Abstract
Human life and sports are inseparable from the coordinated work of bones and muscles. For example, muscles pull bones to produce movement, and the complex interactions between various structures control human movement. Even at rest, the ingenious action of external forces such as bones, muscles, and gravity maintain the person’s spatial position and support all the soft tissues of the human body. This section briefly introduces the anatomical and mechanical characteristics of the human skeleton and muscular system, so that readers have a certain understanding of the anatomical knowledge of the musculoskeletal system, and lay a foundation for the modeling and simulation of the musculoskeletal system.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
1.1 Anatomy of the Musculoskeletal System
Human life and sports are inseparable from the coordinated work of bones and muscles. For example, muscles pull bones to produce movement, and the complex interactions between various structures control human movement. Even at rest, the ingenious action of external forces such as bones, muscles, and gravity maintain the person’s spatial position and support all the soft tissues of the human body. This section briefly introduces the anatomical and mechanical characteristics of the human skeleton and muscular system, so that readers have a certain understanding of the anatomical knowledge of the musculoskeletal system, and lay a foundation for the modeling and simulation of the musculoskeletal system.
1.1.1 Bone
1.1.1.1 Classification of Bones
According to the shape, bones can be divided into long bones, short bones, flat bones, and irregular bones. The long bones are long and tubular, distributed in the limbs of the human body, and divided into two ends. The body is also called the backbone, and the internal cavity is called the medullary cavity, which contains the bone marrow. The body surface consists of 1–2 blood vessel access holes, called nourishing holes. The expansion at both ends is called the epiphysis, and the adjacent part of the backbone and the epiphysis is called the metaphysis. When a person is young, a piece of cartilage is kept here, called epiphyseal cartilage. The epiphyseal cartilage cells continue to multiply and ossify, making bones continue to grow. After a person reaches adulthood, the epiphyseal cartilage will ossify, the backbone and the epiphysis will merge into one, leaving an epiphyseal line in between.
The short bones are cube-like, and are mostly distributed in groups in the firmly connected and flexible parts. They are mainly composed of cancellous bone, and are surrounded by a thin layer of compact bone. For example, the wrist bone at the wrist joint and the tarsal bone at the ankle are short bones.
The flat bones are in the shape of a plate and mainly constitute the walls of the cranial cavity, chest cavity and pelvis, such as the skull and ribs.
Irregular bones, such as vertebrae, have irregular shapes, so these bones are not easy to classify. The maxilla with cavity in the bone, the ischium, and the pubis that make up the pelvis are irregular bones.
1.1.1.2 Bone Structure
Bone is composed of bone, periosteum, and bone marrow.
Bone is composed of bone tissue, which is a supporting connective tissue composed of minerals and collagen fibers. The surface of each bone in the human body is covered by a layer of dense connective tissue, which is called periosteum. Bone tissue in the human body is divided into two types: cancellous bone and compact bone. The two types of bone tissues are produced and maintained by osteoblasts and osteoclasts. Under the action of these two types of cells, bones can obtain maximum strength with the smallest volume and weight.
-
Cancellous bone: Cancellous bone is spongy. It is a porous three-dimensional bone tissue formed by interlaced and arranged trabecular bones. It is mainly distributed inside the bone and filled with red marrow. Trabecular bones in cancellous bone are arranged along the stress direction during the formation and reconstruction. Similar to the scaffolds used in construction, the trabecular bones give the bones the greatest strength. The nutrition of cancellous bone comes from the outer layer of compact bone, and nutrients reach the cancellous bone area through the vascular system that forms the tube in the compact bone. With the advancement of image acquisition and image processing technology, through the reconstruction and analysis of the images obtained after the Micro-CT technology scans the bones, the microstructure parameters of the cancellous bone can be obtained (Table 1.1), so that the condition of bone quality is scientifically evaluated. This evaluation method is of great significance to the research of diseases such as osteoporosis.
-
Compact bone: The most obvious difference between compact bone and cancellous bone is that compact bone is much denser than cancellous bone. This is intuitive knowledge. Compact bone, also known as “bone compact,” has a dense texture, strong resistance to compression and distortion, and is mainly distributed in the outer layer of the bone, while cancellous bone is mainly distributed inside the bone. In compact bone, the bone plates are arranged in concentric circles, and the central Haval tube is surrounded by a small cavity. The Haval tube contains blood vessels and nerves. It is through these blood vessels that bone tissue can get nourishment. In addition, we can also see that some tree-like bony tubules are arranged radially centered on the Haval tube, and tiny blood vessels and nerve branches are distributed in the bony tubules to nourish the distant bone tissue.
Periosteum adheres tightly to the surface of the bone. It is a dense connective tissue membrane, which contains abundant blood vessels, nerves, and lymphatic vessels, so it plays an important role in the nutrition, regeneration, and sensation of bones (Fig. 1.1). Periosteum is divided into inner and outer layers. The outer layer is dense and the inner layer is loose. The inner layer of the periosteum has an important relationship with bone repair and regeneration. Once bone damage occurs, the osteogenic function of the periosteum is active, thereby promoting bone regeneration. When the periosteum is severely damaged, the bone regeneration function will be severely affected.
Bone marrow is the soft tissue that fills the bone marrow cavity and cancellous bone. It is divided into red bone marrow and yellow bone marrow. Red bone marrow contains red blood cells and other immature blood cells at different developmental stages, and is red. Red bone marrow has hematopoietic function, and the bone marrow of fetuses and infants is all red bone marrow. After the age of 5, the red bone marrow in the long bone backbone is replaced by adipose tissue to become yellow bone marrow. The yellow bone marrow has lost its hematopoietic ability, but in chronic excessive blood loss or severe anemia, the yellow bone marrow can be transformed into red bone marrow and the hematopoietic ability can be restored. The epiphyses of long bones such as vertebrae, iliac bones, ribs, sternum, and femurs are red bone marrow for life.
1.1.1.3 Human Bones
The human body has 206 bones, which can be divided into axial bones and appendage bones. For adults, there are 80 axial bones and 126 appendage bones (Fig. 1.2) [1].
The axial bones form the central part of the human body, consisting of trunk bones (51 pieces) and skull and related bones (29 pieces). The trunk bone includes 26 spine bones (24 vertebrae, 1 sacrum, 1 coccyx), 1 sternum, and 24 ribs (12 pairs), which are involved in the formation of the spine, pelvis, and bony contours. The skull bones include 8 skulls, 6 ossicles, and 14 facial skulls.
The appendage bones include 4 upper limb girdle bones, 60 free upper limb bones, 60 free lower limb bones, and 2 hip bones (which constitute the pelvis).
1.1.1.4 Bony Landmarks
Bony landmarks refer to bones in certain parts of the human body that form relatively obvious protrusions or depressions on the surface of the body. Because these features are often used for positioning and other functions in clinical practice, they are called bony markers. Important bony landmarks are the mastoid process, the seventh cervical spinous process, the sternum angle, acromion, the xiphoid process, and the greater trochanter of femur.
