Abstract
Multi-drug resistance (MDR) and extensive-drug resistance (XDR) have become common, making care of many patients difficult. The rise in resistance mediated through MDR and XDR organisms has led to serious implications which have been great challenge to manage. It is a global health emergency. There is a critical need to develop newer medications to tackle this disaster. As a result, there has been a pressing need to create new antimicrobial agents for the treatment of Gram-negative pathogens. The discovery and development of newer, potent, and safer antibiotics is not an easy task. It involves a huge economic burden. This chapter lists the antimicrobial agents, β-lactamase/β-lactam inhibitor (BL-BLI) combinations, newer carbapenems, and newer topoisomerase inhibitors. Agents which are in Phase 2 trials have also been included. Substitutes to antimicrobials agents such as bacteriophages, DCAP, peptidic benzimidazoles, odilorhabdins, quorum sensing inhibitors, metal-based antibacterial agents are being tried in resistant cases. There has been surge in newer agents but there is still a large gap in the pipeline of the development of new antimicrobials with MDR pathogens.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Antibiotics in pipeline
- Drug resistance
- Newer carbapenems
- Newer topoisomerase inhibitors
- Agents in phase 2 trials
1 Introduction
Multi-drug resistance (MDR) and extensive-drug resistance (XDR) have become common, making care of many patients difficult. The rise in resistance mediated through MDR and XDR organisms has led to serious implications which have been great challenge to manage. It is a global health emergency. There is a critical need to develop newer medications to tackle this disaster. As a result, there has been a pressing need to create new antimicrobial agents for the treatment of Gram-negative pathogens (Breijyeh et al. 2018).
2 Antibiotic Agents in Pipeline for MDR-GNB (Butler and Paterson 2020)
2.1 Omadacycline
Omadacycline belongs to aminomethylcycline subclass of tetracycline. It has been FDA approved recently for use in patients of community acquired bacterial pneumonia (CABP) and acute bacterial skin and skin structure infections (ABSSI). It acts similarly as tetracyclines by inhibiting bacterial protein synthesis. It kills tetracycline-resistant pathogens (efflux and ribosomal protection) (Gallagher 2019).
2.2 Cefiderocol
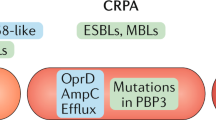
Cefiderocol is a siderophore cephalosporin that was only recently created. Its catechol end attaches to ferric iron and crosses bacterial outer membrane using iron transporters (Ito et al. 2016). Hence it acts by destroying cell wall synthesis. During an acute infection, these transporters are increased. It is effective against all carbapenemases and stable during hydrolysis by all β-lactamases, including KPC-producing Enterobacteriaceae, MBL-producing Pseudomonas aeruginosa, OXA-type beta-lactamase-producing Acinetobacter baumannii, and S. maltophilia. It is one of the most promising therapeutic solutions for pathogens such as carbapenem-resistant Enterobacterales (CRE), carbapenem-resistant Pseudomonas aeruginosa (CRPA), and carbapenem-resistant Acinetobacter baumannii (CRAB) in the future (Ghazi et al. 2018).
It was administered at 2 g IV infused over an hour every 8 hourly. It is mainly discharged in urine and hence requires dose modification as per CrCl (Saisho et al. 2018). No significant drug interaction has been reported (Katsube et al. 2018). Portsmouth et al. (2018) in a Phase II RCT demonstrated cefiderocol noninferior in contrast with IMI for managing cUTI patients. In a Phase 3 preliminary trial, the adequacy of cefiderocol for treatment of CRE diseases (counting HABP, VABP, cUTI, and blood stream infections (BSI)) was assessed. In the therapy of nosocomial pneumonia, cefiderocol + linezolid was compared to meropenem + linezolid.
2.3 Imipenem Plus Relebactam
Imipenem in addition to relebactam (MK7655) is a form of present carbapenem with a novel powerful non-β-lactam, bicyclic diazabicyclooctan with action against class A and C beta-lactamase but not against class D and MBL carbapenemases. Relebactam keeps up imipenem and cilastatin activity against KPC producers and P. aeruginosa. Presently, its combination with imipenem and cilastatin is being studied against Gram-negative microorganisms like E. coli, P. aeruginosa, K. pneumoniae, and others. It is mainly excreted in urine and Phase I trial has shown that PK of the individual agents is not affected significantly when given in combination.
In two Phase 2 trials, its efficacy and safety in patients with cIAI or cUTI have been studied. Here imipenem (500 mg 6 hourly) + relebactam at 125 mg and 250 mg 6 hourly was found similar to imipenem alone (Lucasti et al. 2016). The RESTORE-IMI1 study assessed it against colistin/imipenem in cIAI, cUTI or HAP/VAP patients for efficacy and safety (Motsch et al. 2018).
2.4 Lefamulin (BC-3781)
Lefamulin acts by hindering protein synthesis by restricting 50S ribosomal subunit. It has speedy and excellent penetration in the lungs epithelial lining. Hence, it has pivotal role in the treatment of infections in the respiratory tract. It also has potential in treating ABSSSI due to rapid distribution into skeletal and fatty tissues. It is active against all aerobic Gram-positive pathogens except E. faecalis. It is also active against Gram-negative pathogens (aside from P. aeruginosa and A. baumannii), some anaerobes, and against atypical pathogens (Jacobsson et al. 2017).
