Abstract
Drug use reemerged in China after the 1978 introduction of sweeping economic change initiated by the “Opening Up and Reform” policy, and the high-risk behavior of drug users was the major driver of China’s early HIV epidemic. To combat both the growing drug use and HIV epidemics, China’s National Methadone Maintenance Treatment (MMT) Program was piloted in 2004 and scaled up starting in 2006. By the end of 2015, the program encompassed 785 full-service clinics, 29 mobile vans, and 325 satellite sites nationwide that were providing MMT services to more than 170,000 regular clients who were former heroin injectors. China’s National MMT Program had become the largest opioid substitution therapy program in the world. This important harm reduction program has successfully reduced illicit drug use, HIV incidence, mortality, and criminal activity, as well as improved quality of life. However, there are still a wide range of challenges and gaps remaining, and further work to strengthen this program will be necessary for HIV to be eliminated in this important key population.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
1 The Evolution of China’s Drug Use Epidemic
1.1 The Rise, Fall, and Reemergence of Opioid Drugs
After China was defeated by the British in the two Opium Wars (1839–1842 and 1856–1860), the production and use of opioid drugs increased dramatically nationwide (Jia et al. 2015; Lu and Wang 2008). By 1906, there were more than ten million opioid users in China, accounting for 27% of the adult male population, who had consumed around 39,000 tons of opium (Fang et al. 2006). This astounding prevalence of opioid use might have been the largest in the world history.
Once the People’s Republic of China was founded in 1949, the government initiated a vigorous nationwide campaign against illicit opium cultivation and drug use. During this campaign, cultivation, trafficking, buying and selling, and possession and use of opioid drugs were made illegal and assigned penalties ranging from imprisonment to death. Largely due to the firm and severe actions taken by the Chinese government, one of the most acute drug use epidemics in Chinese and world history ended within 3 years, after which China experienced a relatively drug-free period between the mid-1950s and the mid-1970s (Lu and Wang 2008; McCoy et al. 2001).
However, since China implemented its historic economic reforms in the late 1970s and early 1980s, beginning with the “Opening Up and Reform” policy of 1978, trade of illicit goods, including opioids, reemerged. As neighbor to the world’s largest heroin-producing regions, the “Golden Triangle” (i.e., Myanmar, Thailand, and the Lao People’s Democratic Republic) and the “Golden Crescent” (i.e., Afghanistan and Pakistan), China has become integrated into the largest drug trafficking routes in the eastern hemisphere (Lu and Wang 2008). Very large amounts of opioids, mostly heroin, have since been smuggled into China, mainly from Myanmar into Yunnan province or from Vietnam into Guangxi Zhuang Autonomous Region (hereafter Guangxi).
Due to low prices, widespread availability, and lack knowledge of its deleterious consequences, opioid drug use became prevalent in these regions. Illicit drug use, particularly heroin use, then quickly spread to other neighboring provinces including Sichuan, Guangdong, Guizhou, Hunan, and Xinjiang Uyghur Autonomous Region (hereafter Xinjiang) via drug trafficking routes. As the world’s largest opium-producing region since 2003, the Golden Crescent became a major drug supplier to Xinjiang and other provinces in the northwest region of China. According to data issued by the United Nations Office on Drugs and Crime (UNODC), Xinjiang drug control authorities solved ten Golden Crescent drug trafficking cases in 2004, four of which involved more than 1 kg of heroin. By contrast, more than 600 kg of heroin was captured in 2010 (United Nations Office on Drugs and Crime 2012).
Initially, illicit drug use was concentrated in ethnic minority populations, such as Dai, Jingpo, and Zhuang, living in border regions. More than 80% of people using heroin in Dehong prefecture, Yunnan province, the site of the first HIV outbreak identified among drug users, belonged to Dai and Jingpo ethnic groups. The opioid drug use epidemic in China rapidly worsened in the 1980s, 1990s, and early 2000s (Jia et al. 2015; Liu et al. 2010), and the cumulative total number of registered illicit drug users in the country increased from approximately 70,000 in 1990 to over 1.1 million in 2004.
In 2005, President Hu Jintao called for a “People’s War on Drugs” to address the nation’s ballooning heroin use problem. Five campaigns were launched—drug abuse prevention education; drug addiction treatment and rehabilitation; drug supply reduction and control; antidrug law enforcement scale-up to facilitate a “crackdown” on drug possession, transport, buying, and selling; and control of chemicals used in drug production (Jia et al. 2015). A recent nationwide, retrospective study of nearly 1.2 million drug users that aimed to evaluate the effect of the war on China’s drug use epidemic found that while some important indicators showed improvement between 2005 and 2010 (i.e., proportion of drug users who relapse, risk of relapse, proportion of new drug users who use heroin, and risk of occurrence of new heroin users), other indicators suggest that China’s drug use epidemic was changing (Jia et al. 2015).
1.2 The Arrival of Synthetic Drugs
Traditionally, opioids, especially opium and heroin, have been the most commonly used drugs in China. However, rates of opioid use have plateaued, and drug use has shifted to new types of addictive drugs (Jia et al. 2015; Lu and Wang 2008; Lu et al. 2008). Since the first 3,4-methylenedioxy-N-methylamphetamine (MDMA; also known as “ecstasy”) use case was reported in China in 1994, the use of new psychoactive substances (NPS; also called “synthetic drugs” or “club drugs”) has spread throughout the country very quickly, with concentrations found in southeastern regions and business-centered cities. One study reported that 74% of heroin users had also used synthetic drugs, 14% of whom had switched to using synthetic drugs exclusively (Zhang 2006). Generally, users of synthetic drugs believed that they did not have addictive properties and had have fewer physical and mental health consequences compared to heroin or other opioid drugs (Joe Laidler 2005). Moreover, synthetic drugs are not illegal in China, so users do not risk arrest or incarceration, making them an even more attractive alternative to heroin.
Besides MDMA, other synthetic drugs commonly used in China include crystal methamphetamine (MA; a.k.a. “ice”), ketamine (a.k.a. “K Fen,” “Special K”), “Magu” pills (capsules typically containing a mixture of MA and other drugs including caffeine), and alkyl nitrite inhalants (called “poppers”). Both the variety of synthetic drugs available and the numbers of synthetic drug users have been increasing rapidly since the beginning of the “People’s War on Drugs.” In one nationwide, retrospective study, researchers found a 920% increase in synthetic drug users among all drug users and an 861% increase among new drug users over an 8-year period from 2003 to 2010 (Jia et al. 2015). According to official statistics, the proportion of registered club drug users among all drug users increased from 9.5% in 2004 to 38% in 2012 (National Narcotics Control Commission 2005, 2013). For the first time in 2014, the prevalence of synthetic drug use among registered drug users in China exceeded the prevalence of opioid use (National Narcotics Control Commission 2015).
1.3 Early Responses to the Drug Use Epidemic
To combat the resurgence of drug use, the Chinese government first responded in the 1980s by mobilizing enormous resources to reduce the drug supply. However, this strategy failed because China’s lengthy borders are difficult to monitor and there is a virtually free flow of trade and migration in and out of the country, especially along the southern borders adjoining the Golden Triangle.
In 1990, the Standing Committee of the National People’s Congress issued the Regulation on Prohibition Against Narcotics, which specified three steps to end drug use. First, drug users, when detained by police for the first time, were to be fined and/or encouraged to receive treatment in hospital-based voluntary detoxification centers run by the Ministry of Health. Drug users typically stayed at these centers for 1–4 weeks. Second, relapsed drug users who have previously attended voluntary detoxification treatment, detained by police a second time, were to be sent to compulsory detoxification centers, which are managed by the Public Security Bureau. Drug users sent to compulsory detoxification typically spend at least 6 months undergoing a combination of detoxification therapy, physical exercise, and manual labor. Third, relapsed drug users who have previously been confined in compulsory detoxification centers, detained by police for the third time, were to be sentenced to 2–3 years in reeducation-through-labor camps, which are administered by the Ministry of Justice (Sullivan and Wu 2007).