The mastoid is located below the outer ear, and there is a styloid mastoid on the front and inner side of the front edge of the root, and the facial nerve extends out of the skull. The back half of the deep face of the mastoid is a sigmoid groove.
The spinous process of the seventh cervical vertebra is located at the most prominent bulge on the back of the neck. It is easier to touch when the head is bent forward and is a sign of counting vertebrae.
The sternal angle refers to the forward lateral protrusion at the junction of the sternum stem and the sternum body. It is an important bony marker and a marker for counting ribs. The plane of the sternum angle is the dividing line of the upper and lower mediastinum.
The xiphoid process refers to the protrusion below the sternum, located between the costal arches on both sides. The intersection of the xiphoid process and the left costal arch is a common site for pericardiocentesis.
The acromion rises above the shoulder joint and is the highest point of the shoulder.
The greater trochanter refers to the protrusion of the outer upper part of the thigh. When flexing the hip, the line from the ischial tuberosity to the anterior superior iliac spine passes through the femoral trochanter.
The above lists only some of the important bony markers. Readers of other bony markers can refer to books on human anatomy.
1.1.2 Muscle
The muscles in the human body can be divided into skeletal muscle, cardiac muscle, and smooth muscle according to their function and structure. Since this section focuses on the anatomy of the musculoskeletal system, this chapter focuses on skeletal muscle. For the content of myocardium and smooth muscle, readers can refer to anatomy-related books.
1.1.2.1 Skeletal Muscle, Cardiac Muscle, and Smooth Muscle
Skeletal muscles are generally attached to bones and can contract with people’s will. Therefore, skeletal muscles are also called voluntary muscles and are mainly distributed in the trunk and limbs. Of course, there is also an involuntary contraction of skeletal muscles, such as reflexes.
The myocardium composes the wall of the heart and powers the pumping activities necessary for blood circulation, driving the circulatory system. The contraction of the myocardium is not dominated by consciousness. Its contraction requires electrical impulse stimulation. In addition, the conduction pathway ensures the synchronous contraction of myocardial fibers, making it functionally integrated.
Smooth muscle is mainly distributed in the walls of hollow organs, blood vessels, and respiratory tracts. Smooth muscle contracts slowly and steadily, and its contraction strength is weaker than that of skeletal muscle and cardiac muscle.
1.1.2.2 The Structure and Morphology of Skeletal Muscle
Each piece of skeletal muscle includes two parts: muscle belly and tendon. Muscle belly is mainly composed of muscle fibers, red and soft, and has the ability to contract. The tendon is mainly composed of collagen fiber bundles. It is white in color and has no contraction function, but the tendon is very strong and attached to the bone.
Muscles have various shapes, and can be divided into four types according to their appearance: long, short, flat, and orbicularis (Fig. 1.3). The long muscles are mainly distributed in the extremities, and are characterized by their ability to be significantly shortened during contraction, so they can produce large amounts of movement. Long muscles are also divided into many forms. The belly of some long muscles is divided into two or more parts by the intermediate tendon, such as the digastric muscle and rectus abdominis; some long muscles have more than two heads at the beginning and later synthesize a muscle abdominal, called biceps, triceps, or quadriceps. Short muscles are mostly distributed in the deep layer of the trunk, with a small contraction range. The flat muscles are mostly distributed in the chest and abdomen walls, which have the function of protecting internal organs and movement. The orbicularis muscle is mostly distributed around the foramen, composed of circular muscle fibers, which can close the foramen when contracted.
1.1.2.3 The Start, the Stop, the Distribution, and the Function of the Muscle
When the muscles contract, the two bones move closer or apart. One of the bones is relatively fixed while the other moves relatively. The attachment point of the muscle on the fixed bone is called the starting point, and the attachment point on the moving bone is called the end point. The starting point and ending point of the muscle on the bone are relatively speaking, and can be interchanged under certain conditions.
The way the muscles are distributed around the joints is more or less consistent with the motion axis of the joints, that is, at least two groups of muscles or muscle groups with opposite actions are arranged on the opposite side of a motion axis, antagonistic muscles. And two or more muscles that are distributed on the same side of a motion axis and have the same effect are called synergistic muscles. Under the action of synergistic muscles and antagonist muscles, joint flexion, extension, and other actions are completed.
1.1.2.4 Human Muscles
There are about 639 muscles in the body. The muscles of the whole body are composed of about 6 billion muscle fibers. Figures 1.4, 1.5, 1.6, 1.7, 1.8, 1.9, 1.10, 1.11, and 1.12 show the main skeletal muscles of the human body.
1.1.3 Joints
This part first briefly introduces the concepts of direct connection, indirect connection, joint movement, and several types of human joints. Next, we focus on the detailed anatomical features of the spine, knee joint, hip joint, and ankle joint, which are often concerned in the modeling and simulation of the human musculoskeletal system to facilitate readers’ reference in the process of modeling and simulation.
1.1.3.1 Direct Link and Indirect Link
In the human body, bones and bones are connected to form joints, and the way of connection is through fibrous connective tissue, cartilage, or bone. The different ways of connection between bones can be divided into two categories: direct connection and indirect connection.
Direct Connection
The direct connection is relatively strong, inactive, or slightly active. It can be divided into three types: fibrous connection, cartilage connection, and osseointegration. The fiber connection can be divided into two types: ligament connection and seam. Seams are continuous periosteal connections between bones, such as the seams between skulls (Fig. 1.13). Ligament connection refers to the connection between two bones through a cord-like or template-like fibrous connective tissue, such as the calf interosseous membrane (Fig. 1.14).
Cartilage connection refers to the connection between two bones by cartilage, which can be divided into hyaline cartilage union and fibrocartilage union. Cartilage connection has a larger range of motion than fibrous connection. The cartilage in the connection increases the flexibility of the frontal joint and can also allow slight movements, such as the connection between vertebral bodies. At the junction of the ribs and sternum, due to the existence of cartilage connection, the rib cage can be enlarged or reduced to facilitate breathing (Fig. 1.15). The cartilage connection also exists in the pubic symphysis. During human walking or running, the cartilage of the pelvis is slightly connected to make it look like a suspension system to cushion the movement.
Osseointegration refers to the connection of bone tissue between two bones, which is often formed by fibrous connection or ossification of hyaline cartilage. For example, the osseointegration between the ilium, pubis, and ischium of the pelvis.
Indirect Connection
Indirect connection is also called joint or synovial joint. Among several types of bone connection, indirect connection generally has greater mobility.
