Abstract
Sleep is a complex physiological process that plays a fundamental role in maintaining homeostasis and overall health. It has an internal structure characterized by sleep stages, which is often affected by either the high demands of the current 24-h society or by different sleep disorders such as sleep apnea. These disturbances to the regular sleep structure have been strongly associated with reductions in cognitive and behavioral performance, attention deficit, depression, nocturia, memory loss, snoring, and cardiovascular diseases. Therefore, it is crucial to identify sleep problems in an early stage before the overall health is compromised in an irreversible way. Currently, sleep disorders are diagnosed using polysomnography (PSG), which is the gold-standard sleep test usually recorded in a sleep laboratory. This test is often associated with elevated costs and reduced comfort. With this in mind, many studies have focused on the development of wearables and unobtrusive technologies that can be used at home and that can monitor sleep during more than one single night. This chapter discusses unobtrusive state-of-the-art sensors and algorithms for sleep monitoring in adults, with a special focus on heart rate, respiration, and blood oxygenation monitoring.
M. Deviaene–D. Huysmans—These authors have equal contributions to the work.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
1 Physiological Background of Human Sleep
Sleep is a natural, though complex process, which follows an internal architecture of alternating states. As such, sleep cannot be described by a single state of the body. Instead, it consists of different sleep stages. These sleep stages are associated with characteristic patterns at cerebral, cardiac, and respiratory levels. However, sleep disorders could alter these characteristics. Therefore, the detailed analysis of one’s sleep architecture could serve the detection of these sleep disorders.
1.1 Sleep Stages
Sleep stages and their characteristics were first defined by Rechtschaffen and Kales (R&K) in 1968 [132]. Later in 2007, the American Academy of Sleep Medicine (AASM) updated these R&K rules and published a manual for sleep scoring and associated events [26]. These sleep scoring rules are based on patterns and wave characteristics found in the electroencephalogram (EEG),Footnote 1 the electrooculogram (EOG),Footnote 2 and the chin electromyogram (EMG).Footnote 3 To facilitate the analysis, input signals are scored in consecutive windows of 30s, which are referred to as epochs [132]. Every epoch is scored with one of the five sleep stages defined by the AASM. These stages are Wakefulness (W), Rapid Eye Movement sleep (REM sleep), and non-REM (NREM) sleep 1, 2, and 3 (respectively N1, N2, and N3). Usually, stages N1 and N2 are referred to as light sleep and N3 as deep sleep [138].
Apart from patterns in the EEG, EOG, and EMG signals, differences in sleep stages are reflected in the regulation of both branches of the autonomic nervous system (ANS), namely, the parasympathetic nervous system (PNS) and the sympathetic nervous system (SNS) [104]. As such, distinct characteristics can be observed as well at cardiac, respiratory, and cardiorespiratory levels during NREM and REM sleep. These characteristics have been exploited for the development of ambulatory systems for sleep monitoring. The reason for this is that cardiac and respiratory information can be extracted from the Electrocardiogram (ECG),Footnote 4 which can be easily recorded using wearable and unobtrusive technology. This is exactly the focus of this chapter; therefore, an overview of these characteristics or physiological changes during sleep stages is presented next.
1.1.1 NREM Sleep
It is very well-known that during NREM sleep, the PNS activity dominates over the SNS [104]. Compared to wake, the breathing frequency increases, though the variability is reduced. This is accompanied by a reduction in tidal volume,Footnote 5 resulting in a breathing which is more shallow and rapid [57]. Between different NREM stages, there is no significant difference in tidal volume and breathing frequency; however, respiration becomes more regular during deep sleep compared to light sleep [57].
Due to the high activity of the PNS during NREM, bradycardia emerges and the heart rate reaches a minimum during N3 [104, 153]. Additionally, heart rate variability (HRV) is lower during N3 compared to REM and wake, and regular oscillations can be observed during N3. These oscillations are associated with respiratory sinus arrhythmia (RSA), which is the modulation of the heart rate (HR) with respiration. Spectral analysis of the tachogram during NREM reveals a decrease in the low-frequency (LF) band (0.04-0.15 Hz) and an increase in the high-frequency (HF) band (0.15–0.4 Hz) of the HRV [165].
1.1.2 REM Sleep
REM sleep is characterized by muscle atonia, increased physiological activity, and the act of dreaming. During this sleep stage, the PNS is more active compared to the wake. Nevertheless, phasic fluctuations in SNS and PNS activity occur during REM sleep. As such, important distinctions exist between tonic and phasic REM sleep epochs [114]. During tonic REM, the SNS activity drops even below NREM levels, while during phasic REM, the SNS becomes very active and variable [104]. Characteristic rapid eye movements are also only present during phasic periods.
On a respiratory level, both tonic and phasic REM exhibit a decrease in ventilation due to a reduction in ventilatory drive. In general, the respiratory system becomes unstable as the depth of breathing becomes highly variable [57].
A general increase in cardiovascular instability is an important feature of REM sleep. During tonic REM sleep, there is marked bradycardia and hypotension, resulting in a decrease in HR and blood pressure (BP) even below levels of NREM sleep. On the other hand, phasic REM sleep epochs are characterized by great transient increases in HR and BP, produced by a phasic increase in the SNS [20].
These phasic fluctuations during REM sleep result in the instability of cardiovascular and respiratory parameters. Therefore, REM sleep epochs can exhibit a great variety in cardiac and respiratory characteristics among each other. As a consequence, the detection of REM sleep epochs presents a more challenging task for automated sleep scoring algorithms compared to deep sleep.
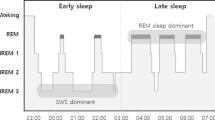
1.2 Sleep Architecture
For healthy persons, a normal night of sleep consists of five to six cycles, where REM and NREM phases are alternated with occasional awakenings. A hypnogram is the visualization of a person’s sleep architecture over time. The hypnogram of a healthy adult is depicted in Fig. 8.1a. One cycle typically lasts for 90–110 min. An initial wake period is followed by light sleep, where a person transients from N1 to N2. Thereafter, deep N3 sleep is reached. The cycle is terminated with a phase of REM sleep. In this fashion, NREM and REM alternate throughout the night,; however, their relative distribution changes. The duration of NREM sleep decreases and is compensated by an increase in REM sleep. Within NREM sleep, the portion of N3 will drop, though replaced by lighter N2 sleep. During final cycles, N3 may not even occur. The average distribution of different sleep stages throughout the night is given in Table 8.1. A longer sleep time will lead to an increase in REM sleep. The effect of aging will lead to a decrease in total sleep time as awakenings will occur more often. In patients with obstructive sleep apnea (OSA), the amount of REM and N3 sleep will be heavily affected due to arousals, which result in fragmented sleep. A hypnogram of an adult with severe OSA is depicted in Fig. 8.1b.
2 Polysomnography at a Sleep Laboratory
The gold-standard test in sleep medicine is polysomnography (PSG). This test is typically carried out for one night at a sleep laboratory during which several physiological signals are measured while the subject is sleeping with the aim of evaluating one or more aspects of their sleep. Within the most common purposes of a PSG study, one can find the evaluation of sleep quality, the identification of sleep stages, sleep-wake activity, and the diagnosis of sleep disorders such as OSA.
It is still common clinical practice to evaluate the PSG by manual scoring of sleep stages and events (e.g., apneas) according to the AASM rules. By using multiple physiological and contextual signals recorded in a PSG, characteristic patterns can be identified, allowing to score these events. The most common signals recorded during a PSG test are listed below. In some cases, these signals can vary depending on the specific sleep laboratory.
EEG: This set of signals is mainly useful in the identification of sleep stages, and hence helps to determine arousals and the wakefulness of the patient. This is done by evaluating characteristic waves in different frequency domains: Delta (3 Hz or lower), Theta (3.5–7.5 Hz), Alpha (7.5–13 Hz), and Beta (14 Hz or greater). For example, Delta activity is observed during N3 sleep, Theta activity is characteristic of REM sleep, Alpha activity is used as a marker of relaxed wakefulness, and Beta activity is often observed during wakefulness and drowsiness.
EMG: In a PSG test, the EMG can be obtained from different locations such as the chin and the limbs. The measurement of chin EMG provides an indication of muscle tone, which is reduced with sleep onset and is very low during REM sleep [15], whereas limb EMG can help to identify periodic limb movements, which can be an additional cause of sleep disturbance [15].
EOG: The potential obtained in this signal provides an objective measurement of eye movement and is useful in the identification of REM sleep and the sleep onset. Sleep onset is characterized by slow and rolling eye movements with a symmetric onset and offset, whereas in REM sleep, sharp rapid eye movements can be observed which are more asymmetric with a fast onset and a slow offset [15].
ECG: At least 1 ECG lead (commonly lead II) is recorded during PSG. ECG signals are useful for the identification of cardiac comorbidities but can also provide information on disturbances of the heart rhythm caused by sleep-related disorders.
Audio: Recording sounds by using a microphone placed in the neck near the trachea can be used to detect snoring and other tracheal sounds [15]. Recording sound in the PSG room (e.g., the audio registration of the video), on the other hand, can be useful as additional information to verify the nature of arousals and other events.
Respiration: A direct measurement of airflow via a pneumotachograph is the gold-standard method to measure respiration and define apneas [62]. For this method, the use of a mask is necessary; therefore, it is only used in combination with therapeutic positive airway pressure (PAP) devices. In clinical practice, the combination of a nasal pressure sensor and an oronasal thermistor is the standard used for diagnostic PSGs. These measurements are more comfortable for the patient and provide an approximation of the airflow exchange. The end-tidal CO2 is also an interesting parameter, this is the concentration of CO2 at the end of an exhaled breath. Reliably measuring the end-tidal CO2 is, however, difficult. Therefore, transcutaneous CO2 measurements are often used.
Respiratory effort: This is commonly measured by belts around the abdomen and thorax using respiratory inductance plethysmography (RIP). These signals provide information related to the respiratory effort, and hence also play an important role when diagnosing breathing-related sleep disorders.
Oximetry: The standard measurement of the blood oxygen saturation (SpO2) during a PSG is done by means of an optical measurement in transmission mode. This is typically done with a sensor at the fingertip but can also be measured in alternative locations (e.g., earlobe). The SpO2 measurement has been defined as a mandatory signal for quantifying the apnea-hypopnea index (AHI) used to measure OSA severity [44] (together with respiration and EEG). This measurement is accompanied by a pulse photoplethysmography (PPG) signal, which also provides cardiac-related information such as HR.
Body position and behavioral observation: This provides additional diagnostic information, as some sleep disorders are influenced by the orientation during sleep [15]. Position can be monitored with sensors, but also by video recording, the latter being the most common in standard PSG.
The signals listed above are an important source of information that allows to obtain a complete picture of the person’s physiology during sleep. This facilitates the task of diagnosing and following up sleep-related conditions. Nevertheless, it has several disadvantages related to patient comfort, the test cost, and the availability of sleep laboratory beds. The rather obtrusive sensors that need to be attached to the patient, combined with the unusual sleep setting and possible sensor verification from the nursing staff, significantly reduce patient comfort during the night. This leads to a suboptimal setting when aiming to evaluate a typical night of sleep. In addition, the PSG procedure implies a high cost, not only because of the equipment required for the recording of the signals and the sleep laboratory installations, but also because of the need for the test to be supervised and annotated by trained personnel. This high cost causes a limited number of beds available for PSG studies when compared to the high prevalence of sleep-related disorders. These limitations have motivated the development of sleep monitoring systems for home monitoring, which will not only tackle these challenges but will also allow multiple night monitoring. Devices for home monitoring have the potential to enable a broader patient screening, early detection of sleep-related conditions, and a longer follow-up.
3 Wearables and Unobtrusive Technologies for Sleep Monitoring at Home
3.1 Out of Center (Home) Poly(somno)Graphy Devices
Extended home sleep monitoring can be done using PSG-like devices adapted in size to enable its use at home. These measure a reduced set of the most important physiological signals from a standard in-lab PSG and can be denominated “Out of Center” (OOC) PSG portable devices [44]. When no EEG is included for the correct measurement of sleep, the devices are classified as polygraphy (PG) rather than PSG.
Multiple of these are currently available in the market and can be classified according to the number of signals that are measured. An initial classification scheme based on this principle was proposed by the AASM in 1994 [40]. An updated AASM classification scheme was proposed by Collop et al. [44] in 2011, with the aim to better classify new emerging portable sleep monitoring devices. This classification is done based on measurements of Sleep, Cardiovascular, Oximetry, Position, Effort, and Respiratory (SCOPER) parameters. For a review on some of the OOC devices, the reader is referred to [44, 62].
An example of a PG OOC device is shown in Fig. 8.2. These devices allow to monitor some of the main PSG signals at the cost of a certain degree of discomfort for the patient, as most require strapping devices to the chest or head and even using a nasal cannula. This remaining discomfort can limit the monitoring time and affect the measurement.
The need for an even higher comfort than the one provided by PG OOC devices, lower cost, and longer monitoring time has led to the recent development of wearables and sensors placed around the patient. These sensors not only measure less signals than an in-lab PSG, but also measure these either in a less obtrusive way or by applying an indirect measurement of some of the physiological parameters. This has been accompanied by the development of application-specific algorithms based on robust signal processing and machine learning techniques, to monitor some of the main sleep disorders such as OSA.
3.2 Home Sleep Monitoring with Unobtrusive Sensors
With the advance and miniaturization of electronics over the last decades, more compact and less obtrusive devices have been developed. These have further enabled the monitoring of physiological signals in non-clinical settings in the form of wearables and sensors around the patient. Application-specific integrated circuits have played a crucial role in the electronics being used for ambulatory healthcare monitoring.
The main areas of wearables and unobtrusive technologies that are available for sleep-related monitoring in non-clinical settings (i.e., at home) with an increased comfort include the following: Actigraphy, portable EEG devices, portable ECG devices and patches, ballistocardiography (BCG) devices, radar-based monitoring, and capacitively coupled biopotentials. It is worth noting that these technologies vary in the accuracy of the target measurements and their relevance to specific sleep-related disorders. These bring different levels of increased comfort, while in some cases compromising the sensitivity to artefacts caused by motion, sensor positioning, and other uncontrolled factors typical in a home setting.