It is currently being studied in the management of ABSSSI and CABP. Phase 2 studies reported comparable cure by lefamulin 100 mg and 150 mg along with vancomycin in ABSSSI patients, whereas LEAP 1, LEAP 2, and Phase 3 studies have shown that lefamulin in treating CABP is noninferior in contrast to moxifloxacin with/without linezolid (Alexander et al. 2018).
2.5 Solithromycin
Solithromycin is a fourth-generation macrolide with 67% bioavailability that is not influenced by food. It is degraded by CYP3A4. It is primarily discharged in bile and just 10% in urine. There is no requirement of dose adjustment in hepatic impairment. No effect on QTc has been reported. It has important role in patients of respiratory tract infections because it reaches in higher concentrations in ELF and alveolar macrophages. Due to unique chemical structure, it has high intracellular accumulation. Subsequently, it is active against both extra and intracellular microbes. It has activity against Gram-positive and Gram-negative aerobes, and against Gram-positive anaerobes (Jamieson et al. 2015).
Investigations are being carried out for its role in CABP and urogenital gonorrhea patients. As per SOLITAIRE studies, solithromycin’s 5 days treatment is not inferior when compared to moxifloxacin in patients of CABP. First, 800 mg oral or IV dose of solithromycin was given on day 1 and then 400 mg oral daily dose from day 2 to 5 (File et al. 2016; Barrera et al. 2016). In SOLITAIR-J (Phase 3) trial, once 1200 mg oral solithromycin was compared to ceftriaxone + azithromycin in intramuscular dose for efficacy and safety in patients of urogenital gonorrhea.
2.6 Sulopenem
Sulopenem is a newer carbapenem available in oral and IV dosage form. It is active against Gram-positive and -negative pathogens and not against CRE, P. aeruginosa, or MRSA. It is administered intravenously1000 mg/day or orally 500 mg twice a day alongside oral probenecid 500 mg twice a day (Kosowska-Shick et al. 2009).
It is tried in patients of cIAI and CABP. In a Phase 2 study, its efficacy was compared to ceftriaxone along with amoxy-clav in patients of CABP. A Phase III Sulopenem for Resistant Enterobacteriaceae (SURE) trial is being conducted for comparing it with ertapenem in patients of cIAI. Other indications are UTIs, acute prostatitis, gonococcal urethritis, and pelvic inflammatory disease.
2.7 Murepavadin
It (POL7080) is a new class of antibiotics called outer membrane protein targeting antibiotics. It produces its effect through a new mechanism by targeting lipopolysaccharide transport protein D (LptD). LptD has role in synthesis of lipopolysaccharide in the external membrane of P. aeruginosa. Hence, it has significant role against P. aeruginosa. The volume of distribution is high and t1/2 of 2–5 h. It has linear and dose-related pharmacokinetics (Martin-Loeches et al. 2018).
2.8 Aztreonam/Avibactam
It has efficacy against MBL-producing microbes and is destroyed by KPCs, ESBL, and class C (AmpC) beta-lactamases. But the combination demonstrated ten times potency against all these strains as compared to aztreonam given singly. But activity is limited against P. aeruginosa or A. baumannii compared to aztreonam monotherapy. It may be an effective treatment for MBL-producing pathogens related infections (Butler and Paterson 2020).
2.9 Ceftobiprole Medocaril
It is a fifth-generation cephalosporin with activity against both Gram-positive and -negative microbes, including MRSA and Enterococcus spp. It kills MRSA by inhibiting penicillin binding protein-2. It has activity against Streptococcus (including those which are resistant to penicillin and macrolide), H. influenzae, and N. gonorrhoeae. It has limited activity in A. baumannii. It is a prodrug and 500 mg is administered intravenously in 2 h, at every 8 h. It is mainly discharged in urine, and therefore, dose is adjusted according to CrCl.
It is approved in many countries for ABSSSI. It has been demonstrated as noninferior to vancomycin plus ceftazidime in complicated ABSSSI (Noel et al. 2008). Several double-blind RCTs have reported its efficacy in patients of pneumonia. Awad et al. (2014) in a Phase 3 study showed it is noninferior to ceftazidime + linezolid in HABP patients. Currently, Phase 3 studies are being performed to evaluate efficacy in patients with S. aureus infections.
2.10 Delafloxacin
It is a fluoroquinolone inhibiting MRSA and Gram-positive pathogens. Its diverse structure from other quinolones confers weak acidity (So et al. 2015). Subsequently, it inhibits more infections related to S. aureus. It has more potent role in UTI. It is active against Gram-positive, Gram-negative and anaerobic microbes. It is mainly excreted in urine and has 58.8% bioavailability. It is administered intravenously 300 mg or orally 450 mg every 12 h. It does not increase CYP3A, prolong QTc, and dose adjustment for hepatic dysfunction as other fluoroquinolones (Hoover et al. 2017).
It was used in the patients of ABSSSI. Phase 3 trial has shown that it is noninferior in comparison to vancomycin plus aztreonam in the treatment of MRSA. Phase II trial reported similar efficacy vs. tigecycline and linezolid and higher efficacy vs. vancomycin alone. Phase 3 trials evaluated its efficacy in patients of CABP and urogenital gonorrhea.
