Abstract
Tuberculosis (TB) continues to exert a significant impact on the healthcare burden all over the world, including India. The spectrum of tuberculosis is diverse, and treatment regimens, as well as duration, vary with the site of involvement. With the availability of efficacious anti-TB drugs, prompt treatment can help to cure the patient and significantly reduces the morbidity and mortality associated with the disease. However, the first-line anti-TB drugs can have potential adverse effects, mainly gastrointestinal and hepatotoxicity, which can lead to drug discontinuation, thus bearing an influence on the prognosis of the patient. Rifampicin (RMP), isoniazid (INH), and pyrazinamide (PZA) have the potential to cause drug-induced liver injury (DILI), especially in patients with underlying risk factors. Anti-tuberculous therapy (ATT)-related DILI has been reported to cause significantly worse outcomes when compared to DILI related to other drugs. Thus, it is vital for healthcare professionals to carefully assess the risk–benefit ratio while starting these drugs in patients, especially in whom empiric therapy is being contemplated. Specific guidelines have been laid to diagnose and manage ATT-related DILI. This chapter aims to summarize the mechanism of ATT-related DILI, its clinical features, and diagnosis and provides a guide to its clinical management.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Key Points-
1.
ATT constitutes one of the most prevalent drugs which lead to drug-induced liver injury.
-
2.
Among the first-line antitubercular therapy drugs, pyrazinamide is believed to be most hepatotoxic, followed by isoniazid and rifampicin.
-
3.
There are several risk factors like age, gender, nutritional status, concomitant chronic viral hepatitis, and presence of underlying chronic liver disease, which are reported to influence the predilection of a patient with TB to develop ATT-related hepatotoxicity.
-
4.
Prompt withdrawal of hepatotoxic ATT medications remains the cornerstone for the immediate management of ATT-related DILI.
-
5.
With the current data, it would be acceptable to suggest that a sequential regimen of starting ATT with or without pyrazinamide rather than a concomitant regimen would be suitable as a re-introductory regimen especially in patients having a higher risk of developing ATT-related hepatotoxicity.
1 Introduction
Although the majority of tuberculosis (TB) cases (85%) are treated successfully with anti-tuberculous therapy (ATT) drugs, treatment-related adverse effects remain a prime reason for treatment discontinuation. Skin reactions, gastrointestinal upset, and hepatotoxicity are among the most common adverse effects of ATT drugs. Drug-induced liver injury (DILI) leads to discontinuation of the drug in about 11% of patients receiving a combination of rifampicin (RMP), isoniazid (INH), and pyrazinamide (PZA) [1]. DILI is primarily of three types: (a) direct, (b), idiosyncratic, and (c) indirect [2]. (Table 23.1) ATT drugs constitute one of the most prevalent groups which lead to idiosyncratic DILI [3, 4]. Overall, DILI due to ATT drug therapy has been reported in around 5% to 28% of patients [3]. The reported mortality after the onset of jaundice due to ATT DILI is about 4% to 12%. Patients with ATT-related ALF are also reported to have higher mortality (67%) [4]. Among the first line of ATT drugs that are used (INH, PZA, RMP, and ethambutol), the first three are associated with hepatotoxicity. Among the three, PZA is the most hepatotoxic, followed by INH and RMP [5]. The following section describes in detail about these hepatotoxic ATT drugs.
2 Isoniazid (INH)
INH has bactericidal properties and is effective both against the extra- and intracellular organisms. It acts by inhibiting the mycolic acid synthesis. INH-induced liver toxicity is primarily hepatocellular, causing necrosis and steatosis. The toxic metabolites of INH bind to cellular macromolecules and lead to DILI [6]. Around 0.5% of the patients being treated with INH monotherapy develop raised aminotransferase levels [7]. In patients wherein combination therapies of INH are used (without RMP), the usual incidence of liver toxicity is around 1.6%, whereas in patients with regimens including both INH and RMP, the incidence of hepatotoxicity is around 2.5% [8]. INH is primarily cleared by the liver and is metabolized by two pathways, cytochrome P4502E1 (CYP2E1) and N-acetyltransferase 2 (NAT2) pathways [9]. (Fig. 23.1) The NAT2 pathway leads to the formation of diacetyl hydrazine which is a nontoxic compound. The other pathway involving the hydrolysis and cytochrome P4502E1 pathway leads to the formation of toxic metabolites like acetyl diazine and other reactive acetyl onium ions and acetyl radicals, which have the capacity to covalently bind to cellular macromolecules and cause DILI. Hydrolysis constitutes the minor pathway for INH metabolism; however, in the presence of RMP and in slow acetylators, this minor pathway could dominate, leading to increased incidence of DILI [10]. Genotypes of NAT2 which have been associated with slow acetylation have about a fourfold higher risk of having INH-related DILI [11]. In a meta-analysis that included 474 cases and 1446 controls, the odds ratio to develop INH-related hepatotoxicity was 4.6 in slow acetylators [12]. Glutathione is known for its free radical scavenging properties and removal of toxic metabolites of drugs, and it was hypothesized that individuals having polymorphisms at the glutathione S-transferase (GST) loci would have a higher incidence of ATT DILI. In a pivotal study by Roy et al. [13], it was shown that null mutations of GSTM1 were two times more common in cases with anti-TB DILI when compared to controls. INH-related hepatotoxicity thus appears to be an immune-related idiosyncratic phenomenon due to the toxic metabolites [14].
