Abstract
Calcium ions serve as an important intracellular messenger in many diverse pathways, ranging from excitation coupling in muscles to neurotransmitter release in neurons. Physiologically, the concentration of free intracellular Ca2+ is up to 10,000 times less than that of the extracellular concentration, and increases of 10- to 100-fold in intracellular Ca2+ are observed during signaling events. Voltage-gated calcium channels (VGCCs) located on the plasma membrane serve as one of the main ways in which Ca2+ is able to enter the cell. Given that Ca2+ functions as a ubiquitous intracellular messenger, it is imperative that VGCCs are under tight regulation to ensure that intracellular Ca2+ concentration remains within the physiological range. In this chapter, we explore VGCCs’ inherent control of Ca2+ entry as well as the effects of alternative splicing in CaV2.1 and posttranslational modifications of CaV1.2/CaV1.3 such as phosphorylation and ubiquitination. Deviation from this physiological range will result in deleterious effects known as calcium channelopathies, some of which will be explored in this chapter.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Voltage-gated calcium channels
- CACNA1C
- CACNA1D
- CACNA1A
- Cav1.2
- Cav1.3
- Cav2.1
- Channelopathies
- Splicing
- Modulation
1 Ion Channels in Biophysics and Physiology
1.1 Introduction to LTCC
L-type calcium channels (LTCC) are a subset of voltage-gated calcium channels (VGCC). LTCCs comprise calcium channel (Cav) isoforms Cav1.1–Cav1.4 and are encoded by the human genes CACNA1S, CACNA1C, CACNA1D, and CACNA1F, respectively. They are called “L-type” because of their long-lasting Ba2+ conductance, which is attributed to the slow inactivation kinetics of LTCCs (~500 ms). Unlike the other VGCCs, LTCCs are the only group that can bind to various 1,4-dihydropyridines (DHP) and are thus also called dihydropyridine receptors (DHPR).
LTCCs are transmembrane proteins found on the plasma membrane of excitable cells such as neurons, skeletal, cardiac, and smooth muscles [1, 2]. Similar to other VGCCs, LTCCs are voltage-gated and they open in response to membrane depolarization, thereby allowing for the selective influx of calcium ions (Ca2+) into the cytoplasm. This Ca2+ influx regulates various downstream functions like synaptic vesicle anchorage and release, gene expression, and excitation–contraction (EC) coupling [3]. While the topological structure of LTCCs is generally similar across the tissues they are expressed in, their functions differ according to their tissue localization and biophysical properties. Further discussions will be focused on the cardiovascular system for the purpose of this review.
1.2 Structure and Localization of LTCC
LTCCs are transmembrane protein complexes made up of four to five subunits depending on where they are expressed—α1-, β-, a2δ-, and γ-subunits [2]. In skeletal and cardiac muscles, the γ-subunit is not associated with Cav1.2 and Cav1.3 isoforms. The ~250 kDa α1-subunit forms the main pore of the channel complex and is comprised of four repeat domains (DI–IV), with each domain made up of six transmembrane segments (S1–S6) that are linked by intracellular loops. To date, there are ten known mammalian isoforms of α1-subunit of which 4 are LTCCs. The S4 of each domain acts as the voltage sensor for the channel due to the presence of positively charged amino acids, while the S5 and S6 segments form the activation gate of the α1-subunit and the S5–S6 reentrant loop lines the selectivity filter. Upon membrane depolarization, the change in membrane potential is “sensed” by the four S4 segments, resulting in a conformational change from close to open state, thereby facilitating the flux of Ca2+ ions across the membrane.
The auxiliary β- and a2δ-subunits are necessary for the proper expression and insertion of the α1-subunit into the plasma membrane. It was reported that the overexpression of either the β- or a2δ-subunits enhanced the current density of the α1-subunit [4]. Conversely, the current density is reduced when either of these subunits was transiently knocked down. These data suggest that the function of the α1-subunit is regulated by the coexpression of the auxiliary subunits.
Co-immunoprecipitation experiments revealed that the β-subunit physically associates with the α1-subunit. More importantly, this association occurs within a region between DI and DII linker (I–II loop), named as the α1-interacting domain (AID) [5]. Interestingly, in vitro experiments revealed a potential mechanism by which the binding of the β-subunit to the AID is important in regulating the expression of the α1-subunit. Of note, disruption to this interaction was reported to have resulted in the poly-ubiquitination of the α1-subunit, leading to proteasomal degradation and thus decreased trafficking of the α1-subunit to the plasma membrane [6].
1.3 LTCC in the Cardiovascular System—Function
In the cardiovascular system (CVS), LTCC isoforms Cav1.2 and Cav1.3 are found to be expressed. Cav1.2 is the predominant isoform expressed in excitable cells [1]. Conversely, Cav1.3 is found to be dominantly expressed in the sinoatrial node (SAN) and the atrioventricular node (AVN) and is important for pacemaking activity [7].
Cav1.2 and Cav1.3 are responsible for the initiation of the excitation–contraction (EC) coupling [3], a process whereby an electrical signal is converted into mechanical signals. Macroscopically, this can be seen simply as “contraction” of the muscle cells. Microscopically, the depolarizing electrical signals are sensed by the S4 “voltage sensors,” and the ensuing protein conformational change leads to channel activation. The resultant Ca2+ influx causes a transient increase in intracellular Ca2+ concentration. The binding of Ca2+ by the ryanodine receptors (RyR) localized to the membrane of sarcoplasmic reticulum (SR) activates the RyRs to open to release Ca2+ within the intracellular store of the SR, and this process further increases cytoplasmic Ca2+ concentration. This process, also known as calcium-induced calcium release (CICR), triggers a cascade of downstream biochemical signals, ultimately allowing for the contraction of muscle fibers via activation of tropomyosin. Although the sliding motion of a few tropomyosin proteins may seem insignificant, nevertheless, the coordinated, simultaneous sliding of tropomyosin across the entire muscle fiber is sufficient to generate much mechanical force for various processes such as vasocontraction, contraction of the myocardium during systole, and concentric movements such as weightlifting.
In the heart, this coordinated EC coupling process and pumping action of the myocardium are essential for maintaining a constant blood supply throughout the body. In the vessels, Cav1.2 is essential for maintaining the basal vascular tone of blood vessels, contributing to the maintenance of blood pressure. In both events, mutations of Cav1.2 or Cav1.3 result in channelopathies and could lead to serious health complications such as those discussed subsequently.
1.4 Channelopathies in the CVS—Cav1.2
1.4.1 Timothy Syndrome
Timothy Syndrome (TS) was first discovered by Katherine W. Timothy and is a rare multi-organ disorder that affects not only the myocardium but also the brain. TS is associated with a gain-of-function mutation in the α1-subunit of Cav1.2. There are two unique mutations categorized, G406R and G402S, which occur in the mutually exclusive exons 8 or 8a of the α1-subunit [8, 9]. As such, TS can be further categorized as a classical type I TS or an atypical type II TS depending on which exon is affected. Of note, exon 8 and 8a are both found in the S6 segment of DI, which forms part of the activation gate. In type I TS, G406R mutation was observed in exon 8a, while in type II TS, either G406R or G402S can be found in exon 8. In both events, this gain-of-function mutation results in reduced voltage-dependent inactivation (VDI) of the Cav1.2 channel, thereby resulting in a sustained increase in Ca2+ influx, long QT syndrome (LQTS), and thus arrhythmias. In most cases, arrhythmias remain the primary underlying cause of death for patients presenting with TS. As TS is a multisystem disorder, it was observed that in addition to cardiac symptoms, patients with TS also present with extracardiac phenotypes. These typically include syndactyly, dysmorphic facial features, and mental retardation.
1.4.2 Brugada Syndrome
In contrast to TS, Brugada Syndrome (BS) occurs due to loss-of-function mutations in the α1-subunit of Cav1.2. This results in shorter QT intervals and contributes to the manifestation of arrhythmias [10, 11]. While gain-of-function mutations within the α1-subunit are responsible for TS, loss-of-function mutations in the β-subunit also contribute to the progression of BS. It has been reported that in Chinese hamster ovary (CHO) cells, the loss-of-function mutations in both α1- and β-subunits led to decreased current density. Despite this, however, it is interesting to note the surface expression of Cav1.2 in BS was not affected when investigated in neuronal rat brain [11].
Despite the differences in mutations, these results, when taken together, strongly suggest that the function of Cav1.2 within the myocardium needs to be tightly regulated. As seen earlier, dysregulation of either the main pore-forming α1-subunit or the auxiliary β-subunit could result in serious health complications.
1.5 Channelopathies in the CVS—Cav1.3
1.5.1 Cardiac Dysfunction/Arrhythmia
The Cav1.3 isoform is encoded by the CACNA1D gene, and like Cav1.2, channelopathies due to mutations in CACNA1D could result in abnormal heart functions. Cav1.3 is activated at a more hyperpolarizing potential relative to Cav1.2, enabling its contribution to pacemaking in the SAN and AVN [7]. In a study done to better understand the contributions of Cav1.3 mutations to cardiac symptoms, a family presenting with Cav1.3 mutations was recruited and their electrocardiogram (ECG) studied [12]. It was then reported that severe bradycardia was observed at rest between a 12- to 24-h period in individuals with Cav1.3 mutations but not in the healthy individuals. Yet, it is interesting to note that unlike Cav1.2 mutations, these affected individuals did not present with any abnormalities to either the QRS complex or the QT intervals, thereby indicating that this bradycardia was associated with the conductance of the nodes. Further screening and characterizing of mutations in this family revealed the insertion of a glycine residue in various positions of the α1-subunit. Of note, the insertion of a glycine residue at position 404 was reported to be found only in the mutually exclusive exon 8b. Again, this exon is located in the S6 of DI, which is part of the activation gate. Functional studies using patch-clamp experiments into the differences of biophysical properties in tsA-203 cells between wild-type and mutant Cav1.3 revealed that the insertion of the glycine residue results in a nonconducting variant of Cav1.3. Moreover, reverse transcriptase-polymerase chain reaction (RT-PCR) results showed that exon 8b is predominant in the SAN and not in the ventricles of the myocardium. Thus, the cardiac symptom presented due to this Cav1.3 mutation is due to SAN dysfunction and arrhythmia and not due to ventricular dysfunctions.
