Abstract
Antimicrobial resistance is one of the most urgent health crises in the twenty-first century. Multiple factors including population explosion, industrial expansion, lifestyle changes, ease of global migration, and over-the-counter access to antimicrobials in the pharmacy contribute to the rapid emergence and spread of resistant pathogens. The resistant microbes are ubiquitously distributed both in the hospitals and in other environments. However, the prevalence of antibiotic resistance traits is very high in the six bacterial species, which are named as “ESKAPE” pathogens, an acronym for Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species. Resistant bacteria neutralize the bactericidal or bacteriostatic activity of antibiotics either by altering amino acid sequences of the target molecule or by modifying the chemical structure of antibiotics. In addition, proteins located in the bacterial cell surface contribute significantly to antibiotic resistance by reducing the effective intracellular concentration of antibiotics by reducing membrane permeability or increasing expelling activity. In the ESKAPE pathogens, antibiotic resistance genes are most often genetically linked with mobile genetic elements and disseminate rapidly by horizontal and vertical gene transfer. In the present report, we have provided updated and comprehensive pictures of antibiotic resistance in the ESKAPE pathogens.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1.1 Introduction
Antimicrobial-resistant bacterial pathogens responsible for several infectious diseases are a predominant threat to human health and global economy. Several factors contributing to this threat include population explosion, industrial expansion, lifestyle changes, ease of global migration, lack of adequate medical facilities in the developing countries, and – the most alarming of all – emergence of antimicrobial resistance. Antimicrobial resistance (AMR) among community- and hospital-associated bacterial species is exponentially growing, and it has been estimated that, by 2050, it would be responsible for the death of one person every 3 s (Review on Antimicrobial Resistance 2016). The imprudent usage of antimicrobials (including antibiotics, antivirals, antifungals, etc.) has aggravated this lurking threat of AMR. At a global level, from 2000 to 2010, the usage of antimicrobials was observed to have increased by >30%, with the low- and middle-income countries (LMICs) being the major contributors, on account of high prevalence of infectious diseases, easy availability, and reduced cost of antimicrobials (Klein et al. 2021). Since the last 70 years, the compelling enrichment of the AMR genes in bacterial population has been ascribed to the activities of humans such as rampant antibiotic usage in hospitals, agriculture, poultry, and animal husbandry.
Antibiotics are known as the chemical compounds produced by the microorganisms, which either kill or inhibit the growth of other microbes in their vicinity and help the bacteria to outcompete other strains present in their niche and to gain fitness advantage (Fig. 1.1, Lew 2014). The development of antibiotic resistance against the pathogenic bacteria develops as soon as the concerned pathogen develops various resistance mechanisms rendering the action of the antibiotic to be ineffective (Fig. 1.1, Das et al. 2017). The microorganisms harboring the antimicrobial resistance genes (ARGs) are mostly referred to as the antibiotic-resistant strains or the superbugs. Hospitals are considered as the nodal points for the AMR dissemination as the antibiotic usage in hospitals exerts selective pressure and accelerates the progression to acquiring antibiotic resistance (Dijkshoorn et al. 2007). The AMR strains are ubiquitous in the hospitals as well as in other environments, such as water bodies, soil, human body, livestock, and industrial effluents. However, the problem of resistance is not uniformly distributed across all the bacterial pathogens. The Infectious Diseases Society of America (IDSA) has identified six different bacterial species to be threats due to their virulence and evolution of resistance mechanisms against commonly prescribed antibiotics. They are named as “ESKAPE” pathogens, an acronym for Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species. This group of bacterial pathogens includes both Gram-negative and Gram-positive species that are proficient in “escaping” or evading the antimicrobial actions of conventional antibiotics. These pathogens are accountable for life-threatening infections, especially among the children, elderly, immunocompromised, as well as those who are critically ill. ESKAPE pathogens are associated with high mortality and morbidity resulting in higher healthcare costs (Founou et al. 2017). These pathogens have been recently listed in the list of 12 bacteria by WHO to accelerate the development of new antibiotics (Tacconelli et al. 2018). The pathogens have been divided into three categories, namely, critical, high, and medium priority, in accordance with the urgency of requirement for new antibiotics. Carbapenem-resistant K. pneumoniae, A. baumannii, and P. aeruginosa along with extended-spectrum β-lactamase (ESBL) Enterobacter spp. are listed in the critical priority. Vancomycin-resistant E. faecium (VRE) and methicillin- and vancomycin-resistant S. aureus (MRSA and VRSA) are listed high-priority group. Drawing attention toward the ESKAPE pathogens would help to combat the mounting challenge of AMR.
Action of antibiotics and mechanism of antibiotic resistance. Target of different antibiotics is fairly distinct. Antibiotics can impede DNA replication, transcription, translation, cell wall biosynthesis, or integrity of nucleic acids or cell membrane by inhibiting activity of the key molecules involved in the metabolic or maintenance process. However, bacteria can neutralize the bactericidal or bacteriostatic activity of antibiotics by altering composition of the target molecules or by introducing chemical modification in the antibiotic molecules. Some enzymes involved in the antibiotic resistance process can hydrolyze the antibiotics. Several proteins located in the cell membrane confer antibiotic resistance by reducing the effective intracellular concentration of antibiotics by reducing permeability or increasing expelling activity. Few antibiotics are unable to kill bacteria because of the overproduction of their target molecules. Several mobile genetic elements disseminate antibiotic resistance genes rapidly through horizontal gene transfer
The AMR crisis has been responsible for more than 35,000 deaths and around two million infections annually in the USA (https://www.cdc.gov/drugresistance/). The infection due to AMR bacteria has claimed the lives of 58,000 babies in India in a single year (Gandra et al. 2019). Indeed, the global epidemic of antibiotic resistance will unfold before all of us in no time. Hence, a comprehensive approach to unravel the origin of the resistance determinants in these ESKAPE pathogens, along with their arsenals of AMR including those associated with dissemination and maintenance of the resistance traits, will help to tackle this menace.
1.2 Antibiotics for the Treatment of Infections Caused by ESKAPE Pathogens
The commonly used treatment regimens for infections by ESKAPE pathogens include the antibiotics delivered singly or in combination (Table 1.1). Currently used treatment options are dwindling with the emergence of MDR strains, predisposing us toward the looming threat. Various alternative therapies such as bacteriophage therapy, nanoparticle-based antimicrobials and drug delivery systems, antimicrobial peptides, adjuvants, phytochemicals, and photodynamic therapy are looked as an option to combat AMR (Mandal et al. 2014).
Antibiotics used in combinations have often been found to be more efficient in combating infections by MDR organisms. When treating E. faecium and S. aureus, the Gram-positive members of the ESKAPE pathogens, with a combination of fosfomycin and daptomycin it has been observed to successfully clear the infection (Snyder et al. 2016; Coronado-Álvarez et al. 2019). On the other hand, antibiotic combinations checked against S. aureus include the antibiotic daptomycin or vancomycin and a newly added antibiotic ceftaroline. Colistin (polymyxin E) has been put into use as the last resort antibiotic against Gram-negative bacilli. A combination of colistin or tigecycline with other antibiotics has been tested to treat infections caused by K. pneumoniae and A. baumannii and has shown promising results.
1.3 Origin and Evolution of Antimicrobial Resistance Traits in ESKAPE Pathogens.
The origin of the antibiotics and the antibiotic resistance genes (ARGs) dates back to millions and billions of years (Martinez 2009, Baltz 2008). A study by D’Costa et al. (2011) showed the presence of resistance genes against β-lactams, glycopeptide, and tetracycline antibiotics in the metagenomic samples of 30,000-year-old permafrost, woolly mammoths, and animal and plant species of the Pleistocene. The antibiotic production and the selection of resistance genes are a result of Darwinian selection, which provides antibiotic-resistant bacteria with a selective advantage of niche exploitation (Waksman and Woodruff 1940). The producers of antibiotics are equipped with self-resistance gene determinants, and their expression is co-regulated with antibiotic biosynthesis gene. These resistance mechanisms can get disseminated to non-producer species in a niche where different strains co-exist together.