Although important work has been done in the evaluation of the usefulness of some of these technologies related to specific sleep monitoring purposes, additional validation is still required in order to assess the performance of these technologies on their own, or combined with others, and of application-specific algorithms that have been developed for these. An overview of the different wearable sensor technologies listed above is provided next.
3.2.1 Actigraphy
Actigraphy devices aim to measure the movement from the limbs and/or torso of the person during sleep. The measurement of movement has been identified as important in sleep-related conditions as it can provide information regarding the state of the person, which can be related to physiological changes [105]. In this way, different types of movements can be identified as normal or abnormal and can give information which, if correctly analyzed, can aid in specific diagnosis and sleep characterizations. Parameters that can be estimated from actigraphy measurements include sleep quality, latency, duration, efficiency, fragmentation, circadian rhythm, sleep-wake periods, and activity levels [105].
The AASM indicates in their guidelines that actigraphy is reliable in measuring sleep for healthy adults [120]. Nevertheless, these devices only allow to gather general sleep information, as detailed data of sleep-wake physiology are not included [27]. In addition, there are several limitations in different areas including sensor placement, the number of axes and sensors, sensitivity for wake periods [27, 105], data quantification modes, validation, and scoring algorithms. A more detailed description of these limitations is provided in [105], as well as an overview of the main contributors to actigraphy scoring algorithms.
The most common measurement of actigraphy is the use of a multi-axial accelerometer worn around the wrist (i.e., wrist actigraphy). Other locations that have been studied include the diaphragm, the chest, the leg/ankle, and the trunk [21, 79]. In addition, some smartphone applications use the information from the accelerometer included in the phone when the latter is placed on top of the mattress, but these are expected to be less accurate [27].
Examples of commercially available wrist-based actigraphy devices include the Apple Watch, Biostrap, Empatica, Fitbit, Garmin Vivosmart, Whoop, Xiaomi, Lark, and Sleep Tracker. Currently, there is a high number of actigraphy wrist-worn devices in the market [105, 140], most of which measure at least one additional physiological parameter, with PPG-based heart rate being the most common one. The main differentiators between actigraphy devices are as follows: (a) the availability of raw data for the development of new algorithms, (b) the type of scoring algorithm tackling a specific sleep-related condition, and (c) proper clinical validation against the PSG gold standard.
3.2.2 Portable EEG Devices
In contrast with actigraphy measurements, EEG can provide more physiological information. The challenge in portable EEG monitoring is that the unobtrusiveness of these devices is rather limited or implies a compromise in the type of EEG signals that can be acquired, depending on electrode positioning and electrode-tissue interface. Standard EEG monitoring at the PSG laboratory is performed with glued-on electrodes. Frontal, central, and occipital derivations are recorded. A full EEG with a complete “10–20” electrode set is barely performed in sleep labs. Nonetheless, the reduced electrode set that is used still implies discomfort to the patient and requires installation by trained personnel.
Because of the lower comfort of using a hat-like device at home during multiple nights, the difficulty for correct electrode placement, and considering the added value of monitoring EEG for sleep-related disorders, more compact devices have been designed. These devices aim to monitor a limited set of EEG data with a reduced discomfort for the patient. Some of these are available as individually glued electrodes [45] and collect one or two EEG channels together with other PSG signals, but still require training for a correct installation; these could be categorized as OOC PSG-like devices as described in Sect. 8.3.1.
Other more portable options include the use of headbands [2, 4,5,6, 9] which also record EEG signals from a subset of dry electrodes distributed in the band. Although these collect EEG, not all of them provide the raw data, as some focus on their functionality as a sleep tracker or “sleep coach”, with the purpose of providing feedback on the activities previous to sleep, guide respiration exercises, and emit tones in different frequencies, among other feedback mechanisms that aim to increase the quality of sleep.
Hardware implementations with even higher comfort have been studied by acquiring the EEG signals from around-ear [28, 50] and in-ear [69, 82, 113] electrodes. Some commercial products include these implementations with purposes of productivity increase [172] or as an application-independent platform [107]. Ear EEG has even been tested for sleep monitoring purposes. Results indicate that the automatic sleep scoring using these sensors can reach an accuracy close to that achieved by manual scoring of scalp EEG [113].
3.2.3 Portable ECG Devices and Patches
Portable ECG monitoring has seen a big advancement in the last decade. Holter monitors that allow to record up to a 12-lead ECG have become smaller, and hence these could be used as part of a solution to perform sleep monitoring at home. Similarly, small form-factor PG devices currently offer the capability of monitoring multiple ECG leads. The main disadvantage in comfort that a Holter or PG device implies relies on the use of wires connecting individual contact electrodes with the recorder unit. To overcome this, miniature ECG recorders have been developed in the form of a chest patch. These allow to conveniently monitor one lead (or few leads) without the discomfort of using cables by using a relatively small patch as the one shown in Fig. 8.3. This type of patch can be worn for up to 1 or 2 weeks and enable a more comfortable way of ECG monitoring, which could be of added value for home sleep monitoring. Within the available ECG patches in the market, one can find the MCOT [75] from Biotelemetry inc., Zio XT [157] from iRythm, and an investigational device from VivaLNK [152], among others.
As an alternative to ECG patches, there are also solutions based on tight chest bands and t-shirts that use dry electrodes, which could also be a source of ECG during a night of sleep monitoring.
These signals also have the potential to be a source of respiratory activity by computing the ECG-derived respiration (EDR), when aiming to perform home sleep monitoring with a reduced subset of signals.
3.2.4 Optical Pulse Monitoring: PPG and SpO2
Another way of measuring cardiac activity is by means of an optical pulse readout using PPG in either transmission or reflection mode. This allows to obtain the pulse information, hence providing a source of heart rate monitoring. In addition, given an adequate location of the sensor, the use of the correct wavelengths, and dedicated algorithms, SpO2 can also be monitored.
Besides the standard finger-based PPG/SpO2 monitors, wearables monitoring PPG generally have the form factor of a smartwatch or smart bracelet with an optical readout in the back. There are currently multiple commercial offerings of smartwatches that monitor PPG, including brands such as Fitbit, Apple, Huawei, Samsung, Garmin, and Polar among others. Some of these have lately added SpO2 functionality to their offering and are even seeking FDA approval. This addition could play an important role in home monitoring of sleep-related conditions such as OSA. A review of developments and challenges of wearable PPG is provided in [32]. Other investigational devices available in the market that measure PPG signals include small wearable units such as the ones offered by Byteflies [3], which also offer units that can be used for ECG monitoring in the form of a patch.
Compared to ECG signals, PPG signals have a less sharp characteristic and may be more challenging to process when trying to obtain accurate beat-to-beat HR and HRV metrics, but these have the advantage of potentially enabling SpO2 measurements, which is of added value in sleep-related conditions.
3.2.5 Ballistocardiography and Pressure-Based Devices
Another way to obtain cardiac data is via BCG, which aims to monitor small movements or changes in pressure at the body surface (e.g., chest, back, ...) with the aim of deriving HR and even trying to obtain beat-to-beat HR and HRV. The same principle can be used to monitor respiratory activity, as this causes a change in pressure of the torso in the bed, for the case of sleep monitoring.
The advantage of being able to obtain respiratory and cardiac-related signals from one type of sensor has led to multiple companies offering pressure-based sleep monitoring solutions. The company Beddit (now bought by Apple) offers a piezoelectric-based sensor [1] that monitors average HR, average breathing rate, and snoring sounds (recorded via the microphone of the connected smartphone) and provides metrics of sleep time, bedtime, time to fall asleep, time away from the bed, wake-up time, and sleep efficiency. Similarly, Withings offers a sleep tracking mat [170] to be placed under the mattress, which detects snoring, performs heart rate and respiration rate tracking, and provides a sleep quality assessment within a coaching program. The company mentions it can also help identify signs of OSA. Another mat-based solution is offered by Emfit, with a sensor also placed below the mattress that aims to measure HRV, respiratory activity, and respiratory effort [59]. This sensor is shown in Fig. 8.4.
BCG setups for heart activity and pressure-based respiratory activity have thus the advantage of not requiring direct contact with the body. Nevertheless, the extracted heart activity tends to be less accurate than that of an ECG signal (and even of PPG signal) due to the motion-based measurement, as opposed to the electrical or optical-based measurements of the ECG and PPG. In addition, motion during sleeping can distort the measurements, and patients with high BMI are likely to cause sensor saturation [72]. The question of whether these unobtrusive signals can be used for monitoring specific sleep-related conditions needs to be answered with real-life validation studies.
3.2.6 Radar-Based Monitoring
A different technology that also aims to monitor the chest movement to extract respiratory and cardiac activity is the use of radar signals. This technology sends radiofrequency waves that are reflected in the person’s skin. The phase of the signal is modulated by the physiological movement, generating a phase difference between the emitted and received signals, which is then used to calculate the distance changes. The waves are mainly pointed to the chest or the back of the torso. Electromagnetic signals of different frequencies have been used for this purpose, with higher frequency and power resulting in higher sensitivity to small displacements [123]. Carrier frequencies between hundreds of MHz up to more than 200 GHz have been used [92]. More details on the use of radar signals for vital signs monitoring can be found in the work of Kranjec et al. [86], Li et al. [92], and Mercuri et al. [111].
Radar technology has been demonstrated to be able to monitor respiratory and cardiac activity [91, 123, 128]. It has the advantage of monitoring through non-metallic obstacles [86] placed relatively far from the subject. Nevertheless, it is commonly affected by motion artefacts [92], and the acquisition of beat-to-beat HR is more challenging than when using an ECG signal.
Some radar-based solutions are available commercially, including the S+ device by ResMed [135], which monitors breathing and movement, and provides a sleep report based on these measurements. The device has not been tested for the monitoring of specific sleep-related conditions at the moment of writing this chapter, but it is mentioned that it monitors the sleep stages to create a personalized sleep chart. Similar radar-based devices have been tested with promising results regarding sleep stage classification [41].
3.2.7 Capacitively Coupled Biopotentials: ECG and Bioimpedance-Based Respiratory Activity
Considering the discomfort of using contact electrodes to monitor biopotentials (e.g., ECG), the capacitively coupled acquisition of these signals is a technology that has gained interest. The main physiological signals that could be useful in a sleep monitoring setting and can be acquired in a capacitively coupled manner include the capacitively coupled ECG (ccECG) and capacitively coupled bioimpedance (ccBIOZ) for respiration monitoring.
These measurements are done by replacing the skin-electrode galvanic contact with capacitive coupling, hence enabling monitoring through clothing and bedsheets. In this coupling, the skin forms one “plate” of the capacitor, a conductive surface forms the second “plate” of the capacitor, and any non-conductive materials between these conductive surfaces form the dielectric. This completes the standard structure of a capacitor, and hence the connection from the acquisition circuit to the skin is replaced from a galvanic connection to capacitive coupling. An illustration of a capacitively coupled electrode interface is shown in Fig. 8.5.
ccECG acquisition has been explored since 1967 [137], but it is only in the last few decades that it has been more widely explored for a broad number of applications. These applications include sensors placed in the bathroom seat [19, 83, 97], in a wheelchair [129], in a car seat [38, 90, 106, 149], in an airplane sea [146, 147], in an office chair [13, 18, 94, 108], and in a bed [76, 95, 166, 171]. In the field of sleep monitoring, bed implementations have been tested during multiple hours [89, 95, 162], including comparison against polysomnography signals with reported HR coverages of up to 98% [89]. An initial evaluation toward the extraction of features that could be used in the identification of sleep apnea epochs was also done [34].
In the case of ccECG, the signal can be acquired using at least one pair of electrodes, typically accompanied by a third electrode for active noise canceling, denominated driven right leg (DRL). On the other hand, the acquisition of ccBIOZ requires 4 electrodes to perform a “4-point measurement”, in which 2 electrodes are used to inject a known amount of high-frequency current through the body, while the remaining 2 electrodes perform a voltage readout. The 4-point measurement has the advantage that the injected current does not flow through the same electrodes used for voltage sensing, hence the impedances at the electrode-tissue interfaces are not included in the measurement.
The acquisition of ccBIOZ has been less studied than the acquisition of ccECG signals. Within the reported research in this field, Abad [11] explored in 2009 the use of contactless BIOZ for bioimpedance spectroscopy (BIS) purposes. In this work, he demonstrated that commercial BIOZ devices are unsuitable for contactless measurements and proposed a multi-frequency current source to be used in ccBIOZ BIS measurements. With the purpose of measuring both ventilation and HR values, Macias et al. [103] reported a ccBIOZ system integrated into a car seat. Here, a 4-point measurement was implemented using textile electrodes on the back of the seat and in the steering wheel (measurements were in galvanic contact at the steering wheel point). Although both cardiac and respiratory activities were acquired under controlled conditions, it was concluded that the system did not achieve acceptable performance due to the capacitive behavior of the electrode-tissue interface. A more recent system integrating both ccECG and ccBIOZ [37] was demonstrated to successfully acquire these signals in prototypes in the form factor of a car seat and a bed mattress. In addition, the system was shown to be able to provide a flexible interconnection that enables the real-time selection of up to 8 simultaneous ccECG electrodes (i.e., 4 ccECG channels) from an array of up to 64 electrodes, as a solution for the varying quality of the ccECG depending on user position. The prototypes presented in [37] are shown in Fig. 8.6 as an example of the possible implementations of ccECG and ccBIOZ measurements. It is worth noting that in the specific case of a mattress with the sensors, the mattress can be covered by normal bed linen and the patient can wear standard pyjamas, which significantly increases the comfort when compared to contact-based methods.

Replicated from [37] with permission from the authors
Example of prototypes acquiring ccECG and ccBIOZ measurements simultaneously. a For sleep monitoring (covered by a normal bedsheet when in use). b For driver monitoring.
Such a multi-electrode approach, together with quality-based signal processing algorithms [33, 34] and optimizations in the electronic design [35, 36, 96, 155], aims to overcome the main challenges of capacitively coupled signals: the sensitivity to motion related to the varying electrode coupling for different positions or body shapes [17, 46, 167, 175] and the variability of signal quality depending on the electrostatic charges in the surroundings of the patient [46].
