Abstract
Titanium and titanium alloys are widely used in different biomedical applications owing to their high biocompatibility, high corrosion resistance, good mechanical properties, and good osseointegration ability. Titanium and its alloys rapidly form a surface oxide layer in air and aqueous environments. This passive and thin (a few nanometers) surface oxide hinders active corrosion and ensures a low metal ion release, enhancing biocompatibility. Compared to that of other biomedical alloys, this surface oxide is exceptionally resistant to chemical attack by halides, primarily chlorides; the presence of fluorides can, in some cases, result in localized corrosion of titanium and its alloys. However, the combination of proteins, inflammatory conditions and bacteria, which for instance generate hydrogen peroxide, can result in a reduction of the corrosion resistance of titanium-based materials. Titanium and its alloying elements, such as aluminum and vanadium, can then be released as ions, which might trigger an immune system response and reduce biocompatibility. Several surface modifications have been proposed in order to improve the bone-bonding ability of titanium and its alloys, facilitate the healing process, and enhance the success of the implant with a decreased risk of micromotions. Moreover, antimicrobial ions/nanoparticles can be added to the surface to reduce the infection risk. Surface modification of titanium (e.g., with artificially grown, micrometer-thick, titanium oxide layers) can significantly increase the corrosion resistance under critical conditions (e.g., inflammatory response and infection); however, the surfaces are not completely inert and the effect of metal ion/nanoparticle release should be carefully taken into account.
This chapter reviews and discusses the current strategies for modifying and controlling the surface of titanium-based implant materials, with particular focus on corrosion resistance, bone integration, inflammatory and infection control, and interactions with the physiological environment.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Titanium (Ti) and Ti alloy implant materials can release metal ions and particles into the physiological environment. These can be simple metal ions, aqueous complexes, ions bound to proteins or metal (oxide) particles. Their form (chemical speciation) is decisive for any biological response and might be changed with time or upon a changed environment.
While direct immune response to Ti species has been debated for a long time, newer research shows clear evidence that T-cell-mediated hypersensitivity specific to Ti(IV) exists (Chan et al. 2011; Hamann 2018; Evrard et al. 2010; Hosoki et al. 2016). Hypersensitivity reactions to Ti have traditionally been overshadowed by those to other metals (Evrard et al. 2010; Hosoki et al. 2016) and are—due to chemical limitations—difficult to diagnose by patch testing (Hamann 2018). While Ti and its oxides, such as Ti dioxide (TiO2), have long been considered nontoxic and biocompatible, newer studies show that this is not always true (Jin and Berlin 2015). Small (<4 μm) released Ti oxide particles can be taken up in cells (Kumazawa et al. 2002), be enriched into the implant-adjacent tissue or distal organs (Swiatkowska et al. 2018; Olmedo et al. 2008; Sarmiento-González et al. 2008), and cause different immunological responses (Thewes et al. 2001). Due to the low solubility of TiO2, TiO2 particles, comprising 80% of the total detected Ti, have been found in human post-mortem studies in different organs, such as spleen, liver, and kidney (Peters et al. 2020). TiO2 nanoparticles are of relatively low toxicity as compared to other metal oxides or metal nanoparticles; however, it is now evident that they can cause the generation of reactive oxygen species, inflammatory response, genotoxicity, metabolic changes, and potentially carcinogenesis (Grande and Tucci 2016; Shakeel et al. 2016).
The alloying elements in Ti alloys, such as aluminum (Al), niobium (Nb), tin (Sn), vanadium (V), nickel (Ni), or palladium (Pd), are often of greater short-term health concern than Ti (Chen and Thyssen 2018). Other common alloying elements of similar or lower health concern, as compared to Ti, are tantalum (Ta), zirconium (Zr), iron (Fe), and molybdenum (Mo). Chromium (Cr), which is a common metal allergen, can also be an alloying element for titanium alloys (Hamann 2018). These and other alloying elements stabilize different phases of titanium, resulting in different, or a mixture of, crystal structures with unique mechanical, machinability, and corrosion properties (Noël et al. 2018). Commercially pure (cp) Ti is used as coating material or for some dental applications (Gilbert 2017). For many biomedical applications, the use of Ti alloys is necessary, as the mechanical properties of pure Ti are insufficient. The Ti alloy containing 6 wt% Al and 4 wt% V (Ti6Al4V) is commonly used for parts of artificial joints (such as the stem of an artificial hip joint prosthesis), which require high corrosion resistance and high fatigue strength, but not necessarily high wear resistance (Gilbert 2017); titanium and its alloys have very poor wear and fretting resistance. Ti and its alloys possess a comparably high osseointegration (tight integration of the implant with the bone), relatively low density (closer to that of natural bone), and relatively high biocompatibility compared with alternative alloys.
The interface between the Ti (alloy) surface and the physiological environment is dynamic and both sides are influenced by each other. For example, released metals can cause immunological reactions, which in turn can cause a more corrosive environment, triggering more metal release. Infections, specific diseases, and other factors (such as implant design) can also cause aggressive environments leading to corrosion and ultimately health effects or implant failure. This chapter will discuss these corrosion processes, how they are affected by the physiological environment, and how metal release, corrosion, and infections could be minimized by means of surface engineering. A specific focus is on the complex physiological environment in which corrosion resistance, modulation of the inflammatory response, bioactivity, and ability of infection control play interconnected roles. The recent strategies of surface modification of Ti in order to obtain a multifunctional action, which takes all the above-cited parameters into account, are discussed.
2 Corrosion Resistance of Ti and Its Alloys in the Biological Environment
2.1 Principles of Corrosion of Ti and Its Alloys
A metal is a conductive material, and as such, electrons can freely move within it. Corrosion of metals occurs via the oxidation of the metal and the reduction of an oxidant, most often oxygen, water, or protons. These two half-cell reactions are balanced such that the number of electrons produced by metal oxidation is equal to the number consumed in the reduction of oxidants. Due to the electron conductivity of the metal, the reduction half–cell reaction can occur at a very different location and over a differently sized surface area than the oxidation half-cell reaction; these differences are critical for a number of localized corrosion types of Ti metal and its alloys.
Ti metal is thermodynamically unstable in water or air. It is rapidly oxidized and reacts even with hydrogen, nitrogen, and many other elements. Its high affinity for oxygen is key to its ability to form a protective surface oxide that hinders further Ti metal oxidation and ensures Ti and its alloys can withstand the relatively corrosive physiological environment to a large extent. In order to understand the corrosion of Ti and Ti alloys, we need to understand the conditions under which the Ti surface oxide can form and reform.
At physiologically relevant pH values, Ti metal is oxidized to TiO2 in several steps (McCafferty 2010; Schmets et al. 1974), with the following reactions showing the equilibrium states under standard conditions:
or
or
where E° denotes the standard electrode potential in V vs. the standard hydrogen electrode (SHE) and under standard conditions (25 °C, activity of 1, 1 atmosphere gas pressure). For other solute concentrations, the reader is referred to the equations given in Schmets et al. (1974).
All of these reactions occur at potentials far more negative than the stability range of water, which means that the thermodynamic driving force for Ti oxidation to the TiIV valence state is very high, compared to that of most other metals (Pourbaix 1974). This driving force ensures that a damaged surface oxide is rapidly repaired under benign conditions. This further ensures a very low corrosion rate, under so-called passive conditions, under which subsequent Ti oxidation is limited by restricted mass transport through the formed Ti surface oxide. Under more aggressive, nonpassive conditions, this high thermodynamic driving force toward Ti oxidation can cause a high corrosion rate and large potential differences when coupled with other metals, phases, or intermetallic precipitates, even within the same alloy.
Alloying elements can either improve or degrade the corrosion resistance compared to commercially pure Ti metal.
The Ti-Ni alloy (commercial name “nitinol”), which is used for its shape memory effect in cardiovascular stents and orthodontic appliances, is an example of a Ti alloy with significantly lower corrosion resistance than Ti metal (Ding et al. 2018; Noguchi et al. 2008), accompanied with some Ni release (Saylor et al. 2016; Sullivan et al. 2015), approximately in the same range as, or lower than, austenitic Ni-containing stainless steel (Hedberg and Odnevall Wallinder 2016; Eliades et al. 2004; Suárez et al. 2010). This Ni release can cause a number of clinical adverse effects (Faccioni et al. 2003; Mani et al. 2007; Gong et al. 2013).
Ti alloys containing Al and either V or Nb are widely used for different biomedical applications, especially in orthopedic artificial joint prostheses (Gilbert 2017; Milošev 2017). The Ti alloy containing 6 wt% Al and 4 wt% V (Ti6Al4V) has been reported to have a slightly less protective passive layer than does commercially pure Ti (Shukla et al. 2005). In the same study (Shukla et al. 2005), a higher alloyed Ti alloy with 13.4 wt% Al and 29 wt% Nb (Ti13.4Al29Nb) showed improved corrosion resistance compared with Ti metal over 1 week of exposure in Hank’s solution, a simple physiological simulant containing a number of salts and glucose at a pH value of about 7.4. A detailed X-ray photoelectron spectroscopy study of specimens exposed to Hank’s solution revealed a spontaneous formation of primarily TiO2 in the surface oxide of Ti6Al4V and small amounts of Al2O3 on its outermost surface at the interface with the solution (Milošev et al. 2000). A similar study on Ti6Al7Nb showed that the surface oxide on this alloy formed less sub-oxides of TiO and Ti2O3 as compared to Ti6Al4V and possessed a higher corrosion resistance (Milošev et al. 2008).