2.11 Cefepime/Zidebactam (FEP–ZID)
Cefepime/zidebactam is a novel mix of a cephalosporin, cefepime and BLI, zidebactam. Zidebactam is a bicyclo-acyl hydrazide. Zidebactam has higher binding for PBP2 and inhibits enzymes of class A and C. Zidebactam not only protects cefepime from β-lactamases but also extends its spectrum of antibacterial activity (Papp-Wallace and Bonomo 2016). It inhibits CRE, P. aeruginosa, and A. baumannii. FEP–ZID inhibits all three Ambler classes of carbapenemases and P. aeruginosa. FEP–ZID inhibits many MDR Gram-negative pathogens (Sader et al. 2017).
2.12 Cefepime/Enmetazobactam
Enmetazobactam (earlier known as AAI101) is a new ESBL inhibitor. It is a penicillanic acid sulfone derivative. It has activity against many beta-lactamases, but no add-on benefits occur while treating Pseudomonas aeruginosa with cefepime. This combination provides an option against ESBL-producing pathogens which is carbapenem free (Papp-Wallace and Bonomo 2016). It is indicated in cUTIs including acute pyelonephritis, cIAIs, and HABP or VABP. As per the ALLIUM Phase 3 trial, piperacillin/tazobactam was found inferior to it in cUTIs patients. With ESBL-producing bacteria, this combination demonstrated a cure rate of 73.7% as compared to 51.6% in patients who were on piperacillin/tazobactam.
2.13 Cefepime/Taniborbactam
Taniborbactam (earlier known as VNRX-5133) is a BLI that inhibits both serine-BL and MBL. It is a newer cyclic boronate. It enhances cefepime’s potency while treating Pseudomonas aeruginosa and Enterobacteriaceae producing beta-lactamases such as KPC, OXA, CTX-M, VIM, and NDM-type beta-lactamases (Papp-Wallace and Bonomo 2016). In an in vitro study, this combination showed more potent activity as compared to ceftazidime/avibactam against various ESBL, AmpC, and MBLs producing urinary Gram-negative bacilli. A Phase 3 RCT is presently under process to evaluate cefepime/taniborbactam vs. meropenem in patients of cUTIs.
2.14 Sulbactam/Durlobactam
Durlobactam (earlier known as ETX2514) is a newer diazabicyclooctenone BLI which inhibits class A, C, and D BL. It inhibits Enterobacterales. In a study (Phase 2), it was contrasted to imipenem-cilastatin in cUTI patients, including AP and no significant difference was observed. It has shown very good activity against CRAB as compared to colistin, minocycline, amikacin, and sulbactam alone. Presently, a Phase 3 trial is comparing sulbactam/durlobactam + imipenem/cilastatin vs. colistin + imipenem/cilastatin against A. baumannii-calcoaceticus complex infection (Papp-Wallace and Bonomo 2016).
2.15 Dalbavancin (Butler and Paterson 2020)
It is a new second-generation semisynthetic lipoglycopeptide anti-microbial. It belongs to the same group as that of vancomycin which is available for patients with MRSA infection. It was developed to improve over the currently available natural glycopeptides like vancomycin and teicoplanin. It is synthesized from a complex glycopeptide, A-40926, which is derived from a new Actinomadura strain.
Similar to other glycopeptides, it exerts killing of bacteria by disrupting cell wall biosynthesis. It stops transpeptidation by binding to d-alanyl-d-alanyl residue on growing peptidoglycan chain. Thus, peptidoglycan elongation and cell wall synthesis are inhibited. It also forms dimers and anchors itself to the lipophilic membrane of microorganisms.
It inhibits Gram-positive microbes including MRSA and MRSE. It is administered once for 2 weeks. It has been approved for intravenous use in treating ABSSSIs caused by MSSA and MRSA.
It is contraindicated for those who are hypersensitive such as prone to skin reactions or anaphylaxis. Caution is to be taken for patients who are hypersensitive to other glycopeptides.
The most well-known adverse reactions reported in Phase II and III trials were nausea, diarrhea, headache, rash, itching. Others are hematologic disorders, bronchospasm, hepatotoxicity, Red Man Syndrome, C. difficile colitis, and anaphylactic shock. Ototoxicity is not reported with it. There is no evidence of teratogenicity in animals.
2.16 Oritavancin (Butler and Paterson 2020)
It is a semisynthetic glycopeptide. It has activity against serious Gram-positive bacterial infections. Its chemical structure as a lipoglycopeptide is the same as vancomycin. Its 4′-chlorobiphenylmethyl group destroys Gram-positive bacterial cell membrane. It also reduces transpeptidation and transglycosylation.
It is approved for treating ABSSSI. It has demonstrated rapid inhibition of both resistant and susceptible Gram-positive bacteria, including S. aureus, MRSA, enterococci, and streptococci. It was more active than metronidazole or vancomycin against C. difficile strains. It is useful as a therapy for exposure to B. anthracis causing anthrax.
3 Newer Carbapenems (Butler and Paterson 2020)
-
1.
Ertapenem
It is mainly indicated in cIAIs, ABSSSI, cUTIs, acute pelvic infections, and CABP. The net negative charge on it enhances its plasma protein binding (95%), and therefore, it has long half-life. So, administered once a day. P. aeruginosa, Acinetobacter spp., and B. cepacia are less inhibited by it. It has poor activity against ESBL-producing microbes as compared to other carbapenems, but it is approved for treating such infections. It was useful in treating early onset VAP due to ESBL-producing microbes, with clinical and microbiological success rate of 80% and 75%, respectively.
