Abstract
Sarcomas, despite being a disparate group of malignant diseases, share a common propensity to metastasise to the lungs, regardless of origin of the primary. This risk correlates with location, size, grade and histological subtype [1]. Often this is the only clinical evidence of disease in patients after appropriate complete resection of their primary sarcoma. They may appear at the time of local recurrence in an incompletely resected or inappropriately treated primary sarcoma.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
18.1 Introduction
Sarcomas, despite being a disparate group of malignant diseases, share a common propensity to metastasise to the lungs, regardless of origin of the primary. This risk correlates with location, size, grade and histological subtype [1]. Often this is the only clinical evidence of disease in patients after appropriate complete resection of their primary sarcoma. They may appear at the time of local recurrence in an incompletely resected or inappropriately treated primary sarcoma.
Approximately 20% of patients with resected sarcoma will develop isolated pulmonary metastatic disease at some point in the course of their disease [2]. There appear to be particular subtypes of sarcoma with higher pulmonary metastatic rates, such as tenosynovial sarcoma, spindle cell sarcoma from extremities and extra-skeletal osteosarcoma [3, 4]. As a more general rule, high-grade sarcomas make up 90% of pulmonary metastatic disease and low-grade sarcomas only 10%. The observation that pulmonary metastatic disease is common, and often isolated, is a strong impetus to target that disease aggressively.
Since the introduction of safe methods of anaesthesia and resection of pulmonary tissue, pulmonary metastasectomy for colorectal and other malignancies, including sarcoma, have become an increasingly popular therapy. The hope is that the burden of disease will be reduced, time to further progression will be prolonged and direct invasive complications and further “tertiary” spread will be prevented. Systemic agents may be considered relatively ineffective or held in reserve, whilst surgical control is possible, and finally, some patients may be considered cured of their metastatic disease in that they die of unrelated causes or achieve incredibly long disease-free intervals.
The complex interplay between patient selection and class effect of an intervention is rarely as evident as in the mainstream practice of pulmonary metastasectomy. Using the much cited but somewhat anachronistic criteria from the International Registry of Lung Metastases [5] (Table 18.1), a surgeon could choose only to operate on patients with a solitary lung metastasis from a primary malignancy that was resected more than 3 years ago. With modern peri-operative care, minimally invasive techniques and optimal lung parenchymal preservation, that surgeon would be expected to have exceptional results in terms of low mortality, good early return to normal activity and prolonged disease-free and overall survival. However, if there are therapeutic benefits of metastasectomy beyond the selection of “winners”, that same surgeon is doing a disservice to the patients who present with two metastases, or present with their solitary metastasis just 2.5 years after original diagnosis. Conversely a surgeon who attempts to resect all lung metastases in all patients without discrimination may impose greater harms than any expected benefits on that patient population. This raises the question of whether there is a state of oligometastatic disease for which intervention is beneficial that can be distinguished from a more generalised state of systemic disease for which surgical intervention is futile and harmful.
18.2 The Oligometastatic Disease Concept
The concept of oligometastatic disease is that between the states of loco-regional malignancy and widespread metastatic malignancy, there exists a state of limited systemic metastatic disease for which local ablative therapy could be curative [6]. The definition of oligometastatic disease is elusive. It is easy to identify the extremes – solitary, single organ involvement is definitely an indication; widespread innumerable lesions are definitely not. But what of six metastases in one organ? What of a single metastasis in each of two disparate organs? Where is the blurred line between the two putative metastatic states? Is it probabilistic or stochastic events that result in failure of disease control? Does removing four metastases necessarily bring poorer results than removing three? What about the inherent biology of the particular patient’s malignancy and their individual host response?
The above conundrums drive clinicians to define their own therapeutic guidelines, arbitrary as they must be, without high-quality evidence. Being the largest and most promulgated series, the International Registry of Lung Metastases (IRLM) provides the basis for most clinical guidelines. These are particularly relevant for sarcoma as 2173 of the 5206 cases reported were for sarcoma. However, IRLM pre-dated the introduction of 18FDG-PET scanning and wide-scale use of minimally invasive and complex sublobar resection techniques. There have also been advances in therapeutic agents for some sub-groups of sarcoma in the decades since the IRLM was published.
