Abstract
The etiology of primary angle-closure glaucoma (PACG) is multifactorial but much is still to be investigated. Environmental or inducible factors are not evidently identified. Gene variants confirmed in association with PACG account for less than 5% of PACG heritability. Considerably smaller number of genes were mapped and less gene variants known to associate with PACG than primary open-angle glaucoma (POAG), another major form of glaucoma. But PACG loci are clearly distinctive from the associated gene variants of POAG. The genetic components of PACG include large ethnic differences in prevalence, familial trends of occurrence, the heritability of phenotype and susceptible genes which are identified principally by candidate gene investigations, familial linkage analyses, and genome-wide association studies (GWAS). The only PACG endophenotype with known genetic association is anterior chamber depth. More PACG genes will be mapped by GWAS and whole-genome sequencing with family analysis. Genotype-phenotype correlation studies on big cohorts with longitudinal follow up for the establishment of pharmacogenomics database and genetic biomarkers will be key areas of attention for PACG.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
15.1 Introduction
Primary angle-closure glaucoma (PACG) is a complex disease with multifactorial etiology, which involves complicated anatomical, physiological and genetic mechanisms [1]. Narrow to closed anterior chamber angle, pupillary block, and plateau iris are essential anatomical features in PACG. The former is a pre-requisite of obstruction to aqueous outflow in the trabecular meshwork. Pupillary block is usually a triggering factor for acute angle-closure attack [2]. The plateau iris is a common cause of persistent occludable angle after iridotomy [3]. PACG is also linked to other anatomical abnormalities, such as shortened axial length, shallowed anterior chamber depth, and increased lens volume as seen in cataract. Environmental risk factors for PACG are not readily quantifiable, except that aging plays an important role. Angle-closure glaucoma (ACG) can be secondary to ocular diseases like chronic uveitis and rubeosis iridis that lead to synechial angle closure. ACG can also develop with some congenital conditions, mainly nanophthalmos and Axenfeld Rieger Syndrome, which are resulted from angle dysgenesis [4,5,6]. Therefore, there has to be differentiation of primary and secondary forms of ACG for treatment plan since the pathology is so different. The genetic basis for such complex disease mechanisms is understandably complicated [7]. However, in comparison with primary open-angle glaucoma (POAG), another major glaucoma form, there is currently no gene known to cause PACG directly [8]. The number of genes confirmed to have an association with PACG is also limited.
Albeit such complex mechanistic background with unknown environmental risk, the genetic basis of PACG is evidently attributed to ethnic diversities in prevalence, familial linkage, and phenotype heritability [9, 10]. Genes with strong and clear susceptibility for PACG have been mapped by candidate gene approach, family linkage analysis, and genome-wide association study (GWAS) [8, 11].
15.2 Genetic Epidemiology of PACG
PACG prevalence is known to be diversified among different ethnic populations, in general lower in Caucasians and higher in Asian populations [7]. Its occurrence was noticeably high in the Inuit population including Eskimos in the Arctic regions. Almost 5% of the Eskimos populations over 40 years old in Greenland and Alaska have PACG, about 40 times higher than Europeans [12, 13]. In a systemic review of PACG studies in Europeans published during 1948–2011, PACG prevalence for people over 40 years old was 0.4% (95% confidence interval [CI]: 0.3%–0.5%), with female to male ratio 3.25 to 1 [14]. PACG occurs more in Asians than Europeans. In a meta-analysis and review of 50 population-based studies, PACG is the highest in Asia at 1.09% (95% CI: 0.43–2.32%) against 0.60% (95% CI: 0.16–1.48%) in Africa, 0.42% (95% CI: 0.13–0.98%) in Europe, and 0.26% (95% CI: 0.03–0.96%) in North America [15]. When two big Indian studies were included in the meta-analysis, PACG prevalence in Asia was decreased to 0.73% (95% CI: 0.18–1.96%) [16]. It is notable in this study that in contrast to POAG, in which the prevalence is essentially similar among different Asian populations, PACG at age between 40 and 80 years occurs more in East Asia (Mongolia, China, Korea, and Japan) at 1.07% (95% CI: 0.28–2.74%), than South Central Asia (India, Iran, Nepal, and Sri Lanka) at 0.69% (95% CI: 0.13–2.07%) or South East Asia (Singapore, Myanmar, and Thailand) at 0.64% (95% CI: 0.19–1.49%). People in East Asia are 5.55 times (95% CI: 1.52–14.73) more likely than people in South East Asia to develop PACG after adjustment for gender and age [16]. Overall in Asia, males aged between 40 and 80 years have a higher likelihood to have POAG (odds ratio [OR]: 1.37, 95% CI: 1.17–1.59) than females, but less to have PACG (OR: 0.54, 95% CI: 0.41–0.71). For this age range, people of urbanized habitation have less PACG at 0.73% than rural living people at 0.94%. Notably, the trend was reversed for POAG, 2.24% against 1.53%. In a recent study in Eastern India, with 7408 people living in rural areas and 7248 in cities, PACG is also higher in rural living at 1.03% (95% CI: 0.99–1.07%) than in city dwellers at 0.97% (95% CI: 0.94–1.00%) [17].