The golden era of antibiotics got shadowed due to the emergence of resistance to the frontline antimicrobial agents, such as sulfonamides (Davies and Davies 2010). The resistance against the “wonder drug” – penicillin – was observed even before its large-scale usage in the clinical settings, which was followed by the discovery of penicillinase in S. aureus and S. pneumoniae in 1940. This clearly depicted the presence of resistance genes conferring resistance against penicillin in the natural environment (Davies and Davies 2010; Ogawara 2016). Another analytical study of microbial DNA analysis from the dental plaque of ancient human remains showed the existence of ARG sequences sharing homology to the genes encoding resistance against the aminoglycosides, β-lactams, bacitracin, macrolides, and tetracycline in the genome of clinical strains (Warinner et al. 2014; Olaitan and Rolain 2016). The hypothesis of the acquisition of resistance genes from antibiotic producer organisms by the pathogens via horizontal gene transfer (HGT) was formerly proposed in the 1970s (Benveniste and Davies 1973). This was in accordance to the observations that the activity of aminoglycoside-modifying enzymes in actinomycetes shared similar biochemical activity to the different enzymes present in pathogenic strains. Another example includes the vanHAX genes – ARGs present in the antibiotic-producing bacteria found in soil were found in clinical isolates as well and shared considerable similarity between the protein sequences along with conserved organization and arrangement of genes (Barna and Williams 1984; Marshall et al. 1998). The integration of the van operons on conjugative plasmids or transposons has led to an enhancement of their dissemination (Courvalin 2008). It has been speculated that while these enzymes have no direct linkage with resistance functions in producers, they may have a role in other metabolic functions (Benveniste and Davies 1973; Martínez 2018). This is supported by comparative genome sequence analysis studies depicting the diversity of ARGs, and these studies have shown that they are encoded by a diverse group of unrelated genes, which suggest that their origin is through multiple convergent paths that results in a similar function (Shaw et al. 1993).
Recent reports have provided an evidence of the transfer of intrinsic resistance gene from the environmental strains to the pathogenic strains. For example, the plasmid-encoded CTX-M, an extended-spectrum β-lactamase (ESBL) of class A gene of pathogenic bacteria, showed similarity with CTX-M gene found in the genome of a nonpathogenic environmental strain of Kluyvera species (Humeniuk et al. 2002; Cantón and Coque 2006). Similarly, the quinolone resistance determinant qnr, originally located in the genome of a nonpathogenic environmental Shewanella and Vibrio species, was lately found to be translocated to a conjugative plasmid in Klebsiella (Poirel et al. 2005). Another gene called qepA encoding a major facilitator superfamily (MFS) efflux pump was initially linked to a conjugative plasmid in clinical isolates of E. coli (Périchon et al. 2007). However, it was recently found in the metagenomic samples of river sediments polluted by untreated urban wastewaters (Cummings et al. 2011).
The introduction and usage of the antibiotics into the clinical settings was observed to have two opposite effects: first, the rapid and desired one is that of microbial growth inhibition by targeting the essential cellular processes and, second, the undesirable one is the emergence of AMR in pathogens by elimination of the sensitive variants (Das et al. 2020). The development of resistance is a natural evolutionary process with various factors such as the type of environment; the microbial community density in that specific habitat; the antibiotic regimen in health, food, agriculture, and animal husbandry sectors; etc. influencing its frequency of emergence (Holmes et al. 2016).
1.4 Genomic Insights into Antimicrobial-Resistant ESKAPE Pathogens
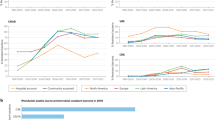
These ESKAPE pathogens encompassing both Gram-positive and Gram-negative bacteria are usually characterized as the carrier of drug resistance genes and are common causes for many life-threatening nosocomial infections. Both chromosome and plasmid carry several horizontally acquired resistance genes and act as potential reservoirs for other bacterial species. Prevalence of different classes of ARGs in the genome of ESKAPE pathogens varies widely (Fig. 1.2). Maximum prevalence of most of the ARGs is reported in the genome of P. aeruginosa followed by A. baumannii.
Prevalence of antibiotic resistance genes in the genome of ESKAPE pathogens. A total of 28,222 whole genome sequences (W) and 7566 plasmid (P) sequences isolated from Enterococcus faecium [N = 1738 (W), 668 (P)], Staphylococcus aureus [N = 8724 (W), 1943 (P)], Klebsiella pneumoniae [N = 8385 (W), 4392(P)], Acinetobacter baumannii [N = 4336 (W), 424 (P)], Pseudomonas aeruginosa [N = 4527 (W), 52 (P)], and Enterobacter cloacae [N = 512(W), =87(P)] were analyzed to understand the prevalence of antibiotic resistance genes in the genome of ESKAPE pathogens. Data source: The Comprehensive Antibiotic Resistance Database (https://card.mcmaster.ca/genomes)
1.4.1 Gram-Positive ESKAPE (GP-ESKAPE) Pathogens
ESKAPE pathogens that belong to Gram-positive bacteria include Enterococci spp. and Staphylococcus aureus.
1.4.1.1 Vancomycin-Resistant Enterococcus
The increasing rate of antimicrobial resistance among Enterococcus is a serious concern, especially the incidence of vancomycin-resistant Enterococcus (VRE), which is mainly associated with E. faecium and E. faecalis. E. faecium has been classified into two major clades, viz., Clade A and Clade B, based on the CRISPR analysis, multi-locus sequence typing (MLST), and whole genome database to understand the clonal pattern. Clade A (Clades A1 and A2) set of organisms are mainly found in hospitals, whereas Clade B group of organisms are of nonclinical background and mainly associated with community origin. Clade A1 includes epidemic hospital strains and is also known to harbor virulence and antibiotic resistance genes, and Clade A2 include the strains responsible for causing animal and sporadic human infections (Santajit and Indrawattana 2016). Multi-locus sequence typing of E. faecium identified a global polyclonal cluster, which includes the sequence type ST17 followed by the descendant types ST16, ST78, ST63, ST64, and ST174. E. faecium 17 (CC17) is often characterized as the carrier of different multidrug-resistant gene markers and known to cause many serious infections. Apart from the CC17 clonal complex, many other significant sequence types such as ST203, ST910, ST78, and ST192 are also responsible for the evolution, emergence, and rising proportion of VRE infections (De Oliveira et al. 2020). But in the case of E. faecalis, MLST analysis revealed the most prevalent clones responsible for clinical infection and outbreak that include ST6, ST9, ST16, ST21, ST28, ST40, and ST87, and along with the hospital-derived infections, these STs are also frequently reported in the community, farm animals, and food products.
The glycopeptide resistance in Enterococcus is mainly mediated by the vancomycin resistance operon (Van operon) and is attributed by the inducible production of peptidoglycan precursors D-alanyl-D-lactate (D-Ala-D-Lac), and the substitution of D-Ala-D-Lac for the D-Ala-D-Ala dipeptide confers a higher level of vancomycin resistance to Enterococcus spp. The Van operon mainly consists of vanS-vanR, a response regulator; vanX, a D-Ala-D-Ala dipeptidase gene; vanH, a D-lactate dehydrogenase gene; and a variable ligase gene that is located either in chromosome or within plasmid. VanA and VanB are the most predominant type among these nine types of VREs (vanA, vanB, vanC, vanD, vanE, vanG, vanL, vanM, and vanN) and also showed enhanced resistance pattern toward all glycopeptide antibiotics (Ahmed and Baptiste 2018). The vanA gene cluster consists of seven open reading frames transcribed from two different promoters, and this vanA operon is typically linked with transposons (Tn) which was originally detected on the non-conjugative highly conserved transposon Tn1546-like element. The transposons carrying vanA gene cluster are generally carried on self-transferable conjugative plasmids, and it appears to be responsible for the spread of glycopeptide resistance in Enterococci. The vanB operon has a similar genetic backbone to vanA but is generally carried by large elements of 90–250 kb, and the transfer of vanB resistance alleles occurs through the acquisition or transfer of transposons such as Tn1547, Tn1549, and Tn5382. The conjugative vanB transposon, known as Tn1549, is widely prevalent among VanB-type Enterococcus and is mainly a chromosomal transposon. The major dissemination of VanB-type resistance is primarily due to the spread of vanB2 cluster carried on Tn916-like conjugative transposons. The vanC operon is genetically different from vanA and vanB and is also less virulent than those of Enterococci spp. carrying inducible vanA and vanB operon. Similar to vanC, vanD and vanE gene clusters are also detected in various Enterococcus species and are located in the chromosome of the host organism, whereas vanG operon has been found to be transferable via a conjugative plasmid from E. faecalis. The family of van genes was expanded after the discovery of vanL, vanM, and vanN operons in Enterococcus spp. which were classified mainly based on their genetic structure, transferability, inducibility, and resistance profile against glycopeptides.
1.4.1.2 Staphylococcus aureus
Methicillin-resistant Staphylococcus aureus (MRSA) is a major clinical concern and responsible for the cause of many nosocomial and community-acquired infections. The acquisition of methicillin resistance mecA gene transforms a methicillin-susceptible S. aureus (MSSA) to a MRSA strain. This mecA gene encodes the additional penicillin-binding protein 2a (PBP2a), a peptidoglycan transpeptidase, and is located on a mobile genetic element Staphylococcal cassette chromosome mec (SCCmec) which is a site-specific transposon-like element exclusively found among Staphylococcus species. The SCCmec elements are integrated in the chromosomes of MRSA strains and are composed of MecI (a repressor), MecR1 (a transducer), and cassette chromosome recombinase (CCR) gene complex that mediates the integration and excision of the element from the chromosome.