1.6 Regulation of Cav1.2
As discussed earlier, it is imperative that the activity of Cav in the heart is tightly regulated to function within a specific narrow range, the deviation of which could lead to serious health implications. Therefore, it is only natural that various mechanisms, for example, posttranslational modifications (PTMs), are in place to properly regulate the function of these calcium channels. An in-depth review of Cav1.2 post-translation modification has been recently published [13].
Cav1.2 is known to be phosphorylated by various protein kinases, namely, serine/threonine protein kinases A (PKA), C (PKC), G (PKG), and Ca2+/Calmodulin-dependent protein kinase II (CaMKII) [14]. It has been proposed that phosphorylation of serine residues in Cav is a mechanism that regulates protein–protein interactions. Of note, PKA phosphorylation of serine 1928 (S1928) was reported to transiently disrupt the interaction between Cav1.2 and the β2-adrenergic receptor (β2AR). Yet, despite being the most abundant phosphorylation site of Cav1.2 in the myocardium, S1928 was not involved in the β-adrenergic upregulation of Cav1.2 in the heart. Interestingly, S1928 can also be phosphorylated by PKC. However, unlike the prior PKA-dependent phosphorylation event, S1928 phosphorylation by PKC was reported to increase Cav1.2 current density. Furthermore, PKG was also reported to phosphorylate S1928. In this case, however, a reduced calcium current was reported in the transfected human embryonic kidney (HEK) 293 cells. Despite phosphorylation of the same serine residue within the full-length Cav1.2 channel, it is intriguing that phosphorylation by different protein kinases resulted in different downstream effects on the channel. From this, it can be seen that S1928 phosphorylation, while important, was not solely responsible for the changes in the function of Cav1.2. Nevertheless, it is imperative that S1928 phosphorylation be considered as part of the possible mechanisms for regulating Cav1.2 channel function.
Ubiquitination is another common PTM known to regulate protein expression and turnover rates. Ret finger protein 2 (Rfp2), or tripartite motif-containing 13 (TRIM13), poly-ubiquitinates lysine residues located within the intracellular II–III loop, leading to proteasomal degradation of Cav1.2 [15]. However, it remains to be proven if Rfp2 physically associates with Cav1.2. Yet, when the β-subunit is co-expressed with the α1C-subunit, there is a significant reduction in ubiquitination of the α1C-subunit. Therefore, it can be hypothesized that the auxiliary β-subunit is necessary for the expression of Cav1.2. A recent study has shown that disruption of the interaction between the α1C-subunit and the β-subunit by a novel binding partner, Galectin-1 (Gal-1), led to increased ubiquitination and turnover of Cav1.2 α1-subunit protein [6]. More importantly, the study also revealed that overexpression of Gal-1 is associated with hypotension. Conversely, knockdown of Gal-1 protein via siRNAs led to increased blood pressure. It can thus be said that although the α1-subunit is the main pore-forming subunit, its expression at the protein level is regulated tightly by auxiliary subunits like the β-subunit. Of interest, Gal-1 binding to the I–II loop is hugely reduced in the presence of alternative exon 9*, an exon that is selectively expressed in smooth but not cardiac muscle.
1.7 Conclusion
All in all, this section has discussed the importance of LTCC Cav1.2 and Cav1.3 in the CVS. Modulation of Cav function has to be tightly regulated such that its activity remains within a physiological range, outside of which could lead to the pathogenesis of cardiovascular diseases. Both de novo or familial genetic mutations of the CACNA1C gene are associated with a variety of diseases comprising cardiac and extracardiac symptoms. Thus, further studies to understand the regulation of Cav1.2 in the context of cardiovascular diseases are necessary to better treat cardiac diseases and improve the quality of life of patients.
2 CaV2.1
Much like the previous CaV1 channel family, channels in the CaV2 channel family comprise hetero-multimetric assemblies of a pore-forming CaVα1 subunit, auxiliary CaVβ, and CaVα2δ subunits, with the α1-subunit determining the channel subtype. There are three-channel subtypes in the CaV2 family, CaV2.1, CaV2.2, and CaV2.3, that are encoded by three genes CACNA1A, CACNA1B, and CACNA1E, respectively [16,17,18]. In this chapter, we will focus mainly on the history of CaV2.1 as well as the structure and function of this channel along with the various mechanisms that govern its modulation.
2.1 History of CaV2.1 Channel
CaV2.1 gives rise to both the P-type Ca2+ currents, aptly named P-type as it was first recorded in Purkinje neurons [19, 20], and Q-type Ca2+ currents that were first recorded in cerebellar granule cells [21]. Although both currents displayed very similar electrophysiological properties, they differed in their inactivation kinetics as well as their sensitivity to ω-Agatoxin IVA, with P-type Ca2+ channels exhibiting a higher sensitivity to ω-Agatoxin IVA [21]. Hence, it was initially thought that P-type and Q-type Ca2+ currents were generated by different α1 subunits [21], although both P-type and Q-type currents were found to be required for neurotransmitter release [22,23,24,25]. What eventually resolved this mystery was a combination of molecular cloning and electrophysiological methods.
The amino acid sequence of CaV2.1 was first obtained in 1991 from the cloned cDNA sequence of a rabbit brain calcium channel, then referred to as BI [16], or also as class A calcium channel by Snutch’s group [26]. Northern blot analysis of the BI voltage-gated calcium (CaV) channel showed that it was highly expressed in the brain, particularly in the cerebellum, and at a far lower level in the heart. Using mutant mice models with different patterns of cerebellar degeneration, it was deduced that BI calcium channels were highly expressed in both Purkinje cells and granule cells [16]. This was later confirmed in a later study where the spatial distribution of BI mRNA in the rat cerebellum (rbA for rat variant) showed a high expression of rbA mRNA in Purkinje cells and a lower expression of rbA mRNA in granule cells [27]. The electrophysiological and pharmacological properties as well as expression patterns were also similar to that observed of P-type channels in Purkinje cells, leading to postulations that BI/rbA Ca2+ channels correspond to the P-type Ca2+ channels [28], although there was initial caution to concluding that the BI channel was the same as the P-type Ca2+ channel due to certain differences in sensitivity to ω-Agatoxin IVA and inactivation kinetics [29].
Subsequently, there was also standardization of the calcium channel nomenclature, with class A calcium channel subunit (α1A) gradually being the accepted name. Evidence for α1A corresponding to P-type Ca2+ channel became more compelling when a study co-expressed different calcium channel β subunits with rat α1A in Xenopus oocytes and was able to generate a current waveform similar to the P-type Ca2+ current observed in Purkinje cells when α1A was expressed with β2a. Interestingly, when α1A was expressed with β1b or β3, current waveforms similar to the Q-type Ca2+ current observed in cerebellar granule cells were produced. A more native expression system involving rat neostriatal and cortical neurons further confirmed the effect of the β-subunit expression on α1A channel kinetics [30]. Coupled with the in situ localization results showing that α1A transcripts were also found to be highly expressed in Purkinje cells and granule cells, cells where P-type channels are highly expressed, it was highly conceivable that α1A transcripts could correspond to P and Q-type Ca2+ channels [27]. The most convincing piece of evidence for α1A giving rise to P and Q-type Ca2+ channels finally came when screening of a rat brain cDNA library was performed [31]. Three alternatively spliced α1A isoforms were identified, with a valine insertion in the domain I–II linker (Val421), an insertion of Asn and Pro (N1605–P1606), due to the use of an alternative 5′ splice donor site, in the extracellular linker between transmembrane segments S3 and S4 of domain IV, and 10 different amino acid residues in the carboxyl tail adjacent to domain IV S6 (also identified as EF hand-like motif). Expression of the different splice variants in Xenopus oocytes revealed alterations in channel properties. When α1A was co-expressed with β2a, there was slower inactivation kinetics similar to that observed in P-type Ca2+ channels. On the other hand, when α1A was co-expressed with β1, β3, or β4 subunits, faster inactivation kinetics similar to those observed in Q-type Ca2+ channels was seen. Sensitivity to ω-Aga-IVA was also found to be affected by alternative splicing. When the α1A splice variant lacking N1605–P1606 was expressed in HEK 293 cells, the sensitivity of α1A to ω-Aga IVA was reduced, similar to native P-type channels. α1A splice variants containing N1605–P1606 was shown to be more sensitive to ω-Aga IVA, resembling Q-type channels. It was thus proposed that both P-type and Q-type are phenotypic variants arising from the alternative splicing of the α1A transcript [31], hence solving the issue of the molecular origins of the P/Q-type Ca2+ channel.
In the following sections, we will continue to explore alternative splicing and its possible physiological roles.
2.2 CaV2.1 Channel Diversity
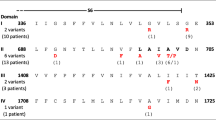
Following the discovery of the three alternatively spliced loci in the human CACNA1A, further studies have revealed a total of seven and nine alternative splice sites in human (Fig. 5.1) and rat cerebellum, respectively [32, 33]. However, between human and rat cerebellum, there are only five common splice loci, some of which we will examine in greater detail.
