Abstract
Recent advance in endoscopic imaging technology enables the endoscopists to detect esophageal squamous cell carcinoma (ESCC) more accurately than conventional white light imaging (WLI) and Lugol chromoendoscopy. Especially, a combination of narrow-band imaging (NBI) (Kaltenbach T, Gastroenterology 134:327–40, 2008) and magnifying endoscopy opened a brand new door of the endoscopic diagnostic field. NBI is classified in the category of equipment-based image-enhanced endoscope (IEE). Equipment-based IEE includes blue laser imaging (BLI) and i-scan optical enhancement (OE), which were developed after NBI.
Equipment-based IEE combined with magnifying endoscopy can visualize the microstructure of the squamous epithelial surface and microvasculature. Based on the morphological changes in these structures, we can make diagnosis ESCC more correctly and objectively. Therefore, in addition to the previous conventional strategy of endoscopic diagnosis, new diagnostic strategies based on morphological changes in the microvasculature and epithelial surface are now required and needed for the endoscopists.
In this chapter, we explained diagnostic strategies by practical endoscopy including detection, differential diagnosis, evaluation of depth of invasion, and histological confirmation of ESCC.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Endoscopic diagnosis
- Lugol chromoendoscopy
- Image enhanced endoscopy
- Narrow-band imaging
- Endoscopic ultrasound
5.1 Endoscopic Imaging of the Esophagus and ESCC
Endoscopy plays an important role in the detection and evaluation of the lateral and vertical extent of ESCC as well as other gastrointestinal cancers. Endoscopic imaging technology is now dramatically improved, and in particular, magnifying endoscopy and equipment-based IEE [1] provided dramatic breakthroughs in the endoscopic diagnosis of ESCC. High vision technology also contributed to the improvement of image quality.
In an endoscopic image, nonneoplastic and noninflammatory squamous epithelium appears as a flat surface, with a pink colored mucosa and an irregular vascular network (Figure 5.1a). In contrast, superficial cancerous lesions show an irregular surface (Figure 5.1b) and a reddish or whitish color change, while advanced cancerous lesions show clearly apparent irregular elevations or irregular ulceration (Figure 5.1c). In the most advanced ESCC, the esophageal lumen is obstructed by tumor and the endoscope cannot pass the stricture (Figure 5.1d).
The macroscopic findings of ESCC by endoscopy are very important for understanding the location, shape, and extent of the cancerous lesion, because these parameters are usually used for making decisions on their treatment. The distance of the tumor from the incisor teeth is usually measured by endoscopy. The Japanese Classification of Esophageal Cancer classifies the macroscopic tumor type into 6 categories (Types 0–5, Fig. 5.2) [2]. Tumor is defined as type 0 and recognized as superficial when the invasion is limited to the submucosa. Superficial (Type 0) ESCC is divided into 3 subtypes (0-I, 0-II, and 0-III). When the tumor invasion extends to the muscularis propria or beyond, the tumor is classified as advanced. Advanced ESCC is divided into 4 categories (Types 1, 2, 3, and 4). When a tumor cannot be classified into any of the first 5 categories (Types 0–4), it is classified as Type 5.
5.2 Endoscopic Detection and Differential Diagnosis of Superficial ESCC
Detection of advanced ESCC by endoscopy is easy. However, early detection of superficial ESCC is not always easy even for experienced endoscopists, because the endoscopic changes are usually minimal. Therefore, an ideal strategy for the early detection of ESCC is required.
5.2.1 Conventional White Light Imaging (WLI)
Conventional WLI of superficial ESCC shows disappearance of the vascular network in the mucosa (Figure 5.3a) and/or an uneven surface with a thin white coating (Figure 5.3b) or a reddish color change (Figure 5.3c). The presence of these features in a suspected lesion indicates the possible presence of superficial ESCC.
5.2.2 Lugol Chromoendoscopy
Iodine solution (Lugol solution) stains nonneoplastic esophageal squamous epithelium dark brown (Figure 5.4a). In contrast, neoplastic lesions do not stain (Figure 5.4b) [3]. Thus, Lugol chromoendoscopy is a useful method for detecting and identifying the lateral extension of ESCC. However, it causes unpleasant side effects including chest pain and discomfort in those who undergo endoscopic examination, and occasionally causes allergic reactions including flushing, asthma, and iodine shock. Sodium thiosulfate solution is useful in reducing these adverse symptoms. Intravenous administration of steroids before the examination is sometimes effective in preventing allergic reactions.