Although ccECG and ccBIOZ signals are likely to provide less coverage (in terms of time with high signal quality) than their contact-based counterparts, signal processing and system optimization approaches such as the ones mentioned above are expected to enable the use of the technology for home monitoring during extended periods of time without a compromise in the patient comfort. This is of added value when considering the more realistic scenario of monitoring at home and the increased analysis that an unobtrusive monitoring during multiple nights can allow.
3.2.8 Multiparametric Devices Dedicated for Sleep Monitoring
Taking advantage of the patch form factor used in some of the latest ECG monitors as well as other form factors enabled by miniaturized electronics, devices are now available which aim to combine some of the sensors/techniques mentioned above. This subsection aims to give a brief overview of the less obtrusive devices currently available in the market or being developed, which are specifically tailored for sleep monitoring at home and are significantly different than the PSG-like and PG OOC devices.
The company Beddr offers a small form-factor device called SleepTuner [23] to be placed in the forehead, which monitors actigraphy via a 3-axis accelerometer and uses optical sensors to monitor PPG (including PPG-derived HR) and SpO2. Based on these sensors, the company’s software performs sleep-related analysis which includes sleep duration, position, and stopped breathing events. Another patch-based solution is offered by the company Tatch [10], which aims to monitor respiratory effort, flow, oxygen level, heart rate, body position/movement, and snoring sounds. The company Onera [7] is currently developing a patch-based solution together with data analytics to enable the “first at-home medical grade sleep diagnostic patch system”.
The WatchPAT devices offered by Cardio Sleep Solutions [151] allow to monitor actigraphy, SpO2, chest motion, HR, body position, snoring, and peripheral arterial tonometry (PAT), which have been demonstrated to be adequate for the detection of sleep apnea [44]. Other solutions focus solely on the use of applications from smartphones [8, 136]; these mainly aim to quantify the quality of sleep or provide an early assessment of risk for sleep-related disorders such as OSA without directly monitoring physiological signals.
4 Machine Learning Algorithms for Sleep Staging at Home
Sleep scoring standards are developed mainly based on EEG signals. The current EEG sensor technologies, however, pose a certain level of obtrusiveness. This has motivated the search for alternative sensors and signals, which allow reliable and comfortable monitoring of sleep physiology. As a consequence, the development of novel algorithms for automated sleep staging based on these unobtrusive signals has been an active topic of research. As described in Sect. 8.3, cardiac and respiratory signals can indeed be more comfortably acquired by emerging unobtrusive sensor technologies compared to EEG-based monitoring. Therefore, sleep staging based on cardiac and respiratory signals presents the first leap toward home-based sleep monitoring. These sleep staging approaches are discussed in the following sections. First, the focus is on state-of-the-art algorithms, based mainly on ECG and/or RIP signals extracted from the PSG. Next, an overview of sleep staging algorithms based on data from wearable or unobtrusive sensor technologies is given with special attention to stand-alone actigraphy, BCG, and PPG. Finally, an outlook on the signal processing challenges commonly encountered when working with wearable data and future research in sleep staging is presented.
Algorithms are compared based on the performance of a 3-class classification task of Wake versus NREM versus REM (WNR). Nevertheless, many studies report a 2-class sleep staging performance, generally being sleep versus Wake. However, different ways exist of combining sleep stages, as Wake and REM share some characteristics and one could define “active sleep” (Wake, REM, N1) versus “quiet sleep” (N2 and N3) [98]). As REM is, therefore, difficult to classify, a 3-class WNR is preferred for better comparison. Studies in which a 4-class classification task reached superior performance to 3-class classification are also discussed. Typically, this classification task is defined as Wake versus REM versus Light sleep versus Deep sleep (WRLD).
Furthermore, the discussed studies and algorithms have been trained subject independent unless mentioned otherwise. This implies that the training data set does not contain data from subjects which have been included in testing. The studies also report performances by at least an average accuracy and Cohen’s kappa \(\kappa \) score [43]. As such, algorithmic performances can be compared by equal measures. The average accuracy is the percentage of epochs correctly classified compared to the gold-standard annotations. The \(\kappa \) score is a measure of agreement that corrects for the level of agreement achieved by chance.
4.1 State-of-the-art Algorithms Based on Cardiac and Respiratory Signals
As PSG provides the gold standard for sleep staging, cardiac and respiratory-based sleep staging algorithms have been developed based on these PSG-derived signals. It allows direct comparison of all PSG signals without synchronization issues. Sleep stage annotations are directly applicable and high-quality data is assured, thus enabling state-of-the-art performances. In general, sleep staging algorithms are built from a feature extraction phase followed by a classification phase. A multitude of cardiac and respiratory features have been developed in the literature, typically modeling the ANS variation in the temporal and spectral space.
For a long time, algorithms reaching state-of-the-art performance used a combination of signals as input. For instance, Harper et al. showed in 1987 that classification performance can improve when combining modalities [71]. Some earlier studies explored sleep staging based on single modalities, such as ECG [173] or RIP [101], with the advantage of requiring less sensors. However, until 2018, performances of these studies were indeed inferior compared to co-occurring studies with multimodal input.
Therefore, these studies published before 2018 and based on a single modality are not mentioned in this chapter. Although, a complete review on automated sleep stage scoring was made by Faust et al. [61]. An overview of discussed papers which reached state-of-the-art performance is found in Table 8.2.
In 2006, Redmond and Heneghan tackled the challenging task of sleep staging based on cardiac and respiratory signals [134]. This was achieved by extraction of temporal and spectral features of the ECG RR-interval (time elapsed between two successive R-waves) and of the respiratory effort signal in standard 30 s epochs.
Furthermore, EDR features and spectral features from the cross-spectrum of the RR and EDR were calculated. As such, the feature set consisted of the power in the LF and HF band of the RR-interval, the EDR, the RR-EDR cross-spectrum, and the respiratory effort signals. Other features were the LF/HF power ratio of RR, mean RR, standard deviation of RR, difference between the longest and shortest RR-interval in the epoch, breath-by-breath correlation, and breath length variation. These features served as inspiration for subsequent studies. The accuracy and \(\kappa \) score of the subject-independent algorithm were, respectively, 67% and 0.32 for a 3-class WNR sleep staging task on healthy subjects. The authors improved the algorithm’s performance by a linear discriminant classifier model using a time-dependent a priori probability. The accuracy and \(\kappa \) score then reached 76% and 0.46, respectively [133].
Willemen et al. improved sleep staging performance in 2014 by the combination of ECG, RIP, and actigraphy [168]. The study was performed on 36 healthy subjects and a total of 85 nights. A set of 13 feature groups was defined for an ECG, respiratory 1 Hz movement signal, extracted per epoch of 60 s. By transformations, a total of 750 features was obtained and subsequently reduced to 40 task-specific features by forward feature selection. These one-minute epochs were applied for classification, which is different from other studies that commonly classify sleep per 30 s epochs. This one-minute window accounts for the slow dynamics of the breathing rate and heart rate variability, as the HRV Task Force recommends interval lengths of at least 10 times the wavelength of the lowest frequency bound [30]. However, 60 s would only be a reliable choice for the HF band and too short to be fully reliable in the LF band. To validate the classified epochs, the 30 s epochs of the PSGs hypnogram were transformed to 60 s interval values by a set of decision rules. One RBF-kernel support vector machine (SVM) was optimized for different binary classification tasks. Three-class sleep staging of WNR achieved a mean accuracy and kappa of 81% and 0.62, respectively. It is noted that the study population’s average age was relatively low: 22.1 ± 3.2 years. Similar results were obtained by Domingues et al., who performed a similar study [56].
Willemen et al. also developed a sleep staging algorithm for OSA patients [169], in which RR interbeat interval (IBI) series, the breathing signal, inter breath interval series, and the inspiration-to-expiration ratio interval series were extracted from the ECG and respiratory belt signals for 25 subjects. Sixteen feature groups were extracted from these signals in 60 s epochs. This window length was found to achieve the best results to distinguish apneic from healthy breathing in a study by de Chazal et al. [39]. By detrending the first input time series over different intervals and afterward transforming extracted features, a total of 510 features was defined. A triple layer validation scheme was constructed to train the classifier parameters, perform feature selection ,and define a test set. The study obtained an accuracy and \(\kappa \) score of, respectively, 70% and 0.41 for WNR classification of OSA patients.
Fonseca et al. compared three of their developed sleep staging methods based on conditional random fields (CRF), hidden Markov models (HMMs), and Bayesian linear discriminants (LDs) [64]. Features were extracted using windows centered on non-overlapping epochs of 30 s, where the window length depended on the feature type. Additionally, they explored the incorporation of time information in their classifiers and applied their methods on 102 healthy subjects as well as 102 patients with OSA. In general, the best performing classifier was a CRF boosted with time information (CRFt). Although, CRFt performed not significantly better than standard CRF in the case of OSA patients. This can be subscribed to the fact that OSA leads to the decrease of REM and N3 presence and an increase in sleep fragmentation due to arousals associated with respiratory events (i.e., apneas) [139]. Therefore, the presence and progression of their sleep stages might depend more on the occurrence of disordered breathing events than on a healthy sleep architecture. Three-class sleep staging of WNR achieved a mean accuracy and \(\kappa \) of, respectively, 81.8% and 0.59 for healthy subjects compared to 77% and 0.50 for OSA patients. On a healthy data set, the developed CRFt algorithm performs comparable to [168], both for WNR and WLRD classification tasks. With respect to OSA patients, Fonseca et al. reached a substantial improvement in performance compared to [168], in which an accuracy and \(\kappa \) of 70% and 0.41, respectively, was reported. Moreover, the study of Fonseca et al. included only two out of three modalities, which can be seen as an advantage for long-term home monitoring.
In 2018, Li et al. developed a sleep staging algorithm based on a single lead ECG signal from extensive public data sets [93]. They were able to surpass state-of-the-art algorithms using a single modality, however, by extraction of respiratory information from the ECG. First, the authors derived spectrograms of the cardiorespiratory coupling in 5 min windows centered on each 30 s epoch. They applied convolutional neural networks (CNN) on the spectrograms for subsequent feature extraction (i.e., representation learning). Then, the extracted features were combined with handcrafted ECG features into an SVM model. With an accuracy and \(\kappa \) of 81.6% and 0.63 for WNR classification, this model is competitive to [64, 168], albeit with the application of a single modality.
The current state-of-the-art sleep staging model is described by Radha et al. [131], applying exclusively a single lead ECG signal as an input. A set of 132 handcrafted HRV features was fed into an Long Short-Term Memory (LSTM) network. This feature set consisted of time- and frequency-domain features, entropy and regularity features, and miscellaneous features. To extract the feature vector of a 30 s epoch, a window of 4.5 minutes of IBI data centered around this epoch was considered. The LSTM network type is chosen for its ability to capture long-term temporal dependencies. To determine the optimal number of LSTM layers and cells per layer, 18 combinations were trained and compared. The final model consisted of 2.6 \(\cdot \) \(10^5\) parameters. This potentially involves a substantial time complexity; however, the study does not mention training time and memory consumption. The model was validated on 195 healthy subjects and 51 OSA patients. The algorithm reached an accuracy and \(\kappa \) of 76.5% and 0.63 on the former and 78.5% and 0.60 on the latter for a 4-class WRLD classification task. Interestingly, authors observed a negative correlation between performance and age, presumably by changes in autonomic function [177] and alteration in sleep architecture [148].
4.2 Sleep Staging Approaches Based on Wearable and Unobtrusive Sensor Technologies
The sleep staging algorithms described in the previous section report state-of-the-art performances, yet these were developed on PSG data. In order to monitor patients at home, different wearable or unobtrusive sensor technologies were implemented as described in Sect. 8.3. Among these, actigraphy, BCG, and PPG have played a more important role in sleep staging research and specific algorithms have been developed.
As actigraphy is purely motion based, it is not suitable for refined sleep monitoring. Nevertheless, it presents an established method for sleep/wake classification. These studies are discussed in Sect. 8.4.2.1 and summarized in Table 8.3. On the contrary, BCG enables the recording of multiple physiological signals: cardiac, respiratory, and movement information. This modality has been explored for sleep staging by several studies, which are described in Sect. 8.4.2.2. Furthermore, PPG has gained interest in sleep research as the classic finger-based recording shifted to a smartwatch configuration. Studies applying PPG in sleep staging are discussed in Sect. 8.4.2.3. Table 8.4 gives an overview of discussed papers on sleep staging approaches based on BCG and PPG. Other suitable modalities for wearable or unobtrusive sleep staging such as arterial blood pressure, peripheral arterial tonometry, oximetry, audio, video, and temperature are discussed in [138]. Furthermore, radar technology for sleep staging in OSA has been explored by [47].
4.2.1 Actigraphy
Actigraphy or activity-based sleep tracking is a reliable and valid methodology for monitoring sleep-wake and circadian rhythm patterns in healthy adults [99]. The sleep staging capacity of actigraphy is limited as it is known to overestimate sleep time. This is because it cannot differentiate motionless periods of wakefulness from sleep. On the other hand, it presents a potential tool for the unobtrusive screening of certain sleeping disorders. However, the technology is not able to diagnose sleep disorders that involve altered motility during sleep such as OSA [126, 142], and performance will be impacted by disorders altering the ANS [66]. Therefore, actigraphy is usually combined with cardiac and respiratory signals [55, 56, 168]. Devot et al. compared sleep staging using cardiac, respiratory, and actigraphy signals to sleep staging based solely on actigraphy. As expected, they obtained superior results with the former approach [55]. In order to minimize obtrusive sensors while preserving classification performance, Long et al. retained the respiratory signal in combination with actigraphy [100] and achieved comparable results as Devot et al. In [63], a surrogate actigraphy signal was estimated from body motion artefacts derived from the ECG and respiratory effort signals. The surrogate signal was combined with RIP or ECG+RIP in a sleep-wake classifier. This approach achieved similar results as classification in combination with the reference actigraphy signal, both in a healthy as mixed population including insomniacs. The authors concluded that in setups where RIP is the only modality, as it is one of the most applied modalities in home sleep monitoring, actigraphy posed a significant added value. In case both RIP and ECG are acquired, the application of actigraphy is redundant.