2.3 Exon 31
Exon 31 encodes for the NP insert in the extracellular loop of CaV2.1 domain IV S3–S4 and inclusion of NP decreases CaV2.1 affinity for ω-Aga-IVA as well as slowing channel activation and deactivation kinetics [31, 34]. It is worth noting that NP is encoded by a 6 nucleotide mini-exon (AATCCG) flanked by GT/AG acceptor-donor sites which are nested within intron 31 of humans, which is different from that observed in the rat variant where inclusion of NP was due to an alternative 5′ splice donor site located at the 3′ end of exon 31 [31]. When examining splice variant distribution in a human cerebellum cDNA library, 95% of the splice variants examined contained the +NP variant [31]. However, when single-cell RT-PCR of rat Purkinje cells was performed, the majority of the CaV2.1 transcripts were found to lack exon 31, which agrees with the required concentration of ω-Aga-IVA needed to almost completely block Ca2+ channel currents in rat Purkinje cells [24]. One possible explanation as to why the results from the human cerebellar cDNA library and the single-cell RT PCR of rat Purkinje cells do not match could be due to the proportion of Purkinje cells to granule cells in the cerebellum, where the granule cells can outnumber the Purkinje cells by 100–300 times [35, 36]. A human cDNA library constructed from bulk cerebellar tissue would hence have a higher proportion of granule cell transcripts, possibly masking the exact transcript expression profile in Purkinje cells.
2.4 Exon 37
Exon 37, together with exon 36, encodes for a Ca2+ binding site, known as an EF-hand-like motif, comprising 29 amino acids [31, 37, 38]. The general EF-hand motif consists of an α-helix E, a linker region, and an α-helix F [39]. Exon 37 encodes for part of the linker region as well as the α-helix F region. Mutually exclusive splicing of exon 37 results in variants EFa and EFb [31, 33]. Both splice variants are highly similar, with only a substitution of 10 amino acids out of a region of 30 amino acids [31]. Electrophysiological characterization involving transient overexpression of splice variants in HEK 293 cells revealed that both splice variants possessed almost similar properties, with the exception of EFa being able to undergo Ca2+-dependent facilitation (CDF) and Ca2+-dependent inactivation (CDI) (both processes will be explored in greater detail later), while EFb was only able to undergo CDI [40]. Subsequent experiments involving single-channel recordings of the two splice variants showed that EFa, when in the CDF mode, had an increase in channel open probability as well as an increase in channel open duration. On the other hand, EFb was found to be locked in a normal gating mode [41]. How the differences in amino acid sequences between the two splice variants determine whether the channel is able to undergo CDF is still unknown, but chimeric channel analysis involving the EF-hand region and the pre-IQ-IQ domain of CaV2.1 and CaV1.3 as well as CaV2.2 showed that both the EF-hand region and the pre-IQ-IQ domain of CaV2.1 are required for eliciting CDF [42, 43].
While the physiological significance for the splice variants is not known, an unequal distribution of splice variants has been observed in the cerebellum, with EFa being the dominant splice variant expressed in adulthood [44, 45]. However, it was also observed in mice where EFb was the dominant variant from the embryonic stage up till P5, after which there was a developmental switch from P7 onward to an EFa dominant expression pattern in the cerebellum [45]. Coincidentally, the developmental switch observed in the cerebellum between P5 and P7 coincides with a time period where a climbing fiber (CF) is selectively strengthened, a process that is critical for proper cerebellar circuitry formation [46], hence suggesting that the developmental switch of the splice variants could be required for CF strengthening and proper formation of cerebellar circuitry.
Chronic reduction of network activity in rat primary hippocampal neuron cultures via toxin application resulted in the upregulation of EFa but not EFb mRNA, with the greatest increase observed at 24 hr. An increase in CaV2.1 protein expression was also observed following network deprivation, which was blocked when EFa was knocked down with miRNA, suggesting that neurons are able to control EFa and EFb splice variant levels in a homeostatic manner [47].
While the verdict is still open on the physiological significance of exon 37 splice variants, the evidence presented earlier seems to suggest that modulation of splice variant expression is activity dependent. To date, the splicing factors governing the expression of exon 37 splice variants are still unknown.
2.5 Exon 43/44
Alternative splicing of exons 43 and 44 gives rise to combinations where both exons can be present or absent in four combinations (±43/±44). Transcript scanning of a human cerebellum cDNA library showed that 43+/44+ splice variant was the most abundant (80–90% of total colonies counted), followed by 43+/44−, 43−/44+ and 43−/44− [33, 48]. Overexpression of the different splice variants in HEK 293 cells followed by electrophysiological characterization revealed that alternative splicing at exons 43 and 44 did not affect CDF. However, Ca2+ current amplitude and CDI were shown to be affected. CDI was the greatest in 43−/44−, while the other splice variant combinations had similar CDI values. 43−/44− splice variant had a Ca2+ current amplitude that was twofold larger than that of the 43+/44+ splice variant [33]. Given the increases in current amplitude and CDI, with CDI being affected by global increases in Ca2+, it was postulated that the various splice variants at this particular locus affect surface channel expression. Furthermore, the presence of exon 44 was required for binding to Rab3-interacting molecules (RIM), scaffolding proteins important for the anchoring of CaV2.1 to synaptic vesicles at the active zone. Disrupting binding of CaV2.1 to α-RIMs was found to result in a release of suppression of voltage-dependent inactivation (VDI), and hence, CaV2.1 splice variants lacking exon 44 were found to have a stronger VDI [48].
2.6 Exon 47
Addition of a pentanucleotide GGCAG at the start of exon 47 results in an in-frame translation of exon 47 to produce a long version of the C terminus (termed as 47), allowing for the insertion of a polyglutamine (polyQ) tract. On the other hand, omission of GGCAG in splice variants causes a frameshift, resulting in the generation of a stop codon near the beginning of exon 47, thus producing a shorter variant of the channel (Δ47) [33, 49]. Studies involving knock-in mouse models of the human splice variants at this particular locus show no change in the intrinsic electrophysiological properties of the calcium channel [50,51,52], although studies utilizing heterologous transient overexpression systems provided conflicting evidence [53,54,55]. This further highlights the need to study the effects of calcium channel mutations, specifically polyQ expansion discussed here, in a more physiological setting. While the basic properties of the calcium channel are not altered by alternative splicing, it must be noted that the longer splice variant containing an expanded polyglutamine tract is an underlying cause for spinocerebellar ataxia 6 (SCA6), which will be covered in greater detail in the later section subsequently concerning CaV2.1 channelopathies.
2.7 Modulation of Calcium Channels
2.7.1 Voltage-Dependent Inactivation (VDI)
VGCCs open in response to membrane depolarization, allowing for the influx of Ca2+ ions. However, as Ca2+ is an important second messenger for many molecular pathways in the cell, there exist feedback mechanisms such as VDI and Ca2+-dependent inactivation (CDI) to prevent unregulated and excessive Ca2+ entry.
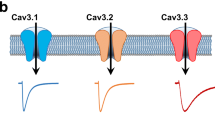
VDI is common across all VGCC subtypes, but the degree of VDI varies for individual subtypes and is greatly modulated in high voltage-activated (HVA) channels, such as CaV1 and CaV2, by CaVβ subunits [56, 57]. VDI has both fast and slow components to it, with fast inactivation occurring on a timescale of milliseconds, while slow inactivation is generally observed over a more prolonged membrane depolarization time frame (~1 min) and is not as well understood [58, 59]. Hence for this section, we will be focusing on fast VDI.
Generally, when HVA channels are co-expressed with β1b or β3 subunits, VDI is observed to be accelerated, while β4 is observed to not affect VDI by much and the inactivation kinetics are like that of α1 alone. However, when expressed with β2a, inactivation kinetics is significantly slowed down [27, 60].
To study VDI on its own, Ba2+ is used as the charge carrier instead of Ca2+ to avoid evoking Ca2+-dependent inactivation [61]. The earliest attempt to uncover structural determinants of calcium channel inactivation involved chimeric channels produced from rat CaV2.1 and marine ray CaV2.3. Subsequent electrophysiological analysis of the chimeric channel showed that differences in domain IS6 of CaV2.1 and CaV2.3 were the reason for the difference in inactivation kinetics between the two CaV2 subtypes [62]. Further evidence for the importance of S6 segment to VDI came from studies where the S6 segments of domain II or III of slowly inactivating CaV1.2 were swapped with the corresponding S6 segments of rapidly inactivating CaV2.3, transforming CaV1.2 to a rapidly inactivating phenotype [63]. Additionally, mutations in IIS6 and IVS6 regions of CaV2.1 in familial hemiplegic migraine 1 (FHM1) patients resulted in altered inactivation kinetics [64, 65]. Introduced point mutations in IIS6, IIIS6, and IVS6 of L-type calcium channels were also found to underlie an increase in inactivation kinetics [66,67,68]. One other compelling piece of evidence for S6 to be critical for VDI comes from the G406R mutation in TS patients, as mentioned in the earlier section. G406 is at the end of IS6 segment, and mutation to the G406R results in a near-total abolishment of VDI [69]. These studies thus support the notion that all four S6 regions of HVA channels are involved in VDI.
Apart from S6 segments of HVA channels being implicated in VDI, the intracellular loop linking domain I–II has been implicated in VDI [64, 68, 70, 71], leading some to propose the hinged-lid model as a molecular basis for VDI [72]. An alternative theory based on current kinetics and steady-state activation of CaV1.2 proposed that the calcium channel can exist in four different states, a closed resting state where the pore is closed and the voltage sensors lock the pore (R), an activated closed state where the pore is closed but the voltage sensors are in their “up” position (A), an activated open state where the pore is open and the voltage sensors are in their “up” position (O), and a deactivated open state where the pore is open but the voltage sensors are in their down position [73]. A recent review by Hering et al. [74] discusses this model in greater detail along with the recently discovered crystal structure of CaV1.1 [75, 76].
2.7.2 Ca2+-Dependent Inactivation (CDI)
CDI serves as a form of negative feedback regulation for VGCCs and was first discovered in Paramecium where it was observed that inactivation of VGCCs occurred at a faster rate in solutions containing Ca2+ than solutions containing Ba2+, and increased buffering of intracellular Ca2+ resulted in decreased CDI, suggesting that accumulation of intracellular Ca2+ is required for CDI [77, 78]. This was also supported by the observation that CDI has a U-shaped dependency on voltage, a very telling sign of a Ca2+-regulated process [79]. However, the extent to which Ca2+ chelators affect CDI differs between CaVα subunits and will be explored further subsequently.
