial mastectomy), and 5 weeks (Goldberg and Whelan 2020) or 5–7 weeks (Sanders et al. 2007) of the WBI (standard dose of almost 50 Gy). Based on patients and the tumor characteristics, an extra increased dose of 10 or 16 Gy is provided to the tumor bed (Bartelink et al. 2015). Today, HF regimes with a dose of 15–16 fractions are the favorite regimes (Miranda et al. 2019). Whole breast irradiation, as part of BCT, has low toxicity, good cosmesis, and well-established results. Current examinations have observed tumor control rates and the toxicities related to the shorter radiation delivery options. HF-WBI includes treating the WB with a greater dose of radiation on a daily basis. The following study state HF-WBI as an accelerated WBI (Shaitelman et al. 2014). Theoretical arguments in support of shorter radiation therapy courses expected that these treatments lead to more patient conformity, greater choice of breast conservation over the mastectomy, improved life quality, and cost efficiency to the patient and the wider national healthcare organization (McCarthy et al. 2006). In APBI, the area in which radiation is being targeted is different compared with WBI, so this is examined that an approach concerns to different toxicity rates as well as local control rates. Several consensus guidelines were reported for HF-WBI and APBI to give guidance to the physicians on the best patients for these different approaches outside the medical trials settings (Smith et al. 2011; Shah et al. 2013). As most of the BC recurrences occur near the cavity of lumpectomy, APBI administered entirely to a small volume of tissues near an original lumpectomy position has achieved greater attention and is discussed now as a replacement to WBI.
2.2.1 HF Whole Breast Irradiation (HF-WBI)
WBI treats a whole breast with 2.5 or 3.20 Gy every day for the total dose of about 39 or 42.5 Gy/13–16 fractions over 3–5 weeks (Whelan et al. 2002, 2010; Yarnold et al. 2011) or hypofractionated WBI treats with 40 or 42.5 Gy in 15–16 fractions for 3 weeks (Smith et al. 2011). Hypofractionation, as compared to conventional fractionation, requires a shorter course of treatment, reduced number of fractions, and total dose, and results with lower costs and improved patient convenience. In several past years, so many randomized trials have tested hypofractionation in contrast to conventional fractionation after BCS for the patients of BC (Whelan et al. 2010; Yarnold et al. 2011). For appropriately selected patients, these experiments initially described in 2005 revealed that HF yields overall survival and disease-free survival rates compared to conventional fractionation (Whelan et al. 2010; Yarnold et al. 2011; Haffty and Buchholz 2013). Moreover, recently reported follow-up of 10 year of these trials have revealed that conventional and hypofractionation have similar long-term toxicity profiles (Haffty and Buchholz 2013; Whelan et al. 2010). As a consequence, clinical practice guidelines were published recently, establishing HF as a suitable therapeutic option mostly for early breast cancer patients (Smith et al. 2011). The reasons for the slow adoption of HF-WBI are multifactorial, together with concerns about struggles achieving the dose homogeneity and reducing acute toxicity while supplying a greater dose per fraction for women with large breasts.
2.3 Partial Breast Irradiation (PBI)
WBI is related to the dose-dependent, lung cancer (Taylor et al. 2017) and higher occurrence of cardiotoxicity, with the gradual increase in the hazard over time after exposure. It is very important to give proper attention to long-term toxicity in women who were cured of early breast cancer. PBI is a limited form in which radiation is focused on a tumor volume, the place for the majority of recurrences (Smith et al. 2000). By supplying radiation dose to a reduced selected volume, PBI lowers radiation exposure to organs at risk comprising skin, lung, ribs, heart, and contralateral breast tissue; thereby minimizing potentially late adverse effects. The number of studies have described the higher risk for toxicity (Huo et al. 2016) and local recurrence (Liu et al. 2017; Korzets et al. 2019). Previous meta-analyses have revealed that PBI is related to less number of deaths as well as the absence of BC recurrence (Liu et al. 2017). The main outcome IBTR and chronic and acute toxicities at 5 years with partial breast irradiation are compared with whole breast irradiation in numerous randomized trials. Ipsilateral breast tumor recurrence rates remained similar among WBI and PBI with no notable changes observed with PBI techniques. However, partial breast irradiation has fewer chronic and acute toxicities than WBI (Shah et al. 2021). During past decades, partial breast irradiation has appeared to replace WBI.
2.4 Accelerated Partial Breast Irradiation (ABPI)
APBI technology was initiated in the 1990s (Ribeiro et al. 1990) into clinical practice together with many techniques, such as 3D conformal radiotherapy, intraoperative RT with photons or electrons, single brachytherapy, multicatheter, and intensity-modulated radiotherapy. APBI offers several benefits over traditional radiation therapy. Because in APBI, the radiation beams are focused so narrowly, therefore exposure to healthy tissues and organs in the adjacent area containing the lungs, heart, muscles, ribs, and skin can be reduced. With APBI, acute radiation side effects (ARS) are usually minor. After APBI, late radiation side effects (LRS) are fairly less common but comprise adverse breast cosmesis, or fat necrosis, fibrosis, telangiectasia’s, and focal skin pigmentation variations (Correa et al. 2017).
BCS together with the whole breast irradiation was gold-standard therapy for the early EBC patients, which can produce cancer outcomes similar to the mastectomy (Formenti et al. 2012a). Whereas whole breast irradiation is mostly well tolerated, it brings the risk of late effects, for example, radiation pneumonitis, secondary malignancy, and cardiotoxicity. Whole breast irradiation is typically carried once a day over several successive weeks, making access to effective radiotherapy challenging for women suffering from some socioeconomic obstacles. After BCS, recurrence patterns recommend that maximum local recurrences take place mostly at or adjacent to the breast tissue or nearby post-excision lumpectomy cavity (Veronesi et al. 2001). It is predicted that 15–25% (Wenz et al. 2015) of candidates undergoing BCS may be eligible for the APBI, i.e., patients with minor invasive ductal breast cancer (IDBC) without involvement of lymph node. The standards of patient selection having ages above 40, status post-lumpectomy, negative clinical lymph nodes, BC (in situ OR invasive disease) measuring <3 cm, negative margins (at least 2 mm), and no lymph vascular space invasion (LVSI). Women with EBC and their caretakers must be familiar with this favorable treatment option. APBI irradiates only tumor beds in 1–3 weeks (Correa et al. 2017), as it decreases the problem of care so it is a favorable treatment for many patients. Moreover, owing to the reduced irradiation range of accelerated partial breast irradiation, it is predicted to decrease harms and increase life quality and cosmetic effect than WBI (Mouw and Harris 2012).