In general, voluntary and compulsory detoxification treatment mainly serve to force drug users to quit drug use and prevent them from committing crimes associated with drug use, as well as demonstrate the government’s commitment to addressing the drug problem. However, due to limited resources, many compulsory detoxification centers have become overcrowded, understaffed, and underfunded. Furthermore, drug users in these settings are provided very little psychosocial counseling and health education, and staff receive very little skills training and capacity building. Consequently, a significant body of research has found that it is difficult for drug users released from detoxification centers to successfully reintegrate into society and relapse rates exceed 90%. Clearly, this method of dealing with drug use is not effective (Liu et al. 2006). Furthermore, the broader international community has criticized compulsory detoxification treatment centers in China and elsewhere, noting a myriad of human rights violations and calling for their closure.
Nevertheless, drug use and addiction has traditionally been viewed by Chinese society as a moral failing of the individual and as a complex social problem that affects families, neighbors, and even entire communities. Therefore, it has been thought that the solution to China’s drug use should consider the rights of community members whose lives are affected by drug users (Li et al. 2010). In this social and cultural context, it is not surprising that the initial response to drug use has been punitive, and hence, the Chinese government continued to scale up compulsory detoxification treatment centers. According to official statistics, nearly 700 centers were operating across China, covering more than 300,000 people, in 2012 (National Narcotics Control Commission 2013).
2 Public Health Implications of Drug Use
Studies indicate that people who use drugs often experience extremely stressful and chaotic lives, including dealing with unemployment, homelessness, family disruption, loss of economic productivity, and social instability (World Health Organization et al. 2004). Apart from social instability caused by drug use, drug users are more likely to engage in criminal behaviors. For example, according to data published by the National Narcotics Control Commission, 133,000 individuals committed drug-related crimes (e.g., theft, violence, drug trafficking, prostitution) in 2012 nationwide, an increase of 18% over the prior year (National Narcotics Control Commission 2013). In some areas of China, crimes associated with drug use accounted for about 70–80% of all criminal activity. In Lanzhou, a city in northwestern China, approximately 70% of drug users reported that they had committed crimes (Fang et al. 2006; Shi et al. 2007).
In addition to negative social consequences, drug use also has major health consequences. Previous studies conducted in various countries have consistently indicated that drug users have a much higher risk of death than non-drug users (Hulse et al. 1999; Morgan et al. 2006). It has been reported that leading causes of death among drug users are overdose, AIDS-related disease, and suicide (Brugal et al. 2005; Cao et al. 2013; Degenhardt et al. 2006; McCowan et al. 2009).
2.1 Opioids and Risk of Infectious Disease
Many drug users shift from smoking opioids to injecting them, typically heroin, soon after they realize that injecting is more cost-effective and has a stronger effect. Unfortunately, sharing of drug injecting equipment is a common practice among people who inject drugs (PWID) worldwide, which increases the risk of infection with HIV and other infectious diseases, such as hepatitis C virus (HCV). Behavioral surveillance data in China have shown that the prevalence of needle sharing among PWID has been quite high.
In addition to risky drug injecting behaviors, a majority of drug users tend to engage in risky sexual behaviors and are less likely to consistently use condoms compared to nonusers. This exposes not only injecting partners but also sexual partners to risk of HIV, HCV, and other infectious agents (Liu et al. 2010; Sullivan and Wu 2007). Although most drug users in China are male, female drug users may be at comparatively greater risk for HIV infection since they tend to have sexual partners that are drug users and are more likely to be involved in the sex industry (Sullivan and Wu 2007). Given that the sexual partners of drug users are a likely bridge to the general population, targeting this population for HIV prevention and intervention has been a top priority in China (State Council AIDS Working Committee Office and the United Nations Theme Group on HIV/AIDS in China 2004).
2.2 Synthetic Drugs and Risk of Infectious Disease
Synthetic drugs are generally taken by smoking, snorting, inhaling, or swallowing and less commonly by injecting. They are known for acting very quickly on the nervous system, giving the user an immediate “rush” of energy, confidence, and euphoria. Unlike opioids, where the primary risk of infectious disease comes with the sharing of injecting equipment, synthetic drugs bring risk of infectious disease through their very strong influence on sexual behavior. Synthetic drugs are known to increase sexual desire and suppress inhibitions, exaggerate sexual pleasure and prolong sexual episodes, and generally promote high-risk sexual behaviors such as having multiple sex partners, having sex without condoms, and engaging in “sexual marathons,” group sex, or homosexual sex (Corsi and Booth 2008; Urbina and Jones 2004; Volkow et al. 2007). Synthetic drug users thereby expose themselves to risk of acquiring HIV and other sexually transmitted infections (STIs) via heterosexual or homosexual contact (see Chaps. 7 and 8 for more information). The remainder of this chapter will focus on PWID who use traditional opioid drugs (e.g., heroin) and address how opioid substitution therapy has been used as a harm reduction strategy among PWID to combat China’s HIV epidemic.
3 HIV Among PWID
In 1989, the first outbreak of HIV was found among 146 PWID in remote, rural southwestern Yunnan province near the border of Myanmar (Ma et al. 1990; Shao et al. 1991; Zheng et al. 1994). Since then, the HIV epidemic has spread at an alarming rate from Yunnan to other neighboring provinces including Sichuan, Guangxi, Guangdong, and Xinjiang along drug trafficking routes (Sun et al. 2007). As of 2002, all 31 provinces in mainland China have reported cases of HIV infection associated with injecting drug use (State Council AIDS Working Committee Office and the United Nations Theme Group on HIV/AIDS in China 2004).
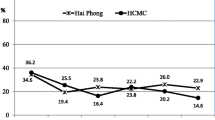
According to sentinel surveillance data collected annually from 1998 to 2004, HIV prevalence among PWID in China’s five most affected provinces—Yunnan, Guangxi, Sichuan, Xinjiang, and Guangdong—ranged from 20% to 30%, while in all other provinces during the same period ranged from 2% to 5%. Overall, HIV prevalence among all PWID nationwide reached a peak of 11% in 2004 (Wang et al. 2015). By 2004, a cumulative total of approximately 100,000 HIV cases had been reported, 42% of which were among PWID (Chinese Center for Disease Control and Prevention 2004).
3.1 The Benefits and Barriers of Harm Reduction for PWID
Drug abuse poses serious problems for communities, families, and individuals. Solutions sometimes seem uncertain, difficult, and controversial. This was the case for opioid substitution therapy as a means of reducing the harms faced by PWID in China.
Since Dole and Nyswander introduced orally administered maintenance doses (80–120 mg) of methadone as a drug substitution treatment for opioid addiction in 1960s (Ausubel 1966), methadone maintenance treatment (MMT) quickly became the most common model of drug replacement therapy for opioid dependence in the world. MMT has helped millions of people in recovery from opioid addiction, allowing them to improve their health, resume their family and social lives, hold steady jobs, and generally become productive members of their communities.
Although the many benefits of MMT have been adequately documented (Fiellin et al. 2001; Langendam et al. 1999; Ward et al. 1999), there were several barriers associated with introducing MMT to China. Internationally, it is now widely accepted that drug addiction is essentially a chronic condition, which has physical, social, cultural, and legal consequences. However, traditionally, the notion that illicit drug use is a failure of willpower or a flaw of moral character rather than a chronic medical condition is deeply rooted in Chinese society. Opponents argued that MMT is unacceptable because it simply “replaces one drug of dependence with another” and insisted that abstinence is the only acceptable treatment goal. Some public officials, especially law enforcement officials, held the view that allowing the long-term medical use of methadone was condoning drug use. Consequently, law enforcement officials believed that tackling the drug use problem through punitive measures, such as incarceration and detoxification, was the only right course to take (see Chap. 19 for more information).
3.2 Toward a More Supportive Policy Environment
To convince government officials, and especially law enforcement officials, to be open to the idea of MMT as a harm reduction method for reducing HIV/AIDS and drug use-related crimes, public health experts from the National Center for AIDS/STD Prevention and Control (NCAIDS), Chinese Center for Disease Control and Prevention (China CDC), took the bold step of exploring the feasibility and effectiveness of initiating an MMT program in China. With support from international organizations including the World Health Organization (WHO), the United Nations (UN), and the World Bank, several workshops, conferences, and seminars were held to establish a platform for discussing the feasibility of MMT in the Chinese political and cultural context (Yin et al. 2010). Study tours for government officials from multiple sectors were organized in Australia, the Netherlands, the United Kingdom, and the United States to provide opportunities to see and hear from those involved in MMT programs in other settings. These tours improved key officials’ perception of MMT and other harm reduction strategies (Wu et al. 2007; Yin et al. 2010).