4.2.2 Ballistocardiography
The following studies have applied a BCG-based bed sensor for sleep staging. Kortelainen et al. used commercial Emfit material to configure a BCG system [85]. From the acquired signal, they extracted the IBI and movement activity. IBI features trained a hidden Markov Model for a WNR task, while the motion signal served as an additional input for wake stage detection. Nine healthy subjects were included in the study, of which in total 18 sleep recordings were acquired. The three-class WNR classification task resulted in an accuracy and \(\kappa \) of 79% and 0.44, respectively. It is noted, however, that the training and test set contain recordings from the same subjects as a leave-one-out cross-validation (LOOCV) was performed on these 18 recordings. This approach could lead to an overestimation of the subject-independent classification performance.
In the same year, 2010, a similar study by Migliorini et al. was published [112]. Seventeen recordings from 11 healthy subjects were acquired, using the commercial Emfit sensor material as well. Similarly, a LOOCV was performed for parameter optimization. The achieved accuracy score was comparable to [85]; however, a higher \(\kappa \) of 0.55 was reached. As opposed to Kortelainen et al., the authors included features from the respiratory component, which is inherently present in the BCG signal.
Kurihara and Watanabe implemented a pneumatic system based on an air tube and pressure sensor to acquire the BCG. They obtained similar sleep stage performances as Kortelainen et al. using a comparable data set [87].
In 2016, Hwang et al. used a polyvinylidene fluoride sensor for sleep staging in 12 healthy and 13 OSA patients [73]. The motion signal was applied for wake detection, while information extracted from the respiratory signal was investigated for REM and deep sleep (N3). The 4-class classification had an average accuracy of 70.9% and \(\kappa \) of 0.48, where no significant difference was found between the control and OSA populations. Comparing to a later study of Fonseca et al. [64] in 2018, who also applied a WRLD classification on OSA patients, the current method reached similar performance, though by the application of an unobtrusive device.
4.2.3 Pulse Photoplethysmography
Studies on wearable PPG sleep staging can be traced back to 2017. Beattie et al. [22] from Fitbit research performed sleep staging in 60 healthy subjects based on a wrist-worn device, measuring three-dimensional accelerometry and PPG. The interval between peaks of the PPG wave was taken as a surrogate for an ECG-derived IBI. As such, motion, breathing variability, and HRV could be extracted from this modality. However, the PPG signal is more sensitive to movement artefacts compared to ECG, especially when worn as wearable at the wrist. Similar to BCG research by [85], no IBI information could be extracted in periods of heavy motion. In the case of unlikely sleep architecture patterns, the authors applied a post-processing step by smoothing, e.g., an isolated wake epoch during a long period of deep sleep is converted to the annotation of its surrounding epochs. This assumption is only reasonable when monitoring healthy subjects. After LOOCV, the overall accuracy was 69% with a \(\kappa \) of 0.52 for a 4-class WRLD task.
A similar study was published in 2017 by Fonseca et al. [66]. Although, the study included a larger data set of 152 healthy subjects, from which a validation set was held out for testing. Features and machine learning techniques were similar to their earlier study [65] (later discussed in [64] and described in Sect. 8.4.1), with the exclusion of respiratory signals. The performance of the current study for both WNR and WRLD tasks was lower and could partially be subscribed to the reduced number of input signals. However, as the authors have pointed out themselves, a respiratory rate could technically be deduced from the PPG signal [88]. This is potentially beneficial, as it could provide features capturing changes in sympathetic tone, important for detection of REM [66].
Previous studies have performed sleep staging based on wearable PPG in a healthy population. However, sleep staging in a pathological population is essential as total sleep time is an important outcome for severity assessment, e.g., OSA. Uçar et al. [160] and Casal et al. [31] applied sleep-wake classification in an OSA population. As data processing becomes more challenging in a pathological population, non-wearable PPG signals were used in these studies. However, it offers the potential of integrating these algorithms with signals from wearable devices.
4.3 Signal Processing Challenges Presented by Wearable Systems
The signal processing of wearable data is associated with specific challenges. This includes sensitivity to motion and synchronization between the wearable device and PSG system.
First, the presence of motion is ambiguous. On the one hand, movement induces excessive noise in the overall BCG signal, which impedes the IBI extraction and HRV analysis. On the other hand, it provides valuable information on the patient’s sleep architecture, similar to actigraphy. Heavy motion can mainly be subscribed to wake stages and thereby it compensates for the loss of information regarding HRV. Moreover, the separation between wake and REM is improved by the inclusion of motility information, as the cardiac activity presents similar characteristics during both stages [85].
Furthermore, synchronization between wearable and standard devices is beneficial as it enables quality control of the wearable signal. Comparison of the HR or respiration rate extracted from both devices can act as a quality indicator. Synchronized signals allow direct comparison of predicted and ground truth hypnograms as well.
The synchronization procedure is usually achieved by alignment of tachograms, derived from the heartbeats detected in the wearable and from the R-peaks detected in the ECG signal from the standard device [22, 66]. However, in case of heavy motion due to restlessness or sleep disorders (such as OSA), the tachogram is hard to derive and thereby troubling synchronization. In [72], a method for synchronization of BCG recordings of OSA patients was proposed, based on artefacts rather than IBI. First, artefacts were detected in the BCG recordings without training the algorithm on artefact annotations. Then, a segment including several subsequent artefacts defined the artefact template. Next, a corresponding data pattern was sought in the thoracic belt of the PSG to align the segments. Figure 8.7 displays a notable artefact pattern found in the BCG signal, which can be linked to a corresponding pattern in the thoracic belt.
Furthermore, it is noted that the equivalence of tachograms derived from the ECG and the PPG or BCG device is only valid in the absence of cardiovascular health problems. For instance, ectopic beats during arrhythmia can be traced by the ECG. In some cases, these beats do not affect the pumping mechanism of the heart. Therefore, these ectopics are sometimes not acquired by the BCG or PPG [66, 85].
4.4 Future Research in Sleep Staging at Home
On a future prospect, cardiac and respiratory-based sleep staging will be explored by deep learning networks, as intended by [131]. Currently, deep learning-based algorithms are more actively developed within the field of EEG-based sleep staging [122, 156, 159]. This entails an algorithmic pipeline where both feature extraction and classification are optimized by extensive neural networks. The advantage is the automated training procedure of the complete pipeline and often superior classification performances. However, one of the requirements to properly develop these algorithms is the availability of large amounts of data. In the field of EEG-based signal processing, data is often provided by the publicly available Physionet Sleep-EDF database [68, 81]. Additionally, it contains EOG, EMG, oronasal respiration signals, and body temperature. Equivalently, the availability of a large data set containing ECG, respiration, and sleep stage scoring could benefit the development of these cardiac and respiratory-based algorithms. This would, moreover, allow benchmarking of algorithms, which is currently difficult due to the variety in data sets.
Another potential issue is the suitability of these cardiac and respiratory-based sleep staging algorithms for real-time applications. At present, most studies focus on increasing sleep staging performance, which has a theoretical maximum defined by the inter-rater agreement of 82.6% for 5 sleep stages [141]. The developed algorithms often require several minutes or more of sleep data for pre- and post-processing or to include time information. Fewer studies investigate the suitability of algorithms or design them specifically for real-time applications. Real-time processing is, however, not necessary for the diagnosis of many sleep disorders, nor do these sleep disorders pose a threat that requires real-time monitoring. Considering the fact that offline monitoring is sufficient for these sleep disorders relaxes the constraints of newly developed wearable hardware as internal algorithmic processing is not a priority. In contrast, online monitoring is critical in the field of neonatal care. First, it serves to optimize the timing of nurse intervention so as to minimize the sleep disturbance of the neonate. This was achieved by sleep staging based on EEG monitoring, though presenting a non-wearable approach [16]. Second, online monitoring is required to generate alarms as motor responses often precede changes in vital signs, such as seizures and apneas. Movements could be real-time detected based on a BCG approach [77]. As unobtrusiveness and real-time sleep staging are crucial in this field, research in neonatal care could complement the field of sleep disorders and its advances in unobtrusive techniques and wearability.
The last challenge concerns the classic 30 s epoch length for annotation, analysis, and validation. This epoch length was optimized for EEG-based sleep analysis on paper [102]. At a paper speed of 10mm/s, one page meant a 30 s recording, which served well to visualize spindles and delta waves [51]. The 30 s epoch length was further recommended by the R&K manual [132]. The sleep stage annotation of such an EEG epoch is defined as the sleep stage which comprises the largest portion of this 30 s. This procedure is efficient for hand scoring and a reasonable approach for a healthy population, in which sleep stages have a certain stability and persist over several epochs [138, 145]. Nevertheless, half-minute epochs are less suited for a population with fragmented sleep (e.g., OSA), which is associated with short-term awakenings, arousals, and critical respiratory events. As such, classic sleep staging is less reliable in this population and they might benefit from a smaller time scale in sleep scoring and sleep analysis [145]. Additionally, the probability distribution of a short-term epoch over different sleep stages conveys more information than classical hypnograms, as proposed in [154]. Therefore, current sleep staging algorithms might not only require further validation and adaptation in a variety of age groups and disorders, but also a shift in valuing the gold standard.
5 Detection, Screening, and Phenotyping of Sleep Apnea in an Ambulatory Setting
Obstructive sleep apnea is the most common sleep-related breathing disorder, and it is estimated that worldwide almost 1 billion people are affected by this disorder [25]. However, most of these subjects remain undiagnosed, and consequently untreated. OSA patients experience repetitive complete or partial cessations of breathing during the night which are caused by a narrowing of the upper airway. In many countries, diagnosis of sleep apnea is currently based on manually scoring these events from an overnight in-hospital polysomnography. The AASM has defined a set of scoring rules which are considered as the gold standard for scoring OSA [26]. According to the AASM2012 rules, events are scored if they last longer than 10 s. An apnea is scored when an airflow amplitude decrease of more than 90% occurs, a hypopnea, on the other hand, only requires a decrease in airflow amplitude of at least 30%, but accompanied by either an oxygen desaturation of more than 3% or an arousal. The apnea-hypopnea index is computed as the number of apneas and hypopneas per hour of sleep. Subjects are diagnosed with OSA if they either have an AHI larger than 5 accompanied with symptoms, or if their AHI is larger than 15, independent of the presence of symptoms [143].
Many researchers have been developing methods for automated in-home screening and diagnosis of sleep apnea. In this section, an overview will be given of methods using signals that can be easily acquired in a home environment. The methods will be ordered according to the SCOPER system, which was introduced in Sect. 8.3.1. A short overview of the use of these five categories of sensors in the diagnosis of sleep apnea is given below:
-
1.
Sleep: A measurement of sleep, for example, using actigraphy, will enable the calculation of the hours of sleep; using this measure instead of the recording time leads to a better estimation of the AHI [120]. These methods were the topic of Sect. 8.4.
-
2.
Cardiovascular: This category includes ECG, PPG, and PAT as well as all other measures of the heart rate. Bradycardia can be observed during apneas, followed by tachycardia when breathing is retaken [70], as can be observed in Fig. 8.8. Moreover, these signals can be used to derive an estimate of respiration and detect autonomic arousals.
-
3.
Oximetry: The SpO2 signal is very useful for OSA screening, since apneas often result in an oxygen desaturation as can be seen from the example in Fig. 8.8.
-
4.
Position: Visual and non-visual measures (e.g., using an accelerometer combined with a gyroscope [80]) can determine the body position of a subject. Studies have shown that OSA severity can be position dependent. In fact, a higher AHI and more severe apneas have been observed during supine sleep [124]. Differentiating between lateral and supine sleep could thus help to improve automated OSA detection algorithms. No studies, however, propose to use position measurement on its own for the detection of OSA. Therefore, the analysis of position sensors will not be discussed further.
-
5.
Effort and Respiration: The reduction in airflow is the primary effect of apneas. Sensors measuring respiratory effort provide extra information which helps to differentiate between central and obstructive apneas.
An overview of current research and commercial devices for OSA detection categorized according to the SCOPER system can be found in [109]. In this review, sound recording devices were defined as the sixth category, in addition to sleep, cardiovascular, oximetry, position, effort, and respiratory parameters. In this section, the focus will be on the detection algorithms, rather than the wearable sensors, which were already discussed in Sect. 8.3.
Most OSA detection algorithms consist of four main steps: starting with the signal preprocessing phase, next feature extraction, feature selection, and finally classification. Two classification problems are studied: event-based or subject-based classification. In the case of event-based classification, the goal is to detect all apneic events within the recording, and this is often done by splitting the recording into 1 min windows. Based on the number of windows classified as apneic, the AHI can be estimated. Subject-based classification, on the other hand, extracts features over the whole recording which will then be correlated to the AHI and used to predict the OSA severity category of a patient. In this section, features commonly used for either one of those classification tasks in the framework of OSA detection will be discussed per SCOPER category. Additionally, studies describing automatically generated features using deep learning will be briefly discussed in Sect. 8.5.5.
5.1 Cardiovascular
5.1.1 ECG
The effects of apneic events on the ECG signal have been known since the 1980s [70, 116], but the research into sleep apnea screening using ECG signals really took a boost in 2000 with the Computers in Cardiology Challenge [115] and the subsequent release of the Physionet Apnea-ECG database [127]. This data set is still one of the most used data sets for ECG-based OSA screening. An extensive overview of ECG-based methods for OSA screening can be found in [60, 110]. The ECG-based screening approaches proposed in [110] obtain subject-based classification accuracies of 72–100% and an area under the curve (AUC) of 89–100%.
The used features are generally based either on changes in HR [70] or changes in respiration, captured using the EDR [116]. The respiration can be extracted from the ECG since ECG waveform characteristics are altered by respiratory-induced movements of the chest electrodes and changes in the electrical impedance of the thoracic cavity. The simplest measure of EDR is the amplitude of the R-waves, but many more elaborate methods have been proposed. A comparative study of 10 EDR algorithms is discussed in [164], where it was shown that the EDR signals computed from changes in the QRS slopes are most robust in the presence of artefacts, changing respiratory rates, and different ECG-recording systems.