2.5 Deep Inspiration Breath Hold (DIBH)
The BH approach was first reported in treatment BC in 2001 (Sixel et al. 2001) and became well-known (Lai et al. 2020) only recently. Its greatest benefit is that it delivers less amount of radiation dose to the lungs and heart (Lai et al. 2020; Latty et al. 2015). However, the extent of advantages varies individually according to the lung capacity and anatomical features (Latty et al. 2015) of the patients; with the rarity of cases having no benefits (Sixel et al. 2001) or even higher heart doses (Dell’Oro et al. 2019) have been reported. In BC radiation therapy, deep inspiration breath-hold is a very dominant heart-sparing technique.
In BC management, RT has played an important role for decades. On an individual basis, important changes have been observed in the radiotherapy practice focusing on optimized care, owing to the convenience of modern RT technologies. Maximum of the candidates after BCS require postoperative whole breast irradiation with or without a boost to the tumor bed, while PBI is sufficient in low-risk cases. The irradiation of the chest wall (CW) is needed infrequently unless combined with the post-mastectomy irradiation and nodal irradiation.
Most patients with breast cancer are long-term survivors, therefore therapeutic interventions do not endanger the candidates’ well-being and overall health. The main dangers due to radiations are lung damage and radiogenic heart resulting in important morbidity numerous decades or years after RT (Darby et al. 2005). The additional risk of cardiac mortality or secondary lung cancer was valued as 0.04 and 0.11 per 1 Gy rise of the radiation dose to a heart and whole lung, respectively (Taylor et al. 2017). Radiation-induced heart disease (RIHD) mostly shows the damage of capillary and coronary vessels of the heart which makes a progressive process of fibrotic leading to circulatory changes with possibly fatal ischemic heart disease (IHD) (Andratschke et al. 2011). The harmful effect of dose-dependent radiation disclosure to the heart has been revealed in retrospective analyses and simulations of radiotherapies of the patients of BC, with IHD (van den Bogaard et al. 2017). The radiation dose to the heart and therefore radiation-induced heart disease (RIHD) incidence is greater in the case of left sides and the hazard is more probable in the young patients (Jacobse et al. 2019). It is expected that every 1Gy dose to the heart increases the IHD incidence by 7.4% that might be enhanced by smoking (Taylor et al. 2017) and pre-existing cardiovascular hazard issues (Darby et al. 2013).
In the systematic evaluation of contemporary publications, a 3.7 and 5.2 Gy dose to heart in right and left sides, respectively, whereas the radiation dose of 9 Gy (Taylor et al. 2017) to an ipsilateral lung is recommended. Hence, a lot of struggles have been put to avoid or reduce the heart exposure.
There are numerous methods to save the heart from exposure to radiation. Breathe hold and prone positioning techniques work by sparing the heart from the radiation fields. The advanced proton irradiation and IMRT approaches are not applied extensively, but the small volume to be treated during PBI or exclusion of RT are choices in case of low risk. These approaches have changeable effects on heart and lung exposures: whereas prone RT lessens lung doses dramatically (Kahán et al. 2018). Figure 18.2 shows the treatment length of five radiotherapy techniques used in the treatment of BC.
2.6 Three-Dimensional Conformal RT (3D CRT)
Better computerized treatment planning systems make it easier to develop several treatment plans for a patient. The long-term cardiac toxicity of breast irradiation is one of the most significant issues. The risk of long-term severe cardiac problems linearly increases with the mean radiation dose to the heart, with an estimated risk of 7.4% reported with each 1 Gy rise in mean heart dose. Covering the whole breast parenchyma with a standard 2D tangential beam approach is sometimes difficult. This difficulty can be overcome using the conformal technique (Darby et al. 2013). 3D-CRT treatment is a sophisticated approach that employs imaging technology to produce a three-dimensional image of a patient’s tumor as well as surrounding organs and tissues. As a result, malignant cells might be exposed to a larger and more effective dosage of radiation.
A major problem is to improve the radiation dose uniformity to the target tumor volume while reducing the risk of complications related to treatment. In current years, particularly conformal RT, inverse or forward IMRT, which is a sophisticated and more advanced method of 3DCRT, is becoming attractive for breast irradiation because it gives improved normal tissue sparing and reduced inhomogeneity (Cheung 2006). Simultaneously, the radiation dose obtained by the surrounding healthy normal tissues might be considerably lowered. 3D-CRT is utilized to treat cancers that were previously thought to be too near to essential organs and structures for radiation treatment. For example, 3DCRT permits radiation to be administered to malignancies in the neck and head while reducing exposure to the salivary glands, spinal cord, optic nerve, and other vital tissues.
If 3D-CRT is indicated for a patient, a radiologist will use one of the following imaging methods to produce three-dimensional pictures of the tumor and surrounding tissues:
-
Computed tomography (CT)
-
Positron emission tomography-computed tomography (PET-CT)
-
Positron emission tomography (PET)
-
Magnetic resonance imaging (MRI)
Because 3D CRT provides for more precise and accurate radiation treatment delivery, it may be suggested for malignancies near critical organs.
2.7 Intensity-Modulated Radiation Therapy (IMRT)
IMRT is a new excellent form of 3DCRT and is increasingly adopted for the treatment of BC. As the likelihood of dose inhomogeneity increases for women with large breasts, IMRT is the technique of choice. Patients of left-sided BC are more likely to benefit from this technique to decrease dose to heart, contralateral breast irradiation, and deep-seated tumor bed irradiation. Anatomical complexity and variations in-depth of regional nodal regions have made the breast a particularly difficult area to treat with radiation. IMRT is a kind of cancer therapy that uses sophisticated computer algorithms to calculate and administer radiations directly to cancer cells from a variety of angles. It enables cancer patients to get greater, more effective radiation doses while reducing harm to healthy tissues and organs surrounding them. This improves the chances of a cure while decreasing the probability of adverse effects.
Firstly, the patient will undergo an imaging test known as a CT scan, which will map her tumor in 3D. Then, by using modern computer algorithms a team of radiation treatment professionals, including physicians and physicists, will calculate and administer radiations directly to the tumor from various angles. A radiation therapist will place the candidate on the treatment table at the start of each treatment session, putting marks on the skin to determine where the radiation therapy will be delivered. Treatment sessions are not painful. The 3D CT scan determines the form, size, kind, and position of the tumor, which instructs the clinician on how to alter the IMRT beam to attack the tumor while avoiding healthy tissues. A moveable gantry of the linear accelerator will provide an X-ray beam to the tumor, and a computer within the accelerator will modify the form of the beam to match the shape of the tumor using a device known as a multi-leaf collimator. By adjusting or modulating the direction and intensity of the radiation beam, the collimator will enable increased dosage to the tumor while protecting healthy tissue from the radiation. As compared to traditional RT techniques, IMRT reduces toxicity to OARs and improves the quality of life. Computerized dose estimates are used in combination with 3D computed tomography (CT) scans to calculate how much radiation should be applied based on tumor shape. Multiple fields of IMRT coming from dissimilar beam directions are commonly combined to produce a custom-tailored dose of radiation that boosts tumor dose while decreasing exposure to normal organs.