By the late 1990s and early 2000s, senior-level officials within various arms of the Chinese Central Government were becoming more aware of the seriousness of the nation’s HIV epidemic and of the urgent need for a more comprehensive response. Thus, a policy environment more supportive of innovative new strategies and alternative approaches, such as harm reduction strategies, was developing. Representatives from multiple sectors—the Ministries of Health, Finance, Public Security, and Justice, as well as the Development Commission—met to discuss the idea of introducing harm reduction interventions including MMT, needle and syringe exchange, and condom use promotion. The group decided to take the next steps toward formulation of policies endorsing these measures and supporting the conduct of small pilot studies. Thus, harm reduction was included as an important component in China’s First 5-Year Action Plan for the Containment and Control of HIV/AIDS (2001–2005; State Council 2001; Sun et al. 2010) (see Chap. 18 for more information).
4 MMT’s Pilot Phase
In 2002, the National Working Group for Community-based Methadone Maintenance Treatment for Opioid Users (hereafter the National Working Group) was chartered and tasked with creating a plan for an MMT program in China as well as coordinating and overseeing execution of that plan and evaluating the resulting MMT program structure. It was composed of officials from the Ministry of Health, Ministry of Public Security, and State Food and Drug Administration (SFDA), as well as experts on opioid addiction and HIV. NCAIDS served as the secretariat for the National Working Group, carrying out the plan, providing technical support to MMT clinics, and conducting monitoring and evaluation activities. The resulting national MMT protocol was formalized in 2003, when the Ministry of Health, the Ministry of Public Security, and the SFDA jointly issued the Temporary Protocol for Community-Based Maintenance Treatment for Heroin Addicts (Ministry of Health et al. 2006; Yin et al. 2010).
The protocol detailed the purchase of raw materials and production, storage, transport, distribution, and security of methadone to ensure safety, quality, and security. The protocol outlined eligibility criteria for participation in MMT program (i.e., several failed attempts to stop the use of heroin, at least two terms in a compulsory detoxification center or one term in a reeducation-through-labor camp, at least 20 years of age, a local resident where the clinic was located, and capable of “complete civil liability,” meaning having ability to take responsibility one’s own actions). An exception to most of these criteria was made for drug users with HIV. The protocol also included operating guidelines and requirements for MMT clinics and stipulated that the daily cost per drug user client could not exceed 10 RMB (the equivalent at that time of 1.20 USD), irrespective of dose. Clients were permitted to miss a maximum of 15 days in a 3-month period. Failure to obey MMT program rules and failure to follow clinic doctors’ directions, which included maintaining abstinence from opioid use while in treatment, resulted in expulsion from the program (Ministry of Health et al. 2006; Yin et al. 2010).
Under the governance of the Ministry of Health, the Ministry of Public Security, and the SFDA, eight pilot MMT clinics were opened in the five provinces with the high prevalence of drug use and HIV infection among drug users—two clinics were located in Sichuan, one in Yunnan, two in Guizhou, one in Guangxi, and two in Zhejiang. All became operational between March and June 2004 (Cao et al. 2013; Pang et al. 2007; Yin et al. 2010). A total of 1029 opioid users were enrolled in pilot MMT clinics at the end of 2004. To monitor the work and assess the effectiveness of the pilot clinics, an information management system was developed by the NCAIDS. This system has since been integrated into China’s National HIV/AIDS Comprehensive Response Information Management System (CRIMS), which has been instrumental in improving the quality and timeliness of data on the National MMT Program (as well as all other HIV response programs), facilitating program monitoring and evaluation as well as targeted improvements in services (Mao et al. 2010) (see Chap. 24 for more information).
At 1 month, 6 months, and 12 months after starting treatment, MMT clients at the eight pilot clinics were surveyed on changes in drug using behaviors, drug-related criminal activity, employment, and relationships with family members. Sociodemographic data were kept up-to-date and HIV serostatus was assessed as well. Through this evaluation, researchers found that MMT clients engaged in less injecting drug use and crime and experienced improved family relationships and individual social functioning after an adequate daily dose (usually 60–120 mg) was attained. Reduced rates of HIV were also observed. The pilot study had successfully demonstrated the feasibility, safety, and benefits of MMT in the China setting (Pang et al. 2007).
5 MMT Scale-Up
With the pilot deemed a success, China’s first national MMT conference was convened in Sichuan in 2004 for the purpose of sharing experiences, troubleshooting problems, and advocating for rapid nationwide scale-up. Government officials from the three governing ministries (i.e., Health, Public Security, and SFDA), drug use and HIV experts, and key staff from each of the eight pilot clinics participated.
At the end of 2004, the support for MMT was further bolstered among policymakers when Vice-Premier Wu Yi recommended MMT be scaled up in regions with serious HIV epidemics in a speech at the State Council Special Assembly on HIV/AIDS Prevention and Control. Early in 2006, China’s State Council issued the HIV/AIDS Prevention and Treatment Regulation, which specifically endorsed the use of MMT as an important harm reduction measure (State Council 2006a; Sun et al. 2010; Yin et al. 2010). In the same year, the Second 5-Year Action Plan for the Containment and Control HIV/AIDS (2006–2010) was issued, and specific targets for scaling up MMT were included (State Council 2006b; Sun et al. 2010; Yin et al. 2010).
The National Working Group and NCAIDS immediately got to work scaling up the MMT program nationwide—they were under enormous pressure to meet an ambitious target of opening 300 clinics by the end of 2006. The team successfully opened a total of 320 clinics, which, by the end of 2006, were serving 37,345 drug users. Based on lessons learned from the pilot phase, the National Working Group revised the temporary MMT protocol, and in mid-2006, China’s National Protocol for Community-Based Methadone Maintenance Treatment for Opioid Addicts was issued. The new protocol featured several important changes that intended to expand coverage and improve service quality. First, clients were no longer required to have failed attempts to quit using drugs and a history of detoxification. Second, clients were no longer required to have local registrations, and a transfer system was developed to manage clients who were relocating. Third, rules for clients in the program were made more tolerant and grounds for expulsion were limited. Fourth, a detailed clinical guideline for delivery of methadone treatment was added to support standardized clinical practice. Fifth, comprehensive interventions were added, including ancillary services such as counseling, psychosocial support; testing for HIV, syphilis, hepatitis C virus, and tuberculosis; and referrals to treatment, peer education, health education, group activities, social support, and skills training for employment. Finally, the fee for MMT services was not specified, so that in some areas, where heroin is easily obtained at low cost, the fee could be reduced or even waived (Yin et al. 2010).
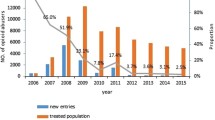
In 2007, the Chinese Central Government again allocated funding to support further expansion of the MMT program, enabling areas with less than 500 registered drug users to establish MMT clinics. A target of 500 MMT clinics was set, and by the end of 2007, a total of 503 MMT clinics were operational in 23 provinces. A cumulative total of 97,554 clients had been served (Yin et al. 2010).
In 2008, the National People’s Congress issued a revised Law on Drug Control, which integrated MMT into existing antidrug strategies, thereby requiring drug users to undergo community-based drug treatment, rather than closed-setting, compulsory detoxification (Standing Committee of the National People’s Congress of China 2008). The revised law also stipulated that drug users in community-based treatment were to be provided with vocational training and employment assistance. Moreover, the law directed “the health sectors of provinces, autonomous regions and municipalities to cooperate with the Public Security Bureau and the Food and Drug Administration to implement community-based MMT.” This important legislation was critical to the long-term sustainability of MMT in China (Yin et al. 2010).
Today, China’s National MMT Programs is the single largest opioid substitution therapy program in the world. As of the end of 2015, a total of 785 full-service “bricks and mortar” clinics were operating across the country. These clinics further support 29 mobile vans and 325 satellite sites, which enable drug users in remote, rural areas and in smaller villages and towns to access methadone. Since 2011, this network has been providing methadone services to approximately 200,000 drug users each year. At the end of 2015, roughly 170,000 former PWID were regular clients of China’s National MMT Program (Wu and Pisani 2017).