OSA detection algorithms typically use statistical, frequency-domain, and nonlinear features extracted from both the HR and the EDR. Recently, measures of cardiovascular interactions have also been identified as relevant for OSA detection.
Statistical features: Different time-domain features of the RR-interval time seriesFootnote 6 and EDR have been proposed by De Chazal et al. [48] and are often used in the literature. An overview of these features can be found in Table 8.5.
Frequency-domain features: Multiple methods have been applied to extract frequency information from the heart rate, but the power spectral density and wavelet decomposition [29] are the most popular. Often the power in the standard HRV frequency bands is considered: very low-frequency range (0.003–0.04 Hz), low-frequency range (0.04–0.15 Hz), and the high-frequency range (0.15–0.4 Hz).
Nonlinear features: An overview of nonlinear parameters used on cardiorespiratory signals for sleep apnea detection is given in [165]. Analysis of the sample entropy of the HRV signal has shown a reduced complexity for apneic subjects compared to controls [12]. This can be linked to the cyclic pattern of bradycardia and tachycardia during apneas. Detrended fluctuation analysis has also been applied on the HRV of apneic subjects, but only slight changes in long-term control mechanisms of the heart rate could be observed [165].
Cardiorespiratory interactions: The HRV is modulated by respiration through the mechanisms called respiratory sinus arrhythmia. It has been observed that the information shared between respiration and HRV decreases during apneas and these reductions have been used as features to detect apneas [163]. An overview of different methods to estimate the RSA from the HRV and a respiratory measurement (e.g., the EDR or a respiratory belt) can be found in [118].
5.1.2 PPG
From the PPG signal, the pulse rate (PR) can be extracted as an alternative for the HR. All features proposed for the HR could, therefore, also be estimated from the PR. Moreover, decreases in the amplitude fluctuation of the PPG (DAP) have been linked to vasoconstriction due to sympathetic arousals at the end of apneas. The use of these DAP events has been studied for the detection of OSA in children [67]. Additionally, characteristics of the PPG waveform such as pulse amplitude, width, and slope transit time have been linked to respiration and their behavior can be useful for sleep apnea detection [53].
5.1.3 PAT
The peripheral arterial tonometry [144] sensor was developed for the detection of sleep apnea. It is based on a pulsatile plethysmography signal measured on the finger which can capture vasoconstriction and tachycardia related to apneas. Decreases in PAT amplitude of 33% in combination with a tachycardia of 15% were used in [144] for the detection of apneas.
5.1.4 Contactless Cardiovascular Measurements
Several contactless alternatives for ECG recording have been tested for sleep apnea detection. In [34], a multi-channel contactless capacitively coupled electrocardiography embedded in a mattress was proposed. The ECG-based apnea features defined in [163] were extracted from ccECG signals of healthy volunteers. The HR features achieved high similarity to the features extracted from the reference ECG signal. Signal morphology features, on the other hand, showed lower similarity with the reference resulting in problems with the EDR extraction. The similarity in HR features shows the potential of ccECG sensors for the detection of sleep apnea.
Ballistocardiography has also been studied in sleep apnea subjects. In [178], for instance, Zink et al. optimized the algorithm for BCG beat-to-beat detection in a sleep apnea population and obtained a correlation coefficient \(R^2\) of 0.95 between the beat-to-beat cycle lengths extracted from the BCG and ECG. Whereas Hwang et al. investigated the correlation between the oxygen desaturation index (ODI, see Sect. 8.5.2) and HR features extracted from three different BCG sensors [74].
Researchers have also focused on extracting heart rate from radar or infrared (IR) video recordings next to the breathing movements. Zhu et al. have validated IR-based heart rate monitoring in sleep apnea subjects and discussed the open challenges in this field [176].
5.2 Oximetry
The SpO2 signal has been widely studied for sleep apnea screening since it can easily be acquired in a home environment. In clinical practice, the SpO2 signal is often characterized by simple statistics such as the ODI, which counts the number of times a desaturation larger than 4% occurs per hour of sleep, or time spent below an oxygenation level of 90% (T90). It has been shown that these simple parameters can reliably confirm moderate to severe OSA, but that a negative test result does not rule out mild OSA [158]. Therefore, researchers have been developing a range of more elaborate SpO2 parameters in order to detect subtle changes due to apneas. In [158], four categories of commonly used SpO2 parameters were defined: desaturation characteristics, time series variables, frequency spectrum variables, and nonlinear variables.
Desaturation characteristics: The desaturation characteristics include the desaturation depth, duration, and area. These can be computed compared to a baseline level or another reference point. Additionally, these parameters can be calculated on subparts of the desaturation event, e.g., on the downward and upward part separately. Some studies also considered desaturation slopes or higher order derivatives of the signals [54]. In Fig. 8.9, an overview of these features is given for an example oxygen desaturation.
Time series analysis variables: These parameters include statistical measures that can be computed over the full SpO2 signal or window based. These statistics include the following: the mean, minimum, quantile values, standard deviation, higher order statistical moments, and cumulative time spent below certain SpO2 values (e.g., T90) [158].
Frequency spectrum variables: Studies have shown that OSA subjects have an unstable or overly sensitive respiratory control system [58]. Therefore, instead of going back to a stable breathing pattern after an apnea, often another apnea is triggered. As such, apneas tend to be grouped together, as can be seen from Fig. 8.10. When the apneas follow each other closely, a periodic pattern of desaturations can occur as is shown in the lower right plot of Fig. 8.10. Different studies have used the power in the 0.01–0.033 Hz frequency band to capture this periodicity [158]. Other measures of the PSD have been proposed, such as wavelets [117], autocorrelation analysis, or the use of phase rectified signal averaging (PRSA) [54].
Nonlinear analysis variables: The recurrent desaturations during the night also cause the SpO2 signals to have a higher irregularity, variability, and complexity. These can, respectively, be measured using the sample entropy, central tendency measure, and Lempel-Ziv complexity [14].
Terrill et al. concluded in their review [158] that the studies which obtained the best OSA detection results used features from multiple of these four categories. These categories thus contain complementary information. However, including more than three to four features in the classifier did not lead to a significant increase in performance. SpO2-based OSA screening methods typically obtain accuracies of 80–95% with an AUC of 90–95%, depending on the used features, data set, and AHI threshold [158].
5.3 Effort and Respiration
5.3.1 Airflow
The AASM rules for visuals scoring of apneic events rely mainly on the airflow measured using an oronasal thermal and nasal pressure sensor [26]. Therefore, several researchers have developed methods for the automatic detection of sleep apnea on these signals. All drops in peak signal amplitude of more than 90% are scored as apneas, whereas drops of more than 30% could represent a hypopnea. These drops are relative to pre-event baseline breathing which is defined as “the mean amplitude of stable breathing and oxygenation in the 2 min preceding onset of the event or the mean amplitude of the 3 largest breaths in the 2 min preceding onset of the event” [26]. This baseline can be difficult to define for subjects with high AHIs and its definition is ambiguous to be translated into algorithms. Moreover, breathing and movement artefacts will further complicate this baseline extraction for automated algorithms [42]. Therefore, Ciołek et al. proposed a robust airflow envelope tracking using nonlinear filters. Using this reliable baseline, rule-based methods can then be applied to detect apneas and hypopneas when a decrease in airflow amplitude larger than a predefined threshold is observed.
These rule-based methods, however, have as disadvantage that they cannot differentiate if hypopneas are associated with arousals or desaturations. Therefore, more elaborate respiratory features have been proposed in order to capture changes that might have a correlation with arousals or desaturations. Koley et al. proposed statistical features of the respiratory amplitudes and intervals over windows of 8 s [84]. Additionally, they extracted the area and length of the respiratory curve and frequency-domain features using the PSD. In this study, the deviation of each of the feature values from the subject’s mean values was also considered.
5.3.2 Respiratory Effort
Similar processing methods can be applied to respiratory effort signals obtained by RIP abdominal and thoracic belts. Despite the absence of airflow during obstructive apneas, the respiratory effort is still present, which challenges the detection of apneas when using this signal modality. However, when the effort is measured in combination with other modalities like airflow or SpO2, it can be used to differentiate between central and obstructive events [119]. When both the abdominal and thoracic belts are monitored, the thoracoabdominal paradoxFootnote 7 [26] can also be used as marker for apneic events.
A more extensive overview of methods using airflow and respiratory effort signals to detect OSA can be found in [110, 161]. The methods based on respiration reported in [110] obtained subject-based classification accuracies of 82–96% and an AUC of 88–90%.
5.3.3 Contactless Measures of Respiration
A lot of research has been conducted toward contactless sensors to measure respiratory effort. Respiratory movements can be extracted by pressure sensors in the mattress. An example of such a sensor is the Emfit, discussed in Sect. 8.3.2.5. In [72], the use of this sensor for the detection of sleep apnea was investigated. Rather than focusing on the breathing cessations, this study used unsupervised learning (i.e., clustering) to detect breathing distortions in the respiratory signal which are linked to arousals and large chest movements when breathing is regained. The amount of breathing distortions could be correlated to the AHI.
Kagawa et al. [78] proposed a system in which two Doppler radars are installed underneath the mattress in order to measure thoracic and abdominal effort. The system was tested for the detection of sleep apnea, a rule-based algorithm including the detection of paradoxical breathing showed promising results.
In [176], it was shown that the breathing rate can also be extracted accurately from IR video recordings in OSA subjects.
Castro et al. [37] proposed to measure the respiration using a capacitively coupled bioimpedance sensor embedded in a mattress. This system, however, still needs to be tested on OSA subjects.
5.4 Sound
Snoring is one of the most common symptoms of OSA, and differences in acoustic characteristics of snoring have been observed between OSA patients and simple snorers [150]. Moreover, due to apneas, subjects often make grasping and choking sounds. Researchers have developed acoustic features that can be used for the automatic detection of sleep apnea using sound recordings. Solà-Soler et al. have proposed snore intensity, pitch, frequency, and spectral envelope parameters [150]. Their study showed that the snore-to-snore variability of these features was increased in OSA subjects. Moreover, multiscale entropy [24] of audio recordings has also been shown to be useful to detect apneas.
5.5 Automatically Generated Features Using Deep Learning
All features mentioned before are handcrafted, they are extracted based on previous knowledge of the effect apneas have on the signals. The signals might, however, contain more information than these features. Therefore, more and more researchers have moved toward automatic feature extraction using deep learning, avoiding the challenging task of feature engineering. In [121], 21 studies detecting sleep apnea using deep learning were compared. Most studies were based on the ECG signal, but also SpO2 and respiration were considered. The convolutional neural network (CNN) was the most popular network. It is, however, not clear if this is the best choice since some studies suggested that recurrent neural networks (RNNs) outperformed CNN [121]. The included ECG-based methods report global screening accuracies of 79.5–100%.
5.6 Multimodal OSA Detection
Since the scoring rules for sleep apnea are based both on a reduction in airflow and the presence of oxygen desaturation, the combination of respiration and oximetry has frequently been studied [119, 161]. Moreover, cardiac signals are often added to capture the presence of arousals. Xie et al. [174] investigated the combination of SpO2 and ECG-based features. They concluded that the SpO2-based classifier outperformed the ECG-based one and that only a slight increase in performance could be obtained when both feature sets were combined. Similar results were obtained in our own study when PPG features were added to a SpO2-based classifier [53]. Behar et al., on the other hand, tested the combination of oximetry, sound, and actigraphy. When comparing the different modalities, oximetry outperformed the other two with a classification accuracy of 85.1%, but an increase in performance of 3.3% was obtained when all three modalities were combined.
5.7 Comparison of Methods and Modalities
When comparing the OSA detection performances which are reported by studies using different modalities, automatic classification using respiratory signals obtained lower performances than ECG and SpO2-based methods. Although, manual scoring of OSA is mainly based on respiration. This might be due to a higher noise level in the respiratory signals [110].
ECG-based methods seem to outperform other modalities in single sensor applications. But this might be due to the fact that many ECG-based algorithms use public data sets, such as the Apnea-ECG database, which are less distorted by noise and might be easier to classify [110]. When different modalities are compared on the same data set, the SpO2 signal performs best most of the times [53, 174]. In order to validate the potential added value of deep learning compared to feature-based algorithms, comparative studies on more challenging data sets than the Apnea-ECG data set should be performed.
Another observation is the fact that combining different sensor modalities often does not result in a relevant improvement of performance, probably because one of the sensors performs quite well and dominates the analysis [110]. When SpO2-based methods are combined with other modalities, they tend to dominate the performance [53, 174]. Not all apneic events can, however, be detected using the SpO2 signal since the AASM rules allow scoring apneas when no desaturation is present and hypopneas with only an arousal [26]. Therefore, sometimes the SpO2 remains stable during apneas. For the databases used in [54], 11.5% of annotated apneas could not be linked to an oxygen desaturation larger than 1%. Therefore, further research should be conducted to better merge different modalities in order to detect apneas that were missed by individual modalities. Additionally, combining different modalities improves the classification of apneas into event subtypes (central vs. obstructive) [119].
Although the Apnea-ECG database has stimulated the research into apnea detection methods greatly, most of the recordings only contain ECG signals. The database can, therefore, not be used to develop multimodal algorithms nor can it be used to compare the performances of different modalities. Moreover, the control group was composed of healthy subjects, instead of subjects with other sleep-related complaints which are seen in the sleep lab. Papini et al. have shown in their study [125] a drop in accuracy of 15% and a drop in sensitivity of 30% for algorithms trained on the apnea-ECG data set which were tested on a database including a wider spectrum of sleep disorders. These results show that the performance of apnea detection algorithms is strongly dependent on the data set used to train the algorithm. Therefore, one should consider the target population for which the application is being developed and train on a similar data set with the same pretest probability to have OSA.