In Chinese, a meta-analysis of 11 population-based studies conducted in different parts of China during January 1990 to July 2010 involving 35,968 adult Chinese reported a pooled PACG prevalence of 1.4% (95% CI: 1.0–1.7%), with women more likely to have PACG than men (OR: 1.75; 95% CI: 1.20–2.56; P = 0.004) [18]. In a recent meta-analysis of 30 cross-sectional studies reported between 1995 and 2016 from various regions of China, PACG prevalence was 1.40% (95% CI: 1.17–1.68%) for Chinese aged between 45 and 89 years [19]. There was also less PACG male patients than females (OR: 0.53; 95% CI: 0.46–0.60) [19]. PACG prevalence was reportedly 0.5% (95% CI: 0.3–0.7%) in a rural population aged over 40 years in the Handan of northern China [20]. In the same population, the prevalence of primary angle closure was higher at 1.5% (95% CI: 1.2–1.8%) and even higher for primary angle-closure suspects at 10.4% (95% CI: 9.6–11.2%). Moreover, females are more likely to develop PACG than males with an OR ranging from 1.75 to 1.89 (P < 0.05) [18,19,20]. Occurrence of POAG was similar, with an overall prevalence at 1.02% (95% CI: 0.67–1.57%) [21].
Ethnic differences in the prevalence of PACG and gender bias in disease susceptibility indicated the presence of genetic influences. In terms of environmental influence, rural living poses a higher risk than urbanized inhabitation.
15.3 Sporadic and Familial PACG
Sporadic PACG is usually late-onset with disease incidence increases with age. Familial history is also long known to be a risk factor across all populations [7, 22, 23]. In Greenland Eskimos, who are Inuit by race, family history poses more than three times risk of PACG [12]. A high heritability of narrow angle of about 60% has been revealed in a study of 100 Chinese probands with 327 first-degree relatives [24]. Among the 515 sibling pairs, a high probability of 50% was detected for narrow angle, with a sevenfold increase in likelihood of narrow angle when compared with the general population.
In 303 South Indian sibling pairs, primary angle closure (PAC)/PACG was found in 11.4% of PAC/PACG siblings but only in 4.9% of primary angle-closure suspects (PACS) siblings (P = 0.07) and even none in open-angle (OA) siblings (P = 0.002). There was more angle closure in PACS (35.0%) and PAC/PACG siblings (36.7%) than in OA siblings (3.7%; P < 0.001). Multivariable analysis after adjustment for age and gender revealed a 13.6-fold of higher likelihood of having angle closure if one has angle-closure siblings than with OA siblings (95% CI: 4.1–45.0; P < 0.001) [25]. In a recent study also in southern India of 636 sibling pairs (482 PACS and 154 PAC/PACG), the occurrence of PAC/PACG among siblings of PAC/PACG was 8.4%, which was higher than the 3.5% of PAC/PACG among siblings of PACS [26]. In Central Asia, familial segregation of angle closure was also reported in an Iranian study, with siblings of PACG patients at higher risk [27].
15.4 Phenotype Heritability
Hereditability of anatomical and ophthalmic features in relation to both major forms of glaucoma, POAG and PACG, have been reported in different ethnic populations. Compared with the general population, PACG has greater central cornea thickness (CCT), shorter axial length (AL), shallower anterior chamber depth (ACD), bigger cup-to-disc ratio, and narrower angle width. These are independent risk factors [17]. Intraocular pressure (IOP) is one dominant risk factor for PACG. Its heritability has been estimated to range from 0.36–0.50 [24, 28]. In Greenland Eskimos, the corneoscleral size was found to be inheritable [13]. For cup-to-disc ratio, the heritability ranged from 0.48 to 0.80 [29, 30]. The variance in drainage angle width in Chinese children appeared to be largely attributable to genetic effects, with a heritability of approximately 70% [31]. The variance of optic nerve head parameters, namely disc area (DA), cup area (CA), and cup/disc area ratio (CDAR) appears to be attributable to additive genetic and unshared environmental effects. Approximately 80% of these phenotypic variances are genetically determined [32]. Genetic variants have been tested in a recent study on Chinese PACG patients, and three SNPs, rs3753841 in COL11A1, rs1258267 in CHAT, and rs736893 in GLIS3, were associated with PACG and also had a mild association with ACD [33]. In the same cohort, rs7290117 in ZNRF3 was associated with axial length in PACG patients, but not with PACG [34]. Besides, a number of genetic variants associated with the endophenotypes of glaucoma had been identified in population-based samples. A SNP rs1015213 at the PCMTD1-ST18 locus has been associated with ACD in a European population [35]. SNP rs33912345 in SIX6, a POAG gene, has been associated with optic disc parameters in Europeans [36], and retinal nerve fiber layer thickness in Europeans and Chinese [36, 37]. Three SNPs (rs7126851, rs7104512, and rs10835818) in the ELP4 gene, which neighbors and plays a crucial role in the expression of PAX6, were associated with disc area in Caucasians [38]. In a GWAS of optic disc parameters in population-based cohorts, SNPs at chromosomal regions 1p22 (near CDC7), 10q21.3-q22.1 (near ATOH7), and 16q12.1 were associated with optic disc area, and SNPs at 9p21 (near CDKN2B), 14q22.3-q23 (near SIX1), 11q13, 13q13, 17q23, and 22q12.1 were associated with vertical cup-to-disc ratio [39].