To study CDI, a double-voltage pulse protocol is used where a prepulse voltage step to various potentials is delivered, and a test pulse of a fixed voltage is delivered after a brief pause [77]. The difference between the remaining current of Ba2+ and Ca2+ after a stipulated duration is taken to be a measure of pure CDI. [80] It must however be noted that for channels exhibiting faster inactivation kinetics such as CaV1 channels, shorter depolarizing pulses, and consequently a shorter index r will be used [81].
Advances in experimental techniques allowed for the isolation and recording of Ca2+ currents in both multicellular and single myocytes, revealing the existence of CDI [82,83,84]. Single-channel recordings of an L-type calcium channel from an adult rat cardiac myocyte revealed that Ca2+ influx of a single channel was sufficient for CDI to occur [80]. However, while it was agreed that Ca2+ influx through the calcium channel was responsible for providing negative feedback, the mechanism by which it exerted its effects was then still largely unknown. Identification of an EF-hand Ca2+ binding motif in the C-terminal region of CaV1.2 [38] gave rise to the possibility that the binding of Ca2+ to this region could be responsible for the initiation of CDI. Chimeric channel studies involving CaV1.2 (observed to have strong CDI) and CaV2.3 (observed to have little CDI) helped to provide the first evidence for the EF-hand motif to be involved in CDI. When the C-terminal region of CaV2.3 and CaV1.2 were swapped, it resulted in CaV1.2 exhibiting weak CDI and CaV2.3 exhibiting strong CDI [85]. These results implied that the proximal third of the carboxyl terminal (CI region) as well as the EF-hand motif within this region were integral to CDI. Subsequent studies utilizing point mutations in the critical residues within the EF-hand region required for Ca2+ binding were unable to completely eliminate CDI, suggesting that the Ca2+ sensor may reside somewhere else within the CI region [86, 87].
Calmodulin (CaM), a Ca2+ binding protein, is a ubiquitously expressed cytoplasmic protein and is involved in many Ca2+-related processes. Downstream of the EF-hand region is an IQ CaM-binding motif that was shown to be essential for CDI [88]. Coexpression of mutant CaM that was unable to bind Ca2+ along with CaV1.2 resulted in ablation of CDI, confirming the role of CaM as a Ca2+-sensor in initiating CDI of L-type calcium channels. Glutathione S-transferase (GST) pulldown experiments involving GST fusion proteins with various regions of CaV1.2 CI region confirmed that the IQ domain in CaV1.2 is the site for CaM interaction [89]. GST pulldown experiments also demonstrated that the IQ domains of CaV2 family were able to interact with CaM in a Ca2+-dependent manner. Further evidence for CaM being the Ca2+ sensor for VGCCs came from studies where Ca2+-free CaM (apoCaM) being pre-associated with the α1-subunit were reported [90,91,92].
Using the C-terminus of the rat CaV2.1 α1-subunit as bait, a yeast two-hybrid screen of a rat brain cDNA library identified CaM to be interacting with the C-terminus. When low Ca2+ buffering conditions were used (0.5 mM EGTA), CDI of CaV2.1 channels was observed [93]. On the other hand, under high Ca2+ buffering conditions (10 mM EGTA), CDI was not observed in transfected cells [81, 94], suggesting that CDI in CaV2.1 is dependent on global increases in Ca2+. This hypothesis was later confirmed with recombinant mutant CaM co-expression with CaV2.1 in HEK 293 cells, where it was observed that Ca2+ binding to the N-lobe of CaM (sensitive to global increases in Ca2+) was responsible for CDI [81, 95]. This is in contrast to CDI of CaV1.2, where CDI was observed even in high Ca2+ buffering conditions and even at single-channel level [96], demonstrating that CDI in CaV1.2 is dependent on local increases in Ca2+ near the channel pore. In this initial study demonstrating the importance of CaM to Ca2+ regulation of CaV2.1 channels, a site downstream of the IQ-like motif, calmodulin-binding domain (CBD), was thought to be vital for CaM binding and consequently Ca2+ regulation of the channel [93, 94, 97]. However, subsequent studies have called the importance of this binding site into question, where deletion of CBD was found to have no effect on CDI [44, 81]. However, there is consensus for the importance of the IQ-like motif for CDI of CaV2.1 channels to occur [43, 81, 97, 98].
While the abovementioned lines of evidence present a common mechanism by which VGCCs are Ca2+ regulated, the IQ domain, discovery of another site for CaM binding in CaV1.2/1.3 but not CaV2 channels adds another layer of control to Ca2+ regulation of VGCCs. Given that C-lobe of CaM has a stronger binding affinity to Ca2+, it has always been traditionally viewed that local increases in Ca2+ drive CaM C-lobe mediated processes, while global increases in Ca2+ were thought to only drive CaM N-lobe mediated processes [95, 99]. A chimeric channel consisting of the N-terminus of CaV1.2 and CaV2.2 was found to demonstrate strong CDI even in the presence of strong Ca2+ buffering. Likewise, when the N-terminus of CaV1.2 was substituted in CaV2.1, CDI was observed under strong buffering conditions, demonstrating CDI driven by local Ca2+ increase, unlike the usual CDI driven by the global increase in Ca2+ in CaV2 channels [81, 100]. Subsequent alanine point mutations of the N-terminus combined with in situ FRET as well as electrophysiological experiments confirmed the existence of a CaM-binding element in the N-terminus of CaV1.2/1.3 which was subsequently named as NSCaTE [100]. NSCaTE was shown to bind to the N-lobe of Ca2+/CaM with a local Ca2+ sensitivity, resulting in CDI.
2.7.3 Ca2+-Dependent Facilitation (CDF)
On the flipside of CDI is Ca2+-dependent facilitation (CDF), a positive feedback regulatory mechanism of VGCCs where further Ca2+ entry is increased due to enhanced channel opening. CDF has been observed in CaV1.2, CaV1.3, CaV2.1, and CaV3 channels.
The common mechanism underlying CDF in CaV1.2/1.3 is through the actions of CaMKII [101, 102]. In CaV1.2, CaMKII becomes tethered to the α1 subunit near the IQ domain, where it is then able to be activated by Ca2+/CaM and subsequently phosphorylating the channel and inducing CDF [103, 104]. CaMKII also induces CDF in CaV1.2 by phosphorylating β2A, which when bound to CaV1.2 increases channel open probability, resulting in CDF [105,106,107].
Like CaV1.2, CDF of CaV1.3 is also dependent on CaMKII. However, when CaV1.3 and CaMKII were co-expressed in HEK 293T cells, no CDF was observed. Only when CaV1.3, CaMKII, and densin-180, a scaffolding protein that is highly expressed at excitatory synapses and CaMKII-interacting, was CDF elicited [108, 109]. In hippocampal neurons, a long duration form of CDF was found to be dependent on CaMKII and densin-180, and also functionally coupled to KCa3.1, an intermediate-conductance Ca2+-gated potassium channel that is thought to be important in regulating neuronal excitability [110].
CDF of CaV2.1 is widely studied in the Calyx of Held synapse, where Ca2+ currents are largely mediated by CaV2.1 channels [111]. At this synapse, when high-frequency depolarizations are applied, CDF followed by CDI is observed in CaV2.1 channel recordings [112]. Efforts to elucidate the molecular mechanisms underlying CDF came in the form of studies overexpressing recombinant CaV2.1 where it was discovered that like CDI, CDF is also dependent on CaM binding to the IQ domain of CaV2.1 [81, 93, 94]. As mentioned earlier, the N-lobe of CaM detects increases in global Ca2+ and induces CDI in CaV2.1 channels. The binding of Ca2+ to the C-lobe of CaM is largely triggered by local Ca2+ increase and results in CDF [81], with single-channel recordings confirming the local Ca2+ sensitivity of CaM in inducing CDF [41]. In L-type channels, binding of Ca2+ to the C-lobe of CaM results in CDI while in CaV2.1, CDF is evoked. How is it possible that binding to the same C-lobe results in opposite Ca2+ regulation? Crystal structures of Ca2+/CaM bound to the IQ peptide of CaV2.1 channels revealed that CaM is able to exist in both parallel and antiparallel conformations [43, 98]. The ability of the C-lobe of CaM to bind in an antiparallel conformation upstream of the IQ domain in CaV2.1, as opposed to a parallel conformation for L-type channels, led to the proposition that this difference in binding conformation underlies the difference in CDF or CDI [98]. Structural analysis of the Ca2+/CaM-CaV2.1 complex along with alanine scanning mutagenesis and chimeric channel experiments suggested that differences in CaM C-lobe mediated effects could be due to differences in multiple interactions with binding sites within and upstream of the IQ domain. Chimeric channel experiments pointed to an important role for the EF-hand domain, preIQ-domain, and the IQ domain for CDF to occur, as substitution of any of the abovementioned regions with the corresponding region from CaV1.3 resulted in a decrease in facilitation [43]. Coincidentally, a recent chimeric channel experiment involving CaV2.1 and CaV2.2 also demonstrated the importance of these three domains [42]. Furthermore, alternative splicing of exon 37 of CaV2.1 results in mutually exclusive splice variants, of which one preserves CDF while the other splice variant does not support CDF [40].
These studies, while mainly centered on the IQ-domain as being critical to Ca2+/CaM regulation of VGCC, also demonstrate the importance of other regions in the vicinity of the IQ-domain, which will be important to consider when investigating the effects of Ca2+/CaM-mediated regulation.
2.7.4 CaV2.1 Channelopathies
Human mutations in CaV2.1 α1-subunit result in several neurological disorders in an autosomal-dominant inheritance fashion, such as episodic ataxia type 2 (EA2), familial hemiplegic migraine type 1 (FHM1), and spinocerebellar ataxia type 6 (SCA6) [49, 113]. It must be noted that with advances in RNA sequencing, changes in alternative splicing of CaV2.1 have been implicated in psychiatric disorders such as autism spectrum disorder (ASD) [114, 115].
