Abstract
The Gastric cancer (GC) is the third deadliest malignant disease worldwide. The most common conventional therapies include the use of anticancer drugs; however, their use is ineffective and is limited due to the poor solubility of the drug and its ability to damage the immune system, since anticancer drugs have a small therapeutic drug, overdosing can lead to the toxicity in the systemic organs such as lung, liver and kidneys. Nanotechnology, which has been developed about a decade ago is considered to be a more advantageous therapy compared to the conventional methods for the therapy of cancers like GC. Varied type of nanoparticles that are multifunctional are now used to enhance the solubility and effectiveness of the drug for the treatment, prevention and diagnosis with the annual clinical trials. Moreover, they are biocompatible and less toxic to the normal healthy cells. The organic and inorganic nanoparticles that are used in the cancer diagnosis and drug delivery system include lipid, protein, metal and polymer-based materials. This chapter gives an overview on the types of nanoparticle used in the research for the GC therapy. Additionally, we have briefly described the combinational approaches, including gene therapy and immunotherapy, along with nanoparticles that includes antibody mediated, enzyme and ligand mediated strategies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
13.1 Introduction
Gastric cancer (GC) is the fifth most common diagnosed malignant disease after colorectal cancer and the third most common cause for the cancer-related deaths globally with the annual death record of 783,000 and an estimated survival rate of 31% in the US, according to the analysis of GLOBOCAN in 2018 (Rawla and Barsouk 2019). The occurrence of the disease is due to risk factors including diet, urban life style, chemical exposure (Fortunato and Rushton 2015), genetically inherited mutations, GERD (Ye et al. 2001) and Helicobacter pylori infections (Ahmed 2005). The disease is highly symptomatic in its advanced stage and recurrent as a local or distant metastatic disease, especially after resection of gastric tumors that have rapid spree of disease in their early stages. Even though there are endless efforts made in the discovery and development of novel diagnostic and therapeutic tools to bring better results in the survival rates of these cancer patients, the prognosis rate is very low; thus, it requires more advanced therapies. The tremendous development in therapies include chemo- and radiation therapies, which are highly advantageous; however, there are various side effects and are less effective at the site of the tumor. Moreover, unlike other systemic tumors, GC is a localized tumor and possesses loco-regional metastasis and is generally associated with negative prognostic factors (Imano et al. 2012; Ishigami et al. 2009, 2010). Thus, the cancer therapies are higher risk for healthy tissue and are partial in terms of full recovery. In recent years nanotechnology has been highly researched since its exciting advances has got potential advantageous in the field of science including anticancer therapies, drug delivery mechanisms and imaging.
The nanotechnology is a multidisciplinary research determination that includes nanomedicine or nanoparticles that have unique physical and chemical properties, which are highly beneficial for the early and loco-regional diagnosis and therapy. Moreover, the traditional use of nanomedicine minimizes the toxicity via targeting therapies at the tumor site as well improving the pharmacokinetics. Researchers have already designed a multifunctional theragnostic nanoparticles that gained intensive consideration since it has an effective dual function—it can be used for both diagnosis and therapy (Chen et al. 2014; Muthu et al. 2014; Wang et al. 2013). In this chapter we highlight the emerging research advances and applications of nanoparticles for biomedical imaging, diagnosis and therapy.
13.2 Nanoparticles in Biomedical Imaging for GC Diagnosis and Therapy
The traditional imaging techniques used for diagnosis of various cancers like GC includes computed tomography (CT), positron emission computed tomography (PET) and magnetic resonance imaging (MRI) etc., which come with undesirable side effects and rapid clearance of the tracer used (Li et al. 2011, 2013; Mirkin et al. 2015). The current, advanced research technologies are developing a diverse set of nanoparticles and clearly describing their importance in molecular imaging. To enhance the imaging efficacy, the use of nanoparticles as contrast agents could be a promising strategy. The theragnosis or theragnostics, that are loaded with numerous components, simultaneously achieves disease detection as well therapy (Chen et al. 2014; Muthu et al. 2014; Wang et al. 2013). The molecular imaging is the process of developing molecular probes to view the characterization and functionalization at their molecular level without disturbing them. Furthermore, the multi component nanoparticles that have been developed have improved resolution to overcome the limitations like single imaging. It is also advantageous for better penetration into tissue and temporal resolution time (Key and Leary 2014). There are many nanoparticles, including organic and inorganic nanoparticles for cancer therapeutics and imaging; however, the nanoparticles with much specificity for the tumor cells and maximum circulation half life time are considered to be more beneficial. The nanoparticles are developed as such to show better affinity towards the over expressed receptor proteins in cancer tissues.
13.3 Inorganic Nanoparticles
The inorganic nanoparticles have the physicochemical properties similar to the inorganic components like metals.
13.3.1 Gold Nanoparticles
The nanoparticles that are mostly used for imaging are inorganic nanoparticles, which are widely used as versatile tools with unique optical properties. For instance, gold (Au) nanoparticles have potential biocompatibility, unique physical and chemical properties like higher X-ray absorption coefficient and less toxicity. They are synthesized in organic solvents and to make it stable, the stabilizing agents are added to the Au nanoparticles which chemically and physically are absorbed on to their surface. The Au nanoparticles are produced under benign conditions for safety and less toxicity in the application of cancer therapy. For instance, silica capped Au nanoclusters (AuNCs) are conjugated with folic acid-(FA) in order to target folate receptor (FR+) in MGC-803 cell lines and were tested in vivo in nude mice models with gastric tumors; the results of this investigation showed highly efficient florescent imaging in CT scans (Zhou et al. 2013). Similarly, FA conjugated with another nanoprobe, AuNCs, was designed by Zhou et al. (2013). The designed nanoprobe, AuNCs@SiO2-FA, was effectively targeted against GC cells that showed FR expression. Based on the in vitro studies, they suggested that FA nanoprobe is strongly attracted to FR+ than FR− cells. The designed nanoprobe was created with enhanced emitting fluorescence properties. Thus, this could lead to its potential application in targeting cancer cells and imaging in vivo in the future. Au nanorods coated with indocyanine green-loaded mesoporous silica (ICG-loaded Au@SiO2) were reported by Luo et al. (2011) for efficient imaging in CT and fluorescence imaging. The X-ray CT scanning showed enhanced contrast and sustained the nanomaterial generated NI fluorescence for almost 12 h after intratumoral injections in GC tissue. Thus, this could be a novel dual mode contrasting agent for imaging in GC. Later, Tsujimoto et al. (2014) explored the diagnosis and therapeutic efficacy by using photodynamic therapy (PDT), specifically, using ICG lactosomes in xenograft nude mice which had peritoneal metastasis of GC which enhanced the permeation and retention effect. The report from their PDT images revealed existence of the peritoneal tumor over the abdominal wall in xenograft mice. Additionally, they also observed reduction in the size and weight of the tumor with improved survival rate. Thus, this could be a potential novel device used for the diagnosis and therapy of peritoneal dissemination in GC. Ferumoxtran-10 was used earlier to enhance MRI and to diagnose GC lymph node metastasis; however, its use was fatal with adverse side effects including hypersensitivity (Tatsumi et al. 2006). Recently, Chang et al. (2019) developed monodisperse nanoparticles such that they have grown the silver (Ag) shell on the surface of the Au nanobipyramid core, that is of high stability and uniformity. Additionally, it also possesses surface enhanced Raman scattering (SERS) activity. It was later altered with 4-mercaptobenzoic acid (MBA), a Raman reporter molecule, and conjugated with FA and reduced bovine serum albumin (rBSA) to finally develop nanoprobe, AU-NBP@Ag-NR-rBSA-FA, in order to spot the live MGC-803 and A-549 cancer cells in Petri dishes. The results suggested that with good stability under optimal condition, SERS activity could detect live cancer cells through SERS mapping. Thus, this novel core shell with high stability, bearing ultrasensitive SERS and with Raman imaging is both advantageous and efficient for targeting cancer cells and can be used in clinical and theragnostic applications. The Au nanoparticles are further made more specific to the target site by conjugating them with various targeted ligands including peptides, antibodies and proteins for a more efficient diagnosis, drug delivery and therapy. For instance, Liang et al. (2015) conjugated CD44v6 mAb of CD44 + gastric cancer stem cells (CD44 + GCSCs) as a targeting ligand with Au nanostars-PEGylated nanoprobe. Later, they evaluated the cytotoxicity, endocytosis and cellular affinity and the results suggested that they have better biocompatibility, excellent targeting efficiency and photothermal ablation ability. Additionally, this procedure is also an ideal novel strategy to overcome the resistance in PDT and moreover, the results show better prognosis and also reduced recurrence and metastasis.