The joint is composed of articular surface, joint capsule, and joint cavity (Fig. 1.16). The articular surface is the contact surface of the related bones that participate in the formation of the joint. For the joint, it generally includes at least two articular surfaces, one concave and the other convex, the concave one is the joint socket, and the convex one is called the joint head. The articular surface is covered with articular cartilage. The outer layer of the joint capsule is a fibrous membrane, and the inner layer is a synovial membrane. The synovial membrane is rich in vascular networks, which can produce synovial fluid. It provides a liquid environment in the joint cavity, which can not only increase lubrication but also be used for the metabolism of articular cartilage. The joint cavity is a closed space formed by the synovial layer of the joint capsule and the articular surface, which contains synovial fluid and is under negative pressure, which has a certain effect on the stability of the joint.
The articular cartilage covering the articular surface can reduce friction during exercise, and the synovial fluid produced by the synovial layer can reduce friction and act as a mediator of metabolism. Ligaments can support the joint capsule and stabilize the joint.
1.1.3.2 Movement and Classification of Joints
Joint Movement
There are four types of joint movement including flexion and extension, contraction and extension, rotation, and circular rotation. The contraction and extension refer to the movement of the joints along the sagittal axis. For the contraction of the fingers and toes, artificially stipulate the movement of moving closer or apart with the middle finger and the second toe as the central axis. Circumferential rotation means that the upper end of the moving bone rotates in situ, while the lower end makes circular motions, such as shoulder joints and hip joints.
Classification of Joints
There are many types of joints, which can be classified according to the number of bones, or according to the way that one or more joints move at the same time. The commonly used joint classification is classified according to the number of joint motion axes. It can be divided into single-axis joints, double-axis joints, and multi-axis joints. Among them, single-axis joints can only move around one axis of motion, including two forms: flexion joints and axle joints. Biaxial joints also include the following two forms: elliptical joints and saddle joints. Multi-axis joints can move in multiple directions, including ball and socket joints and flat joints (sliding joints). The sketches of the above joints are listed in Fig. 1.17, please refer to the readers.
1.1.3.3 Spine
The Connection of the Spine
The spine is formed by the connection of 24 vertebrae, 1 sacrum, and 1 coccyx, forming the central axis of the human body.
The Connection of the Vertebrae
The vertebrae are connected by ligaments, cartilage, and synovial joints. Specifically, it can be divided into intervertebral body connection and intervertebral arch connection.
The connection between the vertebral bodies is connected by the intervertebral disc, the anterior longitudinal ligament, and the posterior longitudinal ligament (Fig. 1.18). Among them, the intervertebral disc is a fibrocartilage disc that connects two adjacent vertebral bodies. It is composed of a nucleus pulposus in the center and an annulus fibrosus in the surrounding part. The fibrous annulus is firmly connected to the upper and lower parts of each vertebral body, protecting and restricting the bulging of the nucleus pulposus to the surrounding. The thickness of the 23 intervertebral discs is different. The middle chest is thinner and the waist is the thickest. The thickness of the cervical intervertebral disc is in the middle of the two, and the thickness of the intervertebral disc varies with age.
The anterior longitudinal ligament starts from the anterior edge of the foramen magnum and reaches the first or second sacral vertebral body. The longitudinal fibers are firmly attached to the vertebral body and intervertebral disc, which can prevent excessive extension of the spine and forward prolapse of the intervertebral disc.
The posterior longitudinal ligament is located behind the vertebral body in the spinal canal. It starts from the axis and descends to the sacrum. It has the effect of restricting excessive flexion of the spine. The result is relatively loose with the vertebral body.
The intervertebral arch connection includes the vertebral arch, spinous process, the ligament connection between the transverse processes, and the synovial connection between the lower articular processes (Fig. 1.18). The ligaments involved include ligamentum flavum, supraspinous ligament, nape ligament, and interspinous ligament.
The Overall View and Movement of the Spine
The function of the spine is to protect the spinal cord and support the trunk. The spine of an adult male is about 70 cm long, and a female is about 60 cm long. Observing the spine from the side (Fig. 1.19), it can be found that there are four physical curvatures of the adult spine, of which the cervical curvature and lumbar curvature are forward convex, and the thoracic curvature and sacral curvature are kyphotic. And to reduce shocks is of great significance.
The spine has a large range of activities, and it can do flexion, extension, lateral flexion, and circular movement. However, the range of motion and the nature of motion of each part of the spine are different. In the neck, the intervertebral disc is thick and the joint capsule is loose, so the range of flexion, extension, and rotation is greater. The thoracic intervertebral disc is thin, and the articular surface of the articular process is in a coronal position, and the spinous process is in an imbricate shape. Under the restriction of these factors, the range of motion of the thoracic spine is small.
1.1.3.4 Hip Joint
The hip joint is composed of the acetabulum and the femoral head, and is a multiaxial ball and socket joint. The acetabular lip made of fibrocartilage is attached to the periphery of the acetabulum to increase the depth of the acetabulum. The transverse acetabular ligament closes the notch of the acetabulum, so that the half-moon-shaped acetabular articular surface expands into a ring shape, which can hold the femoral head tightly (Fig. 1.20).
The following ligaments are found mainly around the hip joint capsule:
-
Iliac ligament: This is the strongest ligament. It starts from the anterior and inferior iliac spine and passes through the front of the joint capsule in a herringbone shape to the intertrochanteric line. It can limit the overextension of the thigh, and it has a great effect on maintaining the human upright posture.
-
The femoral head ligament: It connects the femoral head fovea and the transverse acetabular ligament. It is wrapped by synovial membrane and contains blood vessels that nourish bone tissue.
-
Pubic ligament: From the suprapubic branch to the deep fusion between the anterior and inferior wall of the joint capsule and the ilium ligament, its function is to limit the abduction and pronation of the thigh.
-
Ischial ligament: It starts from the ischial body, fuses with the joint capsule obliquely outwards, and is attached to the root of the greater trochanter, which can limit the internal rotation of the thigh.
-
Annulus: It is the annular thickening of the deep fibers of the joint capsule around the femoral neck, which can restrain the femoral head from protruding outward.
1.1.3.5 Knee Joint
The knee joint is composed of the lower end of the femur, the upper end of the tibia and the patella. It is the largest and most complex joint in the human body (Fig. 1.21).
The joint capsule of the knee joint is very thin and loose, attached to the periphery of each joint surface, and there are ligaments around the joint capsule to strengthen the joint's stability. There are mainly the patellar ligament, fibular collateral ligament, tibial collateral ligament, popliteal oblique ligament, and cruciate knee ligament.
The knee cruciate ligament is divided into the anterior cruciate ligament and the posterior cruciate ligament (Fig. 1.22). The anterior cruciate ligament starts from the anterior medial side of the tibial intercondylar bulge, and the fibers are fan-shaped attached to the medial femoral condyle. The posterior cruciate ligament starts from the rear of the tibial intercondylar bulge and is attached to the lateral surface of the medial femoral condyle. The cruciate ligament of the knee firmly connects the femur and tibia, preventing the tibia from shifting forward and backward along the femur. The anterior cruciate ligament is most tense when the knee is extended, which prevents the tibia from moving forward. The posterior cruciate ligament is most tense when the knee is bent, which prevents the tibia from moving backward.
