Abstract
In 2016, WHO formally validated the elimination of lymphatic filariasis as a public health problem in Sri Lanka. This brought the country closer to the end of a decades-long effort to reduce the burden of this painful, debilitating and stigmatizing condition. The disease is traceable in Sri Lanka as far back as the third century BC. In 1937–1939, the first countrywide survey found that Mf rates ranged from 20 to 24% across the island. The first organized response to lymphatic filariasis came in 1947 in the form of the Anti-Filariasis Campaign (AFC). Several features of Sri Lanka’s approach to lymphatic filariasis are especially noteworthy. The technical soundness of the country’s lymphatic filariasis programme was promoted by a collaboration of partners. Systematic surveys and surveillance were undertaken, including active searches, routine surveillance and sentinel surveillance. Mapping of endemic areas aided in targeting disease control efforts. Differential strategies were pursued for urban and rural settings; biomedical and public health approaches were complemented by robust social and communications sciences; and rigorous studies confirmed the elimination of the disease. A strong public health system proved to be vital for the success of the drive to eliminate lymphatic filariasis. The dedication of the health staff of the AFC and regional anti-filariasis units was noteworthy. Political support for the national effort to eliminate lymphatic filariasis was unwavering and sustained over time. Domestic resources largely financed the many activities associated with the national programme.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
7.1 Background
In 2016, WHO formally validated the elimination of lymphatic filariasis as a public health problem in Sri Lanka. This brought the country closer to the end of a decades-long effort to reduce the burden of this painful, debilitating and stigmatizing condition. Sri Lanka’s successful fight to eliminate lymphatic filariasis overcame considerable obstacles. It underscores the importance of strong national leadership, effectiveness of recommended strategies for elimination of lymphatic filariasis, value of decentralized services and engagement of affected communities.
Sri Lanka, a tropical island, has a widely varying topography and climate. Large swathes of the country experience heavy rainfall and humid conditions. These are the very conditions that facilitate the breeding of mosquitoes that serve as vectors for lymphatic filariasis. More than half (53%) of the country’s over 20 million people live in three provinces where lymphatic filariasis was endemic [1]. These endemic provinces extended in a crescent along the western and southern shores of the country [1].
Lymphatic filariasis is one of four leading vector-borne diseases in Sri Lanka, along with dengue, malaria and Japanese encephalitis, and has long been a cause of disability in the country [1]. The disease is traceable in Sri Lanka as far back as the third century bc [1]. References to “elephantiasis” have been found in some early Buddhist texts and medical chronicles penned by the physician king Buddhadasa in the fourth century ad. More recent historical references to the disease as a serious problem date to the colonial period when the country was under British administration and known as Ceylon [1]. The disease finds mention in the 1821 book by John Davy as well as in official British records such as the reports of the Principal Civil Medical Officer and the Inspector General of Prisons in 1879. The earliest microfilaria case (Filaria sanguinis hominis) was detected in 1892 from Matara Hospital.
Some information about the extent of the problem appeared with small surveys done at the beginning of the twentieth century. In 1914, an early epidemiological study reported hotspots of infection in the southern, north-western, western and eastern parts of the country, with the highest microfilaria (Mf) rate (26.6%) recorded from Toppur in Trincomalee district [1]. Raised Mf rates (ranging from 8.8% to 14.2%) were also found in the southern part of the country [1]. The long-term effects of filariasis in the form of elephantiasis, hydrocele and chyluria were also reported in this survey, besides the presence of Mf. Another survey was conducted in 1925 in the southern province during which night blood films were taken. The Mf rate in this survey was found to be 4.8% and the type of filariasis present was presumed to be due to Wuchereria bancrofti. By the 1930s, the problem appears to have worsened. In 1937–1939, the first countrywide survey found that Mf rates ranged from 20 to 24% across the island [1].
The earliest epidemiological surveys found a nationwide prevalence of W. bancrofti, one of three species of thread-like worms that cause lymphatic filariasis, which is carried by mosquitoes. However, subsequent surveys found localized hotspots of Brugia malayi, primarily due to favourable local breeding conditions for the Mansonia species of mosquito that carries the Brugia malayi strain [1]. W. bancrofti predominated in urban areas, while B. malayi cases were largely confined to rural areas [1]. There was geographical variation in terms of both the Mf rate and type of vectors involved, indicating that filariasis in Sri Lanka was highly localized and was restricted to areas environmentally conducive to the breeding of specific mosquito vectors. Subsequent studies showed that bancroftian filariasis emerged as a problem after the Second World War, mainly in the south-western coastal belt. The problem was traced to the proliferation of mosquitoes in bucket latrines in which wastewater used to stagnate, providing ideal grounds for vector breeding [1].
