Abstract
The epidemic of diabetes mellitus has already become a serious global health threat. In the past three decades, the number of people with diabetes mellitus has quadrupled globally, and diabetes mellitus is known as the ninth major cause of death in the world nowadays. The increasing prevalence of type 2 diabetes mellitus is in coincidence with the augmentation of obesity in most developed countries as well as in developing countries. A sedentary lifestyle is well-known as one of the major reasons for the rising epidemic of type 2 diabetes mellitus besides the other reasons such as adopting energy-dense diets relative to the actual need for energy and population aging. Exercise as a regular physical activity at a medium to vigorous intensity is found to be an efficient influencer that would switch back most of the known type 2 diabetes mellitus factors toward healthier positions. Exercise is proven to have clinical benefits, such as improved insulin sensitivity, reductions in glycosylated hemoglobin (A1C) and increased peak oxygen consumption (VO2peak) which are definitely preventive toward diabetes. Exercise training can favorably affect glycemic parameters, the lipid profile, blood pressure, and high-sensitivity C-reactive protein. Exercise improves blood glucose control in type 2 diabetes, reduces cardiovascular risk factors, and regulates body weight by reducing body fat percentage and enhancing lean mass. In this chapter, the effect of regular exercise on the prevention of diabetes and short-term glucose and energy metabolism will be discussed. In addition, the effect of exercise on most common complications of type 2 diabetes including cardiovascular diseases, dyslipidemia, nephropathy, neuropathy, and retinopathy will be reviewed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Background
Diabetes is classified into four types according to the American Diabetes Association: type 1 diabetes, an autoimmune disease induced after pancreatic β-cell damage by immune system; type 2 diabetes mellitus (T2DM), an state of disruption in insulin signaling “insulin resistance” and simultaneously β-cell exhaustion; gestational diabetes mellitus which occurs usually after second trimester of gestation without previous diabetes symptoms; some rarer types of diabetes due endocrine disease drugs side effects [1, 2]. International Diabetes Federation estimates more than 9% of all adults worldwide now have diabetes mellitus, and this number is growing. Diabetes mellitus is a major risk factor of different disorders including renal failure, peripheral neuropathy, retinopathy, and especially cardiovascular diseases. The level of glycated hemoglobin A1c (HbA1c) seems to be a key predictor of diabetes-associated morbidity and mortality; So that reduction in serum HbA1c by 1% results in 14% lower of myocardial infarctions and more than 20% decrease in diabetes associated death risk [3].
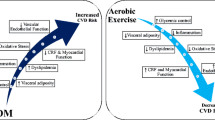
It is well known that metabolic dysfunction in T2DM is accompanied with chronic inflammation [4]. Increase in secretion of inflammatory adipokines including leptin and resistin along with diabetogenic pro-inflammatory cytokines from adipocytes such as tumor necrosis factor-alpha (TNF-𝛼) and interleukin-6 (IL-6) are the fundamental characteristic of T2DM. The interplay between inflammatory mediators and insulin resistance is a key to management diabetes. Strong evidences have demonstrated that intensive lifestyle changes dedicated on increasing physical activity can prevent the occurrence of diabetes more effective than pharmacological interventions [5]. Exercise is proven to induce beneficial changes in glycemic markers such as insulin resistance, HbA1C and fasting insulin which is definitely preventive toward T2DM. Along with these changes, exercise can favorably alter the lipid profile, blood pressure, and inflammatory markers [6]. Reduction in visceral and abdominal fat is found to be the major link between exercise and insulin resistance improvement. The results of aerobic, resistance, and combined exercise on obese men showed a change in cytokine/adipokine level as well as a decrease in insulin resistance [7]. This chapter tends to provide an update on the effect of different exercise programs on type 2 diabetes-related markers, mechanisms of action, and short-term and long-term outcomes.
2 Classification and Diagnosis of Diabetes
Diabetic patients usually fall into one of these two categories; type 1 diabetes (5–10% of total cases) occurs when the immune system arises against pancreas β-cells and insulin production increasingly declines to insufficient level. Type 2 diabetes with 90–95% of all diabetic cases is a chronic condition when body becomes resistant to insulin action and pancreatic β-cells gradually lose the ability to secrete adequate insulin [8]. Type 1 diabetes incidence is much more in youngsters than adults however, it occurs at any age. On the other hand, T2DM has known as a disease for adults with low prevalence among adolescents. Patients predispose to diabetes commonly experience lower level of hyperglycemia so-called prediabetes, an asymptomatic treatable state characterized by one of the following: (1) impaired fasting glucose (100–125 mg/dL), (2) 2-h plasma glucose 140–199 mg/dL, (3) HbA1C 5.7–6.4% mg/dL [5]. Plasma glucose or HbA1c more than that described for prediabetes is classified as diabetes. There is a probability that the diagnosis of diabetes type becomes unclear especially at the onset of the disease in adults [9]. Although prevalent signs such as polyuria and polydipsia are common among type 1 and type 2 diabetes, a decisive distinction is important. Certain diagnostic criteria for type 1 diabetes include the presence of ketoacidosis and using βcell-specific autoantibodies.
Gestational diabetes mellitus is the occurrence of diabetes usually between 24 and 28 weeks of pregnancy in women without previous history of diabetes [8]. Gestational diabetes mellitus diagnosis includes the one-step 75-g oral glucose tolerance test or two-step approach with a 50-g no fasting screen followed by a 100-g oral glucose tolerance test for those who screen positive. Cutoff diagnosis for fasting, 1 and 2 h are plasma glucose equal or higher than 92 mg/dL, 180 mg/dL, and 153 mg/dL, respectively [1].
3 Treatment Goals
Glycemic goals for adults with T2DM are set under 7.5% for HbA1c and less than 130 mg/dL for fasting blood glucose according to American Diabetes Association (ADA) guidelines [10]. The therapeutic strategy should be comprehensive and along with pharmacotherapy comprise series of self-management education and smoke disuse counseling as well as prescribing dietary and exercise regimen [11]. Lifestyle management is described as an essential approach for diabetes care. The combination of physical activity with calorie restriction is proven to not only improve well-being status but also prevent weight gain in the long term and overall morbidity [12]. The American Diabetes Association’s recommendation for prevention or postponement of type 2 diabetes is annual monitoring for patients with prediabetes to diagnose any progression toward diabetes. In addition, contributing to an intensive physically active lifestyle program to reach and maintain minimum 5% weight loss and increase moderate-intensity physical activity to at least 200–300 min/week. There are also recommendations for using new wearable technologies and mobile application to enhance education and or encourage patients to follow recommendations [13]. Furthermore, the assessment of clinical therapies, psychological, physical science, and sociology in elderly adults is necessary as part of treatment considerations [10]. Patient-centered care is critical to achieving optimal medical treatment results and psychological well-being. Medical treatment of diabetes necessitates the patient’s full adherence to the treatment regimen [14]. A major effort suggested to fight against diabetes is through weight loss and health behavior changes [12]. Studies investigating perceived barriers and facilitators of diabetic patients performing the exercise suggest that supports from family members and an overall greater sense of well-being and fitness were the main factors associated with higher exercise adherence.