-
2.
Doripenem
It is a wide range carbapenem administered parenterally. Its molecular structure provides stability against β-lactamase and also resistance against renal DHP-I. Similar to imipenem or ertapenem, it inhibits Gram-positive cocci. Against Gram-negative, the activity is same as meropenem. But it is not active against MRSA, E. fecium, etc. It is very active against ESBL producers. Dose modification is needed when CrCl is <30 ml/min. The most common adverse events with it are nausea and loose stools. The chances of seizures are lower than with others.
-
3.
Biapenem
It is a parenteral carbapenem. It is presently undergoing Phase II trials. It has higher penetration into respiratory system and body fluids. It has activity against Gram-positive microbes like S. pneumoniae, MSSA, and Gram-negative such as A. baumannii, ESBL producers, S. marcescens, E. cloacae, and C. freundii. It has been reported to have moderate activity against P. aeruginosa. The T1/2 is 1 h and administered 300 mg two times a day. Dose is modified as per the CrCl. The adverse events associated with it include nausea, vomiting, diarrhea, and skin eruption.
-
4.
Panipenem/Betamipron
Panipenem is combined with betamipron because betamipron halts renal excretion of panipenem. It is indicated for LRTI, UTI, obstetric/gynecological, and surgical infections. The recommended dose is 0.5 + 0.5 g two times a day as IV infusion in 30–60 min. It has been reported in three different Phase 3 RCT as efficacious when compared to imipenem+cilastatin in respiratory infections and UTI. It is useful to treat Enterobacteriaceae and common pathogens of respiratory tract. But against H. influenzae, meropenem is the most active carbapenem. P. aeruginosa is resistant to it.
-
5.
Tomopenem
It is 1-methyl carbapenem. It acts by inhibiting PBP activity and hampers peptidoglycan biosynthesis of cell wall in bacteria. It has lesser chances of resistance development. It is beneficial against MRSA, P. aeruginosa (ceftazidime resistant), and microbes producing ESBL.
-
6.
Tebipenem
Tebipenem pivoxil (earlier known as SPR994) is an oral prodrug. It is activated in plasma and effective against ESBL-producing pathogens. TBPM-PI-HBr is its novel formulation. It has high stability level against DHP-I. Its metabolite is well absorbed into the blood from intestine. It is used to treat UTIs. Various studies reported that tebipenem has more potency than imipenem but equal to that of meropenem against E. coli, P. mirabilis, and K. pneumoniae. It is not affected by generation of ESBL- and AmpC-BL. Results of a Phase 3 trial (ADAPT-PO) is pending where it was compared with ertapenem intravenous in AP or cUTI patients.
-
7.
Other Newer Carbapenems
-
(a)
Razupenem (SMP-601) is under Phase 2 trials. It inhibits ESBL-synthesizers, but not carbapenemases. Its utility can be increased by combining it with other drugs. It has add-on effect with amikacin or ciprofloxacin against B. cepacia and S. marcescens.
-
(b)
2-(Thyazol-2-ylthio)-1β-methyl carbapenems group has members such as SM-197436, SM-232721, and SM-232724. They are very effective against MRSA but insufficient against E. faecium. These carbapenems are highly inhibitory for Gram negative microbes such as H. influenzae, B. fragilis, and M. catarrhalis. They are similarly active as imipenem against E. coli, Proteus, and K. pneumoniae. Other indications include hospital acquired bacterial infections by Gram-positive and -negative bacteria mainly MRSA and VRE.
-
(c)
CS-023 (earlier known as RO 4908463) is another new molecule which is lesser effected by DHP-I than imipenem or meropenem. It is highly inhibitory for Gram-positive and -negative microbes. Against MRSA, it seems to be better than imipenem and meropenem. It has lower protein binding.
-
(d)
ME 1036 (CP5609) is a carbapenem administered parenterally. It has an excellent activity against CABP pathogens.
-
(e)
Trinems (earlier known as tribactams): To its carbon 1 and 2, a cyclohexane ring is attached. Sanfetrinem, as a hexatil ester, is administered orally. Sanfetrinem inhibits potent class A β-lactamase producers such as P. vulgaris and K. oxytoca.
-
(a)
3.1 Meropenem/Nacubactam
Nacubactam is a new intravenous BLI which acts by inhibiting serine β-lactamases (class A and C and few class D) and PBP2 in Enterobacteriaceae. In placebo-controlled studies, its pharmacokinetics, tolerability, and safety were evaluated in healthy individuals. They were administered once, increasing dose from 50 to 8000 mg, multiple increasing doses from 1000 to 4000 mg every 8 hourly for 7 days, or nacubactam + meropenem 2 g each every 8 hourly for 6 days. Nacubactam exhibited tolerance, with mild to moderate side effect of IV administration and headache. There were no dose-related clinical changes in safety test, or any serious or dose-limiting adverse event reported. Its pharmacokinetics was linear even after once or multiple doses. It was excreted mainly unchanged through kidney. The combination did not alter the pharmacokinetics of the individual drugs significantly. The study results are encouraging, and further clinical development is needed (Mushtaq et al. 2018).
CRE infections (KPC 2 and 3 carbapenemases) are very difficult to treat with present agents. Nacubactam is a bridged diazabicyclooctane BLI (mainly class A and C BL). It has also intrinsic antibiotic and BL “enhancer” activity against Enterobacteriaceae. The combination inhibits carbapenem-resistant K. pneumoniae. Studies also suggest that it has an alternative pathway of action as compared to avibactam (Papp-Wallace and Bonomo 2016).