The health system responded to the problem early on, keeping in view the results of the various surveys. As early as 1926, steps were taken to strengthen the country’s primary health care system and improve sanitation efforts [2]. The first organized response to lymphatic filariasis came in 1947 in the form of the Anti-Filariasis Campaign (AFC) established by the Department of Health under the administrative control of the Deputy Director of Public Health Services. Under this initiative, a central laboratory, a supply store, a workshop, and 17 peripheral investigation units with entomological assistants were established [1]. Subsequently, more health personnel were allocated for the AFC [1].
The Campaign mainly focused on night blood surveys, detection of clinical cases, health education for the general public, localization of infective foci and identification of insect vectors and their breeding sites. Initially, AFC activities were limited to parasitological investigation and control, vector control and limited health education campaigns in a few affected urban council towns. It was found that W. bancrofti was responsible for transmission of the disease in urban areas while Brugia malayi was the cause in rural areas.
7.2 Road to Elimination of Lymphatic Filariasis
A year after the AFC was launched, the first filariasis clinic was established at Dehiwala to enable patients with filariasis to obtain health services. Originally held once a week, the clinic soon expanded to three times a week, with specific, separate dedicated opening hours for men and for women [1]. The clinic helped to detect a large number of clinical cases of filariasis among family members and neighbours of patients who visited the clinic. The treatment consisted mainly of lithium antimony thiomalate, stibamine glucoside and the newly introduced diethylcarbamazine citrate or DEC. The new drug was administered orally in specified doses three times a day for seven days to a limited number of patients to see the impact on Mf count. A second clinic was established in August the same year. Along with treatment, mosquito control measures—DDT spraying in houses and water pools around them—were also launched in the areas that came under the two clinics. A WHO expert, who reviewed the situation in Sri Lanka, made a series of recommendations on various components of AFC implementation. One of the policy recommendations was to provide an efficient sewerage system in urban areas and give priority to targeting infection with W. bancrofti. All municipalities had to undertake mosquito control measures as a part of general public health activity. Intensive training of entomological staff was recommended for filariasis control. Several of these recommendations were made part of operational procedures and additional clinics were established to address the disease.
Initially, the key campaign activities included night blood surveys, detection of clinical cases, public education, and mapping of vectors and their breeding spots [1].
It quickly became clear that the ambitious national campaign was understaffed, leading to an increase in staff numbers that more than doubled the per capita distribution of parasitological staff. Antilarval measures were expanded, a special health education unit attached to the campaign was established, and entomological work was reorganized and strengthened [1].
In the 1960s, Mf-positive persons were provided with three weeks of DEC treatment, and the contacts of Mf-positive individuals were given a week-long course of DEC. Blood films of all Mf cases and contacts were done within six weeks of treatment completion and at six-month intervals, with treatment repeated where necessary [1].
Efforts to manage and mitigate the symptoms of lymphatic filariasis were launched. All of the typical symptoms of lymphatic filariasis were found in the country. Genital symptoms were most frequently associated with bancroftian filariasis, while B. malayi cases manifested most often with affection of the limbs and glands [1]. Across the country, swelling of the legs was by far the most common clinical condition associated with lymphatic filariasis [1].
The first mass administration of DEC was implemented in 1969 in Walgama, a semi-urban area in Matara district with a population of over 10 000 people. At that time, about 230 people in this place were under treatment for filariasis. Mosquito breeding was very high in coconut husk soakage pits and quarry pits. The water supply came mainly from open wells, and also supplied sanitation pit latrines that were in use. Health personnel visited every registered household to give the required doses of DEC every day for five days. All the people were followed up and complaints of adverse reactions, fever, etc. were attended to. A night blood examination survey conducted from October 1970 to September 1971 showed that the Mf rate in Walgama had fallen to 1.52% from 3.9% in 1969.
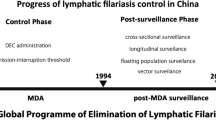
By the early 1980s, the average Mf rate in endemic districts had been reduced to below 1% (Fig. 7.1) [2]. Further progress was made in reducing the Mf rate and, in 2002, Sri Lanka embarked on a targeted five-year campaign of mass drug administration (MDA) that was rolled out in all endemic districts. It was a carefully planned operation, based on analysis of data pertaining to Mf prevalence, clinical and transmission data in endemic districts as well as data from non-endemic areas. Each of the eight endemic districts was designated as one implementation unit (IU). Nine districts fell in the category of non-endemic and eight others were called “uncertain areas”. The strategy was to administer one dose of DEC for the clearance of microfilaraemia and sustain it for one year; and albendazole to enhance the effect of Mf clearance.