13.3.2 Quantum Dots
Quantum dots (QD) are fluorescent semiconductor nanoparticles and are alternatives to organic fluorescent dyes. They have unique electrical and optical properties with broad absorption features and continued emission of fluorescence due to their quantum size affects that increases their longevity. These are highly advantageous in the research field for biological imaging. Peng et al. (2018) found a multiplexed QD probe based spectrum for molecular imaging to evaluate the stromal activation, expression of lysyl oxidase (LOX) and their spatial relationship histologically, which was proposed as stromal marker in GC. LOX is an amine oxidase enzyme that modifies elastin and collagens in ECM and mediates cross linking of fibers. However, its aberrant expression is invasive in various cancers like GC and was found to promote recurrence. Similarly, the expression of caveolin-1 (Cav-1) and light chain 3B (LC3B) are used as biomarkers for the detection of GC in the Epstein—Barr virus associated with GC (EBVaGC) and non EBVaGC using QDs. The loss of Cav-1 expression is a marker for metastasis and early recurrence of disease; whereas, LC3B is a biomarker of autophagy that localizes to the membrane of autophagosome. Later, He et al. (2012) performed QD based immunofluorescence histochemistry to determine the expression of markers LC3B and Cav-1, that are labelled with QDs in about 118 GC patients, and detected EBV encoded small RNA in situ hybridization in EBVaGC. The study concluded that the lower expression of Cav-1 could be a novel predictor for detection of GC progression and LC3B is correlated with lower invasion. Furthermore, to make the use of QD nanoprobes more specific, Ruan et al. (2012) prepared a nanoprobe coupling with HER2-mAb and RNase A (HER2-RDQs) against in-situ and subcutaneous GC mouse models by using MGC803 cell lines. The prepared QDs nanoprobes enhances the imaging and selectively kills GC cells immediately after 3 h and 6 h of post injection in subcutaneous and in-situ GC cells, respectively. They determined that RNase A in the nanoprobe separates and attacks the RNAs in cytoplasm and averts protein synthesis to ultimately induce apoptosis. Thus, this improves the survival time and inhibits growth of GC tissue.
Recently, researchers have been using luciferase-luciferin system to develop bioluminescence imaging of cancer cells; however, the visible bioluminescence released naturally from fireflies is harmful as it is absorbed strongly into haemoglobin and melanin. Thus, longer wavelengths of luminescence is only desirable for bio-molecular imaging. Alternatively, Tsuboi and Jin (2018) have employed bioluminescence resonance energy transfer (BRET), that is coupled with emission and developed from luciferin, to near infrared fluorophores for bioluminescence imaging, using QDs and fluorescent proteins as energy acceptors. The BRET coupled NIR-QDs is further conjugated with the recombinant Renilla luciferase (RLuc) protein on the QDs surface, that is already coated with glutathione through hexa histidine tag (His6) of recombinant protein, which has immunoglobulin binding domain of protein G (GB1). This is further conjugated with anti-EGFR mAb to detect EGFR. EGFR is a glycoprotein and its aberrant activation leads to various cancers including breast and GC. The designed nanoprobe is efficient in producing sensitive NIR images of EGFR in live GC cells. In recent decades immunotherapy that includes antigen presenting cells like dendritic cells would be a promising tool in developing immunity against cancer. Li et al. (2015) for the first time developed a fused vaccine by fusing both allogenic dendritic cells and inactive GC cells (MGC803) combined with cytokine induced killing cells. The fused cells were then labelled with CulnS2/ZnS NIR-QDs. They further determined prophylactic and immunotherapeutic efficacy by injecting the vaccine into three different mice which included tumor free, tumor suffering and post-surgery models (Li et al. 2015). The reports from the animal imaging studies suggested the migration of the vaccine through NIR-QDs. Additionally, the fused cells and fused cells along with cytokine induced killing cells targeted the cytotoxic T lymphocytes against the tumor cells that resulted in reduction in tumor size and promoted the prophylactic effect in vivo (Li et al. 2015). Thus, this could be helpful for future research studies to prevent metastasis and strategy for the early stage tumor therapy.
Like the QDs, fluorescent carbon dots in recent decades have been more encouraged for imaging however, they are more advanced than the QDs due to the later having limitations, such as photobleaching and hazardous properties due to the use of heavy metal elements. The carbon dots are with high biocompatibility, low photobleaching and better photoluminescence and are a promising nanoparticle for biomolecular imaging and drug delivery. The carbon dots based polyethylenimine (PEI) complex was developed by Wang et al. (2014a), as a siRNA carrier for targeting antiapoptotic protein survivin. The designed nanoprobe exhibited high quantum yield and biocompatibility. The reported images from confocal fluorescence clearly illustrated the uptake of siRNA-Cdots@PEI complex by the MGC-803 cells. Moreover, the presence of siRNA in the tumor cells that induced apoptosis and promoted cell cycle arrest at G1 phase were also observed in Westernblot analysis and qRT-PCR, suggesting that they have better gene silencing efficiency. Thus, the use of fluorescent carbon dots would be a successor for the QDs to serve as potential tools in the area of drug delivery and imaging.