The other problem with definition of an oligometastatic disease state in sarcoma is the extreme heterogeneity of disease under the sarcoma umbrella. Well-differentiated soft tissue sarcoma, osteosarcoma and Ewing’s tumours are not all likely to respond to the same surgery as a class effect. An elderly patient with significant comorbidity clearly has much less to gain (and greater potential for harm) than a fit 40-year-old. Therefore, some groupings must be looked at individually within any guidelines.
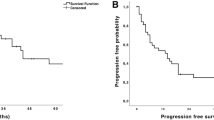
Historical experience of the natural history of these diseases and their response to pulmonary metastasectomy are the only evidence we have. For example, a 15-year experience of soft tissue sarcoma at Memorial Sloan Kettering Cancer Center at the turn of the century yielded 719 cases of pulmonary metastatic disease from over 3000 cases [7]. As there was a consistent therapeutic protocol to resect this disease from the lungs, we can get some insight into the expected outcomes. The entire metastatic group 3-year survival rate was 25%, with a median survival of 15 months, from time of detection of pulmonary metastases. At one extreme, those with completely resected disease had a 3-year survival rate of 46%, with a median survival of 33 months, but those with no resection had a median survival of only 11 months.
There is a point when treating teams decide there is too much disease to justify intervention, even in such a centre. This defines their local institutional definition of oligometastatic disease, but is also a self-fulfilling prognosticator. The ideal use of pulmonary metastasectomy would result in improved survival of the entire population by not imposing harms on futile cases, but reaping the benefits of intervention in all other cases. The authors were able to define groups for which pulmonary metastasectomy yielded disappointing results, namely, liposarcoma, peripheral nerve sheath tumour and patients over 50.
Given the ubiquitous finding of complete resection as the most important factor for prolonged survival, the concept of oligometastatic disease is not just defined by a number or a size of a lesion. Special patterns of disease are either particularly amenable to resection or particularly adverse. Some patterns correlate with aggressive or indolent tumour biology. The following have been gleaned from the author’s direct and secondary experience over the last two decades:
-
The “contaminated” lobe.
-
Bilateral mirror image involvement.
-
Direct invasion of adjacent structures.
-
The “kissing metastasis” vs pleural spread.
-
Endobronchial disease.
-
“The Sky by Night” appearance.
The contaminated lobe is the finding of multiple metastases in the distribution of a single pulmonary artery branch. This may manifest itself in the basal segments of a lower lobe, or the lingula, for example. These are relatively easy to take anatomically and eradicate the known disease in that lobe or segment, but also include any disease below the sensitivity of imaging detection. Thus, numerically unfavourable disease may in fact be successfully controlled with minimal loss of lung.
Bilateral disease as a prognosticator has conflicting evidence. The plethora of small case series from single institutions makes it difficult to distinguish the numerical from the bilaterality prognosticator, given that by definition, there must be two or more lesions. In the larger series, it appears that there is no difference between 2 and 3 metastases in a single lung or divided between two lungs [5, 8,9,10]. Mirror image metastases, especially affecting the upper or lower lobes, may in fact be prognostically better than a metastasis in each lobe of one lung.
A solitary metastasis that directly invades an adjacent structure, such as aorta, azygos, vertebra, oesophagus, diaphragm or rib is another special case that warrants aggressive intervention. Prolonged disease-free survival is seen with en bloc resection of aortic wall, diaphragm and ribs and is far more favourable than droplet or kissing metastasis of the pleural cavity. For involvement of head or neck of ribs, dislocation of the rib from its transverse process or even limited resection of adjacent vertebral body can achieve local control. More extensive involvement of the vertebral body is difficult to justify resection in the metastatic setting. Multi-level posterior rod stabilisation and anterior expandable cage insertion is usually a major 12-hour undertaking with the risks of paraplegia, chronic implant infection and chronic pain.
The “kissing metastasis” is an entity seen where a subpleural metastasis invades through the surface of the visceral pleura of the lung and rubs against either diaphragmatic, mediastinal or parietal pleura. The mechanism for this, as opposed to widespread droplet metastases, or trans-coelomic spread is unclear. However, it appears to confer much better prognosis than multiple or remote pleural metastases and is worth resecting radically en passant. It is usually not detectable preoperatively in any case, as the kissing metastasis appears fused with the lung metastasis of origin.