15.5 Mapping the PACG Genes by Candidate Gene Analysis
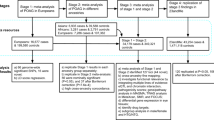
Many attempts have been made to map PACG genes in different ethnic populations utilizing cohorts of PACG patients and controls [9]. A candidate gene analysis has led to the identification of nine genes associated with PACG (Table 15.1). In a meta-analysis, we summarized all reported genetic associations from candidate gene analysis and affirmed five genes (HGF, HSP70, MFRP, MMP9, and NOS3) to be associated with primary angle-closure disease [10]. Most candidate gene association studies did not involve a big sample size. Some of the genes have not been replicated. They are statistically linked to susceptibility to PACG, not directly causative. Understanding of the functions and properties of these genes have given some clues to the disease mechanism but not the elucidation of the pathogenesis [9]. It is notable that MTHFR and HGF have been linked to the regulation of axial length, and shorter axial length is a trait of PACG.
Different investigation strategies other than direct comparison of patient and control genotypes have recently identified novel PACG genes. In an exploration of gene expressions in peripheral blood of Korean patients with acute PACG, microarray analysis of RNA extracted from mononuclear cells showed upregulation of 347 gene transcripts and downregulation of 696 transcripts by more than twofold than controls. Further molecular studies including RT-PCR have confirmed the association of PACG with thrombospondin-1 (TSP-1), transforming growth factor (TGF-β1), and prostaglandin-endoperoxide synthase (2PGE2) [54]. In a big Iranian pedigree with 8 affected individuals with PAC, confirmed PACG, and PACS, investigations by extensive family linkage analysis, segregation analysis, whole-genome sequencing, and sequence screening of other unrelated patients and controls have identified COL18A1 mutations evident for causing the iridocorneal angle closure in these patients [53]. Future work on the structural and functional roles of type XVIII collagen, especially in the human iris and cornea, should help to reveal the pathophysiology of angle closure.
15.6 Mapping the PACG Genes by Genome-wide Association Studies
So far three major GWAS have been conducted for PACG, having identified 9 genes with specific polymorphisms associated with PACG with high statistical significance (Table 15.2). The primary cohort was mixed in ethnicities and validation has been conducted in multiple ethnic populations including Caucasians, Indians, Malays, Chinese, Koreans, and Japanese [55, 59, 61]. In a previous meta-analysis, we have assessed replication studies on the GWAS SNPs reported by Vithana E et al. [55] and Nongpiur ME et al. [59], and affirmed 3 of them, rs11024102 of PLEKHA7, rs3753841 of COL11A1 rs1015213 of PCMTD1-ST18, to be significantly associated with PACG (Table 15.2) [10]. In subsequent replication studies, three of the associated SNPs, rs1015213 of PCMTD1-ST18, rs3816415 of EPDR1, and rs3739821 of DRM2-FAM102A showed consistent associations with PACS in a Chinese cohort [56]. Two SNPs of high GWAS significance, rs11024102 of PLEKHA7 and rs3753841 of COL11A1, were not replicated in a South Indian cohort [57]. The latter, COL11A1 rs3753841, however, was replicated in a combined cohort of Australian Caucasians and Nepalese patients and controls but not in each individual cohort [62]. Three other GWAS significant SNPs, GLS3 rs736893, FERMT2 rs726893, and GLS3 rs1258267 were also not associated with PACS in Chinese [56] (Table 15.2).
In a GWAS of ACD, genome-wide significant association was observed at an intronic SNP rs1401999 in the ABCC5 gene [59]. This locus was also associated with an increased risk of PACG, suggesting a shared genetic component between PACG and its endophenotype. After testing tagging SNPs spanning the PARL-ABCC5-HTR3D-HTR3C region in 422 Chinese PACG patients and 400 controls all living in urban areas, we have recently revealed significant associations of PACG with 2 synonymous ABCC5 SNPs, rs939336 (p.Cys594; OR = 1.46; 95% CI:1.08–1.97; P = 0.013;) and rs1132776 (p.Ala395; OR = 1.47; 95% CI: 1.10 to 1.95; P = 0.009) [60].