The conserved structure of SCCmec and mecA has facilitated the molecular detection of methicillin resistance, and as a result, five major MRSA clones, SCCmec I–V, have been identified. Hospital-associated MRSA (HA-MRSA) isolates are characterized by the larger SCCmec types I–III and are mostly limited to healthcare settings, but community-associated MRSA (CA-MRSA) isolates are associated with novel, small variant of SCCmec types IV and V (Naorem et al. 2020). mecC, another mec allele which shows approximately 70% nucleotide sequence homology with the classical mecA gene, and are is mainly found in the livestock-associated MRSA (LA-MRSA). Borderline oxacillin-resistant S. aureus (BORSA) are resistant to oxacillin but do not carry mecA and mecC genes, and this may be due to the occurrence of mutations in both the promoter and coding sequence of mecA.
The nonsense or nonsynonymous mutation in mecA gene may be responsible for ceftaroline resistance in MRSA which is mainly observed in S. aureus ST239 strain, whereas the daptomycin resistance is mainly linked to the mutation in mprF gene which encodes for an enzyme called lysyl-phosphatidylglycerol synthetase and is one of the common mutations observed in MRSA strains. MRSA isolates have also developed resistance toward mupirocin due to the mutations in the chromosomal gene ileS or the plasmid-located genes mupA and mupB. Fluoroquinolone resistance in MRSA is mediated either by efflux pump genes, viz., norA, norB, norC, mdeA, qacA, and qacB, or by point mutations in the ParC subunit of topoisomerase IV (De Oliveria et al. 2020). Tetracycline resistance is primarily observed due to the acquisition of tet and otr genes with the most common tetracycline resistance mechanism being mediated by tetA, tetM, and tetK genes. MRSA strains acquire tigecycline resistance due to mutations in the transcriptional regulator mepR and in the efflux pump mepA resulting in the increased efflux of the drug. Vancomycin resistance in MRSA is successfully achieved by horizontal transfer of a plasmid-borne vanA gene transposon from vancomycin-resistant Enterococcus which results into the emergence of vancomycin-resistant S. aureus (VRSA). On the other hand, the chloramphenicol resistance in S. aureus can occur through the acquisition of cfr gene, while the poxtA gene is found to be responsible for oxazolidinone and phenicol resistance in MRSA (Antonelli et al. 2018).
Mobile genetic elements (MGEs) such as SCCmec, plasmids, and transposons are the critical factors for the acquisition and dissemination of the resistance determinants in S. aureus. In MRSA, the mecA or mecC genes, carried within SCC element, can be horizontally transferable. The association of mecA with SCC is not only important for mecA acquisition or transfer but is also a key factor for the co-existence of multiple resistance determinants in the same locus. This is enabled by the plasticity of the SCCmec element that can host several resistant genes that are associated with high risk of horizontal transmission.
In S. aureus, transposons (Tn) predominantly encode antibiotic resistance genes, and they are either inserted into the chromosome or in the mobile genetic element such as Tn552-related transposon (harbor penicillin-resistant gene blaZ), Tn554 (encode resistance to spectinomycin and macrolide-lincosamide-streptogramin B antibiotics), Tn5801 (a conjugative transposon carrying tetM gene), Tn4001 (associated with several multi-resistance plasmids and SCCmec elements), and the plasmid-borne transposon Tn1546 (encodes the vanA operon).
The major S. aureus clones responsible for the emergence of multidrug resistance are identified as ST239, ST59, ST398, ST8, and ST9. ST239 is found to responsible for the global dissemination of HA-MRSA strains (Giulieri et al. 2020). The novel S. aureus clone ST772, also known as Bengal Bay clone ST772, is reported as a multidrug-resistant S. aureus lineage in community and healthcare-associated environments. While a variety of clonal complexes such as CC1, CC8, CC30, and CC45 have been identified among S. aureus strains, majority of the MRSA isolates are detected among CC398, CC9, and CC8 clonal complex (Li et al. 2019).
1.4.2 Gram-Negative ESKAPE (GN-ESKAPE) Pathogens
The ESKAPE pathogens that come under the umbrella of Gram-negative organisms include Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species.
1.4.2.1 Klebsiella pneumoniae
Among Enterobacteriaceae, K. pneumoniae is known to be an invasive and virulent pathogen and is broadly classified into two subtypes: classical K. pneumoniae (cKp) and non-classical K. pneumoniae (ncKp). The clones of ncKp can cause severe infections, which are difficult to treat due to their continuous mutation and acquisition of antibiotic-resistant genes. Carbapenem-resistant K. pneumoniae (CRKP) strains are clinically prominent and have been found to be associated with many severe infections. The spread of CRKP that has been driven by many clones is largely attributed to ST307, ST11, ST15, ST101, and ST258 strains, along with the ST258 derivative ST512 (De Oliveira et al. 2020).
1.4.2.2 Acinetobacter baumannii
Multidrug-resistant A. baumannii typically cause several major infections in hospitalized patients, especially in the intensive care setting. The spread of carbapenem-resistant A. baumannii (CRAB) isolates is largely associated with three international clonal lineages: CC1, CC2, and CC3. CC1 is prevalent worldwide, while CC2 and CC3 are highly prevalent in Europe and North America (Dagher et al. 2019).
1.4.2.3 Pseudomonas aeruginosa
P. aeruginosa is an opportunistic pathogen causing complicated and life-threatening infections. The flexibility and adaptability of P. aeruginosa genome is a key feature in pathogens’ high stability, ability to persist and evade antibiotic action. P. aeruginosa lineages ST235 and ST175 have emerged as high-risk dispersed clones and remain a major contributor of hospital-acquired infection due to their enhanced capacity to acquire and maintain foreign antibiotic resistance determinants (Treepong et al. 2018).
1.4.2.4 Enterobacter Species
Enterobacter is an extremely diverse group of bacteria, and multidrug-resistant Enterobacter species are responsible for an increasing cause of hospital-acquired infection. Currently, in the USA, E. aerogenes ST4 and ST93 and carbapenem-resistant E. cloacae ST178 and ST78 represent the prevalent lineages associated with nosocomial infection (De Oliveira et al. 2020).
Among these GN-ESKAPE pathogens, the most common drug resistance mechanism employed is the production of enzymes that can degrade or destroy the antibiotics. Beta-lactamase is one such enzyme, which has the ability to hydrolyze all the β-lactam antibiotics including the last-line drug carbapenem. They comprise of extended-spectrum β-lactamases (ESBLs), AmpC, and carbapenemases. Among the ESBLs, TEM, SHV, and CTX-M are most commonly found in GN-ESKAPE pathogens. The TEM beta-lactamase hydrolyzes cephalosporins and penicillins and is widely spread in K. pneumoniae, Enterobacter spp., and non-fermentative P. aeruginosa. CTX-Ms have been identified among all the ESKAPE pathogens, while among SHV enzymes, SHV-1 is the most clinically relevant and commonly found in K. pneumoniae. Other class A ESBLs, viz., PER, VEB, GES, and OXA families, have also been reported across all Gram-negative ESKAPE pathogens. K. pneumoniae carbapenemase (blaKPC), a serine carbapenemase enzyme able to degrade all the beta-lactams including carbapenems, is predominantly detected in clinical isolates of K. pneumoniae. Furthermore, OXA-type carbapenemases are commonly found in Acinetobacter spp., followed by K. pneumoniae and Enterobacter spp. The most prominent metallo-𝛽-lactamases (MBLs) encountered among GN-ESKAPE pathogens are imipenemase metallo-𝛽-lactamases (IMP), Verona integron-encoded metallo-𝛽-lactamases (VIM), and New Delhi metallo-beta-lactamase-1 (NDM-1). IMP- and VIM-type MBLs were first detected in clinical P. aeruginosa isolates and later have been identified in other ESKAPE pathogens. Similarly, NDM-type enzymes have also been detected across all the Gram-negative ESKAPE bacteria. AmpC beta-lactamases including penicillinase and cephalosporinase are usually identified in many Enterobacter spp., P. aeruginosa, and Acinetobacter spp.
Resistance to aminoglycoside antibiotic in GN-ESKAPE organism occurs mainly through the production of aminoglycoside-modifying enzymes (AMEs) which are further classified into three groups, i.e., aminoglycoside acetyltransferases (AACs), aminoglycoside phosphotransferases (APHs), and aminoglycoside nucleotidyl-transferases (ANTs). The 16S rRNA methylases (NpmA and Rmt gene family) encoded on the plasmids also confer resistance to all aminoglycosides in GN-ESKAPE pathogens (Ishizaki et al. 2018).