4 Types of Exercises and Physical Activity
Aerobic exercises are activities engaging larger muscles and mostly rely on energy generated by aerobic metabolism. The aerobic training may have mild to vigorous intensity and usually involve long duration. Running, jogging, cycling, and swimming are a sample of aerobic exercises. Resistance training includes activities aimed to enhance muscular power and endurance by using bodyweight, machines, or elastic bands [15]. Stretching exercises tend to increase flexibility such as yoga, upper and lower body stretch, and calf stretch. Standing on toe, tai chi, and heel to toe walk are among balance exercises that help especially elders prevent falling.
5 Effect of Exercise in the Prevention of Diabetes
ADA recommendations for the prevention of T2DM include physical activity more than 150 min/week and dietary intervention in order to attain 5–7% weight loss within 3–6 months. Similarly, the Diabetes Prevention Program (DPP) has recommended a series of behavioral and lifestyle modifications to achieve and maintain at least 7% of weight loss and 150 min of physical activity per week. The intensity of physical activity should be like brisk walking [16]. The 7% weight reduction is recommended to achieve in the first 6 months of intervention as 0.5–1 kg weight loss per week the exercise modality is permitted to be personalized and is the least assessed change leading to lessen the risk of developing diabetes [16]. Widespread evidence resulted from diverse studies across countries and populations of all ages support the fact that exercise training has an effective role in the prevention of T2DM through promote insulin sensitivity and also changes body mass and composition. In this regard, a follow-up study on adult Swedish men and Chinese men and women with prediabetes showed a reduction in T2DM development through exercise intervention. Another study comparing the effectiveness of exercise and diet modification on T2DM revealed similar preventive results. This preventing effect was observed with the fact that no significant change in the body mass index was detected in either of groups [17]. Epidemiological studies demonstrated that various intensity of exercise throughout the week was associated with a decreased incidence of diabetes at long-term follow-up in both genders of different age groups [18]. Exercise training is well recognized to have an obvious diabetes preventive effect by ameliorating metabolism homeostatic, physical fitness, cardiovascular health in patients with T2DM mellitus and prediabetes. Moreover, to prevent or delay the most prevalent comorbidities after T2DM diagnosed in older adults such as neuropathy, nephropathy,, heart failure, depression, and cognitive impairment, targeted exercise prescriptions of different modalities including aerobic, resistance, or combined exercise programs have been proven to provide significant clinical benefits in all of the mentioned burdens [19]. In a study with a diabetes preventive approach, comparing the effect of 8 weeks of the aerobic exercise with the high-intensity resistance training on body composition and glucose homeostatic of obese sedentary adults without diabetes resulted in no significant difference within groups, except a significant increase in leg lean body mass observed within the high-intensity functional exercise group [20]. A study exploring the effect of leisure-time physical activity on prevention of T2DM who were prediabetic based on impaired glucose tolerance test. Results from 4 years of follow-up indicated that participants who increased physical activity with moderate to high intensity had 63–65% less chance of developing diabetes [21]. In 2015 a systematic review evaluating cost-effectiveness of dietary and physical activity promotion program to prevent diabetes was published. Of 28 reviewed studies, 22 reported the cost-effectiveness of the intervention program, and the cost was even lower for group intervention sessions [2]. Despite the benefits and effectiveness of the lifestyle intervention programs, the absence of such programs in communities and low insurance coverage is a serious challenge [22].
6 Short-Term Effect of Exercise on Diabetes
6.1 Energy and Glucose Metabolism
Physical activity is an energy-consuming action and induces much higher energy expenditure than resting state. A 77 kg man running with 8 km/h speed for half an hour burns an additional 324 kcal to usual energy expenditure. The energy source for muscles may change from glucose to fatty acids during activity based on the intensity of exercise [23]. However, the effect of exercise on energy metabolism is not limited to absolute energy consuming during exercise period. It is well-known that after a bout of exercise, energy expenditure stays elevated hours after activity. A study on 10 young male participant showed that 45 min of high intensity aerobic exercise induce higher energy expenditure for 14 h post exercise. The amount of burnt energy in this period was about 40 percent of total energy consumption during exercise [24]. The post-exercise increase in energy consumption can be stretch out to 22 h by replacing aerobic with high intensity resistance training [25]. Another study on overweight young adults demonstrated that a resistance training based on American College of Sports Medicine (ACSM) guidelines including one or three set of 10 different exercise induced a higher resting energy expenditure (about 5%) for 72 h. Surprisingly the result showed that one set of exercise (15 min) was as effective as three sets (35 min) of the same exercise program [26]. This post-exercise energy expenditure is known as recovery energy expenditure and as previously mentioned is affected by type of exercise and the fact that which muscle groups have been trained [27]. Recently a skeletal muscle originate protein has discovered that induced after physical activity. The production of this protein so called Irisin is controlled by peroxisome proliferator-activated receptor gamma coactivator 1-alpha (PGC-1α) transcriptional coactivator, which in turn upregulated by exercise. Irisin is proposed as a link between physical activity and health benefits of therefrom [28]. Increase in circulating irisin level is involved in browning of white adipose tissues and escalation of the thermogenesis and energy expenditure [29]. Despite the fact that irisin is secreted from skeletal muscle cells, there is still a debate on the effect of different exercise regimens on irisin production based on recent clinical trials [30]. Increased oxidative stress following short-term and long-term physical training found to inhibit inflammatory processes and improve insulin sensitivity by decreasing the vaspin serum concentration [31].
6.2 Glucose Metabolism and Insulin Resistance
Skeletal muscles have two well-controlled mechanisms to uptake glucose from the bloodstream and both of these mechanisms are dependent on glucose transporter type 4 (GLUT4). In the resting state, translocation of GLUT4 to muscle membrane where it imports glucose into the cell fully relies on presence of insulin. Insulin signaling consists of rapid phosphorylation of the insulin receptor, insulin receptor substrate-1/2 on tyrosine residues, and the activation of phosphatidylinositol 3-kinase; however, exercise has no effect on any of these actions. Insulin resistance disrupts this pathway and reduces the capability of insulin target cells to uptake glucose efficiently. However, when a muscle cell is in a contracting during exercise, second pathway is activated. Though the exact underlying mechanism of exercise stimulating effect on GLUT4 translocation is not fully understood, it is known that the pathway is independent of insulin. Shortly various changes in energy levels in consequence of muscle contraction such as increased AMP/ATP, increases in intracellular Ca2+ level, increased reactive oxygen species, and Protein Kinase-C which cause activation of various signaling cascades, some of which are likely acting as activator of GLUT4 translocation [32]. Despite different key regulators (contraction vs insulin signaling) some molecular signaling is common between two pathways [33]. Interesting results of the first animal studies in this area showed that knock out insulin receptors in skeletal muscle of mice had no deficit in glucose uptake stimulated by exercise [34]. In addition to distinct mechanism of glucose uptake by muscle cells, the increase in blood flow due to exercise in muscle tissue increase glucose availability contributes to higher glucose consumption. Improvement of glucose metabolism may be extent to insulin action by the exercise. Cassidy et al. demonstrated high-intensity intermittent training improves peripheral insulin sensitivity in 72 h after the last workout bout and attributed this action to accelerate glycogen breakdown and synthesis [35]. Way et al. conducted a study to explore the effect of systemic training on insulin sensitivity in T2DM patients and if the short inactivity period changes the insulin sensitivity after exercise. They observed that exercise group had significantly higher insulin sensitivity than control group that lasts for 72 h after last training session during inactive period [36].