After staining with Lugol solution , superficial ESCC shows a pink color change (Figure 5.4c). [4]) reported that when used as a diagnostic index for high-grade intraepithelial squamous neoplasia and SCC, the pink color sign has sensitivity and specificity of 91.9% and 94.0%, respectively. [5]) also reported that its sensitivity and specificity for the diagnosis of high-grade intraepithelial neoplasia or invasive cancer were 88% and 95%, respectively.
In some cases, multiple Lugol-voiding lesions (multiple LVLs) could be detected in the entire esophagus (Fig. 5.5) [6, 7]. This phenomenon was explained by the “field carcinogenesis” theory [8], in which multiple neoplastic lesions develop not only in the esophagus but also in the head and neck region and lung, and so on. The patients with multiple LVLs in the background esophageal mucosa are at risk of multiple cancers in the upper aerodigestive tract. Abstention from drinking decreases the risk of multiple developments of ESCC after endoscopic resection for superficial ESCC [9].
5.2.3 Equipment-Based Image-Enhanced Endoscopy (IEE)
Equipment-based IEE can accurately diagnose superficial ESCC.
Among the equipment-based IEE technologies, narrow-band imaging (NBI) [10, 11] can provide a highly accurate diagnosis of superficial ESCC. The NBI system uses two narrow-band wavelengths of 415 nm and 540 nm, corresponding to the peaks of absorption of hemoglobin. Therefore, thin blood vessels such as capillaries in the epithelium or mucosal layer can be seen more distinctly by NBI than by conventional WLI. Under NBI observation, most of the area of a superficial ESCC is seen as brownish (Figure 5.6a, b) [12, 13]. In addition, the morphological changes of the intrapapillary capillary loop (IPCL) have been recognized as a useful parameter for ESCC diagnosis [14]. With magnification, irregularities in the IPCL are also more clearly identified by NBI than by conventional WLI (Figure 5.6c, d) [12, 13].
(a) Slight reddish color changed is identified but its margin is unclear. (b) well-demarcated brownish area is clearly identified. (c) Magnifying white light images show irregular microvascular pattern. (d) Narrow-band image enhanced the irregular microvascular pattern compared to the conventional white light image
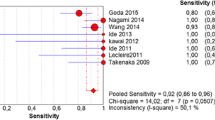
Using the simple criteria of “brownish area” and “irregular microvascular pattern” as diagnostic findings of superficial ESCC, we [15] reported in the prospective multicenter randomized controlled trial that NBI detected more frequently superficial ESCC than did WLI (97% vs. 55%, P < 0.001). In addition, the sensitivity and accuracy of NBI for the diagnosis of superficial ESCC was 97.2% and 88.9%, respectively. Even small lesions (< 10 mm) were more effectively detected by NBI with magnification than by WLI (94% vs. 39%, P = 0.03).
[16]) also reported in their retrospective study that the specificity of NBI for diagnosis of superficial ESCC was significantly superior to that of conventional WLI (95.4% vs. 84.7%, P < 0.001), while the sensitivity of NBI and Lugol chromoendoscopy was equivalent (90.9% vs. 100%, not significant). Furthermore, most of the Lugol-unstained lesions overlooked by NBI were low-grade intraepithelial neoplasia or lesions with atypical findings. This means that Lugol chromoendoscopy detects the lesions unnecessary to treat while NBI detects those indicated for endoscopic treatment. These results indicate that NBI is a useful and less invasive screening method than Lugol chromoendoscopy for identifying superficial ESCC.
In contrast, the false-positive rate of NBI without magnification is high. Therefore, NBI is recommended for use with magnification to provide both higher sensitivity and higher specificity.
BLI (Fujifilm, Tokyo, Japan) is also one of the methods of equipment-based IEE. BLI uses two different lasers as light sources. Of note, one short wavelength laser is used to apply a blue light to the tissue, highlighting the mucosal vascular pattern morphology. The second laser produces high-contrast white light images. Diao et al. reported magnifying BLI has a diagnostic profile similar to that of magnifying NBI [17].
5.3 Estimation of the Depth of Invasion of Superficial ESCC
Estimation of the depth of tumor invasion is important to decide the appropriate treatment because the depth of invasion is closely associated with metastasis to lymph nodes [18]. The frequency of metastasis to the lymph nodes in mucosal ESCC is 3% [18]. The risk increases to 12% for cancer invading the muscularis mucosae, and increases markedly to 26%–46% in those that invade the submucosa [18].