3 Rifampicin (RMP)
RMP possesses bactericidal properties and leads to inhibition of mycobacterial DNA-dependent RNA polymerase. RMP is metabolized by deacetylation to deacetyl rifampicin and hydrolysis to 3 formyl rifampicin. These metabolites are usually excreted in the bile. RMP-medicated hepatotoxicity is idiosyncratic in nature [15]. RMP-related DILI is usually hepatocellular, and it potentiates the hepatotoxicity of other ATT drugs. RMP may also cause dose-dependent interference in the bilirubin uptake as it competes with it for clearance at the sinusoidal membrane. This can lead to mild unconjugated hyperbilirubinemia without hepatocellular injury. However, RMP can also inhibit the major bile salt exporter pump, which impedes the secretion of conjugated bilirubin. This can transiently lead to conjugated hyperbilirubinemia [16]. Idiosyncratic type of RMP-induced DILI is known to occur in the first month of therapy [17].
4 Pyrazinamide (PZA)
PZA is a derivative of nicotinic acid and undergoes deamidation to form pyrazinoic acid, which is the active form of PZA. The half-life of PZA is longer than RMP and INH. When given at a high dose of 40–50 mg/kg, hepatotoxicity appears in about 15% of patients [18]. Doses of 25–30 mg/kg, which are currently employed in the ATT regimens, are much safer. PZA has the potential to cause both dose-dependent and idiosyncratic type of DILI. PZA can also lead to hypersensitive reactions with eosinophilia, liver injury, and granulomatous hepatitis [19].
5 Fluoroquinolones (FQL)
FQL are used primarily as second-line agents to treat TB in the setting of multidrug-resistant cases or in patients where first-line agents cannot be used. Hepatotoxicity related to FQL is extremely uncommon and related to hypersensitivity type of reactions with eosinophilia and fever [20].
6 Clinical Features
The clinical features of ATT-related DILI have a wide spectrum of variation in terms of severity. The presentation can range from asymptomatic elevation of transaminases to acute hepatitis leading to acute liver injury and acute liver failure. A mild increase in aminotransferases while the patient is on ATT is seen in around 20% of patients, and they are usually asymptomatic. This phenomenon is labeled as hepatic adaptation wherein the elevated transaminases normalize with the continuation of ATT drugs [5]. When symptomatic, the majority of patients have nonspecific symptoms like nausea, vomiting, and abdominal pain. In a study from a large TB center in the UK, ATT-related DILI was reported in 6.9% of patients. Around half the cases of DILI occurred within the first 2 weeks of starting ATT and 87.6% occurred within 8 weeks. The commonest symptoms among patients presenting with ATT-related DILI were nausea and vomiting in 54% of patients followed by abdominal pain in 18% and skin complaints in 17%. Clinical jaundice was noted in around 12% of patients [21]. In a study from Western India, 82 patients with DILI were evaluated, of which 49% were due to ATT drugs. The most common symptoms noted in this study were nausea and vomiting in around 90% of patients with DILI, followed by abdominal pain in 73% and anorexia in 69% of patients. The authors also showed that there was significantly higher mortality for patients with ATT-related DILI (17.5%) vs. those without (2.4%) [22]. In a pivotal study from South India, ATT was the etiology for DILI in 58% of all cases presenting with DILI (n = 313) over a period of 11 years, and ATT was the culprit in around 76% of cases of drug-induced acute liver failure (ALF) [4]. It was also noted in this study that the majority of the patients were relatively younger in age (mean age around 40 years). The mortality rate reported in this study was high (67%) among patients with ALF due to ATT. In another key study by Kumar et al [23], 1223 consecutive patients with ALF were evaluated, and ATT was determined to the etiologic agent in 70 (5.7%) patients. The authors noted that the median time duration of ATT intake before the onset of ALF was about 30 days. In comparison to patients having ALF due to hepatitis E virus (HEV) and non-A non-E etiology, patients with ATT-related ALF were older in age and had a lesser elevation of liver enzymes. The mortality rate was noted to be high among patients with ATT-ALF (67.1%). The authors suggested three factors that independently predicted mortality on the basis of their study - serum bilirubin ≥10.8 mg/dl, elevated prothrombin time (PT) (≥26 seconds), and the presence of high-grade (III/IV) hepatic encephalopathy at presentation [23]. It is thus vital to understand that ATT-related DILI can have a wide variation in its clinical presentation, which can range from the asymptomatic rise of transaminases and mild symptoms of nausea to severe acute liver injury and ALF.