The meniscus are two meniscus-shaped fibrocartilage plates between the inner and outer condyles of the femur and the inner and outer condyles of the tibia. They are called the inner and outer meniscus respectively. The medial meniscus is larger and C-shaped, and the lateral meniscus is smaller and O-shaped.
1.1.3.6 Ankle
The ankle is also called the ankle joint (Fig. 1.23). The ankle joint is composed of the lower end of the tibia and the fibula, and the talus pulley. It is similar to a single-axis flexion joint, and its axis of rotation is variable during dorsiflexion or plantar flexion. The joint capsule of the ankle joint is attached to each joint. The front and back walls of the capsule are thin and loose. There are thickened and strengthened ligaments on both sides, namely the medial ligament and the lateral ligament (Fig. 1.24). The lateral ligament is composed of the discontinuous anterior talofibular ligament, calcaneofibular ligament, and posterior talofibular ligament. The three ligaments all originate from the lateral malleolus and stop at the talus and root bone forward, downward and backward respectively. All three ligaments are weak.
The ankle joint can do dorsiflexion (extension) and plantarflexion exercises. The talus pulley is wide in front and narrow at the back. When dorsiflexion, the front of the wider pulley is embedded in the joint socket, and the ankle joint is more stable. In plantar flexion, since the back of the narrow pulley enters the joint socket, although slight lateral movement can be done, the joint is actually not stable enough, so the ankle joint is often sprained when going down the stairs or down the mountain.
The tarsal bones and metatarsal bones connect to form an upward arch, called the arch of the foot (Fig. 1.25). The arch, muscles, and ligaments form a functionally inseparable complex. Traditionally, the arch of the foot is divided into a longitudinal arch in the front and rear directions, and a transverse arch in the inner and outer directions.
1.2 Introduction to Bone Tissue
1.2.1 Bone Structure
The bones can be divided into long bone, short bone, flat bone, and irregular bone based on different shapes. The bone, take long bone as an example, mainly includes the following parts (Fig. 1.26) [2]:
-
Diaphysis, a long cylindrical tube, is the main portion of the bone. It is hollow, forming a medullary cavity, which stores bone marrow. The hollow structure of the diaphysis not only ensures the strength but also reduces its mass.
-
Epiphyses are the proximal and distal ends of the bone. They are usually covered with articular cartilage and form articular surfaces to bear the load. They are bigger than the middle of bone to reduce the stress on the joint surface through more contact area.
-
Metaphysis is located between diaphysis and epiphysis. During the growth of bone, the cartilage at metaphysis lengthens the bone axially. When the bone stops growing, the cartilage ossifies, forming an epiphyseal line.
-
Compact bone and cancellous bone are composed of bone tissue. They are important research and description objects in modeling and simulation of musculoskeletal system. They will be introduced in detail later.
-
Articular cartilage is a thin layer of hyaline cartilage attached to the epiphysis of the joint (Fig. 1.1). The shape of articular cartilage is consistent with the surface of the attached bone. It reduces friction and the impact of joint during movement. Due to the lack of perichondrium and blood vessels, its repair ability is limited.
-
Periosteum is a connective tissue covering the surface of bone except the articular surface. It contains abundant blood vessels, nerves, and lymphatic vessels. Periosteum protects bones, assists in fracture healing, and provides attachment points for ligaments and tendons.
-
Endosteum is a membranous connective tissue attached to the surface of medullary cavity. It contains osteoblasts and osteoclasts, which promote bone repair and reconstruction.
-
Bone marrow is a soft tissue that fills the medullary cavity and cancellous bone space. Adult bone marrow is divided into red bone marrow and yellow bone marrow. Red bone marrow is mostly stored in the marrow cavity of long bone and the cancellous bone space of flat bone and irregular bone. It can produce red blood cells, platelets, and white blood cells. Yellow bone marrow is mainly adipose tissue, which stores energy.
1.2.2 Compact Bone
Compact bone is distributed on the surface of bone and covered with periosteum. Compact bone is hard, with strong pressure resistance and high density. The repeated arrangement of osteons forms compact bone. Each osteon consists of concentric lamellae arranged around a haversian canal. In long bones, these tube-like units are oriented in the same direction as the long axis of the bone.
The direction of osteon has great effect on the mechanical properties of compact bone. For example, the long bone, as a slender rod structure, is often subjected to bending deformation. The direction of the osteon at the shaft is parallel to the axial direction of the bone, which can significantly improve the bending resistance of the long bone and reduce the probability of fracture. The mechanical environment of bone is variable. For example, infants learn to walk, athletes long-term engaged in a specific project training will change the stress conditions of bone. As a result, the direction of the osteon will also change to adapt to the new mechanical environment.
1.2.3 Cancellous Bone
Cancellous bone is located in the interior of a bone, and does not contain osteons. It is composed of interlaced irregular trabecula with columnar or plate shape. The space between trabeculae contains bone marrow, containing rich blood vessels. Cancellous bone constitutes the main internal structure of long bone, short bone, flat bone, and irregular bone, such as the central area of epiphysis of long bone, as shown in Fig. 1.27.
Trabecular arrangement of cancellous bone seems to be less organized than that of compact bone. In fact, the direction of trabeculae is roughly consistent with the direction of bone stress, so the cancellous bone can ensure that the bone will not be damaged while conducting the force. Due to variability of stress direction in the area of cancellous bone, the structure of trabeculae is also complex. It remodels with the changes of mechanical environment, age, and disease (such as femoral head necrosis, osteoporosis), as shown in Fig. 1.28.
Cancellous bone is similar to the porous material in engineering structure, which has high strength and low density. Although the strength of cancellous bone is lower than that of compact bone, it significantly reduces the bone mass. Lightweight bone is conducive to the muscle to drive it. The interlaced trabeculae also provide adequate support and protection for the bone marrow.
1.2.4 Cells in the Bone
The cells in bone tissue include osteogenic cell, osteoblast, osteocyte, and osteoclast.
-
Osteogenic cells are stem cells derived from mesenchyme and are usually located in connective tissues such as bone marrow and endosteum. They proliferate and develop into osteoblasts by cell division.
-
Osteoblasts synthesize and secrete collagen fibers and other organic components of bone matrix, which is called osteoid. When they are surrounded by the osteoid, they become osteocytes. Osteoblasts are basophilic monocytes derived from osteogenic cell induced by bone morphogenetic protein. Osteoblasts cover the surface of developing or reconstructing bone in the form of monolayer cells. The content of osteoblasts is high in the bone of minors. In adult bone, osteoblasts are located on the surface of the endosteum and at the site of bone reconstruction.
-
Osteocytes are the main cells in bone tissue. They no longer undergo cell division and are mainly distributed between the adjacent bone plates or scattered in the bone plate. Osteocytes maintain daily metabolism of the bone tissue, such as the exchange of nutrients and wastes with the blood.