13.3.3 Superparamagnetic Iron Oxide Nanoparticles
The magnetic nanoparticles have similar chemical and structural properties to QDs and Au nanoparticles; they are both highly biocompatible with magnetic saturation and have large functional surfaces. The superparamagnetic iron oxide nanoparticles (SPIONs) are widely used as contrasting agents in MRI and have large magnetic moments. Liu et al. (2012a), for the first time, used SPIONs coated with SiO2, labelled them with near infrared fluorescence dye and monoclonal antibody/mAb (anti-CD146), and administered them into a xenograft GC model. The imaging results obtained after 30 min of administration were highly efficient. Later, Bao et al. (2011) used BRCAA1 mAb conjugated with fluorescent magnetic nanoparticles in vivo to diagnose the gastric tumor using magnetic resonance and fluorescent imaging. Furthermore, FDA have approved humanized mAb and trastuzumab or herceptin against the extracellular domain of HER-2 conjugated with superparamagnetic nanoparticles, which is used for therapy as well for imaging in GC (Kulhari et al. 2015; Kataoka et al. 2016; Fornaro et al. 2011). Later, HAI-178 mAb was developed by conjugating fluorescent magnetic, QD nanoparticles wrapped by silicon by Wang et al. (2014b) with the help of Dr. Jian et al. in both in vitro and in vivo GC cells. α-subunit of ATP synthase is over expressed in GC cells and tissues. HAI-178 antibody was prepared against the α-subunit of ATP synthase by Dr. Pan et al. (2011). They also suggested that this could be taken as a dual model both for imaging and therapy, even in the early stages of gastric cancer, which showed better biocompatibility with inhibition of GC cell growth within 2 h of post injection. Wu et al. (2012) developed a novel dual modal combining both optical and magnetic resonance bioimaging with carbonate nanoprobe fixed with rare earth ions, including silica coated magnetic nanoparticle Gd2(CO3)3:Tb, of diameter 16 nm dispersed in water via the micro-emulsion method. The modal is advantageous with the delivery of nanoprobe into the gastric cancer cell lines, SGC7901 in a very short period with less toxicity and no adverse effects in the kidney—even if over doses were taken. The magnetic resonance imaging of the nanoprobe displays a clear T (1)-weighted effect that serves as a positive contrast agent with high potentiality. As another step in the cancer research, gene therapy is a challenging but promising therapeutic strategy for cancer therapy; however, this have been limited due to the improper delivery mechanisms. Thus, the molecular imaging that possesses tracking efficiency would be supportive for gene therapy. Chen et al. (2012) constructed a non-viral antibody directed vector called scFv(CD44v6)-PEG-g-PEI-SPION for the diagnosis and gene therapy both in vitro and in vivo. This was designed using a superparamagnetic iron oxide nanoparticle for siRNA delivery; the study also analysed the targeting ability for the cellular uptake and distribution of siRNA at the target site, which was evident in vitro and in vivo MRI imaging. They further determined that siRNA is effectively transferred to the target site and also mediates the silencing of genes in vitro (Chen et al. 2013). Thus, this could be a promising gene vector for cancer gene therapy. Similarly, Luo et al. (2017) also designed the SPIONs for the gene delivery system to deliver a programmed death ligand 1(PD-L1) siRNA to target PD-L1 cells into SGC-7901 cells, encapsulated with FA-PEG-SS-PEI polymer, where T2-weighted contrast was used to enhance the MRI imaging. PD-L1 is a trans-membrane protein where clusters of differentiation 274 (CD274) binds to PD-1 that exists on the surface of T-cells. PD-L1 suppresses the adaptive immune system and inhibits apoptosis in T-regulatory cells. These are highly expressed in tumor tissues resulting in poor prognosis. Moreover, the results suggested are as follows, with efficient MRI tracing imaging and after internalization, blocking of PD-L1 in vitro was exhibited. Additionally, they also determined that polyplex FA-PEG-SS-PEI-SPION/siRNA after internalization showed down regulation of PD-L1 at both the mRNA and protein level and also showed decrease in cytokine secretion levels when co-cultured with T-cells. Thus, this highlights the nanoparticle as an efficient gene nanocarrier and also restores the immune response. Additionally, Wang et al. (2015) designed another SPION, coated with dense silica (dSiO2) and labelled with 800ZW. They conjugated the entire designed nanoparticle 800zw-SPION@dSiO2 with YY146 to target CD146 in a MKN45 xenograft model, as a novel biomarker for detecting GC metastasis. CD146 is a cell surface protein, correlated with the progression of tumor cells that act aberrantly. Moreover, it also acts as unique biomarker for inducing EMT in GC cell progression and metastasis. YY146 is a mAb synthesised as anti-CD146. Furthermore, the NIRF imaging and histology of the GC tumor was evaluated for pharmacokinetics. The non-invasive in vivo monitoring results suggested binding of CD146 marker to be successful. Thus, this could be a novel strategy for image-guided therapeutic intervention in diagnosis and therapy of GC. Multi drug resistance is always a tedious hurdle for the therapy in cancer. miRNA-16 in GC plays a crucial role in altering the resistance developed against drugs like Adriamycin (ADR). Sun et al. (2014) developed a magnetic nanoparticle, coated with iron oxide nitrate, using PEG conjugated with miRNA-16, to enhance the sensitivity in GC cells to ADR. The developed nanoprobe delivery carrier showed better biocompatibility when administered into SGC7901/ADR nude mice. The reports suggested effective delivery of miRNA-16 as evident from imaging modalities including bioluminescence imaging. Additionally, reduction in the tumor size with the enhancement of apoptosis was probably due to the GC cells developing sensitivity against ADR, after the injection of nanoprobe was also observed. Thus, this could be a novel strategy in developing therapeutic application for multi drug resistance GC therapy.
13.4 Organic Nanoparticles
The organic nanoparticles are equally efficient for diagnosis and drug delivery; however, they have gained less attention when compared with inorganic nanoparticles. There are very few organic nanoparticles used in image based therapy; for instance, DPA-TSB/2,5,2′,5′-tetra (4-N, N-diphenylamine styryl) biphenyl is a water dispersible organic nanoparticle, has two photon absorption (TPA) properties that are efficient in producing 3D fluorescent imaging, which could be a promising tool in biological imaging, since it shows no surfactants and easy cytoplasm internalization. Chen et al. (2016) used DPA-TSB nanoparticle in SGC-7901 gastric cancer cell lines to evaluate certain characteristics including intracellular Ca2+, MMP alterations, apoptosis and accumulation of ROS. They determined that the nanoparticle taken in the concentration of >4 μg/ml showed significant results affecting the discussed factors listed above and can be used as an imaging marker at an ideal concentration and for drug delivery.
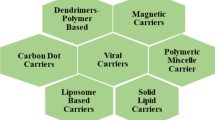
The organic nanoparticles are solid particles and are capable of carrying molecules including drugs that are encapsulated within. The organic nanoparticles that are widely employed for drug delivery as drug vehicles or carriers include dendrimers, liposomes and micelles.