7 Risk Factors for ATT-Related DILI
The factors mentioned below have been reported to influence the predilection of a patient with TB to develop ATT-related hepatotoxicity (Fig. 23.2):
-
(a)
Age: Age has been incriminated as a risk factor to increased predisposition to ATT-related DILI in various studies. In a study assessing over 500 patients on standard ATT, a 3.5-fold higher risk for ATT-related DILI was observed in patients over the age of 60 years [1]. In another study, it was noted that PZA-related adverse effects and DILI were higher (2.6-fold times) in patients above 60 years [24]. The incidence of INH-related DILI is noted to be higher among patients aged above 50 years [25, 26]. Data from another prospective clinical study noted that age over 35 years was an independent predictor to develop ATT-related DILI. Those aged less than 35 years had a 17% risk of ATT-related DILI when compared to 33% among patients who were over 35 years old [27].
The incidence of ATT-induced hepatitis reported in children from various parts of the world ranges from 1.8% to 6.5%, the variations being attributed to the regimen used, drug doses, diagnostic criteria, and type of surveillance, whether active or passive [28, 29]. With the recent increase in pediatric doses of rifampicin (to 10-20 mg/kg/day from previous 10 mg/kg/day) and isoniazid (to 10–15 mg/kg/day from previous 5 mg/kg/day) recommended for use in children, there are concerns about the increase in the incidence of liver injury. A recent Indian study reported an overall incidence of ATT-induced hepatotoxicity in children as 2.3%: 1.9% with old doses of ATT and 2.7% with revised doses; the increase was, however, not statistically significant [30].
-
(b)
Gender: Various studies have reported that women have a higher predilection (fourfold higher risk) to develop ATT-related DILI when compared to men [31]. The activity of the cytochrome enzyme (CYP3A) is reported to be on the higher side in females which in part can explain this higher risk [32].
-
(c)
Nutritional status: Several studies have noted a link between the presence of underlying malnutrition and increased risk of developing ATT-related DILI [33]. In a study by Warmelink et al., it was noted that patients who had a loss of weight of two kgs or more within a span of 4 weeks of ATT had a higher predilection to develop ATT-related DILI [34].
-
(d)
Alcohol intake: Several studies have also linked alcohol consumption to a higher risk of ATT-related DILI. The propensity of alcohol to induce liver enzymes is the postulated mechanism for this link [35, 36].
-
(e)
Concomitant chronic viral infection: Studies have linked a higher predilection of having ATT-related DILI in patients with underlying chronic hepatitis B (CHB) infection. In a study by Wang et al. [37], patients with CHB had a higher risk of developing ATT-related DILI when compared to patients who were uninfected (16% vs. 4.7% p < 0.001). This study also demonstrated that the degree of hepatotoxicity is linked directly to the viral load at the time of starting the ATT. Similar data have also been noted in those patients infected with chronic hepatitis C (CHC) infection. In a study from Miami, it was observed that 30% of patients with CHC infection developed ATT-related DILI when compared with 11% of uninfected patients. The authors similarly noted a trend to increased severity of DILI in those with higher hepatitis C viral load [38]. A study by Anand et al. noted that the presence of concomitant CHB and underlying chronic liver disease were significantly associated with the development of ATT-related DILI [39]. Human immunodeficiency virus (HIV) infection also increased the risk of ATT-related DILI. Various studies from the highly active antiretroviral therapy (HAART) era have noted the risk of ATT-related DILI to be around 4% to 27% among patients on ATT having concomitant HIV infection [40].
-
(f)
Presence of underlying liver disease: The presence of underlying cirrhosis increases the risk for ATT-related DILI. ATT-related DILI in a patient with underlying cirrhosis can trigger an acute-on-chronic liver failure (ACLF), which carries a higher risk of mortality.