Several studies demonstrated acceleration of insulin sensitivity induced by the increase in insulin-sensitive glucose transporter on the cell membrane and oxidative enzymes in skeletal muscle. Obese diabetic patients benefit from increased physical activity by the increase in muscle oxidative capacity, increase in muscle mass, decreased blood glucose level, and decreased deposition of total fat [12]. Observations have shown that aerobic exercise even at a low intensity, which lasts 60 min, would enhance insulin action for at least 24 h in obese, insulin-resistant adults. It affects by increasing oxidative capacity, lipid, and glucose metabolism, and insulin sensitivity [8].
A suggested strategy in order to avoid postprandial hyperglycemia in diabetic patients is to benefit the glucose-lowering effect of exercise by performing the session approximately 1 h after a meal to compensate with peak postprandial rise in glucose [19]. Recorded evidence has shown that systematic training programs statistically and clinically affected the glycemic level in a favorable way, and this change has nothing to do with weight loss [37]. A great decrease in blood glucose after exercise intervention was observed; doing exercise causes a decrease in peripheral insulin resistance which leads to increase in peripheral glucose uptake, while liver glucose production remains the same [7].
Exercise may induce hypoglycemia more likely in patients with type 1 diabetes and unlikelier in T2DM patients using insulin or insulin secretagogue medications. It is suggested to perform a short-term (10 s) high-intensity sprint or bouts before, after or between a modest-intensity exercise session in addition to insulin and dietary carbohydrate change to protect against exercise induced hypoglycemia. Nocturnal hypoglycemic events may also occur typically within 6–15 h post-exercise, although risk can extend out to 48 h which can be avoided by insulin and carbohydrate dose and uptake timing adjustment and permanent glucose monitoring [8].
7 The Long-Term Effect of Exercise on Diabetes
Type 2 diabetic patients are 14.6 years earlier exposed to the risk of coronary heart disease, peripheral vascular disease and stroke. Diabetes mellitus also causes impaired renal function, induces albuminuria, and decreased estimated glomerular filtration rate. In addition, patients with T2DM are susceptible to other complications like retinopathy, gastrointestinal motility dysfunction, and even cognitive function and mental health disorders [5]. In addition to all of former complications, diabetes is strongly linked with oxidative stress and inflammation. Inflammation and insulin resistance are known to amplify each other. This chronic state of inflammation is involved in incidence of different diabetes-associated complication including the risk of cardiovascular and renal damage [38]. Insulin resistance is found to be related to skeletal muscle mitochondrial dysfunction. It is observed that mitochondrial content and activity enhancement alongside insulin sensitivity is achieved by endurance exercise training. Moreover, skeletal muscle GLUT4 is observed to be increased with endurance exercise training this effect is a cause of the muscle glucose uptake increased [32]. When Van Germet et al. compared the effect of 6–7% weight loss via exercise or hypocaloric diet on inflammatory marker in inactive, and overweight/obese postmenopausal women. They reported that despite significant decrease in circulating levels of the inflammatory marker, high sensitive c-reactive protein and leptin in both groups; Exercise were found to have more beneficial effect on high sensitive C-reactive protein due to altering body fat and fitness [39]. Evaluations on groups of sedentary T2DM adults after performing 10–20-min training three times per week for 6 weeks of high-intensity functional training, showed a significant increasing in beta-cell function, while decreasing fat storage, preserving lean body mass, improvements of cardiovascular health, lipid metabolism, and LDL cholesterol plus increased insulin sensitivity [20]. Interventions of exercise alone in patients with T2DM have proved to be effective in terms of prevention consisted of improvements in the management of blood glucose levels, body weight, lipids, blood pressure, cardiovascular disease, mortality, and overall quality of life [32].
7.1 Blood Glucose Control
Besides the acute and independent effect of physical activity on blood glucose, chronic exercise ameliorates insulin resistance and glucose control [40]. Resistance exercise may enhance glucose uptake during inactive stats by hypertrophy of skeletal muscle mass, a responsive tissue to insulin signaling. After comparing 12 weeks of aerobic, resistance, and combined exercise in T2DM patients, a glucose level of all three exercise group was decreased however these changes were significantly greater in patients performed combined exercise [7]. A meta-analysis study comparing several trials results showed that all intensities resistance exercise significantly reduced HbA1c [3]. Additionally, aerobic, resistance, and combined protocols of trainings favorably changed A1C [6].
7.2 Bodyweight Management
The prevalence of overweight or obesity is high in patients with T2DM. This excessive weight comes with a burden. Improvements in body composition by the time in order to the elimination of weight burden on joints in overweight patients and decreasing eventual joint pain by exercise may have resulted in better exercise adherence [19]. The metabolic improvements caused by exercise training in type 2 diabetes patients are mostly attributed to decrease of visceral adiposity rather than weight loss in general [19]. In a study evaluating the impact of physical activity on diabetes risk factors an inverse association between physical activity and BMI and prevalence of overweight was found [41]. Exercise reduces body fat percentage which was justified the consequential decrease homeostasis model assessment of insulin resistance and a significant increase in serum omentin-1 [7]. Omentin-1 is an adipocytokine produce mainly from omental and epicardial adipose tissue. Although the effect of omentin-1 on pathogenesis of insulin resistance and diabetes has not been proven, studies have revealed that lower serum omentin-1 is related to increased incidence of diabetes [42].
Physical inactivity is reported to definitely incite accumulation of visceral fat, inflammation and metabolic disorders [43]. Physical activity, as a strategy used to reduce body weight, is effective in correcting the alterations in insulin sensitivity, appetite, serum omentin-1 concentration induced by overweight and obesity. In addition, weight reducing the effect of exercise lowers serum concentrations of vaspin which may lead to inhibition of inflammatory processes and insulin resistance [31]. Decreased liver and visceral fat which plays a key pathogenic role in type 2 diabetes patients was an achievement of Cassidy et al. study, evaluating the effect of vigorous intermittent exercise program on regional fat deposition in patients with T2DM. Therefore, they suggested that high-intensity intermittent exercise is an effective strategy to decrease liver fat in type 2 diabetes patients plus the modest improvements in glycemic control [35]. The magnitude of exercise training on the body fat mass varies according to the type, volume, and intensity of the protocol. Physical activity generally has been reported to cause adaptations in white adipose tissue, such as shrinking cell size, adipocytokine secretion, and modification of inflammation [20].