Next to the Apnea-ECG data set, the National Sleep Research Resource (NSRR) [49] also provides PSG data sets, of which the Sleep Heart Health Study (SHHS) [130] has been used the most for the automatic detection of sleep apnea. This data set, however, was recorded in the general population, whereas sleep experts advise against OSA screening in the general population, but rather advise to screen groups with a high pretest probability in order to ensure a high post-test probability [44].
The availability of large public data sets, ideally including wearable data recorded simultaneously with the gold-standard PSG, is even more important for algorithms based on deep learning. These algorithms are completely data-driven and their performance tends to improve if more data is available.
Another important factor when comparing different algorithms is the used testing method. In order to obtain a fair generalization performance, the test set should be patient independent. However, studies often do not mention specifically if subject independence of the test set was imposed [121]. Especially for cardiovascular signals, the classification performance can increase significantly if part of the data from a test set patient was included in the training set since cardiovascular features can be highly patient dependent.
5.8 Future of Sleep Apnea Screening: Beyond the AHI?
Most of the studies developing automated screening algorithms for OSA validate their methods based on the AHI, which is used to define OSA severity in clinical practice. The AHI, however, only takes into account the number of apneas, but not their severity. This might explain why the AHI does not correlate well with the sleepiness of patients nor with cardiovascular outcome [52]. Moreover, when an AHI cutoff of 15 events per hour of sleep is considered, prevalences of up to 50% can be observed in middle-aged male populations [25]. Therefore, researchers are searching for alternatives for the AHI in order to better phenotype OSA subjects and prioritize them for treatment.
In [58], Eckert reviews phenotypic approaches for OSA, with a focus on the PALMFootnote 8 score. This score describes four traits causing OSA: an impaired upper airway anatomy, a low respiratory arousal threshold, an unstable ventilatory control system, and ineffective upper airway dilator muscles. According to the most dominant trait, other treatments could be proposed. Measures of each of the causes were defined based on gold-standard PSG and PAP drops, but should still be tested on wearable measurements.
In [52, 158], on the other hand, SpO2 severity parameters are proposed which correlate better than the AHI with the cardiovascular risk of OSA subjects.
This area of research is promising to enhance the phenotyping of OSA subjects, and in the future, these developed parameters could also be extracted from wearables in a home environment.
6 Conclusion
Sleep monitoring used to be a clearly defined domain based on EEG analysis. Bringing sleep monitoring to a home environment resulted in the emergence of a multitude of sensors and sleep staging algorithms. Within this chapter, unobtrusive state-of-the-art sensors and algorithms for sleep monitoring in adults were discussed as alternatives to the costly and uncomfortable in-hospital PSG. These novel technologies have the potential to enable a broader patient screening, early detection of sleep-related conditions, and a long-term follow-up at home.
Recently developed wearables and sensors placed around the patient were introduced, which measure PSG signals in a less obtrusive way or apply indirect measurements of the physiological parameters. The focus was on devices monitoring heart rate, respiration, and blood oxygenation, but actigraphy and portable EEG devices were also briefly discussed. An important aspect of these recently developed devices is that, although these provide increased comfort and a higher amount of data, the acquired data is of variable quality. This is caused by both the use of these technologies in an uncontrolled environment, as well as by the inherent characteristics of the technologies. In order to be able to exploit these solutions optimally, it is of high importance that research around this topic also includes the development and evaluation of algorithms for an automatic assessment of the quality of the data, as well as compensation methods for data of intermediate quality. Moreover, these novel devices require the development of application-specific algorithms for sleep monitoring.
The evaluation and comparison of sleep staging algorithms depend on many parameters, apart from studied population and algorithmic details. It includes sensor types, applied input signals, and mutual combinations. In general, good performances have been achieved based on solely the cardiac signal, being ECG or PPG, as it conveys respiratory information as well. The latest state-of-the-art sleep staging algorithms are furthermore based on deep learning techniques, which are expected to become even more important for future implementations. However, a validation of wearable or unobtrusive signals is often lacking. Therefore, the field of sleep staging at home would benefit from the development of algorithms that consider the limitations of wearable/unobtrusive data from the start.
Obstructive sleep apnea is the most common sleep-related breathing disorder, and it, however, often remains undiagnosed. Therefore, researchers have been developing OSA detection algorithms using signals that can be easily acquired in a home environment. ECG and SpO2-based algorithms have obtained the most promising results. However, most of the studies did not include experiments at home. These algorithms should thus be further tested on signals acquired unobtrusively from a home environment. Moreover, not much performance gain has been shown from multimodal algorithms, and smarter ways to combine different signal modalities should thus be investigated.
Notes
- 1.
The EEG captures the electrical activity from the brain, commonly obtained from the scalp using surface electrodes.
- 2.
The EOG records the electrical signal caused due to the opposite polarity between the front and back of the eye, which acts as a dipole.
- 3.
The EMG records the electrical activity of the muscles.
- 4.
The ECG records the electrical activity of the heart.
- 5.
Tidal volume corresponds to the volume of air inspired/expired with each breathing cycle.
- 6.
Time differences between consecutive R-peaks in the ECG.
- 7.
During obstructive apneas, the respiratory effort signals from the thoracic and abdominal belts are often out of phase, and this phenomenon is called the thoracoabdominal paradox.
- 8.
PALM is an acronym for the measured parameters for each of the four studied traits: Pcrit, arousal threshold, loop gain, and muscle responsiveness.
References
Beddit. https://www.beddit.com/. [Accessed 3 Feb 2020]
Bitbrain dry eeg. https://www.bitbrain.com/neurotechnology-products/dry-eeg. [Accessed 15 Jan 2020]
Byteflies. https://www.byteflies.com/. [Accessed 3 Feb 2020]
Dreem. https://dreem.com/en. [Accessed 15 Jan 2020]
Muse. https://choosemuse.com/. [Accessed 15 Jan 2020]
Neurovigil. https://neurovigil.com/. [Accessed 15 Jan 2020]
Onera health. https://www.onerahealth.com/. [Accessed 21 Jan 2020]
Sleep score labs. https://www.sleepscore.com/. [Accessed 21 Jan 2020]
Sleep sheperd. https://sleepshepherd.com/. [Accessed 15 Jan 2020]
Tatch health. https://www.tatchhealth.com/. [Accessed 21 Jan 2020]
Abad DG (2009) Development of a capacitive bioimpedance measurement system. MS thesis
Al-Angari HM, Sahakian AV (2007) Use of sample entropy approach to study heart rate variability in obstructive sleep apnea syndrome. IEEE Trans Biomed Eng 54(10):1900–1904
Aleksandrowicz A, Leonhardt S (2007) Wireless and non-contact ecg measurement system -the aachen smartchair-. Acta Polytech 47(4–5)
Alvarez D, Hornero R, Marcos JV, Wessel N, Penzel T, Glos M, Del Campo F (2013) Assessment of feature selection and classification approaches to enhance information from overnight oximetry in the context of apnea diagnosis. Int J Neural Syst 23(05):1350020
American Association of Sleep Technologists: Sleep technology technical guideline. standard polysomnography (2012)
Ansari AH, De Wel O, Pillay K, Dereymaeker A, Jansen K, Van Huffel S, Naulaers G, De Vos M (2019) A convolutional neural network outperforming state-of-the-art sleep staging algorithms for both preterm and term infants. J Neural Eng
Atallah L, Serteyn A, Meftah M, Schellekens M, Vullings R, Bergmans J, Osagiator A, Oetomo SB (2014) Unobtrusive ecg monitoring in the nicu using a capacitive sensing array. Physiol Meas 35(5):895
Baek HJ, Chung GS, Kim KK, Park KS (2011) A smart health monitoring chair for nonintrusive measurement of biological signals. IEEE Trans Inf Technol Biomed 16(1):150–158
Baek HJ, Kim JS, Kim KK, Park KS (2008) System for unconstrained ecg measurement on a toilet seat using capacitive coupled electrodes: the efficacy and practicality. In: 2008 30th annual international conference of the IEEE engineering in medicine and biology society. IEEE, pp 2326–2328
Bassetti C, Dogas Z, Peigneux P (2014) Sleep medicine textbook. European sleep research society (2014)
Bates A, Ling MJ, Mann J, Arvind DK (2010) Respiratory rate and flow waveform estimation from tri-axial accelerometer data. In: 2010 international conference on body sensor networks. IEEE, pp 144–150
Beattie Z, Oyang Y, Statan A, Ghoreyshi A, Pantelopoulos A, Russell A, Heneghan C (2017) Estimation of sleep stages in a healthy adult population from optical plethysmography and accelerometer signals. Physiol Meas 38(11):1968
Beddr: Sleep tuner. https://www.beddrsleep.com/how-it-works. [Accessed 21 Jan 2020]
Behar J, Roebuck A, Shahid M, Daly J, Hallack A, Palmius N, Stradling J, Clifford GD (2014) Sleepap: an automated obstructive sleep apnoea screening application for smartphones. IEEE J Biomed Health Inform 19(1):325–331
Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MS, Morrell MJ, Nunez CM, Patel SR, Penzel T, Pépin JL et al (2019) Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med 7(8):687–698
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, Marcus CL, Mehra R, Parthasarathy S, Quan SF et al (2012) Rules for scoring respiratory events in sleep: update of the 2007 aasm manual for the scoring of sleep and associated events. J Clin Sleep Med 8(05):597–619
Bianchi MT (2018) Sleep devices: wearables and nearables, informational and interventional, consumer and clinical. Metabolism 84:99–108
Bleichner MG, Debener S (2017) Concealed, unobtrusive ear-centered eeg acquisition: ceegrids for transparent eeg. Front Hum Neurosci 11:163
Bsoul M, Minn H, Tamil L (2010) Apnea medassist: real-time sleep apnea monitor using single-lead ecg. IEEE Trans Inf Technol Biomed 15(3):416–427
Camm AJ, Malik M, Bigger JT, Breithardt G, Cerutti S, Cohen RJ, Coumel P, Fallen EL, Kennedy HL, Kleiger R et al (1996) Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation 93:1043–1065
Casal R, Di Persia LE, Schlotthauer G (2019) Sleep-wake stages classification using heart rate signals from pulse oximetry. Heliyon 5(10):e02529
Castaneda D, Esparza A, Ghamari M, Soltanpur C, Nazeran H (2018) A review on wearable photoplethysmography sensors and their potential future applications in health care. Int J Biosens Bioelectron 4(4):195
Castro I, Varon C, Moeyersons J, Gomez AV, Morales J, Deviaene M, Torfs T, Van Huffel S, Puers R, Van Hoof C (2019) Data quality assessment of capacitively-coupled ecg signals. In: Proceedings of the 2019 computing in cardiology conference (CinC), Singapore, pp 8–11
Castro I, Varon C, Torfs T, Van Huffel S, Puers R, Van Hoof C (2018) Evaluation of a multichannel non-contact ecg system and signal quality algorithms for sleep apnea detection and monitoring. Sensors 18(2):577
Castro ID, Mercuri M, Torfs T, Lorato I, Puers R, Van Hoof C (2018) Sensor fusion of capacitively coupled ecg and continuous-wave doppler radar for improved unobtrusive heart rate measurements. IEEE J Emerg Select Top Circuits Syst 8(2):316–328
Castro ID, Morariu R, Torfs T, Van Hoof C, Puers R (2016) Robust wireless capacitive ecg system with adaptive signal quality and motion artifact reduction. In: 2016 IEEE international symposium on medical measurements and applications (MeMeA). IEEE, pp 1–6
Castro ID, Patel A, Torfs T, Puers R, Van Hoof C (2019) Capacitive multi-electrode array with real-time electrode selection for unobtrusive ecg and bioz monitoring. In: 2019 41st annual international conference of the IEEE engineering in medicine and biology society (EMBC). IEEE, pp 5621–5624
Chamadiya B, Heuer S, Hofmann U, Wagner M (2009) Towards a capacitively coupled electrocardiography system for car seat integration. In: 4th European conference of the international federation for medical and biological engineering. Springer, pp 1217–1221
de Chazal P, Penzel T, Heneghan C (2004) Automated detection of obstructive sleep apnoea at different time scales using the electrocardiogram. Physiol Meas 25(4):967–983
Chesson AL Jr, Berry RB, Pack A (2003) Practice parameters for the use of portable monitoring devices in the investigation of suspected obstructive sleep apnea in adults. Sleep 26(7):907–913