The formation of the passive surface oxide on Ti and Ti alloys is required for high corrosion resistance. Its formation is, however, strongly dependent on environmental conditions, as discussed in the following section.
2.2 Physiological Environments from a Corrosion Perspective
The physiological environment is highly complex, locally different, and dynamic over time. Only recently, it has been acknowledged that simple salt-based solutions, such as 0.9% sodium chloride, Hank’s solution, Ringer’s solution, and phosphate-buffered saline, cannot simulate the physiological environment in a relevant and sufficient way for Ti alloys (Gilbert 2017; Zhang et al. 2018a; Hedberg et al. 2019b).
Halides are important to many localized types of corrosion of passive metals. Ti has been considered to have low susceptibility to chloride-induced corrosion; however, in combination with fluorides and other factors, the chlorides contribute to the corrosion process in a synergistic manner (Li et al. 2007). Fluoride is actively used in the cleaning and protection of natural teeth; therefore, especially Ti-based dental implants and orthodontic Ni-Ti wires are regularly exposed to fluorides. The TiO2-containing passive film of Ti and its alloys is susceptible to fluoride attack. It was found that fluorides increase the corrosion rates of Ti and its alloys under conditions of relevance for dental environments (Li et al. 2007; Mirjalili et al. 2013; Noguchi et al. 2008; Reclaru and Meyer 1998).
The physiological environment also contains a high number of complexing agents and proteins. The high ionic strength of the physiological environment ensures their rapid adsorption even on similarly charged surfaces (Fukuzaki et al. 1995; Hedberg et al. 2014; Claesson et al. 1995). Proteins and other complexing agents, such as peptides, amino acids, organic acids, or different anions, can form a complex either directly with Ti or with any of its alloying elements. This can occur either directly with the metal, with a metal ion in solution, or—most relevant for passive conditions—directly with the surface oxide. It has been suggested that this process plays an important role for the depletion of Al2O3 from the surface oxide of Ti6Al4V, and that it is accelerated in the presence of hydrogen peroxide (Hedberg et al. 2019b).
Inflammatory and immunological reactions can result in a chemical attack and a very high redox potential in the in vivo environment or locally on the implant surface. Most importantly, there is increasing evidence that the surface reactions and corrosion trigger the biological response, which in turn increases the corrosion rate (Hedberg 2018; Gilbert 2017; Milošev 2017). For example, immune and inflammatory cells can produce a range of highly oxidizing species, including hydrogen peroxide, hydroxyl radical, and hypochlorous acid, resulting in an extremely oxidative environment (Gilbert and Kubacki 2016).
2.3 Pitting and Crevice Corrosion
Pitting and crevice corrosion are localized corrosion types that are important to most passive metals and alloys. For Ti alloys, most pitting or crevice corrosion cases have been found in conjunction with the crevice induced in modular tapered junctions (Gilbert 2017), schematically illustrated in Fig. 1.1. The difference between pitting and crevice corrosion is its initiation: pitting corrosion requires the damage of the surface oxide, which is often unlikely to occur for Ti alloys, while the crevice already provides the optimal conditions for initiation of this localized corrosion process. Once initiated, the propagation and failure or repassivation steps of pitting and crevice corrosion are similar and involve a large passive area providing the necessary reaction surface area for the cathodic reaction and a very small confined space for the anodic reaction (metal oxidation), which is also driven by significant amounts of proton reduction within its interior (Noël 1999; He et al. 2009). If pitting corrosion occurs, it is often located in the vicinity of a crevice (Gilbert 2017), as the local chemical environment there is far more anaerobic, acidic and enriched in chlorides, fluorides, or other anions able to attack the Ti surface oxide. The anodic half-cell reactions inside the crevice or pit require cathodic half-cell reactions. These cathodic half-cell reactions can involve the reduction of oxygen on passive surfaces of the Ti metal or alloy—far away from the crevice or pit. Another even more important cathodic reaction is the reduction of protons resulting in the formation of hydrogen gas or absorbed hydrogen in the metal (Noël 1999, He et al. 2009), which embrittles the metal and can cause cracking, Fig. 1.1. Protons inside the confined space originate from hydrolysis of the released metal ions. These positively charged protons and metal ions also attract negatively charged counterions, such as chlorides, fluorides, or sulfates, to maintain charge neutrality inside the crevice or pit. This results in an extremely concentrated and aggressive solution chemistry. Although crevice corrosion of CP Ti requires temperatures above ~60 °C (Noël 1999), it may proceed at lower temperatures on more susceptible alloys. Crevice and pitting corrosion are often combined with mechanically assisted corrosion types, which then can result in cracking or faster propagation. A change in the geometry, replenishing of the solution inside the confined space, and/or a shift in potential due to oxidants may result in repassivation of the surface. Although crevice and pitting corrosion are rarely observed directly from retrieved Ti alloy implant materials, they are suspected to be part of the overall corrosion mechanism (Hall et al. 2018; Gilbert 2017).
Schematic illustration of the local chemical environment during pitting and crevice corrosion of Ti or its alloys. Inside the confined space of the crevice or pit, the solution chemistry is characterized by a very low pH, an anaerobic environment, and a very high concentration of ions. Charge neutrality is ensured by the free movement of electrons inside the metal and the migration of ions in and out of the confined spaces. The corrosion reactions result in the buildup of corrosion products on the surface of the confined spaces and as particles. Micromotion is often present for crevices of orthopedic and dental implants
2.4 Mechanically Assisted Corrosion Types
Ti and its alloys are usually not intended for wear-exposed parts of biomedical implants due to their relatively low wear resistance, compared to cobalt-chromium (Co-Cr) alloys or ceramic materials. Nevertheless, mechanically induced corrosion types are still of high importance for biomedical Ti (alloys) and therefore an important target for surface engineering.
An important type of corrosion of Ti alloys as biomedical materials is mechanically assisted crevice corrosion (MACC) (Hall et al. 2018; Gilbert 2017), which is the combination of fretting corrosion and crevice corrosion. Fretting corrosion requires micromotion between the Ti (alloy) surface and a hard countersurface able to damage the surface oxide (Swaminathan and Gilbert 2012). In implant materials, such as dental implants (screws) or modular taper junctions of joint prostheses, cyclic micromotions are common. The hard countersurface can, for instance, be an oxide-coated metal, a ceramic material, or particles deriving from the corrosion process (Fig. 1.1) or wear. This oxide damage then initiates or accelerates localized corrosion, most often crevice corrosion.
Stress corrosion cracking can be a result of hydrogen embrittlement (“hydrogen-induced cracking (HIC)” (Clarke et al. 1997; Tal-Gutelmacher and Eliezer 2005)) due to absorbed hydrogen (Fig. 1.1) or be related to the stresses that occur during oxide growth (“oxide-induced stress corrosion cracking”—OISCC) (Gilbert 2017). MACC and OISCC can ultimately result in the buildup of a relatively thick (several hundreds of micrometers) Ti oxide layer, termed “direct conversion to oxide” (Gilbert 2017; Gilbert et al. 2012). These thick Ti oxide layers have been found in vivo (Gilbert et al. 2012), especially in modular taper junctions providing the optimal geometry of a crevice in combination with micromotions. The combination of OISCC and direct conversion to oxide can result in rapidly growing pits filled with oxide. As these oxides have a higher volume than the metal (Pilling-Bedworth ratio = 1.73 (Nelson and Oriani 1993)), the material cracks, and the pit can propagate further. This can result in millimeter-long oxide-filled pits and cracks (Gilbert et al. 2012), Fig. 1.2.
Example of OISCC: oxide-filled deep-plunging pit resulting in cracking in a Ti6Al4V/Ti6Al4V taper region. (Reprinted with permission from John Wiley and Sons (Gilbert et al. 2012))
2.5 Selective, Galvanic, and Intergranular Corrosion
Ti6Al4V contains both alpha (hexagonal closed-packed structure) and beta (body-centered cubic structure) Ti phases. It has been shown for retrieved implants that pits and directly converted oxide propagate along the beta phases and then convert the alpha phases into oxide (Gilbert et al. 2012). This selective corrosion is due to a lower corrosion resistance of the beta phase as compared to the alpha phase (Noël et al. 2018). It has been hypothesized that the combination of hydrogen peroxide (from inflammatory reactions) and active potentials, for example, due to crevice corrosion, can provide conditions that selectively dissolve the beta phase of Ti6Al4V alloys (Gilbert et al. 2012).