IMRT corrects 3DCRT flaws and improves dosage distribution.
-
IMRT plans are computer-generated plans that give rise to complicated field forms by using several tiny fields termed beamlets to avoid key normal structures.
-
IMRT plans adjust the number of fields and the intensities within each field to provide more precise doses to cancer while saving normal tissues from damage.
-
To improve treatment results, IMRT also aids in dosage escalation to the tumor.
-
Reduced toxicity also improves the quality of life for many people.
Even when dosages are not raised, IMRT has the potential to minimize treatment toxicity. Thus, IMRT may be a therapeutic option if the patient has already had conventional radiation therapy and is having recurring tumors in the treated region. Radiation treatment, especially IMRT, inhibits cancer cell division and proliferation, therefore reducing or halting tumor development.
Each IMRT treatment plan can be customized for individual cases by varying the collimator angle, gantry angle, and shaping the tangential fields with MLC leaves so that primary tumor volume is adequately covered while OARs are excluded from high dose region simultaneously. Treatment field modification for each patient should be applied with great caution while taking the location of the primary tumor area, the contour of the breast, and normal tissue anatomy into consideration. Forward treatment planning using the field-in-field method gives outstanding dose homogeneity in the irradiated regions. However, a more advanced IMRT technique, i.e., inverse planning is used in the case of the highly complex target volume (Vicini et al. 2002). Several other IMRT techniques, forward planned step-and-shoot method, arc therapy, topotherapy, static or dynamic MLC-based IMRT, and tomotherapy, can all improve dose homogeneity (Caudrelier et al. 2009). The superiority of IMRT over 3DCRT in terms of dosimetric results is documented in the literature, providing excellent tumor coverage and better sparing of OARs (Fong et al. 2009; Yim et al. 2015; Hall and Wuu 2003). Moreover, dosimetric studies have successfully documented better cosmesis and low skin toxicity using the IMRT technique (Freedman et al. 2006; Pignol et al. 2008). The risk of moist dermatitis was found to be associated with the size of the breast. These trials report a significant reduction in moist dermatitis using IMRT. It was found that more skin toxicity is reported in patients with medium breast volume as compared to large or small breast volume when treated with IMRT (Pignol et al. 2008). Some IMRT approaches are considered better at sparing one structure, while others are good at sparing other structures. There is no disagreement in the amount and orientation of radiation beams being used among different planning studies. An arc of 180°–360° and up to 11 beams are recommended. Because of the use of sharp dose gradients in this technique, an effect due to breathing motion and errors in patient setup procedure for dose distribution must be taken into consideration, when evaluating the benefits of IMRT over the 3DCRT technique (Erven et al. 2008). Expertise in treatment planning beginning from immobilization of tumor to treatment confirmation, rigorous quality assurance (QA), and toxicity evaluation is crucial before executing the IMRT approach to avoid unessential high doses to OARs to obtain tumor coverage.
2.8 Volume Modulated Arc Therapy (VMAT)
VMAT is a novel RT technique that supplies a continuous dose of radiation during the rotation of the treatment machine. This is a kind of IMRT where the dosage is delivered in arcs ranging from 0° to 360° as it rotates. As a result, dosage compliance improves as a result of this increase in flexibility. Due to its ability to administer radiation at faster rates, VMAT reduces the entire treatment time to less than 5 min (compared with IMRT treatment which takes approximately 20–30 min). VMAT may be used to create complex plans that are difficult to develop using IMRT. VMAT planning and treatment are precisely challenging and necessitates a high level of accuracy. The VMAT technique, like a three-dimensional conformal therapy, generally takes approximately 20 min. The majority of this time is spent precisely situating the patient. Daily X-ray scans are obtained to ensure that everything is as planned. VMAT employs the same sort of radiation as other forms of radiotherapy.
RT is an essential element of a multidimensional approach to treat BC and, depending on the number of factors, a variety of fractionation schemes and treatment approaches have been examined and analyzed successively. As reported by published data, VMAT finds limited clinical applications for breast cancer treatment, yet it is possibly the preferred solution applicable to partial or whole breast treatment and conventional or modified fractionation schemes. Also from a technological standpoint, attractive alternatives of the VMAT technique have been tested and tried out by computer software or simulation to investigate upcoming prospects (Cozzi et al. 2017; Liu et al. 2016).
2.9 Proton Therapy
Photons employed in conventional radiation therapy have different dosimetric characteristics than protons. Currently, photon (X-ray)-based intensity-modulated external beam radiotherapy is the most frequent radiation treatment for most malignancies. Charged particles, especially intensity-modulated proton therapy, are being used in more effective and noninvasive radiation for malignant diseases as a result of recent technological, scientific, and clinical research developments. Most of the energy of proton beams is concentrated in their outermost range (the Bragg peak), leading to an increase in radiation dose to clinical targets and a decrease in radiation doses to nearby normal tissues. The linear energy transfer (LET) of photon beams is low but in proton beams the spread-out Bragg peak (SOBP) is high. Due to this, proton beam treatment has specific biological advantages over photon radiation (Mohan et al. 2013).
Researchers investigated both the likelihood of recurrence and cardiac toxicity induced by poor radiation dose coverage on lymph nodes (LN) targets in BC (Stick et al. 2017). Forty-one candidates with left-sided BC required adjuvant complete nodal irradiation were compared to “realistic” photon programs. Darby et al. (2013) models were used to estimate cardiotoxicity risk. Twenty randomized controlled trials were used to estimate recurrence risk following a compromise in LN coverage. The increased absolute cardiac morbidity was low. Using photons, the probable further risk of BC recurrence after 10 years was 0.1%, while using protons, it was just 0.02%. It was found that proton therapy can lower the predicted cardiac toxicity risk up to 2.9% and the chance of the return of BC by 0.9% for individual candidates. Several further studies confirmed the dosimetry benefits of protons over current photon techniques (Cuaron et al. 2015; Mast et al. 2014; Bradley and Mendenhall 2018). The lung volume getting 20 Gy (V-20) when using photons was 30% greater than when using protons, and the heart dosage was 4–10 Gy as compared to 1 Gy when using photons (MacDonald et al. 2013). According to available studies, based on normal dosage procedures, proton treatment can retain the mean cardiac dose below or at 3 Gy (RBE), which includes lymphatics, even the most complex chest wall irradiation. It’s not clear whether photon-based RT can keep these individuals’ dosages at the same lower level. Numerous organizations use different approaches to maximize the distribution of doses. Heart and coronary artery dosage vary widely based on the candidate anatomy, such as the heart’s closeness to a chest wall and the chest wall curve.