7.3 Hypertension
Previously, the effect of physical activity on blood pressure of diabetic patients was investigated. This cross-sectional study on 1766 person has demonstrated that diabetic active patients have significantly lower blood pressure than diabetic inactive patients [44]. Physical activity and diastolic blood pressure are found to have an inverse relationship whereas patients with highest active lifestyle had lowest prevalence of hypertension [41]. Clinical trial study on diabetic hypertensive patients showed that even single bout of aerobic exercise with maximal intensity results in 8 h of post-exercise lower blood pressure [45]. Patients with T2DM are more susceptible to exercise hypertension. Although exercise is proven to be beneficial to diminish and control hypertension, poorly controlled hypertensive T2DM patients are recommended to avoid high-intensity training, particularly resistance exercises [19].
7.4 Dyslipidemia
It is estimated that 30–60% of T2DM patients struggle with dyslipidemia [46]. Increase in serum triglyceride, VLDL, IDL and decrease in HDL cholesterol are the common changes in lipid profile among diabetic patients. Unlike type 1 diabetes, severe glucose control in T2DM does not lead to normal lipid profile [47, 48]. Along with routine therapies for dyslipidemia such as pharmacotherapy studies have evaluated the effect of exercise intervention. Physical activities have long been known as an effective strategy to modify dyslipidemia. Contributing the obese and overweight groups of adults in a study with 6 and 12 weeks of moderate exercise showed that regular exercise in overweight subjects decreases HDL-c, leptin, adiponectin and resistin levels and diastolic blood pressure. In the obese group, regular moderate exercise lowered the level of HDL-c, homocysteine, leptin, resistin, IL-6, and adiponectin [49]. In addition, Shakil-ur-Rehman et al. evaluated the effect of 25 weeks of supervised structured aerobic training on serum lipid profile. The results of this study suggest a favorable change in patients received exercise intervention in comparison with control groups [50]. In another clinical trial, even mild to moderate intensity of exercise as usually performed in yoga training was effective in improving dyslipidemia in diabetic patients [51].
7.5 CVD Risk
The evidence from a large cohort study firmly indicates that people with T2DM are at high risk of different cardiovascular diseases including peripheral arterial disease, heart failure, and ischemic stroke. A previous meta-analysis study investigated the effect of exercises of CVD risk factors indicated that aerobic exercise alone or in combination with resistance exercise leads to better glycemic control, systolic blood pressure, triglyceride, and waist circumference which are CVD risk factors. In addition, results showed that resistance exercise alone may not induce similar improvement on CVD risk factors as aerobic exercise did [52].
Cassidy et al. conducted a study to examine the effects of high-intensity intermittent exercise on cardiac function, fat deposition, and glycemic control in patient with T2DM. They found that an intermittent training program increased left ventricular wall mass; they explained that this physiological hypertrophy is a significant effect of exercise that is empowering the cardiac contractile capabilities and should not be confused with “pathological hypertrophy.” Unlike physiological hypertrophy, pathological hypertrophy occurs with an increase collagen accumulation in cardiac tissue. T2DM patients have reduced cardiac contractile function. This study showed that exercise training could improve end-diastolic blood volume, systolic and diastolic function and reduce peak torsion. The researchers suggested that high-intensity intermittent training could be an effective strategy to reverse cardiac dysfunction [35]. Evidence-based results of some studies showed that aquatic exercise improved exercise capacity, cardiovascular system, metabolic profile, and muscle function high level of exercise training in patients with T2DM [53]. For diabetic patients with sedentary lifestyle history and additional cardiovascular risk factors, cardiac screening comprising a stress test to avoid the eventual risk of cardiac events during exercise is recommended [19]. Modulations of exercise, in any stage of treatment, are considered as a potential non-pharmaceutical therapy to improve cardiac structure and function [35]. Chronic inflammation is involved in CVD pathogenesis. Regular exercises are feasible treatment strategy toward reducing risk of CVD in patients with T2DM. One of the underlying mechanisms is regulation of inflammatory cytokines production. Exercise may directly reduce the inflammatory cytokines secretion, for example, reducing body fats or indirectly suppressing the inflammation by upregulating anti-inflammatory cytokines like IL-10 [43]. Muscle has been recognized as an endocrine tissue and is able to influence other systems such as the immune system. Generally, acute bout of exercises is proven to induce an immediate pro-inflammatory response and some of the anti-inflammatory molecules at the same time. Prolonged and regular exercise might improve an anti-inflammatory activity and attenuates the acute response to exercise, which is probably involved in decrease the risk of inflammatory induce diseases such as atherosclerosis [54]. A recent study comparing aerobic and resistance exercise showed that both of these training programs are effective against cardiovascular autonomic abnormalities among diabetic patients. Though, no significant difference between aerobic and resistance exercise was reported [55].
7.6 Retinopathy
As one of the most common complications of diabetes, retinopathy pathogenesis depends on fasting blood glucose and the daily glycemic fluctuation. Patients with good glycemic control have lower risk to develop retinopathy [56]. Observational studies have demonstrated that the severity of retinopathy among diabetic patients is reversely correlated with physical activity. Therefore, patients with proliferative diabetic retinopathy are the less active of all evaluated groups. Interestingly the analysis of data showed that beneficial effect of physical activity is independent of HbA1c level [57, 58]. Similarly, the results of a 10-year prospective cohort of diabetic patients indicated that patients with higher physical activity are less likely to suffer from diabetic retinopathy [59]. Prescription of exercise and activity should be considered with caution, as high intensity of aerobic or resistance exercise may increase the risk of vitreous hemorrhage or retinal detachment [37].
7.7 Nephropathy
Aerobic exercise training is convincingly reported to decrease urine protein excretion likely due to improved glycemic control and reducing blood pressure. However, depending on the amount of blood pressure acute rise by exercise, there is a probability of an acute increase in urinary protein excretion. Resistance exercise training also seems to be of benefit in the glomerular filtration rate [37]. It is shown that combination of calorie restriction and exercise regimen in type 2 diabetic patients leads to mild weight loss of 6% and improvement of kidney function [32]. In addition, an animal study on obese diabetic rat models showed that 10 weeks of treadmill running caused a significantly less glomerular mesangial expansion and tubule-interstitial fibrosis in comparison with sedentary control group. Furthermore, exercised rats had significantly lower plasma advanced glycation end products such as Nɛ-carboxymethyllysine [60]. Regarding the increased risk for cardiovascular disease by microalbuminuria and proteinuria, it is recommended to perform an exercise electrocardiogram stress test in individuals with these disorders plus sedentary lifestyle history whenever aimed to begin exercise at a higher level intensity than the everyday living activities [37].
7.8 Neuropathy
Diabetes peripheral neuropathy is commonly associated with multiple issues such as pain, infection, sensory loss and risk of falling. A study following a 1-h session per week of a supervised Tai Chi practice intervention for 12 weeks found significant improvement in all mentioned symptoms of neuropathy including sensory function, balance, and plantar sensory perception in addition to glucose controlling effect and musculoskeletal and cardiovascular fitness. The study suggests that Tai Chi exercise improve diabetes peripheral neuropathy patients control their posture, physical fitness and preventing falls. Another study found that moderate-intensity treadmill running was a key in reversing the progression of diabetic peripheral neuropathy [61]. A clinical trial on patients with T2DM without neuropathy symptoms carried out to investigate the effect of aerobic and resistance exercise.