6 China’s National MMT Program
6.1 Program-Level Organization and Management
The National MMT Program is managed at both the national and provincial level, with working groups established at each. The National Working Group consists of the National Health Commission (formerly the Ministry of Health), the Ministry of Public Security, the SFDA, as well as relevant technical agencies. It is responsible for overall management of the program, oversight of the methadone supply chain, training of key staff at the provincial level, and monitoring and evaluation of the program at the national level. The National Working Group secretariat, NCAIDS, is responsible for the coordination and routine administration of the program. The Provincial Working Groups consist of the provincial-level officials affiliated with the agencies included in the National Working Group. Provincial Working Groups are responsible for organizing, administering, supervising, and providing MMT program services in their province. The secretariat of each Provincial Working Group is responsible for routine operation and monitoring.
6.2 Clinic-Level Organization and Management
Clinics can be affiliated with a local CDC site, community hospital, mental health center, community-based health center, voluntary detoxification center, or penal system-based hospital. Currently, a majority of clinics are affiliated with CDCs and hospitals. Each full-service “bricks and mortar” clinic includes several functional areas, such as a counseling room, HIV testing room, and waiting room, which are equipped with computers, telephones, Internet connections, and methadone dispensing equipment and supplies. Each clinic has at least eight trained staff members, including at least two doctors and two nurses. At least two staff members from each MMT clinic are required to participate in a 10-day training course held by the national MMT training center covering addiction theory, clinical practice, and administrative skills for delivery of MMT services prior to the opening of clinic.
Methadone is supplied to each clinic based on the clinic’s actual demand as evaluated by the Provincial Working Group—clinics are prohibited from obtaining methadone from any other source. The Provincial Working Group must request quantities of methadone from the National Working Group. Clinics are responsible for managing their own methadone supplies under the strict oversight of both the Provincial Working Group and the National Working Group.
Although the ideal clinic size is approximately 300 clients, clinics vary considerably in size, from a few dozen to nearly 1500 clients (average is approximately 250 clients per clinic). The program follows an outpatient model—clients attend clinics daily to obtain their methadone dose, which is taken under the direct observation of clinic staff. There are no options for take-home doses nor any way to obtain methadone outside the clinics. The daily dose recommended by China’s MMT protocol is 80–120 mg.
Clients are charged a maximum of 10 RMB (roughly 1.5 USD) per day for treatment received regardless of the dose. Although the National MMT Program is funded by the Chinese Central Government via the National Health Commission in collaboration with the Ministry of Public Security and the SFDA and provincial and local governments allocate funds for the establishment of clinics, these funders do not cover regular operating costs. Day-to-day operations are funded by client treatment fees.
MMT clinics are responsible not only for administering the program, supervising the routine treatment of clients, and reporting on operational progress in a timely manner but also for educating clients about risk reduction, providing psychological support, and providing disease prevention consultations, urine tests, and medical management.
6.3 Client Enrollment and Treatment
When an opioid user approaches an MMT clinic to seek treatment, they are informed of the treatment procedure and expectations of clients. If the prospective client chooses to enroll, then he or she is asked to provide written informed consent for treatment. Upon enrollment of a new client, the MMT clinic is obliged to notify the relevant narcotics control department of the local Public Security Bureau branch.
Before treatment starts, the new client is provided a standardized card identifying their participation in the MMT program and is entered into a baseline assessment. The baseline assessment consists of the collection of identification, contact, and sociodemographic information as well as information on historical and current drug use behavior, high-risk sexual behavior, and health and sexual health history. Then, clients provide a blood sample for HIV and HCV testing. The results of these tests become a part of the client’s baseline data. All clients who are found to have HIV and/or HCV infection are referred to treatment.
Clinic doctors are responsible for the initiation of methadone treatment according to current clinical guidelines. The clinic doctor then may adjust the client’s dose in accordance with their response to treatment, and an individualized methadone treatment protocol should be developed and adjusted until the correct maintenance dosage is determined. Once on a maintenance dose, daily doses may be administered by clinic nurses or pharmacists depending on the clinic.
Since MMT clients are prohibited from using opioids or any other kinds of illegal drugs while in MMT, clients receive urine drug-screening tests on a regular and irregular basis. Urine tests are administered and results recorded by clinic doctors. Other clinic staff are not permitted to administer urine drug tests.
Transfers between clinics are permitted and are facilitated by a proximity card system, which was introduced in 2008. This system enables clients to obtain methadone when they move or travel. MMT clients may choose to discontinue treatment via an application process. Discontinuation applications are approved by the local branch of the Public Security Bureau.
6.4 Data Management
Client information is confidential and is therefore securely stored. MMT clinics are strictly prohibited from releasing confidential client information to any institution or individual without the permission of the client, unless they are required to do so by law. To securely store and restrict access to client, clinic, and program information, China’s MMT Data Management System was developed and launched simultaneously with the opening of the first eight MMT clinics in 2004. The system has since been upgraded and integrated into CRIMS as of early 2008. Because Internet outages remain a challenge in some areas, the system was designed to allow for off-line data entry by MMT staff using client software. Data are then uploaded to CRIMS when the terminals are back online (Mao et al. 2010).
Each patient is given a unique treatment number upon entry into the MMT program and each clinic uploads its daily service records to the system in real time. Data collected include that generated from enrollment and the baseline assessment (e.g., identification, contact, and sociodemographic information) as well as treatment initiation and daily visits to obtain methadone doses. Daily methadone dose records, results of urine drug-screening tests, and results of HIV and HCV tests at entry, 6 months, 12 months, and then at 12-month intervals thereafter are entered into the system. In addition, if clients discontinued taking methadone for 30 consecutive days or died, reasons for dropout and causes of death were collected (see Chap. 24 for more information).
6.5 Staff Training and Capability Building
With approval by the National Working Group, the National MMT Training Center was set up at the Yunnan Institute of Drug Abuse in 2005. The mission of the National MMT Training Center was to offer providers in new MMT clinics basic support and clinical and operational training. At least two staff members from each MMT clinic were required to participate in a 10-day training course at the center covering addiction theory, clinical practice, and administrative skills for the delivery of MMT services prior to the opening of each clinic. To assist the staff of a newly opened clinic, the center provided onsite training for the first 7 days of operation to guide them in the practice of addiction treatment and data management (Li et al. 2013).
In 2008, the National MMT Training Center modified its capacity-building programs after performing a situational analysis and skills and capacity assessment of existing clinics (Li et al. 2013). The new technical training program for MMT service providers covers a broader range of topics and is meant to better strengthen their skills and ability to offer quality services. In addition, the center trains core MMT providers to themselves be trainers, so that they can provide training to staff at other clinics in their province and conduct week-long field visits to new clinics to provide on-site technical support and performance coaching to new service providers (see Chap. 27 for more information).
7 Evaluations of the National MMT Program
According to official government statistics, as of the end of 2014, a total of 767 MMT clinics were operating in 28 provincial-level administrative regions, treating 184,000 regular, active clients, and having a major impact on China’s HIV epidemic (National Health and Family Planning Commission 2015). HIV incidence declined by 80% among MMT clients from 2006 to 2013, suggesting an estimated 13,000 new HIV infections were averted by the program. Among all newly diagnosed HIV cases nationwide, the proportion attributed to injecting drug use fell from 44% in 2003 to under 8% in 2013. Furthermore, sentinel surveillance data indicate that HIV prevalence among drug users fell from 7.5% in 2005 to 3.6% in 2013 (World Health Organization China Office 2014).
Many observational studies have also been conducted to evaluate the performance of the National MMT Program and to investigate MMT client outcomes. This effort has been greatly facilitated in more recent years by CRIMS (Mao et al. 2010). The open cohort of MMT clients whose demographic, behavioral, health, and treatment data are contained within CRIMS is the largest in the world, making it a very powerful tool for examining a broad range of MMT-related questions. A selection of these observational studies are highlighted here. Overall, both government figures and results of observational studies alike point to benefits of MMT for opioid drug users across a broad range of outcomes.
7.1 Evaluation of the Pilot
To evaluate the MMT program while still in its pilot phase, Pang et al. conducted three successive cross-sectional studies at the eight pilot clinics (Pang et al. 2007). The first was in April to August 2004 among 585 clients who had been in MMT 1 month. The second was in December 2004 among 609 clients who had been in MMT at least 4 months. And the third, was in September to November 2005 among 468 clients who had been retained at least 12 months. Each study consisted of an interview and HIV testing was performed at 1 month and at 12 months.