13.4.1 Dendrimers
The dendrimers are regularly branched synthetic polymers. The architecture is designed in layers that includes internal region that encloses a single compound, central core and terminal groups, that develop into a globular conformation. Polyamidoamine (PAMAM) was the first oral drug delivery hyper branched polymer-based dendrimer to be synthesized and commercialized. They can easily cross the intestinal epithelial barriers and pass through the paracellular pathway. In order to determine the efficiency of PAMAM, which is orally administered for its stability and transport through the gastrointestinal tract, Goldberg et al. (2011) conjugated 7-ethyl-10 hydroxy-camptothecin, SN-38, which is a topoisomerase-1 poison against CRC, GC and hepatic metastasis cell line to G3.5 PAMAM dendrimer. This is further ester-linked with glycine and βalanine. However, the G3.5-Gly-SN38 was found to be more effective with less stability in vitro; specifically, it showed the release of the drug within 48, 24 and 6 h into the liver, intestine and stomach, respectively, with an IC50 of 0.60. Additionally, the reports suggested that drug SN38 conjugated with PAMAM had a better and enhanced transepithelial transport than free SN38. Geraldo et al. (2011) developed a functionalized PAMAM dendrimer by combining it with FA coating it with 3-mercaptopropionic acid (MPA) and CdSe QDs cap. The Fourier transform infrared spectroscopy (FTIR) and high-resolution electron microscopy analysis showed the supramolecular complex had efficient transfer of biomarker to the selective GC cells. Later Nie et al. (2016) combined PAMAM dendrimer with QDs to act as a carrier for doxorubicin drug that attached with PEG and assembled with micelles to form vesicles. The entire vesicle was made with small conjugates and made to be pH sensitive under redox conditions. The reports suggested rapid drug release with enhanced cytotoxicity in MGC803 cells in vitro and in vivo; the vesicles showed better antitumor activity and systemic toxicity and no toxicity effects to healthy cells. In another work by Barzegar Behrooz et al. (2017) for cancer therapy, the study designed the PMAM dendrimer-PEG complex conjugated with AS1411 aptamer to deliver 5-FU and was observed with FTIR and atomic force microscopy (AFM). Their results suggested that the designed nanoparticle had more stability and accumulation of 5-FU in MKN45 GC cells. METase is L-methionine diamino-γ-mercaptomethane lyase enzyme destroys methionine (MET), where MET is an amino acid, essential for the self-growth of cancer cells. Recently, rMETase has been widely encouraged as a chemotherapeutic agent in GC therapy. Li et al. (2018) developed a synthetic nanoparticle G5-PAMAM-Au composed with hyaluronic acid, that acts as a CD44 receptor, a marker of CSC for carrying rMETase into xenograft nude mice. Increase in METase expression was determined with the inhibition of proliferation rate, increase in c-caspase 3 expression, Cyc C, Ros levels and inhibition of CD44 GC progression after administration into the mice, moreover, the nanoparticle designed was with better aqueous solubility and biocompatibility. The dendrosomes are another type of spherical and biodegradable nanomaterial used in anticancer therapy. Farnesiferol C is a natural anticancer drug; however, the use of this phytochemical is limited due to the lack of bioavailability. Aas et al. (2015), to improve the bioavailability of this phytochemical, combined farnesiferol C with dendrosome (DFC) against AGS GC cell lines. Their RT-PCR and MTT assay results suggested enhanced anti-proliferative and apoptotic activity with the increase in Bax/Bcl-2 ratio. The nanodrug developed was very significant in inhibiting the proliferation of GC cell in terms of dosage and in a time-dependent manner, when compared with the farnesiferol alone. The gene therapy was made much more successful with the use of gene carriers. PAMAM was also used in gene therapy as a carrier of miR-34a along with phenylboronic acid (PBA) and PEG-α-maleimide-ω-N-hydroxy succinimide. The resulted PPP conjugated with miR-34a, a tumor suppressor protein, was injected into the xenograft GC model to protect the gene from degradation by nucleases. The FACs analysis and confocal laser scanning microscopy revealed uptake of miR-34a by the GC cells through endocytosis. It was also suggested that the miR-34a showed an anti-proliferative effect via promoting apoptosis. On the other hand, metastasis was also regulated by downregulating Notch signalling pathway. Thus, these nanoparticles can be utilized as a novel strategy in the clinical field of cancer therapy through the delivery of genes, drugs or antibodies (Song et al. 2019). Thus, dendrimers are considered as an important tool for the therapy of cancer, since they are more functional when conjugated with ligands that have the ability to cross the barriers and reach the target site causing no effect to the healthy cells.
13.4.2 Liposomes
Liposomes are natural or synthetic phospholipids with an internal aqueous core and external lipid bilayer, surrounding it just like a biological membrane. They are amphiphilic in nature which enables them to carry both a hydrophilic drug, that is enclosed within the aqueous phase, and a hydrophobic drug that are absorbed into their outer membrane. Moreover, due to the cationic nature, they can easily attract and bind electrostatically with the anionic nucleic acids; additionally, they have vigorous diffusion, circulation and penetration properties. Previously, the liposome was used to target the gastric bacteria, Helicobacter pylori, which causes peptic ulcers, chronic gastritis and GC. Thamphiwatana et al. (2013) designed a robust chitosan modified with Au nanoparticle to stabilize liposome and use it as a carrier of antimicrobial drug doxycycline that rapidly triggers the bacteria at gastric pH. The gold stabilizer linked to the lysosome detaches from it at a neutral pH, and this then freely attaches to the bacteria and releases the drug. The results suggested that effective delivery of the drug, that remains inactive in the lumen of stomach later, binds to the bacteria at the mucus layer. This could be an efficient therapeutic strategy for the delivery of antimicrobial drugs for the treatment of gastric infections, which are one of the causes of GC. This is similar to the docetaxel drug which is used for chemohyperthermia therapy in GC. Yoshida et al. (2012) have developed a docetaxel drug encapsulated into magnetoliposome and injected it in the hind limb of balb mice, which had human MKN45 GC cells maintained at 43° C. The tumor progression rate gradually decreased after injection, when compared with the injection of doxetaxel drug alone, and showed an increase in the concentration of the tumor necrosis factor α. In the clinical field of gene therapy, liposome use was advantageous in the delivery of the gene to the target site in GC. For instance, Xin et al. (2015) developed a poly(D, L-lactide-co-glycolide acid) PLGA with PEGylated liposome that increases the capacity of drug loading and control drug release properties. This so developed nanoparticle was conjugated with ScFV, a single chain variable fragment that enhances the drug targeting efficiency in effective delivering. Furthermore, the stealth PLGA liposome CAGE scFv was encapsulated with rMETase and injected into a murine model to deliver it at the site of GC cells. They showed that the therapeutic efficacy increased in in vitro and in vivo with delivery of drug into SGC-7901 cells and also observed low toxicity in healthy cells. The cationic liposome nucleic acid (CL-NA) was used by Wonder et al. (2018) to determine the transfection efficiency of the exogenous nucleic acid-DNA or RNA in vivo in order to validate their early in vitro results. For this, they have stabilized the nanoparticle CL-NA by PEGylating it and injecting it into the human peritoneal metastatic GC mouse model. Biodistribution of DNA was assessed through confocal and whole organ imaging and showed positive results. Additionally, the accumulation of the nanoparticle by the healthy tissue was observed in low levels. Thus, this strategy can be employed for the delivery of peptides, including siRNA and proteins through peptide target nanoparticle therapy. Liposomes were also used to overcome the limitations of PDT in GC treatment. The PDT involves the wide use of Al (III) phthalocyanine chloride tetra sulfonic acid (AlPcS4) due to its low photobleaching, high quantum yields and easy penetration. However, in GC tissues, its penetration is limited due to its attraction towards serum albumin. In this regard, Xin et al. (2018) tested the use of nanoparticles including Au, liposome and nano micelles and its penetrating efficacy of AlPcS4. This report showed that the Au nanorods used for the delivery of AlPcS4 enhanced the anti-proliferative nature of the drug, along with the PDT effect and singlet O2 generation. Furthermore, the liposome used induced the inhibition of GC cell and enhanced the efficacy by blocking the serum albumin whereas, the micellar nanoparticle developed a PDT effect with limited cytotoxicity. Currently, the drug delivery is now targeting the delivery of antibodies for the therapy of cancer. Yang et al. (2018a) for the first made use of gastric cancer initiating cells (CICs) to initiate GC and used CD44+ cells as a marker. Later siRNA loaded cationic liposomal nanoparticle was used for the delivery of siRNA to a special AT rich sequence and binding of protein 1 (SATB1), that promotes cancer metastasis, invasion and progression in various cancer like GC. They finally constructed SATB1 siRNA entrapped inside a cationic liposome and conjugated it with CD44 antibodies and triggered it against gastric CICs. The siRNA delivery to the CICs site was reported with the suppression of SATB1. Thus, this could be taken as a novel strategy for the down-regulating the expression or even knocking down tumor promoting genes.