Peripheral neuropathy reduces sensation in the hands and feet of patients with T2DM, consequently, their awareness of eventual sores that may happen during impact-full activities even walking or running will be affected. In this regard, proper footwear, routine foot supervision, and low-impact exercises such as cycling, swimming, and resistance training are necessary for patients with peripheral neuropathy, peripheral vascular disease and are advised [19]. Recently a systematic review evaluated 12 randomized clinical trials on the effect of aerobic exercise on nerve function of patients with T2DM. Despite heterogeneity of exercise protocols, 11 studies have reported the beneficial effect of aerobic training on nerve function [62].
8 Efficacy of Different Exercise Regimen on Type 2 Diabetes
8.1 Aerobic
The effect of aerobic exercise on a different aspect of T2DM has been assessed in several studies. These aspects will be discussed in following. Studies on the effect of aerobic exercise on glycemic control have shown that regular training induces favorable alteration in fasting blood glucose, glycated hemoglobin A1C, and insulin sensitivity [6, 63,64,65]. In addition, aerobic exercise could interfere with complications emerged with diabetes such as dyslipidemia, hypertension, nephropathy, and CVD. Moreover, studies have revealed that regular adherence to exercise enhances the quality of life in diabetic patients [66].
Aerobic exercise is shown to acutely increase muscle glucose uptake up to fivefold by insulin-independent mechanisms. If exercise prolonged, muscle glycogen repletion post-exercise demand, holds glucose uptake elevated for about 2 h by insulin-independent and up to 48 h by insulin-dependent mechanisms. The short duration of near-maximal intensity aerobic exercise (20 min) may cause about 24 h of post-exercise insulin action improvements [8]. Aerobic training is a very consistently reported physical activity to improve glycemic control, insulin resistance and dyslipidemia in patients with type 2 diabetes [3]. The results of several studies comparing the effect of different kinds of exercise on quality of life indicated improved physical activity, glucometabolic control, patients’ feeling of physical and mental well-being, leptin and adiponectin levels, HbA1c, body fat percentage. The aerobic exercise can safely and effectively improve the quality of life of in patients with T2DM [61]. De Castro et al. investigated the effect of 12 weeks of resistance, aerobic, and combined exercise on diabetes-induced rats. They found reduction abdominal fat storage and increase serum adiponectin and omentin. In addition, exercised rats performed much better in controlling blood glucose as well as decrease in IL-6 and CRP serum concentration [67]. Aerobic exercise when compared with the resistance and combined training protocols was more effective in reducing abdominal fat deposits, preventing hyperglycemia, decrease in serum IL-6 and CRP and increasing circulating adiponectin and omentin in the visceral adipose tissue [20].
8.2 Resistance
Evidence from several clinical trials raised a debate on effectiveness of resistance exercise on handling glycemic abnormalities. Few studies such as McGinley et al.’s [68] meta-analysis has reported that despite all benefits from strength exercises, no significant improvement in HbA1c gained after using resistance bands. However, noteworthy research studies claimed different outcomes. Recent studies emphasizing the importance and necessity of systematic resistance exercise in efficient controlling of insulin action and management of blood glucose and other cardiovascular risk factors [3]. Both aerobic and resistance training is proven to create fitness in skeletal muscle, adipose tissue, and liver, and regulated insulin sensitivity which is dependent on weight loss. 150 min per week of resistance working out with machines or free weights showed decrease in A1C by 0.57%. However, aerobic exercise showed a significantly greater reduction (difference of 0.18%) of A1C compared with resistance exercise [8]. In the case of older patients, even low-intensity resistance exercise for 16 weeks results in gaining muscular size and strength and significantly better glucose control [69]. A published research surveying progressive resistance training in adult participants with T2DM demonstrated that exercised participants had a significant improvement in mental health status along with attenuated body. Considering the fact that there were also studies that found no significant change, the effect of strength exercise on the quality of life in patients with T2DM was considered to be uncertain [61].
It was observed that participants who performed either resistance exercise alone or combined resistance and aerobic exercise consisted of longer time adherence than those randomized to only aerobic exercise. Resistance exercise participants also reported more sense of enjoyment and more support from their trainers. This might explain their greater long-term exercise adherence. Participants who remained adherent to exercise over time documented to have the same barriers to exercise such as work commitments, weather and illness/injury, but they benefited more facilitators including perceived health benefits, family support and use of strategies to maintain activity level, when were compared with those whose exercise adherence diminished over time [14].
8.3 Combined
Combined training is found to be the most effective for the aim of glycemic control when compared to either aerobic or resistance training alone [8]. Results from several studies documented improvements in anthropometric and biochemical parameters including increased muscle mass, better glycemic control, decreased in total intra-myocytic fat. In addition, patients receiving combined exercise had higher fatty acid oxidation capacity, physical function and mental health [61]. Most of the studies demonstrated that achieving both aerobic and resistance exercise by diabetic patients results in the strongest effect on increasing insulin sensitivity compared with when doing only aerobic exercise [7]. Interesting evidence demonstrated that resistance exercises, being less efficient in reducing serum glucose than aerobic workout when is performed prior to aerobic exercise at the same session. Results in greater stability in glucose levels, and less hypoglycemic experiences, both during the exercise session and after its completion, were reported in combined exercises [70].
9 Physical Activity Recommendation for Patients with Type 2 Diabetes
Since the challenges related to controlling blood glucose depend on diabetes type, activity type, and presence of diabetes-related morbidities, exercise recommendations should be designed to achieve the precise necessities of each person [8]. According to the American Diabetes Association recommendation for youngsters with type 1 or type 2 diabetes should have moderate- or high-intensity aerobic exercise for 60 min or more per day. It is recommended to resistance exercise for at least 3 days per week to strengthen muscles and bones. Type 1 and type 2 diabetic adults should follow moderate- to high-intensity aerobic exercise for 150 min or more per week in at least 3 sessions per week and a 2-day rest for recovery. Performing high-intensity or interval training depending on individual fitness level may need shorter duration: at least 75 min/week and 2–3 sessions/week of strength training on nonconsecutive days is also recommended. Additionally in order to increase flexibility, muscular strength, and balance, flexibility and balance training such as yoga and tai chi are recommended 2–3 times/week for older adults with diabetes [11]. For patients with T2DM and or prediabetes in order to prevent or manage the progression of the disease morbidity a minimum of 210 min/week of moderate-intensity exercise or 125 min/week of high-intensity exercise recommended. Exercise intensity should be selected depending on disease level, health condition, and primary individual fitness evaluation [19]. Given that performing aerobic exercises, such as jogging, brisk walking, cycling, and swimming, engages large and multiple groups of muscles, relatively prolonged periods of performing time are required. In relation to morbidity and common health complications of type 2 diabetes patients such as being obese or overweight with physical disability, vision difficulty, or cardiovascular burdens, it is almost infeasible to achieve the adequate volume and intensity of the aerobic exercise to meet the expected results. On the other hand, resistance exercise especially high-intensity progressive resistance workout can be performed in a residential setting. Hence resistance exercises are more achievable and a safe choice for inactive older diabetic patients to achieve the goal without additional difficulties. Strength exercise should be carried out at 75–85% (1 RM) using muscular strength to move a weight or to work against a resistive load in a more adjustable way.