3 Toxicity Concerns
Although BC is the second major cause of cancer mortality among women worldwide, the annual rate of death from this disease has declined steadily over time (Breasted 1930; Rahusen et al. 2002). This substantial decrease is believed to have resulted from increased use of screening mammography and immense improvement in treatment. The use of mammography results in early detection of abnormal growth of tissues is limited to lactiferous ducts, known as ductal carcinoma in situ (DCIS). Soon after the breakthrough of X-rays by Roentgen in 1895, a second-year medical student in Chicago, Emil Grubbe, have claimed to irradiate breast cancer patient in 1896. He safeguarded the adjacent skin surrounding the tumor with tinfoil. Later on, German scientist Herman Gocht delivered radiations to two women with advanced BC cases while guarding the skin with flexible lead (Gocht 1897; Bland et al. 2018). Although toxic after-effects of radiotherapy are generally mild in most women, well-being may be impaired by these effects, at the minimum in the initial period after radiotherapy. One of the major obstacles in the analysis of radiation dose delivered to various parts is that the multitude of parameters is variable, such as patient’s weight and height, shape and size of the breast, and treatment modality. Thus, retrospective study of radiations administered to different parts of breast should be interpreted with caution (Schnur et al. 2011; Raj et al. 2006). One study suggested the factors that impact RT-induced toxicity are woman’s buildup, such as breast size and weight bring about additional skin folds and spreading within these folds, rather than radiation dose inhomogeneity. So, careful patient positioning is necessary at the time of simulation to eradicate these skin folds as much as can be achieved. Supine position is advocated to remove these folds and decrease spreading (Formenti et al. 2012b). Women undergoing treatment are recommended to routinely use cotton pads placed in the inframammary fold (IMF) to lessen the effect of skin reaction (Back et al. 2004).
3.1 Breast Cancer Screening Techniques
The American Cancer Society recommends regular mammographic screening in women ages 55 years and older (Berry et al. 2005). However, in younger women, it is a concern that mammographic screening may be less sensitive due to dense breast tissues. Magnetic resonance imaging is currently under consideration as an alternate screening technique for young women. Nonetheless, investigators are concerned about the False-Positive Rate (FPR) of MRI screening. Although screening mammography does involve an added dose of radiation, the exposure is negligible, so it is a widespread inexpensive early detection tool to aid in the diagnosis of BC. It is reasonable to screen patients for second cancers before their expected development. Most often RT-induced cancers develop within 10–15 years after radiotherapy, so a patient should be screened about 8–10 years after being treated with radiations between ages 20 and 30 years. The likelihood of developing secondary breast cancer before ages 25–30 is very rare (Aisenberg et al. 1997), so a woman treated before 20 may start undergoing screening at the age of 25 (Raj et al. 2006). With new techniques, less radiation is delivered to the heart even to patients which have tumors on the left side. Though new treatment techniques such as IMRT, breathe hold technique, and hypofractionation have limited the radiation-induced cardiac toxicities to large extent, still the skill of radiation oncologist to use the technique remains one of the most important factors in reducing radiation dose to the heart. Evidence from numerous studies suggests that patients irradiated during adolescence have a higher risk of developing secondary BC since the rampant growth of breast tissues during puberty time subject these patients to DNA damage in mammary epithelial cells (MECs). For patients of ages greater than 30 years, only a little increase in the probability of secondary cancer was observed (Aisenberg et al. 1997; Swerdlow et al. 2000). Various studies regarding mantle radiation have demonstrated that for low dose range, i.e., 5 Gy, there is the linear rise in the risk of breast cancer with dose (Mattsson et al. 1993; Little et al. 1999; Boice 2001; Preston et al. 2002). For high radiation dose, i.e., 20 Gy, it was found that high doses were co-related with a high probability of breast cancer development.
3.2 Skin Toxicity
Skin toxicity is the most typical acute impact of breast carcinoma. It ranges from erythema (redness) to desquamation (peeling of the skin), necrosis, and ulceration. This scale of skin irradiation is called “skin toxicity.” Skin toxicity is observed in 75–100% of patients undergoing radiotherapy treatment. During radiotherapy treatment of breast cancer, skin toxicity may bring about physical irritation, emotional suffering, and body image concerns (Schnur et al. 2011).
Skin toxicity occurring within 3 months post-irradiation is called early reaction and if a reaction occurs after 3 months, it is known as a late reaction. There are approved process of assessment of toxic effects on the skin using Radiation Therapy Oncology Group (RTOG) scoring as depicted in Fig. 18.3 (Wong et al. 2011).
3.3 Cardiac Toxicity
Particular awareness has been devoted to the possible cardiac toxicity of breast radiotherapy in recent years. Many young women receiving radiotherapy demonstrate the risk of long-term cardiotoxicity and increased probability of developing secondary breast cancer. While many breast cancer patients completely recover from the disease, there is a serious concern about the long-term risks of treatment. Detection of early-stage disease and improvements in treatment modalities have increased breast cancer survival, but cardiotoxicity, which is one of the major reactions of BC therapy, remains the area of concern. Side effects of cancer treatment using anthracyclines have been established for 30 years, but acute effects of cardiotoxicity due to radiotherapy and chemotherapy have been investigated more recently. Pericarditis, pericardial effusion, and arrhythmias are commonly diagnosed cardiac problems post-radiation therapy. If the radiation syndrome to intimal coronary endocytes and pericardial is severe, it finally leads to fibrosis and myocyte ischemia in the long run. Radiation toxicity to coronary endocytes causes inflammation, ultimately leading to the blood clot. It has been observed that cardiac diseases post-radiotherapy are more frequent in women receiving radiation dose to the left breast, but the situation has changed a lot with current treatment modalities (Yeboa and Evans 2016).
The major drawback of using the older RT approach for treating BC and draining lymph nodes is that a fairly high radiation dose is delivered to heart volume. There exist clear and strong evidence of cardiovascular morbidity and mortality in patients dosed with old techniques. Although radiation exposure to the cardiovascular system is considerably reduced by the use of modern radiotherapy techniques, it is not eliminated. Numerous studies of Hodgkin’s disease survivors have indicated the risk of developing secondary BC post-mantle field radiation therapy for this disease. The risk of BC development after mantle field radiotherapy appears to be dependent on factors such as radiation dose administered to healthy surrounding tissues, patient’s age at the time of breast irradiation, and if chemotherapy is included in the entire treatment planning process. It is noteworthy that besides late cardiac complications associated with tangential breast radiotherapy; others include rib fracture, lymphedema, pneumonitis, brachial plexopathy, and poor cosmesis. These concerns have led investigators in the modification of radiotherapy techniques to reduce not only the volume but also the dose of incidental cardiac irradiation (Raj et al. 2006).
