Abstract
Ophthalmic oncology has emerged as a distinct subspecialty of ophthalmology over the last few decades. A close collaboration is often needed between several specialties for the ideal management of these cases. While primary ocular malignancies form the bulk of the cases that an ocular oncologist manages, not uncommonly they may be called upon to comanage systemic malignancies with secondaries in the eye. A variety of intraocular tumors have been described in the eye but the commonest remain the retinoblastoma in children and choroidal melanoma in the adults. The management of these tumors has undergone a sea of change due to the tremendous advances made on all fronts. These include advances in imaging, chemotherapy protocols, newer approaches in delivery of chemotherapy, newer uses of lasers, identification of genetic and molecular markers, etc.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1.1 What Constitutes Ophthalmic Oncology?
Ophthalmic oncology is one of the advanced and multidisciplinary ophthalmic subspecialties that involves the diagnosis and management of intraocular, ocular surface, and ocular adnexal (orbit, eyelid, and lacrimal system) tumors. Most tumors arise primarily from the site (one of the sites mentioned above) where they are found. Not infrequently, they can also metastasize from known or unknown primary malignancy elsewhere or spread by contiguity from adjacent sites such as paranasal sinuses, nasopharynx, or intracranial cavity. On occasions, the ophthalmologist may be the first to diagnose a systemic malignancy that has metastasized to the eye or orbit, causing ophthalmic symptoms before causing symptoms related to the primary malignancy.
1.2 Who Are the Personnel Involved in the Management?
An ideal practice of Ophthalmic Oncology involves close collaboration between many specialists, both within ophthalmology and beyond. Apart from the ophthalmologist, other specialists involved include, the diagnostic and interventional radiologist, radiation oncologist along with radiation physicist, pediatric and adult oncologist, ocular pathologist, geneticist, ocular prosthetician and anaplastologist, etc. Each one serves a distinct and important role with the ophthalmologist playing the lead role. Depending on background training of the ophthalmic oncologist, additional help may be needed from other ophthalmic subspecialists such as corneal surgeon, vitreoretinal surgeon, oculoplastic and orbital surgeon, etc.
Considering the complexity of the issues and numerous advances in various fields like chemotherapy, targeted therapy, tele- and brachytherapy, etc., one often needs the help of super specialists within each of the above-mentioned specialties. For example: a pediatric rather than an adult oncologist would be appropriate to advise, administer, and monitor the chemotherapy for retinoblastoma. Likewise, a general pathologist may not be best equipped to interpret a vitreous biopsy done for suspected intra ocular lymphoma. One needs a pathologist with special interest in ophthalmic pathology—not just with histopathologic techniques but also immunohistochemical techniques and even molecular genetic studies to come to reliable conclusions. Similarly, one needs an interventional radiologist who has experience in children to be able to cannulate the ophthalmic artery in a small child.
Given the rapid expansion in knowledge and application of numerous techniques for organ/vision salvage, therefore, ideally, an ophthalmic oncologist should be fellowship trained—either a vitreoretinal surgeon (intraocular tumors) or an oculoplastic surgeon (ocular surface and ocular adnexal tumors), and not just a general ophthalmologist attempting to manage everything including tumors of the eye.
1.3 What Are the Commonest Tumors One Comes Across?
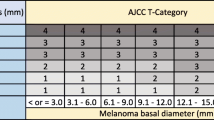
The incidence and prevalence of most ocular and adnexal tumors are generally constant in most ethnic groups worldwide and geographically as well. However, there are specific tumors that are more common in certain ethnic and geographical situations, which one should be aware of. While metastatic tumors in the choroid are said to be the commonest intra ocular tumors seen [1], retinoblastoma still remains the commonest intra ocular tumor that an ophthalmologist is called upon to manage—a tumor that threatens vision and life of a child. In the Asian population, choroidal melanoma is not as common as in the Caucasian population [2], but is still seen reasonably frequently—hence often misdiagnosed and mismanaged. On the contrary, both ocular surface neoplasms and sebaceous gland carcinomas of the eyelid are much more common in Asians compared to the Caucasian population [3]. Likewise, a combination of fair complexion and increased sun exposure has led to a significant increase in basal cell carcinoma and melanoma in the Australian population [4]. Patients with xeroderma pigmentosa, have been shown to have an increased risk of all cutaneous and ocular surface neoplasms [5]. An overview of common and less common intraocular and ocular adnexal tumors is shown in Table 1.1.
1.3.1 Presentation
Traditionally neglect and delay in presentation has been the norm in developing countries like India so much so that the commonest presentation of retinoblastoma in the 1970s was orbital presentation with proptosis [6]. Fortunately, the awareness levels have improved significantly and currently eye salvage is possible in a higher percentage of cases.