Among the GWAS associated genes, PLEKHA7, which encodes pleckstrin-homology-domain-containing protein 7, a junctional protein, was studied in cultured lens epithelial cells and iris tissue obtained from PACG patients, and non-pigmented ciliary epithelium (h-iNPCE) and primary trabecular meshwork cells [63]. The results revealed PLEKHA7 to be a novel Rac1/Cdc42 GAP with a regulatory role of Rac1 and Cdc42 in the tight junction permeability of the blood-aqueous barrier. SNP rs11024102 disrupts PLEKHA7 function, leading to deleterious effects in the blood-aqueous barrier integrity and likely aqueous humor outflow. This is thus a putative mechanism for PACG as caused by PLEKHA7.
15.7 Future Perspectives
Advancements in the knowledge of molecular genetics of a disease will benefit patients. Genes known to be causative of a disease can be studied for genetic markers for pre-symptomatic diagnosis and prediction of prognosis. Responses to treatment can be related to genomics. For a disease causative gene, the mechanism and disruptive pathways leading to pathogenesis can be elucidated by investigating the gene functions, properties, and interaction networks. New therapeutic agents can be tested based on the pathology. For PACG, no causative gene has been identified. A number of susceptible genes, with gene variants associated with the disease, are known. But the information is yet insufficient to establish a genetic marker or to throw light to the disease mechanism. GWAS on large samples of well-characterized patients is needed to find more PACG genes. Exome sequencing and whole-genome sequencing together with family linkage and sibling pair studies should help to identify more PACG genes and sequence variants that are responsible for the disease development.
References
Quigley HA. Angle-closure Glaucoma – simpler answers to complex mechanisms. Am J Ophthalmol. 2009;148:657–69.
Sundin OH, Leppert GS, Silva ED, Yang JM, Dharmaraj S, Maumenee IH, Santos LC, Parsa CF, Traboulsi EI, Broman KW, Dibernardo C, Sunness JS, Toy J, Weinberg EM. Extreme hyperopia is the result of null mutations in MFRP, which encodes a frizzled-related protein. Proc Natl Acad Sci U S A. 2005;102:9553–8.
Nongpiur ME, Ku JY, Aung T. Angle closure glaucoma: a mechanistic review. Curr Opin Ophthalmol. 2011;22:96–101.
Ritch R. Plateau iris is caused by abnormally positioned ciliary processes. J Glaucoma. 1992;1:23–6.
Carricondo PC, Andrade T, Prasov L, Ayres BM, Moroi SE. Nanophthalmos: a review of the clinical Spectrum and genetics. J Ophthalmol. 2018;2018:2735465.
Salmon JF. Predisposing factors for chronic angle-closure glaucoma. Prog Retinal Eye Res. 1998;18:121.
Wang X, Liu X, Huang L, Fang S, Jia X, Xiao X, Li S, Guo X. Mutation survey of candidate genes and genotype-phenotype analysis in 20 southeastern Chinese patients with Axenfeld-Rieger syndrome. Curr Eye Res. 2018 Nov;43(11):1334–41.
Wiggs JL, Pasquale LR. Genetics of glaucoma. Hum Mol Genet. 2017;26:R21–7.
Ahram DF, Alward WL, Kuehn MH. The genetic mechanisms of primary angle closure glaucoma. Eye (Lond). 2015;29:1251–9.
Rong SS, Tang FY, Chu WK, Ma L, Yam JC, Tang SM, Li J, Gu H, Young AL, Tham CC, Pang CP, Chen LJ. Genetic associations of primary angle-closure disease: a systematic review and Meta-analysis. Ophthalmology. 2016;123:1211–21.
Aung T, Khor CC. Glaucoma genetics: recent advances and future directions. Asia Pacific J Ophthalmol. 2016;5:256–9.
Alsbirk PH. Primary angle-closure glaucoma. Oculometry, epidemiology, and genetics in a high risk population. Acta Ophthalmol Suppl. 1976;127:5–31.
Alsbirk PH. Variation and heritability of ocular dimensions. A population study among adult Greenland Eskimos. Acta Ophthalmol. 1977;55:443–56.
Day AC, Baio G, Gazzard G, Bunce C, Azuara-Blanco A, Munoz B, Friedman DS, Foster PJ. The prevalence of primary angle closure glaucoma in European derived populations: a systematic review. Br J Ophthalmol. 2012;96:1162–7.
Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121:2081–90.
Chan EW, Li X, Tham YC, Liao J, Wong TY, Aung T, Cheng CY. Glaucoma in Asia: regional prevalence variations and future projections. Br J Ophthalmol. 2016;100:78–85.
Paul C, Sengupta S, Banerjee S, Choudbury S. Angle closure glaucoma in rural and urban populations in eastern India – the Hooghly River Glaucoma study. Indian J Ophthalmol. 2018;66:1285–90.
Cheng JW, Cheng SW, Ma XY, Cai JP, Li Y, Wei RL. The prevalence of primaryglaucoma in mainland China: a systematic review and meta-analysis. J Glaucoma. 2013;22:301–6.
Song P, Wang J, Bucan K, Theodoratou E, Rudan I, Chan KY. National and subnational prevalence and burden of glaucoma in China: a systematic analysis. J Glob Health. 2017;7:020705.