Endobronchial disease is a feature of some metastatic sarcoma, particularly epithelioid sarcoma. The latter may even mimic the behaviour of a non-small cell lung cancer, with spread to draining lymph nodes. Lung-sparing resectional surgery can be undertaken where appropriate, such as sleeve lobectomy or segmentectomy, as long as good surgical margins are achievable. Failing this, endobronchial therapies such as laser, stenting and brachytherapy can result in good palliation and prolongation of survival.
The CT appearance of “The Sky at Night” is a clearly unfavourable phenotype. Multiple small lesions, randomly distributed throughout the lungs, are not only suggestive of biologically aggressive disease that can thrive in different micro-environments; it is technically near-impossible to embark on a radical metastasectomy whilst preserving adequate lung function for quality survival. Conversely, scattered, but peripherally based metastases can be completely resected bilaterally (“pruning” of the lung), with the prospect of prolonged disease-free survival. Thus, the surgeon must consider the pattern of disease as much as the number and location of metastases.
18.3 Assessment for Surgery
The typical patient presenting with metastatic sarcoma is significantly different to the far more common patient requiring resection of non-small cell lung cancer. Not only is the median age much younger (55 years cf. 69 years; author’s data), but they have much lower rates and dosage of tobacco exposure, therefore relatively free of chronic obstructive pulmonary and atherosclerotic vascular disease.
Spirometry and carbon monoxide diffusing capacity are commonly tested prior to lung resection, but, in the asymptomatic non-smoker under 60 years having pulmonary metastasectomy, is a cost without benefit. Patients requiring more than lobectomy and repeat surgery and higher-risk patients should have appropriate physiological testing such as echocardiography, cardio-pulmonary exercise testing or angiography if indicated by symptoms, known comorbidity or cardiovascular risk factors. Death is a very rare occurrence for metastasectomy in specialist centres, but care must be taken not to inflict significant respiratory disability in a previously well-functioning individual.
The main aim of assessment is related to tumour factors. Despite upstaging rates of less than 5% [11], fluorodeoxyglucose (18FDG)-positron emission tomography (PET) scan has long been a standard of care prior to consideration of metastasectomy. This is particularly important to rule out local relapse at the primary site. Such disease should be completely resected with curative intent prior to pulmonary metastasectomy. PET scans can also identify unusual sites of extra-pulmonary metastases, such as mediastinal fat, mesentery, tongue, and peripheral muscle, that may be missed with a conventional CT scan. In general, these would rule out pulmonary metastasectomy.
PET scans have poor positive predictive value for extra-thoracic disease in tumours that do not avidly uptake 18FDG. Therefore, magnetic resonance imaging of the primary tumour site may be required to rule out concomitant local relapse. SPECT bone scans should be used if there are any undiagnosed skeletal symptoms in such patients. These are also useful in patients with myxoid or round cell liposarcomas as they have an additional predilection for bony metastases [12].
18.4 Surgical Oncology Principles
Thoracic surgeons dealing with pulmonary metastases have to negotiate the conflict between preservation of maximal lung parenchyma and fulfilling the requirement for good radial margins around a sarcoma. Whilst the wide margins mandated for primary resection are not required in the lung, any close or involved margin will likely result in local recurrence and predicts for poor survival as an independent risk factor [5].
Metastases to the lung are blood-borne and therefore can be subject to the fluid mechanics of the pulmonary vasculature as well as their tropism for the lung micro-environment. Therefore, for small multiple lesions within a single vessel delta, it may make oncological sense to perform an anatomical segmental, multi-segmental or lobar resection, rather than attempting a non-anatomic wedge resection. This would ensure that any undetected disease in that distribution would be removed along with the macroscopic disease.