Ocular and adnexal tumors affect all ages. However, each type of tumor has usually a distinct age range of presentation. While retinoblastomas occur in children in the age group of 2–5 years [7], choroidal melanomas tend to occur in the adult age group. However, one must be cognizant of exceptions and be alert to avoid misdiagnosis. Retinoblastoma can occur in relatively older children and on occasion in adults [8], while choroidal melanoma has been reported in young children as well [9].
1.4 What Changes Were Seen in the Investigational Approach?
While most ocular and adnexal tumors can be reliably suspected and diagnosed based on history and clinical examination alone, imaging of the eye and orbit are frequently employed to narrow down and further refine preoperative diagnosis. Advances in technology have provided us with high resolution images of the eye and orbit. Ocular surface lesions may be imaged with (ASOCT) which may help in staging the disease and guide surgical treatment. For intra ocular tumors, ultrasonography still remains an important ophthalmologist performed investigation. It is an excellent cost-effective and reliable tool useful in diagnosis and follow up for some tumors. Additional information can be obtained from fluorescein and indocyanine green angiography. In case of tumors in ciliary body area, ultrasound biomicroscopy is valuable. Swept source optical coherence tomography has been a good addendum to imaging shallow tumors of the choroid [10, 11].
Contrast enhanced computed tomography (CECT) remains the imaging of choice for most orbital and ocular adnexal tumors, partly because of good bone and soft tissue differentiation, easy readability and also its cost-benefit ratio. However, in certain situations such as soft tissue tumors, apical orbital or optic nerve/sheath lesions and in young children who may require repeated imaging, magnetic resonance imaging (MRI) is the preferred modality of imaging, considering the possibility for greater soft tissue detail. In children with retinoblastoma, the radiation exposure of CT scan can increase the risk of second tumors and hence MRI is preferred—especially if the patient is less than 2 years old and with suspected germ line mutation [12].
When primary malignancy of the eye or adnexa or suspected, a positron emission tomography combined with computed tomography (PET-CT) is often employed to detect systemic spread and thus stage the disease prior to management.
Documentation has become easier with wide-angle imaging provided by Retcam and Optos fundus cameras. These not only provide crucial documentation but permit accurate comparison between visits to assess regression or otherwise of the tumor and appropriately change the approach to management [13]. They also help communicate with the patient/relatives better.
1.5 What Changes Have Taken Place in the Management Approaches?
In the management of retinoblastoma, several paradigm shifts have taken place. Historically most globes were enucleated. Currently with a combination of chemotherapy and local aggressive treatment, the threshold for enucleation is raised significantly, with attempts made to salvage most eyes even in unilateral cases. Chemotherapy has acquired the role of primary treatment. While systemic administration is still the most common route of administration, intra-arterial and intravitreal routes of administration of these agents have enabled salvage of many more eyes than before. External beam radiation which was the treatment of choice in the past has now become the last therapeutic option. While plaque therapy is nothing new, the greater access to this facility has enabled its application to several posterior segment, anterior segment as well as surface tumors- both as primary treatment (choroidal melanoma) as well as salvage treatment after chemotherapy (retinoblastoma).
Direct high intensity thermal laser photocoagulation of retinoblastoma tumors has been replaced by slow heating using transpupillary thermotherapy. Photodynamic therapy has been found useful in eyes with choroidal hemangioma (with verteporfin) and some cases of retinoblastoma (with Indocyanine green dye) [14].
Ocular surface and adnexal tumors (sebaceous gland carcinoma of the eyelid, adenoid cystic carcinoma (ACC) of the lacrimal gland) which were managed with orbital exenteration are being managed by more conservative techniques of chemoreduction, topical immunotherapy (OSSN) [15], followed by local excision and a combination of postoperative adjuvant radiotherapy and chemotherapy(ACC) with better globe, vision and life preservation.
Targeted systemic therapy with Rituximab, BRAF inhibitors, etc. (based on histological type and molecular genetics) is playing increasing role in conditions such as orbital lymphoma and some metastatic melanomas [16,17,18].
1.6 Redefining the Role of Genetics and Molecular Markers
Genetics is no longer restricted to broad genetic counseling based on the known inheritance patterns of the tumors. Specific molecules can serve as biomarkers for the diagnosis and prognostication of intraocular malignancies. In addition, some distinctive molecules closely related to the growth profiles of different tumors can serve as valuable indicators of prognosis and for survival analysis.