Liang Y, Friedman DS, Zhou Q, Yang XH, Sun LP, Guo L, Chang DS, Lian L, Wang NL. Handan eye study group. Prevalance and characteristics of primary angle-closure diseases in a rural adult Chinese population: the Handan eye study. Invest Ophthalmol Vis Sci. 2011;52:8672–9.
He M, Foster PJ, Ge J, Huang W, Zheng Y, Friedman DS, Lee PS, Khaw PT. Prevalence and clinical characteristics of glaucoma in adult Chinese: a population-based study in Liwan District. Guangzhou Invest Ophthalmol Vis Sci. 2006;47:2782–8.
Lowe RF. Primary angle closure glaucoma. Family histories and anterior chamber depths. Br J Ophthalmol. 1964;48:191–5.
Leighton DA. Survey of the first-degree relatives of glaucoma patients. Trans Ophthalmol Soc U K. 1976;96:28–32.
Amerasinghe N, Zhang J, Thalamuthu A, He M, Vithana EN, Viswanathan A, Wong TY, Foster PJ, Aung T. The heritability and sibling risk of angle closure in Asians. Ophthalmology. 2011;118:480–5.
Kavitha S, Zebardast N, Palaniswamy K, Wojciechowski R, Chan ES, Friedman DS, Venkatesh R, Ramulu PY. Family history is a strong risk factor for prevalent angle closure in a south Indian population. Ophthalmology. 2014;121:2091–7.
Zebardast N, Kavitha S, Palaniswamy K, Sengupta S, Kader MA, Raman G, Reddy S, Ramulu PY, Venkatesh R. Angle closure phenotypes in siblings of patients at different stages of angle closure. Ophthalmology. 2016;123:1622–4.
Yazdani S, Akbarian S, Pakravan M, Afrouzifar M. Prevalence of angle closure in siblings of patients with primary angle-closure glaucoma. J Glaucoma. 2015;24:149–53.
Klein BE, Klein R, Lee KE. Heritability of risk factors for primary open-angle glaucoma: the beaver dam eye study. Invest Ophthalmol Vis Sci. 2004;45:59–62.
Chang TC, Congdon NG, Wojciechowski R, Muñoz B, Gilbert D, Chen P, Friedman DS, West SK. Determinants and heritability of intraocular pressure and cup-to-disc ratio in a defined older population. Ophthalmology. 2005;112:1186–91.
He M, Liu B, Huang W, Zhang J, Yin Q, Zheng Y, Wang D, Ge J. Heritability of optic disc and cup measured by the Heidelberg retinal tomography in Chinese: the Guangzhou twin eye study. Invest Ophthalmol Vis Sci. 2008;49:1350–5.
He M, Ge J, Wang D, Zhang J, Hewitt AW, Hur YM, Mackey DA, Foster PJ. Heritability of the iridotrabecular angle width measured by optical coherence tomography in Chinese children: the Guangzhou twin eye study. Invest Ophthalmol Vis Sci. 2008;49:1356–61.
Tu YS, Yin ZQ, Pen HM, Yuan CM. Genetic heritability of a shallow anterior chamber in Chinese families with primary angle closure glaucoma. Ophthalmic Genet. 2008;29:171–6.
Zhuang W, Wang S, Hao J, Xu M, Chi H, Piao S, Ma J, Zhang X, Ha S. Genotype-ocular biometry correlation analysis of eight primary angle closure glaucoma susceptibility loci in a cohort from northern China. PLoS One. 2018;13:e0206935.
Wang S, Zhuang W, Ma J, Xu M, Piao S, Hao J, Zhang W, Chi H, Xue Z, Ha S. Association of Genes implicated in primary angle-closure Glaucoma and the ocular biometric parameters of anterior chamber depth and axial length in a northern Chinese population. BMC Ophthalmol. 2018;18:271.
Day AC, Luben R, Khawaja AP, Low S, Hayat S, Dalzell N, Wareham NJ, Khaw KT, Foster PJ. Genotype-phenotype analysis of SNPs associated with primary angle closure glaucoma (rs1015213, rs3753841 and rs11024102) and ocular biometry in the EPIC-Norfolk eye study. Br J Ophthalmol. 2013;97:704–7.
Khawaja AP, Chan MPY, Yip JLY, Broadway DC, Garway-Heath DF, Viswanathan AC, Luben R, Hayat S, Hauser MA, Wareham NJ, Khaw KT, Fortune B, Allingham RR, Foster PJ. A common Glaucoma-risk variant of SIX6 alters retinal nerve Fiber layer and optic disc measures in a European population: the EPIC-Norfolk eye study. J Glaucoma. 2018;27:743–9.
Cheng CY, Allingham RR, Aung T, Tham YC, Hauser MA, Vithana EN, Khor CC, Wong TY. Association of common SIX6 polymorphisms with peripapillary retinal nerve fiber layer thickness: the Singapore Chinese eye study. Invest Ophthalmol Vis Sci. 2014;56:478–83.