For lung cancer, the accepted rule of wedge resection is to achieve a radial margin of at least the diameter of the tumour. For sarcoma metastases, this is not so vital, as they grow radially from a pulmonary vessel base, whereas lung cancer is a bronchiolo-alveolar and bronchial-based disease, which can more widely spread microscopically, either directly (lepidic growth) or as spread through alveolar spaces. Therefore, a margin of 5 mm after removal of the conventional triple row of staples (equating to at least 10 mm in total) is the minimum adequate margin for an intra-parenchymal metastasis. Visceral pleural margins are often measured in fractions of a millimetre for subpleural deposits, but as the next structure is the pleural cavity, it is either completely resected, or there will be pleural contamination no matter what the surgeon does. Therefore, there is no advantage in taking additional parietal pleura unless there is direct invasion or a kissing metastasis.
Lung-sparing techniques allow for good margins whilst achieving the thoracic surgeon’s other aim of preservation of lung function. These include bronchoplastic or sleeve resections at the lobar, segmental or, rarely, the carinal level. The specifics of sleeve resection will be discussed in the conduct of surgery section. Anatomic sublobar resections can allow resection of larger deep lesions, or geographic resections of impalpable deep lesions whilst sparing substantial portions of the involved lobe. A description of anatomically straightforward sublobar resections will be presented in the conduct of surgery section and listed in Table 18.2.
Navigational bronchoscopy can be used to mark small or impalpable lesions with either methylene blue for direct visualisation, indocyanine green (ICG) for near-infrared imaging or radio-opaque material for cone beam CT localisation in hybrid operating theatres. These techniques extend the reach of minimally invasive techniques, where palpation of small lesions can be difficult or, in the case of robotic surgery, impossible.
18.5 Conduct of Surgery
18.5.1 Access
The “gold standard” access for lung resection has long been one or other variation of the thoracotomy. These variations include the posterolateral thoracotomy, which involves the division of latissimus dorsi and trapezius muscles. The rib below the entry space (usually the sixth rib) is either divided posteriorly, shingled with 1 cm excised posteriorly or simply allowed to fracture. The costo-vertebral ligament may or may not be lysed to facilitate rib-spreading.
Muscle-sparing variations include those that enter the same space by mobilising the trapezius and latissimus muscles and retracting them in the posterior auscultatory triangle. An anterior muscle-sparing thoracotomy can be achieved by making an incision from the inferior border of the scapula anteriorly. The latissimus, pectoral and serratus anterior muscles are mobilised and split or retracted, and the fourth or fifth interspace is entered. Whilst muscles are spared, all of these procedures involve rib-spreading, the major cause of short- and long-term morbidity for simple lung resections.
Bilateral lesions have traditionally been accessed by sternotomy, or, less commonly, clamshell incisions. Sternotomy is less painful than thoracotomy, but may result in significant medium- to long-term morbidity from superficial or deep sternal wound infection, sternal dehiscence or instability. This is a particular risk for patients with diabetes, obesity or chronic obstructive pulmonary disease. It also has the disadvantage of poor access to lower lobe, particularly left lower lobe, without compromising cardiac function by pressure of the surgeon’s hands or retractors. Clamshell incisions give superior access but are also quite morbid, with division of the sternum and internal thoracic vessels transversely and the intercostal neuralgia of bilateral thoracotomies at a single sitting.
Video-assisted thoracic surgery (VATS) or thoracoscopic surgery has considerably minimised the morbidity of access to the lungs for metastasectomy. This is especially the case for bilateral disease, which can be comfortably dealt with in staged resections separated by as little as a week. There are now many variations of VATS, including port number and placement, robotic-assisted techniques and uniportal techniques.
The standard VATS procedure for wedge resection is arguably the three-port technique (Fig. 18.1). This allows multiple angles to visualise and manipulate the lung, the ability to “bring the lung to the finger” for palpation of deeper nodules, and multiple angles for best stapler application.
For simple subpleural nodules, or if an anatomic resection is mandated, a two-port VATS is quite useful, with two angles for both visualisation and stapling. Uniportal VATS techniques can be employed by enlarging the axillary utility incision and placing a wound protector sleeve. Palpation of the lung is more limited, however.