13.4.3 Micelles
Like liposomes, micelles are amphiphilic polymers with a central hydrophilic shell and external hydrophobic core. They are extensively used as drug vehicles in the therapy of various cancers including GC. Paclitaxel is a chemodrug used for GC therapy; however, due to the failure in the first line therapy, when used for advanced stage of cancer, new formulation of paclitaxel, NK105, was taken with a recommended dose of 150 mg, per phase I. This is further encapsulated in the polymeric micelles nanoparticle and injected into GC patients and evaluated in Phase II trials. The overall response rate (25%), progression free survival (3.0 months), overall survival (14.4) were determined, that suggest for better efficacy of NK105 which warrants for future evaluation of phase III trial (Kato et al. 2012). Harada et al. (2012) developed a polymeric micelle encapsulated with docetaxel. They assessed NC-6301, PEG-poly aspartate encapsulated with docetaxel, linked via ester bonds with the native form of docetaxel, and injected this into the xenograft mice with human breast cancer and the orthotopic mice model with human scirrhous GC. They observed that the tolerated dose in mice of breast cancer was 50 mg/kg and was 10 mg/kg with the native drug. Moreover, mice with GC showed reduction in the size of metastatic lymph node. In another work from Wang et al. (2014c), they designed a pluronic-poly[α-(4-aminobutyl)-1-glycolic acid] (PAGA) micelle to load 5-FU through a self-assembly method against human GC cells. The MTT assay results suggested inhibition in the growth of tumor cells. The pluronic PAGA used for the delivery of 5-FU was highly effective with tunable drug release and could potentially be used as a drug delivery system in the anticancer therapy. Similarly, Vijayaraj Kumar and Venkata Subrahmanya Lokesh (2014) also designed amphiphilic PEGylated micelles to encapsulate and deliver rapamycin, against CRL 1739 in human GC and CRL 1658 NIH-3 T3 in mouse embryonic fibroblast cells. The results suggest enhanced antiproliferative activity in the GC cell. Later, NC-6300 that includes incorporation of epirubicin in micelle was designed by Yamamoto et al. (2015) was used to target against tissue factor (TF) cells. The tissue factor (TF) is the initiator of coagulation, which plays a key role in cancer progression and metastasis, thus, a marker for GC. They have developed mAb against TF and conjugated it with NC-6300. The reports indicated enhanced antitumor effect of the drug, when administered as anti-TF-NC-6300 than in the vital NC-6300 form. Micelles also serves as a nano-vehicle for the delivery of combinatorial drugs to overcome the obstacle of multidrug resistance. β-casein micelles are administered orally by Bar-Zeev et al. (2016) to deliver a combination of chemodrugs including paclitaxel and tariquidar, a P-glycoprotein inhibitor. The results assessed from the spectrophotometry revealed a high loading capacity of nanoparticle used; zeta potential analysis showed the solubility of the drug and the enhanced affinity of the drug via spectrofluorometry. MDR in GC was also controlled by the downregulation of P-gp expression. They also developed another β-casein nano-vehicle for the delivery of SN-38 and elacridar in order to treat multidrug resistance GC cells, that overexpresses breast cancer resistance protein (BCRP). The multi drug resistance reversal was observed with cytotoxicity developed in BCRP in GC cells. Thus, this can be used as a nano-vehicle for the delivery of combinational drugs to overcome the obstacle of resistance (Bar-Zeev et al. 2018). Thus, micelles are found to be more effective nano-vehicles; moreover, their conjugation with ligands could be a novel strategy for the delivery of drug.
13.5 Nanoparticles for Drug Delivery
The drug delivery system includes the delivery of chemodrugs, including 5-FU, docetaxel and cisplatin, to the target site. However, release of higher doses of drug at the site of healthy cells is a major obstacle, as it develops adverse effect, including high toxicity developed in systemic organs. Thus, improvements in the drug delivery system, that specifically limits the delivery only at the tumor site necessitates for a vehicle or a carrier. As discussed earlier, nanoparticles are used as nano-vehicles to carry the chemodrug more efficiently by conjugating them with the markers and mAb to potentiate the transfer of drug. Table 13.1 includes some of the nano-vehicles and chemodrugs worked on so far for the inhibition of GC cells.
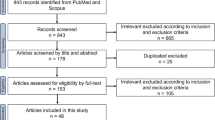
13.6 The Preclinical and Clinical Trials of Nanoparticles
The biocompatible nano-vehicles that have been employed widely in clinical trials are polymer, lipid and protein based. The advances developed in the field of nanotechnology clinical trials that occur annually occur to evaluate their therapeutic efficiency, and their pharmacokinetics and pharmacodynamics, for the safety of the drug use. Below are the few nanodrugs used for the GC therapy as illustrated in Table 13.2. Furthermore, research scientists should collaborate with industries in order to upscale the trials and bring out the promising drug products to the clinic.
13.7 Conclusion and Future Perspective
The tremendous potentiality of the nanotechnology, that includes use of organic and inorganic nanoparticles, open doors to new applications and development for the therapy of dreadful diseases like cancers. GC is currently a serious, malignant disease with a high mortality rate. Therefore, development of nanoparticles for the diagnosis and therapy of GC is critical. The use of inorganic nanoparticles for the tumour imaging is a potential approach. However, the use of organic particles for imaging is still challenging due to the difficulties in tracking them. A well elucidation of the molecular mechanism involved in cancer progression supports the identification of diagnostic markers and therapeutic targets that are essential for the cancer therapy. Thus, nanotechnology could be a potential novel research technology in identifying these biological markers and targets for cancer therapy.
The development of nanoparticles with multifunctional system that includes imaging and therapy requires safe delivery of the synthesized nanoparticles. Thus, researches are now evaluating a better administration route for the safe delivery of these drugs for the most effective results. Moreover, the current researcher envisions, that within a decade or so, with the advancement in novel formulations, applications and evaluation of clinical trials could use nanotechnology routinely for clinical therapies to diagnose the cancer in its early stages. However, the use of nanoparticles made from carbon, copper, supermagnetic and platinum, which are highly toxic and easily accumulate in liver and spleen, may not be possible. Therefore, polymer-based drug carriers that are biodegradable and have little to no side effects need to be considered. Additionally, the need for research centres, like Nanotechnology characterization laboratory, are required for testing the toxicity of nanodrugs. Advances in the nanoformulation is achieved only by the collaborative work of oncologists, pharmacists, medical researchers and gastroenterologists. Their collaboration is necessary for the that would be the synthesis of novel nanoparticles to further transfer the formulation for the clinical therapy of the patient.