Intergranular corrosion, for which the corrosion occurs preferentially along grain boundaries, is relatively rare for Ti and its alloys in biomedical applications, but has been observed as a consecutive corrosion mechanism following other corrosion types such as MACC (Gilbert 2017).
Due to the very negative standard potential of Ti and its alloys (see Sect. 1.2.1), this metal can be susceptible to galvanic corrosion when coupled with other metals and when the oxide is damaged. Also, due to its high corrosion resistance in aqueous environments, the surface of Ti and its alloys could act as the cathodic site when coupled to another, less corrosion-resistant alloy. This could result in hydrogen absorption. Coupling to other metals is common in most orthopedic and dental implants (Cortada et al. 2000; Lucas et al. 1981). Galvanic corrosion has, however, not been found to be a dominating corrosion type for biomedical Ti alloys (Cortada et al. 2000; Lucas et al. 1981; Gilbert 2017). Any galvanic effects of incorporated noble metal nanoparticles in the oxide of Ti alloys have recently been studied and are discussed in Sect. 1.4.3.
2.6 The Role of Cells, Proteins, and Reactive Oxygen Species
The Ti (alloy) material is not only influenced by the physiological environment but does also change the physiological environment by triggering different cell and immune responses, which in turn influence corrosion mechanisms. This two-way response is a relatively new paradigm within corrosion science and has been supported and proposed by a number of recent scientific studies and discussions (Gilbert 2017; Hedberg 2018; Hedberg et al. 2019a, b; Gilbert and Kubacki 2016; Gilbert et al. 2015; Milošev 2017; Yu et al. 2015; Zhang et al. 2018a). There is a large arsenal of chemical species and cells in the response of the human body to the metal or alloy. Each of them alone is often not of great concern, but combined with other factors, their action can be devastating to the corrosion process.
A recent study demonstrated a combined effect of mechanical stress and proteins on the corrosion resistance of, and metal release from, Nitinol (Ni-Ti) alloys (Zhang et al. 2020a).
Several studies have shown the combined action of proteins, such as serum albumin, and hydrogen peroxide, which is one of the chemical species produced under inflammatory conditions, on the corrosion resistance of, and metal release from, Ti6Al4V (Yu et al. 2015; Zhang et al. 2018a; Hedberg et al. 2020, 2019b). It has been hypothesized that hydrogen peroxide primarily forms a complex with TiO2, weakening its bonds and chemical stability, while serum albumin primarily complexes aluminum from the surface oxide (Hedberg et al. 2019b). These complexation processes result first in the enrichment and then the depletion of aluminum in the surface oxide and in the growth of a relatively thick oxide (Hedberg et al. 2019b), similar to those found in vivo. These complexation and metal complex detachment processes take time and are not necessarily possible to detect in short-term accelerated corrosion tests (Zhang et al. 2018a; Hedberg 2018).
It should be emphasized that proteins are not necessarily detrimental to the corrosion process but can also be neutral or beneficial—this depends on the circumstances (Hedberg 2018). In addition to their complexation abilities, they can also have shielding effects, reducing the access to an oxidant, and they can also act as biomarkers, attracting certain cells (both beneficial and detrimental to the corrosion process).
As outlined in Sect. 1.2.2, inflammatory and infection conditions can be considered a worst-case environment. Direct etching tracks related to immune cells have been observed on Co-Cr alloys (Hall et al. 2017), but would most probably result in a thicker oxide, instead of etching, in the case of Ti alloys. The immune system also reacts to protein aggregates, which can be induced by metal ions or nanoparticles (Hedberg et al. 2019a), and wear particles (Sundfeldt et al. 2006). The immune system also reacts to relatively low amounts of released metal ions in the case of sensitization (allergy) to one or several of the metals in the alloys (Chen and Thyssen 2018).
From an engineering perspective, it is, hence, interesting to target the avoidance of infections, the decreased release of metal ions and the increased wear resistance of biomedical Ti alloys.
3 Ti Surfaces and Inflammatory Reaction
3.1 Host Response to Ti Surfaces
The host response to an implanted biomaterial depends on the material characteristics (e.g., composition, surface texture, degradability, mechanical properties) and host-specific features (such as age, anatomic factors, comorbidities, immune response). This response begins at implantation time and lasts for the whole duration of the material’s presence in the human body (Londono and Badylak 2015). The host response is of particular importance because it can affect the implant properties (e.g., degradation, surface alteration) and its functional outcome (e.g., fibrous encapsulation vs. physiological integration).
Upon implantation, the biomaterial surface comes in contact with the physiological fluids and water; ions and proteins sequentially interact within a few seconds. The protein layer, which covers the surface, depends on the material surface properties and affects the cellular/bacterial adhesion to it (Kasemo 2002). The first cells to approach the protein-covered surfaces are neutrophils, with the aim of remoinge bacteria and debris or damaged tissues in analogy to the conventional wound-healing process in the absence of an implant (Ratner 2001; Londono and Badylak 2015). In 1 day, macrophages reach the surface. As in wound-healing without an implant, the macrophages modulate inflammation (inevitably associated with wounds) to achieve tissue repair. In the presence of a foreign material, the surface properties and host characteristics affect the macrophage response (Ratner 2001, Londono and Badylak 2015). Typically, macrophages can show a pro-inflammatory polarization (M1 state) related to rapid immune activation or an anti-inflammatory polarization (M2) related to wound healing and tissue remodeling. A proper balance between these two states can guarantee a physiological healing, assuring the removal of damaged tissues without the development of chronic inflammatory response (Hotchkiss et al. 2016). In the presence of nondegradable implants (e.g., Ti implants), the macrophages identify the implant as a possible foreign body and try to engulf and digest it: a process often called “frustrated phagocytosis,” which ultimately results in the fibrous encapsulation of the implant (Ratner 2001, Londono and Badylak 2015). Metal ions and nanoparticles significantly affect the host response to implants. For example, metal ions can bind host proteins and cause an immunological response resulting in hypersensitivity (Yao et al. 2015). These phenomena are particularly evident for toxic metals such as Ni, Co, and Cr ions released from Co-Cr alloys, or their micro or nanosized particles produced in metal-on-metal joint replacement (recently highly debated). Hypersensitivity and excessive immune response are rarely reported for Ti alloys (Yao et al. 2015). In the case of Ti implants, it has been supposed that the collagenous capsule can evolve into bone mineralization, due to the presence of ions and bone stem cells at the implant site (Ratner 2001). Ti-bone bonding ability has been widely studied, and several surface modifications have been proposed in order to improve it, such as nano/micro textures, bioactive surface layers (obtained by chemical or electrochemical treatments), bioactive coatings (e.g., bioactive glasses or hydroxyapatite), and surface grafting of bioactive molecules (Souza et al. 2019; Oliver et al. 2019; Spriano et al. 2018, 2010; Kokubo and Yamaguchi 2016; Lugovskoy and Lugovskoy 2014; Chen et al. 2013). The cited surface treatments can induce a significant improvement in the biological response to Ti in terms of osteoblast adhesion, proliferation, and differentiation (in vitro) and of bone formation (in vivo). However, it has been reported that in certain cases a too rapid and conspicuous bone apposition can be associated with an excessive inflammatory response, which can even lead to late implant failure (Stanford 2010). Considering these aspects, the development of Ti surfaces able to improve bone bonding and healing in a physiological manner with strict control of the inflammatory host response is of great interest in the biomaterials field. The strategies currently under investigation for the modulation of inflammatory response to Ti surfaces are discussed in the following section.
Finally, prosthetic infections are always coupled with a strong inflammatory reaction, which can exacerbate the situation and lead to implant failure. The strategies for the preparation of antibacterial surfaces are discussed in Sect. 1.4.
3.2 Surface Modifications for Inflammatory Control
The meaning of biocompatibility evolved away from the original concept of an inert, mechanically resistant implant to the concept of a bioactive implant able to improve and fasten tissue integration (especially in the bone contact field) and is today mainly focused on the modulation of the host response to the implant: the goal is a physiological healing, which arises from the modulation of the inflammatory response.
As opposed to bioactivity, bone integration, and even antibacterial activity (see Sect. 1.4), the immunomodulation is still less explored and is actually highly debated in the scientific literature.
Some strategies for the control of the inflammatory response and foreign body reaction have, however, been proposed, such as the tailoring of protein adsorption, the modulation of macrophage polarization, the use of topographical patterns able to modulate macrophage response, the use of biomimetic coatings, the local delivery of anti-inflammatory drugs, the regulation of nitrogen monoxide (NO), and the induction of macrophage apoptosis (Spriano et al. 2018).
Some interesting strategies applied to Ti surfaces are briefly summarized below.