Uniportal VATS also has some advantages in the setting of simple resection of a subpleural, easily identified lesion, or for cases where an anatomic segmental or lobar resection is required. Visualisation is more akin to the thoracotomy view, which leads to less disorientation for the less expert VATS surgeon; however palpation and localisation is far more difficult than multi-port VATS. Despite the displeasing aesthetics of placing the intercostal catheter through the access incision and therefore more awkward closure, there are possibly fewer superficial wound problems and neuralgia than normally associated with the same catheter placed in a two-port or three-port telescope port. The main advantages of uniportal surgery are the ease of teaching the technique and its low cost compared to all other minimally invasive techniques. It is therefore well suited to low-income countries and emerging economies.
Other than for anatomic segmental or lobar resections, robotic surgery is not the ideal approach for metastasectomy. It requires four intercostal ports and a subcostal port, is expensive (in capital and disposable expenditure) for a simple wedge metastasectomy and adds considerable theatre time to what should be a quick procedure for staff and the patient. The only value for an institution is to improve setup skills and efficiency for technical and nursing staff and to amortise the large capital cost of the robot across more cases. However, deeper lesions requiring segmental resections after preoperative localisation with ICG lend themselves well to the robotic approach, especially for posterior and lateral basal segments of the lower lobe.
18.5.2 Wedge Metastasectomy
Once access to the lung is achieved by any means above, consideration turns to how a surgical margin will be achieved whilst minimising loss of lung parenchyma and avoiding prolonged air leakage from the cut surface.
By far the most useful and widespread technique is a stapled wedge metastasectomy. Commercial staplers usually provide three rows of staggered staple lines on either side of a proposed lung incision and simultaneously divide the tissue with an integrated blade. Other than severely emphysematous lungs, this results in an air-tight, haemostatic seal of the cut lung surface. Stapling of particularly thick tissue can result in air leaks from nearby fracturing of visceral pleura or the cutting out of a portion of staples. This can be minimised by compressing the tissue for longer and by intermittently and slowly advancing the stapler firing to allow further compression of the progressing staple line. For severely emphysematous lungs, a thicker tissue staple cartridge with a reinforcing sheet of absorbable material is recommended to prevent staples cutting out or missing lung tissue altogether by stapling “air”.
For very small peripheral surface lesions, pinpoint diathermy is useful to preserve lung, especially if multiple wedge metastasectomies or additional anatomic segmental or lobar resections are required. This focussed diathermy ablation is usually sufficient to weld the very peripheral bronchioles and vessels, and the apposition of these wounds against parietal pleura is usually sufficient to prevent prolonged air leaks.
Laser incisions are even more haemostatic and airtight than pinpoint diathermy, but increases the capital expenditure and disposable costs. For very peripheral lesions, it is particularly effective. It is also technically effective for deeper lesions where lung-sparing is critical, but its drawback is the difficulty in achieving reliable oncological margins without techniques such as suture fixation of the lesion, which potentially results in trans-coelomic spread or disruption of tumour.
18.5.3 Anatomic Sublobar Resections
One way of avoiding lobectomy for deep lesions is to determine what anatomic segment is affected by tumour and divide the relevant bronchial, venous and arterial supply.
The simplest segmentectomy is the lingulectomy. The fissure is more often complete, and even if it isn’t, access to the interlobar pulmonary artery is usually straightforward. The superior pulmonary vein usually has very obvious lingular and upper division tributaries. Once the singular vessels are divided, the upper lobe bronchus can be clear of the segmental node and the singular branch isolated for stapler division. A notional “neo-fissure” is created along the approximation of the inter-segmental plane, taking care to secure good oncologic margins.
By exclusion, the next most useful and straightforward sublobar resection is the left upper lobe superior trisegmentectomy (or divisionectomy). This is otherwise known as a lingula-sparing left upper lobectomy. Basically, the lingular structures are preserved, meaning the truncus anterior, and any posterior pulmonary arteries are divided after dividing the superior division tributary of the superior pulmonary vein. Once the superior division bronchus has been cleared and divided, the neo-fissure is staple-divided exactly as for lingulectomy.
Lower lobe superior segmentectomies of either lung are usually straightforward, especially if there is a good fissure, or at least good access to the interlobar pulmonary artery. The superior segmental tributary of the inferior pulmonary vein (V6) and the superior segmental pulmonary artery (A6) are divided then, after removing the segmental node, the superior segmental bronchus (B6) is divided. The neo-fissure is then estimated, taking care to secure good oncologic margins.