4 Newer Topoisomerase Inhibitors
-
1.
Gepotidacin (Earlier Known As GSK2140944)
It is a new type-II topoisomerase inhibitor. It interacts with DNA gyrase (GyrA subunit) and topoisomerase IV (ParC subunit) and thereby inhibits DNA replication of bacteria. In a Phase 3 trial involving patients of cUTIs, it is being compared with nitrofurantoin. But it has lesser activity against Gram-negative microbes. It does not inhibit C. trachomatis. Three N. gonorrhoeae isolates are reported to have resistance against it (Taneja and Kaur 2016).
-
2.
Zoliflodacin
It acts by inhibiting type-II topoisomerase (GyrB sububit). The efficacy of this mechanism has been established against ceftriaxone- and ciprofloxacin-resistant N. gonorrhoeae and fluoroquinolone-resistant and VRSA isolates. It also inhibits C. trachomatis, C. pneumoniae, M. genitalium, and M. ureaplasma. A Phase 2 study demonstrated that oral zoliflodacin was more efficient than ceftriaxone alone in uncomplicated urogenital and rectal gonococcal infections but not pharyngeal infections. A Phase 3 trial is comparing it against ceftriaxone + azithromycin in uncomplicated gonorrhea patients (Kocsis et al. 2016).
-
3.
Finafloxacin
It is a fluoroquinolone and inhibits bacterial type-2 topoisomerase. It is useful in acute otitis externa caused by S. aureus and P. aeruginosa. It is very active under acidic environment, where bacteria like H. pylori live. It inhibits both Gram-positive and -negative microbes. It has post-antibiotic effect.
The oral bioavailability is good with T1/2 around 10 h. It is available as 0.3% otic suspension. To prevent dizziness, it is gently warmed in hands for 1–2 min before administering.
On topical application, ear itching and nausea have been reported. On oral or intravenous application, patients have reported GI side effects such as nausea, diarrhea, flatulence. Other ADRs noted are fatigue, musculoskeletal ailments, headaches, and injection site reactions. Rhinitis and nasopharyngitis are also noted (Kocsis et al. 2016).
5 Agents in Phase 2 Trials (Taneja and Kaur 2016; Vissichelli and Stevens 2019)
-
1.
BOS228 (earlier known as LYS228) is monobactam administered intravenously. It inhibits both serine and MBL producing microbes. Its Phase 2 trial was done for Gram negative cUTI and cIAI.
-
2.
Benapenem resembles ertapenem structurally and has longer T1/2. In Phase 2 trial, it was used intravenously in the treatment of cUTI including pyelonephritis. As per the Phase I trials data supports once a day intravenous administration.
-
3.
Nafithromycin (earlier known as WCK 4873) is an oral ketolide. A Phase 2 trial was done on CABP patients. It inhibits both Gram-positive (S. aureus and S. pneumoniae) and Gram-negative (H. influenzae, M. pneumoniae, M. catarrhalis, L. pneumophila, and Chlamydophila pneumoniae) bacteria.
-
4.
MGB-BP-3 act by binding to bacterial DNA. In a Phase 2 trial it was administered to patients of C. difficile-associated diarrhea (CDAD). Its structure resembles the distamycin, thiazotropsin, and netropsin (lexitropsins: actinomycetes-derived minor groove binders).
-
5.
XF-73 (exeporfinium chloride) is a porphyrin derivative and active against Gram-positive. It is a topically applied. In a Phase 2 trial, its effect was studied in patients at risk of post-operative nasal infections by S. aureus. The findings of the trial were found positive.
-
6.
TNP-2092 (CBR 2092) is an amalgam of rifamycin-quinolizinone. In a Phase II trial, it was administered intravenously against Gram-positive ABSSSI infections. In another study, it was studied against infections due to catheter and prosthetic joint. It has high potency against Gram-positive bacteria. This is due to components: rifamycin which is an RNA polymerase inhibitor and quinolone which is a DNA gyrase and topoisomerase IV inhibitor.
-
7.
Auranofin is a gold complex earlier used in treatment of rheumatoid arthritis. It inhibits thioredoxin reductase. It has gained interest for activity against C. difficile, H. pylori, MRSA, S. pneumoniae, and E. faecalis.
-
8.
MBN-101 (bismuth ethanedithiol, BisEDT) is under Phase 2 trial for orthopedic infection patients. In a Phase 1b/2a trial, it is being used topically in infected diabetic foot. It was used to treat stomach aches and travelers’ diarrhea. It is also used in combinations for treating H. pylori infections.
-
9.
Afabicin (AFN 1720, Debio 1450) is a prodrug. In a Phase 2 trial, it was used against S. aureus bone or joint infection. Its Phase 2 trial for ABSSSI has completed. It mainly inhibits FabI, an enzyme essential for final step of fatty acid chain synthesis in S. aureus.
-
10.
OPS-2071 is a quinolone-like agent. In a Phase 2 trial, it was used against enteric infections and C. difficile. During another Phase 2 trial, it was evaluated as an adjuvant agent in Crohn’s disease.
-
11.