2.8 Episodic Ataxia Type 2 (EA2)
EA2 is a neurological disorder that commonly affects patients in their childhood and is characterized by paroxysmal attacks of ataxia, vertigo, nausea, and may be accompanied by migraine. Symptoms may last from minutes to days. Emotional and physical stress as well as caffeine and alcohol may trigger attacks. In between attacks, EA2 patients may exhibit a progressive cerebellar syndrome with nystagmus as well as cerebellar atrophy in the vermis [116, 117]. Most of the EA2-related CACNA1A mutations reported disrupting the open reading frame resulting in a truncated channel. The EA2 mutations that do not affect the open reading frame are mainly located in the pore-forming loops of the channel [117, 118].
2.9 Familial Hemiplegic Migraine Type 1 (FHM1)
Clinically, patients with FHM1 exhibit hemiplegic migraines with an aura that might be accompanied by other symptoms such as nausea and ataxia and may last for hours to weeks. Some FHM1 patients exhibit permanent cerebellar symptoms comprising progressive cerebellar ataxia that might be accompanied by nystagmus [119, 120]. Mutations in CACNA1A have been identified as the underlying genetic cause of FHM1 [113]. The majority of the FHM1 mutations in CACNA1A affect conserved amino acid residues in critical functional regions of CaV2.1 such as the pore-lining loop as well as the S4 voltage sensors (see [121, 122] for reviews and references). The functional changes brought about by the FHM1 mutations have been probed in heterologous expression systems and reveal that the mutations bring about a gain-of-function where there is increased Ca2+ influx as a result of increased channel open probability and a decrease in voltage activation of the channel [123,124,125]. A similar result was also observed in knock-in mouse models of R192Q and S218L mice, where there was a larger CaV.2.1 current density in cerebellar granule cells despite no change in membrane expression of functional CaV2.1 channels [126, 127].
Interestingly, alternative splicing of CACNA1A at exon 47 affects the impact of FHM1 mutations on the channel kinetics. Using three FHM1 mutations, R192Q, S218L, and K1336E, expressed in a CaV2.1 (+47) and CaV2.1 (Δ47) background, it was shown that the FHM1 mutations result in different biophysical changes in channel properties depending on which splice variant the mutations are expressed in. Depending on the proportion of splice variants expressed in various neuronal subtypes, the same FHM1 mutations could result in varying degrees of symptoms [128].
2.10 Spinocerebellar Ataxia Type 6 (SCA6)
SCA6 is a polyglutamine disease caused by expansion of the trinucleotide (CAG) repeat in exon 47 of the CACNA1A gene, with longer expansions resulting in earlier onset of the disease [129]. SCA6 patients have a late onset of mild but slowly progressive cerebellar ataxia affecting the limbs and gait as well as slight vibratory and proprioceptive sensory loss and may be accompanied by nystagmus and dysarthria. Postmortem examination of the cerebellum revealed a severe loss of Purkinje cells particularly in the vermis, moderate loss of granule cells, dentate nucleus neurons as well as neuronal loss in the inferior olive [49, 130]. In situ hybridization with probes for detecting exons 46–47 of human CACNA1A mRNA as well as RT-PCR showed that Purkinje cells had the highest expression of CaV2.1 protein with an expanded polyglutamine tract and partially explains the selective neurodegeneration observed in the cerebellum of SCA6 patients [131]. Unlike most polyglutamine diseases, SCA6 rarely results in intranuclear inclusions but instead, cytoplasmic aggregates are more commonly observed and were found to be sufficient to result in cell death [132, 133]. It was initially thought that the polyglutamine expansion of CaV2.1 would affect channel function and subsequently result in cell death [53,54,55]. However, as discussed earlier, the knockin mouse models of SCA6 showed no differences in CaV2.1 channel kinetics in cerebellar Purkinje cells [50,51,52].
Apart from its channel function, another interesting role for CaV2.1 was discovered. Similar to the C-terminal fragment of L-type channels translocating to the nucleus and functioning as a transcription factor [134], a 75 kDA C-terminal fragment of CaV2.1 (α1ACT) was found in the nucleus of Purkinje cells and was found to be toxic when the fragment contained the SCA6 polyglutamine expansion [135]. CACNA1A was later found to be bicistronic, with an internal ribosomal entry site (IRES) encoding for α1ACT that also served as a transcription factor for a number of genes found to be important for proper Purkinje cell and neural development. When α1ACT contained the SCA6 polyglutamine expansion, its normal gene expression regulation was abolished and resulted in increased cell death [136].
2.11 Psychiatric Disorders
Genome-wide association studies (GWAS) have uncovered a strong link between SNPs in CACNA1C and psychiatric disorders such as schizophrenia (SCZ), bipolar disorder, and major depressive disorder, which is not entirely unexpected given its high expression in affected brain regions such as the hippocampus [114, 137,138,139,140,141]. CaV2.1 was however not shown to be linked to any psychiatric disorders in the GWAS studies although some FHM1 and EA2 patients also presented with SCZ symptoms, difficulties in learning, and attention deficit disorder [142]. Interestingly, analysis of transcript isoforms from the PsychENCODE study showed changes in alternative splicing of CACNA1A in ASD [114].
3 Conclusion
In this chapter, we presented the varied roles in the body that VGCCs are involved in, from the heart to skeletal muscles and the brain. Given its importance, many mechanisms exist to modulate channel function, preventing excitotoxicity due to Ca2+ overload. Changes in splice isoforms have also been shown to alter channel kinetics and function and may be a way in which the cell modulates Ca2+ entry. Much is still unknown about the combinatorial effects of the splice variants as well as the splice factors responsible for the different splice variant expressions. More work will definitely be required if we wish to modulate VGCCs for therapeutic treatments.
References
Jeftinija DM et al (2007) The Ca(V) 1.2 Ca(2+) channel is expressed in sarcolemma of type I and IIa myofibers of adult skeletal muscle. Muscle Nerve 36:482–490. https://doi.org/10.1002/mus.20842
Takahashi M, Seagar MJ, Jones JF, Reber BF, Catterall WA (1987) Subunit structure of dihydropyridine-sensitive calcium channels from skeletal muscle. Proc Natl Acad Sci U S A 84:5478–5482. https://doi.org/10.1073/pnas.84.15.5478
Gez LS, Hagalili Y, Shainberg A, Atlas D (2012) Voltage-driven Ca(2+) binding at the L-type Ca(2+) channel triggers cardiac excitation-contraction coupling prior to Ca(2+) influx. Biochemistry 51:9658–9666. https://doi.org/10.1021/bi301124a
Buraei Z, Yang J (2013) Structure and function of the β subunit of voltage-gated Ca2+ channels. Biochim Biophys Acta (BBA) – Biomembr 1828:1530–1540. https://doi.org/10.1016/j.bbamem.2012.08.028
Hidalgo P, Gonzalez-Gutierrez G, Garcia-Olivares J, Neely A (2006) The alpha1-beta-subunit interaction that modulates calcium channel activity is reversible and requires a competent alpha-interaction domain. J Biol Chem 281:24104–24110. https://doi.org/10.1074/jbc.M605930200
Hu Z et al (2018) Regulation of blood pressure by targeting CaV1.2-Galectin-1 protein interaction. Circulation 138:1431–1445. https://doi.org/10.1161/circulationaha.117.031231
Mangoni ME et al (2003) Functional role of L-type Cav1.3 Ca2+ channels in cardiac pacemaker activity. Proc Natl Acad Sci U S A 100:5543–5548. https://doi.org/10.1073/pnas.0935295100
Barrett CF, Tsien RW (2008) The Timothy syndrome mutation differentially affects voltage- and calcium-dependent inactivation of CaV1.2 L-type calcium channels. Proc Natl Acad Sci U S A 105:2157–2162. https://doi.org/10.1073/pnas.0710501105
Splawski I et al (2005) Severe arrhythmia disorder caused by cardiac L-type calcium channel mutations. Proc Natl Acad Sci U S A 102:8089–8096.; discussion 8086-8088. https://doi.org/10.1073/pnas.0502506102
Antzelevitch C et al (2007) Loss-of-function mutations in the cardiac calcium channel underlie a new clinical entity characterized by ST-segment elevation, short QT intervals, and sudden cardiac death. Circulation 115:442–449. https://doi.org/10.1161/circulationaha.106.668392
Simms BA, Zamponi GW (2012) The Brugada syndrome mutation A39V does not affect surface expression of neuronal rat Cav1.2 channels. Mol Brain 5:9. https://doi.org/10.1186/1756-6606-5-9
Baig SM et al (2011) Loss of Ca(v)1.3 (CACNA1D) function in a human channelopathy with bradycardia and congenital deafness. Nat Neurosci 14:77–84. https://doi.org/10.1038/nn.2694