For mucosal ESCC, minimally invasive treatment such as endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD) is indicated, because of the low risk of metastasis. Superficial ESCC invading the muscularis mucosae is usually indicated for surgical resection because of the risk of lymph node metastasis, but may still be treated by ESD, especially in comorbid patients. Superficial ESCC with submucosal invasion necessitates surgical resection and/or chemoradiotherapy (CRT).
However, accurate diagnosis of the depth of tumor invasion has been difficult. Minashi et al. reported a new treatment strategy of diagnostic endoscopic resection and selective chemoradiotherapy [19]. In this strategy, based on the pathological findings of endoscopic resection, patients received the following: (1) no additional treatment for patients with mucosal ESCC with a negative resection margin and no lymphovascular invasion, (2) prophylactic CRT with 41.4 Gy delivered to locoregional lymph nodes for patients with submucosal ESCC with a negative resection margin or mucosal ESCC with lymphovascular invasion, or (3) definitive CRT (50.4 Gy) with a boost to the primary site for patients with a positive vertical resection margin. The survival rate of this strategy is compatible with esophagectomy and could be minimally invasive treatment strategy.
5.3.1 Conventional WLI
In conventional WLI , irregularity of the surface is one of the most important features for evaluation of the depth of invasion. Apparent nodules or apparent depressions indicate tumor invasion beneath the mucosal layer. The so-called “tatami-no-me sign ” is also a useful indicator of the depth of invasion (Fig. 5.7). Tatami is a traditional Japanese style flooring. If the tatami-no-me sign is not seen in the cancerous lesion, the neoplasia may invade the deep layers of the lamina propria mucosae. If the tatami-no-me sign is seen, the lesion has not invaded the deep layers of the lamina propria mucosae.
5.3.2 Lugol Chromoendoscopy
Lugol chromoendoscopy sometimes makes the evaluation of invasion of superficial ESCC difficult, because the deep staining reduces the difference in height between the cancerous lesion and the surrounding normal epithelium. Therefore, the evaluation of invasion by Lugol chromoendoscopy should be done with care. In contrast, the tatami-no-me sign is sometimes more easily seen with Lugol chromoendoscopy because the Lugol solution irritates the mucosa.
5.3.3 Equipment-Based IEE
There has been no evidence that equipment-based IEE is useful for evaluation of the depth of invasion. However, as magnifying NBI can evaluate objectively the irregularity of IPCL, it is expected to improve the accuracy of diagnosis of tumor depth [20].
5.3.4 Endoscopic Ultrasound
Endoscopic ultrasound (EUS) is considered to be the best method for estimation of the depth of invasion of superficial ESCC. To evaluate the depth of invasion, the distinct tissue layers of the esophageal wall should be identified, and 20 MHz or 30 MHz miniature probes should be used. To obtain a clear EUS image, a balloon should be attached to the tip of the endoscope to keep de-aerated water in the esophageal lumen and to prevent regurgitation toward the pharynx. An endoscope with a water-jet function is desirable to keep the esophageal lumen wide open and to obtain clear images. Under good conditions, these high-resolution probes provide nine-layered echo structures of the esophageal wall (Figure 5.8a).
(a) EUS image of the normal esophageal wall by 20 MHz mini probe demonstrates 9-layered structures (arrow). The first 5 layers correspond to the echogenic luminal surface (high echo), mucosa (low echo), lamina propria (high echo), muscularis mucosae (low echo), and submucosa (high echo). Next are inner circular (low echo) and outer longitudinal layers (low echo) of muscularis propria. They are separated by a thin hyperchoic layer of the connective tissue (high echo). (b) EUS image demonstrates a low echoic mass located in the submucosal layer
Generally, a tumor can be seen by EUS as a low echoic mass (Figure 5.8b). If the cancerous lesion invades the submucosal layer, EUS shows a low-echo mass in the high-echo layer corresponding to the submucosal layer. In protruding superficial ESCC (Type 0-I) and advanced ESCC, the ultrasound waves are attenuated by the deeper layers and the EUS image becomes poor. In such cases, evaluation of tumor depth can be difficult.
EUS is also a useful method for evaluating paraesophageal lymph node metastasis of ESCC. [21]) compared lymph node staging obtained by EUS and contrast-enhanced computed tomography (CT) in patients with ESCC. In their prospective case series, the overall accuracy of EUS was 64% (sensitivity 68%, specificity 58%, positive predictive value [PPV] 68%), while that of CT was 51% (sensitivity 33%, specificity 75%, PPV 64%). Although EUS diagnosis is more accurate than contrast-enhanced CT, this is not a satisfactory outcome. Lymph node metastasis in the neck or the abdominal field is anatomically difficult to detect by EUS. Thus, a combination of EUS and CT should be performed for evaluation of lymph node staging in patients with ESCC.