Efflux pump also plays an important role in the mechanism of antimicrobial resistance in GN-ESKAPE pathogens, and till date, six major families of efflux pumps have been characterized, which include resistance-nodulation-division (RND), multidrug and toxic compound extrusion (MATE), small multidrug resistance (SMR), proteobacterial antimicrobial compound efflux (PACE), major facilitator superfamily (MFS), and ATP-binding cassette (ABC) families. AcrAB-TolC and MexAB-OprM, belonging to the RND-type efflux pump-mediated resistance, are of major concern as they play an important role in the multidrug resistance phenotype among Gram-negative bacteria. MexAB-OprM efflux system is mainly observed in P. aeruginosa that exhibits resistance toward fluoroquinolone, aminoglycoside, and beta-lactams. Similarly, the overproduction of AcrAB-TolC is characteristic of multidrug-resistant K. pneumoniae and Enterobacter strains. The overexpression of AdeABC, AdeFGH, and AdeIJK RND-type efflux pumps leads to the development of MDR in A. baumannii (Santajit and Indrawattana 2016). The chromosomally encoded OqxAB efflux pump observed in K. pneumoniae and Enterobacter spp. contributes to reduced susceptibility to quinolone and chloramphenicol. The alterations in AcrAB-TolC and KpnEF efflux pump systems as well as the loss of putative porin, KpnO, may drive the aminoglycoside resistance in K. pneumoniae (Navon-Venezia et al. 2017).
The dissemination of resistance determinants among the GN-ESKAPE pathogens is mainly mediated by plasmids, insertion sequences, transposon, and other genetic elements. Insertion sequences (IS) are capable of self-transposition and mobilizing the neighboring genes. Significant among them are ISAba125, which is mainly associated with NDM gene, and ISEcp1, which appears to be responsible for mobilizing many antibiotic-resistant genes like blaCTX-M, blaCMY-2, blaOXA, and blaACC. Other IS elements such as ISAba1, IS1247, ISKpn23, IS26, and ISEnca1 are also found to be associated with mobilization of the resistance determinants. The composite transposons that are found to be carrying AMR genes include Tn9 (IS1, chloramphenicol resistance), Tn10 (IS10, tetracycline resistance), Tn5 (IS50, aminoglycoside and bleomycin resistance), and, more recently, Tn6330 (ISApl1), which is responsible for mobilizing the colistin resistance gene mcr-1. Among ESKAPE pathogens, AMR genes are frequently associated with the Tn3 family (Tn1, Tn2, and Tn3), Tn7-like unit transposons, and Tn552-like elements. The IS elements also play a significant role in the deactivation of the uptake system, i.e., ompK36 porin in K. pneumoniae, which results in elevated carbapenem resistance. Similarly, the insertional inactivation of the mgrB regulatory gene in K. pneumoniae leads to the overexpression of the pmrHFIJKLM operon, which results in colistin resistance (Kumar et al. 2018). Integron, a gene-capture system, is known to be an important tool for horizontal dissemination of diverse resistance determinant, and recently, carbapenemase genes blaKPC, blaVIM, and blaNDM are found to be carried within class 1 integron. Plasmids are known to be the most significant vehicle for the transfer of resistance determinants such as ESBLs (blaCTX-M, blaTEM, blaVEB, blaPER), AmpC (blaDHA, blaCMY), carbapenemases (blaKPC, blaIMP, blaNDM, blaVIM, blaOXA-23), and colistin resistance gene (mcr) in GN-ESKAPE pathogens. Plasmids can harbor several IS and MGEs associated with AMR genes, and multidrug-resistant GN-ESKAPE pathogens carry the resistant determinants within a wide variety of plasmid incompatibility groups, viz., IncF, IncP, IncL, IncN, IncH, and IncX3, that facilitate the horizontal transfer within intra- and interspecies level (De Oliveira et al. 2020).
1.5 Ecology of Antimicrobial Resistance Genes in ESKAPE Pathogens
Comprehensive genomic studies of pathogenic and nonpathogenic bacterial species and the Comprehensive Antibiotic Resistance Database (CARD) catalogue 175,753 alleles with potential resistance functions against 249 clinically important antibiotics (https://card.mcmaster.ca). Most of the AMR genes reported in ESKAPE pathogens are acquired through HGT and are physically linked with replicative and/or integrative MGEs. HGT leads to evolution of bacteria by introducing multiple fitness factors even in case of single event of acquisition. Various studies have reported MGEs as the preexisting source of AMR genes, which are widely distributed in the genome of environmental, clinical, as well as human-associated microbial species (Partridge et al. 2018). Six major classes of MGEs are often found in the genome of ESKAPE pathogens, namely, transposons, gene cassettes and integrons, genomic islands, plasmids, bacteriophages, and ICEs (Partridge et al. 2018). These MGEs are involved in the exchange of AMR genes between various pathogens as well as between pathogenic and commensal bacterial population living commonly or transiently in similar environmental niches.
1.5.1 Plasmids
Plasmids are the self-replicating extrachromosomal modules that often endow the host with various fitness factors. However, they do not confer essentiality for the survival of bacteria under optimal growth conditions (Actis et al. 1999; Heuer and Smalla 2012; Nojiri 2013). They are ubiquitous in different domains of life and encode adaptive functions, such as heavy metal or antibiotic resistance, pathogenicity, or the ability to survive in a particular environmental niche and degradation of xenobiotics. The basic structure of the plasmid consists of genes encoding replicative functions and other accessory genes, involved in functions for segregation and selective advantage to the host. The accessory functions of AMR are encoded by either one or more resistance genes and may be linked with MGEs such as integron (In), insertion sequence (IS), and/or transposon (Tn) located in the plasmid backbone (Partridge et al. 2018).
The excessive usage of antibiotics such as ciprofloxacin and norfloxacin in the late 1980s led to the emergence of resistance mechanisms in Gram-negative bacteria. The emergence of plasmid-mediated quinolone resistance (PMQR) was observed since 1998. The first plasmid-mediated conferring quinolone resistance (presently known as qnrA1) was reported in Klebsiella pneumoniae (Martínez-Martínez et al. 1998). Thereafter, the other plasmid-encoded genes such as qnrA, qnrB, qnrC, qnrD, qnrS, and qnrVC were described in several Gram-negative pathogens (Poirel et al. 2017). These genes encode proteins that belong to the pentapeptide repeat family that provides protection to DNA gyrase and topoisomerase IV from the action of quinolone antibiotics. Smillie et al. (2010) reported 14% of the sequenced plasmids to be conjugative in nature that act as conveyors for AMR traits and virulence factors. The emergence of mcr-1, the plasmid-mediated colistin resistance gene in the genome of Gram-negative pathogens, lately is an evidence of continuous evolution of bacterial species through HGT (Liu et al. 2016). The dissemination of OXA β-lactamase genes illustrates their horizontal transfer through plasmids among different bacterial phyla dating back to millions of years (Barlow and Hall 2002).
1.5.2 Bacteriophages
Phages constitute the most abundant and rapidly replicating biological entities on Earth (Jackson et al. 2011) having an estimated number of ~1030–1032 (Chibani-Chennoufi et al. 2004), outnumbering the bacterial population by a factor of 10 (Hendrix et al. 1999). They exploit host resources for their multiplication, and most of them are lytic in nature as the host is killed; hence, they are also known as antibacterial agents (Clokie et al. 2011). Lysogenic phages can integrate their genome into the host chromosome and replicate passively as a part of the host chromosome (Marti et al. 2014).
A recent study found 70% of phage DNA samples from 80 healthy individuals to be positive for various ARGs like bla-CTXM-1, blaTEM, and qnr genes (Quirós et al. 2014). Most of the enteric pathogens such as Enterococcus species (Mazaheri et al. 2010), Salmonella enterica, and P. aeruginosa (Blahová et al. 1992) harbor phages, which have been shown in vitro to act as disseminator of ARGs.
1.5.3 Transposons
Transposons are the jumping genetic elements which hop and integrate into the host chromosomal DNA. These elements show either intracellular or intercellular movement using the functions of their own integrase. Usually, for their integration, there is no requirement of sequence homology between the insertion site and the transposon element. However, in some cases, transposons may require specificity to a particular nucleotide sequence at the insertion site (Craig 1997). The insertion of transposon within a gene leads to disruption of the gene function and may modulate the gene expression if inserted into the regulatory sequences.
Members of ESKAPE contain various transposons such as Tn5 which encodes resistance to kanamycin and neomycin and Tn10 which encodes for tetracycline resistance. Transposons have been linked to the spread of blaNDM-1 gene in ESKAPE pathogens (Nordmann et al. 2012), which is a growing public threat.