Chung KY, Song K, Shin K, Sohn J, Cho SH, Chang JH (2017) Noncontact sleep study by multi-modal sensor fusion. Sensors 17(7):1685
Ciołek M, Niedźwiecki M, Sieklicki S, Drozdowski J, Siebert J (2014) Automated detection of sleep apnea and hypopnea events based on robust airflow envelope tracking in the presence of breathing artifacts. IEEE J Biomed Health Inform 19(2):418–429
Cohen J (1960) A coefficient of agreement for nominal scales. Educ Psychol Measur 20(1):37–46
Collop NA, Tracy SL, Kapur V, Mehra R, Kuhlmann D, Fleishman SA, Ojile JM (2011) Obstructive sleep apnea devices for out-of-center (ooc) testing: technology evaluation. J Clin Sleep Med 7(05):531–548
Compumedics: Sompte sleep monitor. https://www.compumedics.com.au/products/somte/. [Accessed 15 Jan 2020]
Czaplik M, Eilebrecht B, Walocha R, Walter M, Schauerte P, Leonhardt S, Rossaint R (2012) The reliability and accuracy of a noncontact electrocardiograph system for screening purposes. Anesthesia Analgesia 114(2):322–327
De Chazal P, Fox N, O’hare E, Heneghan C, Zaffaroni A, Boyle P, Smith S, O’connell C, McNicholas WT (2011) Sleep/wake measurement using a non-contact biomotion sensor. J Sleep Research 20(2):356–366
De Chazal P, Heneghan C, Sheridan E, Reilly R, Nolan P, O’Malley M (2003) Automated processing of the single-lead electrocardiogram for the detection of obstructive sleep apnoea. IEEE Trans Biomed Eng 50(6):686–696
Dean DA, Goldberger AL, Mueller R, Kim M, Rueschman M, Mobley D, Sahoo SS, Jayapandian CP, Cui L, Morrical MG et al (2016) Scaling up scientific discovery in sleep medicine: the national sleep research resource. Sleep 39(5):1151–1164
Debener S, Emkes R, De Vos M, Bleichner M (2015) Unobtrusive ambulatory eeg using a smartphone and flexible printed electrodes around the ear. Sci Rep 5:16743
Dement W, Kleitman N (1957) Cyclic variations in eeg during sleep and their relation to eye movements, body motility, and dreaming. Electroencephalogr Clin Neurophysiol 9(4):673–690
Deviaene M, Borzée P, van Gilst M, van Dijk J, Overeem S, Buyse B, Testelmans D, Van Huffel S, Varon C (2020) Multilevel interval coded scoring to assess the cardiovascular status of sleep apnea patients using oxygen saturation markers. Accepted for publication in IEEE Transactions on Biomedical Engineering, available in early access
Deviaene M, Lázaro J, Huysmans D, Testelmans D, Buyse B, Van Huffel S, Varon C (2018) Sleep apnea detection using pulse photoplethysmography. In: 2018 computing in cardiology conference (CinC), vol 45. IEEE, pp 1–4
Deviaene M, Testelmans D, Buyse B, Borzée P, Van Huffel S, Varon C (2018) Automatic screening of sleep apnea patients based on the spo 2 signal. IEEE J Biomed Health Inform 23(2):607–617
Devot S, Dratwa R, Naujokat E (2010) Sleep/wake detection based on cardiorespiratory signals and actigraphy. In: 2010 annual international conference of the IEEE engineering in medicine and biology. IEEE, pp 5089–5092
Domingues A, Paiva T, Sanches JM (2014) Hypnogram and sleep parameter computation from activity and cardiovascular data. IEEE Trans Biomed Eng 61(6):1711–1719
Douglas N, White D, Pickett CK, Weil J, Zwillich C (1982) Respiration during sleep in normal man. Thorax 37(11):840–844
Eckert DJ (2018) Phenotypic approaches to obstructive sleep apnoea-new pathways for targeted therapy. Sleep Med Rev 37:45–59
emfit: Emfit sleep apnea monitor. https://www.emfit.com/emfit-qs-for-diagnosing-sleep-apnea. [Accessed 3 Feb 2020]
Faust O, Acharya UR, Ng E, Fujita H (2016) A review of ecg-based diagnosis support systems for obstructive sleep apnea. J Mech Med Biol 16(01):1640004
Faust O, Razaghi H, Barika R, Ciaccio EJ, Acharya UR (2019) A review of automated sleep stage scoring based on physiological signals for the new millennia. Computer methods and programs in biomedicine
Flemons WW, Littner MR, Rowley JA, Gay P, Anderson WM, Hudgel DW, McEvoy RD, Loube DI (2003) Home diagnosis of sleep apnea: a systematic review of the literature: an evidence review cosponsored by the american academy of sleep medicine, the american college of chest physicians, and the american thoracic society. Chest 124(4):1543–1579
Fonseca P, Aarts RM, Long X, Rolink J, Leonhardt S (2016) Estimating actigraphy from motion artifacts in ecg and respiratory effort signals. Physiol Meas 37(1):67–82
Fonseca P, Den Teuling N, Long X, Aarts RM (2018) A comparison of probabilistic classifiers for sleep stage classification. Physiol Meas 39(5):aabbc2. https://doi.org/10.1088/1361-6579/aabbc2
Fonseca P, Long X, Radha M, Haakma R, Aarts RM, Rolink J (2015) Sleep stage classification with ecg and respiratory effort. Physiol Meas 36(10):2027
Fonseca P, Weysen T, Goelema MS, Møst EI, Radha M, Lunsingh Scheurleer C, van den Heuvel L, Aarts RM (2017) Validation of photoplethysmography-based sleep staging compared with polysomnography in healthy middle-aged adults. Sleep 40(7):zsx097
Gil E, Vergara JM, Laguna P (2008) Detection of decreases in the amplitude fluctuation of pulse photoplethysmography signal as indication of obstructive sleep apnea syndrome in children. Biomed Signal Process Control 3(3):267–277
Goldberger AL, Amaral LA, Glass L, Hausdorff JM, Ivanov PC, Mark RG, Mietus JE, Moody GB, Peng CK, Stanley HE (2000) Physiobank, physiotoolkit, and physionet: components of a new research resource for complex physiologic signals. Circulation 101(23):e215–e220
Goverdovsky V, Looney D, Kidmose P, Mandic DP (2015) In-ear eeg from viscoelastic generic earpieces: Robust and unobtrusive 24/7 monitoring. IEEE Sens J 16(1):271–277
Guilleminault C, Winkle R, Connolly S, Melvin K, Tilkian A (1984) Cyclical variation of the heart rate in sleep apnoea syndrome: Mechanisms, and usefulness of 24 h electrocardiography as a screening technique. The Lancet 323(8369):126–131
Harper RM, Schechtman VL, Kluge KA (1987) Machine classification of infant sleep state using cardiorespiratory measures. Electroencephal Clin Neurophysiol 67(4):379–387. https://doi.org/10.1016/0013-4694(87)90126-X. http://www.sciencedirect.com/science/article/pii/001346948790126X
Huysmans D, Borzée P, Testelmans D, Buyse B, Willemen T, Huffel SV, Varon C (2019) Evaluation of a commercial ballistocardiography sensor for sleep apnea screening and sleep monitoring. Sensors 19(9):2133
Hwang SH, Lee YJ, Jeong DU, Park KS (2016) Unconstrained sleep stage estimation based on respiratory dynamics and body movement. Methods Inf Med 55(06):545–555
Hwang SH, Lee YJ, Jeong DU, Park KS et al (2016) Oxygen desaturation index estimation through unconstrained cardiac sympathetic activity assessment using three ballistocardiographic systems. Respiration 92(2):90–97
Inc B (2020) Mcot patch. https://www.myheartmonitor.com/device/mcot-patch/. [Accessed 3 Feb 2020]
Ishida S, Shiozawa N, Fujiwara Y, Makikawa M (2007) Electrocardiogram measurement during sleep with wearing clothes using capacitively-coupled electrodes. In: 2007 29th annual international conference of the IEEE engineering in medicine and biology society. IEEE, pp 2647–2650
Joshi R, Bierling BL, Long X, Weijers J, Feijs L, Van Pul C, Andriessen P (2018) A ballistographic approach for continuous and non-obtrusive monitoring of movement in neonates. IEEE J Trans Eng Health Med 6:1–10
Kagawa M, Tojima H, Matsui T (2016) Non-contact diagnostic system for sleep apnea-hypopnea syndrome based on amplitude and phase analysis of thoracic and abdominal doppler radars. Med Biol Eng Comput 54(5):789–798
Kelly JM, Strecker RE, Bianchi MT (2012) Recent developments in home sleep-monitoring devices. ISRN Neurol 2012
Kemp B, Janssen AJ, Van Der Kamp B (1998) Body position can be monitored in 3d using miniature accelerometers and earth-magnetic field sensors. Electroencephal Clin Neurophysiol/Electromyography Motor Control 109(6):484–488
Kemp B, Zwinderman AH, Tuk B, Kamphuisen HA, Oberye JJ (2000) Analysis of a sleep-dependent neuronal feedback loop: the slow-wave microcontinuity of the eeg. IEEE Trans Biomed Eng 47(9):1185–1194
Kidmose P, Looney D, Jochumsen L, Mandic DP (2013) Ear-eeg from generic earpieces: A feasibility study. In: 2013 35th annual international conference of the IEEE engineering in medicine and biology society (EMBC). IEEE, pp 543–546
Kim KK, Lim YK, Park KS (2004) The electrically noncontacting ecg measurement on the toilet seat using the capacitively-coupled insulated electrodes. In: The 26th annual international conference of the IEEE engineering in medicine and biology society, vol 1. IEEE, pp 2375–2378
Koley BL, Dey D (2013) Automatic detection of sleep apnea and hypopnea events from single channel measurement of respiration signal employing ensemble binary svm classifiers. Measurement 46(7):2082–2092
Kortelainen JM, Mendez MO, Bianchi AM, Matteucci M, Cerutti S (2010) Sleep staging based on signals acquired through bed sensor. IEEE Trans Inf Technol Biomed 14(3):776–785
Kranjec J, Beguš S, Drnovšek J, Geršak G (2013) Novel methods for noncontact heart rate measurement: A feasibility study. IEEE Trans Instrum Meas 63(4):838–847
Kurihara Y, Watanabe K (2012) Sleep-stage decision algorithm by using heartbeat and body-movement signals. IEEE Trans Syst, Man, Cybern-Part A: Syst Humans 42(6):1450–1459
Lázaro J, Gil E, Bailón R, Mincholé A, Laguna P (2013) Deriving respiration from photoplethysmographic pulse width. Med Biol Eng Comput 51(1–2):233–242
Lee HJ, Hwang SH, Yoon HN, Lee WK, Park KS (2015) Heart rate variability monitoring during sleep based on capacitively coupled textile electrodes on a bed. Sensors 15(5):11295–11311
Leonhardt S, Aleksandrowicz A (2008) Non-contact ecg monitoring for automotive application. In: 2008 5th international summer school and symposium on medical devices and biosensors. IEEE, pp 183–185
Li C, Cummings J, Lam J, Graves E, Wu W (2009) Radar remote monitoring of vital signs. IEEE Microwave Mag 10(1):47–56
Li C, Lubecke VM, Boric-Lubecke O, Lin J (2013) A review on recent advances in doppler radar sensors for noncontact healthcare monitoring. IEEE Trans Microw Theory Tech 61(5):2046–2060
Li Q, Li Q, Liu C, Shashikumar SP, Nemati S, Clifford GD (2018) Deep learning in the cross-time frequency domain for sleep staging from a single-lead electrocardiogram. Physiol Meas 39(12):124005
Lim YG, Hong KH, Kim KK, Shin JH, Lee SM, Chung GS, Baek HJ, Jeong DU, Park KS (2011) Monitoring physiological signals using nonintrusive sensors installed in daily life equipment. Biomed Eng Lett 1(1):11–20
Lim YG, Kim KK, Park KS (2007) Ecg recording on a bed during sleep without direct skin-contact. IEEE Trans Biomed Eng 54(4):718–725
Lim YG, Lee JS, Lee SM, Lee HJ, Park KS (2014) Capacitive measurement of ecg for ubiquitous healthcare. Ann Biomed Eng 42(11):2218–2227
Lim YK, Kim KK, Park KS (2004) The ecg measurement in the bathtub using the insulated electrodes. In: The 26th annual international conference of the IEEE engineering in medicine and biology society, vol 1. IEEE, pp 2383–2385
Lisenby M, Richardson P, Welch A (1976) Detection of cyclic sleep phenomena using instantaneous heart rate. Electroencephalogr Clin Neurophysiol 40(2):169–177
Littner M, Kushida CA, Anderson WM, Bailey D, Berry RB, Davila DG, Hirshkowitz M, Kapen S, Kramer M, Loube D, Wise M, Johnson SF (2003) Practice parameters for the role of actigraphy in the study of sleep and circadian rhythms: an update for 2002. Sleep 26(3):337–341. https://doi.org/10.1093/sleep/26.3.337
Long X, Fonseca P, Foussier J, Haakma R, Aarts RM (2013) Sleep and wake classification with actigraphy and respiratory effort using dynamic warping. IEEE J Biomed Health Inform 18(4):1272–1284
Long X, Yang J, Weysen T, Haakma R, Foussier J, Fonseca P, Aarts RM (2014) Measuring dissimilarity between respiratory effort signals based on uniform scaling for sleep staging. Physiol Meas 35(12):2529
Loomis AL, Harvey EN, Hobart GA III (1938) Distribution of disturbance-patterns in the human electroencephalogram, with special reference to sleep. J Neurophysiol 1(5):413–430
Macías R, García M, Ramos J, Bragos R, Fernández M (2013) Ventilation and heart rate monitoring in drivers using a contactless electrical bioimpedance system. J Phys: Conf Ser, 434, 012047. IOP Publishing
Mancia G (1993) Autonomic modulation of the cardiovascular system during sleep
Matar G, Lina JM, Carrier J, Kaddoum G (2018) Unobtrusive sleep monitoring using cardiac, breathing and movements activities: an exhaustive review. IEEE Access 6:45129–45152
Matsuda T, Makikawa M (2008) Ecg monitoring of a car driver using capacitively-coupled electrodes. In: 2008 30th annual international conference of the IEEE engineering in medicine and biology society. IEEE, pp 1315–1318
MBrainTrain: ceegrids. https://mbraintrain.com/concealed-eeg/. [Accessed 3 Feb 2020]
McDonald NJ, Anumula HA, Duff E, Soussou W (2012) Noncontact ecg system for unobtrusive long-term monitoring. In: 2012 annual international conference of the IEEE engineering in medicine and biology society. IEEE, pp 1614–1618
Mendonça F, Mostafa SS, Ravelo-García AG, Morgado-Dias F, Penzel T (2018) Devices for home detection of obstructive sleep apnea: A review. Sleep Med Rev 41:149–160
Mendonça F, Mostafa SS, Ravelo-García AG, Morgado-Dias F, Penzel T (2018) A review of obstructive sleep apnea detection approaches. IEEE J Biomed Health Inform 23(2):825–837