At first, an effect of surface topography on the host immunoresponse has been widely documented in the literature. A reduced attachment of macrophages and the production of anti-inflammatory factors (M2 polarization) have been documented on sandblasted and acid etched surfaces (SLA type) plasma treated to be super-hydrophilic (Hotchkiss et al. 2016) compared to standard tissue culture polystyrene. A combined effect of roughness and wettability has been noticed for these materials. Similarly, it has been observed that a nanotextured Ti oxide layer rich in OH groups (hydrophilic, but not super hydrophilic) on the surface of Ti microbeads implants can significantly reduce macrophage adhesion and increase the production of anti-inflammatory mediators (Barthes et al. 2020). An anti-inflammatory response of macrophages, mediated by an enhancement of the endothelial cells response and by the reduction of monocytes adhesion, has also been observed on nano- and sub-micrometer-sized rough Ti coatings, intended for cardiovascular applications (Lu and Webster 2015).
On the other hand, M1 macrophage polarization has been observed on TiO2 nanotubes with a diameter around 100 nm (He et al. 2020, Shen et al. 2019a). However, under oxidative stress, a shift to M2 polarization has been observed in coculture with mesenchymal stem cells (MSc) (Shen et al. 2019b), upon higher MSc recruitment followed by osteogenic differentiation. Moreover, it has been observed that different nanotextures, produced on commercially pure Ti by anodization, able to give an analogous osteogenic activity in vitro, promote different osteointegration in vivo. This effect has been explained by different macrophage polarization mediated by surface roughness.
Ti surfaces have been enriched with various ions, for example, copper (Cu), silver (Ag), and zinc (Zn), in order to promote a multifunctional response (e.g., addition of antibacterial activity) to the implant. Cu2+ ions have been introduced on micro-arc oxidized (MAO) Ti by hydrothermal treatment (Huang et al. 2019), by addition of Cu2+ ions into the anodization electrolyte (Huang et al. 2018), by selective laser melting of pure Cu (Xu et al. 2018), or by plasma immersion ion implantation (PIII) (Chen et al. 2021). The effect of Cu on the inflammatory response is controversial. Cu addition onto MAO Ti surfaces (Huang et al. 2018, 2019) induced macrophage polarization to the non-favorable inflammatory M1 state, however, a favorable microenvironment for osteogenesis, has been reported due to the release of the pro-osteogenic factor by macrophages cultured on these surfaces. Moreover, an antibacterial activity mediated by macrophages has been observed on these materials. On the other hand, an anti-inflammatory effect has been observed on Ti6Al4V alloy enriched with Cu by selective laser melting (Xu et al. 2018) and on PIII Ti (Chen et al. 2021). It has been observed that the addition of magnesium (Mg) to MAO Ti surfaces is able to promote M2 macrophage polarization (Li et al. 2018a).
An anti-inflammatory effect modulated by calcium (Ca) ions can be cited, considering the reduction of pro-inflammatory factors produced by macrophages on acid etched Ti, enriched with nanoscaled Ca phosphates (Nanotite, Biomet 3i) (Hamlet and Ivanovski 2011). A particular hybrid M1-M2 polarization of macrophages has been observed on hydroxyapatite-coated rough Ti surfaces (Zhang et al. 2019). Finally, ceria (CeO2) coatings on Ti substrates showed the ability to affect fibronectin orientation and macrophage polarization (M2 state) mediated by the valence state of the Ce ions (Shao et al. 2020).
At last, the strategy of grafting specific organic molecules on Ti surfaces can be reported. The effect of some coupling agents, often used for grafting of biomolecules, on the inflammatory response has been tested. It has been observed that (3-glycodoxypropyl)trimethoxy silane (GPTMS) increases the adsorption of complement proteins and the pro-inflammatory polarization (M1) of macrophages and reduces osteointegration of sandblasted, acid etched Ti, in a dose-dependent manner (Araújo-Gomes et al. 2019). On the other hand, amino propyl triethoxy silane (APTES) induced M2 macrophage polarization on NaOH treated Ti (Zhang et al. 2018b). A reduction of the inflammatory response has been observed on TiO2 nanotubes loaded with anti-inflammatory agents such as dexamethasone (Shen et al. 2020) or Interleukin 4(IL4) (Yin et al. 2019). Different peptides, such as a mussel-inspired peptide (Bai et al. 2020) or the cationic peptide cecropin B (Xu et al. 2013), have been coupled with Ti by coordination chemistry or polydopamine-mediated grafting, respectively. Both peptides enabled anti-inflammatory macrophage activity, improvement of osteoblast adhesion and activity, and antibacterial action. A macrophage recruitment agent (SEW2871), intercalated in layer-by-layer chitosan-gelatin coatings on dual acid-etched Ti (He et al. 2020), promoted rapid macrophage recruitment, anti-inflammatory activity, and osteogenesis in in vivo tests. Finally, a multifunctional response (anti-inflammatory, antibacterial, and pro-osteogenic) has been observed after surface grafting of two antibiotics: bacitracin (polydopamine-mediated covalent grafting to Ti6Al4V; Nie et al. 2016) or minocycline (introduced in layer-by-layer chitosan/gelatin coating onto Ti substrates; Shen et al. 2019b).
All these strategies are interesting and promising, but they are often difficult to implement due to the complexity of the biological system to be controlled. In fact, it should be remembered that inflammatory response should be controlled, but not completely suppressed, because it is necessary for tissue healing. Proteins (such as fibronectin), which act as pro-inflammatory agents, can also act as tissue repairing agents and their adsorption must not be completely avoided. The in vivo protein adsorption conditions and cross-talk among different cell types are complex mechanisms, usually different from the ones reproduced in conventional simple in vitro experiments. Moreover, it should be considered that surface modifications, which involve the use of active molecules, can significantly increase the complexity of the regulatory processes of the medical devices.
3.3 Inflammatory Response and Corrosion Resistance
As outlined in Sect. 1.2, there is increasing evidence that inflammatory response, which results in high redox potentials and the presence of hydrogen peroxide, has a considerable role in the degradation of Ti (alloys) and the release of metal ions. This is also true for Ti alloys that were optimized for osseointegration, although their corrosion resistance is higher and their metal release is lower, than that of Ti alloys with a thin, native, passive surface oxide (Hedberg et al. 2020).
4 Ti Surfaces for Bone Integration and Infection Control
4.1 Recent Strategies to Combine Bioactivity and Antibacterial Activity
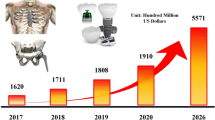
Prosthetic infections concern 1–2% of hip and knee replacements, and the percentage increases in the case of revision surgery or fixation of open fractures (up to 30–40%) (Trampuz and Widmer 2006). Moreover, prosthetic infections are among the most critical complications in orthopedic surgery because they are associated with both high morbidity and high hospital costs (Trampuz and Widmer 2006; Zimmerli et al. 2004). Even if a strict antibiotic and antibacterial perioperative prophylaxis is currently applied, which can significantly reduce the risk of infection, both orthopedic and dental implant-associated infections are mainly related to bacterial contamination of the implanted surfaces by the formation of a bacterial biofilm (Zimmerli et al. 2004; Subramani et al. 2009). The biofilm is a polysaccharidic structure, in which bacteria can grow and remain mostly unreached by systemic antibiotics and antimicrobial treatments. In this context, the development of antibacterial surfaces able to limit bacterial adhesion and proliferation is particularly promising.
A first strategy can be the reduction of bacterial adhesion to Ti surfaces without the introduction of any active antibacterial agent. This solution has the advantage that it is not time-limited (no consumption of antibacterial agent due to release), it does not involve potentially toxic substances, and does not require complex certification procedures associated with the release of active agents. On the other hand, it hardly fights infections in cases of severe bacterial contamination (e.g., septic situations). In this scenario, nanotextures have been proposed as potential anti-adhesive Ti surfaces. Nanopatterns, 10–100 nm in depth, have been reported to reduce bacterial adhesion and to impart mechanical stresses to bacterial cell walls, reducing bacterial viability (Linklater et al. 2020). The flexibility and the geometric features (e.g., sharp edges) of these nanotextures can further improve their effectiveness against bacteria. Mammalian cells, in contrast, can better accommodate stresses on nanotextured surfaces due to the higher deformability of their membrane, with resulting high biocompatibility and even cell stimulation ability (focal contact formation) for the host cells. Similarly, a reduced bacterial adhesion has been documented on bioactive nanotextured Ti oxide layers, even in the absence of any antibacterial agent (Ferraris et al. 2019). Recently, the role of surface microstructure of metal surfaces (induced by electron beam or thermal treatments) in reducing bacterial adhesion has also been reported (Ferraris et al. 2019b, 2020).
Several strategies have also been proposed for the realization of bactericidal Ti surfaces. The introduction of inorganic antibacterial agents (e.g., Ag, Cu, and Zn) by means of surface doping (e.g., ion implantation, in situ reduction, or alloys), growth and doping of TiO2 layers (e.g., anodization), or deposition of doped coatings (e.g., plasma spray, sputtering, or sol-gel), grafting of antimicrobial polymers, antimicrobial peptides, biomolecules, or antibiotics (by direct grafting, covalent grafting mediated by silanes, catechol or phosphates, or entrapment into coatings) can be cited among the most popular ones (Ferraris and Spriano 2016; Chouirfa et al. 2019; Hickok and Shapiro 2012).