Loh KWZ, Liang MC, Soong TW, Hu Z (2020) Regulation of cardiovascular calcium channel activity by post-translational modifications or interacting proteins. Pflügers Arch: Eur J Physiol. https://doi.org/10.1007/s00424-020-02398-x
Patriarchi T et al (2016) Phosphorylation of Cav1.2 on S1928 uncouples the L-type Ca2+ channel from the β2 adrenergic receptor. EMBO J 35:1330–1345. https://doi.org/10.15252/embj.201593409
Lerner M et al (2007) The RBCC gene RFP2 (Leu5) encodes a novel transmembrane E3 ubiquitin ligase involved in ERAD. Mol Biol Cell 18:1670–1682. https://doi.org/10.1091/mbc.e06-03-0248
Mori Y et al (1991) Primary structure and functional expression from complementary DNA of a brain calcium channel. Nature 350:398–402. https://doi.org/10.1038/350398a0
Dubel SJ et al (1992) Molecular cloning of the alpha-1 subunit of an omega-conotoxin-sensitive calcium channel. Proc Natl Acad Sci U S A 89:5058–5062. https://doi.org/10.1073/pnas.89.11.5058
Williams ME et al (1992) Structure and functional expression of alpha 1, alpha 2, and beta subunits of a novel human neuronal calcium channel subtype. Neuron 8:71–84. https://doi.org/10.1016/0896-6273(92)90109-q
Llinas R, Sugimori M, Lin JW, Cherksey B (1989) Blocking and isolation of a calcium channel from neurons in mammals and cephalopods utilizing a toxin fraction (FTX) from funnel-web spider poison. Proc Natl Acad Sci U S A 86:1689–1693. https://doi.org/10.1073/pnas.86.5.1689
Llinas RR, Sugimori M, Cherksey B (1989) Voltage-dependent calcium conductances in mammalian neurons. The P channel. Ann N Y Acad Sci 560:103–111. https://doi.org/10.1111/j.1749-6632.1989.tb24084.x
Randall A, Tsien RW (1995) Pharmacological dissection of multiple types of Ca2+ channel currents in rat cerebellar granule neurons. J Neurosci 15:2995–3012
Wheeler DB, Randall A, Tsien RW (1994) Roles of N-type and Q-type Ca2+ channels in supporting hippocampal synaptic transmission. Science 264:107–111. https://doi.org/10.1126/science.7832825
Hillman D et al (1991) Localization of P-type calcium channels in the central nervous system. Proc Natl Acad Sci U S A 88:7076–7080. https://doi.org/10.1073/pnas.88.16.7076
Mintz IM et al (1992) P-type calcium channels blocked by the spider toxin omega-Aga-IVA. Nature 355:827–829. https://doi.org/10.1038/355827a0
Usowicz MM, Sugimori M, Cherksey B, Llinas R (1992) P-type calcium channels in the somata and dendrites of adult cerebellar Purkinje cells. Neuron 9:1185–1199. https://doi.org/10.1016/0896-6273(92)90076-p
Starr TV, Prystay W, Snutch TP (1991) Primary structure of a calcium channel that is highly expressed in the rat cerebellum. Proc Natl Acad Sci U S A 88:5621–5625. https://doi.org/10.1073/pnas.88.13.5621
Stea A et al (1994) Localization and functional properties of a rat brain alpha 1A calcium channel reflect similarities to neuronal Q- and P-type channels. Proc Natl Acad Sci U S A 91:10576–10580. https://doi.org/10.1073/pnas.91.22.10576
Snutch TP, Reiner PB (1992) Ca2+ channels: diversity of form and function. Curr Opin Neurobiol 2:247–253. https://doi.org/10.1016/0959-4388(92)90111-w
Tsien RW, Ellinor PT, Horne WA (1991) Molecular diversity of voltage-dependent Ca2+ channels. Trends Pharmacol Sci 12:349–354. https://doi.org/10.1016/0165-6147(91)90595-j
Mermelstein PG et al (1999) Properties of Q-type calcium channels in neostriatal and cortical neurons are correlated with beta subunit expression. J Neurosci 19:7268–7277
Bourinet E et al (1999) Splicing of alpha 1A subunit gene generates phenotypic variants of P- and Q-type calcium channels. Nat Neurosci 2:407–415. https://doi.org/10.1038/8070
Kanumilli S et al (2006) Alternative splicing generates a smaller assortment of CaV2.1 transcripts in cerebellar Purkinje cells than in the cerebellum. Physiol Genomics 24:86–96. https://doi.org/10.1152/physiolgenomics.00149.2005
Soong TW et al (2002) Systematic identification of splice variants in human P/Q-type channel alpha1(2.1) subunits: implications for current density and Ca2+-dependent inactivation. J Neurosci 22:10142–10152
Hans M et al (1999) Structural elements in domain IV that influence biophysical and pharmacological properties of human alpha1A-containing high-voltage-activated calcium channels. Biophys J 76:1384–1400. https://doi.org/10.1016/S0006-3495(99)77300-5
Harvey RJ, Napper RM (1988) Quantitative study of granule and Purkinje cells in the cerebellar cortex of the rat. J Comp Neurol 274:151–157. https://doi.org/10.1002/cne.902740202
Wetts R, Herrup K (1983) Direct correlation between Purkinje and granule cell number in the cerebella of lurcher chimeras and wild-type mice. Brain Res 312:41–47. https://doi.org/10.1016/0165-3806(83)90119-0
Kretsinger RH (1976) Calcium-binding proteins. Ann Rev Biochem 45:239–266. https://doi.org/10.1146/annurev.bi.45.070176.001323
Babitch J (1990) Channel hands. Nature 346:321–322. https://doi.org/10.1038/346321b0
Kretsinger RH (2013) In: William J. Lennarz & M. Daniel Lane (Eds.), Encyclopedia of biological chemistry, 2nd ed., Academic Press, pp. 316–321.
Chaudhuri D et al (2004) Alternative splicing as a molecular switch for Ca2+/calmodulin-dependent facilitation of P/Q-type Ca2+ channels. J Neurosci 24:6334–6342. https://doi.org/10.1523/JNEUROSCI.1712-04.2004
Chaudhuri D, Issa JB, Yue DT (2007) Elementary mechanisms producing facilitation of Cav2.1 (P/Q-type) channels. J Gen Physiol 129:385–401. https://doi.org/10.1085/jgp.200709749
Thomas JR, Hagen J (2018) Soh, D. & Lee, A. Molecular moieties masking Ca(2+)-dependent facilitation of voltage-gated Cav2.2 Ca(2+) channels. J Gen Physiol 150:83–94. https://doi.org/10.1085/jgp.201711841
Mori MX, Vander Kooi CW, Leahy DJ, Yue DT (2008) Crystal structure of the CaV2 IQ domain in complex with Ca2+/calmodulin: high-resolution mechanistic implications for channel regulation by Ca2+. Structure 16:607–620. https://doi.org/10.1016/j.str.2008.01.011
Chaudhuri D, Alseikhan BA, Chang SY, Soong TW, Yue DT (2005) Developmental activation of calmodulin-dependent facilitation of cerebellar P-type Ca2+ current. J Neurosci 25:8282–8294. https://doi.org/10.1523/JNEUROSCI.2253-05.2005
Chang SY et al (2007) Age and gender-dependent alternative splicing of P/Q-type calcium channel EF-hand. Neuroscience 145:1026–1036. https://doi.org/10.1016/j.neuroscience.2006.12.054
Kano M, Watanabe T, Uesaka N, Watanabe M (2018) Multiple phases of climbing fiber synapse elimination in the developing cerebellum. Cerebellum 17:722–734. https://doi.org/10.1007/s12311-018-0964-z
Thalhammer A et al (2017) Alternative Splicing of P/Q-Type Ca(2+) Channels Shapes Presynaptic Plasticity. Cell Rep 20:333–343. https://doi.org/10.1016/j.celrep.2017.06.055
Hirano M et al (2017) C-terminal splice variants of P/Q-type Ca(2+) channel CaV2.1 alpha1 subunits are differentially regulated by Rab3-interacting molecule proteins. J Biol Chem 292:9365–9381. https://doi.org/10.1074/jbc.M117.778829
Zhuchenko O et al (1997) Autosomal dominant cerebellar ataxia (SCA6) associated with small polyglutamine expansions in the alpha 1A-voltage-dependent calcium channel. Nat Genet 15:62–69. https://doi.org/10.1038/ng0197-62
Watase K et al (2008) Spinocerebellar ataxia type 6 knockin mice develop a progressive neuronal dysfunction with age-dependent accumulation of mutant CaV2.1 channels. Proc Natl Acad Sci U S A 105:11987–11992. https://doi.org/10.1073/pnas.0804350105
Aikawa T et al (2017) Alternative splicing in the C-terminal tail of Cav2.1 is essential for preventing a neurological disease in mice. Hum Mol Genet 26:3094–3104. https://doi.org/10.1093/hmg/ddx193
Saegusa H et al (2007) Properties of human Cav2.1 channel with a spinocerebellar ataxia type 6 mutation expressed in Purkinje cells. Mol Cell Neurosci 34:261–270. https://doi.org/10.1016/j.mcn.2006.11.006
Matsuyama Z et al (1999) Direct alteration of the P/Q-type Ca2+ channel property by polyglutamine expansion in spinocerebellar ataxia 6. J Neurosci 19:RC14
Piedras-Renteria ES et al (2001) Increased expression of alpha 1A Ca2+ channel currents arising from expanded trinucleotide repeats in spinocerebellar ataxia type 6. J Neurosci 21:9185–9193
Toru S et al (2000) Spinocerebellar ataxia type 6 mutation alters P-type calcium channel function. J Biol Chem 275:10893–10898. https://doi.org/10.1074/jbc.275.15.10893
Lacerda AE et al (1991) Normalization of current kinetics by interaction between the alpha 1 and beta subunits of the skeletal muscle dihydropyridine-sensitive Ca2+ channel. Nature 352:527–530. https://doi.org/10.1038/352527a0
Varadi G, Lory P, Schultz D, Varadi M, Schwartz A (1991) Acceleration of activation and inactivation by the beta subunit of the skeletal muscle calcium channel. Nature 352:159–162. https://doi.org/10.1038/352159a0