Recent researches have proposed that the magnitude of heart toxicity has decreased due to the use of more conformal techniques (Giordano et al. 2005). However, perfusion defects are detected even in patients suffering from BC treated with modern RT techniques (Marks et al. 2005). Several studies indicated the hike in the risk of ischemic cardiac events post-radiotherapy for left-sided BC though the exact magnitude of this risk is lowered (Feng et al. 2011). Current explorations have also indicated that other heart risk factors such as smoking, hypertension, and radiation-induced damage may be synergistic in their effects (Harris et al. 2006; Hooning et al. 2007). Therefore, women with a considerable probability of net gain should not avoid radiotherapy just on account of the concerns related to cardiac toxicity. Since minimizing radiation dose to the heart is a worthy endeavor, cautious treatment planning is necessary to ensure that patient’s risks are minimized (Jagsi 2014). Figure 18.4 represents a summary of publications to investigate clinical evidence of radiation-induced cardiac toxicities for breast cancer patients.
3.4 Comparison of RT Techniques for Breast Cancer
Approaches to decrease radiation dose to the heart are currently under investigation. These techniques encompass respiratory gating and deep inspiration breath-hold, heart blocks, tomotherapy, mixed electron/photon beams, and IMRT. Oftentimes, breast treatment is inevitable for suitable coverage of axillary lymph nodes. There is a dire need to search for different strategies to prevent the development of cancer in such patients. For the present, it is crucial to screen these patients carefully for the development of secondary BC. It is expected that modern treatment methods and modalities, such as mixing photon and electron beams, use of protons, and cone-beam CT, will cause the decrease in PTV margins, which will eventually result in better sparing of healthy organs (Vicini et al. 2007).
With the increase in the treatment of BC using radiations over time, it is necessary to be well informed about the long-term cardiotoxic effects. Meta-analyses reported the increase in mortality due to cardiovascular causes for women undergone radiotherapy treatment from the 1960s to 1980s (Group 2000). Thus, radiation oncologists and medical physicists face the challenge to develop novel ways of breast cancer treatment without delivering excessive doses to the heart. There have been a lot of advancements in cardiac avoidance which include careful patient positioning and verification, heart blocking, APBI, DIBH, active breathing technique, hypofractionation, IMRT, and use of protons. DIBH is one of the most beneficial techniques in BC RT as it involves gating radiation doses to deliver treatment when the least cardiac volume is in the field (Yeboa and Evans 2016).
Comparison of different modalities reveals that median cardiac volume receiving dose higher than 50% of was reduced from 19% to 3% with DIBH (Lu et al. 2000). Hence, DIBH or inspiratory gating greatly reduces the heart volume and toxicity in the current era. APBI is another modality of cardiac avoidance and treats the fraction of normal breast. Hypofractionation of WBRT has equivalent cosmesis and clinical outcomes. Proton therapy is also widely used as it is also reported to reduce the cardiac dose. Comparison of proton therapy with DIBH photon IMRT reveals that the mean radiation dose to the heart was decreased from 1.6 to 0.009 Gy with the use of proton therapy (Yeboa and Evans 2016).
Technological advancements in radiotherapy have played a crucial role in improving disease control and toxicity outcomes. The aim is to minimize radiation exposure to non-targeted tissues, mainly lung and heart, while enhancing the dose to critical breast cancer tumors, including regional lymph nodes. The choice of treatment modality depends largely on the laterality of breast cancer and patient anatomy. Prone positioning or DIBH is used to achieve physical displacement of the heart from the breast. IMRT and VMAT are preferred over 3D-CRT in cases when a high dose is to be delivered to the target region and at the same time smaller doses to contralateral breast and lung tissues. Proton therapy also improves target coverage and reduces integral doses to OARs. Hypofractionation scheme further improves the outcomes, but at least 10 years of follow-up is required to confirm the expectations (Erven et al. 2008).
References
Aisenberg AC, Finkelstein DM, Doppke KP, Koerner FC, Boivin JF, Willett CG (1997) High risk of breast carcinoma after irradiation of young women with Hodgkin’s disease. Cancer 79(6):1203–1210
Andratschke N, Maurer J, Molls M, Trott K-R (2011) Late radiation-induced heart disease after radiotherapy. Clinical importance, radiobiological mechanisms and strategies of prevention. Radiother Oncol 100(2):160–166
Back M, Guerrieri M, Wratten C, Steigler A (2004) Impact of radiation therapy on acute toxicity in breast conservation therapy for early breast cancer. Clin Oncol 16(1):12–16
Bartelink H, Maingon P, Poortmans P, Weltens C, Fourquet A, Jager J, Schinagl D, Oei B, Rodenhuis C, Horiot J-C (2015) Whole-breast irradiation with or without a boost for patients treated with breast-conserving surgery for early breast cancer: 20-year follow-up of a randomised phase 3 trial. Lancet Oncol 16(1):47–56
Berry DA, Cronin KA, Plevritis SK, Fryback DG, Clarke L, Zelen M, Mandelblatt JS, Yakovlev AY, Habbema JDF, Feuer EJ (2005) Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med 353(17):1784–1792
Bland KI, Copeland EM III, Klimberg VS (2018) History of the therapy of breast cancer. In: The breast. Elsevier, Amsterdam, pp 1–19. e13
Boice JD Jr (2001) Radiation and breast carcinogenesis. Med Pediatr Oncol 36(5):508–513
Bradley JA, Mendenhall NP (2018) Novel radiotherapy techniques for breast cancer. Annu Rev Med 69:277–288
Breasted JH (1930) The Edwin Smith surgical papyrus: published in facsimile and hieroglyphic transliteration with translation and commentary in two volumes