There is a bacterial competition with host cells for surface colonization of implanted biomaterials, as reported in the well-known “race for the surface” (Gristina 1987). Therefore, implant surfaces able to reduce bacterial contamination and at the same time improve tissue adhesion (bioactive and antibacterial) can be of particular interest.
In this view, inorganic antibacterial agents, as well as antibiotics, have been coupled to bioactive Ti surfaces, such as Ca phosphates, hydroxyapatite, or bioactive glass coatings, bioactive TiO2 layers (obtained in the form of thick coatings, chemically modified thin layers, or nanotubes), porous coatings intended for bone ingrowth, or complex multilayer coatings (Ferraris and Spriano 2016; Chouirfa et al. 2019; Spriano et al. 2018; Raphel et al. 2016).
The above-cited solutions can simultaneously counteract bacterial infection and promote bone regeneration; however, it has been pointed out that in some cases infections can activate macrophages (lipopolysaccharide (LPS) stimulation) to recruit osteoclasts and induce infection-mediated osteolysis (Raphel et al. 2016). In these cases, the immunomodulation strategies discussed in Sect. 1.3 can be of interest to overcome the problem.
All the solutions discussed above are generally tested on bulk plane Ti (alloy) samples or model implants. Currently, additive manufacturing (AM) is becoming popular for the realization of customized Ti implants and the transfer of the developed technologies for generating bioactive and antibacterial surfaces on AM implants is under investigation (Li et al. 2020). Strategies able to modify both the inner and outer surfaces of pores are advantageous for this purpose.
4.2 Mechanical Stability
In order to be suitable for clinical applications, innovative antibacterial and bioactive surfaces should be able to sustain implantation loads and friction, as well as mechanical stresses, for the whole implant life. Otherwise, the effective surface exposed to the biological environment will not be the designed one (with antibacterial and bioactive functionalities) and the formation of wear debris can stimulate inflammatory reactions.
Adhesion and mechanical stability have been pointed out as critical issues in the application of anti-adhesive polymers (Raphel et al. 2016); however, they are not always well described for innovative multifunctional surfaces.
Coating adhesion is one of the key factors for the applicability of a coating to implantable medical devices. It can be measured in vitro by means of tensile tests, as suggested by ISO standard 13779-4, indentation, scratch, tape, pull-out or bending tests, as reported in the scientific literature for various antibacterial and bioactive coatings (Verné et al. 2008; Utku et al. 2015; Onoki et al. 2008; Ferraris et al. 2020b; Stan et al. 2013; Surmeneva et al. 2017). Moreover, the realization of customized implant simulation tests in non-vital animal bone has been reported as a successful strategy to test the resistance of new surfaces to implantation friction and loads (Ferraris et al. 2015; Li et al. 2018b).
The adhesion strength of coatings and modified surface layers is strongly affected by the surface pretreatment before coating deposition (e.g., realization of intermediate layers, chemical and electrochemical pretreatments aimed at improving the coating-substrate affinity, and mechanical interlocking), as well as by the process parameters (e.g., in the preparation of TiO2 nanotubes) or by post-treatments (such as thermal treatments or sterilization processes) and by coating thickness (Stan et al. 2013; Onoki et al. 2008; Utku et al. 2015; Li et al. 2018b; Surmeneva et al. 2017). Recently, it has been evidenced that the addition of graphene oxide to vancomycin-loaded strontium (Sr)doped hydroxyapatite electrodeposited on Ti surfaces can significantly improve the coating’s mechanical properties, such as hardness, elastic modulus, and adhesion (Zhang et al. 2020b). Considering bioactive and antibacterial surfaces, the reactivity in physiological environment is another critical factor to be considered, because it can affect their mechanical and chemical stability (Ferraris et al. 2020c).
4.3 Chemical Stability and Corrosion Resistance
For surface oxides incorporated with antimicrobial metal nanoparticles, such as Ag (Hedberg et al. 2020) and Cu (Bernstein et al. 2017) nanoparticles, galvanic effects could occur under certain circumstances. While only a slight effect was found in a study on Ti6Al4V with an artificially grown oxide with embedded Ag nanoparticles (Hedberg et al. 2020), a more pronounced galvanic effect was found for Ti6Al4V without such a thick oxide and coated with silver (Furko et al. 2016).
All in all, it is more likely that such surface engineering efforts would benefit the overall corrosion performance by reducing the extent of infection/inflammation; however, under certain circumstances, this galvanic couple could be a triggering factor for other corrosion types.
4.4 Ion/Nanoparticles Release
Infection control requires a certain release of antibacterial metal ions, such as Ag and Cu (Spriano et al. 2018). Ideally, this release is limited to ions, and does not include the metal nanoparticles themselves. However, some release of metal nanoparticles can be expected. Indeed, an increased release of particles was observed in vitro for Ti6Al4V with embedded Ag nanoparticles as compared to a Ag-free counterpart; however, it was unclear if this was due to released Ag nanoparticles or due to Ag-ion-induced protein aggregation (Hedberg et al. 2020). The actual measurable and stable ion release is strongly influenced by the solution chemistry of the metal. Ti ions are very unstable in most aqueous and physiologically relevant solutions, while the stability of Al, Ag, and V ions is strongly influenced by the presence of complexing agents such as proteins (Hedberg et al. 2020) and that of Cr ions can be influenced by the redox potential. This may result in the underestimation of Ti ion release and be a main explanation for the primarily TiO2-rich oxide growth and the frequently observed presence of TiO2 particles in vivo.
5 Conclusions
Even if Ti and Ti alloys are well-known for their high corrosion resistance and biocompatibility because they are usually greater than those of other metals used for biomedical implants, environmental conditions, especially infections and inflammatory conditions, can strongly affect their surface condition and corrosion. Relevant corrosion types are often caused by a combination of geometrical factors (i.e., crevices), mechanical factors, such as micromotions and fretting, physiological factors, such as inflammation and the presence of complexing proteins, and/or the coupling to other metals. Considering the importance of the physiological environment, the development of new Ti surfaces able to improve tissue bonding and physiological healing with a modulation of the inflammatory host response and control of infection development is of great interest.
Bioactive and antibacterial titanium surfaces have been widely explored in the scientific literature and some surface treatments are already on the market and there is clinical application with encouraging results. However, some concerns related to excessive inflammatory response and possibly infection-mediated osteolysis still exist. In this scenario, surfaces able to promote physiological healing, and also taking the inflammatory response to the implant into account, seem to be very promising. This topic is less explored and its clinical application is not yet ready. For this reason, it is worthy to be investigated in further scientific research.