9.1 Type/Intensity/Duration
Moderate to high intensity aerobic exercise has been shown to reduce the risk of cardiovascular disease, thereby reducing the mortality of type 1 and type 2 diabetes. In type 1 diabetes, aerobic exercise improves the quality of life of patients by increasing cardiorespiratory fitness, reducing insulin resistance, and improving blood lipid levels and endothelial function. In patients with type 2 diabetes, exercise training result in lower A1C, triglycerides, blood pressure and insulin resistance. In order to promote skeletal muscle oxidative capacity, insulin sensitivity and glycemic control in type 2 diabetic adults, high intensity interval training (HIIT) can be performed. In addition, diabetes is known to be a factor that causes low muscle strength and accelerates muscle strength and functional decline, so it is necessary to participate in resistance exercise to improve muscle mass, body composition, fitness, bone mineral density, metabolic constants, and so on. On the other hand, resistance exercise can reduce blood glucose in patients with type 1 diabetes. Therefore, in combination with resistance and aerobic exercise in one exercise, it is recommended to perform resistance exercise first to lower blood glucose. Due to the formation of advanced glycation end products, these terminal glycation end products accumulate and accelerate during normal aging, so it is common to have limited joint mobility in elderly patients with T2DM. Therefore, flexibility training or balance training can increase the range of motion around the joints to reduce the risk of falling. In the case of peripheral neuropathy, yoga and tai chi are recommended to improve symptoms and quality of life. High-intensity physical exercise may bring some health risks to diabetic patients, including acute complications such as heart disease and hyperglycemia. For those who wish to increase their exercise intensity, it is recommended to exercise under medical supervision. However, if you want to do low- or medium-intensity physical exercise, you do not need medical monitoring before exercise. Most international guidelines recommend 3–7 days per week, at least 150 min per week for moderate to strong exercise, or more than 75 min per week for aerobic exercise. It is recommended to perform moderate to resistance exercise 2–3 days per week. Resistance exercise while performing flexibility and balance exercises such as yoga and Tai Chi was recommended. For each type of exercise, time and individual abilities should also be considered, and intensity and time should be appropriately increased and supervised by an exercise physiologist with knowledge of diabetes or a certified fitness professional. Proper exercise can lead to increased body heat and elevated core temperatures, resulting in increased blood flow and increased sweating. This can lead to poor glycemic control, neuropathy, dehydration, and heat-related diseases. Due to changes in joint structures related to glycemic excursions, and in order to prevent exercise-related overuse injuries and excessive aggravation to joint surfaces and structures, exercise training progression for individuals with diabetes should apply appropriately and personalized programs, particularly when taking statin medications for lipid control. Additionally, patients with peripheral neuropathy contributing exercise should take proper foot care and be supervised to prevent, and detect eventual problems early to reduce the risk of ulceration and amputation. Patients with a sign of progressive retinopathy should avoid vigorous aerobic or resistance exercises, such as jumping, jarring, headstand, and breath-holding activities [8].
Taking together, diabetic and prediabetes individuals are strongly advised to contribute a regular exercise in a personalized mode and intensity at least for 150 min per week. To avoid any adverse effects, patients need to consult with and be supervised regularly by expert physiologists to prescribe an appropriate individualized exercise program and follow-up. It is obviously necessary to have social and family support to keep adherence to medical care alongside physical activity to meet the expected management and control of the disease.
References
American Diabetes Association (2018) 2. Classification and diagnosis of diabetes: standards of medical care in diabetes—2018. Diabetes Care 41(Suppl 1):S13–S27
Li R, Qu S, Zhang P, Chattopadhyay S, Gregg EW, Albright A, Hopkins D, Pronk NP (2015) Economic evaluation of combined diet and physical activity promotion programs to prevent type 2 diabetes among persons at increased risk: a systematic review for the Community Preventive Services Task Force. Ann Intern Med 163(6):452–460
Liu Y, Ye W, Chen Q, Zhang Y, Kuo C-H, Korivi M (2019) Resistance exercise intensity is correlated with attenuation of HbA1c and insulin in patients with type 2 diabetes: a systematic review and meta-analysis. Int J Environ Res Public Health 16(1):140
Chen L, Chen R, Wang H, Liang F (2015) Mechanisms linking inflammation to insulin resistance. Int J Endocrinol 2015:1
Zheng Y, Ley SH, Hu FB (2018) Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol 14(2):88
Jorge MLMP, de Oliveira VN, Resende NM, Paraiso LF, Calixto A, Diniz ALD, Resende ES, Ropelle ER, Carvalheira JB, Espindola FS (2011) The effects of aerobic, resistance, and combined exercise on metabolic control, inflammatory markers, adipocytokines, and muscle insulin signaling in patients with type 2 diabetes mellitus. Metabolism 60(9):1244–1252
AminiLari Z, Fararouei M, Amanat S, Sinaei E, Dianatinasab S, AminiLari M, Daneshi N, Dianatinasab M (2017) The effect of 12 weeks aerobic, resistance, and combined exercises on omentin-1 levels and insulin resistance among type 2 diabetic middle-aged women. Diabetes Metab J 41(3):205–212
Colberg SR, Sigal RJ, Yardley JE, Riddell MC, Dunstan DW, Dempsey PC, Horton ES, Castorino K, Tate DF (2016) Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care 39(11):2065–2079
American Diabetes Association (2017) 2. Classification and diagnosis of diabetes. Diabetes Care 40(Suppl 1):S11–S24
American Diabetes Association (2019) 12. Older adults: standards of medical care in diabetes—2019. Diabetes Care 42(Suppl 1):S139–S147
American Diabetes Association (2018) 4. Lifestyle management: standards of medical care in diabetes—2018. Diabetes Care 41(Supplement 1):S38–S50
Osama A-J, Shehab AE-K (2015) Psychological wellbeing and biochemical modulation in response to weight loss in obese type 2 diabetes patients. Afr Health Sci 15(2):503–512