In uveal melanoma, patients with monosomy of chromosome 3 have poorer prognosis (i.e., due to metastatic disease) [19] likely due to mutations identified in BAP1 (BRCA associated protein 1) [20]. Genetic testing of the trans vitreal retinochoroidal vitrector biopsy sample provided accurate stratification of patients with high, intermediate and low risk, based on copy number variations of chromosomes 3 and 8 [21].
Primary intraocular lymphomas (PIOL) are mostly monoclonal B-cell lymphomas that stain positively for B-cell markers, such as CD19, CD20, and CD22. They show restricted expression of either kappa or lambda chain, express germinal center markers such as BCL6 and CD10 and secrete high amounts of IL-10 (an immunosuppressive cytokine) [22]. MYD88 mutations detection by polymerase chain reaction significantly improves the diagnostic yield of vitrectomy specimens [23].
Retinoblastoma develops in the embryonic retina following biallelic loss of RB1. However, there are a wide range of genetic and epigenetic changes that can affect RB1 resulting in different clinical outcomes. In addition, other transformations, such as MYCN amplification, have been known to generate particularly aggressive tumors [24, 25].
Further, genetic studies on specific molecules and pathways could reveal more detailed features of intraocular tumors and provide hints or identifying pivotal molecules that can be targeted therapeutically.
1.6.1 Region Specific Issues
Despite the progress in many fronts in the understanding of the disease, availability of newer chemotherapeutic drugs, etc. there are several challenges one faces in a country like India with diversity in cultures, beliefs, financial capabilities, and geographic locations. Cost of treatment remains the most important factor that controls the final outcome of treatment. Crucial to the success of treatment in a condition like retinoblastoma is the rigidity with which follow up schedules are maintained and interventional treatment is administered—a goal not always attained because of social issues. Reluctance to subject a child to enucleation based on religious beliefs is still an issue to reckon with.
1.6.2 Proactive Approaches
Traditionally medicine has been reactive—investigating and treating only when the patient comes with symptoms or signs. There are several situations in ocular oncology however, where being proactive is desired and probably mandated. Top in this list is the need to screen siblings of a child with retinoblastoma periodically till the risk of occurrence is estimated to be very low. This recommendation is applicable even to yet to be born siblings. Detecting the intra ocular tumor while the child is in utero has enabled early delivery of the child and prompt institution of treatment thus salvaging the eyes [26].
In cases of angiomatosis retinae, the routine evaluation with MRI brain, abdominal ultrasound, etc. for other known associated tumors in the body is a well-known practice.
References
Bornfield N. Uveal metastatic tumors. In: Singh A, editor. Clinical ophthalmic oncology. Philadelphia: Saunders Elsevier; 2007. p. 322. Section 4.
Pal BP, Garge S, Khetan V. Choroidal melanoma: a short review with an Indian perspective. Oman J Ophthalmol. 2017;10:135–44.
Kaliki S, Ayyar A, Dave TV, Ali MJ, Mishra DK, Naik MN. Sebaceous gland carcinoma of the eyelid: clinicopathological features and outcome in Asian Indians. Eye (Lond). 2015;29:958–63.
Kricker A, Weber M, Sitas F, Banks E, Rahman B, et al. Early life UV and risk of basal and squamous cell carcinoma in New South Wales, Australia. Photochem Phtobiol. 2017;93:1483–91.
Takebe H, Nishigori C, Tatsumi K. Melanoma and other skin cancers in xeroderma pigmentosum patients and mutations in their cells. J Invest Dermatol. 1989;92:236S–8S.
Dhir SP, Jain IS, Dar GR, Gupta HD. Survival of retinoblastoma cases in North India. Ind J Ophthalmol. 1980;28:97–100.
de Aguirre Neto JC, Antoneli CB, Ribeiro KB, Castilho MS, Novaes PE, Chojniak MM, Arias V. Retinoblastoma in children older than 5 years of age. Pediatr Blood Cancer. 2007;48(3):292–5. PubMed PMID: 16847922.
Sengupta S, Pan U, Khetan V. Adult onset retinoblastoma. Ind J Ophthalmol. 2016;64:485–91.
Kalki S, Shields CL. Uveal melanoma: relatively rare but deadly cancer. Eye. 2017;31:241–57.
Filloy A, Caminal JM, Arias L, Jordan S, Catala J. Swept source optical coherence tomography imaging of a series of choroidal tumours. Can J Ophthalmol. 2015;50:242–8.
Pellegrini M, Invernizzi A, Ravera V, Cereda MG, Staurenghi G. Swept source optical coherence tomography angiography in choroidal melanoma: an analysis of 22 consecutive cases. Retina. 2019;39:1510–9.