-
Osteoclasts are multinucleated cells formed by fusion of many mononuclear cells. They are mainly distributed in the resorption bays on the bone surface. On the side of osteoclasts towards the bone surface, there are ruffled borders. The ruffled borders and bone surfaces form a microenvironment, in which osteoclasts release lysosomal enzymes and acids to dissolve bone matrix.
1.2.5 Chemical Composition and Mechanical Properties of Bone
Bone is mainly composed of organic and inorganic substances. The main component of organic substances is collagen, which has very good mechanical strength. The collagen exists in many tissues of the human body, such as dermis, blood vessels, ligaments, tendons, and bones. There are stronger covalent bonds and cross-linking between collagen molecules in bone. Thus the chemical properties and structure of collagen fiber in bone are more stable. The space among collagen fibers provides location for the deposition of inorganic substances.
Minerals are inorganic components of bone, which are mainly composed of hydroxyapatite. Minerals first crystallize in tiny spaces of collagen fibers. When the gap is filled, minerals are deposited around the collagen fibers in the form of needle, plate, and rod crystals.
Bone could be regarded as a composite material composed of collagen fiber and hydroxyapatite. The young's modulus of hydroxyapatite along the axial direction may be compared with the Young's modulus of metal materials. The Young's modulus of bone (18 GPa in tension in human femur) is intermediate between that of hydroxyapatite and collagen, but its strength is higher than both [3]. Hydroxyapatite, like cement in reinforced concrete, is a brittle material with high strength but lower tensile strength, contributing the stiffness of bone. Collagen fibers, like steel bars in reinforced concrete, prevent material from brittle cracking, contributing to the toughness of bone. The proportion of inorganic and organic substances in bone changes with age and other factors. The ratio of organic substances to inorganic substance in adult bone is about 3:7 [1]. The proportion of the two in infancy bone is roughly the same. The bone of infant is more elastic, easily deformed, and not easy to fracture. The inorganic composition of the bone in the elderly is high, and the bone is brittle.
1.2.6 Bone Formation
Bone develops from embryonic mesenchyme. The initial shape and position of bone are determined by the distribution of mesenchymal in the form of membrane. Some bones ossify on the basis of membrane, which is called intramembranous ossification; others develop into cartilage first, and then ossification by cartilage, which is called endochondral ossification. Intramembranous ossification is the simpler of the two methods of bone formation. Typically, flat bones, such as the skull, are formed in this way. Most of the bones in the human body are formed by endochondral ossification [2].
1.2.7 Bone Reconstruction
Under the conditions of the growth and development, the disease recovery and the adaptation to the new mechanical environment, the bone reconstruction is the ongoing replacement of old bone tissue by new bone tissue. This process of bone remodeling involves the bone resorption and the bone deposition. During the process of bone resorption, osteoclasts adhere to the bone surface and form a relatively closed microenvironment around the ruffled borders. Osteoclasts release acidic liquid to dissolve inorganic substances in bone tissue, and release protease to dissolve collagen fibers and other organic substances. Osteoclasts phagocytize bone resorption products (proteins and minerals, etc.) into the cells through vesicles, and then excrete them through exocytosis from the side opposite to the ruffled borders. Finally, the products of bone resorption are diffused into adjacent capillaries. During the process of bone deposition, osteoblasts migrate to the area where osteogenesis is needed and secrete bone matrix, which is calcified to form new bone. The annual reconstruction rate of compact bone is about 4%, and that of cancellous bone is about 20% [2]. The rate of bone reconstruction in different parts of the same bone is also different. For example, the distal portion of femur is renewed every four months, while certain areas of femur shaft will not be completely renewed in the whole life cycle of humans [2].
Bone reconstruction makes the newly generated bone tissue adapt to the latest load intensity and form, and changes the shape of bone. From the tissue level, bone reconstruction also has its negative side. Trabecular perforation or loss may occur during the reconstruction of cancellous bone. Reconstruction of compact bone may increase bone porosity and decrease the thickness of the compact bone. All of these may decrease bone strength.
1.3 Biomechanics Theories About Musculoskeletal System
This section is aimed at introducing basic theories in the biomechanics simulation of the musculoskeletal system. It interprets the basic concepts of biomechanics, including stress, strain, displacement, strain energy density and constitutive relations of linear elasticity, hyperelasticity and viscoelasticity. Thus, it clarifies the basic principles of finite element simulation of biomechanics so that readers will understand the inherent mechanism and process while using commercial softwares for finite element analysis.
1.3.1 Concepts of Musculoskeletal Biomechanics
1.3.1.1 Stress
The growth, reconstruction, injury, and rehabilitation of tissues are closely related to the mechanical environment. According to the biomechanics of the musculoskeletal system, the microstructure and density of bones will change along with mechanical stimulation and bone mass will be supremely distributed when sufficient to bear the mechanical burden. Long-term apraxia will lead to bone loss, while proper load will strengthen the bones, with the exception of overloading which causes microfracture. To study tissues’ response to the mechanical environment, we should first describe the weight on tissues quantitatively, namely internal force and stress.
Stress
When tissues are burdened, the force of interaction between different parts inside is called stress. Internal force is a vector and its magnitude and direction are linked with the section. As is shown in Fig. 1.29a, assume that section S of biological tissue is divided into two parts, then the internal force on section S is the resultant force on the section.
Stress vector refers to the internal force on unit area.
As is shown in Fig. 1.29b, imagine that internal force on ΔS is \( \overset{\rightharpoonup }{\Delta F} \), then the average stress on ΔS is \( \overset{\rightharpoonup }{\Delta F} \)/ΔS. When ΔS is approaching 0 to be just one dot, then the stress on that dot is:
The magnitude and direction of the stress vector are related to the direction of the section in concern. For example, in Fig. 1.30a, the stress magnitude on ΔS1 is P/S; but in Fig. 1.30b, the stress magnitude on ΔS2 is 0.
Since the stress vector at one point will change with various section directions, to clearly depict the stress conditions of any random direction on the identified point, we need to introduce the concept of stress tensor.
Stress tensor is defined as:
In the definition, σij refers to nine components of stress tensor σ. ei is the coordinate base vector. The value of σ is irrelevant to the direction of section and does not change with the coordinate system. σ is symmetric tensor and σij = σji. Also, the stress vector in any direction can be calculated on the basis of dot product of stress tensor and unit vector in that direction:
where \( \overset{\rightharpoonup }{\sigma } \) is stress vector, σ is stress tensor, \( \overset{\rightharpoonup }{n} \) is the normal unit vector of the section in concern.
1.3.1.2 Displacement
Tissues change their spatial position in certain mechanical environments, and the displacement of any point is defined as the spatial distance and direction of the point from the initial position to the final position. Displacement is a vector.