1.5.4 Integrative and Conjugative Elements (ICEs)
ICEs are members of a class of self-transmissible bacterial MGEs also called as conjugative transposons or constins (Burrus and Waldor 2004). Their size ranges from ~20 kb to 500 kb, and they carry genes that confer phenotypes like resistance to antibiotics and heavy metals, bacteriocin synthesis, bacterial pathogenesis, carbon source utilization, biofilm formation, restriction modification, and resistance to bacteriophage infection (Johnson and Grossman 2015; Wozniak and Waldor 2010; Van Houdt et al. 2013). Their integration and excision are facilitated either by serine, tyrosine, or DDE recombinases (Johnson and Grossman 2015; Brochet et al. 2009). The integrases consist of highly conserved Arg-His-Arg-Tyr catalytic tetrad located in the carboxy-terminal end of the protein. The insertion takes place at a specific DNA sequence, attB in the bacterial chromosome, mostly located at the downstream of tRNA gene, and harbors multiple modules that are associated with distinct functions including (1) integration/excision module, (2) replication/DNA processing module, (3) regulation module, (4) DNA secretion module, and (5) auxiliary modules. The auxiliary modules are often linked with evolutionarily important traits, including antimicrobial resistance genes, heavy metal resistance genes, and virulence- or toxin-encoding genes, and genetic traits involved in the alternative catabolic pathways. The extrachromosomal ssDNA-ICE formation starts at the origin of transfer (oriT) and, after the recognition, is covalently linked with the 5′ end of the DNA relaxase. The linear ssDNA-ICEs with the DNA relaxase covalently linked get transferred to the recipient cell, and the circularization of ssDNA-ICEs is mediated by relaxase. Complementary strand synthesis occurs before its integration into the host chromosome.
The discovery and identification of ICEs started with emergence of multidrug-resistant bacterial pathogens. Identification of heavy metal and antibiotic resistance determinants transferred via conjugation and their location on the chromosomes instead of in a stable plasmid of various pathogens like Enterococcus (Franke and Clewell 1981), Bacteroides species (Rashtchian et al. 1982), and Clostridium species (Magot 1983; Smith et al. 1981) led to a speculation about the ICEs. Analysis of 1000 genomes identified putative 335 ICEs and 180 conjugative plasmids depicting both the presence of ICEs in most clades of bacteria and their higher frequency of occurrence compared to conjugative plasmids (Guglielmini et al. 2011). Conjugative transposons belonging to Tn916/Tn1545 family in Clostridia, Enterococcus, and Streptococci carry various tetracycline, macrolide, and aminoglycoside resistance genes providing an insight into resistance gene transfer among these group of bacteria (Roberts and Mullany 2011).
1.5.5 Integrons
Integrons are the gene acquisition elements that capture exogenous ORFs via site-specific recombination and provide an active transcription platform to convert the integrated cassette into a functional gene (Hall and Collis 1995). They utilize their own integrase (IntI) for the integration of the cassette. In general, these integrons have three basic modules: (1) integrase encoding gene, (2) a specific integration site (attI), and (3) a functional promoter (Pc). The site-specific integration between the double-stranded host chromosome (attC) and the folded single-stranded exogenous cassette (attI) is catalyzed by integrase enzyme. The integrons identified can be categorized into two classes: the mobile integrons and superintegrons. The physical linkage of mobile integrons with the MGEs (insertion sequences, transposons, ICEs, conjugative plasmids) is involved in the dissemination of antibiotic resistance genes in bacteria. ARGs encoding resistance against aminoglycosides, β-lactams, chloramphenicol, trimethoprim, erythromycin, fosfomycin, rifampicin, quinolones, and several antiseptic compounds are physically linked with the mobile integrons as reported in several studies (Holmes et al. 2016). Superintegrons are a part of bacterial chromosome and represent a “core” gene-capture system in the Gram-negative bacteria that enables adaptation to diverse environments (Mazel 2006). The large number of gene cassettes linked with the integron having an identity of >80% between the attachment sites of these cassettes and no association with mobile genetic elements are the characteristic features of a superintegron subset.
1.6 Resistance Mechanisms of ESKAPE Pathogens
The principal antibiotic resistance mechanisms of ESKAPE pathogens include the following three major mechanisms: (1) the prevention of access to the target site by either change in membrane permeability or efflux of antibiotics from bacterial cell, (2) the inactivation of antibiotic molecule either by hydrolysis or chemical modification, and (3) the alteration of the target site (either protection/replacement/absence/mutation or enzymatic modification of the target site) (Alekshun and Levy 2007; Blair et al. 2015) (Fig. 1.1). These resistance mechanisms could be either intrinsic mechanisms or the acquired resistance mechanisms. Another peculiar resistance mechanism includes the biofilm formation that helps the pathogen to evade the antimicrobial action as well as suppress the effect of immune response cells of the host. Additionally, biofilms also protect the dormant cells called persister cells that cause difficult-to-treat recalcitrant infections (Lewis 2008).
Intrinsic resistance mechanisms are the chromosomally encoded mechanisms that include the accumulation of point mutations in the target ORF or in the regulatory region, various nonspecific efflux pump proteins, antibiotic-inactivating enzymes, and various other mechanisms related to permeability barriers (Fajardo and Martínez 2008; Cox and Wright 2013). These mechanisms provide a low level of antibiotic resistance in the original host such as environmental bacteria or normal commensal bacteria that may behave as an opportunistic pathogen in immunocompromised patients (Wright 2007). On the other hand, the acquired resistance mechanisms lead to the acquisition of new functionalities by import of genetic systems to the bacterial cell, which may get integrated into the genome (genomic recombination) or maintained as the extrachromosomal elements (plasmid acquisition) (van Hoek et al. 2011).
1.6.1 Resistance Due to Decreased Permeability or Active Ejection of Antibiotics
An optimal intracellular concentration of an antibiotic is required for its antimicrobial action for the treatment of an infection. In a bacterium, there are two major factors that prevent the optimum accumulation of the antibiotic: (1) the state of the cell membrane permeability and (2) the action of selective efflux pump proteins (Fig. 1.1).
Reduced membrane permeability to the selective compounds is an important defense mechanism utilized by bacteria, which prevents the antibiotic entry into the cytoplasm (Munita and Arias 2016). The permeability threshold of the peptidoglycan layer of Gram-positive bacteria is in the range of 30–57 kDa (Scherrer and Gerhardt 1971), and its coarse meshwork allows the smaller molecules to penetrate easily, which makes Gram-positive organisms susceptible to various antibiotics (Randall et al. 2013). On the other hand, due to the presence of a much finer molecular sieve, the outer membrane of Gram-negative bacteria (Vaara 1992) comprising of lipid molecules (namely, lipid A) covalently linked to polysaccharide units and tightly packaged with saturated fatty acids has reduced membrane fluidity (Nikaido 2003) and increased permeability threshold. Hence, lipopolysaccharide units of Gram-negative bacteria, such as P. aeruginosa, Salmonella enterica, V. cholerae, etc., act as a major permeability barrier and are responsible for intrinsic resistance in these bacteria to several antibiotics such as azithromycin, erythromycin, polymyxin B, and rifamycin. The modifications of the membrane lipid barrier and alterations of the expression pattern of various outer membrane porins lead to the severalfold reduction in the permeability of antibiotics. Reduction in expression or loss or replacement of the channel proteins of outer membrane also reduces the permeability of selective antibiotics (Blair et al. 2015).
Various genes encoding efflux pump proteins, which may be part of chromosome or part of some acquired genetic element like plasmid, are ubiquitously present in bacteria and encode proteins that can actively transport various antimicrobial compounds by utilization of energy in the form of ATP or through transmembrane ion gradients (Li and Nikaido 2009). The bacterial efflux pump mediates the extrusion of the antibiotics out of the bacterial cell, thereby decreasing the effective concentration of the antibiotic inside the cell. The efflux systems have been confirmed to be present in archaea and prokaryotic and eukaryotic species (Van Bambeke et al. 2003). The principal role of efflux systems in a cell is the ejection of undesirable compounds such as heavy metals (Nies 2003), dyes (Kaatz et al. 1993), organic solvents (Ramos et al. 2002), amphiphilic detergents (Mahamoud et al. 2007), biocides (Costa et al. 2013), metabolites (Van Dyk et al. 2004), and quorum sensing molecules (Pearson et al. 1999) in addition to antibiotics. The presence of efflux pumps has also been attributed in biofilm formation and also in contributing toward AMR in many bacteria (Alav et al. 2018).
The efflux pumps can be divided into single-component transporters or multicomponent transporters differing in terms of structural conformation, range of substrates that they may export, and their distribution in different types of bacterial organisms.
1.6.2 Resistance Due to Inactivation of the Antibiotics
Bacteria can modify or destroy the antibiotic scaffolds by either transfer of a chemical group to the scaffolds or hydrolysis of the core structure (Fig. 1.1). The modification of antibiotics by the enzymatic functions of the acquired genetic traits is the most common antibiotic resistance mechanisms in pathogenic bacteria.