Campana F, Kirova YM, Rosenwald J-C, Dendale R, Vilcoq JR, Dreyfus H, Fourquet A (2005) Breast radiotherapy in the lateral decubitus position: a technique to prevent lung and heart irradiation. Int J Radiat Oncol Biol Phys 61(5):1348–1354
Carr ZA, Land CE, Kleinerman RA, Weinstock RW, Stovall M, Griem ML, Mabuchi K (2005) Coronary heart disease after radiotherapy for peptic ulcer disease. Int J Radiat Oncol Biol Phys 61(3):842–850
Caudrelier J-M, Morgan SC, Montgomery L, Lacelle M, Nyiri B, MacPherson M (2009) Helical tomotherapy for locoregional irradiation including the internal mammary chain in left-sided breast cancer: dosimetric evaluation. Radiother Oncol 90(1):99–105
Cheung K (2006) Intensity modulated radiotherapy: advantages, limitations and future developments. Biomed Imaging Interv J 2(1):e19
Correa C, Harris EE, Leonardi MC, Smith BD, Taghian AG, Thompson AM, White J, Harris JR (2017) Accelerated partial breast irradiation: executive summary for the update of an ASTRO evidence-based consensus statement. Pract Radiat Oncol 7(2):73–79
Cozzi L, Lohr F, Fogliata A, Franceschini D, De Rose F, Filippi A, Guidi G, Vanoni V, Scorsetti M (2017) Critical appraisal of the role of volumetric modulated arc therapy in the radiation therapy management of breast cancer. Radiat Oncol 12(1):1–12
Cross MA, Elson HR, Aron BS (1989) Breast conservation radiation therapy technique for women with large breasts. Int J Radiat Oncol Biol Phys 17(1):199–203
Cuaron JJ, Chon B, Tsai H, Goenka A, DeBlois D, Ho A, Powell S, Hug E, Cahlon O (2015) Early toxicity in patients treated with postoperative proton therapy for locally advanced breast cancer. Int J Radiat Oncol Biol Phys 92(2):284–291
Darby SC, McGale P, Taylor CW, Peto R (2005) Long-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer: prospective cohort study of about 300 000 women in US SEER cancer registries. Lancet Oncol 6(8):557–565
Darby SC, Ewertz M, McGale P, Bennet AM, Blom-Goldman U, Brønnum D, Correa C, Cutter D, Gagliardi G, Gigante B (2013) Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med 368(11):987–998
Dell’Oro M, Giles E, Sharkey A, Borg M, Connell C, Bezak E (2019) A retrospective dosimetric study of radiotherapy patients with left-sided breast cancer; patient selection criteria for deep inspiration breath hold technique. Cancers 11(2):259
Erven K, Weltens C, Van Limbergen E, Van den Bogaert W (2008) Modern radiotherapy techniques for breast cancer. Belgian J Med Oncol 2(6):308–314
Feng M, Moran JM, Koelling T, Chughtai A, Chan JL, Freedman L, Hayman JA, Jagsi R, Jolly S, Larouere J (2011) Development and validation of a heart atlas to study cardiac exposure to radiation following treatment for breast cancer. Int J Radiat Oncol Biol Phys 79(1):10–18
Fletcher GH (1988) Regaud lecture perspectives on the history of radiotherapy. Radiother Oncol 12(4):253–271
Fong A, Bromley R, Beat M, Vien D, Dineley J, Morgan G (2009) Dosimetric comparison of intensity modulated radiotherapy techniques and standard wedged tangents for whole breast radiotherapy. J Med Imaging Radiat Oncol 53(1):92–99
Formenti SC, DeWyngaert JK, Jozsef G, Goldberg JD (2012a) Prone vs supine positioning for breast cancer radiotherapy. JAMA 308(9):861–863
Formenti SC, Hsu H, Fenton-Kerimian M, Roses D, Guth A, Jozsef G, Goldberg JD, DeWyngaert JK (2012b) Prone accelerated partial breast irradiation after breast-conserving surgery: five-year results of 100 patients. Int J Radiat Oncol Biol Phys 84(3):606–611
Freedman GM, Anderson PR, Li J, Eisenberg DF, Hanlon AL, Wang L, Nicolaou N (2006) Intensity modulated radiation therapy (IMRT) decreases acute skin toxicity for women receiving radiation for breast cancer. Am J Clin Oncol 29(1):66–70
Friberg S, Ruden B-I (2009) Hypofractionation in radiotherapy. An investigation of injured Swedish women, treated for cancer of the breast. Acta Oncol 48(6):822–831
Giordano SH, Kuo Y-F, Freeman JL, Buchholz TA, Hortobagyi GN, Goodwin JS (2005) Risk of cardiac death after adjuvant radiotherapy for breast cancer. J Natl Cancer Inst 97(6):419–424
Gocht H (1897) Therapeutische Verwendung der Röntgenstrahlen. Fortschr Gebiete Röntgenstr 1:14–22
Goldberg M, Whelan TJ (2020) Accelerated Partial Breast Irradiation (APBI): where are we now? Curr Breast Cancer Rep 12:1–10
Griem KL, Fetherston P, Kuznetsova M, Foster GS, Shott S, Chu J (2003) Three-dimensional photon dosimetry: a comparison of treatment of the intact breast in the supine and prone position. Int J Radiat Oncol Biol Phys 57(3):891–899
Group EBCTC (2000) Favourable and unfavourable effects on long-term survival of radiotherapy for early breast cancer: an overview of the randomised trials. Lancet 355(9217):1757–1770
Haffty BG (2018) Supine or prone breast radiation: upsides and downsides. Int J Radiat Oncol Biol Phys 101(3):510–512
Haffty BG, Buchholz TA (2013) Hypofractionated breast radiation: preferred standard of care? Lancet Oncol 14(11):1032–1034
Hall EJ, Wuu C-S (2003) Radiation-induced second cancers: the impact of 3D-CRT and IMRT. Int J Radiat Oncol Biol Phys 56(1):83–88
Harris EE, Correa C, Hwang W-T, Liao J, Litt HI, Ferrari VA, Solin LJ (2006) Late cardiac mortality and morbidity in early-stage breast cancer patients after breast-conservation treatment. J Clin Oncol 24(25):4100–4106
Hooning MJ, Botma A, Aleman BM, Baaijens MH, Bartelink H, Klijn JG, Taylor CW, Van Leeuwen FE (2007) Long-term risk of cardiovascular disease in 10-year survivors of breast cancer. J Natl Cancer Inst 99(5):365–375
Huo J, Giordano SH, Smith BD, Shaitelman SF, Smith GL (2016) Contemporary toxicity profile of breast brachytherapy versus external beam radiation after lumpectomy for breast cancer. Int J Radiat Oncol Biol Phys 94(4):709–718
Huppert N, Jozsef G, DeWyngaert K, Formenti SC (2011) The role of a prone setup in breast radiation therapy. Front Oncol 1:31
Jacobse JN, Duane FK, Boekel NB, Schaapveld M, Hauptmann M, Hooning MJ, Seynaeve CM, Baaijens MH, Gietema JA, Darby SC (2019) Radiation dose-response for risk of myocardial infarction in breast cancer survivors. Int J Radiat Oncol Biol Phys 103(3):595–604
Jagsi R (2014) Progress and controversies: radiation therapy for invasive breast cancer. CA Cancer J Clin 64(2):135–152