-
(g)
Genetic predisposition: Polymorphisms of various genes coding for the enzymes involved in the drug metabolism have been linked to increased predisposition to ATT-related DILI. The prime candidates are genes linked to NAT2 and CYP2E1, which can lead to the formation of reactive drug metabolites and trigger hepatotoxicity. Studies have also shown that the presence of HLA-DQB1*0201 allele and the absence of HLA-DQA1*0102 allele were associated with a higher risk of ATT-related hepatotoxicity [35].
8 Pathophysiology
The pathophysiology of ATT-related hepatotoxicity can be understood as follows:
-
1.
The initiating event: The factors leading to the higher formation of drug metabolites as resulting from phase I metabolism or factors which lead to reduced detoxification as a consequence of the failure of phase II metabolism are likely the key inciting event. The reactive drug metabolites lead to cellular stress by overwhelming the antioxidant defense mechanism or binding with lipids, nucleic acids, or cellular enzymes. These metabolites can also lead to lipid peroxidation, which can lead to cell death [41]. The involvement of mitochondria is also considered a key link in the pathophysiology of DILI. When the mitochondrial respiratory chain is affected, it results in the depletion of adenosine triphosphate (ATP) which can, in turn, lead to the production of reactive oxygen species (ROS) [42].
-
2.
The immune response: An innate immune response is known to propagate or inhibit an inflammatory process, and it thus plays a key role in deciding the fate of progression and severity of DILI. Innate immunity not only guides the production of cytokines involved in hepatic inflammation but also assist in liver regeneration. Inhibition of histone modification is another potential link mediating DILI. Histone acetylation is known to have a key role in gene transcription, and thus exhaustion and depletion of the enzyme histone acetyltransferase can result in the inhibition of hepatic regeneration and thus propagating DILI [43].
9 Diagnosis of ATT-Induced Hepatitis
ATT-induced hepatitis is diagnosed based on the international criteria developed for drug-induced hepatitis.
The criteria included are as follows: [5].
-
(a)
Elevation of transaminases higher than 3 times the upper limit of normal (ULN) or 2 times the ULN of bilirubin in the presence of associated symptoms like anorexia, nausea, vomiting, pain in the right upper abdomen, and jaundice.
-
(b)
Elevation of transaminases higher than 5 times the ULN without the presence of associated symptoms.
10 Management of ATT-Related DILI
The guidelines to manage and approach a patient with ATT-related DILI come from the British Thoracic Society (BTS) [44], the American Thoracic Society (ATS) [19], and the National Institute for Clinical Excellence (NICE), UK [45]. (Fig. 23.3). Revised National Tuberculosis Control Programme (RNTCP) from India has also issued its guidelines in 2019 for reinstituting ATT drugs after the diagnosis of ATT-related DILI [46].
-
(a)
Risk stratification: It is apt to screen the patient for risk factors that lead to increased predisposition to ATT-related DILI. These include assessment of nutritional status, alcohol intake, and evaluating for the presence of superimposed co-infections with hepatitis B, hepatitis C, and HIV. It is imperative to rule out underlying chronic liver disease, which could increase the risk of ATT-related hepatotoxicity. Assessment of this risk–benefit ratio is extremely vital when planning to empirically start ATT.
-
(b)
Immediate action: Prompt withdrawal of ATT medications remains the cornerstone for the immediate management of ATT-related DILI. As mild elevations of transaminases would not justify stoppage of ATT (as they may be a consequence of hepatic adaptation), it is recommended that all the potential hepatotoxic ATT drugs need to be stopped only when alanine aminotransferases (ALT) reach three times the ULN with concurrent symptoms attributable to hepatotoxicity or when the ALT becomes five times the ULN in the absence of associated symptoms [9]. Isolated hyperbilirubinemia without elevation of transaminases does not fulfill the definition of DILI by the DILI working group though the BTS guidance suggests careful monitoring and potentially stopping the hepatotoxic drugs [21, 44]. In patients where the clinical situation merits continual of ATT drugs, non-hepatotoxic drugs like FQL, cycloserine, ethambutol (ETH), and aminoglycosides can be considered. After the withdrawal of ATT drugs, the hepatotoxic anti-TB drugs need to be withheld till normalization of transaminases or at least till the ALT drops below two times the ULN [8].
-
(c)
Re-introductory regimens: In view of the high efficacy of the first-line ATT drugs, it is imperative to consider them in the treatment regimen. It has been noted that the risk of having a repeat episode of ATT-related DILI is around 11% to 24% on re-exposure of the same drug regimen [47]. The BTS and ATS guidelines suggest reintroducing the ATT drugs one at a time; however, the World Health Organization (WHO) recommends starting all the drugs simultaneously and starting the drugs in a consecutive manner only in case of a repeat episode of ATT-related DILI. The RNTCP 2019 guidelines from India recommend adding the primary ATT drugs in a consecutive manner after the liver enzymes become less than 2 times ULN. It suggests starting with a full dose of rifampicin first, and the other ATT drugs are added (in full dose) every 3 days, with regular LFT monitoring. A new drug is reinstituted only if the ALT is less than twice the ULN [46].