Gasten AC, Ramdas WD, Broer L, van Koolwijk LM, Ikram MK, de Jong PT, Aulchenko YS, Wolfs RC, Hofman A, Rivadeneira F, Uitterlinden AG, Oostra BA, Lemij HG, Klaver CC, Jansonius NM, Vingerling JR, van Duijn CM. A genetic epidemiologic study of candidate genes involved in the optic nerve head morphology. Invest Ophthalmol Vis Sci. 2012;53:1485–91.
Ramdas WD, van Koolwijk LM, Ikram MK, Jansonius NM, de Jong PT, Bergen AA, Isaacs A, Amin N, Aulchenko YS, Wolfs RC, Hofman A, Rivadeneira F, Oostra BA, Uitterlinden AG, Hysi P, Hammond CJ, Lemij HG, Vingerling JR, Klaver CC, van Duijn CM. A genome-wide association study of optic disc parameters. PLoS Genet. 2010;6:e1000978.
Micheal S, Qamar R, Akhtar F, Khan MI, Khan WA, Ahmed A. MTHFR gene C677T and A1298C polymorphisms and homocysteine levels in primary open angle and primaryclosed angle glaucoma. Mol Vis. 2009;15:2268–78.
Shi H, Zhang J, Zhu R, Hu N, Lu H, Yang M, Qin B, Shi J, Guan H. Primary angle closure and sequence variants within MicroRNA binding sites of genes involved in eye development. PLoS One. 2016;11:e0166055.
Chakrabarti S, Devi KR, Komatireddy S, Kaur K, Parikh RS, Mandal AK, Chandrasekhar G, Thomas R. Glaucoma-associated CYP1B1 mutations share similar haplotype backgrounds in POAG and PACG phenotypes. Invest Ophthalmol Vis Sci. 2007;48:5439–44.
Awadalla MS, Burdon KP, Thapa SS, Hewitt AW, Craig JE. A cross-ethnicity investigation of genes previously implicated in primary angle closure glaucoma. Mol Vis. 2012;18:2247–54.
Cao D, Liu X, Guo X, Cong Y, Huang J, Mao Z. Investigation of the association between CALCRL polymorphisms and primary angle closure glaucoma. Mol Vis. 2009;15:2202–8.
Awadalla MS, Thapa SS, Burdon KP, Hewitt AW, Craig JE. The association of hepatocyte growth factor (HGF) gene with primary angle closure glaucoma in the Nepalese population. Mol Vis. 2011;17:2248–54.
Ayub H, Khan MI, Micheal S, Akhtar F, Ajmal M, Shafique S, Ali SH, den Hollander AI, Ahmed A, Qamar R. Association of eNOS and HSP70 gene polymorphisms with glaucoma in Pakistani cohorts. Mol Vis. 2010;16:18–25.
Awadalla MS, Thapa SS, Hewitt AW, Craig JE, Burdon KP. Association of eNOSpolymorphisms with primary angle-closure glaucoma. Invest Ophthalmol Vis Sci. 2013;54:2108–14.
Shi H, Zhu R, Hu N, Shi J, Zhang J, Jiang L, Jiang H, Guan H. Association of frizzled-related protein (MFRP) and heat shock protein 70 (HSP70) singlenucleotide polymorphisms with primary angle closure in a Han Chinese population: Jiangsu eye study. Mol Vis. 2013;19:128–34.
Awadalla MS, Burdon KP, Kuot A, Hewitt AW, Craig JE. Matrix metalloproteinase-9 genetic variation and primary angle closure glaucoma in a Caucasian population. Mol Vis. 2011;17:1420–4.
Wang IJ, Chiang TH, Shih YF, Lu SC, Lin LL, Shieh JW, Wang TH, Samples JR, Hung PT. The association of single nucleotide polymorphisms in the MMP-9 genes with susceptibility to acute primary angle closure glaucoma in Taiwanese patients. Mol Vis. 2006;12:1223–32.
Cong Y, Guo X, Liu X, Cao D, Jia X, Xiao X, Li S, Fang S, Zhang Q. Association of the single nucleotide polymorphisms in the extracellular matrix metalloprotease-9 gene with PACG in southern China. Mol Vis. 2009;15:1412–7.
Micheal S, Yousaf S, Khan MI, Akhtar F, Islam F, Khan WA, den Hollander AI, Qamar R. Ahmed a polymorphisms in matrix metalloproteinases MMP1 and MMP9 are associated with primary open-angle and angle closure glaucoma in a Pakistani population. Mol Vis. 2013;19:441–7.
Suri F, Yazdani S, Chapi M, Safari I, Rasooli P, Daftarian N, Jafarinasab MR, Ghasemi Firouzabadi S, Alehabib E, Darvish H, Klotzle B, Fan JB, Turk C. Elahi E.COL18A1 is a candidate eye iridocorneal angle-closure gene in humans. Hum Mol Genet. 2018;27:3772–86.