1.6.2.1 Inactivation of Antibiotics by Hydrolysis.
The inactivation of β-lactam antibiotics is one of the most common antibiotic resistance mechanisms, which is mediated by the hydrolase activity of β-lactamases (De Pascale and Wright 2010). β-Lactams including penicillins, monobactams, cephalosporins, and carbapenem have a common β-lactam ring and are commonly prescribed antibiotics across the globe. The metallo-β-lactamase or serine β-lactamase hydrolyzes the β-lactam ring that confers the resistance against β-lactams in most of the bacterial species. In a β-lactam-sensitive bacterial cell, the presence of an active site serine residue of the penicillin-binding protein acts as a site for the nucleophilic attack and inactivation of the enzymes due to formation of a slowly hydrolyzing covalent β-lactam-PBP intermediate (Andersson and Hughes 2010). The hydrolysis of antibiotic scaffolds such as macrolide macrocycle lactone ring and fosfomycin epoxide ring and the amidohydrolysis of bacitracin undecaprenyl pyrophosphate have been implicated in the development of antibiotic resistance (Das et al. 2020).
1.6.2.2 Inactivation of Antibiotics by Chemical Modifications.
The modification of antibiotic scaffolds via enzymatic modification through the covalent transfer of different chemical groups is another very common resistance mechanism (Fig. 1.1). Various enzymes involved in drug resistance by modification of the antibiotic structure have been characterized (De Pascale and Wright 2010). These enzymes lead to inactivation of antibiotics using any of the seven modifications:
-
1.
Phosphate group transfer to the antibiotic scaffold from either ATP or GTP, called O-phosphorylation. Resistance against chloramphenicol, fosfomycin, macrolide, and rifampicin antibiotics has been reported due to phosphorylation process.
-
2.
Modification of the antibiotics by the transfer of adenosine monophosphate (AMP) moiety, called O-nucleotidylylation. This confers resistance against different members of aminoglycosides and lincosamide classes of antibiotics.
-
3.
A glycosyl moiety addition to the antibiotics such as macrolides and rifampin called O-glycosylation.
-
4.
ADP-ribose transfer from NAD leads to inactivation of rifampin known as O-ribosylation.
-
5.
Transfer of an acetyl group from acetyl-CoA to the antibiotic, called O- and N-acetylation. Several antibiotics are inactivated due to acetylation such as aminoglycosides, chloramphenicol, fluoroquinolone, and streptothricin.
-
6.
Addition of a hydroxyl group (-OH), called hydroxylation, leads to inactivation of an antibiotic.
-
7.
There can be a chemical complex formation that prevents antibiotic access to the target (Das et al. 2020).
1.6.3 Resistance due to Alteration of the Target Site of the Antibiotic
1.6.3.1 Mutations of the Target Site
Most antibiotics target the essential cellular functions of a bacterial cell (Fig. 1.1). The antibiotics act on specific target molecules, and accumulations of point mutations in the target gene alter the amino acid composition of the translated protein, and therefore, the affinity of antibiotic to its target is reduced or lost leading to a reduction in antibiotic efficiency (Andersson and Hughes 2010). Such mechanisms of resistance are widely prevalent in enteric pathogens against commonly prescribed antibiotics that inhibit (1) the DNA replication machinery and repair in the quinolone resistance-determining region by affecting parC-parE and gyrA-gyrB gene functions (Hooper 2001), (2) transcription by altering rpoB-encoded protein (rifampicin), (3) protein synthesis by altering rpsL gene function (streptomycin), (4) alteration of cell wall biosynthesis by modification of pbp gene function (β-lactam), and (5) various metabolic enzymes by altering embB, katG, and mshA functions (SXT).
1.6.3.2 Enzymatic Modification of the Target Site
The RNA modification enzymes such as rRNA methyltransferase, which transfer a methyl group to some specific nucleotides of 16S or 23S rRNA gene, confer resistance against several protein synthesis inhibitors such as aminoglycoside and macrolide antibiotics routinely used in clinical settings to treat Gram-negative and Gram-positive bacterial infections (Holmes et al. 2016). Several genes (aviR, cfr, emtA, ermA, ermB, ermC) encode 23S rRNA methyltransferases that confer resistance against lincosamides, phenicols, oxazolidinones, pleuromutilins, and streptogramin-A antibiotics in Gram-negative bacteria (Das et al. 2020). However, the absence of Ksg methyltransferase in E. coli leads to kasugamycin resistance. In a similar manner, inactivation of pseudouridine synthase rulC gene that modifies the 23S rRNA confers significant resistance against clindamycin, linezolid, and tiamulin in various enteric pathogens (Das et al. 2020).
1.6.3.3 Target Protection
The genetic determinants that encode proteins involved in the protection of target have been characterized in the bacterial chromosome as well as MGEs. Fluoroquinolones (Qnr), tetracycline (Tet[M] and Tet[O]), and fusidic acid (FusB and FusC) are the antibiotics affected by this mechanism. Tet[M] and Tet[O] proteins are a member of the translation factor superfamily of GTPases (Fig. 1.1). They bear homology with the elongation factors (EF-G and EF-Tu) required in the synthesis of protein, and their interaction with the ribosome leads to dislodging of the tetracycline antibiotic from its binding site (Munita and Arias 2016). Another example of target protection includes the qnr family of quinolone resistance genes present on the plasmids in various pathogens encoding pentapeptide repeat proteins that bind and protect DNA gyrase and topoisomerase IV from the bactericidal action of quinolones (Blair et al. 2015). The resistance against cationic peptides such as polymyxins is most commonly linked to the alterations in the expression of regulators that affect LPS production and lead to alterations in the target or even absence of the LPS production that reduces binding of the drug (Poirel et al. 2017).
1.6.3.4 Substitution or Bypassing of the Target Site
Bacteria that easily evolve new targets with similar biochemical functions to the original target but differ from the target molecules of the antimicrobial molecule utilize this strategy (Fig. 1.1). The most common clinical examples are methicillin resistance as seen in S. aureus owing to the acquisition of PBP (PBP2a) and peptidoglycan modifications due to van gene clusters leading to vancomycin resistance in enterococci. Another route to evade the action of antibiotics is to “bypass” the metabolic pathway either by overproduction of the enzyme encoded by the antibiotic target or amino acid changes in the enzyme as seen in resistance to trimethoprim-sulfamethoxazole (TMP-SMX) (Munita and Arias 2016).
Deeper insights of the existing and new mechanisms of antibiotic resistance are required to design novel therapeutic agents. Advances in genomics, structural biology, and systems biology can be tapped to circumvent this problem. However, the mobilization of these various resistance genes via MGEs into the pathogens has made the treatment of several infections challenging due to the lack of appropriate antibiotics. Deciphering the mobile genetic elements and their propagation within the indigenous flora and the invading pathogens could pave the way for a better understanding of pathogen biology and emergence of drug resistance in the pathogens of public health importance.
1.7 Conclusion
Antimicrobial resistance is set to have devastating effects on global public health as the emergence and evolution of drug-resistant pathogens continue to threaten modern medicine and simultaneously the food security, agricultural sectors, and animal health. ESKAPE pathogens represent the peak for resistance and pathogenesis and a major cause of life-threatening infections and are characterized by their exacerbated ability for acquisition of multiple resistant genes. So, there is an urgent need for a rapid diagnostic assay, which will help to reduce the unnecessary consumption, blanket prescription, and release of antibiotics in the environment. This will ultimately minimize the selective pressure in the environment. The improved diagnostic solution will help to treat patients effectively and will reduce transmission dynamics of the resistance determinants. An interdisciplinary and one health approach is also the need of the hour to bring the development of the solutions to the global antimicrobial resistance challenge as well as the treatment and management of ESKAPE pathogens. Along with the quest and urgency for developing novel therapeutics to treat multidrug-resistant ESKAPE infections, it is also important to explore other novel alternative therapeutic strategies such as antimicrobial peptides, nanoparticles, phage therapy, and anti-virulence therapy to combat drug resistance pathogens as the currently available antibiotics have often been found lacking and there is a dearth of new drugs in the pipeline. It is necessary to maintain sustainable stewardship practices, AMR surveillance, and patient education in order to stay ahead of the emerging drug-resistant ESKAPE pathogens and to control the AMR crisis in both clinical and community settings.