5.3.5 Optical Coherence Tomography
Optical coherence tomography (OCT) is a high-resolution across-sectional optical imaging technique in real time and provides micrometer-scale spatial resolutions with millimeter-scale tissue imaging depths by measuring the echo time delays of light back-reflected from the tissue. OCT is similar in principle to ultrasonography but uses light waves rather than acoustical waves. As the axial resolution of OCT is 10 μm, much higher than that of EUS, the resolution of which is greater than 100 μm, OCT images can identify structures on a microscopic scale. [22]) reported in their prospective study that the accuracy for EP/LPM by using OCT was significantly higher than that by using EUS (OCT, 94.6%; HF-EUS, 80.6%; P < 0.05). Interobserver agreement of OCT and EUS was good and moderate, respectively. Then, they concluded that the preoperative staging of superficial ESCC by using OCT was more useful than that by using EUS. However, OCT is still not the standard method for assessment of the depth of invasion of ESCC. The clinical usefulness of OCT should be assessed by multicenter prospective randomized controlled study.
5.4 Endoscopic Diagnosis of Advanced ESCC
Type 1 ESCC is easy to identify by endoscopy. However, the discrimination of type 0-I and type 1 is sometimes difficult because of borderline lesions. In such cases, the tumor volume and esophageal wall hardness should be considered, because the former suggests deeper invasion and the latter indicates invasion of the muscular layer. To discriminate type 2 and type 3 tumors, it is important to identify whether the tumor ridge is well-demarcated or poorly demarcated. Esophageal metastasis from breast cancer sometimes shows scirrhous infiltration resulting in a type 4 appearance. In cases of severe stricture, macroscopic evaluation is difficult because the endoscope cannot pass through the stricture. In such cases, tumor types are classified based only on images of the oral side of the tumor.
5.5 Differential Diagnosis of Squamous Cell Carcinoma and Adenocarcinoma
Adenocarcinoma is the other major histological esophageal cancer. This histological type is closely associated with Barrett’s esophagus in the background esophageal mucosa. As Barrett’s esophagus is not covered by squamous epithelium but columnar epithelium, the surface pattern is relatively easy to identify by endoscopy. However, it should be histologically confirmed to contain gastric fundic glands, gastric cardia, or intestinal-type epithelium containing goblet cells. Clinically, the cancerous lesion combined with Barrett’s esophagus in the background mucosa is relatively easy to diagnose as adenocarcinoma. In contrast, cardiac cancer extends to the esophagus is sometimes difficult to diagnose by endoscopy as squamous cell carcinoma or adenocarcinoma. In such a case, the superficial spread of IIc-like extension, which is frequently observed in the squamous cell carcinoma , could be one of the key endoscopic findings for differential diagnosis.
5.6 Histological Confirmation by Biopsy
Confirmation of histology by biopsy specimen is required to decide the treatment. Biopsy specimens should be carefully taken by biopsy forceps from viable tumor tissue, not necrotic tissue. If other histological types of tumors such as adenocarcinoma or small cell carcinoma are identified by histological examination, the treatment strategy will be changed in some cases.
5.7 Virtual Biopsy
The endocytoscopy system (ECS) enables in vivo observation of cellular nuclei in the gastrointestinal tract at up to 1400-fold magnification (Fig. 5.9) [23,24,25]. This technology has been predicted to provide the possibility of “virtual biopsy,” especially in the esophagus and colon. Inoue et al. reported that ECS could characterize various tissues including nonneoplastic lesions, inflammatory lesions, and neoplastic lesions. [26]) reported in their prospective ex vivo study that ECS images of the esophagus closely corresponded with those of conventional histology. If ECS could be applied in clinical practice, the number of biopsies required and the risks of biopsy including bleeding would be reduced.
References
Kaltenbach T, et al. American Gastroenterological Association (AGA) institute technology assessment on image-enhanced endoscopy. Gastroenterology. 2008;134:327–40.
Japan Esophageal Society. Japanese classification of esophageal cancer the 11th edition: part II and III. Esophagus. 2017;14:37–65.
Mori M, et al. Lugol staining pattern and histology of esophageal lesions. Am J Gastroenterol. 1993;88:701–5.
Shimizu Y, et al. Endoscopic diagnosis of early squamous neoplasia of the esophagus with iodine staining: high-grade intra-epithelial neoplasia turns pink within a few minutes. J Gastroenterol Hepatol. 2008;23:546–50.