Mercuri M, Lorato IR, Liu YH, Wieringa F, Van Hoof C, Torfs T (2019) Vital-sign monitoring and spatial tracking of multiple people using a contactless radar-based sensor. Nat Electron 2(6):252–262
Migliorini M, Bianchi AM, Nisticò D, Kortelainen J, Arce-Santana E, Cerutti S, Mendez MO (2010) Automatic sleep staging based on ballistocardiographic signals recorded through bed sensors. In: 2010 annual international conference of the IEEE engineering in medicine and biology, pp 3273–3276. https://doi.org/10.1109/IEMBS.2010.5627217
Mikkelsen KB, Tabar YR, Kappel SL, Christensen CB, Toft HO, Hemmsen MC, Rank ML, Otto M, Kidmose P (2019) Accurate whole-night sleep monitoring with dry-contact ear-eeg. Sci Rep 9(1):1–12
Molinari S, Foulkes D (1969) Tonic and phasic events during sleep: psychological correlates and implications. Percept Mot Skills 29(2):343–368. https://doi.org/10.2466/pms.1969.29.2.343 PMID: 4310916
Moody G, Mark R, Goldberger A, Penzel T (2000) Stimulating rapid research advances via focused competition: The computers in cardiology challenge 2000. In: Computers in cardiology 2000, vol 27 (Cat. 00CH37163). IEEE, pp 207–210
Moody GB, Mark RG, Zoccola A, Mantero S (1985) Derivation of respiratory signals from multi-lead ecgs. Comput Cardiol 12(1985):113–116
Morales JF, Varon C, Deviaene M, Borzée P, Testelmans D, Buyse B, Van Huffel S (2017) Sleep apnea hypopnea syndrome classification in spo 2 signals using wavelet decomposition and phase space reconstruction. In: 2017 IEEE 14th international conference on wearable and implantable body sensor networks (BSN). IEEE, pp 43–46
Morales Tellez JF, Deviaene M, Milagro J, Testelmans D, Buyse B, Willems R, Orini M, Van Huffel S, Bailón R, Varon C (2019) Evaluation of methods to characterize the change of the respiratory sinus arrhythmia with age in sleep apnea patients. In: Proceedings of EMBC. IEEE (2019)
Moret-Bonillo V, Alvarez-Estévez D, Fernández-Leal A, Hernández-Pereira E (2014) Intelligent approach for analysis of respiratory signals and oxygen saturation in the sleep apnea/hypopnea syndrome. Open Med Inform J 8:1
Morgenthaler T, Alessi C, Friedman L, Owens J, Kapur V, Boehlecke B, Brown T, Chesson A Jr, Coleman J, Lee-Chiong T et al (2007) Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: an update for 2007. Sleep 30(4):519–529
Mostafa SS, Mendonça F, Ravelo-García AG, Morgado-Dias F (2019) A systematic review of detecting sleep apnea using deep learning. Sensors 19(22):4934
Mousavi S, Afghah F, Acharya UR (2019) Sleepeegnet: automated sleep stage scoring with sequence to sequence deep learning approach. PLoS ONE 14(5):e0216456
Obeid D, Sadek S, Zaharia G, El Zein G (2010) Multitunable microwave system for touchless heartbeat detection and heart rate variability extraction. Microw Opt Technol Lett 52(1):192–198
Oksenberg A, Khamaysi I, Silverberg DS, Tarasiuk A (2000) Association of body position with severity of apneic events in patients with severe nonpositional obstructive sleep apnea. Chest 118(4):1018–1024
Papini GB, Fonseca P, Margarito J, van Gilst MM, Overeem S, Bergmans JW, Vullings R (2018) On the generalizability of ecg-based obstructive sleep apnea monitoring: merits and limitations of the apnea-ecg database. In: 2018 40th annual international conference of the IEEE engineering in medicine and biology society (EMBC). IEEE, pp 6022–6025
Paquet J, Kawinska A, Carrier J (2007) Wake detection capacity of actigraphy during sleep. Sleep 30(10):1362–1369
Penzel T, Moody GB, Mark RG, Goldberger AL, Peter JH (2000) The apnea-ecg database. In: Computers in cardiology 2000, vol 27 (Cat. 00CH37163). IEEE, pp 255–258
Petkie DT, Benton C, Bryan E (2009) Millimeter wave radar for remote measurement of vital signs. In: 2009 IEEE radar conference. IEEE, pp 1–3
Pinheiro E, Postolache O, Girão P (2012) A practical approach concerning the capacitive acquisition of the electrocardiogram in a moving wheelchair. In: Proceedings of the XX IMEKO world congress
Quan SF, Howard BV, Iber C, Kiley JP, Nieto FJ, O’Connor GT, Rapoport DM, Redline S, Robbins J, Samet JM et al (1997) The sleep heart health study: design, rationale, and methods. Sleep 20(12):1077–1085
Radha M, Fonseca P, Moreau A, Ross M, Cerny A, Anderer P, Long X, Aarts RM (2019) Sleep stage classification from heart-rate variability using long short-term memory neural networks. Sci Rep 9(1):1–11
Rechtschaffen A, Kales A (1968) A manual of standardized terminology, techniques, and scoring system for sleep stages for human subjects. Natl Inst Health 204
Redmond SJ, de Chazal P, O’Brien C, Ryan S, McNicholas WT, Heneghan C (2007) Sleep staging using cardiorespiratory signals. Somnologie-Schlafforschung und Schlafmedizin 11(4):245–256
Redmond SJ, Heneghan C (2006) Cardiorespiratory-based sleep staging in subjects with obstructive sleep apnea. IEEE Trans Biomed Eng 53(3):485–496
ResMed: S+ sleep monitor. https://splus.resmed.com/. [Accessed 3 Feb 2020]
Resonea: Drowzle pro. https://www.resonea.com/drowzle-pro/. [Accessed 21 Jan 2020]
Richardson P (1967) The insulated electrode: a pasteless electrocardiographic technique. In: 20th Annual conference on engineering in medicine and biology, vol 9, pp 15–17
Roebuck A, Monasterio V, Gederi E, Osipov M, Behar J, Malhotra A, Penzel T, Clifford G (2013) A review of signals used in sleep analysis. Physiol Meas 35(1):R1
Roehrs T, Zorick F, Wittig R, Conway W, Roth T (1989) Predictors of objective level of daytime sleepiness in patients with sleep-related breathing disorders. Chest 95(6):1202–1206
Roomkham S, Lovell D, Cheung J, Perrin D (2018) Promises and challenges in the use of consumer-grade devices for sleep monitoring. IEEE Rev Biomed Eng 11:53–67
Rosenberg RS, Van Hout S (2013) The american academy of sleep medicine inter-scorer reliability program: sleep stage scoring. J Clin Sleep Med 9(01):81–87
Sadeh A, Acebo C (2002) The role of actigraphy in sleep medicine. Sleep Med Rev 6(2):113–124
Sateia MJ (2014) International classification of sleep disorders. Chest 146(5):1387–1394
Schnall RP, Shlitner A, Sheffy J, Kedar R, Lavie P (1999) Periodic, profound peripheral vasoconstriction as a new marker of obstructive sleep apnea. Sleep 22(7):939–946
Schulz H (2008) Rethinking sleep analysis comment on the aasm manual for the scoring of sleep and associated events. J Clin Sleep Med 4(02):99–103
Schumm J, Axmann S, Arnrich B, Tröster G (2010) Automatic signal appraisal for unobtrusive ecg measurements. Int. J. Bioelectromagn 12(4):158–164
Schumm J, Setz C, Bächlin M, Bächler M, Arnrich B, Tröster G (2010) Unobtrusive physiological monitoring in an airplane seat. Pers Ubiquit Comput 14(6):541–550
Scullin MK, Bliwise DL (2015) Sleep, cognition, and normal aging: integrating a half century of multidisciplinary research. Perspect Psychol Sci 10(1):97–137
Singh RK, Sarkar A, Anoop C (2016) A health monitoring system using multiple non-contact ecg sensors for automotive drivers. In: 2016 IEEE international instrumentation and measurement technology conference proceedings. IEEE, pp 1–6
Solà-Soler J, Fiz JA, Morera J, Jané R (2012) Multiclass classification of subjects with sleep apnoea-hypopnoea syndrome through snoring analysis. Med Eng Phys 34(9):1213–1220
Solutions CS (2020) Watch pat. https://cardiosleepsolutions.com/product/watchpat-one/. [Accessed 21 Jan 2020]
Solutions VCH (2020) Vivalnk ecg patch. http://www.vivalnk.com/ecg-monitor. [Accessed 3 Feb 2020]
Somers VK, Dyken ME, Mark AL, Abboud FM (1993) Sympathetic-nerve activity during sleep in normal subjects. N Engl J Med 328(5):303–307
Stephansen JB, Olesen AN, Olsen M, Ambati A, Leary EB, Moore HE, Carrillo O, Lin L, Han F, Yan H et al (2018) Neural network analysis of sleep stages enables efficient diagnosis of narcolepsy. Nat Commun 9(1):1–15
Sun Y, Yu XB (2016) Capacitive biopotential measurement for electrophysiological signal acquisition: A review. IEEE Sens J 16(9):2832–2853
Supratak A, Dong H, Wu C, Guo Y (2017) Deepsleepnet: A model for automatic sleep stage scoring based on raw single-channel eeg. IEEE Trans Neural Syst Rehabil Eng 25(11):1998–2008
iRhythm Technologies: Zio xt. https://www.irhythmtech.com/products-services/zio-xt. [Accessed 3 Feb 2020]
Terrill PI (2019) A review of approaches for analysing obstructive sleep apnoea-related patterns in pulse oximetry data. Respirology
Tsinalis O, Matthews PM, Guo Y, Zafeiriou S (2016) Automatic sleep stage scoring with single-channel eeg using convolutional neural networks. arXiv preprint arXiv:1610.01683
Uçar MK, Bozkurt MR, Bilgin C, Polat K (2018) Automatic sleep staging in obstructive sleep apnea patients using photoplethysmography, heart rate variability signal and machine learning techniques. Neural Comput Appl 29(8):1–16
Uddin M, Chow C, Su S (20148) Classification methods to detect sleep apnea in adults based on respiratory and oximetry signals: a systematic review. Physiol Meas 39(3):03TR01
Ueno A, Akabane Y, Kato T, Hoshino H, Kataoka S, Ishiyama Y (2007) Capacitive sensing of electrocardiographic potential through cloth from the dorsal surface of the body in a supine position: A preliminary study. IEEE Trans Biomed Eng 54(4):759–766
Varon C, Caicedo A, Testelmans D, Buyse B, Van Huffel S (2015) A novel algorithm for the automatic detection of sleep apnea from single-lead ecg. IEEE Trans Biomed Eng 62(9):2269–2278
Varon C, Morales J, Lázaro J, Orini M, Deviaene M, Kontaxis S, Testelmans D, Buyse B, Borzée P, Sörnmo L, Laguna P, Gil E, Bailón R (2020) A comparative study of ecg-derived respiration in ambulatory monitoring using the single-lead ecg. Submitted to scientific reports
Varon C, Van Huffel S (2017) Complexity and nonlinearities in cardiorespiratory signals in sleep and sleep apnea. In: Complexity and nonlinearity in cardiovascular signals. Springer, pp 503–537
Vehkaoja A, Salo A, Peltokangas M, Verho J, Salpavaara T, Lekkala J (2014) Unconstrained night-time heart rate monitoring with capacitive electrodes. In: XIII mediterranean conference on medical and biological engineering and computing 2013. Springer, pp 1511–1514
Weil MB, Oehler M, Schilling M, Maier LS (2012) First clinical evaluation of a novel capacitive ecg system in patients with acute myocardial infarction. Clin Res Cardiol 101(3):165–174
Willemen T, Van Deun D, Verhaert V, Vandekerckhove M, Exadaktylos V, Verbraecken J, Van Huffel S, Haex B, Vander Sloten J (2014) An evaluation of cardiorespiratory and movement features with respect to sleep-stage classification. IEEE J Biomed Health Inform 18(2):661–669
Willemen T, Varon C, Dorado AC, Haex B, Vander Sloten J, Van Huffel S (2015) Probabilistic cardiac and respiratory based classification of sleep and apneic events in subjects with sleep apnea. Physiol Meas 36(10):2103
Withings: Sleep mat. https://www.beddit.com/. [Accessed 3 Feb 2020]
Wu KF, Zhang YT (2008) Contactless and continuous monitoring of heart electric activities through clothes on a sleeping bed. In: 2008 international conference on information technology and applications in biomedicine. IEEE, pp 282–285
X, P.: Potential x smart earbuds. https://www.potential-x.com/. [Accessed 3 Feb 2020]
Xiao M, Yan H, Song J, Yang Y, Yang X (2013) Sleep stages classification based on heart rate variability and random forest. Biomed Signal Process Control 8(6):624–633
Xie B, Minn H (2012) Real-time sleep apnea detection by classifier combination. IEEE Trans Inf Technol Biomed 16(3):469–477
Zaunseder S, Henning A, Wedekind D, Trumpp A, Malberg H (2017) Unobtrusive acquisition of cardiorespiratory signals. Somnologie 21(2):93–100
Zhu K, Li M, Akbarian S, Hafezi M, Yadollahi A, Taati B (2019) Vision-based heart and respiratory rate monitoring during sleep-a validation study for the population at risk of sleep apnea. IEEE J Transl Eng Health Med 7:1–8
Ziegler D, Laux G, Dannehl K, Spüler M, Mühlen H, Mayer P, Gries F (1992) Assessment of cardiovascular autonomic function: age-related normal ranges and reproducibility of spectral analysis, vector analysis, and standard tests of heart rate variation and blood pressure responses. Diabet Med 9(2):166–175
Zink MD, Brüser C, Stüben BO, Napp A, Stöhr R, Leonhardt S, Marx N, Mischke K, Schulz JB, Schiefer J (2017) Unobtrusive nocturnal heartbeat monitoring by a ballistocardiographic sensor in patients with sleep disordered breathing. Sci Rep 7(1):13175
Acknowledgements
This research received funding from Agentschap Innoveren en Ondernemen (VLAIO) 150466 OSA+, imec sbo funds Wearablehealth, and the Flemish Government (AI Research Program). SVH, CV, DH, and MD are affiliated to Leuven.AI - KU Leuven institute for AI, B-3000, Leuven, Belgium. KU Leuven Stadius acknowledges the financial support of imec.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Deviaene, M. et al. (2022). Sleep Monitoring in Adults Using Wearables and Unobtrusive Technology. In: Gargiulo, G.D., Naik, G.R. (eds) Wearable/Personal Monitoring Devices Present to Future. Springer, Singapore. https://doi.org/10.1007/978-981-16-5324-7_8
Download citation
DOI: https://doi.org/10.1007/978-981-16-5324-7_8
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-5323-0
Online ISBN: 978-981-16-5324-7
eBook Packages: EngineeringEngineering (R0)