Kahán Z, Rárosi F, Gaál S, Cserháti A, Boda K, Darázs B, Kószó R, Lakosi F, Gulybán Á, Coucke PA (2018) A simple clinical method for predicting the benefit of prone vs. supine positioning in reducing heart exposure during left breast radiotherapy. Radiother Oncol 126(3):487–492
Kirby AM, Evans PM, Donovan EM, Convery HM, Haviland JS, Yarnold JR (2010) Prone versus supine positioning for whole and partial-breast radiotherapy: a comparison of non-target tissue dosimetry. Radiother Oncol 96(2):178–184
Kirby AM, Evans PM, Helyer SJ, Donovan EM, Convery HM, Yarnold JR (2011) A randomised trial of supine versus prone breast radiotherapy (SuPr study): comparing set-up errors and respiratory motion. Radiother Oncol 100(2):221–226
Korzets Y, Fyles A, Shepshelovich D, Amir E, Goldvaser H (2019) Toxicity and clinical outcomes of partial breast irradiation compared to whole breast irradiation for early-stage breast cancer: a systematic review and meta-analysis. Breast Cancer Res Treat 175(3):531–545
Lai J, Hu S, Luo Y, Zheng R, Zhu Q, Chen P, Chi B, Zhang Y, Zhong F, Long X (2020) Meta-analysis of deep inspiration breath hold (DIBH) versus free breathing (FB) in postoperative radiotherapy for left-side breast cancer. Breast Cancer 27(2):299–307
Latty D, Stuart KE, Wang W, Ahern V (2015) Review of deep inspiration breath-hold techniques for the treatment of breast cancer. J Med Radiat Sci 62(1):74–81
Little M, Weiss H, Boice J Jr, Darby S, Day N, Muirhead C (1999) Risks of leukemia in Japanese atomic bomb survivors, in women treated for cervical cancer, and in patients treated for ankylosing spondylitis. Radiat Res 152(3):280–292
Liu H, Chen X, He Z, Li J (2016) Evaluation of 3D-CRT, IMRT and VMAT radiotherapy plans for left breast cancer based on clinical dosimetric study. Comput Med Imaging Graph 54:1–5
Liu G, Dong Z, Huang B, Liu Y, Tang Y, Li Q, Zhu Y (2017) Efficacy and safety of accelerated partial breast irradiation: a meta-analysis of published randomized studies. Oncotarget 8(35):59581
Lu H-M, Cash E, Chen MH, Chin L, Manning WJ, Harris J, Bornstein B (2000) Reduction of cardiac volume in left-breast treatment fields by respiratory maneuvers: a CT study. Int J Radiat Oncol Biol Phys 47(4):895–904
MacDonald SM, Patel SA, Hickey S, Specht M, Isakoff SJ, Gadd M, Smith BL, Yeap BY, Adams J, DeLaney TF (2013) Proton therapy for breast cancer after mastectomy: early outcomes of a prospective clinical trial. Int J Radiat Oncol Biol Phys 86(3):484–490
Marks LB, Yu X, Prosnitz RG, Zhou S-M, Hardenbergh PH, Blazing M, Hollis D, Lind P, Tisch A, Wong TZ (2005) The incidence and functional consequences of RT-associated cardiac perfusion defects. Int J Radiat Oncol Biol Phys 63(1):214–223
Mast ME, Vredeveld EJ, Credoe HM, van Egmond J, Heijenbrok MW, Hug EB, Kalk P, van Kempen-Harteveld LM, Korevaar EW, van der Laan HP, Langendijk JA, Rozema HJ, Petoukhova AL, Schippers JM, Struikmans H, Maduro JH (2014) Whole breast proton irradiation for maximal reduction of heart dose in breast cancer patients. Breast Cancer Res Treat 148(1):33–39. https://doi.org/10.1007/s10549-014-3149-6
Mattsson A, Rudén B-I, Hall P, Wilking N, Rutqvist LE (1993) Radiation-induced breast cancer: long-term follow-up of radiation therapy for benign breast disease. J Natl Cancer Inst 85(20):1679–1685
McCarthy EP, Ngo LH, Roetzheim RG, Chirikos TN, Li D, Drews RE, Iezzoni LI (2006) Disparities in breast cancer treatment and survival for women with disabilities. Ann Intern Med 145(9):637–645
Miranda FA, Teixeira LA, Heinzen RN, de Andrade FEM, Hijal T, Buchholz TA, Moraes FY, Poortmans P, Marta GN (2019) Accelerated partial breast irradiation: current status with a focus on clinical practice. Breast J 25(1):124–128
Mohan R, Mahajan A, Minsky BD (2013) New strategies in radiation therapy: exploiting the full potential of protons. Clin Cancer Res 19(23):6338–6343
Moignier A, Broggio D, Derreumaux S, Beaudré A, Girinsky T, Paul J-F, Drubay D, Lefkopoulos D, Franck D, Aubert B (2015) Coronary stenosis risk analysis following Hodgkin lymphoma radiotherapy: a study based on patient specific artery segments dose calculation. Radiother Oncol 117(3):467–472
Mouw KW, Harris JR (2012) Irradiation in early-stage breast cancer: conventional whole-breast, accelerated partial-breast, and accelerated whole-breast strategies compared. Oncology 26(9):820
Nilsson G, Holmberg L, Garmo H, Duvernoy O, Sjögren I, Lagerqvist B, Blomqvist C (2012) Distribution of coronary artery stenosis after radiation for breast cancer. J Clin Oncol 30(4):380–386
Pignol J-P, Olivotto I, Rakovitch E, Gardner S, Sixel K, Beckham W, Vu TTT, Truong P, Ackerman I, Paszat L (2008) A multicenter randomized trial of breast intensity-modulated radiation therapy to reduce acute radiation dermatitis. J Clin Oncol 26(13):2085–2092
Piroth MD, Petz D, Pinkawa M, Holy R, Eble MJ (2016) Usefulness of a thermoplastic breast bra for breast cancer radiotherapy. Strahlenther Onkol 192(9):609–616
Preston DL, Mattsson A, Holmberg E, Shore R, Hildreth NG, Boice JD Jr (2002) Radiation effects on breast cancer risk: a pooled analysis of eight cohorts. Radiat Res 158(2):220–235
Rahusen FD, Bremers AJ, Fabry HF, Van Amerongen AT, Boom RP, Meijer S (2002) Ultrasound-guided lumpectomy of nonpalpable breast cancer versus wire-guided resection: a randomized clinical trial. Ann Surg Oncol 9(10):994–998
Raj KA, Marks LB, Prosnitz RG (2006) Late effects of breast radiotherapy in young women. Breast Dis 23(1):53–65
Ribeiro G, Dunn G, Swindell R, Harris M, Banerjee SS (1990) Conservation of the breast using two different radiotherapy techniques: interim report of a clinical trial. Clin Oncol 2(1):27–34
Sanders ME, Scroggins T, Ampil FL, Li BD (2007) Accelerated partial breast irradiation in early-stage breast cancer. J Clin Oncol 25(8):996–1002
Schnur JB, Ouellette SC, DiLorenzo TA, Green S, Montgomery GH (2011) A qualitative analysis of acute skin toxicity among breast cancer radiotherapy patients. Psycho-Oncology 20(3):260–268
Shah C, Vicini F, Wazer DE, Arthur D, Patel RR (2013) The American Brachytherapy Society consensus statement for accelerated partial breast irradiation. Brachytherapy 12(4):267–277