References
Actis LA, Tolmasky ME, Crosa JH (1999) Bacterial plasmids: replication of extrachromosomal genetic elements encoding resistance to antimicrobial compounds. Front Biosci 4:D43–D62
Ahmed MO, Baptiste KE (2018) Vancomycin-resistant enterococci: a review of antimicrobial resistance mechanisms and perspectives of human and animal health. Microb Drug Resist (Larchmont, N.Y.) 24(5):590–606
Alav I, Sutton JM, Rahman KM (2018) Role of bacterial efflux pumps in biofilm formation. J Antimicrob Chemother 73:2003–2020
Alekshun MN, Levy SB (2007) Molecular mechanisms of antibacterial multidrug resistance. Cell 128:1037–1050
Andersson DI, Hughes D (2010) Antibiotic resistance and its cost: is it possible to reverse resistance? Nat Rev Microbiol 8:260–271
Antonelli A, D’Andrea MM, Brenciani A et al (2018) Characterization of poxtA, a novel phenicol-oxazolidinone-tetracycline resistance gene from an MRSA of clinical origin. J Antimicrob Chemother 73:1763–1769
Baltz RH (2008) Renaissance in antibacterial discovery from actinomycetes. Curr Opin Pharmacol 8:557–563
Barlow M, Hall BG (2002) Phylogenetic analysis shows that the OXA beta-lactamase genes have been on plasmids for millions of years. J Mol Evol 55:314–321
Barna JC, Williams DH (1984) The structure and mode of action of glycopeptide antibiotics of the vancomycin group. Annu Rev Microbiol 38:339–357
Benveniste R, Davies J (1973) Aminoglycoside antibiotic-inactivating enzymes in actinomycetes similar to those present in clinical isolates of antibiotic-resistant bacteria. Proc Natl Acad Sci U S A 70:2276–2280
Blahová J, Hupková M, Krčméry V, Schäfer V (1992) Imipenem and cefotaxime resistance: transduction by wild-type phages in hospital strains of Pseudomonas aeruginosa. J Chemother 4:335–337
Blair JMA, Webber MA, Baylay AJ et al (2015) Molecular mechanisms of antibiotic resistance. Nat Rev Microbiol 13:42–51
Brochet M, Da Cunha V, Couvé E et al (2009) Atypical association of DDE transposition with conjugation specifies a new family of mobile elements. Mol Microbiol 71:948–959
Burrus V, Waldor MK (2004) Shaping bacterial genomes with integrative and conjugative elements. Res Microbiol 155:376–386
Cantón R, Coque TM (2006) The CTX-M beta-lactamase pandemic. Curr Opin Microbiol 9:466–475
Centers for Disease Control and Prevention (2019) CDC’s antibiotic resistance threats in the United States (AR Threats Report). https://www.cdc.gov/drugresistance/
Chibani-Chennoufi S, Bruttin A, Dillmann M-L, Brüssow H (2004) Phage-host interaction: an ecological perspective. J Bacteriol 186:3677–3686
Clokie MRJ, Millard AD, Letarov AV, Heaphy S (2011) Phages in nature. Bacteriophage 1:31–45
Comprehensive Antibiotic Resistance Database (2020) Nucleic acids research. https://card.mcmaster.ca/
Coronado-Álvarez NM, Parra D, Parra-Ruiz J (2019) Clinical efficacy of fosfomycin combinations against a variety of gram-positive cocci. Enferm Infecc Microbiol Clin 37:4–10
Costa SS, Viveiros M, Amaral L, Couto I (2013) Multidrug efflux pumps in Staphylococcus aureus: an update. Open Microbiol J 7:59–71
Courvalin P (2008) Predictable and unpredictable evolution of antibiotic resistance. J Intern Med 264:4–16
Cox G, Wright GD (2013) Intrinsic antibiotic resistance: mechanisms, origins, challenges and solutions. Int J Med Microbiol 303:287–292
Craig NL (1997) Target site selection in transposition. Annu Rev Biochem 66:437–474
Cummings DE, Archer KF, Arriola DJ et al (2011) Broad dissemination of plasmid-mediated quinolone resistance genes in sediments of two urban coastal wetlands. Environ Sci Technol 45:447–454
D’Costa VM, King CE, Kalan L et al (2011) Antibiotic resistance is ancient. Nature 477:457–461
Dagher TN, Al-Bayssari C, Chabou S et al (2019) Investigation of multidrug-resistant ST2 Acinetobacter baumannii isolated from Saint George hospital in Lebanon. BMC Microbiol 19(1):29
Das B, Chaudhuri S, Srivastava R et al (2017) Fostering research into antimicrobial resistance in India. BMJ 358:j3535
Das B, Verma J, Kumar P et al (2020) Antibiotic resistance in Vibrio cholerae: understanding the ecology of resistance genes and mechanisms. Vaccine 38(Suppl 1):A83–A92
Davies J, Davies D (2010) Origins and evolution of antibiotic resistance. Microbiol Mol Biol Rev 74:417–433
De Oliveira DMP, Forde BM, Kidd TJ et al (2020) Antimicrobial resistance in ESKAPE pathogens. Clin Microbiol Rev 33(3):e00181. https://doi.org/10.1128/CMR.00181-19
De Pascale G, Wright GD (2010) Antibiotic resistance by enzyme inactivation: from mechanisms to solutions. Chembiochem 11:1325–1334
Dijkshoorn L, Nemec A, Seifert H (2007) An increasing threat in hospitals: multidrug-resistant Acinetobacter baumannii. Nat Rev Microbiol 5:939–951
Fajardo A, Martínez JL (2008) Antibiotics as signals that trigger specific bacterial responses. Curr Opin Microbiol 11:161–167
Founou RC, Founou LL, Essack SY (2017) Clinical and economic impact of antibiotic resistance in developing countries: a systematic review and meta-analysis. PLoS One 12:e0189621
Franke AE, Clewell DB (1981) Evidence for conjugal transfer of a Streptococcus faecalis transposon (Tn916) from a chromosomal site in the absence of plasmid DNA. Cold Spring Harb Symp Quant Biol 45(Pt 1):77–80
Gandra S, Tseng KK, Arora A et al (2019) The mortality burden of multidrug-resistant pathogens in India: a retrospective, observational study. Clin Infect Dis 69:563–570
Giulieri SG, Tong SYC, Williamson DA (2020) Using genomics to understand meticillin- and vancomycin-resistant Staphylococcus aureus infections. Microb Genom 6(1):e000324
Guglielmini J, Quintais L, Garcillán-Barcia MP et al (2011) The repertoire of ICE in prokaryotes underscores the unity, diversity, and ubiquity of conjugation. PLoS Genet 7:e1002222
Hall RM, Collis CM (1995) Mobile gene cassettes and integrons: capture and spread of genes by site-specific recombination. Mol Microbiol 15:593–600
Hendrix RW, Smith MCM, Burns RN et al (1999) Evolutionary relationships among diverse bacteriophages and prophages: all the world’s a phage. Proc Natl Acad Sci 96:2192–2197
Heuer H, Smalla K (2012) Plasmids foster diversification and adaptation of bacterial populations in soil. FEMS Microbiol Rev 36:1083–1104
Holmes AH, Moore LSP, Sundsfjord A et al (2016) Understanding the mechanisms and drivers of antimicrobial resistance. Lancet 387:176–187
Hooper DC (2001) Mechanisms of action of antimicrobials: focus on fluoroquinolones. Clin Infect Dis 32(Suppl 1):S9–S15
Humeniuk C, Arlet G, Gautier V et al (2002) Beta-lactamases of Kluyvera ascorbata, probable progenitors of some plasmid-encoded CTX-M types. Antimicrob Agents Chemother 46:3045–3049
Ishizaki Y, Shibuya Y, Hayashi C et al (2018) Instability of the 16S rRNA methyltransferase-encoding npmA gene: why have bacterial cells possessing npmA not spread despite their high and broad resistance to aminoglycosides? J Antibiot 71:798–807
Jackson RW, Vinatzer B, Arnold DL et al (2011) The influence of the accessory genome on bacterial pathogen evolution. Mob Genet Elements 1:55–65
Johnson CM, Grossman AD (2015) Integrative and conjugative elements (ICEs): what they do and how they work. Annu Rev Genet 49:577–601
Kaatz GW, Seo SM, Ruble CA (1993) Efflux-mediated fluoroquinolone resistance in Staphylococcus aureus. Antimicrob Agents Chemother 37:1086–1094
Klein EY, Milkowska-Shibata M, Tseng KK et al (2021) Assessment of WHO antibiotic consumption and access targets in 76 countries, 2000-15: an analysis of pharmaceutical sales data. Lancet Infect Dis 21:107–115
Kumar A, Biswas L, Omgy N et al (2018) Colistin resistance due to insertional inactivation of the mgrB in Klebsiella pneumoniae of clinical origin: first report from India. Rev Esp Quimioter 31:406–410
Lew K (2014) Antibiotics, 1st edn. Marshall Cavendish Benchmark, New York
Lewis K (2008) Multidrug tolerance of biofilms and persister cells. Curr Top Microbiol Immunol 322:107–131