References
Araújo-Gomes N, Romero-Gavilán F, Zhang Y, Martinez-Ramos C, Elortza F, Azkargorta M, Martín de Llano JJ, Gurruchaga M, Goñi I, van den Beucken JJJP, Suay J (2019) Complement proteins regulating macrophage polarisation on biomaterials. Colloids Surf B: Biointerfaces 181:125–133
Bai J, Wang H, Chen H, Ge G, Wang M, Gao A, Tong L, Xu Y, Yang H, Pan G, Chu PK, Geng D (2020) Biomimetic osteogenic peptide with mussel adhesion and osteoimmunomodulatory functions to ameliorate interfacial osseointegration under chronic inflammation. Biomaterials 255:120197
Barthes J, Cazzola M, Muller C, Dollinger C, Debry C, Ferraris S, Spriano S, Vrana NE (2020) Controlling porous titanium/soft tissue interactions with an innovative surface chemical treatment: responses of macrophages and fibroblasts. Mater Sci Eng C 112:110845
Bernstein A, Suedkamp N, Mayr HO, Gadow R, Burtscher S, Arhire I, Killinger A, Krieg P (2017) Chapter 5 - thin degradable coatings for optimization of osseointegration associated with simultaneous infection prophylaxis. In: Ficai A, Grumezescu AM (eds) Nanostructures for antimicrobial therapy. Elsevier, Amsterdam, pp 117–137. https://doi.org/10.1016/B978-0-323-46152-8.00005-6
Chan E, Cadosch D, Gautschi OP, Sprengel K, Filgueira L (2011) Influence of metal ions on human lymphocytes and the generation of titanium-specific T-lymphocytes. J Appl Biomater Biomech 9(2):137–143. https://doi.org/10.5301/jabb.2011.8567
Chen JK, Thyssen JP (eds) (2018) Metal allergy - from dermatitis to implant and device failure, 1st edn. Springer, Cham. https://doi.org/10.1007/978-3-319-58503-1
Chen C, Zhang S-M, Lee I-S (2013) Immobilizing bioactive molecules onto titanium implants to improve osseointegration. Surf Coat Technol 228:S312–S317
Chen L, Wang D, Qiu J, Zhang X, Liu X, Qiao Y, Liu X (2021) Synergistic effects of immunoregulation and osteoinduction of ds-block elements on titanium surface. Bioact Mater 6:191–207
Chouirfa H, Bouloussa H, Migonney V, Falentin-Daudré C (2019) Review of titanium surface modification techniques and coatings for antibacterial applications. Acta Biomater 83:37–54
Claesson PM, Blomberg E, Fröberg JC, Nylander T, Arnebrant T (1995) Protein interactions at solid surfaces. Adv Colloid Interface Sci 57:161–227
Clarke CF, Hardie D, Ikeda BM (1997) Hydrogen-induced cracking of commercial purity titanium. Corros Sci 39(9):1545–1559
Cortada M, Giner L, Costa S, Gil FJ, Rodríguez D, Planell JA (2000) Galvanic corrosion behavior of titanium implants coupled to dental alloys. J Mater Sci Mater Med 11(5):287–293. https://doi.org/10.1023/a:1008905229522
Ding R, Shang J-X, Wang F-H, Chen Y (2018) Electrochemical Pourbaix diagrams of NiTi alloys from first-principles calculations and experimental aqueous states. Comput Mater Sci 143:431–438. https://doi.org/10.1016/j.commatsci.2017.11.033
Eliades T, Pratsinis H, Kletsas D, Eliades G, Makou M (2004) Characterization and cytotoxicity of ions released from stainless steel and nickel-titanium orthodontic alloys. Am J Orthod Dentofacial Orthop 125(1):24–29
Evrard L, Waroquier D, Parent D (2010) Allergies to dental metals. Titanium: a new allergen. Revue médicale de Bruxelles 31(1):44
Faccioni F, Franceschetti P, Cerpelloni M, Fracasso ME (2003) In vivo study on metal release from fixed orthodontic appliances and DNA damage in oral mucosa cells. Am J Orthod Dentofacial Orthop 124(6):687–693
Ferraris S, Spriano S (2016) Antibacterial titanium surfaces for medical implants. Mater Sci Eng C 61:965–978
Ferraris S, Bobbio A, Miola M, Spriano S (2015) Micro- and nano-textured, hydrophilic and bioactive titanium dental implants. Surf Coat Technol 276:374–383
Ferraris S, Cochis A, Cazzola M, Tortello M, Scalia A, Spriano S, Rimondini L (2019) Cytocompatible and anti-bacterial adhesion Nanotextured titanium oxide layer on titanium surfaces for dental and orthopedic implants. Front Bioeng Biotechnol 7:103. https://doi.org/10.3389/fbioe.2019.00103
Ferraris S, Warchomicka F, Ramskogler C, Tortello M, Cochis A, Scalia A, Gautier di Confiengo G, Keckes J, Rimondini L, Spriano S (2019b) Surface structuring by electron beam for improved soft tissues adhesion and reduced bacterial contamination on Ti-grade 2. J Mater Process Technol 266:518–529
Ferraris S, Warchomicka F, Iranshahi F, Rimondini L, Cochis A, Spriano S (2020) Electron beam structuring of Ti6Al4V: new insights on the metal surface properties influencing the bacterial adhesion. Materials 2020(13):409. https://doi.org/10.3390/ma13020409
Ferraris S, Perero S, Costa P, Gautier di Confiengo G, Cochis A, Rimondini L, Renaux F, Vernè E, Ferraris M, Spriano S (2020b) Antibacterial inorganic coatings on metallic surfaces for temporary fixation devices. Appl Surf Sci 508:144707
Ferraris S, Yamaguchi S, Barbani N, Cristallini C, Gautier di Confiengo G, Barberi J, Cazzola M, Miola M, Vernè E, Spriano S (2020c) The mechanical and chemical stability of the interfaces in bioactive materials: the substrate-bioactive surface layer and hydroxyapatitebioactive surface layer interfaces. Mater Sci Eng C 116:111238
Fukuzaki S, Urano H, Nagata K (1995) Adsorption of protein onto stainless-steel surfaces. J Ferment Bioeng 80(1):6–11. https://doi.org/10.1016/0922-338X(95)98168-K
Furko M, Lakatos-Varsányi M, Balázsi C (2016) Complex electrochemical studies on silver-coated metallic implants for orthopaedic application. J Solid State Electrochem 20(1):263–271. https://doi.org/10.1007/s10008-015-3026-1
Gilbert J (2017) Corrosion in the human body: metallic implants in the complex body environment. Corrosion 73(12):1478–1495. https://doi.org/10.5006/2563
Gilbert JL, Kubacki GW (2016) Chapter three - oxidative stress, inflammation, and the corrosion of metallic biomaterials: corrosion causes biology and biology causes corrosion A2 - Dziubla, Thomas. In: Butterfield DA (ed) Oxidative stress and biomaterials. Academic, Boston, pp 59–88. https://doi.org/10.1016/B978-0-12-803269-5.00003-6
Gilbert JL, Mali S, Urban RM, Silverton CD, Jacobs JJ (2012) In vivo oxide-induced stress corrosion cracking of Ti-6Al-4V in a neck–stem modular taper: emergent behavior in a new mechanism of in vivo corrosion. J Biomed Mater Res B 100(2):584–594
Gilbert JL, Sivan S, Liu Y, Kocagöz SB, Arnholt CM, Kurtz SM (2015) Direct in vivo inflammatory cell-induced corrosion of CoCrMo alloy orthopedic implant surfaces. J Biomed Mater Res A 103(1):211–223. https://doi.org/10.1002/jbm.a.35165
Gong Z, Li M, Guo X, Ma Z, Shi J (2013) Stent implantation in patients with metal allergy: a systemic review and meta-analysis. Coron Artery Dis 24(8):684–689
Grande F, Tucci P (2016) Titanium dioxide nanoparticles: a risk for human health? Mini Rev Med Chem 16(9):762–769
Gristina AG (1987) Biomaterial-centered infection: microbial adhesion versus tissue integration. Science 237:1588–1595
Hall DJ, Pourzal R, Lundberg HJ, Mathew MT, Jacobs JJ, Urban RM (2017) Mechanical, chemical and biological damage modes within head-neck tapers of CoCrMo and Ti6Al4V contemporary hip replacements. J Biomed Mater Res B. https://doi.org/10.1002/jbm.b.33972
Hall DJ, Pourzal R, Lundberg HJ, Mathew MT, Jacobs JJ, Urban RM (2018) Mechanical, chemical and biological damage modes within head-neck tapers of CoCrMo and Ti6Al4V contemporary hip replacements. J Biomed Mater Res B 106(5):1672–1685. https://doi.org/10.1002/jbm.b.33972
Hamann C (2018) Metal allergy: titanium. In: Chen J, Thyssen JP (eds) Metal allergy. Springer, Cham, pp 443–466
Hamlet S, Ivanovski S (2011) Inflammatory cytokine response to titanium chemical composition and nanoscale calcium phosphate surface modification. Acta Biomater 7:2345–2353
He X, Noël JJ, Shoesmith DW (2009) Crevice corrosion of grade-12 titanium. In: Papavinasam S, Berke N, Brossia S (eds) Advances in electrochemical techniques for corrosion monitoring and measurement. ASTM International, West Conshohocken, pp 281–299. https://doi.org/10.1520/STP48753S
He Y, Xu K, Li K, Yuan Z, Ding Y, Chen M, Lin C, Tao B, Li X, Zhang G, Liu P, Cai K (2020) Improved osteointegration by SEW2871-encapsulated multilayers on micro-structured titanium via macrophages recruitment and immunomodulation. Appl Mater Today 20:100673
Hedberg YS (2018) Role of proteins in the degradation of relatively inert alloys in the human body. NPJ Materials Degrad 2:26. https://doi.org/10.1038/s41529-018-0049-y