Delpazolid (earlier known as RMX2001, LCB01-0371) is an oxazolidinone which inhibits Gram-positive microbes and TB. In a Phase 2 trial, it is being evaluated orally in the patients of TB.
-
12.
Sutezolid (earlier known as PNU-100480, PF-2341272) is an oxazolidinone which was developed along linezolid. In a Phase 2 trial, it was administered orally to treat TB patients. Recently, a Phase 2 trial has started to evaluate it in combination with moxifloxacin, bedaquiline, and delamanid.
-
13.
DNV-3837 (earlier known as MCB-3837) is a prodrug and hybrid of oxazolidinone-quinolone. In a Phase 2 trial, it was administered IV to treat CDI. It inhibits Gram-positive microbes such as MRSA, B. anthracis, C. difficile, and Francisella tularensis.
-
14.
Telacebec (earlier known as Q203) is an imidazo [1,2-a] pyridine amide. It is administered orally. In a Phase 2 trial, it was studied in TB patients.
-
15.
Macozinone (PBTZ169) is a benzothiazinone derivative. In a Phase 2 trial, it was studied in the treatment of TB.
-
16.
OPC-167832 is an oral, 3,4-dihyrdo-carbostyril derivative. It has important role in treating pulmonary TB. It inhibits cell wall synthesis.
-
17.
GSK656 (earlier known as GSK3036656) is a boron containing leucyl t-RNA synthetase inhibitor. In a Phase 2 trial, it was evaluated in pulmonary TB patients orally.
6 Substitutes to Antimicrobials Agents (Taneja and Kaur 2016; Vissichelli and Stevens 2019)
-
1.
Bacteriophages
They are bactericidal agents. These viruses infect mainly bacteria. With increasing antimicrobial resistance, there is gain in interest. They inhibit many bacterial functions and are very particular. They do not affect eukaryotes. They can enter and inhibit biofilms.
A clinical trial studied Biophage-PA (a bacteriophage) against MDR P. aeruginosa in chronic otitis. The P. aeruginosa number was significantly reduced with its use. No adverse events were reported.
Two phage mixture (T4-like coliphage or commercial Russian coliphage) in ORS was assessed against E. coli in children with acute diarrhea in another study. There were no adverse effects reported. But the phage mixture was not found to have significant effect over the control group in controlling diarrhea.
In a Phase 1/2 double-blind RCT, PhagoBurn (mixture of 12 anti-P. aeruginosa bacteriophages) efficacy and tolerability for treating P. aeruginosa-infected burn wounds were studied. It was applied directly into the wounds.
Various studies have reported synergism between antibiotics and bacteriophages. But the genesis of bacterial resistance to phages is unavoidable.
-
2.
DCAP
The compound 2-((3-(3,6-dichloro-9H-carbazol-9-yl)-2-hydroxypropyl)-amino)-2-(hydroxy-methyl) propane1,3-diol is an antimicrobial drug. It inhibits Gram-positive and -negative bacteria like E. coli and P. aeruginosa. DCAP has two ways leading to cell destruction. First, it improves ion movement across membrane and so decreases membrane potential. Second, it hampers cell membrane permeability. It is active against Gram-negative bacteria due to effect on inner membrane.
It is active in dormant phase and biofilms. They do not affect RBC and destroy mammalian cell only at high concentrations and after 6 h. Synthesis of two analogues of DCAP have been reported. They were active against B. anthrax and F. tularensis. It showed synergistic effects when given together with ampicillin or kanamycin (targeting cell wall by different mechanism).
-
3.
Odilorhabdins (ODLs)
Ribosomes are an important target for antimicrobials. But with increasing drug resistance, the efficacy of antibiotics acting on ribosome is reduced. Gram-positive Actinomycetes and Gram-negative Xenrhabdus produce a variety of metabolites with the help of genes which encode non-ribosomal peptide synthetases (NRPSs) and polyketide synthases (PKSs). ODLs are modified peptide agents produced by NRPSs gene of Xenorhabdus nematophila. They are active against Gram-positive and -negative pathogens, including CRE. They bind to bacterial small subunit of ribosomes and inhibit them. They bind to rRNA or tRNA and introduce miscoding during translation process.
-
4.
Peptidic benzimidazoles
The benzimidazole-containing agents have antibacterial, antiviral, antifungal, anthelmintic, anticancer, and anti-inflammatory activities against various diseases. Benzimidazole-containing agents inhibit peptide deformylase (PDF). PDF inhibits ribosomal synthesis of protein in bacteria, protozoans, and some fungi. Many such agents have shown in vitro activities and hence can be potent newer agents for resistant Gram negative bacteria.
The anti-microbial activity of these agents was demonstrated against Gram positive microbes (S. aureus and E. faecium) and Gram negative microbes (E. coli and P. aeruginosa), C. albicans and C. tropicalis. There was low to moderate antimicrobial activities. The antioxidant activities were also present.
-
5.
Quorum Sensing (QS) Inhibitors
Bacterial chemical communication or quorum sensing refers to organized bacterial gene activity to coordinate in process like production of virulence factor, antibiotics damage and biofilm formation. Auto-inducers (AIs) are the molecules which perform intra- and inter-species coordination. The most common QS mediators in Gram positive are oligopeptides while in Gram negative are N-acyl homoserine lactones (AHLs). (S)-4,5-Dihydroxy-2,3-pentanedione ((S)-DPD), is a QS modifier present in both Gram positive and negative bacteria. To activate QS, LsrK is phosphorylated to phosphoryl DPD. So, DPD derivatives act as antimicrobial agents by inhibiting LsrK. Isobutyl-DPD and phenyl-DPD inhibit QS when combined with gentamicin and small molecules. Modifying or inhibiting QS has evolved as an important treatment tool that can stop several bacterial virulence factors like biofilm formation and reduce the bad effect of bacterial infections. QS inhibitors can be combined with other antimicrobials to combat drug resistance.