Li H, Andersen PS, Stegger M et al (2019) Antimicrobial resistance and virulence gene profiles of methicillin-resistant and -susceptible Staphylococcus aureus from food products in Denmark. Front Microbiol 10:2681
Li X-Z, Nikaido H (2009) Efflux-mediated drug resistance in Bacteria. Drugs 69:1555–1623
Liu Y-Y, Wang Y, Walsh TR et al (2016) Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect Dis 16:161–168
Magot M (1983) Transfer of antibiotic resistances from Clostridium innocuum to Clostridium perfringens in the absence of detectable plasmid DNA. FEMS Microbiol Lett 18:149–151
Mahamoud A, Chevalier J, Alibert-Franco S et al (2007) Antibiotic efflux pumps in gram-negative bacteria: the inhibitor response strategy. J Antimicrob Chemother 59:1223–1229
Mandal SM, Roy A, Ghosh AK et al (2014) Challenges and future prospects of antibiotic therapy: from peptides to phages utilization. Front Pharmacol 5:105
Marshall CG, Lessard IA, Park I, Wright GD (1998) Glycopeptide antibiotic resistance genes in glycopeptide-producing organisms. Antimicrob Agents Chemother 42:2215–2220
Marti E, Variatza E, Balcázar JL (2014) Bacteriophages as a reservoir of extended-spectrum β-lactamase and fluoroquinolone resistance genes in the environment. Clin Microbiol Infect 20:O456–O459
Martinez JL (2009) The role of natural environments in the evolution of resistance traits in pathogenic bacteria. Proc Biol Sci 276:2521–2530
Martínez JL (2018) Ecology and evolution of chromosomal gene transfer between environmental microorganisms and pathogens. Microbiol Spectr 6(1):141–160. https://doi.org/10.1128/microbiolspec.MTBP-0006-2016
Martínez-Martínez L, Pascual A, Jacoby GA (1998) Quinolone resistance from a transferable plasmid. Lancet 351:797–799
Mazaheri Nezhad Fard R, Barton MD, Heuzenroeder MW (2010) Novel bacteriophages in Enterococcus spp. Curr Microbiol 60:400–406
Mazel D (2006) Integrons: agents of bacterial evolution. Nat Rev Microbiol 4:608–620
Munita JM, Arias CA (2016) Mechanisms of antibiotic resistance. Microbiol Spectr 4:34
Naorem RS, Urban P, Goswami G, Fekete C (2020) Characterization of methicillin-resistant Staphylococcus aureus through genomics approach. 3 Biotech 10:401
Navon-Venezia S, Kondratyeva K, Carattoli A (2017) Klebsiella pneumoniae: a major worldwide source and shuttle for antibiotic resistance. FEMS Microbiol Rev 41:252–275
Nies DH (2003) Efflux-mediated heavy metal resistance in prokaryotes. FEMS Microbiol Rev 27:313–339
Nikaido H (2003) Molecular basis of bacterial outer membrane permeability revisited. Microbiol Mol Biol Rev 67:593–656
Nojiri H (2013) Impact of catabolic plasmids on host cell physiology. Curr Opin Biotechnol 24:423–430
Nordmann P, Gniadkowski M, Giske CG et al (2012) Identification and screening of carbapenemase-producing Enterobacteriaceae. Clin Microbiol Infect 18:432–438
Ogawara H (2016) Self-resistance in streptomyces, with special reference to β-lactam antibiotics. Molecules 21(5):605. https://doi.org/10.3390/molecules21050605
Olaitan AO, Rolain J-M (2016) Ancient resistome. Paleomicrobiol Hum 4:75–80
Partridge SR, Kwong SM, Firth N, Jensen SO (2018) Mobile genetic elements associated with antimicrobial resistance. Clin Microbiol Rev 31(4):e00088. https://doi.org/10.1128/CMR.00088-17
Pearson JP, Van Delden C, Iglewski BH (1999) Active efflux and diffusion are involved in transport of Pseudomonas aeruginosa cell-to-cell signals. J Bacteriol 181:1203–1210
Périchon B, Courvalin P, Galimand M (2007) Transferable resistance to aminoglycosides by methylation of G1405 in 16S rRNA and to hydrophilic fluoroquinolones by QepA-mediated efflux in Escherichia coli. Antimicrob Agents Chemother 51:2464–2469
Poirel L, Jayol A, Nordmann P (2017) Polymyxins: antibacterial activity, susceptibility testing, and resistance mechanisms encoded by plasmids or chromosomes. Clin Microbiol Rev 30:557–596
Poirel L, Rodriguez-Martinez J-M, Mammeri H et al (2005) Origin of plasmid-mediated quinolone resistance determinant QnrA. Antimicrob Agents Chemother 49:3523–3525
Quirós P, Colomer-Lluch M, Martínez-Castillo A et al (2014) Antibiotic resistance genes in the bacteriophage DNA fraction of human fecal samples. Antimicrob Agents Chemother 58:606–609
Ramos JL, Duque E, Gallegos M-T et al (2002) Mechanisms of solvent tolerance in gram-negative bacteria. Annu Rev Microbiol 56:743–768
Randall CP, Mariner KR, Chopra I, O’Neill AJ (2013) The target of Daptomycin is absent from Escherichia coli and other gram-negative pathogens. Antimicrob Agents Chemother 57:637–639
Rashtchian A, Dubes GR, Booth SJ (1982) Tetracycline-inducible transfer of tetracycline resistance in Bacteroides fragilis in the absence of detectable plasmid DNA. J Bacteriol 150:141–147
Review on Antimicrobial Resistance (2016) Tackling drug-resistant infections globally: final report and recommendations
Roberts AP, Mullany P (2011) Tn916-like genetic elements: a diverse group of modular mobile elements conferring antibiotic resistance. FEMS Microbiol Rev 35:856–871
Santajit S, Indrawattana N (2016) Mechanisms of antimicrobial resistance in ESKAPE pathogens. Biomed Res Int 2016:1–8
Scherrer R, Gerhardt P (1971) Molecular sieving by the Bacillus megaterium cell wall and protoplast. J Bacteriol 107:718–735
Shaw KJ, Rather PN, Hare RS, Miller GH (1993) Molecular genetics of aminoglycoside resistance genes and familial relationships of the aminoglycoside-modifying enzymes. Microbiol Rev 57:138–163
Smillie C, Garcillán-Barcia MP, Francia MV et al (2010) Mobility of plasmids. Microbiol Mol Biol Rev 74:434–452
Smith MD, Hazum S, Guild WR (1981) Homology among tet determinants in conjugative elements of streptococci. J Bacteriol 148:232–240
Snyder ADH, Hall Snyder AD, Werth BJ et al (2016) Fosfomycin enhances the activity of Daptomycin against vancomycin-resistant enterococci in an in vitro pharmacokinetic-Pharmacodynamic model. Antimicrob Agents Chemother 60:5716–5723
Tacconelli E, Carrara E, Savoldi A et al (2018) Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis 18:318–327
Treepong P, Kos VN, Guyeux C et al (2018) Global emergence of the widespread Pseudomonas aeruginosa ST235 clone. Clin Microbiol Infect 24:258–266
Vaara M (1992) Agents that increase the permeability of the outer membrane. Microbiol Rev 56:395–411
Van Bambeke F, Glupczynski Y, Plésiat P et al (2003) Antibiotic efflux pumps in prokaryotic cells: occurrence, impact on resistance and strategies for the future of antimicrobial therapy. J Antimicrob Chemother 51:1055–1065
Van Dyk TK, Templeton LJ, Cantera KA et al (2004) Characterization of the Escherichia coli AaeAB efflux pump: a metabolic relief valve? J Bacteriol 186:7196–7204
van Hoek AHAM, Mevius D, Guerra B et al (2011) Acquired antibiotic resistance genes: an overview. Front Microbiol 2:203
Van Houdt R, Toussaint A, Ryan MP et al (2013) The Tn4371 ICE family of bacterial Mobile genetic elements. Landes Biosci 9:242
Waksman SA, Woodruff HB (1940) Bacteriostatic and bactericidal substances produced by a soil Actinomyces. Exp Biol Med 45:609–614
Warinner C, Rodrigues JFM, Vyas R et al (2014) Pathogens and host immunity in the ancient human oral cavity. Nat Genet 46:336–344
Wozniak RAF, Waldor MK (2010) Integrative and conjugative elements: mosaic mobile genetic elements enabling dynamic lateral gene flow. Nat Rev Microbiol 8:552–563
Wright GD (2007) The antibiotic resistome: the nexus of chemical and genetic diversity. Nat Rev Microbiol 5:175–186
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Paul, D., Verma, J., Banerjee, A., Konar, D., Das, B. (2022). Antimicrobial Resistance Traits and Resistance Mechanisms in Bacterial Pathogens. In: Kumar, V., Shriram, V., Paul, A., Thakur, M. (eds) Antimicrobial Resistance. Springer, Singapore. https://doi.org/10.1007/978-981-16-3120-7_1
Download citation
DOI: https://doi.org/10.1007/978-981-16-3120-7_1
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-3119-1
Online ISBN: 978-981-16-3120-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)