Once again, by exclusion, it is possible to perform apex-sparing lower lobectomies by dividing all structures except the superior segmental artery, bronchus and vein. The neo-fissure is then estimated as for a superior segmentectomy. The resulting superior segment is the largest segment of the lower lobe and very useful for filling the pleural space and preserving lung function.
Other more unusual segmental or bisegmental resections are possible with increasingly detailed knowledge of pulmonary vascular anatomy and its variations. Apico-anterior bisegmentectomy of either upper lobe is possible by dividing the truncus anterior and then chasing the upper lobe vein deep into the hilum to preserve the posterior tributary. By exclusion, a posterior segmentectomy on the right is also possible. In the lower lobe, a superior segmentectomy can be extended to an apico-posterior bisegmentectomy, or by exclusion, antero-medial or postero-lateral bisegmentectomies can be achieved by dividing the relevant terminal pulmonary artery branches beyond the lingular or middle lobe branches on the left or right, respectively.
18.5.4 Bronchoplastic Resections
Pneumonectomy should be avoided at almost any cost when the indication is metastasectomy. The mortality is significantly higher than all other lung resections; the reduction in quality of life is obvious even in fit patients. Future interventions other than stereotactic radiation may be prohibitive. Meticulous anatomic surgery may allow a lobectomy or (right side) bilobectomy to be performed in many cases. This may require a hand cut and sewn anastomosis for a close bronchial margin, or resection of a lobe and an adjacent segment across a fissure to achieve an en bloc resection.
If a bronchial margin cannot be secured without division of the origin of a main bronchus, then every endeavour should be made to perform some form of bronchoplastic resection. The simplest is the sleeve bronchoplasty, where the sleeve of bronchus that the involved segment, lobe or lung arises from is removed en bloc with the intended lung resection. The two open ends of bronchus proximally and distally are then carefully re-anastomosed, taking care not to strip too much of the peri-bronchial tissue during preparation. A running suture is quite acceptable as long as any size discrepancy is accommodated. The other favoured method is to perform a running anastomosis of the membranous portion, which can be cut to leave it slightly longer than the bronchial cartilage. The membrane is cinched on the larger bronchus and small bites taken on the smaller bronchus. Individual simple or figure-of-eight sutures can then be placed under vision and held. Cardiac snuggers are useful to bring the bronchial ends together and distribute tension evenly whilst each suture is tied. This technique is favoured over continuous suture if there is obvious tension in the anastomosis.
The most common and straightforward sleeve bronchoplasty is the right upper lobe with attached right main bronchus. The bronchus intermedius or even the lower lobe or lower lobe basal segments can be anastomosed as high as the ostium of the main bronchus if necessary (Fig. 18.2a, b). For more than just right upper lobe sleeve resection, a pericardial release will be required to allow the vascular hilum to move towards the carina. This is achieved by either curved incision of the pericardium below the inferior pulmonary vein (U-release) or circumcision of pericardium all the way around the pulmonary veins (O-release). These provide several centimetres of advancement of the bronchus towards the carina (Fig. 18.3a, b).
The hilum can be mobilised to facilitate bronchial re-anastomosis after sleeve resection. A pericardial U-release (a) and the more extensive O-release (b) are depicted by dashed red line. These allow the pulmonary veins (PVs) and peri-bronchial tissues to move comfortably towards the carina. SVC superior vena cava, IVC inferior vena cava, IPL inferior pulmonary ligament
Sleeve resections can also be applied to segmental resections, especially the superior segment of the left lower lobe. On the right side, the position of the middle lobe bronchus may not allow a sleeve superior segmentectomy; therefore a “cruciate” sleeve resection is indicated, whereby the right middle lobe and superior segment bronchi are resected en bloc with a continuous sleeve of bronchus from the bronchus intermedius to the right lower lobe basal bronchus. This results in the loss of three segments, compared to five segments for a complete right lower lobectomy or seven segments for a right middle and lower bilobectomy (Fig. 18.4).