Sokolov S, Weiss RG, Timin EN, Hering S (2000) Modulation of slow inactivation in class A Ca2+ channels by beta-subunits. J Physiol 527(Pt 3):445–454. https://doi.org/10.1111/j.1469-7793.2000.t01-1-00445.x
Shi C, Soldatov NM (2002) Molecular determinants of voltage-dependent slow inactivation of the Ca2+ channel. J Biol Chem 277:6813–6821. https://doi.org/10.1074/jbc.M110524200
Isom LL, De Jongh KS, Catterall WA (1994) Auxiliary subunits of voltage-gated ion channels. Neuron 12:1183–1194. https://doi.org/10.1016/0896-6273(94)90436-7
Eckert R, Chad JE (1984) Inactivation of Ca channels. Prog Biophys Mol Biol 44:215–267. https://doi.org/10.1016/0079-6107(84)90009-9
Zhang JF, Ellinor PT, Aldrich RW, Tsien RW (1994) Molecular determinants of voltage-dependent inactivation in calcium channels. Nature 372:97–100. https://doi.org/10.1038/372097a0
Stotz SC, Hamid J, Spaetgens RL, Jarvis SE, Zamponi GW (2000) Fast inactivation of voltage-dependent calcium channels. A hinged-lid mechanism? J Biol Chem 275:24575–24582. https://doi.org/10.1074/jbc.M000399200
Kraus RL, Sinnegger MJ, Glossmann H, Hering S, Striessnig J (1998) Familial hemiplegic migraine mutations change alpha1A Ca2+ channel kinetics. J Biol Chem 273:5586–5590. https://doi.org/10.1074/jbc.273.10.5586
Kraus RL et al (2000) Three new familial hemiplegic migraine mutants affect P/Q-type Ca(2+) channel kinetics. J Biol Chem 275:9239–9243. https://doi.org/10.1074/jbc.275.13.9239
Hering S et al (1996) Transfer of high sensitivity for benzothiazepines from L-type to class A (BI) calcium channels. J Biol Chem 271:24471–24475. https://doi.org/10.1074/jbc.271.40.24471
Hering S, Berjukow S, Aczel S, Timin EN (1998) Ca2+ channel block and inactivation: common molecular determinants. Trends Pharmacol Sci 19:439–443. https://doi.org/10.1016/s0165-6147(98)01258-9
Stotz SC, Zamponi GW (2001) Identification of inactivation determinants in the domain IIS6 region of high voltage-activated calcium channels. J Biol Chem 276:33001–33010. https://doi.org/10.1074/jbc.M104387200
Splawski I et al (2004) Ca(V)1.2 calcium channel dysfunction causes a multisystem disorder including arrhythmia and autism. Cell 119:19–31. https://doi.org/10.1016/j.cell.2004.09.011
Berrou L, Bernatchez G, Parent L (2001) Molecular determinants of inactivation within the I-II linker of alpha1E (CaV2.3) calcium channels. Biophys J 80:215–228. https://doi.org/10.1016/S0006-3495(01)76008-0
Herlitze S, Hockerman GH, Scheuer T, Catterall WA (1997) Molecular determinants of inactivation and G protein modulation in the intracellular loop connecting domains I and II of the calcium channel alpha1A subunit. Proc Natl Acad Sci U S A 94:1512–1516. https://doi.org/10.1073/pnas.94.4.1512
Stotz SC, Jarvis SE, Zamponi GW (2004) Functional roles of cytoplasmic loops and pore lining transmembrane helices in the voltage-dependent inactivation of HVA calcium channels. J Physiol 554:263–273. https://doi.org/10.1113/jphysiol.2003.047068
Beyl S et al (2009) Different pathways for activation and deactivation in CaV1.2: a minimal gating model. J Gen Physiol 134:231–241.; S231–232. https://doi.org/10.1085/jgp.200910272
Hering S et al (2018) Calcium channel gating. Pflugers Arch 470:1291–1309. https://doi.org/10.1007/s00424-018-2163-7
Wu J et al (2016) Structure of the voltage-gated calcium channel Ca(v)1.1 at 3.6 A resolution. Nature 537:191–196. https://doi.org/10.1038/nature19321
Wu J et al (2015) Structure of the voltage-gated calcium channel Cav1.1 complex. Science 350:aad2395. https://doi.org/10.1126/science.aad2395
Brehm P, Eckert R (1978) Calcium entry leads to inactivation of calcium channel in paramecium. Science 202:1203–1206. https://doi.org/10.1126/science.103199
Brehm P, Dunlap K, Eckert R (1978) Calcium-dependent repolarization in paramecium. J Physiol 274:639–654. https://doi.org/10.1113/jphysiol.1978.sp012171
Eckert R, Tillotson DL (1981) Calcium-mediated inactivation of the calcium conductance in caesium-loaded giant neurones of Aplysia californica. J Physiol 314:265–280. https://doi.org/10.1113/jphysiol.1981.sp013706
Imredy JP, Yue DT (1994) Mechanism of Ca(2+)-sensitive inactivation of L-type Ca2+ channels. Neuron 12:1301–1318. https://doi.org/10.1016/0896-6273(94)90446-4
DeMaria CD, Soong TW, Alseikhan BA, Alvania RS, Yue DT (2001) Calmodulin bifurcates the local Ca2+ signal that modulates P/Q-type Ca2+ channels. Nature 411:484–489. https://doi.org/10.1038/35078091
Kass RS, Sanguinetti MC (1984) Inactivation of calcium channel current in the calf cardiac Purkinje fiber. Evidence for voltage- and calcium-mediated mechanisms. J Gen Physiol 84:705–726. https://doi.org/10.1085/jgp.84.5.705
Mentrard D, Vassort G, Fischmeister R (1984) Calcium-mediated inactivation of the calcium conductance in cesium-loaded frog heart cells. J Gen Physiol 83:105–131. https://doi.org/10.1085/jgp.83.1.105
Lee KS, Marban E, Tsien RW (1985) Inactivation of calcium channels in mammalian heart cells: joint dependence on membrane potential and intracellular calcium. J Physiol 364:395–411. https://doi.org/10.1113/jphysiol.1985.sp015752
de Leon M et al (1995) Essential Ca(2+)-binding motif for Ca(2+)-sensitive inactivation of L-type Ca2+ channels. Science 270:1502–1506. https://doi.org/10.1126/science.270.5241.1502
Zhou J et al (1997) Feedback inhibition of Ca2+ channels by Ca2+ depends on a short sequence of the C terminus that does not include the Ca2+ -binding function of a motif with similarity to Ca2+ -binding domains. Proc Natl Acad Sci U S A 94:2301–2305. https://doi.org/10.1073/pnas.94.6.2301
Bernatchez G, Talwar D, Parent L (1998) Mutations in the EF-hand motif impair the inactivation of barium currents of the cardiac alpha1C channel. Biophys J 75:1727–1739. https://doi.org/10.1016/S0006-3495(98)77614-3
Zuhlke RD, Reuter H (1998) Ca2+-sensitive inactivation of L-type Ca2+ channels depends on multiple cytoplasmic amino acid sequences of the alpha1C subunit. Proc Natl Acad Sci U S A 95:3287–3294. https://doi.org/10.1073/pnas.95.6.3287
Peterson BZ, DeMaria CD, Adelman JP, Yue DT (1999) Calmodulin is the Ca2+ sensor for Ca2+ -dependent inactivation of L-type calcium channels. Neuron 22:549–558. https://doi.org/10.1016/s0896-6273(00)80709-6
Erickson MG, Alseikhan BA, Peterson BZ, Yue DT (2001) Preassociation of calmodulin with voltage-gated Ca(2+) channels revealed by FRET in single living cells. Neuron 31:973–985. https://doi.org/10.1016/s0896-6273(01)00438-x
Erickson MG, Liang H, Mori MX, Yue DT (2003) FRET two-hybrid mapping reveals function and location of L-type Ca2+ channel CaM preassociation. Neuron 39:97–107. https://doi.org/10.1016/s0896-6273(03)00395-7
Pitt GS et al (2001) Molecular basis of calmodulin tethering and Ca2+-dependent inactivation of L-type Ca2+ channels. J Biol Chem 276:30794–30802. https://doi.org/10.1074/jbc.M104959200
Lee A et al (1999) Ca2+/calmodulin binds to and modulates P/Q-type calcium channels. Nature 399:155–159. https://doi.org/10.1038/20194
Lee A, Scheuer T, Catterall WA (2000) Ca2+/calmodulin-dependent facilitation and inactivation of P/Q-type Ca2+ channels. J Neurosci 20:6830–6838
Liang H et al (2003) Unified mechanisms of Ca2+ regulation across the Ca2+ channel family. Neuron 39:951–960. https://doi.org/10.1016/s0896-6273(03)00560-9
Yue DT, Backx PH, Imredy JP (1990) Calcium-sensitive inactivation in the gating of single calcium channels. Science 250:1735–1738. https://doi.org/10.1126/science.2176745
Lee A, Zhou H, Scheuer T, Catterall WA (2003) Molecular determinants of Ca(2+)/calmodulin-dependent regulation of Ca(v)2.1 channels. Proc Natl Acad Sci U S A 100:16059–16064. https://doi.org/10.1073/pnas.2237000100
Kim EY et al (2008) Structures of CaV2 Ca2+/CaM-IQ domain complexes reveal binding modes that underlie calcium-dependent inactivation and facilitation. Structure 16:1455–1467. https://doi.org/10.1016/j.str.2008.07.010
Dunlap K (2007) Calcium channels are models of self-control. J Gen Physiol 129:379–383. https://doi.org/10.1085/jgp.200709786
Dick IE et al (2008) A modular switch for spatial Ca2+ selectivity in the calmodulin regulation of CaV channels. Nature 451:830–834. https://doi.org/10.1038/nature06529
Zuhlke RD, Pitt GS, Deisseroth K, Tsien RW, Reuter H (1999) Calmodulin supports both inactivation and facilitation of L-type calcium channels. Nature 399:159–162. https://doi.org/10.1038/20200
Dzhura I, Wu Y, Colbran RJ, Balser JR, Anderson ME (2000) Calmodulin kinase determines calcium-dependent facilitation of L-type calcium channels. Nat Cell Biol 2:173–177. https://doi.org/10.1038/35004052
Hudmon A et al (2005) CaMKII tethers to L-type Ca2+ channels, establishing a local and dedicated integrator of Ca2+ signals for facilitation. J Cell Biol 171:537–547. https://doi.org/10.1083/jcb.200505155