Ishihara R, et al. Quantitative analysis of the color change after iodine staining for diagnosing esophageal high-grade intraepithelial neoplasia and invasive cancer. Gastrointest Endosc. 2009;69:213–8.
Muto M, et al. Association of Aldehyde dehydrogenase 2 gene polymorphism with multiple esophageal dysplasia in head and neck cancer patients. Gut. 2000;47:256–61.
Muto M, et al. Association of multiple Lugol-voiding lesions with synchronous and metachronous esophageal squamous cell carcinoma in patients with head and neck cancer. Gastrointest Endosc. 2002;56:517–21.
Slaughter DP, et al. Field cancerization in oral stratified squamous epithelium: clinical implications of multicentric origin. Cancer. 1953;6:963–8.
Katada C, at al. Alcohol consumption and multiple dysplastic lesions increase risk of squamous cell carcinoma in the esophagus, head, and neck. Gastroenterology. 2016;151:860–9.
Gono K, et al. Endoscopic observation of tissue by narrow band illumination. Opt Rev. 2003;10:1–5.
Gono K, et al. Appearance of enhanced tissue feature in narrow-band endoscopic imaging. J Biomed Opt. 2004;9:568–77.
Muto M, et al. Squamous cell carcinoma in situ at oropharyngeal and hypopharyngeal mucosal sites. Cancer. 2004;101:1375–81.
Muto M, et al. Narrow band imaging: a new diagnostic approach to visualize angiogenesis in superficial neoplasia. Clin Gastroenterol Hepatol. 2005;3:S16–20.
Inoue H, et al. Ultra-high magnification endoscopic observation of carcinoma in situ of the oesophagus. Dig Endosc. 1997;9:16–8.
Muto M, et al. Early detection of superficial squamous cell carcinoma in the head and neck region and esophagus by narrow band imaging: a multicenter randomized controlled trial. J Clin Oncol. 2010;28:1566–72.
Takenaka R, et al. Narrow-band imaging provides reliable screening for esophageal malignancy in patients with head and neck cancers. Am J Gastroenterol. 2009;104:2942–8.
Diao W, et al. Diagnostic ability of blue laser imaging combined with magnifying endoscopy for early esophageal cancer. Dig Liver Dis. 2018;50:1035–40.
Kodama M, Kakegawa T. Treatment of superficial cancer of the esophagus: a summary of responses to a questionnaire on superficial cancer of the esophagus. Surgery. 1998;123:432–9.
Minashi K, et al. Efficacy of endoscopic resection and selective Chemoradiotherapy for stage I esophageal squamous cell carcinoma. Gastroenterology. 2019;157:382–90.
Yoshida T, et al. Narrow-band imaging system with magnifying endoscopy for superficial esophageal lesions. Gastrointest Endosc. 2004;59:288–95.
Takizawa K, et al. Lymph node staging in esophageal squamous cell carcinoma: a comparative study of endoscopic ultrasonography versus computed tomography. J Gastro Hepatol. 2009;24:1687–91.
Hatta W, et al. A prospective comparative study of optical coherence tomography and EUS for tumor staging of superficial esophageal squamous cell carcinoma. Gastrointest Endosc. 2011;76:548–55.
Inoue H, et al. In vivo observation of living cancer cells in the esophagus, stomach, and colon using catheter-type con- tact endoscope, ‘Endocytoscopy system’. Gastrointest Endosc Clin N Am. 2004;14:589–94.
Inoue H, et al. Endoscopic in vivo evaluation of tissue atypia in the esophagus using a newly designed integrated endocytoscope: a pilot trial. Endoscopy. 2006;38:891–5.
Kumagai Y, et al. Endocytoscopic observation of esophageal squamous cell carcinoma. Dig Endosc. 2010;22:10–6.
Fujishiro M, et al. Potential and present limitation of endocytoscopy in the diagnosis of esophageal squamous-cell carcinoma: a multicenter ex vivo pilot study. Gastrointest Endosc. 2007;66:551–5.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Muto, M. (2020). Endoscopic Diagnosis of Squamous Cell Carcinoma of the Esophagus. In: Ando, N. (eds) Esophageal Squamous Cell Carcinoma. Springer, Singapore. https://doi.org/10.1007/978-981-15-4190-2_5
Download citation
DOI: https://doi.org/10.1007/978-981-15-4190-2_5
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-4189-6
Online ISBN: 978-981-15-4190-2
eBook Packages: MedicineMedicine (R0)