Cruciate sleeve resection is employed for tumours involving the origin of either the right middle lobe bronchus or the superior segment bronchus of the right lower lobe. Both the middle lobe and the superior segment are sacrificed along with the attached bronchus intermedius and lower lobe bronchus, culminating in a cross-shaped resection specimen, hence the name (inset). The lower lobe basal bronchus is then re-anastomosed into the residual bronchus intermedius
Variations of bronchoplastic techniques include the wedge bronchoplasty and the hinge bronchoplasty. The wedge bronchoplasty is indicated when a hand cut margin of the origin of a lobar bronchus cannot be closed without risking a stricture. A V-excision is made in the lateral sides of the bronchus starting either side of the resection defect. The bronchus can now be closed axially rather than transversely. This will result in some angulation, but it is usually of no functional consequence.
The hinge bronchoplasty is particularly useful on the left side when a hand cut bronchial margin of the secondary carina results in a large bronchial defect medially. The left lower lobe can be rotated inferiorly and medially with the previously inferior lingular bronchial margin being anastomosed to the medial wall of the left main bronchus. Careful suture placement is required to prevent accidental closure or stricturing of the lingular bronchial ostium. An analogous hinge bronchoplasty can be performed on the right if a right middle and lower bilobectomy requires en bloc resection of the right main bronchus opposite the right upper lobe ostium. The previously inferior side of the right upper lobe bronchus is swung inferiorly and medially to anastomosed to the medial wall of the main bronchus. The result is a very functional residual lung (Fig. 18.5a, b). Finally, hinge bronchoplasty is also useful for an extended right lower lobectomy with angled hand cut resection of the posterolateral bronchus intermedius opposite the right middle lobe ostium. This may be required for encroachment of a tumour slightly superior to the superior segment bronchus take-off, but only involving a small area of bronchus intermedius. Once again, the middle lobe bronchus is swung on its remaining attachment, this time superiorly and posteriorly.
Hinge bronchoplasty of the right upper lobe may be indicated during bilobectomy if the tumour involves the medial wall of the main bronchus opposite the right upper lobe ostium. The right upper lobe is swung inferiorly and medially to anastomose onto the end of the main bronchus to create a valuable functioning neo-lung (a). A post-operative chest X-ray demonstrates the re-positioned lobe almost filling the pleural cavity (b)
18.6 Complications of Surgery
As mentioned previously, the average patient having sarcoma metastasectomy is usually free of significant comorbidity. However, there is a cohort of patients in their sixth and seventh decades in whom unexpected non-technical complications are possible. Prolonged air leak or subcutaneous emphysema despite a functioning intercostal catheter are the most common technical complications of any lung resection. Subcutaneous emphysema, whilst dramatic in appearance, is usually benign and self-limiting. There appears to be a higher incidence of this in the VATS era, but this may just be because it is the most obvious reason for prolonged hospital stay beyond 1 or 2 days. This may need intervention for patient comfort and to reduce alarm amongst nursing staff and visiting relatives. The author has found that re-opening the VATS utility port down to the emphysematous plane and applying a VAC dressing (KCI, TX) connected to continuous wall suction is highly effective and can usually prevent a return to the operating room. Prolonged air leak beyond 7 days should trigger the question of whether a thoracoscopic exploration should be undertaken on the next available operating list. Sometimes these are due to unfavourable adhesions resulting in inadequate drainage, or fracturing of peri-staple lung. In most cases re-draining and starting over will eliminate the problem. This is preferred over waiting until an empyema develops.
Bleeding is an unusual complication of wedge metastasectomy, although a port site can continually ooze and form a clotted haemothorax. This should be cleared operatively. For lobar and sublobar anatomic resections, the source of bleeding comes from the hilar vessels themselves and from the bronchial and other small arteries supplying the lymph nodes and bronchi. The hilar vessels are more likely to be an intra-operative problem. Bronchial and nodal vessel bleeding are the most likely to result in return to the operating room. Preventative measures include liberal use of clips and energy such as ultrasonic shears or “smart” bipolar diathermy. This will also prevent prolonged lymphatic ooze.