Lee TS et al (2006) Calmodulin kinase II is involved in voltage-dependent facilitation of the L-type Cav1.2 calcium channel: Identification of the phosphorylation sites. J Biol Chem 281:25560–25567. https://doi.org/10.1074/jbc.M508661200
Abiria SA, Colbran RJ (2010) CaMKII associates with CaV1.2 L-type calcium channels via selected beta subunits to enhance regulatory phosphorylation. J Neurochem 112:150–161. https://doi.org/10.1111/j.1471-4159.2009.06436.x
Koval OM et al (2010) CaV1.2 beta-subunit coordinates CaMKII-triggered cardiomyocyte death and afterdepolarizations. Proc Natl Acad Sci U S A 107:4996–5000. https://doi.org/10.1073/pnas.0913760107
Grueter CE, Abiria SA, Wu Y, Anderson ME, Colbran RJ (2008) Differential regulated interactions of calcium/calmodulin-dependent protein kinase II with isoforms of voltage-gated calcium channel beta subunits. Biochemistry 47:1760–1767. https://doi.org/10.1021/bi701755q
Walikonis RS et al (2001) Densin-180 forms a ternary complex with the (alpha)-subunit of Ca2+/calmodulin-dependent protein kinase II and (alpha)-actinin. J Neurosci 21:423–433
Strack S, Robison AJ, Bass MA, Colbran RJ (2000) Association of calcium/calmodulin-dependent kinase II with developmentally regulated splice variants of the postsynaptic density protein densin-180. J Biol Chem 275:25061–25064. https://doi.org/10.1074/jbc.C000319200
Sahu G, Asmara H, Zhang FX, Zamponi GW, Turner RW (2017) Activity-dependent facilitation of CaV1.3 calcium channels promotes KCa3.1 activation in hippocampal neurons. J Neurosci 37:11255–11270. https://doi.org/10.1523/JNEUROSCI.0967-17.2017
Forsythe ID, Tsujimoto T, Barnes-Davies M, Cuttle MF, Takahashi T (1998) Inactivation of presynaptic calcium current contributes to synaptic depression at a fast central synapse. Neuron 20:797–807. https://doi.org/10.1016/s0896-6273(00)81017-x
Borst JG, Sakmann B (1998) Facilitation of presynaptic calcium currents in the rat brainstem. J Physiol 513(Pt 1):149–155. https://doi.org/10.1111/j.1469-7793.1998.149by.x
Ophoff RA et al (1996) Familial hemiplegic migraine and episodic ataxia type-2 are caused by mutations in the Ca2+ channel gene CACNL1A4. Cell 87:543–552. https://doi.org/10.1016/s0092-8674(00)81373-2
Gandal MJ et al (2018) Transcriptome-wide isoform-level dysregulation in ASD, schizophrenia, and bipolar disorder. Science:362. https://doi.org/10.1126/science.aat8127
Andrade A et al (2019) Genetic associations between voltage-gated calcium channels and psychiatric disorders. Int J Mol Sci:20. https://doi.org/10.3390/ijms20143537
Yue Q, Jen JC, Nelson SF, Baloh RW (1997) Progressive ataxia due to a missense mutation in a calcium-channel gene. Am J Hum Genet 61:1078–1087. https://doi.org/10.1086/301613
Jen J, Kim GW, Baloh RW (2004) Clinical spectrum of episodic ataxia type 2. Neurology 62:17–22. https://doi.org/10.1212/01.wnl.0000101675.61074.50
Jen JC et al (2007) Primary episodic ataxias: diagnosis, pathogenesis and treatment. Brain 130:2484–2493. https://doi.org/10.1093/brain/awm126
Ducros A et al (2001) The clinical spectrum of familial hemiplegic migraine associated with mutations in a neuronal calcium channel. N Engl J Med 345:17–24. https://doi.org/10.1056/NEJM200107053450103
Haan J et al (2005) Migraine genetics: An update. Curr Pain Headache Rep 9:213–220. https://doi.org/10.1007/s11916-005-0065-9
Pietrobon D (2010) CaV2.1 channelopathies. Pflugers Arch 460:375–393. https://doi.org/10.1007/s00424-010-0802-8
Russell MB, Ducros A (2011) Sporadic and familial hemiplegic migraine: pathophysiological mechanisms, clinical characteristics, diagnosis, and management. Lancet Neurol 10:457–470. https://doi.org/10.1016/S1474-4422(11)70048-5
Tottene A et al (2002) Familial hemiplegic migraine mutations increase Ca(2+) influx through single human CaV2.1 channels and decrease maximal CaV2.1 current density in neurons. Proc Natl Acad Sci U S A 99:13284–13289. https://doi.org/10.1073/pnas.192242399
Hans M et al (1999) Functional consequences of mutations in the human alpha1A calcium channel subunit linked to familial hemiplegic migraine. J Neurosci 19:1610–1619
Tottene A et al (2005) Specific kinetic alterations of human CaV2.1 calcium channels produced by mutation S218L causing familial hemiplegic migraine and delayed cerebral edema and coma after minor head trauma. J Biol Chem 280:17678–17686. https://doi.org/10.1074/jbc.M501110200
van den Maagdenberg AM et al (2010) High cortical spreading depression susceptibility and migraine-associated symptoms in Ca(v)2.1 S218L mice. Ann Neurol 67:85–98. https://doi.org/10.1002/ana.21815
van den Maagdenberg AM et al (2004) A Cacna1a knockin migraine mouse model with increased susceptibility to cortical spreading depression. Neuron 41:701–710. https://doi.org/10.1016/s0896-6273(04)00085-6
Adams PJ et al (2009) Ca(V)2.1 P/Q-type calcium channel alternative splicing affects the functional impact of familial hemiplegic migraine mutations: implications for calcium channelopathies. Channels (Austin) 3:110–121. https://doi.org/10.4161/chan.3.2.7932
Ishikawa K et al (1997) Japanese families with autosomal dominant pure cerebellar ataxia map to chromosome 19p13.1-p13.2 and are strongly associated with mild CAG expansions in the spinocerebellar ataxia type 6 gene in chromosome 19p13.1. Am J Hum Genet 61:336–346. https://doi.org/10.1086/514867
Yang Q et al (2000) Morphological Purkinje cell changes in spinocerebellar ataxia type 6. Acta Neuropathol 100:371–376. https://doi.org/10.1007/s004010000201
Ishikawa K et al (1999) Abundant expression and cytoplasmic aggregations of [alpha]1A voltage-dependent calcium channel protein associated with neurodegeneration in spinocerebellar ataxia type 6. Hum Mol Genet 8:1185–1193. https://doi.org/10.1093/hmg/8.7.1185
Ishiguro T et al (2010) The carboxy-terminal fragment of alpha(1A) calcium channel preferentially aggregates in the cytoplasm of human spinocerebellar ataxia type 6 Purkinje cells. Acta Neuropathol 119:447–464. https://doi.org/10.1007/s00401-009-0630-0
Takahashi M et al (2013) Cytoplasmic location of alpha1A voltage-gated calcium channel C-terminal fragment (Cav2.1-CTF) aggregate is sufficient to cause cell death. PLoS One 8:e50121. https://doi.org/10.1371/journal.pone.0050121
Gomez-Ospina N, Tsuruta F, Barreto-Chang O (2006) Hu, L. & Dolmetsch, R. The C terminus of the L-type voltage-gated calcium channel Ca(V)1.2 encodes a transcription factor. Cell 127:591–606. https://doi.org/10.1016/j.cell.2006.10.017
Kordasiewicz HB, Thompson RM, Clark HB, Gomez CM (2006) C-termini of P/Q-type Ca2+ channel alpha1A subunits translocate to nuclei and promote polyglutamine-mediated toxicity. Hum Mol Genet 15:1587–1599. https://doi.org/10.1093/hmg/ddl080
Du X et al (2013) Second cistron in CACNA1A gene encodes a transcription factor mediating cerebellar development and SCA6. Cell 154:118–133. https://doi.org/10.1016/j.cell.2013.05.059
Hamshere ML et al (2013) Genome-wide significant associations in schizophrenia to ITIH3/4, CACNA1C and SDCCAG8, and extensive replication of associations reported by the Schizophrenia PGC. Mol Psychiatry 18:708–712. https://doi.org/10.1038/mp.2012.67
Moskvina V et al (2009) Gene-wide analyses of genome-wide association data sets: evidence for multiple common risk alleles for schizophrenia and bipolar disorder and for overlap in genetic risk. Mol Psychiatry 14:252–260. https://doi.org/10.1038/mp.2008.133
Ripke S et al (2013) Genome-wide association analysis identifies 13 new risk loci for schizophrenia. Nat Genet 45:1150–1159. https://doi.org/10.1038/ng.2742
Cross-Disorder Group of the Psychiatric Genomics, C (2013) Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet 381:1371–1379. https://doi.org/10.1016/S0140-6736(12)62129-1
Green EK et al (2010) The bipolar disorder risk allele at CACNA1C also confers risk of recurrent major depression and of schizophrenia. Mol Psychiatry 15:1016–1022. https://doi.org/10.1038/mp.2009.49
Indelicato E et al (2019) The neuropsychiatric phenotype in CACNA1A mutations: a retrospective single center study and review of the literature. Eur J Neurol 26:66–e67. https://doi.org/10.1111/ene.13765
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Yeow, S.Q.Z., Loh, K.W.Z., Soong, T.W. (2021). Calcium Channel Splice Variants and Their Effects in Brain and Cardiovascular Function. In: Zhou, L. (eds) Ion Channels in Biophysics and Physiology. Advances in Experimental Medicine and Biology, vol 1349. Springer, Singapore. https://doi.org/10.1007/978-981-16-4254-8_5
Download citation
DOI: https://doi.org/10.1007/978-981-16-4254-8_5
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-4253-1
Online ISBN: 978-981-16-4254-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)