-
6.
Metal-Based Antibacterial Agents (Taneja and Kaur 2016; Vissichelli and Stevens 2019)
Metal-based antimicrobials have been of great importance. They have unique modes of action. There are many ongoing research focusing on metal-based drugs. Ruthenium, bismuth, gallium, silver, and copper are the metals used commonly in metal-based antibacterial agents.
-
(a)
Ruthenium (Ru): They are active due to their ability to bind different places in cell like nucleic acids and proteins. Ru complexes exhibits photo-physical properties which can be utilized for knowing cellular accumulation and localization. They too have the pivotal role as antimicrobial agents. They inhibit Gram-negative microbes and some MDR strains due to their damaging effect on microbial cell wall. Studies have tried for the activity of two Ru complexes on Gram-positive (S. aureus and MRSA) and -negative (E. coli and K. pneumoniae) microbes. The inhibition was reported better than chloramphenicol and ciprofloxacin in these resistant microbes. Hence, they may be considered in antibiotic drug development.
-
(b)
Gallium (Ga): Their compounds inhibit microbial iron uptake or iron metabolism by inhibiting iron-dependent enzymes. As they are similar to iron, they incorporate into iron-dependent enzymes. They inhibit Gram-negative such as K. pneumoniae, P. aeruginosa, and A. baumannii and various Gram-positive strains. Ga(NO3)3 is currently being tested intravenously in a Phase 2 study against P. aeruginosa infection in cystic fibrosis patients. Ga-binding proteins in P. aeruginosa are the RpoB and RpoC, two subunits of RNA polymerase. They demonstrated that gallium halts transcription.
-
(c)
Bismuth (Bi): Bismuth subsalicylate, colloidal bismuth subcitrate, and ranitidine bismuth citrate are used in treating H. pylori infections. Bi agents inhibit broad spectrum MBL. Bi showed potent broad-spectrum activity against E. coli, E. faecalis, and M. smegmatis. Bi phosphinates inhibits E. coli, and some Gram-positive such as MRSA and VRE.
-
(d)
Silver (Ag): Silver, colloidal silver, and silver nitrate are used as wound antiseptics. Silver sulfadiazine is used for burn wounds. Silver nanoparticles inhibits multidrug-resistant P. aeruginosa, E. coli, and P. mirabilis strains. N-Heterocyclic carbene–silver (Ag(I)-NHC) complexes are a new class that inhibits antibiotic resistant bacteria.
-
(e)
Copper (Cu): Copper (bis-thiosemicarbazone) (Cu(btsc)) inhibits Gram-positive and -negative microbes such as N. gonorrhoeae, M. tuberculosis, and E. coli. Some studies have synthesized copper complexes with ofloxacin and norfloxacin. These complexes have better binding abilities to DNA.
-
(a)
References
Alexander E, Goldberg L, Das A, Moran GJ, Sandrock C, Gasink LB et al (2018) Oral lefamulin is safe and effective in the treatment of adults with community- acquired bacterial pneumonia (CABP): results of Lefamulin evaluation against pneumonia (LEAP 2) study. Open Forum Infect Dis 5:S761
Awad SS, Rodriguez AH, Chuang Y-C, Marjanek Z, Pareigis AJ, Reis G et al (2014) A phase 3 randomized double-blind comparison of ceftobiprole medocaril versus ceftazidime plus linezolid for the treatment of hospital-acquired pneumonia. Clin Infect Dis 59:51–61
Barrera CM, Mykietiuk A, Metev H, Nitu MF, Karimjee N, Doreski PA et al (2016) Efficacy and safety of Oral solithromycin versus oral moxifloxacin for treatment of community-acquired bacterial pneumonia: a global, double-blind, multicentre, randomised, active-con- trolled, non-inferiority trial (SOLITAIRE-ORAL). Lancet Infect Dis 16:421–430
Breijyeh Z, Jubeh B, Karaman R (2018) Resistance of gram-negative bacteria to current antibacterial agents and approaches to resolve it. Molecules 25:1340. https://doi.org/10.3390/molecules25061340
Butler MS, Paterson DL (2020) Antibiotics in the clinical pipeline in October 2019. J Antibiot 73:329–364
File TM, Rewerska B, Vucinić-Mihailović V, Gonong JRV, Das AF, Keedy K et al (2016) SOLITAIRE-IV: a randomized, double-blind, multicenter study comparing the efficacy and safety of intravenous-to-oral solithromycin to intravenous-to-oral moxifloxacin for treatment of community-acquired bacterial pneumonia. Clin Infect Dis 63:1007–1016
Gallagher JC (2019) Omadacycline: a modernized tetracycline. Clin Infect Dis 69(S1):S1–S5
Ghazi IM, Monogue ML, Tsuji M, Nicolau DP (2018) Humanized exposures of cefiderocol, a siderophore cephalosporin, display sustained in vivo activity against siderophore-resistant Pseudomonas aeruginosa. Pharmacology 101:278–284