The AFC, along with the Medical Supplies Division of the Ministry of Health, worked hard to ensure drug supply in all the IUs to make the MDA campaign successful. On the ground, public health midwives and volunteers—called filariasis prevention assistants (FPAs)—played a key role. They ensured that every identified individual got the designated dose of the two-drug regimen. Each FPA was assigned 50 households to visit twice before MDA was rolled out—to enrol members for MDA and convince them by answering all their queries. In all, 50 000 of these foot soldiers toiled to make the programme a success. The day selected for administration of MDA was designated as National Filariasis Day, which was usually a Sunday. The AFC and the Ministry of Health also recognized the need for an effective, high-impact social mobilization campaign and communication–education support for the MDA programme. It was critical to achieve the goal of making 80% of all eligible household members consume tablets to prevent lymphatic filariasis. A social mobilization project—Communication for Behavioural Impact (COMBI)—was launched with the help of WHO. It included print, radio and television programming on different aspects of the disease, its transmission cycle, treatment with DEC and albendazole as well as morbidity management and control.
Community acceptance of the therapy, as a result of advocacy and persuasive communication, was critical for the success of MDA. When MDA with only DEC was administered for the first time in the entire endemic belt in 1999, the drug could be delivered to only 62.7% of the target population. In 2000, two rounds of MDA reported coverage of 68.2% and 70.5%, respectively. Subsequently, albendazole was added to MDA and was tried in only one district—Colombo—in May 2001. It achieved a coverage of 76.7%. The first national MDA with both the drugs was rolled out in July 2002 and covered 80% of the target population [1]. This could be attributed to the success of COMBI, along with other factors, such as commitment of health workers, continuous supply of drugs and minimal side-effects of the two-drug regimen. Five consecutive rounds of MDA with DEC and albendazole were completed in 2006 and MDA was stopped in 2007. The average Mf rate at the end of the MDA rounds was reported to be 0.03%, much below the WHO elimination target of less than 1% (Fig. 7.2).
In 2008, post-MDA surveillance (using immunochromatographic test [ICT] kits among grade 1 schoolchildren in endemic areas) found no evidence of lymphatic filariasis transmission [2]. Subsequent transmission assessment surveys among schoolchildren and special night blood film surveys in highly endemic hotspots were undertaken to confirm the lack of transmission. Thereupon, Sri Lanka, under the guidance of WHO, compiled a dossier documenting the country’s approach and achievements, leading to the 2016 validation that lymphatic filariasis as a public health problem had been eliminated in the country [2].
7.3 Overcoming the Challenges to Eliminating Lymphatic Filariasis
The long battle to eliminate lymphatic filariasis in Sri Lanka was marked by technical and political challenges. Even though national efforts had, by the 1980s, driven average Mf prevalence under 1% in all endemic districts, hotspots with rates above 1% (the agreed threshold for elimination) were found in Galle district [1]. This necessitated intensified, locally focused efforts to lower Mf rates in this district below the elimination threshold.
The discovery of Brugia malayi also complicated national elimination efforts by requiring specific monitoring for the strain. In addition, massive periodic epidemics of dengue drew substantial national attention and resources, diverting human resources assigned for the elimination of lymphatic filariasis [2].
During the period of the elimination programme, the internal conflict in the northern and eastern parts of the country posed peculiar problems. Due to the separatist conflict in these areas, people were constantly on the move to find safer places. People from the civil war zones moved to different parts of the country, including Puttalam district, which was endemic for filariasis. Such internal migration put extra pressure on the elimination programme, necessitating surveys even in non-endemic districts. The armed conflict, which began in 1983 and ended in 2009, disrupted or fractured various disease control programmes [4]. The health staff worked against all such odds.
7.4 Key Elements of Success
Several features of Sri Lanka’s approach to lymphatic filariasis are especially noteworthy. The technical soundness of the country’s lymphatic filariasis programme was promoted by a collaboration of partners, including the national government, WHO, the Liverpool School of Tropical Medicine (UK), Washington University (USA) and others [2]. Systematic surveys and surveillance were undertaken, including active searches, routine surveillance and sentinel surveillance. Mapping of endemic areas aided in targeting disease control efforts [2]. Differential strategies were pursued for urban and rural settings; biomedical and public health approaches were complemented by robust social and communications sciences; and rigorous studies confirmed the elimination of the disease [2].