Shah C, Jia X, Hobbs BP, Tendulkar RD, Sittenfeld SMC, Al-Hilli Z, Arthur DW, Keisch ME, Khan AJ, Shaitelman SF, Boyages J, Wazer D, Kundu N, Vicini FA (2021) Outcomes with partial breast irradiation vs. whole breast irradiation: a meta-analysis. Ann Surg Oncol 28(9):4985–4994. https://doi.org/10.1245/s10434-020-09447-w
Shaitelman SF, Khan AJ, Woodward WA, Arthur DW, Cuttino LW, Bloom ES, Shah C, Freedman GM, Wilkinson JB, Babiera GV (2014) Shortened radiation therapy schedules for early-stage breast cancer: a review of hypofractionated whole-breast irradiation and accelerated partial breast irradiation. Breast J 20(2):131–146
Sixel KE, Aznar MC, Ung YC (2001) Deep inspiration breath hold to reduce irradiated heart volume in breast cancer patients. Int J Radiat Oncol Biol Phys 49(1):199–204
Skyttä T, Tuohinen S, Boman E, Virtanen V, Raatikainen P, Kellokumpu-Lehtinen P-L (2015) Troponin T-release associates with cardiac radiation doses during adjuvant left-sided breast cancer radiotherapy. Radiat Oncol 10(1):1–8
Smith TE, Lee D, Turner BC, Carter D, Haffty BG (2000) True recurrence vs. new primary ipsilateral breast tumor relapse: an analysis of clinical and pathologic differences and their implications in natural history, prognoses, and therapeutic management. Int J Radiat Oncol Biol Phys 48(5):1281–1289
Smith BD, Bentzen SM, Correa CR, Hahn CA, Hardenbergh PH, Ibbott GS, McCormick B, McQueen JR, Pierce LJ, Powell SN (2011) Fractionation for whole breast irradiation: an American Society for Radiation Oncology (ASTRO) evidence-based guideline. Int J Radiat Oncol Biol Phys 81(1):59–68
Stick LB, Yu J, Maraldo MV, Aznar MC, Pedersen AN, Bentzen SM, Vogelius IR (2017) Joint estimation of cardiac toxicity and recurrence risks after comprehensive nodal photon versus proton therapy for breast cancer. Int J Radiat Oncol Biol Phys 97(4):754–761
Swerdlow A, Barber J, Hudson GV, Cunningham D, Gupta R, Hancock B, Horwich A, Lister T, Linch D (2000) Risk of second malignancy after Hodgkin’s disease in a collaborative British cohort: the relation to age at treatment. J Clin Oncol 18(3):498
Taylor C, Correa C, Duane FK, Aznar MC, Anderson SJ, Bergh J, Dodwell D, Ewertz M, Gray R, Jagsi R (2017) Estimating the risks of breast cancer radiotherapy: evidence from modern radiation doses to the lungs and heart and from previous randomized trials. J Clin Oncol 35(15):1641
van den Bogaard VA, Ta BD, van der Schaaf A, Bouma AB, Middag AM, Bantema-Joppe EJ, van Dijk LV, van Dijk-Peters FB, Marteijn LA, de Bock GH (2017) Validation and modification of a prediction model for acute cardiac events in patients with breast cancer treated with radiotherapy based on three-dimensional dose distributions to cardiac substructures. J Clin Oncol 35(11):1171
Varga Z, Hideghéty K, Mező T, Nikolényi A, Thurzó L, Kahán Z (2009) Individual positioning: a comparative study of adjuvant breast radiotherapy in the prone versus supine position. Int J Radiat Oncol Biol Phys 75(1):94–100
Veronesi U, Marubini E, Mariani L, Galimberti V, Luini A, Veronesi P, Salvadori B, Zucali R (2001) Radiotherapy after breast-conserving surgery in small breast carcinoma: long-term results of a randomized trial. Ann Oncol 12(7):997–1003
Vicini FA, Sharpe M, Kestin L, Martinez A, Mitchell CK, Wallace MF, Matter R, Wong J (2002) Optimizing breast cancer treatment efficacy with intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys 54(5):1336–1344
Vicini FA, Chen P, Wallace M, Mitchell C, Hasan Y, Grills I, Kestin L, Schell S, Goldstein NS, Kunzman J (2007) Interim cosmetic results and toxicity using 3D conformal external beam radiotherapy to deliver accelerated partial breast irradiation in patients with early-stage breast cancer treated with breast-conserving therapy. Int J Radiat Oncol Biol Phys 69(4):1124–1130
Wenz F, Sedlmayer F, Herskind C, Welzel G, Sperk E, Neumaier C, Gauter-Fleckenstein B, Vaidya JS, Sütterlin M (2015) Accelerated partial breast irradiation in clinical practice. Breast Care 10(4):247–252
Whelan T, MacKenzie R, Julian J, Levine M, Shelley W, Grimard L, Lada B, Lukka H, Perera F, Fyles A (2002) Randomized trial of breast irradiation schedules after lumpectomy for women with lymph node-negative breast cancer. J Natl Cancer Inst 94(15):1143–1150
Whelan TJ, Pignol J-P, Levine MN, Julian JA, MacKenzie R, Parpia S, Shelley W, Grimard L, Bowen J, Lukka H (2010) Long-term results of hypofractionated radiation therapy for breast cancer. N Engl J Med 362(6):513–520
Wong S, Kaur A, Back M, Lee KM, Baggarley S, Lu JJ (2011) An ultrasonographic evaluation of skin thickness in breast cancer patients after postmastectomy radiation therapy. Radiat Oncol 6(1):1–10
Würschmidt F, Stoltenberg S, Kretschmer M, Petersen C (2014) Incidental dose to coronary arteries is higher in prone than in supine whole breast irradiation. Strahlenther Onkol 190(6):563–568
Yarnold J, Bentzen SM, Coles C, Haviland J (2011) Hypofractionated whole-breast radiotherapy for women with early breast cancer: myths and realities. Int J Radiat Oncol Biol Phys 79(1):1–9
Yeboa DN, Evans SB (2016) Contemporary breast radiotherapy and cardiac toxicity. Semin Radiat Oncol 1:71–78
Yim J, Suttie C, Bromley R, Morgia M, Lamoury G (2015) Intensity modulated radiotherapy and 3D conformal radiotherapy for whole breast irradiation: a comparative dosimetric study and introduction of a novel qualitative index for plan evaluation, the normal tissue index. J Med Radiat Sci 62(3):184–191
Yu T, Xu M, Sun T, Shao Q, Zhang Y, Liu X, Li F, Wang W, JBJ L Sr (2018) External-beam partial breast irradiation in a supine versus prone position after breast-conserving surgery for Chinese breast cancer patients. Sci Rep 8(1):1–8
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Atiq, A., Atiq, M., Naeem, H., Saeed, N., Abbas, M. (2022). Modern Radiation Therapy Techniques and their Toxicities for Breast Cancer. In: Shakil Malik, S., Masood, N. (eds) Breast Cancer: From Bench to Personalized Medicine. Springer, Singapore. https://doi.org/10.1007/978-981-19-0197-3_18
Download citation
DOI: https://doi.org/10.1007/978-981-19-0197-3_18
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-0196-6
Online ISBN: 978-981-19-0197-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)