Jeoung JW, Ko JH, Kim YJ, Kim YW, Park KH, Oh JY. Microarray-based analysis of gene expression profiles in peripheral blood of patients with acute primary angle closure. Ophthalmic Genet. 2017;38:520–6.
Vithana EN, Khor CC, Qiao C, Nongpiur ME, George R, Chen LJ, Do T, Abu-Amero K, Huang CK, Low S, Tajudin LA, Perera SA, Cheng CY, Xu L, Jia H, Ho CL, Sim KS, Wu RY, CCY T, PTK C, Su DH, Oen FT, Sarangapani S, Soumittra N, Osman EA, Wong HT, Tang G, Fan S, Meng H, DTL H, Wang H, Feng B, Baskaran M, Shantha B, Ramprasad VL, Kumaramanickavel G, Iyengar SK, How AC, Lee KY, Sivakumaran TA, VHK Y, SML T, Li Y, Wang YX, Tay WT, Sim X, Lavanya R, Cornes BK, Zheng YF, Wong TT, Loon SC, VKY Y, Waseem N, Yaakub A, Chia KS, Allingham RR, Hauser MA, DSC L, Hibberd ML, Bhattacharya SS, Zhang M, Teo YY, Tan DT, Jonas JB, Tai ES, Saw SM, Hon DN, Al-Obeidan SA, Liu J, TNB C, Simmons CP, Bei JX, Zeng YX, Foster PJ, Vijaya L, Wong TY, Pang CP, Wang N, Aung T. Genome-wide association analyses identify three new susceptibility loci for primary angle closure glaucoma. Nat Genet. 2012;44:1142–6.
Nongpiur ME, Cheng CY, Duvesh R, Vijayan S, Baskaran M, Khor CC, Allen J, Kavitha S, Venkatesh R, Goh D, Husain R, Boey PY, Quek D, Ho CL, Wong TT, Perera S, Wong TY, Krishnadas SR, Sundaresan P, Aung T, Vithana EN. Evaluation of primary angle-closure Glaucoma susceptibility loci in patients with early stages of angle-closure disease. Ophthalmology. 2018;125:664–70.
Duvesh R, Verma A, Venkatesh R, Kavitha S, Ramulu PY, Wojciechowski R, Sundaresan P. Association study in a south Indian population supports rs1015213 as a risk factor for primary angle closure. Invest Ophthalmol Vis Sci. 2013;54:5624–8.
Awadalla MS, Thapa SS, Hewitt AW, Burdon KP, Craig JE. Association of genetic variants with primary angle closure glaucoma in two different populations. PLoS One. 2013;8:e67903.
Nongpiur ME, Khor CC, Jia H, Cornes BK, Chen LJ, Qiao C, Nair KS, Cheng CY, Xu L, George R, Tan D, Abu-Amero K, Perera SA, Ozaki M, Mizoguchi T, Kurimoto Y, Low S, Tajudin LS, Ho CL, Tham CC, Soto I, Chew PT, Wong HT, Shantha B, Kuroda M, Osman EA, Tang G, Fan S, Meng H, Wang H, Feng B, Yong VH, Ting SM, Li Y, Wang YX, Li Z, Lavanya R, Wu RY, Zheng YF, Su DH, Loon SC, Yong VK, Allingham RR, Hauser MA, Soumittra N, Ramprasad VL, Waseem N, Yaakub A, Chia KS, Kumaramanickavel G, Wong TT, How AC, Chau TN, Simmons CP, Bei JX, Zeng YX, Bhattacharya SS, Zhang M, Tan DT, Teo YY, Al-Obeidan SA, Hon DN, Tai ES, Saw SM, Foster PJ, Vijaya L, Jonas JB, Wong TY, John SW, Pang CP, Vithana EN, Wang N, Aung T. ABCC5, a gene that influences the anterior chamber depth, is associated with primary angle closure glaucoma. PLoS Genet. 2014;10:e1004089.
Tang FY, Ma L, Tam POS, Pang CP, Tham CC, Chen LJ. Genetic association of the PARL-ABCC5-HTR3D-HTR3C locus with primary angle-closure Glaucoma in Chinese. Invest Ophthalmol Vis Sci. 2017;58:4384–9.