A strong public health system proved to be vital for the success of the drive to eliminate lymphatic filariasis. Since Independence, successive governments have prioritized the provision of free health care and education [1]. With broad oversight provided by the Ministry of Health, the health services, beginning in 1989, were decentralized, leading to the creation of provincial health ministries in each of the nine provinces [1].
The dedication of the health staff of the AFC and regional anti-filariasis units was noteworthy. In addition, the provincial and regional health authorities, staff of medical officers of health, including public health midwives and the many local volunteers (FPAs) they recruited played pivotal roles in the national push to eliminate lymphatic filariaris, serving as the interface between communities and drug distribution during MDA rounds [2]. House-to-house contact among roughly 50 000 frontline workers and volunteers, as well as an extensive WHO-supported community mobilization campaign, facilitated successful implementation of the MDA campaign [2]. Health workers trained patients in home-based care and provided adherence support [2].
Political support for the national effort to eliminate lymphatic filariasis was unwavering and sustained over time. Domestic resources largely financed the many activities associated with the national programme [2]. Political leadership ensured the domestic production and procurement of the drug DEC, as well as the importation of albendazole (with WHO support) for the MDA campaign [2].
7.5 Moving Forward
Sri Lanka has expressed strong commitment to maintaining the elimination of lymphatic filariasis, which will require continued vigilance for the remaining hotspots. In particular, Galle, in the southern part of Sri Lanka, remains an area of high endemicity. As needed, high-coverage treatment interventions, using methods such as directly observed therapy, will be conducted. Continued focus is needed on regular parasitological and entomological monitoring, elimination of mosquito breeding sites, and both special and routine surveillance [2]. Sri Lanka has to be on a constant vigil as the disease is still prevalent in neighbouring India from where there is a constant flow of people. From mid-2019, the Sri Lankan Government with the International Organization for Migration (IOM) initiated screening for four diseases, including filariasis, of travellers who request for a visa for more than 6 months.
The country’s experience has also demonstrated the criticality of continuing robust surveillance even after MDA has ended. Such an exercise can help to identify the remaining hotspots of transmission. It may be difficult to obtain representative data in situations where lymphatic filariasis in one community may be below the threshold while the prevalence rate is high in a neighbouring village. Smaller units are more sensitive for detecting the persistence or resurgence of lymphatic filariasis [5]. It is also necessary to keep the health system geared for managing morbidity among chronic patients in previously endemic areas.
An impending threat is that of climate change, as far as vector-borne diseases such as lymphatic filariasis are concerned. By all available evidence, Sri Lanka is highly vulnerable to climate change. Extreme weather events such as high-intensity rainfall followed by flash floods and landslides are already being reported. The temperature pattern too is changing. The zone experiencing an annual average temperature of above 26 °C is increasing. It is feared that mosquito-borne disease transmission in coastal areas will be influenced by not just global climate change causing alterations in temperature, rainfall and humidity, but also due to rising sea levels [6].
References
Anti-Filariasis Campaign of Ministry of Health (2014) National documention on certification of elimination of lymphatic filariasis in Sri Lanka. Colombo: Ministry of Health
A nation rejoices (2016) Elimination of lymphatic filariasis in Sri Lanka. Geneva: World Health Organization
Abdulcader MHM, Padley R (1961) Review of the problems of filariasis of Ceylon. Journal of the Ceylon Public Health Association. 2:101–124
Siriwardhana C, Wickramage K (2014) Conflict, forced displacement and health in Sri Lanka: a review of the research landscape. Confl Health. 8(1):22
Specht S, Suma TK, Pedrique B, Hoerauf A (2019) Elimination of lymphatic filariasis in South East Asia. BMJ. 364:k5198
Ramasamy R, Surendran SN (2012) Global climate change and its potential impact on disease transmission by salinity-tolerant mosquito vectors in coastal zones. Front Physiol 3:198
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 World Health Organization
About this chapter
Cite this chapter
Dilhani Samarasekera, S., Pendse, R. (2021). Lymphatic Filariasis Elimination in Sri Lanka: Overcoming the Odds. In: Singh, P.K. (eds) Elimination of Infectious Diseases from the South-East Asia Region. SpringerBriefs in Public Health. Springer, Singapore. https://doi.org/10.1007/978-981-16-5566-1_7
Download citation
DOI: https://doi.org/10.1007/978-981-16-5566-1_7
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-5565-4
Online ISBN: 978-981-16-5566-1
eBook Packages: MedicineMedicine (R0)