Hedberg YS, Odnevall Wallinder I (2016) Metal release from stainless steel in biological environments: a review. Biointerphases 11(1):018901-018901–018901-018917. https://doi.org/10.1116/1.4934628
Hedberg Y, Karlsson M-E, Blomberg E, Odnevall Wallinder I, Hedberg J (2014) Correlation between surface physicochemical properties and the release of iron from stainless steel AISI 304 in biological media. Colloid Surface B 122:216–222. https://doi.org/10.1016/j.colsurfb.2014.06.066
Hedberg YS, Dobryden I, Chaudhary H, Wei Z, Claesson P, Lendel C (2019a) Synergistic effects of metal-induced aggregation of human serum albumin. Colloid Surf B 173:751–758. https://doi.org/10.1016/j.colsurfb.2018.10.061
Hedberg YS, Žnidaršič M, Herting G, Milošev I, Odnevall Wallinder I (2019b) Mechanistic insight on the combined effect of albumin and hydrogen peroxide on surface oxide composition and extent of metal release from Ti6Al4V. J Biomed Mater Res B 107(3):858–867. https://doi.org/10.1002/jbm.b.34182
Hedberg YS, Gamna F, Padoan G, Ferraris S, Cazzola M, Herting G, Atapour M, Spriano S, Odenvall Wallinder I (2020) Surface modified Ti6Al4V for enhanced bone bonding ability - effects of silver and corrosivity at simulated physiological conditions from a corrosion and metal release perspective. Corros Sci 168:108566. https://doi.org/10.1016/j.corsci.2020.108566
Hickok NJ, Shapiro IM (2012) Immobilized antibiotics to prevent orthopaedic implant infections. Adv Drug Deliv Rev 64:1165–1176
Hosoki M, Nishigawa K, Miyamoto Y, Ohe G, Matsuka Y (2016) Allergic contact dermatitis caused by titanium screws and dental implants. J Prosthodont Res 60(3):213–219
Hotchkiss KM, Reddy GB, Hyzy SL, Schwartz Z, Boyan BD, Olivares-Navarrete R (2016) Titanium surface characteristics, including topography and wettability, alter macrophage activation. Acta Biomater 31:425–434
Huang Q, Li X, Elkhooly TA, Liu X, Zhang R, Wu H, Feng Q, Liu Y (2018) The Cu-containing TiO2 coatings with modulatory effects on macrophage polarization and bactericidal capacity prepared by micro-arc oxidation on titanium substrates. Colloids Surf B Biointerfaces 170:242–250
Huang Q, Ouyang Z, Tan Y, Wu H, Liu Y (2019) Activating macrophages for enhanced osteogenic and bactericidal performance by Cu ion release from micro/nano-topographical coating on a titanium substrate. Acta Biomater 100:415–426
Jin T, Berlin M (2015) Titanium. In: Nordberg GF, Fowler BA, Nordberg M (eds) Handbook on the toxicology of metals, vol 2, 4th edn. Elsevier, Amsterdam, pp 1287–1296
Kasemo B (2002) Biological surface science surface. Science 500:656–677
Kokubo T, Yamaguchi S (2016) Novel bioactive materials developed by simulated body fluid evaluation: surface-modified Ti metal and its alloys. Acta Biomater 44:16–30
Kumazawa R, Watari F, Takashi N, Tanimura Y, Uo M, Totsuka Y (2002) Effects of Ti ions and particles on neutrophil function and morphology. Biomaterials 23(17):3757–3764
Li X, Wang J, E-h H, Ke W (2007) Influence of fluoride and chloride on corrosion behavior of NiTi orthodontic wires. Acta Biomater 3(5):807–815. https://doi.org/10.1016/j.actbio.2007.02.002
Li X, Huang Q, Liu L, Zhu W, Elkhooly TA, Liu Y, Feng Q, Li Q, Zhou S, Liu Y, Wu H (2018a) Reduced inflammatory response by incorporating magnesium into porous TiO2 coating on titanium substrate. Colloids Surf B Biointerfaces 171:276–284
Li T, Gulati K, Wang N, Zhang Z, Ivanovski S (2018b) Understanding and augmenting the stability of therapeutic nanotubes on anodized titanium implants. Mater Sci Eng C 88:182–195
Li J, Cui X, Hooper GJ, Lim KS, Woodfield TBF (2020) Rational design, bio-functionalization and biological performance of hybrid additive manufactured titanium implants for orthopaedic applications: a review. J Mech Behav Biomed Mater 105:103671
Linklater DP, Baulin VA, Juodkazis S, Crawford RJ, Stoodley P, Ivanova EP (2020) Mechano-bactericidal actions of nanostructured surfaces. Nat Rev Microbiol. https://doi.org/10.1038/s41579-020-0414-z
Londono R, Badylak SF (2015) Factors which affects the host response to biomaterials. In: Badylak SF (ed) Host response to biomaterials. Elsevier, Amsterdam
Lu J, Webster TJ (2015) Reduced immune cell responses on nano and submicron rough titanium. Acta Biomater 16:223–231
Lucas LC, Buchanan RA, Lemons JE (1981) Investigations on the galvanic corrosion of multialloy total hip prostheses. J Biomed Mater Res 15(5):731–747. https://doi.org/10.1002/jbm.820150509
Lugovskoy A, Lugovskoy S (2014) Production of hydroxyapatite layers on the plasma electrolytically oxidized surface of titanium alloys. Mater Sci Eng C 43:527–532
Mani G, Feldman MD, Patel D, Agrawal CM (2007) Coronary stents: a materials perspective. Biomaterials 28(9):1689–1710
McCafferty E (2010) Thermodynamics of corrosion: Pourbaix diagrams. In: Introduction to corrosion science. Springer, New York, pp 95–117. https://doi.org/10.1007/978-1-4419-0455-3_6
Milošev I (2017) From in vitro to retrieval studies of orthopedic implants. Corrosion 73(12):1496–1509
Milošev I, Metikos-Hukovic M, Strehblow HH (2000) Passive film on orthopaedic TiAlV alloy formed in physiological solution investigated by X-ray photoelectron spectroscopy. Biomaterials 21(20):2103–2113
Milošev I, Kosec T, Strehblow HH (2008) XPS and EIS study of the passive film formed on orthopaedic Ti–6Al–7Nb alloy in Hank’s physiological solution. Electrochim Acta 53(9):3547–3558. https://doi.org/10.1016/j.electacta.2007.12.041
Mirjalili M, Momeni M, Ebrahimi N, Moayed MH (2013) Comparative study on corrosion behaviour of nitinol and stainless steel orthodontic wires in simulated saliva solution in presence of fluoride ions. Mater Sci Eng C 33(4):2084–2093. https://doi.org/10.1016/j.msec.2013.01.026
Nelson JC, Oriani RA (1993) Stress generation during anodic oxidation of titanium and aluminum. Corros Sci 34(2):307–326
Nie B, Ao H, Zhou J, Tang T, Yue B (2016) Biofunctionalization of titanium with bacitracin immobilization shows potential for anti-bacteria, osteogenesis and reduction ofmacrophage inflammation. Colloids Surf B Biointerfaces 145:728–739
Noël JJ (1999) The electrochemistry of titanium corrosion. PhD Thesis, The University of Manitoba, Manitoba
Noël J, Ebrahimi N, Shoesmith D (2018) Corrosion of titanium and titanium alloys. In: Wandelt K (ed) Encyclopedia of interfacial chemistry: surface science and electrochemistry, vol 6. Elsevier, Amsterdam, pp 192–200
Noguchi T, Takemoto S, Hattori M, Yoshinari M, Kawada E, Oda Y (2008) Discoloration and dissolution of titanium and titanium alloys with immersion in peroxide-or fluoride-containing solutions. Dent Mater J 27(1):117–123
Oliver JN, Su Y, Lu X, Kuo P-H, Du J, Zhu D (2019) Bioactive glass coatings on metallic implants for biomedical applications. Bioact. Mater 4:261–270
Olmedo DG, Tasat DR, Guglielmotti MB, Cabrini RL (2008) Biodistribution of titanium dioxide from biologic compartments. J Mater Sci Mater Med 19(9):3049–3056. https://doi.org/10.1007/s10856-008-3438-x
Onoki T, Hosoi K, Hashida T, Tanabe Y, Watanabe T, Yasuda E, Yoshimura M (2008) Effects of titanium surface modifications on bonding behavior of hydroxyapatite ceramics and titanium by hydrothermal hot-pressing. Mater Sci Eng C 28:207–212
Peters RJ, Oomen AG, van Bemmel G, van Vliet L, Undas AK, Munniks S, Bleys RL, Tromp PC, Brand W, van der Lee M (2020) Silicon dioxide and titanium dioxide particles found in human tissues. Nanotoxicology 14(3):420–432
Pourbaix M (1974) Atlas of electrochemical equilibria in aqueous solution. NACE, Houston
Raphel J, Holodniy M, Goodman SB, Heilshorn SC (2016) Multifunctional coatings to simultaneously promote osseointegration and prevent infection of orthopaedic implants. Biomaterials 84:301e314
Ratner BD (2001) Replacing and renewing: synthetic materials, biomimetics, and tissue engineering in implant dentistry. J Dent Educ 65:1340–1347
Reclaru L, Meyer JM (1998) Effects of fluorides on titanium and other dental alloys in dentistry. Biomaterials 19(1):85–92. https://doi.org/10.1016/S0142-9612(97)00179-8
Sarmiento-González A, Encinar JR, Marchante-Gayón JM, Sanz-Medel A (2008) Titanium levels in the organs and blood of rats with a titanium implant, in the absence of wear, as determined by double-focusing ICP-MS. Anal Bioanal Chem 393(1):335. https://doi.org/10.1007/s00216-008-2449-2