Graaf PD, Goricke S, ROdjan F, Galluzzi P, Maeder P, Castelijns JA, Brisse HJ. Guidelines for imaging retinoblastoma: imaging principles and MRI standardization. Pediatr Radiol. 2012;42:2–14.
Dixon BR, Morawski K. Usefulness of Ret-Cam imaging in diagnosis, treatment and monitoring of retinoblastoma. Acta Ophthalmol. 2017;95(S259).
Hasapreisoglu M, Saktanasate J, Schwendeman R, Shields JA, Shields CL. Indocyanine green—enhanced trans pupillary thermo therapy for retinoblastoma: analysis of 42 tumors. J Pediatr Ophthalmol Strabismus. 2015;52:348–54.
Kaliki S, Singh S, Iram S, Tripuraneni D. Recombinant interferon alpha 2b for ocular surface squamous neoplasia: an efficient and cost-effective treatment modality in Asian Indian patients. Ind J Ophthalmol. 2016;64:702–9.
Annibali O, Chiodi F, Sarlo C, et al. Rituximab as single agent in primary malt lymphoma of the ocular adnexa. Biomed Res Int. 2015;2015:895105. (On line publication).
Sullivan TJ, Grimes D, Bunce I. Monoclonal antibody treatment of orbital lymphoma. Ophthal Plast Reconstr Surg. 2004;20:103–6.
Flaherty KT, Puzanov I, Kim KB, Ribas A, et al. Inhibition of mutated, activated BRAF in metastatic melanoma. N Engl J Med. 2010;363:809–19.
Sandinha MT, Farquharson MA, McKay IC, Roberts F. Monosomy 3 predicts death but not time until death in choroidal melanoma. Invest Ophthalmol Vis Sci. 2005;46(10):3497–501. PubMed PMID: 16186325.
Harbour JW, Onken MD, Roberson DO, Duan S, Cao L, Worley LA, Council ML, Matatall KE, Helms C, Bowcock AM. Frequent mutation of BAP1 in metastasizing uveal melanomas. Science. 2010;330:1410–3.
Bagger M, Andersen MT, Heegaard S, Andersen MK, Kiilgaard JF. Transvitreal retinochoroidal biopsy provides a representative sample from choroidal melanoma for detection of chromosome 3 aberrations. Invest Ophthalmol Vis Sci. 2015;56(10):5917–24. https://doi.org/10.1167/iovs.15-17349. PubMed PMID: 26377078.
Sen HN, Bodaghi B, Hoang PL, Nussenblatt R. Primary intraocular lymphoma: diagnosis and differential diagnosis. Ocul Immunol Inflamm. 2009;17(3):133–41. https://doi.org/10.1080/09273940903108544. Review. PubMed PMID: 19585354; PubMed Central PMCID: PMC2924171.
Bonzheim I, Giese S, Deuter C, Süsskind D, Zierhut M, Waizel M, Szurman P, Federmann B, Schmidt J, Quintanilla-Martinez L, Coupland SE, Bartz-Schmidt KU, Fend F. High frequency of MYD88 mutations in vitreoretinal B-cell lymphoma: a valuable tool to improve diagnostic yield of vitreous aspirates. Blood. 2015;126(1):76–9. https://doi.org/10.1182/blood-2015-01-620518. Epub 2015 Apr 21. PubMed PMID: 25900979.
Theriault BL, Dimaras H, Gallie BL. The genomic landscape of retinoblastoma: a review. Clin Exp Ophthalmol. 2014;42:33–52.
Rushlow DE, Mol BM, Kennett JY, Yee S, Pajovic S, Theriault BL, et al. Characterization of retinoblastomas without RB1 mutations: genomic, gene expression, and clinical studies. Lancet Oncol. 2013;14(4):327–34. https://doi.org/10.1016/S1470-2045(13)70045-7.
Manjandavida FP, Xia J, Zhang J, Tang XY, Yi HR. In utero ultrasonography detection of fetal retinoblastoma and neonatal selective ophthalmic artery chemotherapy. Ind J Ophthalmol. 2019;67:958–60.
Financial Disclosure
Nil.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Editor(s) (if applicable) and The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Gopal, L., Sundar, G., Xinyi, S. (2021). Overview of Ophthalmic Tumors. In: Nema, H.V., Nema, N. (eds) Ocular Tumors. Springer, Singapore. https://doi.org/10.1007/978-981-15-8384-1_1
Download citation
DOI: https://doi.org/10.1007/978-981-15-8384-1_1
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-8383-4
Online ISBN: 978-981-15-8384-1
eBook Packages: MedicineMedicine (R0)