American Diabetes Association (2019) 8. Obesity management for the treatment of type 2 diabetes: standards of medical care in diabetes—2019. Diabetes Care 42(Supplement 1):S81–S89
Young-Hyman D, De Groot M, Hill-Briggs F, Gonzalez JS, Hood K, Peyrot M (2016) Psychosocial care for people with diabetes: a position statement of the American Diabetes Association. Diabetes Care 39(12):2126–2140
Howley E (2015) Type of activity: resistance, aerobic and leisure versus occupational physical activity. http://www.ncbi.nlm.nih.gov/pubmed/11427761. Retrieved 14 June 2015
American Diabetes Association (2017) 5. Prevention or delay of type 2 diabetes. Diabetes Care 40(Suppl 1):S44–S47
Kriska A (2000) Physical activity and the prevention of type 2 diabetes mellitus. Sports Med 29(3):147–151
Orozco LJ, Buchleitner AM, Gimenez-Perez G, i Figuls MR, Richter B, Mauricio D (2008) Exercise or exercise and diet for preventing type 2 diabetes mellitus. Cochrane Database Syst Rev (3):CD003054
Hordern MD, Dunstan DW, Prins JB, Baker MK, Singh MAF, Coombes JS (2012) Exercise prescription for patients with type 2 diabetes and pre-diabetes: a position statement from Exercise and Sport Science Australia. J Sci Med Sport 15(1):25–31
Feito Y, Patel P, Sal Redondo A, Heinrich KM (2019) Effects of eight weeks of high intensity functional training on glucose control and body composition among overweight and obese adults. Sports 7(2):51
Laaksonen DE, Lindström J, Lakka TA, Eriksson JG, Niskanen L, Wikström K, Aunola S, Keinänen-Kiukaanniemi S, Laakso M, Valle TT (2005) Physical activity in the prevention of type 2 diabetes: the Finnish diabetes prevention study. Diabetes 54(1):158–165
Ades PA (2015) A lifestyle program of exercise and weight loss is effective in preventing and treating type 2 diabetes mellitus: why are programs not more available? Prev Med 80:50–52
Romijn J, Coyle E, Sidossis L, Gastaldelli A, Horowitz J, Endert E, Wolfe R (1993) Regulation of endogenous fat and carbohydrate metabolism in relation to exercise intensity and duration. Am J Phys Endocrinol Metab 265(3):E380–E391
Knab AM, Shanely RA, Corbin KD, Jin F, Sha W, Nieman DC (2011) A 45-minute vigorous exercise bout increases metabolic rate for 14 hours. Med Sci Sports Exerc 43(9):1643–1648
Paoli A, Moro T, Marcolin G, Neri M, Bianco A, Palma A, Grimaldi K (2012) High-Intensity Interval Resistance Training (HIRT) influences resting energy expenditure and respiratory ratio in non-dieting individuals. J Transl Med 10(1):237
Heden T, Lox C, Rose P, Reid S, Kirk EP (2011) One-set resistance training elevates energy expenditure for 72 h similar to three sets. Eur J Appl Physiol 111(3):477–484
Cunha FA, Midgley AW, McNaughton LR, Farinatti PT (2016) Effect of continuous and intermittent bouts of isocaloric cycling and running exercise on excess postexercise oxygen consumption. J Sci Med Sport 19(2):187–192
Chen N, Li Q, Liu J, Jia S (2016) Irisin, an exercise-induced myokine as a metabolic regulator: an updated narrative review. Diabetes Metab Res Rev 32(1):51–59
Huh JY, Siopi A, Mougios V, Park KH, Mantzoros CS (2015) Irisin in response to exercise in humans with and without metabolic syndrome. J Clin Endocrinol Metabol 100(3):E453–E457
Pekkala S, Wiklund PK, Hulmi JJ, Ahtiainen JP, Horttanainen M, Pöllänen E, Mäkelä KA, Kainulainen H, Häkkinen K, Nyman K (2013) Are skeletal muscle FNDC5 gene expression and irisin release regulated by exercise and related to health? J Physiol 591(21):5393–5400
Escoté X, Gómez-Zorita S, López-Yoldi M, Milton-Laskibar I, Fernández-Quintela A, Martínez J, Moreno-Aliaga M, Portillo M (2017) Role of omentin, vaspin, cardiotrophin-1, TWEAK and NOV/CCN3 in obesity and diabetes development. Int J Mol Sci 18(8):1770
Stanford KI, Goodyear LJ (2014) Exercise and type 2 diabetes: molecular mechanisms regulating glucose uptake in skeletal muscle. Adv Physiol Educ 38(4):308–314
Kramer HF, Witczak CA, Taylor EB, Fujii N, Hirshman MF, Goodyear LJ (2006) AS160 regulates insulin-and contraction-stimulated glucose uptake in mouse skeletal muscle. J Biol Chem 281(42):31478–31485
Wojtaszewski JF, Higaki Y, Hirshman MF, Michael MD, Dufresne SD, Kahn CR, Goodyear LJ (1999) Exercise modulates postreceptor insulin signaling and glucose transport in muscle-specific insulin receptor knockout mice. J Clin Invest 104(9):1257–1264
Cassidy S, Thoma C, Hallsworth K, Parikh J, Hollingsworth KG, Taylor R, Jakovljevic DG, Trenell MI (2016) High intensity intermittent exercise improves cardiac structure and function and reduces liver fat in patients with type 2 diabetes: a randomised controlled trial. Diabetologia 59(1):56–66
Way KL, Hackett DA, Baker MK, Johnson NA (2016) The effect of regular exercise on insulin sensitivity in type 2 diabetes mellitus: a systematic review and meta-analysis. Diabetes Metab J 40(4):253–271
Sigal RJ, Kenny GP, Wasserman DH, Castaneda-Sceppa C, White RD (2006) Physical activity/exercise and type 2 diabetes: a consensus statement from the American Diabetes Association. Diabetes Care 29(6):1433–1438
Domingueti CP, Dusse LMSA, das Graças Carvalho M, de Sousa LP, Gomes KB, Fernandes AP (2016) Diabetes mellitus: the linkage between oxidative stress, inflammation, hypercoagulability and vascular complications. J Diabetes Complicat 30(4):738–745
Van Gemert WA, May AM, Schuit AJ, Oosterhof BY, Peeters PH, Monninkhof EM (2016) Effect of weight loss with or without exercise on inflammatory markers and adipokines in postmenopausal women: the SHAPE-2 trial, a randomized controlled trial. Cancer Epidemiol Prev Biomarkers 25(5):799–806
Bacchi E, Negri C, Zanolin ME, Milanese C, Faccioli N, Trombetta M, Zoppini G, Cevese A, Bonadonna RC, Schena F (2012) Metabolic effects of aerobic training and resistance training in type 2 diabetic subjects: a randomized controlled trial (the RAED2 study). Diabetes Care 35(4):676–682
Bohn B, Herbst A, Pfeifer M, Krakow D, Zimny S, Kopp F, Melmer A, Steinacker JM, Holl RW (2015) Impact of physical activity on glycemic control and prevalence of cardiovascular risk factors in adults with type 1 diabetes: a cross-sectional multicenter study of 18,028 patients. Diabetes Care 38(8):1536–1543
Wittenbecher C, Menzel J, Carstensen-Kirberg M, Biemann R, di Giuseppe R, Fritsche A, Isermann B, Herder C, Aleksandrova K, Boeing H (2016) Omentin-1, adiponectin, and the risk of developing type 2 diabetes. Diabetes Care 39(6):e79–e80
Pedersen BK (2017) Anti-inflammatory effects of exercise: role in diabetes and cardiovascular disease. Eur J Clin Investig 47(8):600–611