As is shown in Fig. 1.31, the coordinates of A at the initial moment are (x1, y1) and the coordinates of A at the t+Δt moment are (x2, y2), then the displacement of A in Δt time is:
1.3.1.3 Strain
Tissues will deform accordingly in certain mechanical environments, and in order to depict the degree of deformation at any point within the tissue, we need to introduce the concept of strain.
Strain
The measurement of tissue deformation per unit length.
As is shown in Fig. 1.32, the elongation of the tissue in the x-direction at the t moment is L(t) = x2-x1 and at the t + Δt moment is L(t+Δt) = (x2 + u2) − (x1 + u1), then the elongation of the tissue in the x-direction is ΔL = L(t+Δt) − L(t) = [(x2 + u2) − (x1 + u1)] − (x2 − x1) = u2 − u1, the strain of the tissue in the x-direction is ΔL/L(t) = (u2 − u1)/(x2 − x1). As x2 approaches x1 infinitely, the strain at point x1 is:
As with stress, since the strain at a point changes with the direction, we need to introduce the concept of the strain tensor to clearly describe the strain state at a given point in any direction.
Strain tensor is defined as:
where εij is the nine components of the strain tensor ε and ei is the coordinate base vector. The value of ε is independent of the choice of the direction and does not change with the coordinate system. ε is the symmetric tensor, satisfying εij = εji.
1.3.1.4 Strain Energy Density
From an energy perspective, when tissues deform in certain mechanical environments, deformation energy accumulates in the tissue. Current studies show that the change and distribution of this deformation energy are closely related to the reconstruction of tissues [4]. Therefore, in order to quantitatively describe the energy produced by deformation, we need to introduce the concept of strain energy density.
Strain energy density refers to the work done by the stress per unit volume when tissues deform. It is defined as:
Thus, the total strain energy of the tissue is:
where V is the volume of the tissue.
1.3.2 Constitutive Relation of Musculoskeletal System
In the first part, we introduced the concepts of stress and strain to quantitatively depict the mechanical state and degree of deformation within a tissue. As different tissues respond differently to mechanical stimuli, they will exhibit different strains under the same stress state. It is the constitutive relation that is used to depict the relationship between stress and strain, which reflects the inherent material properties of the tissue. The constitutive relation of the tissue is often fit to their functions. For example, bones are the body’s primary load-bearing tissues and therefore have a greater ability to resist deformation; articular cartilage primarily acts as a lubricant and cushion, and the stiffness of the cartilage varies with the loading rate; ligaments are the primary constraining structures between bones, so they have high tensile stiffness but little compressive strength. Moreover, the constitutive relation of the same tissue varies significantly among different cases. For instance, patients with osteoporosis have low bone tissue stiffness and are highly susceptible to fractures; cartilage in patients with osteoarthritis tends to degenerate, thus significantly reducing its cushioning ability. Therefore, it is critical to study the constitutive relation of the tissue to understand the injury, prevention, and treatment of the musculoskeletal system.
In biomechanical simulation studies of the musculoskeletal system, it is necessary to assign a corresponding constitutive relation to a particular tissue. This relation reflects the tissue responsiveness to mechanical stimuli, and the accuracy of the constitutive parameters is directly related to the accuracy of the simulation study. The constitutive relation of the tissue is often measured by mechanical experiments (such as uniaxial tensile, biaxial tensile, three-point bending) to establish function relation between stress and strain (and strain rate) or between strain energy density and strain (and strain rate) based on the tissue’s stress–strain relations and loading history. Strictly speaking, biological tissues are nonlinear viscoelastic materials, but the constitutive relation of the tissue can be simplified in specific simulation issues, thus greatly improving the efficiency of calculations without compromising the accuracy. In biomechanical simulation studies of the musculoskeletal system, the commonly used constitutive relations include linear elastic model, hyperelastic model, and viscoelastic model.
1.3.2.1 Linear Elastic Constitutive Model
Linear Elastic Constitutive Relation
A one-to-one linear relationship between stress and strain in tissues.
As is shown in Fig. 1.33, a one-dimensional stress–strain curve is a straight line, and the function of stress with respect to strain (the constitutive relation) is Hooke’s law, which is:
where σ is the stress, E is the elastic modulus, and ε is the strain. The deformation of the linear elastic tissue is independent of the historical processes it carries. The three-dimensional constitutive relation of linear elasticity can be expressed as tensors, which is:
where σij is the component of the stress tensor, εkl is the component of the strain tensor, and Eijkl is the component of the elastic tensor. For an isotropic body, the component of Eijkl has only two independent components, and the constitutive relation can be further simplified as follows:
Where E is the elastic modulus, G is the shear modulus, and μ is the Poisson’s ratio.
In biomechanical simulation studies of the musculoskeletal system, although the constitutive relation of biological tissues is mostly nonlinear viscoelastic, the forces and deformations on the tissues tend to be in a linear relationship under small loads, under which circumstance adopting the constitutive relation of linear elasticity to depict the material properties of tissues can improve the efficiency of simulation calculations without compromising accuracy. As can be seen from the uniaxial tensile test on bone tissues (Fig. 1.34), the stress and strain exhibit a better linear elastic relation when the strain is less than ε0. Table 1.2 lists several commonly used linear elastic constitutive parameters.
1.3.2.2 Hyperelastic Constitutive Model
Hyperelastic Constitutive Relation
An ideal material with a one-to-one correspondence between force and deformation on the tissue. In the hyperelastic constitutive relation, tissue deformation only relates to the load received but not to the loading history. Linear elastic constitutive relation is a special hyperelastic constitutive relation in the case of small deformation.
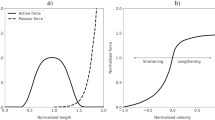
Figure 1.35 shows stress–strain curves for ligaments under axial tension, we can see that although there is a one-to-one correspondence between stress and strain, the stiffness of the tissue changes with strain in a nonlinear pattern. Under which circumstance the response of the tissue to mechanical stimuli can no longer be described by the linear elastic constitutive relation. The one-dimensional stress–strain relation is:
where σ is the stress tensor, ε is the strain tensor of the green, and the function of σ with respect to ε needs to be determined experimentally. The strain in the linear elastic constitutive relation is the Cauchy strain tensor, which is an approximation of the green strain tensor in the case of small deformation.
The three-dimensional hyperelastic constitutive relation is often described as a function of strain energy density with respect to strain:
where W is the strain energy density and ε is the Green strain tensor.
In biomechanical simulation studies of the musculoskeletal system, hyperelastic constitutive relation is of great importance for the accurate simulation of the material properties of soft tissues such as ligaments. Biological tissues generally have certain viscoelastic properties, that is to say, deformation is not only related to the load but also to the loading history, which greatly increases the difficulty of simulating the musculoskeletal system. However, numerous experiments have shown that when the change in strain rate in soft tissues reaches 1000, the corresponding change in stress is within 1–2 times [3]. This phenomenon means that more accurate results can be obtained even ignoring the effects of loading history when the loading rate changes little, thus providing theoretical support for the use of the hyperelastic constitutive relation.