Abbreviations
- AFM:
-
Atomic force microscopy
- AlPcS4:
-
Aluminum phthalocyanine chloride tetrasulfonic acid
- AuNC:
-
Gold nanocages
- BCRP:
-
Breast cancer resistant protein
- BRET:
-
Bioluminescence resonance energy transfer
- CIC:
-
Cancer initiating cells
- CL-NA:
-
Cationic liposome nucleic acid
- CSC:
-
Cancer stem cells
- CT:
-
Computed tomography
- DAC:
-
Deoxycytidine
- DFC:
-
Farnesiferol C with dendrosome
- DPA:
-
Diphenyl amine
- EBVaGC:
-
Epstein-barr virus associated GC
- ECM:
-
Extracellular matrix
- FA:
-
Folic acid
- FR:
-
Folate receptor
- FTIR:
-
Fourier transform infrared spectroscopy
- GC:
-
Gastric cancer
- His6:
-
Histidine tag
- ICG:
-
Indocyanine green loaded mesoporous silica
- LOX:
-
Lysyl oxidase
- mAb:
-
Monoclonal antibody
- MBA:
-
Mercapto benzoic acid
- MET:
-
Methionine
- MMP:
-
Matric metalloproteins
- MPA:
-
Mercapto propionic acid
- MRI:
-
Magnetic resonance imaging
- PAGA:
-
Pluronic-poly[α-(4-aminobutyl)-1-glycolic acid]
- PAMAM:
-
Polyamidoamine
- PBA:
-
Phenylboronic acid
- PDT:
-
Photodynamic therapy
- PEG:
-
Polyethylene glycol
- PEI:
-
Polyethylenimine
- PET:
-
Positron emission tomography
- PLGA:
-
Poly(D, L-lactide-co-glycolide acid)
- QD:
-
Quantum dots
- rBSA:
-
Reduced bovine serum albumin
- rLuc:
-
Renilla luciferase
- ROS:
-
Reactive oxygen species
- SATB1:
-
AT rich sequence binding protein 1
- SERS:
-
Surface enhanced raman scatterings
- SPION:
-
Superparamagnetic iron oxide nanoparticle
- TF:
-
Tissue factor
- TPA:
-
Two photon absorption
References
Aas Z, Babaei E, Feizi MAH, Dehghan G (2015) Anti-proliferative and apoptotic effects of dendrosomal farnesiferol C on gastric cancer cells. Asian Pac J Cancer Prev 16:5325–5329
Ahmed N (2005) 23 years of the discovery of helicobacter pylori: is the debate over? BioMed Central
Bao B, Ali S, Kong D, Sarkar SH, Wang Z, Banerjee S, Aboukameel A, Padhye S, Philip PA, Sarkar FH (2011) Anti-tumor activity of a novel compound-CDF is mediated by regulating miR-21, miR-200, and PTEN in pancreatic cancer. PLoS One 6:e17850
Bar-Zeev M, Assaraf YG, Livney YD (2016) β-Casein nanovehicles for oral delivery of chemotherapeutic drug combinations overcoming P-glycoprotein-mediated multidrug resistance in human gastric cancer cells. Oncotarget 7:23322
Bar-Zeev M, Kelmansky D, Assaraf YG, Livney YD (2018) β-Casein micelles for oral delivery of SN-38 and elacridar to overcome BCRP-mediated multidrug resistance in gastric cancer. Eur J Pharm Biopharm 133:240–249
Barzegar Behrooz A, Nabavizadeh F, Adiban J, Shafiee Ardestani M, Vahabpour R, Aghasadeghi MR, Sohanaki H (2017) Smart bomb AS 1411 aptamer-functionalized/PAMAM dendrimer nanocarriers for targeted drug delivery in the treatment of gastric cancer. Clin Exp Pharmacol Physiol 44:41–51
Cai J, Qian K, Zuo X, Yue W, Bian Y, Yang J, Wei J, Zhao W, Qian H, Liu B (2019) PLGA nanoparticle-based docetaxel/LY294002 drug delivery system enhances antitumor activities against gastric cancer. J Biomater Appl 33:1394–1406
Chang J, Zhang A, Huang Z, Chen Y, Zhang Q, Cui D (2019) Monodisperse Au@ Ag core-shell nanoprobes with ultrasensitive SERS-activity for rapid identification and Raman imaging of living cancer cells. Talanta 198:45–54
Chen Y, Wang W, Lian G, Qian C, Wang L, Zeng L, Liao C, Liang B, Huang B, Huang K (2012) Development of an MRI-visible nonviral vector for siRNA delivery targeting gastric cancer. Int J Nanomedicine 7:359
Chen Y, Lian G, Liao C, Wang W, Zeng L, Qian C, Huang K, Shuai X (2013) Characterization of polyethylene glycol-grafted polyethylenimine and superparamagnetic iron oxide nanoparticles (PEG-g-PEI-SPION) as an MRI-visible vector for siRNA delivery in gastric cancer in vitro and in vivo. J Gastroenterol 48:809–821
Chen F, Ehlerding EB, Cai W (2014) Theranostic nanoparticles. J Nucl Med 55:1919–1922
Chen G, Li S-Y, Malik HT, Ma Y-G, Xu H, Sun L-K (2016) Organic two-photon nanoparticles modulate reactive oxygen species, intracellular calcium concentration, and mitochondrial membrane potential during apoptosis of human gastric carcinoma SGC-7901 cells. Biotechnol Lett 38:1269–1276
Dou Z, Xu Y, Sun H, Liu Y (2012) Synthesis of PEGylated fullerene–5-fluorouracil conjugates to enhance the antitumor effect of 5-fluorouracil. Nanoscale 4:4624–4630
Fernandes E, Ferreira D, Peixoto A, Freitas R, Relvas-Santos M, Palmeira C, Martins G, Barros A, Santos LL, Sarmento B (2019) Glycoengineered nanoparticles enhance the delivery of 5-fluoroucil and paclitaxel to gastric cancer cells of high metastatic potential. Int J Pharm 570:118646
Fornaro L, Lucchesi M, Caparello C, Vasile E, Caponi S, Ginocchi L, Masi G, Falcone A (2011) Anti-HER agents in gastric cancer: from bench to bedside. Nat Rev Gastroenterol Hepatol 8:369
Fortunato L, Rushton L (2015) Stomach cancer and occupational exposure to asbestos: a meta-analysis of occupational cohort studies. Br J Cancer 112:1805
Gao Z, Li Z, Yan J, Wang P (2017) Irinotecan and 5-fluorouracil-co-loaded, hyaluronic acid-modified layer-by-layer nanoparticles for targeted gastric carcinoma therapy. Drug Des Devel Ther 11:2595
Geraldo DA, Duran-Lara EF, Aguayo D, Cachau RE, Tapia J, Esparza R, Yacaman MJ, Gonzalez-Nilo FD, Santos LS (2011) Supramolecular complexes of quantum dots and a polyamidoamine (PAMAM)-folate derivative for molecular imaging of cancer cells. Anal Bioanal Chem 400:483–492
Goldberg DS, Vijayalakshmi N, Swaan PW, Ghandehari H (2011) G3. 5 PAMAM dendrimers enhance transepithelial transport of SN38 while minimizing gastrointestinal toxicity. J Control Release 150:318–325
Harada M, Iwata C, Saito H, Ishii K, Hayashi T, Yashiro M, Hirakawa K, Miyazono K, Kato Y, Kano MR (2012) NC-6301, a polymeric micelle rationally optimized for effective release of docetaxel, is potent but is less toxic than native docetaxel in vivo. Int J Nanomedicine 7:2713