Duclos M, Dejager S, Postel-Vinay N, di Nicola S, Quéré S, Fiquet B (2015) Physical activity in patients with type 2 diabetes and hypertension–insights into motivations and barriers from the MOBILE study. Vasc Health Risk Manag 11:361
de Morais PK, Sales MM, de Almeida JA, Motta-Santos D, de Sousa CV, Simões HG (2015) Effects of aerobic exercise intensity on 24-h ambulatory blood pressure in individuals with type 2 diabetes and prehypertension. J Phys Ther Sci 27(1):51–56
Wang CCL, Hess CN, Hiatt WR, Goldfine AB (2016) Atherosclerotic cardiovascular disease and heart failure in type 2 diabetes—mechanisms, management, and clinical considerations. Circulation 133(24):2459
Ginsberg HN, MacCallum PR (2009) The obesity, metabolic syndrome, and type 2 diabetes mellitus pandemic: Part I. Increased cardiovascular disease risk and the importance of atherogenic dyslipidemia in persons with the metabolic syndrome and type 2 diabetes mellitus. J Cardiometab Syndr 4(2):113–119
Wu L, Parhofer KG (2014) Diabetic dyslipidemia. Metabolism 63(12):1469–1479
Gondim OS, de Camargo VTN, Gutierrez FA, de Oliveira Martins PF, Passos MEP, Momesso CM, Santos VC, Gorjão R, Pithon-Curi TC, Cury-Boaventura MF (2015) Benefits of regular exercise on inflammatory and cardiovascular risk markers in normal weight, overweight and obese adults. PLoS One 10(10):e0140596
Shakil-ur-Rehman S, Karimi H, Gillani SA (2017) Effects of supervised structured aerobic exercise training program on high and low density lipoprotein in patients with type II diabetes mellitus. Pak J Med Sci 33(1):96
Nagarathna R, Tyagi R, Kaur G, Vendan V, Acharya IN, Anand A, Singh A, Nagendra HR (2019) Efficacy of a validated yoga protocol on dyslipidemia in diabetes patients: NMB-2017 India trial. Medicines 6(4):100
Chudyk A, Petrella RJ (2011) Effects of exercise on cardiovascular risk factors in type 2 diabetes: a meta-analysis. Diabetes Care 34(5):1228–1237
Cugusi L, Cadeddu C, Nocco S, Orrù F, Bandino S, Deidda M, Caria A, Bassareo PP, Piras A, Cabras S, Mercuro G (2015) Effects of an aquatic-based exercise program to improve cardiometabolic profile, quality of life, and physical activity levels in men with type 2 diabetes mellitus. PM R 7(2):141–148
Gjevestad GO, Holven KB, Ulven SM (2015) Effects of exercise on gene expression of inflammatory markers in human peripheral blood cells: a systematic review. Curr Cardiovasc Risk Rep 9(7):34
Bellavere F, Cacciatori V, Bacchi E, Gemma M, Raimondo D, Negri C, Thomaseth K, Muggeo M, Bonora E, Moghetti P (2018) Effects of aerobic or resistance exercise training on cardiovascular autonomic function of subjects with type 2 diabetes: a pilot study. Nutr Metab Cardiovasc Dis 28(3):226–233
Hsu C-R, Chen Y-T, Sheu WH-H (2015) Glycemic variability and diabetes retinopathy: a missing link. J Diabetes Complicat 29(2):302–306
Praidou A, Harris M, Niakas D, Labiris G (2017) Physical activity and its correlation to diabetic retinopathy. J Diabetes Complicat 31(2):456–461
Loprinzi PD, Brodowicz GR, Sengupta S, Solomon SD, Ramulu PY (2014) Accelerometer-assessed physical activity and diabetic retinopathy in the United States. JAMA Ophthalmol 132(8):1017–1019
Yan X, Han X, Wu C, Shang X, Zhang L, He M (2019) Effect of physical activity on reducing the risk of diabetic retinopathy progression: 10-year prospective findings from the 45 and up study. Available at SSRN 3347912
Boor P, Celec P, Behuliak M, Grančič P, Kebis A, Kukan M, Pronayová N, Liptaj T, Ostendorf T, Šebeková K (2009) Regular moderate exercise reduces advanced glycation and ameliorates early diabetic nephropathy in obese Zucker rats. Metabolism 58(11):1669–1677
Cai H, Li G, Zhang P, Xu D, Chen L (2017) Effect of exercise on the quality of life in type 2 diabetes mellitus: a systematic review. Qual Life Res 26(3):515–530
Gu Y, Dennis SM, Kiernan MC, Harmer AR (2019) Aerobic exercise training may improve nerve function in type 2 diabetes and pre-diabetes: a systematic review. Diabetes Metab Res Rev 35(2):e3099
Støa EM, Meling S, Nyhus L-K, Strømstad G, Mangerud KM, Helgerud J, Bratland-Sanda S, Støren Ø (2017) High-intensity aerobic interval training improves aerobic fitness and HbA1c among persons diagnosed with type 2 diabetes. Eur J Appl Physiol 117(3):455–467
Gregory JM, Muldowney JA, Engelhardt BG, Tyree R, Marks-Shulman P, Silver HJ, Donahue EP, Edgerton DS, Winnick JJ (2019) Aerobic exercise training improves hepatic and muscle insulin sensitivity, but reduces splanchnic glucose uptake in obese humans with type 2 diabetes. Nutr Diabetes 9(1):1–12
Nojima H, Yoneda M, Watanabe H, Yamane K, Kitahara Y, Sekikawa K, Yamamoto H, Yokoyama A, Hattori N, Kohno N (2017) Association between aerobic capacity and the improvement in glycemic control after the exercise training in type 2 diabetes. Diabetol Metab Syndr 9(1):63
Dede ND, Ipekci S, Kebapcilar L, Arslan M, Kurban S, Yildiz M, Gonen MS (2018) Effect of aerobic exercise training on serum malondialdehyde level and quality of life in type 2 diabetes. In: 20th European congress of endocrinology: 2018: BioScientifica
de Castro CA, da Silva KA, Rocha MC, Sene-Fiorese M, Nonaka KO, Malavazi I, de Freitas Anibal F, de Oliveira Duarte ACG (2018) Exercise and omentin: their role in the crosstalk between muscle and adipose tissues in type 2 diabetes mellitus rat models. Front Physiol:9, 1881
McGinley SK, Armstrong MJ, Boulé NG, Sigal RJ (2015) Effects of exercise training using resistance bands on glycaemic control and strength in type 2 diabetes mellitus: a meta-analysis of randomised controlled trials. Acta Diabetol 52(2):221–230
Takenami E, Iwamoto S, Shiraishi N, Kato A, Watanabe Y, Yamada Y, Yamada S, Ishii N (2019) Effects of low-intensity resistance training on muscular function and glycemic control in older adults with type 2 diabetes. J Diabetes Investig 10(2):331–338
Riddell MC, Sigal RJ (2013) Physical activity, exercise and diabetes. Can J Diabetes 37(6):359–360
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Amanat, S., Ghahri, S., Dianatinasab, A., Fararouei, M., Dianatinasab, M. (2020). Exercise and Type 2 Diabetes. In: Xiao, J. (eds) Physical Exercise for Human Health. Advances in Experimental Medicine and Biology, vol 1228. Springer, Singapore. https://doi.org/10.1007/978-981-15-1792-1_6
Download citation
DOI: https://doi.org/10.1007/978-981-15-1792-1_6
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-1791-4
Online ISBN: 978-981-15-1792-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)