Currently, hyperelastic constitutive relation is often used in simulations of tissues including ligaments and skin, for example:
where the material constants α, β and C1 are measured experimentally, and I1 and I2 are invariants of the strain tensor [9].
1.3.2.3 Viscoelastic Constitutive Model
The response of biological tissues to load has the following characteristics:
-
1.
The strain on the tissue gradually increases while the stress is held constant (Creep, as is shown in Fig. 1.36a).
-
2.
The strain on the tissue gradually decreases while the stress is held constant (Relaxation, as is shown in Fig. 1.36b)
-
3.
The deformation of the tissue lags behind the loading.
-
4.
Stress on the tissue is simultaneously related to strain and strain rate.
A viscoelastic constitutive model is required to simulate these material properties of biological tissues.
Hyperelastic constitutive relation refers to the property between the elastic constitutive relation and the viscous constitutive relation. Therefore, hyperelastic constitutive relation can be obtained by combining the elastic constitutive relation and the viscous constitutive relation.
The known ideal constitutive relation of elastic elements is:
where σ is the stress, E is the elastic stiffness, and ϵ is the strain.
The ideal constitutive relation of viscous elements is.
where σ is the stress, F is the elastic stiffness, and ϵ is the strain rate. A more complex viscoelastic constitutive relation can be constructed by connecting elastic and viscous elements in series and parallel. Classical viscoelastic constitutive relations include the Maxwell model and the Kelvin-Voight model.
-
1.
Maxwell model, connecting elastic and viscous elements in series, as is shown in Fig. 1.37. Its constitutive relation is:
$$ \sigma +{p}_1\dot{\sigma}={q}_1\dot{\epsilon} $$
-
2.
Kelvin–Voight model, connecting elastic and viscous elements in parallel, as is shown in Fig. 1.38. Its constitutive relation is:
$$ \sigma ={q}_0\epsilon +{q}_1\dot{\epsilon} $$
The combination of the classical Maxwell model and Kelvin–Voight model develops the general form of the linear viscoelastic model:
The following quasi-linear viscoelastic constitutive model can be obtained when applying the viscoelastic constitutive model to the simulation of bones:
1.3.2.4 Numerical Model of Bone Remodeling
Biological tissues differ from other engineering materials in that they can adjust their mechanics features to adapt to the change of mechanical environment. In the biomechanics of the musculoskeletal system, such a stress–growth relationship is a key factor to adjust the bone tissues remodeling.
In the bone tissues, bone density and strength distribution are closely related to the mechanical environment. If the burden on bones is at a low level for long (just like weight loss condition of astronauts), bone mass and strength will decline as well. In the orthopedics implantation operations, the stress shielding of implants will lead to bone resorption at the low-stress region, thus causing postoperation refracturing. Adequate increase of bone loading can facilitate bone growth. Yet overloading might cause microdamage.
The stress distribution of bone tissues may change the constitutive parameters of tissues through the bone remodeling mechanism, and vice versa. This interactive process repeats itself to reach a dynamic balance in the end. In the simulation study of musculoskeletal system biomechanics, to simulate this process and acquire the far-reaching impact of mechanical environment on bone tissues, we need to firstly quantitatively depict the relationship between mechanical environment and bone remodeling.
Studies find by now that the change of bone density is significantly correlated with the strain energy density. The response of bones to mechanical stimulation is broken down into four stages, namely absorption, stabilization, growth, and damage. The change rate of bone density can be represented by strain energy density per unit mass, as is shown below:
In the equation, ρ is bone density, W is strain energy density and constant B is 1.0g/cm3, Kmin, Kmax, and Kmicrodamage are threshold values of bone remodeling, which are 0.0036 J/g, 0.0044 J/g, and 0.0358 J/g. Bone density and Young Modulus have the following empirical relationship:
E is the Young Modulus, constant C is 3790 MPa/(g·cm3)2. In line with the above equation, we can establish the relationship between elasticity modulus and strain energy density. Then the distribution of strain energy density could be recalculated based on the updated elasticity modulus and bone remodeling is achieved.
1.3.3 Basic Principles of Musculoskeletal Modeling Simulation
The research of biomechanics of the musculoskeletal system is designed to acquire tissues’ response to specific mechanical environment, thus clarifying impacts of mechanical factors on the movement, growth, remodeling, injuries, and treatment of biological tissues. The biomechanics numerical simulation aims at proper abstraction and simplification of the morphology, materials, loading, and boundary conditions of real tissues, described in the language of mathematics, to forecast mechanical response of tissues in a virtual computer environment. The strengths of numerical simulation technologies are: (1) to obtain information inaccessible through experiment observation, such as internal stress of tissues, strain, and strain energy distribution; (2) to simulate mechanical response of tissues under extreme circumstances, such as the simulation of injuries and damage of the musculoskeletal system; (3) to undertake parametric analysis of specific issues with high efficiency and low cost. Numerical simulation can easily readjust the parameters of the model, such as material, size, and gravity, paving the way for comparative analysis of similar models on a large scale.
Computing mechanical response of biological tissues is in essence calculating the governing equation of biomechanics models.
1.3.3.1 The Governing Equation of Biomechanics Models
The governing equation of biomechanics models includes equilibrium equation, geometric equation, and material equation.
Equilibrium Equation
When tissues are in an equilibrium state, any point inside tissues is in an equilibrium state mechanically. To get to that state, the stress of any point must satisfy the equation:
σ is strain tensor, ▽σ is the divergence of strain tensor, \( \overset{\rightharpoonup }{F} \) is external force vector per unit volume. In the form of component, this equation goes like this:
Geometric Equation
Being loaded, points on tissues might change locations. Such changes are in the forms of metaplasia and rigid body displacement. The geometric equation is to depict the correlation between strain and displacement field. Under the circumstance of slight deformation, this relationship could be demonstrated as:
where ϵ is the Cauchy strain tensor, \( \overset{\rightharpoonup }{u} \) is displacement vector. \( \nabla \overset{\rightharpoonup }{u} \) and \( \overset{\rightharpoonup }{u}\nabla \) are the left and right gradients of the displacement. This expression could be rephrased in the form of component:
When the deformation of tissues is limited, strain is usually defined as the following:
where EIJ is the Green strain tensor, UI is the displacement component described by Lagrange, XJ is the coordinate component by Lagrange. Cauchy strain tensor is the approximation of Green strain tensor under the precondition of slight deformation.
Constitutive Equation
Biological tissues experience deformations in certain stress environment and their deformation degrees are linked with the material characteristics of tissues. The strain and stress on tissues should satisfy the constitutive equation:
The left is the function of stress and strain and the right is the function of strain energy density and strain. The definite form of the constitutive equation is determined by the characteristics of the biological materials. The commonly seen constitutive models include linear elasticity, superelasticity, and viscoelasticity. As to the undefined constant in the constitutive model, it needs to be confirmed in experiments.