Saylor DM, Adidharma L, Fisher JW, Brown RP (2016) A biokinetic model for nickel released from cardiovascular devices. Regul Toxicol Pharmacol 80:1–8. https://doi.org/10.1016/j.yrtph.2016.05.019
Schmets J, van Muylder J, Pourbaix M (1974) Titanium. In: Pourbaix M (ed) Atlas of electrochemical equilibria in - aqueous solutions. NACE, Houston, pp 213–222
Shakeel M, Jabeen F, Shabbir S, Asghar MS, Khan MS, Chaudhry AS (2016) Toxicity of Nano-titanium dioxide (TiO2-NP) through various routes of exposure: a review. Biol Trace Elem Res 172(1):1–36. https://doi.org/10.1007/s12011-015-0550-x
Shao D, Li K, You M, Liu S, Hu T, Huang L, Xie Y, Zheng X (2020) Macrophage polarization by plasma sprayed ceria coatings on titanium-based implants: cerium valence state matters. Appl Surf Sci 504:144070
Shen X, Yu Y, Ma P, Luo Z, Hu Y, Li M, He Y, Zhang Y, Peng Z, Song G, Cai K (2019a) Titania nanotubes promote osteogenesis via mediating crosstalk between macrophages and MSCs under oxidative stress. Colloids Surf B Biointerfaces 180:39–48
Shen X, Gu H, Ma P, Luo Z, Li M, Hu Y, Cai K (2019b) Minocycline-incorporated multilayers on titanium substrates for simultaneous regulation of MSCs and macrophages. Mater Sci Eng C 102:696–707
Shen K, Tang Q, Fang X, Zhang C, Zhu Z, Hou Y, Lai M (2020) The sustained release of dexamethasone from TiO2 nanotubes reinforced by chitosan to enhance osteoblast function and anti-inflammation activity. Mater Sci Eng C 116:111241
Shukla AK, Balasubramaniam R, Bhargava S (2005) Properties of passive film formed on CP titanium, Ti–6Al–4V and Ti–13.4Al–29Nb alloys in simulated human body conditions. Intermetallics 13(6):631–637. https://doi.org/10.1016/j.intermet.2004.10.001
Souza JCM, Sordi MB, Kanazawa M, Ravindran S, Henriques B, Silva FS, Aparicio C, Cooper LF (2019) Nano-scale modification of titanium implant surfaces to enhance osseointegration. Acta Biomater 94:112–131
Spriano S, Ferraris S, Bianchi CL, Cassinelli C, Torricelli P, Fini M, Rimondini L, Giardino R (2010) Bioactive titanium surfaces. In: Sanchez PN (ed) Titanium alloys: preparation, properties and applications. Nova Science, New York. ISBN: 978-1-60876-151-7
Spriano S, Yamaguchi S, Baino F, Ferraris S (2018) A critical review of multifunctional titanium surfaces: new frontiers for improving osseointegration and host response, avoiding bacteria contamination. Acta Biomater 79:1–22
Stan GE, Popa AC, Galca AC, Aldica G, Ferreira JMF (2013) Strong bonding between sputtered bioglass–ceramic films and Ti-substrate implants induced by atomic inter-diffusion post-deposition heat-treatments. Appl Surf Sci 280:530–538
Stanford CM (2010) Surface modification of biomedical and dental implants and the processes of inflammation, wound healing and bone formation Int. J Mol Sci 11(1):354–369. https://doi.org/10.3390/ijms11010354
Suárez C, Vilar T, Gil J, Sevilla P (2010) In vitro evaluation of surface topographic changes and nickel release of lingual orthodontic archwires. J Mater Sci Mater Med 21(2):675–683. https://doi.org/10.1007/s10856-009-3898-7
Subramani K, Jung RE, Molenberg A, Hämmerle CHF (2009) Biofilm on dental implants: a review of the literature. Int J Oral Maxillofac Implants 24(4):616–626
Sullivan SJL, Dreher ML, Zheng J, Chen L, Madamba D, Miyashiro K, Trépanier C, Nagaraja S (2015) Effects of oxide layer composition and radial compression on nickel release in nitinol stents. Shape Memory Superelasticity 1(3):319–327. https://doi.org/10.1007/s40830-015-0028-x
Sundfeldt M, Carlsson LV, Johansson CB, Thomsen P, Gretzer C (2006) Aseptic loosening, not only a question of wear: a review of different theories. Acta Orthop 77(2):177–197
Surmeneva MA, Sharonova AA, Chernousova S, Prymak O, Loza K, Tkachev MS, Shulepov IA, Epple M, Surmenev RA (2017) Incorporation of silver nanoparticles into magnetron-sputteredcalcium phosphate layers on titanium as an antibacterial coating. Colloids Surf B Biointerfaces 156:104–113
Swaminathan V, Gilbert JL (2012) Fretting corrosion of CoCrMo and Ti6Al4V interfaces. Biomaterials 33(22):5487–5503
Swiatkowska I, Mosselmans JFW, Geraki T, Wyles CC, Maleszewski JJ, Henckel J, Sampson B, Potter DB, Osman I, Trousdale RT, Hart AJ (2018) Synchrotron analysis of human organ tissue exposed to implant material. J Trace Element Med Biol 46:128–137. https://doi.org/10.1016/j.jtemb.2017.12.007
Tal-Gutelmacher E, Eliezer D (2005) Hydrogen cracking in titanium-based alloys. J Alloys Compd 404:621–625
Thewes M, Kretschmer R, Gfesser M, Rakoski J, Nerlich M, Borelli S, Ring J (2001) Immunohistochemical characterization of the perivascular infiltrate cells in tissues adjacent to stainless steel implants compared with titanium implants. Arch Orthop Trauma Surg 121(4):223–226
Trampuz A, Widmer AS (2006) Infections associated with orthopedic implants. Curr Opin Infect Dis 19:349–356
Utku FS, Seckin E, Goller G, Tamerler C, Urgen M (2015) Electrochemically designed interfaces: hydroxyapatite coated macro-mesoporous titania surfaces. Appl Surf Sci 350:62–68
Verné E, Ferraris S, Miola M, Fucale G, Maina G, Robotti P, Bianchi G, Martinasso G, Canuto RA, Vitale-Brovarone C (2008) Synthesis and characterisation of bioactive and antibacterial glass-ceramic part 2 – plasma spray coatings on metallic substrates. Adv Appl Ceram 107:245–253
Xu D, Yang W, Hu Y, Luo Z, Li J, Hou Y, Liu Y, Cai K (2013) Surface functionalization of titanium substrates with cecropin B to improve their cytocompatibility and reduce inflammation responses. Colloids Surf B Biointerfaces 110:225–235
Xu Z, Lu Y, Li S, Guo S, He M, Luo K, Lin J (2018) Copper-modified Ti6Al4V alloy fabricated by selective laser melting with pro-angiogenic and anti-inflammatory properties for potential guided bone regeneration applications. Mater Sci Eng C 90:198–210
Yao Z, Lin TH, Pajarinen J, Sato T, Goodman S (2015) Host response to orthopedic implants (metals and plastics). In: Badylak SF (ed) Host response to biomaterials. Elsevier, Amsterdam
Yin X, Li Y, Yang C, Weng J, Wang J, Zhou J, Feng B (2019) Alginate/chitosan multilayer films coated on IL-4-loaded TiO2 nanotubes for modulation of macrophage phenotype. Int J Biol Macromol 133:503–513
Yu F, Addison O, Davenport AJ (2015) A synergistic effect of albumin and H2O2 accelerates corrosion of Ti6Al4V. Acta Biomater 26:355–365
Zhang Y, Addison O, Yu F, Troconis BCR, Scully JR, Davenport AJ (2018a) Time-dependent enhanced corrosion of Ti6Al4V in the presence of H2O2 and albumin. Sci Rep 8(1):3185
Zhang H, Wu X, Wang G, Liu P, Qin S, Xu K, Tong D, Ding H, Tang H, Ji F (2018b) Macrophage polarization, inflammatory signaling, and NF-B activation in response to chemically modified titanium surfaces. Colloids Surf B Biointerfaces 166:269–276
Zhang Y, Cheng X, Jansen JA, Yang F, van den Beucken JJJP (2019) Titanium surfaces characteristics modulate macrophage polarization. Mater Sci Eng C 95:143–151
Zhang C, He L, Chen Y, Dai D, Su Y, Shao L (2020a) Corrosion behavior and in vitro cytotoxicity of Ni–Ti and stainless steel arch wires exposed to lysozyme, ovalbumin, and bovine serum albumin. ACS Omega. https://doi.org/10.1021/acsomega.0c02312
Zhang X, Song G, Qiao H, Lan J, Wang B, Yang H, Ma L, Wang S, Wang Z, Lin H, Han S, Kang S, Chang X, Huang Y (2020b) Novel ternary vancomycin/strontium doped hydroxyapatite/graphene oxide bioactive composite coatings electrodeposited on titanium substrate for orthopedic applications. Colloids Surf A Physicochem Eng Asp 603:125223
Zimmerli WJ, Trampuz A, Ochsner PE (2004) Prosthetic-joint infections. N Engl J Med 351:16. www.nejm.org. Accessed 14 Oct 2004
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Ferraris, S., Hedberg, Y.S., Noël, J.J., Spriano, S. (2022). Interactions Between the Physiological Environment and Titanium-Based Implant Materials: From Understanding to Control. In: Pandey, L.M., Hasan, A. (eds) Nanoscale Engineering of Biomaterials: Properties and Applications . Springer, Singapore. https://doi.org/10.1007/978-981-16-3667-7_1
Download citation
DOI: https://doi.org/10.1007/978-981-16-3667-7_1
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-3666-0
Online ISBN: 978-981-16-3667-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)