He Y, Zhao X, Gao J, Fan L, Yang G, Cho W, Chen H (2012) Quantum dots-based immunofluorescent imaging of stromal fibroblasts caveolin-1 and light chain 3B expression and identification of their clinical significance in human gastric cancer. Int J Mol Sci 13:13764–13780
Hu N, Yin JF, Ji Z, Hong Y, Wu P, Bian B, Song Z, Li R, Liu Q, Wu F (2017) Strengthening gastric cancer therapy by trastuzumab-conjugated nanoparticles with simultaneous encapsulation of anti-MiR-21 and 5-fluorouridine. Cell Physiol Biochem 44:2158–2173
Imano M, Yasuda A, Itoh T, Satou T, Peng Y-F, Kato H, Shinkai M, Tsubaki M, Chiba Y, Yasuda T (2012) Phase II study of single intraperitoneal chemotherapy followed by systemic chemotherapy for gastric cancer with peritoneal metastasis. J Gastrointest Surg 16:2190–2196
Ishigami H, Kitayama J, Kaisaki S, Hidemura A, Kato M, Otani K, Kamei T, Soma D, Miyato H, Yamashita H (2009) Phase II study of weekly intravenous and intraperitoneal paclitaxel combined with S-1 for advanced gastric cancer with peritoneal metastasis. Ann Oncol 21:67–70
Ishigami H, Kitayama J, Kaisaki S, Yamaguchi H, Yamashita H, Emoto S, Nagawa H (2010) Phase I study of biweekly intravenous paclitaxel plus intraperitoneal cisplatin and paclitaxel for gastric cancer with peritoneal metastasis. Oncology 79:269–272
Kataoka H, Mori Y, Shimura T, Nishie H, Natsume M, Mochizuki H, Hirata Y, Sobue S, Mizushima T, Sano H (2016) A phase II prospective study of the trastuzumab combined with 5-weekly S-1 and CDDP therapy for HER2-positive advanced gastric cancer. Cancer Chemother Pharmacol 77:957–962
Kato K, Chin K, Yoshikawa T, Yamaguchi K, Tsuji Y, Esaki T, Sakai K, Kimura M, Hamaguchi T, Shimada Y, Matsumura Y, Ikeda R (2012) Phase II study of NK105, a paclitaxel-incorporating micellar nanoparticle, for previously treated advanced or recurrent gastric cancer. Investig New Drugs 30:1621–1627
Key J, Leary JF (2014) Nanoparticles for multimodal in vivo imaging in nanomedicine. Int J Nanomedicine 9:711
Kulhari H, Pooja D, Rompicharla SV, Sistla R, Adams DJ (2015) Biomedical applications of trastuzumab: as a therapeutic agent and a targeting ligand. Med Res Rev 35:849–876
Li R, Xie L, Zhu Z, Liu Q, Hu Y, Jiang X, Yu L, Qian X, Guo W, Ding Y (2011) Reversion of pH-induced physiological drug resistance: a novel function of copolymeric nanoparticles. PLoS One 6:e24172
Li R, Wu W, Liu Q, Wu P, Xie L, Zhu Z, Yang M, Qian X, Ding Y, Yu L (2013) Intelligently targeted drug delivery and enhanced antitumor effect by gelatinase-responsive nanoparticles. PLoS One 8:e69643
Li C, Liang S, Zhang C, Liu Y, Yang M, Zhang J, Zhi X, Pan F, Cui DJB (2015) Allogenic dendritic cell and tumor cell fused vaccine for targeted imaging and enhanced immunotherapeutic efficacy of gastric cancer. Biomaterials 54:177–187
Li Y-F, Zhang H-T, Xin L (2018) Hyaluronic acid-modified polyamidoamine dendrimer g5-entrapped gold nanoparticles delivering metase gene inhibits gastric tumor growth via targeting cd44+ gastric cancer cells. J Cancer Res Clin Oncol 144:1463–1473
Liang S, Li C, Zhang C, Chen Y, Xu L, Bao C, Wang X (2015) CD44v6 monoclonal antibody-conjugated gold nanostars for targeted photoacoustic imaging and plasmonic photothermal therapy of gastric cancer stem-like cells. Theranostics 5:970
Liu W-F, Ji S-R, Sun J-J, Zhang Y, Liu Z-Y, Liang A-B, Zeng H-Z (2012a) CD146 expression correlates with epithelial-mesenchymal transition markers and a poor prognosis in gastric cancer. Int J Mol Sci 13:6399–6406
Liu P, Wang H, Wang Q, Sun Y, Shen M, Zhu M, Wan Z, Duan Y (2012b) cRGD conjugated mPEG-PLGA-PLL nanoparticles for SGC-7901 gastric cancer cells-targeted delivery of fluorouracil. J Nanosci Nanotechnol 12:4467–4471
Liu D, Li X, Chen C, Li C, Zhou C, Zhang W, Zhao J, Fan J, Cheng K, Chen L (2018) Target-specific delivery of oxaliplatin to HER2-positive gastric cancer cells in vivo using oxaliplatin-au-fe3o4-herceptin nanoparticles. Oncol Lett 15:8079–8087
Luo T, Huang P, Gao G, Shen G, Fu S, Cui D, Zhou C, Ren Q (2011) Mesoporous silica-coated gold nanorods with embedded indocyanine green for dual mode X-ray CT and NIR fluorescence imaging. Opt Express 19:17030–17039
Luo X, Peng X, Hou J, Wu S, Shen J, Wang L (2017) Folic acid-functionalized polyethylenimine superparamagnetic iron oxide nanoparticles as theranostic agents for magnetic resonance imaging and PD-L1 siRNA delivery for gastric cancer. Int J Nanomedicine 12:5331
Mirkin CA, Meade TJ, Petrosko SH, Stegh AH (2015) Nanotechnology-based precision tools for the detection and treatment of cancer. Springer, Cham
Muthu MS, Leong DT, Mei L, Feng S-S (2014) Nanotheranostics-application and further development of nanomedicine strategies for advanced theranostics. Theranostics 4:660
Nie J, Wang Y, Wang W (2016) In vitro and in vivo evaluation of stimuli-responsive vesicle from PEGylated hyperbranched PAMAM-doxorubicin conjugate for gastric cancer therapy. Int J Pharm 509:168–177
Pan J, Sun L-C, Tao Y-F, Zhou Z, Du X-L, Peng L, Feng X, Wang J, Li Y-P, Liu L (2011) ATP synthase ecto-α-subunit: a novel therapeutic target for breast cancer. J Transl Med 9:211
Peng C, Liu J, Yang G, Li Y (2018) Lysyl oxidase activates cancer stromal cells and promotes gastric cancer progression: quantum dot-based identification of biomarkers in cancer stromal cells. Int J Nanomedicine 13:161
Rawla P, Barsouk A (2019) Epidemiology of gastric cancer: global trends, risk factors and prevention. Przeglad Gastroenterologiczny 14:26
Ruan J, Song H, Qian Q, Li C, Wang K, Bao C, Cui D (2012) HER2 monoclonal antibody conjugated RNase-A-associated CdTe quantum dots for targeted imaging and therapy of gastric cancer. Biomaterials 33:7093–7102
Song Z, Liang X, Wang Y, Han H, Yang J, Fang X, Li Q (2019) Phenylboronic acid-functionalized polyamidoamine-mediated miR-34a delivery for the treatment of gastric cancer. Biomater Sci 7:1632–1642