The differential equations of 1, 2, and 3 are the governing equations of biomechanics model. Theoretically, solving equations in line with boundary conditions will get stress and strain of any random point of tissues. Regretfully, due to irregular morphology of biological tissues and nonlinear significance of materials, we are incapable of solving the differential equations. So we resort to the finite difference method and finite element method to succeed in a numerical solution of the equations.
1.3.3.2 Principle of Minimum Potential Energy
The principle of minimum potential energy elaborates on the conditions that mechanical response of tissues should conform to from the angle of energy. Essentially, it is equivalent to the above-mentioned equilibrium equation. The significance of it lies in that it replaces the equilibrium equation in the form of differentials with the strain energy function in the form of scalars, making it the basis of the finite element method.
Principle of Minimum Potential Energy
When the elastic system is in an equilibrium state, the potential energy of the system is no more than that of other possible displacements. Assume that when displacement field is \( \overset{\rightharpoonup }{u} \), the potential energy is Π(\( \overset{\rightharpoonup }{u} \)), then the displacement field \( \overset{\rightharpoonup }{u} \) in the equilibrium state should satisfy:
\( \delta \varPi \left(\overset{\rightharpoonup }{u}\right) \) is the variation of the total potential energy of the system.
According to Hooke’s law (F = ku) of the spring and the equilibrium equation (F = mg), we can get the elongation of the spring (u)which is mg/k.
From the perspective of minimum potential energy principle, the total potential energy is:
where 0.5ku2 is the elastic potential energy of the spring, mgu is the work of gravity. In accordance with the principle of minimum potential energy, the displacement with minimum potential energy of the system is the real displacement of the system:
We come to the conclusion that u = mg/k. Notably, the displacement result on the basis of the minimum potential energy principle is the same as that under the framework of equilibrium equation.
1.3.3.3 Finite Element Simulation
The finite element method combines the minimum potential energy principle with finite element discretization. The primary function of the element realizes piecewise interpolation of the displacement field. So the displacement field with minimum system potential energy, namely the approximation of real displacement, is obtained according to the admissible displacement function. Theoretically, when the element scale is infinitely approaching 0, the simulation result of finite element is approaching the reality. The following is the basic principle of finite element simulation.
-
1.
Finite element discretization
As is shown in Fig. 1.39, the geometric model of tissues is dispersed into finite elements. Strain energy of the elements is Πe and the displacement of element nodes is \( \overset{\rightharpoonup }{u_e}(i) \) (i is the number of nodes, i = 1, 2, … 8). Then the displacement of any random point of the elements can be represented as:
ϕi is the interpolation primary function. The strain energy of elements can be expressed in the displacement function of element nodes:

-
2.
The contribution of work by external forces to total potential energy of the system
As is shown in Fig. 1.40, external forces exerted on tissues are dispersed on various nodes to express the work by external forces as the function of nodes displacement:
N is the total number of nodes, \( {\overset{\rightharpoonup }{F}}_i \) is the vector of external force dispersed, \( {\overset{\rightharpoonup }{u}}_i \) is the displacement vector of nodes.
-
3.
The total potential energy of the system is the combination of strain energy of all elements and the contribution of work done by external forces. The total potential energy is shown in the function of nodes displacement:
$$ \varPi =\sum \limits_{i=1}^N{\varPi}_e+W\left({\overset{\rightharpoonup }{u}}_i\right)=\varPi \left({\overset{\rightharpoonup }{u}}_i\right) $$ -
4.
According to the minimum potential energy principle, we calculate the node displacement in an equilibrium state:
$$ \delta \varPi \left({\overset{\rightharpoonup }{u}}_i\right)=0\kern1em \left({\overset{\rightharpoonup }{u}}_i=\left({u}_i,{v}_i,{w}_i\right)\right) $$

To obtain physical quantity of displacement, strain and stress at a random point, we start with solving equations to acquire element displacement of a random node and then resort to piecewise interpolation.
This section introduces some basic concepts involved in the biomechanics simulation study of the musculoskeletal system, constitutive relationship of biological tissues and finite element simulation. It targets at allowing readers to get a gist of the basic theories and the process of biomechanics simulation of the musculoskeletal system. At present, with the development of mathematics and mechanical theories, philosophies of the meshless method, boundary element, and symplectic geometric algorithm came into being, improving the scope of application of numerical simulation, solution accuracy, and efficiency. In actual biomechanics simulation studies, researchers generally adopt mature commercial software of finite element and material models redeveloped, so as to analyze certain problems case by case. As to the commonly used finite element software (such as Ansys and Abaqus), they will be left to the following chapters.
References
Bai S, Ying D (2013) Systematic anatomy. People’s Medical Publishing House, Beijing
Tortora GJ, Derrickson B (2012) Principles of anatomy and physiology. John Wiley & Sons, Hoboken
Fung YC (1993) Biomechanics: mechanical properties of living tissues, 2nd edn. Springer, New York
Mellal A, Wiskott HW, Botsis J, Scherrer SS, Belser UC (2004) Stimulating effect of implant loading on surrounding bone. Comparison of three numerical models and validation by in vivo data. Clin Oral Implants Res 15(2):239–248. https://doi.org/10.1111/j.1600-0501.2004.01000.x
Akizuki S, Mow VC, Muller F, Pita JC, Howell DS, Manicourt DH (1986) Tensile properties of human knee joint cartilage: I. Influence of ionic conditions, weight bearing, and fibrillation on the tensile modulus. J Orthop Res 4(4):379–392. https://doi.org/10.1002/jor.1100040401
Ashman RB, Cowin SC, Van Buskirk WC, Rice JC (1984) A continuous wave technique for the measurement of the elastic properties of cortical bone. J Biomech 17(5):349–361
Rohlmann A, Zilch H, Bergmann G, Kolbel R (1980) Material properties of femoral cancellous bone in axial loading. Part I: time independent properties. Arch Orthop Trauma Surg 97(2):95–102
Hayes WC, Mockros LF (1971) Viscoelastic properties of human articular cartilage. J Appl Physiol 31(4):562–568
Song Y, Debski RE, Musahl V, Thomas M, Woo SL (2004) A three-dimensional finite element model of the human anterior cruciate ligament: a computational analysis with experimental validation. J Biomech 37(3):383–390
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 People's Medical Publishing House
About this chapter
Cite this chapter
Ni, Y., Gao, Y., Yao, J. (2021). Introduction to Musculoskeletal System. In: Fan, Y., Wang, L. (eds) Biomechanical Modelling and Simulation on Musculoskeletal System. Springer, Singapore. https://doi.org/10.1007/978-981-16-3911-1_1
Download citation
DOI: https://doi.org/10.1007/978-981-16-3911-1_1
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-3910-4
Online ISBN: 978-981-16-3911-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)