Drug injecting in the past 1 month declined from nearly 70% to less than 10%, and among those who continued drug injection behavior, frequency of injecting declined from an average of 90 times per month to 2 times per month. Employment climbed from 23% to above 40%. Self-reported engagement in criminal activity fell from 21% to under 4%. Harmonious relationships with family members were reported by 66% after 12 months compared to 50% at 1 month. Although client satisfaction was also found to be above 95%, program dropout rate was nearly 52% at 12 months. Among clients who dropped out, 31% had been arrested and/or were incarcerated, 12% had moved away, and 12% had been disqualified. By the time of the third survey, a total of 3069 clients had cumulatively been tested for HIV. While 78% had been found to have HIV infection already upon enrollment, a seroconversion rate of only 0.7% in 12 months was found among those who entered MMT without HIV infection (Pang et al. 2007).
7.2 Evaluation of Client Characteristics
Sullivan et al. conducted a retrospective descriptive analysis of MMT client characteristics among all clients who enrolled in treatment in the 6-year period between March 2004 and March 2010 (Sullivan et al. 2015). During this time, a total of 684 clinics were operating in 27 provinces. All routinely collected program data on the 251,974 clients ever enrolled during this time were examined. Overall, mean age of clients was 34 years, 84% were male, 70% were unemployed, 75% had a lifetime history of drug injecting, 17% had a lifetime history of needle sharing, and 7.4% had HIV infection. Over time, fewer clients were female, were unemployed, reported drug injecting, reported needle sharing, and had HIV infection. The 6-month dropout rate was roughly 50%, with median time to first treatment interruption of 162 days (Sullivan et al. 2015).
7.3 Evaluations of Retention
A systemic review and meta-analysis of 74 studies of MMT in China between January 2004 and April 2013 found that approximately one-third of clients drop out of treatment within the first 3 months after enrollment. Among those who dropped out, the most frequent reason was arrest or incarceration (22%). Among those who were retained, 25% had a positive urine drug-screening results, 9% still injected drugs, and 1% sold sex for drugs at 12 months (Zhang et al. 2013).
Cao et al. conducted a 6-year cohort study of 1511 MMT clients attending the first eight clinics in the program beginning in March 2004. Overall 6-year retention rate was 36%. Highest dropout rates were found within the first 12 months of enrollment and among those with the lowest methadone doses. Clients that had daily methadone doses above 30 mg or had relatives who were also in MMT had better odds of being retained and having a history of drug injecting or needle sharing behavior was also associated with improved retention (Cao et al. 2014).
To date, there are many smaller studies of MMT retention and although retention rates do vary considerably, the remain persistently low overall.
7.4 Evaluations of Comorbidities
A broad range of studies in the literature today examine various comorbidities including mental illnesses, blood-borne infections, and sexually transmitted infections as well as other harms. Overall, MMT has been shown to improve the health of drug users.
A cross-sectional study of 1301 MMT clients attending nine clinics across three provinces from 2008 to 2009 found that the prevalence of depression was 38% and the prevalence of anxiety was 18% with 14% of participants displaying symptoms of both depression and anxiety. Multilevel mixed modeling found a significant association between employment status and depression and between employment status and positive urine drug-screening results and anxiety (Yin et al. 2015).
A systemic review and meta-analysis of 90 studies (primarily in Chinese) published between 2004 and 2010 found that the overall national prevalence of HIV among MMT enrollees at baseline was 6%, prevalence of HCV was 60%, and HIV/HCV coinfection was 5%. Although large geographic variation was noted, no significant difference in prevalence of HIV, HCV, or HIV/HCV coinfection was observed over time (Zhuang et al. 2012).
A nationwide study of 296,209 MMT clients who enrolled between March 2004 and December 2012 found an overall HCV prevalence of 55% at baseline and documented a notable decline in prevalence over the study period from 67% in 2005 to 46% in 2012. Those with a history of injecting drug use had an eight-fold greater risk of HCV infection and those with a 9-year or longer history of drug use had a two-fold greater risk of HCV. Substantial geographical heterogeneity was observed in HCV prevalence (Wang et al. 2016).
A systemic review and meta-analysis of 29 studies reporting syphilis infection among MMT clients in China documented a pooled syphilis prevalence of 7.8%. However, substantially greater prevalence of syphilis was found among women compared to men (Wang et al. 2014).
A 7-year retrospective cohort study (2006–2014) of 9240 clients attending 14 MMT clinics in Guangdong province found an overall HIV seroconversion rate of 0.2 per 100 person-years (PY), an HCV seroconversion rate of 20.5 per 100 PY, and a syphilis seroconversion rate of 0.8 per 100 PY. A significant 16% per year decline was observed in the HCV seroconversion rate during the study period. HIV seroconversion was associated with positive urine drug-screening results. Factors associated with HCV seroconversion were unmarried status, injection drug use in the past month, sex in the past 3 months, and higher methadone dose. Being female and having HCV infection at time of MMT enrollment were associated with syphilis seroconversion (Zou et al. 2015).
7.5 Evaluations of Mortality
Cao et al. conducted a 6-year cohort study (2004–2010) among 1511 enrollees in the first eight MMT clinics and found an all-cause mortality rate of 28.6 per 1000 PY (Cao et al. 2013). Most frequent causes of death were drug overdose (34%), HIV/AIDS-unrelated disease (21%), and HIV/AIDS (17%). Risk of death was five-fold greater for clients with HIV infection. Longer duration of retention in MMT was protective against death—clients retained 2–3 years experienced four-fold lesser risk of death and clients retained 4 or more years a ten-fold lesser risk. Furthermore, clients who had HIV infection and remained untreated had two times greater risk of death than those who were on treatment (Cao et al. 2013).
Zhao et al. investigated a nationwide cohort of 23,813 PLWH who reported having become infected via injecting drug use and who received ART between December 2002 and December 2011. The main finding was significantly lower mortality among those who were in MMT (66 per 1000 PY at 6 months, 37 per 1000 PY at 12 months) compared to those who were not in MMT (169 per 1000 PY at 6 months, 74 per 1000 at 12 months). Significant predictors of death were having never received MMT, having a low hemoglobin level, having a low CD4 count, and receiving treatment in settings other than infectious disease hospitals (Zhao et al. 2013).
Liu et al. extracted 306,786 MMT records of clients enrolled in MMT from 2004 to 2011 and found an overall mortality rate of 12 per 1000 PY but 57 per 1000 PY among those who had HIV infection. Methadone doses above 75 mg were associated with a 24% reduction in mortality, and this reduction in mortality was even greater among clients with HIV infection, nearly 50% (Liu et al. 2013).
Zhou et al. examined mortality among 1188 clients at a single clinic in Yunnan over 11 years of follow-up (2004–2015) and found an overall all-cause mortality rate of 34.2 per 1000 PY. Being married, being employed, and having longer MMT retention were all protective factors. HIV infection was a risk factor for death (43% increased risk of death), and the leading cause of death was HIV/AIDS-related causes (53%). Among those with HIV infection, being on treatment was a protective factor and was associated with a four-fold reduction in risk of death (Zhou et al. 2019).
7.6 Other Evaluations
A nationwide retrospective study of 19,026 MMT clients enrolled between April 2008 and March 2010 and retained at least 6 months found that self-reported rates of drug use and drug use-related high-risk behavior declined, and social functioning improved. Upon entry into MMT, 98% of clients had a positive urine drug-screening result, and nearly 100% self-reported drug use in the prior month. By contrast, at 6-month follow-up, 28% had a positive urine drug-screening result and 25% self-reported drug use in the prior month. Greater odds of continued drug use was found among those who had low attendance, reported often seeing drug-using friends, and reported having difficult family relationships. No association was found between continued drug use and methadone dose (Sullivan et al. 2014).
A systematic review and meta-analysis of 38 studies, primarily published in Chinese, found that a broad range of outcomes improved among MMT clients retained at least 6 months compared to baseline. For example, self-reported arrest rate declined from 13% to under 4% and drug-related crime from 10% to 3%. Selling drugs declined from 8% to 3% and selling sex for drugs declined from 5% to 1%. Employment rates rose from 26% to 40% at 6 months and to 60% at 12 months, and the proportion of clients reporting good relationships with family climbed from 40% to 60% at 6 months and to 75% at 12 months (Sun et al. 2015).
8 Challenges and Future Directions
The rapid scale-up of MMT programs in China has benefited hundreds of thousands of drug users, reducing drug use and criminality and improving health, quality of life, social functioning, and productivity. Nonetheless, there are still a wide range of challenges and gaps remaining, which need to be addressed if China is to further improve upon its already impressive National MMT Program.