Sun Z, Song X, Li X, Su T, Qi S, Qiao R, Wang F, Huan Y, Yang W, Wang J (2014) In vivo multimodality imaging of miRNA-16 iron nanoparticle reversing drug resistance to chemotherapy in a mouse gastric cancer model. Nanoscale 6:14343–14353
Tatsumi Y, Tanigawa N, Nishimura H, Nomura E, Mabuchi H, Matsuki M, Narabayashi I (2006) Preoperative diagnosis of lymph node metastases in gastric cancer by magnetic resonance imaging with ferumoxtran-10. Gastric Cancer 9:120–128
Thamphiwatana S, Fu V, Zhu J, Lu D, Gao W, Zhang L (2013) Nanoparticle-stabilized liposomes for pH-responsive gastric drug delivery. Langmuir 29:12228–12233
Tsuboi S, Jin T (2018) Recombinant protein (luciferase-IgG binding domain) conjugated quantum dots for BRET-coupled near-infrared imaging of epidermal growth factor receptors. Bioconjug Chem 29:1466–1474
Tsujimoto H, Morimoto Y, Takahata R, Nomura S, Yoshida K, Horiguchi H, Hiraki S, Ono S, Miyazaki H, Saito D (2014) Photodynamic therapy using nanoparticle loaded with indocyanine green for experimental peritoneal dissemination of gastric cancer. Cancer Sci 105:1626–1630
Vijayaraj Kumar P, Venkata Subrahmanya Lokesh B (2014) Designing and in-vitro characterization of micelle forming amphiphilic PEGylated rapamycin nanocarriers for the treatment of gastric cancer. Curr Drug Deliv 11:613–620
Wang L, Wang Y, Li Z (2013) Nanoparticle-based tumor theranostics with molecular imaging. Curr Pharm Biotechnol 14:683–692
Wang Q, Zhang C, Shen G, Liu H, Fu H, Cui D (2014a) Fluorescent carbon dots as an efficient siRNA nanocarrier for its interference therapy in gastric cancer cells. J Nanobiotechnol 12:58
Wang C, Bao C, Liang S, Zhang L, Fu H, Wang Y, Wang K, Li C, Deng M, Liao Q (2014b) HAI-178 antibody-conjugated fluorescent magnetic nanoparticles for targeted imaging and simultaneous therapy of gastric cancer. Nanoscale Res Lett 9:274
Wang Q, Liu P, Sun Y, Wu H, Li X, Duan Y, Zhang Z (2014c) Pluronic-poly [α-(4-aminobutyl)-l-glycolic acid] polymeric micelle-like nanoparticles as carrier for drug delivery. J Nanosci Nanotechnol 14:4843–4850
Wang P, Qu Y, Li C, Yin L, Shen C, Chen W, Yang S, Bian X, Fang D (2015) Bio-functionalized dense-silica nanoparticles for MR/NIRF imaging of CD146 in gastric cancer. Int J Nanomedicine 10:749
Wang X, Zhang H, Bai M, Ning T, Ge S, Deng T, Liu R, Zhang L, Ying G, Ba Y (2018) Exosomes serve as nanoparticles to deliver anti-miR-214 to reverse chemoresistance to cisplatin in gastric cancer. Mol Ther 26:774–783
Wonder E, Simón-Gracia L, Scodeller P, Majzoub RN, Kotamraju VR, Ewert KK, Teesalu T, Safinya CR (2018) Competition of charge-mediated and specific binding by peptide-tagged cationic liposome–DNA nanoparticles in vitro and in vivo. Biomaterials 166:52–63
Wu Y, Xu X, Tang Q, Li Y (2012) A new type of silica-coated Gd(2)(CO(3))(3):Tb nanoparticle as a bifunctional agent for magnetic resonance imaging and fluorescent imaging. Nanotechnology 23:205103
Wu F-l, Li R-T, Yang M, Yue G-F, Wang H-y, Liu Q, Cui F-b, Wu P-y, Ding H, Yu L-X (2015) Gelatinases-stimuli nanoparticles encapsulating 5-fluorouridine and 5-aza-2′-deoxycytidine enhance the sensitivity of gastric cancer cells to chemical therapeutics. Cancer Lett 363:7–16
Xin L, Cao J-Q, Liu C, Zeng F, Cheng H, Hu X-Y, Shao J-H (2015) Evaluation of rMETase-loaded stealth PLGA/liposomes modified with anti-CAGE scFV for treatment of gastric carcinoma. J Biomed Nanotechnol 11:1153–1161
Xin J, Wang S, Wang B, Wang J, Wang J, Zhang L, Xin B, Shen L, Zhang Z, Yao C (2018) AlPcS4-PDT for gastric cancer therapy using gold nanorod, cationic liposome, and Pluronic® F127 nanomicellar drug carriers. Int J Nanomedicine 13:2017
Xu S, Cui F, Huang D, Zhang D, Zhu A, Sun X, Cao Y, Ding S, Wang Y, Gao E (2019) PD-L1 monoclonal antibody-conjugated nanoparticles enhance drug delivery level and chemotherapy efficacy in gastric cancer cells. Int J Nanomedicine 14:17
Yamamoto Y, Hyodo I, Koga Y, Tsumura R, Sato R, Obonai T, Fuchigami H, Furuya F, Yasunaga M, Harada M (2015) Enhanced antitumor effect of anti-tissue factor antibody-conjugated epirubicin-incorporating micelles in xenograft models. Cancer Sci 106:627–634
Yang F, Zheng Z, Zheng L, Qin J, Li H, Xue X, Gao J, Fang G (2018a) siRNA-encapsulated immunoliposomes conjugated with CD44 antibodies target and eliminate gastric cancer-initiating cells. OncoTargets Ther 11:6811
Yang F, Li A, Liu H, Zhang H (2018b) Gastric cancer combination therapy: synthesis of a hyaluronic acid and cisplatin containing lipid prodrug coloaded with sorafenib in a nanoparticulate system to exhibit enhanced anticancer efficacy and reduced toxicity. Drug Des Devel Ther 12:3321
Ye W, Chow W-H, Lagergren J, Yin L, Nyrén O (2001) Risk of adenocarcinomas of the esophagus and gastric cardia in patients with gastroesophageal reflux diseases and after antireflux surgery. Gastroenterology 121:1286–1293
Yoshida M, Sato M, Yamamoto Y, Maehara T, Naohara T, Aono H, Sugishita H, Sato K, Watanabe Y (2012) Tumor local chemohyperthermia using docetaxel-embedded magnetoliposomes: interaction of chemotherapy and hyperthermia. J Gastroenterol Hepatol 27:406–411
Zhou Z, Zhang C, Qian Q, Ma J, Huang P, Pan L, Gao G, Fu H, Fu S, Song H (2013) Folic acid-conjugated silica capped gold nanoclusters for targeted fluorescence/X-ray computed tomography imaging. J Nanobiotechnol 11:17
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Dariya, B., Pavitra, E., Momin, S., Raju, G.S.R. (2020). Nanotechnology Applications in Gastric Cancer. In: Raju, G., Bhaskar, L. (eds) Theranostics Approaches to Gastric and Colon Cancer. Diagnostics and Therapeutic Advances in GI Malignancies. Springer, Singapore. https://doi.org/10.1007/978-981-15-2017-4_13
Download citation
DOI: https://doi.org/10.1007/978-981-15-2017-4_13
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-2016-7
Online ISBN: 978-981-15-2017-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)