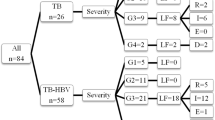
An elegant study randomized 175 patients into 3 different regimens of reintroduction and noted no significant difference in the occurrence of ATT-related repeat DILI [47]. In another study by Tahaoglu et al. [48], the authors concluded that the incidence of ATT-related DILI was higher if the ATT drugs were re-initiated in a full-dose regimen (including pyrazinamide) when compared to a regimen which included a gradual reintroduction of anti-TB drugs without pyrazinamide. In a recent network meta-analysis to assess the impact of various re-introductory regimens on the risk of developing ATT-related hepatotoxicity, four randomized controlled trials with 577 patients were analyzed. It was shown that the sequential regimen with incremental doses of anti-TB drugs was linked to a significantly reduced risk of ATT-related hepatotoxicity when compared to the concomitant full-dose regimen. This meta-analysis also suggested that the re-introductory regimen using RMP first or INH first leads to similar rates of ATT-related hepatotoxicity [49]. With the current data, it would be acceptable to suggest that a sequential regimen with or without PZA rather than a concomitant regimen would be suitable as a re-introductory regimen especially in patients having a higher risk of developing ATT-related hepatotoxicity, e.g., those with malnutrition, concomitant hepatitis B, and hepatitis C infection [47]. Using an incremental dose strategy for RMP and INH, wherein one drug is started at a time using half its dose initially, it would be feasible to identify the drug responsible for hepatotoxicity if and when the transaminases get elevated. This incremental dose regimen would likely be less hepatotoxic as the patient is not exposed to all the hepatotoxic drugs at full dose simultaneously. However, a longer time is required to attain the target dose of ATT drugs for the patient. There is currently no concrete evidence to suggest that 3 times per week regimen is less hepatotoxic than a daily regimen [50]. As INH and RMP are very efficacious in the management of TB, it is imperative that their use is considered in the ATT regimen whenever feasible.
Possible regimens would include [9].
-
(i)
Regimen containing two hepatotoxic drugs:
-
Nine months of RMP and INH, plus ETH.
-
Two months of RMP, INH, amikacin, or streptomycin and ETH, followed by six months of RMP and INH.
-
Six to nine months of RMP, PZA, and ETH.
-
-
(ii)
Drug regimen with one hepatotoxic drug:
-
Two months of INH, ETH, and amikacin or streptomycin, followed by 10 months of INH and ETH.
-
-
(iii)
Drug regimen with no hepatotoxic drugs:
-
Eighteen to twenty-four months treatment with a combination therapy of ETH, FQL, cycloserine, and aminoglycoside or capreomycin can be considered.
-
11 ATT Regimen in Patients with Underlying Cirrhosis
The severity of DILI may be more severe when occurring in the setting of underlying cirrhosis. ATT-related DILI can trigger an ACLF in patients with underlying CLD, which can be associated with high mortality. In a recent study by Devarbhavi et al. [51], ATT was incriminated in the etiology of acute insult in 27.3% of patients who presented with drug-induced ACLF. The authors also noted that mortality was higher in patients with ACLF in whom the acute insult was related to drugs vs. those with non-drug-induced ACLF (46.5% vs. 38.8%). This data emphasizes the extreme vigilance which has to be taken in monitoring therapy with ATT drugs when used in patients with underlying cirrhosis. Table 23.2 provides a guide on the regimen to be used in patients with underlying cirrhosis based on the basis of Child–Turcotte–Pugh (CTP) score [52].
12 Role of Drugs in ATT-Related DILI
Withholding ATT drugs having hepatotoxic potential in case of development of ATT-related DILI is the primary step in the management of such patients. Baniasadi and colleagues evaluated the role of N-acetylcysteine (NAC) in preventing ATT-related DILI in an RCT, which compared ATT with NAC vs. ATT alone. The authors noted that hepatotoxicity related to anti-TB drugs occurred in 37.5% of patients in the group not receiving NAC and none in the group where concomitant NAC was administered [53]. However, more studies are required to confirm the role of NAC in preventing ATT-related DILI, especially in patients with underlying risk factors.