Hoover R, Marbury TC, Preston RA, Quintas M, Lawrence LE, Paulson SK et al (2017) Clinical pharmacology of delafloxacin in patients with hepatic impairment. J Clin Pharmacol 57:328–335
Ito A, Nishikawa T, Matsumoto S, Yoshizawa H, Sato T, Nakamura R et al (2016) Siderophore cephalosporin cefiderocol utilizes ferric iron transporter systems for antibacterial activity against Pseudomonas aeruginosa. Antimicrob Agents Chemother 60:7396–7401
Jacobsson S, Paukner S, Golparian D, Jensen JS, Unemo M (2017) In vitro activity of the novel pleuromutilin lefamulin (BC-3781) and effect of efflux pump inactivation on multidrug-resistant and extensively drug-resistant Neisseria gonorrhoeae. Antimicrob Agents Chemother 61:e01497–e01417
Jamieson BD, Ciric S, Fernandes P (2015) Safety and pharmacokinetics of solithromycin in subjects with hepatic impairment. Antimicrob Agents Chemother 59:4379–4386
Katsube T, Miyazaki S, Narukawa Y, Hernandez-Illas M, Wajima T (2018) Drug-drug interaction of cefiderocol, a siderophore cephalosporin, via human drug transporters. Eur J Clin Pharmacol 74:931–938
Kocsis B, Domokos J, Szabo D (2016) Chemical structure and pharmacokinetics of novel quinolone agents represented by avarofloxacin, delafloxacin, finafloxacin, zabofloxacin and nemonoxacin. Ann Clin Microbiol Antimicrob 15:34
Kosowska-Shick K, Ednie LM, McGhee P, Appelbaum PC (2009) Comparative antipneumococcal activities of sulopenem and other drugs. Antimicrob Agents Chemother 53:2239–2247
Lucasti C, Vasile L, Sandesc D, Venskutonis D, McLeroth P, Lala M et al (2016) Phase 2, dose-ranging study of relebactam with imipenem-cilastatin in subjects with complicated intra-abdominal infection. Antimicrob Agents Chemother 60:6234–6243
Martin-Loeches I, Dale GE, Torres A (2018) Murepavadin: a new antibiotic class in the pipeline. Expert Rev Anti-Infect Ther 16:259–268
Motsch J, de Oliveira C, Stus V, Koksal I, Lyulko O, Boucher H et al (2018) RESTORE-IMI 1: a multicenter, randomized, double-blind, comparator-controlled trial comparing the efficacy and safety of imipenem/relebactam versus colistin plus imipenem in patients with imipenem-non-susceptible bacterial infections. In: Presented in 28th European congress of clinical microbiology and infectious diseases (ECCMID), Madrid
Mushtaq S, Vickers A, Woodford N, Haldimann A, Livermore DM (2018) Activity of nacubactam (RG6080/OP0595) combinations against MBL-producing Enterobacteriaceae. J Antimicrob Chemother 74:953–960
Noel GJ, Bush K, Bagchi P, Ianus J, Strauss RS (2008) A randomized, double-blind trial comparing ceftobiprole medocaril with vancomycin plus ceftazidime for the treatment of patients with complicated skin and skin-structure infections. Clin Infect Di 46:647–655
Papp-Wallace KM, Bonomo RA (2016) New β-lactamase inhibitors in the clinic. Infect Dis Clin N Am 30(2):441–464. https://doi.org/10.1016/j.idc.2016.02.007
Portsmouth S, van Veenhuyzen D, Echols R, Machida M, Ferreira JCA, Ariyasu M et al (2018) Cefiderocol versus imipenem-cilastatin for the treatment of complicated urinary tract infections caused by Gram-negative uropathogens: a phase 2, randomised, double-blind, non-inferiority trial. Lancet Infect Dis 18:1319–1328
Sader HS, Rhomberg PR, Flamm RK, Jones RN, Castanheira M (2017) WCK 5222 (cefepime/zidebactam) antimicrobial activity tested against Gram-negative organisms producing clinically relevant beta-lactamases. J Antimicrob Chemother 72:1696–1703
Saisho Y, Katsube T, White S, Fukase H, Shimada J (2018) Pharmacokinetics, safety, and tolerability of cefiderocol, a novel siderophore cephalosporin for gram-negative bacteria, in healthy subjects. Antimicrob Agents Chemother 62:e02163–e02117
So W, Crandon JL, Nicolau DP (2015) Effects of urine matrix and pH on the potency of delafloxacin and ciprofloxacin against urogenic Escherichia coli and Klebsiella pneumoniae. J Urol 194:563–570
Taneja N, Kaur H (2016) Insights into newer antimicrobial agents against gram-negative bacteria. Microbiol insights 9:9
Vissichelli NC, Stevens MP (2019) Antibiotics in the pipeline for treatment of infections due to Gram-negative organisms. Curr Treat Options Infect Dis 11:115–144
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Khan, I.A. (2022). Newer Antibiotic Agents in Pipeline. In: Shahid, M., Singh, A., Sami, H. (eds) Beta-Lactam Resistance in Gram-Negative Bacteria. Springer, Singapore. https://doi.org/10.1007/978-981-16-9097-6_18
Download citation
DOI: https://doi.org/10.1007/978-981-16-9097-6_18
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-9096-9
Online ISBN: 978-981-16-9097-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)