Anastomotic complications are exceedingly rare for lobar stumps, but are a specific risk for pneumonectomy and sleeve resections. The tension required to close a main bronchial stump actually puts it at greater risk of dehiscence than a sleeve anastomosis at the same site, which allows the bronchial lumina to maintain their natural shape. For right-sided pneumonectomy, a flap reinforcement is strongly advised. The simplest form is to mobilise the pericardial fat pad, which will reach most anastomotic locations. Reversed pleural or pericardial pedicled flaps are another alternative. The intercostal muscle of the thoracic access space can also be mobilised as a pedicled flap, but this will increase the chest wall morbidity from somatic and neuropathic pain.
As with all major surgery in the presence of advanced malignancy, the risk of pulmonary embolus is elevated, and therefore all patients should be placed on prophylactic low molecular weight heparins (LMWH) unless there is a specific contraindication. The addition of sequential calf compression devices or thromboembolic stockings should be in accordance with institutional policy. These adjuncts may be required in lieu of LMWH if there is a known contraindication to that drug class.
When patients have been exposed to chemotherapeutic agents prior to surgery, consideration must be given to the possibility of pneumonitis or cardiac injury. Marrow suppression may result in poor haemopoietic response to blood loss; therefore the threshold for consideration of blood transfusion may be lowered if there has been significant blood loss intra-operatively or post-operatively.
References
Mariani L, Miceli R, Kattan MW, Brennan MF, Colecchia M, Fiore M, et al. Validation and adaptation of a nomogram for predicting the survival of patients with extremity soft tissue sarcoma using a three-grade system. Cancer. 2005;103:402–8.
Gadd MA, Casper ES, Woodruff JM, McCormack PM, Brennan MF. Development and treatment of pulmonary metastases in adult patients with extremity soft tissue sarcoma. Ann Surg. 1993;218:705–12.
Lewis JJ, Brennan MF. Soft tissue sarcomas. Curr Probl Surg. 1996;33:817–72.
Vezeridis MP, Moore R, Karakousis CP. Metastatic patterns in soft-tissue sarcomas. Arch Surg. 1983;118:915–8.
Pastorino U, Buyse M, Friedel G, Ginsberg RJ, Girard P, Goldstraw P, et al. Long-term results of lung metastasectomy: prognostic analyses based on 5206 cases. J Thorac Cardiovasc Surg. 1997;113:37–49.
Kaneda H, Communications YSCT. Oligometastases: defined by prognosis and evaluated by cure: Clin Lung Cancer; 2015.
Billingsley KG, Burt ME, Jara E, Ginsberg RJ, Woodruff JM, Leung DH, et al. Pulmonary metastases from soft tissue sarcoma: analysis of patterns of diseases and postmetastasis survival. Ann. Surg. 1999;229:602–10–discussion610–2.
Cheung F, Alam N, Wright G. Pulmonary metastasectomy: analysis of survival and prognostic factors in 243 patients. ANZ J Surg. John Wiley & Sons, Ltd (10.1111); 2018;88:1316–21.
Migliore M, Jakovic R, Hensens A, Klepetko W. Extending surgery for pulmonary Metastasectomy what are the limits? J Thorac Oncol. 2010;5:S155–60.
Dear RF, Kelly PJ, Wright GM, Stalley P, McCaughan BC, Tattersall MHN. Pulmonary metastasectomy for bone and soft tissue sarcoma in Australia: 114 patients from 1978 to 2008. Asia Pac J Clin Oncol. 2012;8:292–302.
Roberge D, Vakilian S, Alabed YZ, Turcotte RE, Freeman CR, Hickeson M. FDG PET/CT in initial staging of adult soft-tissue sarcoma. Sarcoma. 2012;2012:960194.
Moreau L-C, Turcotte R, Ferguson P, Wunder J, Clarkson P, Masri B, et al. Myxoid\round cell Liposarcoma (MRCLS) revisited: an analysis of 418 primarily managed cases. Ann Surg Oncol. 5 ed. Springer-Verlag; 2011. 19:1081–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Wright, G. (2021). Surgical Management of Pulmonary Metastases from Sarcoma. In: Choong, P.F.M. (eds) Sarcoma . Springer, Singapore. https://doi.org/10.1007/978-981-15-9414-4_18
Download citation
DOI: https://doi.org/10.1007/978-981-15-9414-4_18
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-9413-7
Online ISBN: 978-981-15-9414-4
eBook Packages: MedicineMedicine (R0)