13 Conclusion
TB continues to impose a significant healthcare burden in the world, and in India. Accurate diagnosis and prompt treatment remain the cornerstone to control the wrath imposed by this disease. As the first-line drugs used in the treatment of TB have a predilection for causing hepatotoxicity, identifying the high-risk patients and careful monitoring on therapy play a vital role in the early diagnosis and apt treatment. A knee-jerk reaction of stopping ATT drugs should not be done with a marginal rise in transaminases (hepatic adaptation) as, in most cases, they would normalize and prevent the development of drug-resistant tuberculosis. When specific stopping rules are attained, as mentioned above, stopping ATT drugs and continuing anti-TB medicines without hepatotoxic potential are recommended. A sequential regimen with incremental doses of drugs currently seems to be the norm in planning the re-introductory regimen, especially in patients having risk factors in developing ATT-related DILI.
Abbreviations
- ACLF:
-
acute-on-chronic liver failure
- ALF:
-
acute liver failure
- ALT:
-
alanine aminotransferases
- ATP:
-
adenosine triphosphate
- ATS:
-
American Thoracic Society
- ATT:
-
anti-tuberculous therapy
- BTS:
-
British Thoracic Society
- CHB:
-
chronic hepatitis B
- CHC:
-
chronic hepatitis C
- CLD:
-
chronic liver disease
- CTP:
-
Child–Turcotte–Pugh
- DILI:
-
drug-induced liver injury
- ETH:
-
ethambutol
- FQL:
-
fluoroquinolones
- GST:
-
glutathione S-transferase
- HAART:
-
highly active antiretroviral therapy
- HEV:
-
hepatitis E virus
- HIV:
-
human immunodeficiency virus
- INH:
-
isoniazid
- NAC:
-
N-acetylcysteine
- NAT:
-
N-acetyltransferase
- NICE:
-
National Institute for Clinical Excellence
- PT:
-
prothrombin time
- PZA:
-
pyrazinamide
- RMP:
-
rifampicin
- RNTCP:
-
Revised National Tuberculosis Control Programme
- ROS:
-
reactive oxygen species
- TB:
-
tuberculosis
- ULN:
-
upper limit of normal
- WHO:
-
World Health Organization
References
Schaberg T, Rebhan K, Lode H. Risk factors for side-effects of isoniazid, rifampin and pyrazinamide in patients hospitalized for pulmonary tuberculosis. Eur Respir J. 1996;9:2026–30.
Hoofnagle JH, Björnsson ES. Drug-induced liver injury–types and phenotypes. N Engl J Med. 2019;381:264–73.
Ostapowicz G, Fontana RJ, Schiodt FV, et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med. 2002;137:947–54.
Devarbhavi H, Dierkhising R, Kremers WK. Antituberculosis therapy drug-induced liver injury and acute liver failure. Hepatology. 2010;52:798–9. Author reply 9–800
Devarbhavi H. Antituberculous drug-induced liver injury: current perspective. Trop Gastroenterol. 2011;32:167–74.
Tostmann A, Boeree MJ, Aarnoutse RE, de Lange WC, van der Ven AJ, Dekhuijzen R. Antituberculosis drug-induced hepatotoxicity: concise up-to-date review. J Gastroenterol Hepatol. 2008;23:192–202.
Fountain FF, Tolley E, Chrisman CR, Self TH. Isoniazid hepatotoxicity associated with treatment of latent tuberculosis infection: a 7-year evaluation from a public health tuberculosis clinic. Chest. 2005;128:116–23.
Steele MA, Burk RF, DesPrez RM. Toxic hepatitis with isoniazid and rifampin. A meta-analysis Chest. 1991;99:465–71.
Ramappa V, Aithal GP. Hepatotoxicity related to anti-tuberculosis drugs: mechanisms and management. J Clin Exp Hepatol. 2013;3:37–49.
Sarma GR, Immanuel C, Kailasam S, Narayana AS, Venkatesan P. Rifampin-induced release of hydrazine from isoniazid. A possible cause of hepatitis during treatment of tuberculosis with regimens containing isoniazid and rifampin. Am Rev Respir Dis. 1986;133:1072–5.
Huang YS, Chern HD, Su WJ, et al. Polymorphism of the N-acetyltransferase 2 gene as a susceptibility risk factor for antituberculosis drug-induced hepatitis. Hepatology. 2002;35:883–9.
Wang PY, Xie SY, Hao Q, Zhang C, Jiang BF. NAT2 polymorphisms and susceptibility to anti-tuberculosis drug-induced liver injury: a meta-analysis. Int J Tuberc Lung Dis. 2012;16:589–95.