8.1 Coverage
Despite China’s National MMT Program being the largest in the world with 785 full-service clinics, 29 mobile vans, and 325 satellite sites serving roughly 200,000 clients each year as of the end of 2015 (Wu and Pisani 2017), coverage remains low. According to data released by China’s National Narcotic Control Commission, there were more than 1.27 million registered opioid drug users in China as of the end of 2012 (National Narcotics Control Commission 2013). However, the true number of opioid users in China is known to be much larger and is thought to be still growing. China must again prioritize scale-up of MMT and find new, innovative ways to improve coverage. China must not allow the program to stagnate in the face of an ever-growing and ever-changing drug-using population.
8.2 Retention
Even during the pilot of the MMT program, client retention was a serious challenge (Pang et al. 2007), and it remains so today (Cao et al. 2014; Sullivan et al. 2015; Zhang et al. 2013). Barriers to retention have been well studied and include low methadone doses, clinic accessibility, treatment interruption caused by incarceration, lack of psychosocial support within clinics, concurrent drug use, and misconceptions of clients and providers about methadone treatment goals (Cao et al. 2014; Lin and Detels 2011; Liu et al. 2009; Zhang et al. 2013).
8.2.1 Methadone Dose and Retention
Internationally, a high daily methadone dose (80–120 mg) has been recognized as an important predictor of long-term retention. Many randomized controlled trials and observational studies have clearly demonstrated that higher dosages resulted in longer duration of treatment as well as less concurrent drug use and criminal activity (Kerr et al. 2005; Liu et al. 2006; Peles et al. 2006; Strain et al. 1999). While a majority of clients require at least 60 mg/day, a dose of 80–100 mg or greater is even more strongly correlated with positive outcomes (Joseph et al. 2000). Within China’s National MMT Program, methadone dose is low overall and higher doses have been associated with better retention in care (Cao et al. 2014; Pang et al. 2007; Sullivan et al. 2015; Zhou and Zhuang 2014). Client retention is in urgent need of improvement and fulling understanding the reasons behind low doses, and addressing them is a critical part of solving the poor retention problem.
8.2.2 Police Action and Retention
The historically opposing missions of the public health and public security arms of the Chinese government—one tasked with treating substance use disorder, the other tasked with punishing drug users—have had a negative impact on many MMT clients since the start of the National MMT Program. Diversion of drug users to detention in compulsory detoxification centers or reeducation-through-labor camps rather than to MMT and failure to refer drug users released from these settings to MMT result in considerable lost opportunities to treat underlying substance use disorder. Fear of incarceration discourages enrollment among those who are not yet the target of police action, and arrest and incarceration after MMT enrollment causes treatment interruption. Although cooperation between MMT clinics and local narcotics control and public security forces has improved over time in China, progress has been difficult and slow (Meng and Burris 2013). Improved awareness and knowledge of substance use disorder and MMT is urgently needed among law enforcement in China (see Chap. 19 for more information).
8.3 Service Quality
Wide variations in program effectiveness have been observed between different MMT clinics, which may be correlated with factors such as clinic location, clinic organizational structure, characteristics of clinic staff and their work environment, and the quality of services provided by clinic staff. Further research is needed to explore potential impact of program factors on effectiveness.
8.3.1 Provider Capacity
Although MMT service providers standardly receive related MMT training prior to and after the opening of the MMT clinics, their knowledge and skills in addiction treatment and clinic management may be inadequate. A range of studies have suggested that misunderstanding about the goals of MMT as well as confusion regarding treatment for clients concurrently on treatment for comorbid conditions such as HIV, HCV, tuberculosis, or mental illness may negatively impact methadone prescribing practices and, ultimately, retention. Studies have also documented job dissatisfaction among MMT providers and negative attitudes toward clients, both of which can cause service quality and client retention to suffer. Furthermore, providers have provided feedback on lack of sufficient training, understaffed clinics, high staff turnover rates, unmanageable workloads, lack of respect from fellow medical professionals in other specialties, and concerns for malpractice liability, personal safety, and burnout (Li et al. 2013; Lin et al. 2010).
Good client-provider relationships are known to be correlated with long-term retention and the positive outcomes. Unlike patients in hospitals or medical clinics, MMT clients come to clinics routinely, every day, for a short time to receive their methadone dose. Unless special counseling or consultation sessions are scheduled, providers normally interact only briefly with clients. Thus, the short, perfunctory nature of the typical client-provider interaction during MMT administration can become a barrier to effective development of rapport. One study in China has found that providers with strong negative attitudes were less likely to interact with their clients, suggesting that providers’ general attitudes toward drug users could strongly influence client perceptions of service quality and thereby retention (Li et al. 2012).
Clearly, there is a need for building capacity among MMT service providers and for addressing issues related to job satisfaction in order to improve service quality (see Chap. 27 for more information).
8.3.2 Ancillary Integrated Services
An emerging body of research both internationally and in China has suggested that substance use treatment programs could be a platform for assisting drug users who have HIV infection with overcoming the many barriers they face with respect to linkage and retention in HIV care. Moreover, MMT clinic-based ART services may be an effective strategy to promote treatment adherence, encourage follow-up visit attendance, and achieve improved outcomes for this extremely vulnerable population. Because MMT clients are regularly in contact with the health system for daily administration of methadone and receive ongoing counseling on risk behavior reduction and the importance of treatment adherence, MMT clinics offer a unique opportunity for drug users to also receive HIV-related diagnostic, treatment, and follow-up services. A small, preliminary study suggests that MMT clients with HIV infection would accept integrated MMT/ART services but note concerns about privacy and confidentiality as well as service provider training and experience (Lin et al. 2017). More study will be required to develop a service model that makes sense and can be effective in China setting, and capacity building among staff will be crucial (see Chap. 13 for more information).
9 Conclusion
Since the reemergence of drug use and the identification of the initial outbreak of HIV among injecting drug users, China has taken an active, pragmatic approach in response, resulting in a substantial decline in HIV epidemic among this population. The rapid nationwide scale-up of MMT has been the cornerstone of the response to the epidemic among PWID. To maintain China’s successes in controlling the epidemic among PWID, the National MMT Program must be strengthened to fill service gaps and meet the evolving needs of clients. Future efforts must address low program coverage, poor retention, and uneven service quality, and research is needed to inform the implementation of solutions to these problems as well as the addition of ancillary and integrated services such as ART.
References
Ausubel DP. The Dole-Nyswander treatment of heroin addiction. JAMA. 1966;195(11):949–50. https://doi.org/10.1001/jama.1966.03100110117032.
Brugal M, Domingo-Salvany A, Puig R, Barrio G, García de Olalla P, de la Fuente L. Evaluating the impact of methadone maintenance programmes on mortality due to overdose and AIDS in a cohort of heroin users in Spain. Addiction. 2005;100(7):981–9. https://doi.org/10.1111/j.1360-0443.2005.01089.x.
Cao XB, Wu ZY, Li L, Pang L, Rou K, Wang C, et al. Mortality among methadone maintenance clients in China: a six-year cohort study. PLoS One. 2013;8(12):e82476. https://doi.org/10.1371/journal.pone.0082476.
Cao X, Wu Z, Rou K, Li L, Lin C, Wang C, Luo W, et al. Retention and its predictors among methadone maintenance treatment clients in China: a six-year cohort study. Drug Alcohol Depend. 2014;145:87–93. https://doi.org/10.1016/j.drugalcdep.2014.09.776.
Chinese Center for Disease Control and Prevention. National sentinel surveillance report of HIV infection, 2004. Beijing: Chinese Center for Disease Control and Prevention; 2004.
Corsi KF, Booth RE. HIV sex risk behaviors among heterosexual methamphetamine users: literature review from 2000 to present. Curr Drug Abuse Rev. 2008;1(3):292–6. https://doi.org/10.2174/1874473710801030292.
Degenhardt L, Hall W, Warner-Smith M. Using cohort studies to estimate mortality among injecting drug users that is not attributable to AIDS. Sex Transm Infect. 2006;82(Suppl 3):iii56–63. https://doi.org/10.1136/sti.2005.019273.
Fang YX, Wang YB, Shi J, Liu ZM, Lu L. Recent trends in drug abuse in China. Acta Pharmacol Sin. 2006;27:140–4. https://doi.org/10.1111/j.1745-7254.2006.00270.x.