Khor CC, Do T, Jia H, Nakano M, George R, Abu-Amero K, Duvesh R, Chen LJ, Li Z, Nongpiur ME, Perera SA, Qiao C, Wong HT, Sakai H, Barbosa de Melo M, Lee MC, Chan AS, Azhany Y, Dao TL, Ikeda Y, Perez-Grossmann RA, Zarnowski T, Day AC, Jonas JB, Tam PO, Tran TA, Ayub H, Akhtar F, Micheal S, Chew PT, Aljasim LA, Dada T, Luu TT, Awadalla MS, Kitnarong N, Wanichwecharungruang B, Aung YY, Mohamed-Noor J, Vijayan S, Sarangapani S, Husain R, Jap A, Baskaran M, Goh D, Su DH, Wang H, Yong VK, Yip LW, Trinh TB, Makornwattana M, Nguyen TT, Leuenberger EU, Park KH, Wiyogo WA, Kumar RS, Tello C, Kurimoto Y, Thapa SS, Pathanapitoon K, Salmon JF, Sohn YH, Fea A, Ozaki M, Lai JS, Tantisevi V, Khaing CC, Mizoguchi T, Nakano S, Kim CY, Tang G, Fan S, Wu R, Meng H, Nguyen TT, Tran TD, Ueno M, Martinez JM, Ramli N, Aung YM, Reyes RD, Vernon SA, Fang SK, Xie Z, Chen XY, Foo JN, Sim KS, Wong TT, Quek DT, Venkatesh R, Kavitha S, Krishnadas SR, Soumittra N, Shantha B, Lim BA, Ogle J, de Vasconcellos JP, Costa VP, Abe RY, de Souza BB, Sng CC, Aquino MC, Kosior-Jarecka E, Fong GB, Tamanaja VC, Fujita R, Jiang Y, Waseem N, Low S, Pham HN, Al-Shahwan S, Craven ER, Khan MI, Dada R, Mohanty K, Faiq MA, Hewitt AW, Burdon KP, Gan EH, Prutthipongsit A, Patthanathamrongkasem T, Catacutan MA, Felarca IR, Liao CS, Rusmayani E, Istiantoro VW, Consolandi G, Pignata G, Lavia C, Rojanapongpun P, Mangkornkanokpong L, Chansangpetch S, Chan JC, Choy BN, Shum JW, Than HM, Oo KT, Han AT, Yong VH, Ng XY, Goh SR, Chong YF, Hibberd ML, Seielstad M, Png E, Dunstan SJ, Chau NV, Bei J, Zeng YX, Karkey A, Basnyat B, Pasutto F, Paoli D, Frezzotti P, Wang JJ, Mitchell P, Fingert JH, Allingham RR, Hauser MA, Lim ST, Chew SH, Ebstein RP, Sakuntabhai A, Park KH, Ahn J, Boland G, Snippe H, Stead R, Quino R, Zaw SN, Lukasik U, Shetty R, Zahari M, Bae HW, Oo NL, Kubota T, Manassakorn A, Ho WL, Dallorto L, Hwang YH, Kiire CA, Kuroda M, Djamal ZE, Peregrino JI, Ghosh A, Jeoung JW, Hoan TS, Srisamran N, Sandragasu T, Set SH, Doan VH, Bhattacharya SS, Ho CL, Tan DT, Sihota R, Loon SC, Mori K, Kinoshita S, Hollander AI, Qamar R, Wang YX, Teo YY, Tai ES, Hartleben-Matkin C, Lozano-Giral D, Saw SM, Cheng CY, Zenteno JC, Pang CP, Bui HT, Hee O, Craig JE, Edward DP, Yonahara M, Neto JM, Guevara-Fujita ML, Xu L, Ritch R, Liza-Sharmini AT, Wong TY, Al-Obeidan S, Do NH SP, Tham CC, Foster PJ, Vijaya L, Tashiro K, Vithana EN, Wang N, Aung T. Genome-wide association study identifies five new susceptibility loci for primary angle closure glaucoma. Nat Genet. 2016;48:556–62.
Awadalla MS, Thapa SS, Hewitt AW, Burdon KP, Craig JE. Association of genetic variants with primary angle closure glaucoma in two different populations. PLoS One. 2013;8:e67903.
Lee MC, Shei W, Chan AS, Chua BT, Goh SR, Chong YF, Hilmy MH, Nongpiur ME, Baskaran M, Khor CC, Aung T, Hunziker W, Vithana EN. Primary angle closure glaucoma (PACG) susceptibility gene PLEKHA7 encodes a novel Rac1/Cdc42 GAP that modulates cell migration and blood-aqueous barrier function. Hum Mol Genet. 2017;26:4011–27.
Acknowledgments
This work was supported in part by research grants 14100917 (C.P.P.) from the General Research Fund, Hong Kong; research grants 01122236, 11120801 and 07180256 (L.J.C.) from the Health and Medical Research Fund, Hong Kong; and the Endowment Fund for Lim Por-Yen Eye Genetics Research Centre, Hong Kong.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Ethics declarations
Li Jia Chen, Shi Song Rong, and Chi Pui Pang declare that they have no conflict of interest. No human or animal studies were performed by the authors for this article.
Rights and permissions
Copyright information
© 2021 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Rong, S.S., Pang, C.P., Chen, L.J. (2021). Recent Advances in our Understanding of the Genetic Basis of Primary Angle-Closure Glaucoma. In: Tham, C.C. (eds) Primary Angle Closure Glaucoma (PACG). Springer, Singapore. https://doi.org/10.1007/978-981-15-8120-5_15
Download citation
DOI: https://doi.org/10.1007/978-981-15-8120-5_15
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-8119-9
Online ISBN: 978-981-15-8120-5
eBook Packages: MedicineMedicine (R0)