Roy B, Chowdhury A, Kundu S, et al. Increased risk of antituberculosis drug-induced hepatotoxicity in individuals with glutathione S-transferase M1 'null' mutation. J Gastroenterol Hepatol. 2001;16:1033–7.
Metushi IG, Cai P, Zhu X, Nakagawa T, Uetrecht JP. A fresh look at the mechanism of isoniazid-induced hepatotoxicity. Clin Pharmacol Ther. 2011;89:911–4.
Verma S, Kaplowitz N. Diagnosis, management and prevention of drug-induced liver injury. Gut. 2009;58:1555.
Byrne JA, Strautnieks SS, Mieli-Vergani G, Higgins CF, Linton KJ, Thompson RJ. The human bile salt export pump: characterization of substrate specificity and identification of inhibitors. Gastroenterology. 2002;123:1649–58.
Zierski M, Bek E. Side-effects of drug regimens used in short-course chemotherapy for pulmonary tuberculosis. A controlled clinical study. Tubercle. 1980;61:41–9.
Senousy BE, Belal SI, Draganov PV. Hepatotoxic effects of therapies for tuberculosis. Nat Rev Gastroenterol Hepatol. 2010;7:543–56.
Saukkonen JJ, Cohn DL, Jasmer RM, et al. An official ATS statement: hepatotoxicity of antituberculosis therapy. Am J Respir Crit Care Med. 2006;174:935–52.
Andrade RJ, Tulkens PM. Hepatic safety of antibiotics used in primary care. J Antimicrob Chemother. 2011;66:1431–46.
Abbara A, Chitty S, Roe JK, et al. Drug-induced liver injury from antituberculous treatment: a retrospective study from a large TB Centre in the UK. BMC Infect Dis. 2017;17:231.
Rathi C, Pipaliya N, Patel R, Ingle M, Phadke A, Sawant P. Drug induced liver injury at a tertiary Hospital in India: etiology, clinical features and predictors of mortality. Ann Hepatol. 2017;16:442–50.
Kumar R, Bhatia V, Khanal S, et al. Antituberculosis therapy-induced acute liver failure: magnitude, profile, prognosis, and predictors of outcome. Hepatology. 2010;51:1665–74.
Yee D, Valiquette C, Pelletier M, Parisien I, Rocher I, Menzies D. Incidence of serious side effects from first-line antituberculosis drugs among patients treated for active tuberculosis. Am J Respir Crit Care Med. 2003;167:1472–7.
Millard PS, Wilcosky TC, Reade-Christopher SJ, Weber DJ. Isoniazid-related fatal hepatitis. West J Med. 1996;164:486–91.
Snider DE Jr, Caras GJ. Isoniazid-associated hepatitis deaths: a review of available information. Am Rev Respir Dis. 1992;145:494–7.
Hwang SJ, Wu JC, Lee CN, et al. A prospective clinical study of isoniazid-rifampicin-pyrazinamide-induced liver injury in an area endemic for hepatitis B. J Gastroenterol Hepatol. 1997;12:87–91.
Aishatu G, Rasheedah I, Wahab J, Sheni M, Damilola O, Adeniyi O. Hepatotoxicity due to antituberculosis therapy among paediatric patients seen at the University of Ilorin Teaching Hospital, north Central Nigeria. Ethiop J Health Sci. 2017;27:115–20.
Li Y, Zhu Y, Zhong Q, Zhang X, Shu M, Wan C. Serious adverse reactions from anti-tuberculosis drugs among 599 children hospitalized for tuberculosis. Pediatr Infect Dis J. 2017;36:720–5.
Indumathi CK, Sethuraman A, Jain S, Krishnamurthy S. Revised Antituberculosis drug doses and hepatotoxicity in HIV negative children. Indian J Pediatr. 2019;86:229–32.
Lee AM, Mennone JZ, Jones RC, Paul WS. Risk factors for hepatotoxicity associated with rifampin and pyrazinamide for the treatment of latent tuberculosis infection: experience from three public health tuberculosis clinics. Int J Tuberc Lung Dis. 2002;6:995–1000.
Hunt CM, Westerkam WR, Stave GM. Effect of age and gender on the activity of human hepatic CYP3A. Biochem Pharmacol. 1992;44:275–83.
Singla R, Sharma SK, Mohan A, et al. Evaluation of risk factors for antituberculosis treatment induced hepatotoxicity. Indian J Med Res. 2010;132:81–6.
Warmelink I, ten Hacken NH, van der Werf TS, van Altena R. Weight loss during tuberculosis treatment is an important risk factor for drug-induced hepatotoxicity. Br J Nutr. 2011;105:400–8.