Fiellin DA, O’Connor PG, Chawarski M, Pakes JP, Pantalon MV, Schottenfeld RS. Methadone maintenance in primary care: a randomized controlled trial. JAMA. 2001;286(14):1724–31. https://doi.org/10.1001/jama.286.14.1724.
Hulse GK, English DR, Milne E, Holman CD. The quantification of mortality resulting from the regular use of illicit opiates. Addiction. 1999;94(2):221–9. https://doi.org/10.1046/j.1360-0443.1999.9422216.x.
Jia Z, Liu Z, Chu P, McGoogan JM, Cong M, Shi J, et al. Tracking the evolution of drug abuse in China, 2003–10: a retrospective, self-controlled study. Addiction. 2015;110(Suppl 1):4–10. https://doi.org/10.1111/add.12769.
Joe Laidler KA. The rise of club drugs in a heroin society: the case of Hong Kong. Subst Use Misuse. 2005;40(9–10):1257–78. https://doi.org/10.1081/JA-200066788.
Joseph H, Stancliff S, Langrod J. Methadone maintenance treatment (MMT): a review of historical and clinical issues. Mt Sinai J Med. 2000;67(5–6):347–64.
Kerr T, Marsh D, Li K, Montaner J, Wood E. Factors associated with methadone maintenance therapy use among a cohort of poly-substance using injection drug users in Vancouver. Drug Alcohol Depend. 2005;80(3):329–35. https://doi.org/10.1016/j.drugalcdep.2005.05.002.
Langendam MW, van Brussel GH, Coutinho RA, van Ameijden EJ. Methadone maintenance treatment modalities in relation to incidence of HIV: results of the Amsterdam cohort study. AIDS. 1999;13(13):1711–6.
Li J, Ha TH, Zhang C, Liu H. The Chinese government’s response to drug use and HIV/AIDS: a review of policies and programs. Harm Reduct J. 2010;7:4. https://doi.org/10.1186/1477-7517-7-4.
Li L, Wu Z, Cao X, Zhang L. Provider-client interaction in methadone treatment clinics in China. J Drug Issues 2012;42(2). https://doi.org/10.1177/0022042612446593.
Li J, Wang C, McGoogan JM, Rou K, Bulterys M, Wu Z. Human resource development and capacity-building during China’s rapid scale-up of methadone maintenance treatment services. Bull World Health Organ. 2013;91(2):130–5. https://doi.org/10.2471/BLT.12.108951.
Lin C, Wu Z, Rou K, Pang L, Cao X, Shoptaw S, et al. Challenges in providing services in methadone maintenance therapy clinics in China: service providers’ perceptions. Int J Drug Policy. 2010;21(3):173–8. https://doi.org/10.1016/j.drugpo.2009.09.002.
Lin C, Detels R. A qualitative study exploring the reason for low dosage of methadone prescribed in the MMT clinics in China. Drug Alcohol Depend. 2011;117(1):45–9. https://doi.org/10.1016/j.drugalcdep.2011.01.004.
Lin C, Li L, Cao X. Client acceptability for integrating antiretroviral therapy in methadone maintenance therapy clinics in Sichuan, China. Subst Use Misuse. 2017;52(1):119–26. https://doi.org/10.1080/10826084.2016.1222622.
Liu H, Grusky O, Zhu Y, Li X. Do drug users who frequently receive detoxification treatment change their risky drug use practices and sexual behavior? Drug Alcohol Depend. 2006;84(1):114–21. https://doi.org/10.1016/j.drugalcdep.2006.01.004.
Liu E, Liang T, Shen L, Zhong H, Wang B, Wu Z, et al. Correlates of methadone client retention: a prospective cohort study in Guizhou province, China. Int J Drug Policy. 2009;20(4):304–8. https://doi.org/10.1016/j.drugpo.2008.09.004.
Liu Y, Liang J, Zhao C, Zhou W. Looking for a solution for drug addiction in China: exploring the challenges and opportunities in the way of China’s new Drug Control Law. Int J Drug Policy. 2010;21(3):149–54. https://doi.org/10.1016/j.drugpo.2009.10.002.
Liu E, Rou K, McGoogan JM, Pang L, Cao X, Wang C, et al. Factors associated with mortality of HIV positive clients receiving methadone maintenance treatment in China. J Infect Dis. 2013;208(3):442–53. https://doi.org/10.1093/infdis/jit163.
Lu L, Wang X. Drug addiction in China. Ann N Y Acad Sci. 2008;1141:304–17. https://doi.org/10.1196/annals.1441.025.
Lu L, Fang Y, Wang X. Drug abuse in China: past, present and future. Cell Mol Neurobiol. 2008;28(4):479–90. https://doi.org/10.1007/s10571-007-9225-2.
Ma Y, Li Z, Zhang K. HIV was first discovered among injection drug users in China. Chin J Epidemiol. 1990;11:184–5.
Mao Y, Wu Z, Poundstone K, Wang C, Qin Q, Ma Y, et al. Development of a unified web-based national HIV/AIDS information system in China. Int J Epidemiol. 2010;39(Suppl 2):ii79–89. https://doi.org/10.1093/ije/dyq213.
McCowan C, Kidd B, Fahey T. Factors associated with mortality in Scottish patients receiving methadone in primary care: retrospective cohort study. BMJ. 2009;338:b2225. https://doi.org/10.1136/bmj.b2225.
McCoy CB, McCoy HV, Lai S, Yu Z, Wang X, Meng J. Reawakening the dragon: changing patterns of opiate use in Asia, with particular emphasis on China’s Yunnan province. Subst Use Misuse. 2001;36(1–2):49–69.
Meng J, Burris S. The role of the Chinese police in methadone maintenance therapy: a literature review. Int J Drug Policy. 2013;24(6):e25–34. https://doi.org/10.1016/j.drugpo.2013.03.010.
Ministry of Health, Ministry of Public Security, State Food and Drug Administration. Implementation protocol of the community-based methadone maintenance treatment program for opiate addicts in China. Beijing: Ministry of Health, Ministry of Public Security, and State Food and Drug Administration, People’s Republic of China; 2006.
Morgan O, Johnson H, Rooney C, Seagroatt V, Griffiths C. Changes to the daily pattern of methadone-related deaths in England and Wales, 1993–2003. J Public Health (Oxf). 2006;28(4):318–23. https://doi.org/10.1093/pubmed/fdl059.
National Health and Family Planning Commission. 2015 China AIDS response progress report. Beijing: National Health and Family Planning Commission. http://www.commuhealtibet.org/wp-content/uploads/2016/11/CHN_narrative_report_2015.pdf. Accessed 27 Sep 2018.
National Narcotic Control Commission. Annual report on drug control in China. Beijing: National Narcotics Control Commission, People’s Republic of China; 2005.
National Narcotics Control Commission. Annual report on drug control in China. Beijing: National Narcotics Control Commission, People’s Republic of China; 2013.
National Narcotics Control Commission. Annual report on drug control in China. Beijing: National Narcotics Control Commission, People’s Republic of China; 2015.
Pang L, Hao Y, Mi G, Wang C, Luo W, Rou K, et al. Effectiveness of first eight methadone maintenance treatment clinics in China. AIDS. 2007;21(Suppl 8):S103–7. https://doi.org/10.1097/01.aids.0000304704.71917.64.
Peles E, Kreek MJ, Kellogg S, Adelson M. High methadone dose significantly reduces cocaine use in methadone maintenance treatment (MMT) patients. J Addict Dis. 2006;25(1):43–50. https://doi.org/10.1300/J069v25n01_07.
Shao Y, Chen Z, Wang B, Zeng Y, Zhao SD, Zhang ZR. Isolation of viruses from HIV infected individuals in Yunnan. Chin J Epidemiol. 1991;12:129.
Shi J, Zhao LY, Epstein DH, Zhang XL, Lu L. Long-term methadone maintenance reduces protracted symptoms of heroin abstinence and cue-induced craving in Chinese heroin abusers. Pharmacol Biochem Behav. 2007;87(1):141–5. https://doi.org/10.1016/j.pbb.2007.04.010.
Standing Committee of the National People’s Congress of China. Drug control law. Beijing: Standing Committee of the National People’s Congress of China, People’s Republic of China; 2008.
State Council. China’s action plan for reducing and preventing the spread of HIV/AIDS (2001–2005). Beijing: State Council, People’s Republic China; 2001.
State Council. Regulations on AIDS prevention and treatment. Beijing: State Council, People’s Republic of China; 2006a.