Sharma SK, Balamurugan A, Saha PK, Pandey RM, Mehra NK. Evaluation of clinical and immunogenetic risk factors for the development of hepatotoxicity during antituberculosis treatment. Am J Respir Critic Care Med. 2002;166:916–9.
White MC, Tulsky JP, Lee JR-J, et al. Isoniazid vs. rifampin for latent tuberculosis infection in jail inmates: toxicity and adherence. J Correct Health Care. 2012;18:131–42.
Wang JY, Liu CH, Hu FC, et al. Risk factors of hepatitis during anti-tuberculous treatment and implications of hepatitis virus load. J Infect. 2011;62:448–55.
Ungo JR, Jones D, Ashkin D, et al. Antituberculosis drug-induced hepatotoxicity. The role of hepatitis C virus and the human immunodeficiency virus. Am J Respir Crit Care Med. 1998;157:1871–6.
Anand AC, Seth AK, Paul M, Puri P. Risk factors of hepatotoxicity during anti-tuberculosis treatment. Med J Armed Forces India. 2006;62:45–9.
Dworkin MS, Adams MR, Cohn DL, et al. Factors that complicate the treatment of tuberculosis in HIV-infected patients. J Acquir Immune Defic Syndr. 2005;39:464–70.
Nanashima K, Mawatari T, Tahara N, et al. Genetic variants in antioxidant pathway: risk factors for hepatotoxicity in tuberculosis patients. Tuberculosis. 2012;92:253–9.
Boelsterli UA, Lim PLK. Mitochondrial abnormalities–a link to idiosyncratic drug hepatotoxicity? Toxicol Appl Pharmacol. 2007;220:92–107.
Murata K, Hamada M, Sugimoto K, Nakano T. A novel mechanism for drug-induced liver failure: inhibition of histone acetylation by hydralazine derivatives. J Hepatol. 2007;46:322–9.
Chemotherapy and management of tuberculosis in the United Kingdom: recommendations. Joint tuberculosis Committee of the British Thoracic Society. Thorax. 1998;1998(53):536–48.
National Collaborating Centre for Chronic C, Centre for Clinical Practice at N. National Institute for Health and Clinical Excellence: Guidance. Tuberculosis: Clinical Diagnosis and Management of Tuberculosis, and Measures for Its Prevention and Control. London: National Institute for Health and Clinical Excellence (UK) Royal College of Physicians of London. Updated text, Copyright (c) 2011, National Institute for Health and Clinical Excellence.; 2011.
RNTCP Updated pediatric TB guidelines 2019. Accessed 05 May 2020.
Sharma SK, Singla R, Sarda P, et al. Safety of 3 different reintroduction regimens of antituberculosis drugs after development of antituberculosis treatment-induced hepatotoxicity. Clin Infect Dis. 2010;50:833–9.
Tahaoglu K, Atac G, Sevim T, et al. The management of anti-tuberculosis drug-induced hepatotoxicity. Int J Tuberc Lung Dis. 2001;5:65–9.
Soni H, Kumar MP. Risk of hepatitis with various reintroduction regimens of anti-tubercular therapy: a systematic review and network meta-analysis. Expert Rev Anti-Infect Ther. 2020;18:171–9.
Chang KC, Leung CC, Yew WW, Tam CM. Standard anti-tuberculosis treatment and hepatotoxicity: do dosing schedules matter? Eur Resp J. 2007;29:347–51.
Devarbhavi H, Choudhury AK, Sharma MK, et al. Drug-induced acute-on-chronic liver failure in Asian patients. Am J Gastroenterol. 2019;114:929–37.
Dhiman RK, Saraswat VA, Rajekar H, Reddy C, Chawla YK. A guide to the management of tuberculosis in patients with chronic liver disease. J Clin Exp Hepatol. 2012;2:260–70.
Baniasadi S, Eftekhari P, Tabarsi P, et al. Protective effect of N-acetylcysteine on antituberculosis drug-induced hepatotoxicity. Eur J Gastroenterol Hepatol. 2010;22:1235–8.
Treatment of tuberculosis. MMWR Recomm Rep. 2003;52:1–77.
Conflict of Interest
None.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Satsangi, S., Randev, S., Taneja, S. (2022). Antitubercular Therapy-Related Hepatitis. In: Sharma, V. (eds) Tuberculosis of the Gastrointestinal system. Springer, Singapore. https://doi.org/10.1007/978-981-16-9053-2_23
Download citation
DOI: https://doi.org/10.1007/978-981-16-9053-2_23
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-9052-5
Online ISBN: 978-981-16-9053-2
eBook Packages: MedicineMedicine (R0)