State Council. Action plan on HIV/AIDS prevention and containment (2006–2010). Beijing: State Council, People’s Republic of China; 2006b.
State Council AIDS Working Committee Office and the United Nations Theme Group on HIV/AIDS in China. A joint assessment of HIV/AIDS prevention, treatment and care in China. Beijing: State Council AIDS Working Committee Office and the United Nations Theme Group on HIV/AIDS in China; 2004.
Strain EC, Bigelow GE, Liebson IA, Stitzer ML. Moderate- vs high-dose methadone in the treatment of opioid dependence: a randomized trial. JAMA. 1999;281(11):1000–5. https://doi.org/10.1001/jama.281.11.1000.
Sullivan SG, Wu Z. Rapid scale up of harm reduction in China. Int J Drug Policy. 2007;18(2):118–28. https://doi.org/10.1016/j.drugpo.2006.11.014.
Sullivan SG, Wu Z, Cao X, Liu E, Detels R. Continued drug use during methadone treatment in China: a retrospective analysis of 19,026 service users. J Subst Abus Treat. 2014;47(1):86–92. https://doi.org/10.1016/j.jsat.2013.12.004.
Sullivan SG, Wu Z, Rou K, Pang L, Luo W, Wang C, et al. Who uses methadone services in China? Monitoring the world’s largest methadone programme. Addiction. 2015;110(Suppl 1):29–39. https://doi.org/10.1111/add.12781.
Sun X, Wang N, Li D, Zheng X, Qu S, Wang L, et al. The development of HIV/AIDS surveillance in China. AIDS. 2007;21(Suppl 8):S33–8. https://doi.org/10.1097/01.aids.0000304694.54884.06.
Sun X, Lu F, Wu Z, Poundstone K, Zeng G, Xu P, et al. Evolution of information-driven HIV/AIDS policies in China. Int J Epidemiol. 2010;39(Suppl 2):ii4–13. https://doi.org/10.1093/ije/dyq217.
Sun HM, Li XY, Chow EP, Li T, Xian Y, Lu YH, et al. Methadone maintenance treatment programme reduces criminal activity and improves social well-being of drug users in China: a systematic review and meta-analysis. BMJ Open. 2015;5(1):e005997. https://doi.org/10.1136/bmjopen-2014-005997.
United Nations Office on Drugs and Crime. World drug report 2012. Vienna: United Nations Office on Drugs and Crime; 2012.
Urbina A, Jones K. Crystal methamphetamine, its analogues, and HIV infection: medical and psychiatric aspects of a new epidemic. Clin Infect Dis. 2004;38(6):890–4. https://doi.org/10.1086/381975.
Volkow ND, Wang GJ, Fowler JS, Telang F, Jayne M, Wong C. Stimulant-induced enhanced sexual desire as a potential contributing factor in HIV transmission. Am J Psychiatry. 2007;164(1):157–60. https://doi.org/10.1176/ajp.2007.164.1.157.
Wang BX, Zhang L, Wang YJ, Yan JW, Wan YN, Peng WJ, et al. Epidemiology of syphilis infection among drug users at methadone maintenance treatment clinics in China: systemic review and meta-analysis. Int J STD AIDS. 2014;25(8):550–8. https://doi.org/10.1177/0956462413515444.
Wang L, Guo W, Li D, Ding Z, McGoogan JM, Wang N. HIV epidemic among drug users in China: 1995–2011. Addiction. 2015;110(Suppl 1):20–8. https://doi.org/10.1111/add.12779.
Wang C, Shi CX, Rou K, Zhao Y, Cao X, Luo W, et al. Baseline HCV antibody prevalence and risk factors among drug users in China’s National Methadone Maintenance Treatment Program. PLoS One. 2016;11(2):e0147922. https://doi.org/10.1371/journal.pone.0147922.
Ward J, Hall W, Mattick RP. Role of maintenance treatment in opioid dependence. Lancet. 1999;353(9148):221–6. https://doi.org/10.1016/S0140-6736(98)05356-2.
World Health Organization China Office. Reducing harm, preventing HIV, saving lives: China’s vast methadone maintenance treatment program marks successes even as it addresses key challenges ahead. Beijing: World Health Organization China Office; 2014. http://www.wpro.who.int/china/mediacentre/releases/2014/2014112702/en/. Accessed 27 Sep 2018.
World Health Organization, United Nations Office on Drugs and Crime, Joint United Nations Programme on HIV/AIDS. Substitution maintenance therapy in the management of opioid dependence and HIV/AIDS prevention. Beijing: World Health Organization, United Nations Office on Drugs and Crime, Joint United Nations Programme on HIV/AIDS, 2004. http://www.who.int/hiv/pub/idu/position_paper_substitution_opioid/en/. Accessed 19 Sept 2018.
Wu Z, Pisani E. Fulfilling a promise: universal care. In: Wu Z, editor. HIV/AIDS in China—beyond the numbers. Singapore: People’s Medical Publishing House; 2017. p. 78–99.
Wu Z, Sullivan SG, Wang Y, Rotheram-Borus MJ, Detels R. Evolution of China’s response to HIV/AIDS. Lancet. 2007;369(9562):679–90. https://doi.org/10.1016/S0140-6736(07)60315-8.
Yin W, Hao Y, Sun X, Gong X, Li F, Li J. Scaling up the national methadone maintenance treatment program in China: achievements and challenges. Int J Epidemiol. 2010;39(Suppl 2):ii29–37. https://doi.org/10.1093/ije/dyq210.
Yin W, Pang L, Cao X, McGoogan JM, Liu M, Zhang C, et al. Factors associated with depression and anxiety among patients attending community-based methadone maintenance treatment in China. Addiction. 2015;110(Suppl 1):51–60. https://doi.org/10.1111/add.12780.
Zhang H. An analysis of the group characteristics of new-type drugs abuse in Dehong prefecture. J Yunnan Police Officer Acad. 2006;4:16–8.
Zhang L, Chow EP, Zhuang X, Liang Y, Wang Y, Tang C, et al. Methadone maintenance treatment participant retention and behavioral effectiveness in China: a systematic review and meta-analysis. PLoS One. 2013;8:e68906. https://doi.org/10.1371/journal.pone.0068906.
Zhao Y, Shi CX, McGoogan JM, Rou K, Zhang F, Wu Z. Methadone maintenance treatment and mortality in HIV-positive people who inject opioids in China. Bull World Health Organ. 2013;91(2):93–101. https://doi.org/10.2471/BLT.12.108944.
Zheng X, Tian C, Choi KH, Zhang J, Cheng H, Yang X, et al. Injecting drug use and HIV infection in southwest China. AIDS. 1994;8:1141–7.
Zhou Y, Zhuang G. Retention in methadone maintenance treatment in mainland China, 2004–2012: a literature review. Addict Behav. 2014;39(1):22–9. https://doi.org/10.1016/j.addbeh.2013.09.001.
Zhou Y, Wu Z, McGoogan JM, Luo W, Zhang B, Wu L, et al. Mortality and associated factors among methadone maintenance treatment clients in Yunnan, China: an eleven-year cohort study. J Addict Med. 2019 (under review).
Zhuang X, Liang Y, Chow EP, Wang Y, Wilson DP, Zhang L. HIV and HCV prevalence among entrants to methadone maintenance treatment clinics in China: a systematic review and meta-analysis. BMC Infect Dis. 2012;12:130. https://doi.org/10.1186/1471-2334-12-130.
Zou X, Ling L, Zhang L. Trends and risk factors for HIV, HCV and syphilis seroconversion among drug users in a methadone maintenance treatment programme in China: a 7-year retrospective cohort study. BMJ Open. 2015;5(8):e008162. https://doi.org/10.1136/bmjopen-2015-008162.
Acknowledgments
The authors would like to thank Willa Dong and Jennifer M. McGoogan for providing editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Cao, X., Lin, C., Wang, C., Wu, Z. (2020). The National Methadone Maintenance Treatment Program. In: Wu, Z., Wang, Y., Detels, R., Bulterys, M., McGoogan, J. (eds) HIV/AIDS in China. Springer, Singapore. https://doi.org/10.1007/978-981-13-8518-6_9
Download citation
DOI: https://doi.org/10.1007/978-981-13-8518-6_9
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-8517-9
Online ISBN: 978-981-13-8518-6
eBook Packages: MedicineMedicine (R0)