Abstract
It is important to manage multiple injury patients so as not to experience the lethal triad of hypothermia, metabolic acidosis, and coagulopathy. The treatment method in patients with massive exsanguination is greatly different from that of elective surgery patients, and it is necessary to implement damage control surgery (DCS), based on the patient’s general condition. The strategy is divided into DCS for controlling surgical bleeding and damage control resuscitation (DCR) for nonsurgical bleeding. Damage control surgery consists primarily of abbreviated lifesaving surgery, and DCR consists of maneuvers to avoid the lethal triad and administer critical care such as permissive hypotension, resuscitative fluid administration, and hemostatic resuscitation. Managing multiple trauma with traumatic brain injury (TBI) is different from managing single torso injury and takes into account factors such as avoiding hypotension and abdominal compartment syndrome, the effect of resuscitative endovascular balloon occlusion of the aorta on intracranial pressure, adverse effects of colloids on hemostasis, and indications for higher platelet administration, which are introduced in this chapter, respectively. The management of patients with multiple trauma and TBI remains mostly unknown, although evidence has been steadily accumulated.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Multiple injury
- Traumatic brain injury
- Damage control
- Permissive hypotension
- Massive transfusion protocol
11.1 Introduction
Hypothermia, metabolic acidosis, and coagulopathy constitute a pathological condition that leads to a poor outcome in the treatment and management of patients with multiple injuries and is called the lethal triad [1]. In general, hypothermia refers to a core body temperature <34 °C, acidosis refers to pH <7.2, and coagulation disorder refers to the manifestation of nonmechanical bleeding (described later). In severe trauma, these factors adversely affect each other and can cause a bloody vicious cycle [2]. In recent years, it has been pointed out that hemodilution due to excess fluid resuscitation during trauma management may lead to further resuscitation-associated coagulopathy (RAC). Some authors consider RAC occurring with the lethal triad as “the lethal quartet” [3, 4]. In treating patients with severe multiple trauma and hemorrhagic shock, avoiding and/or recovering from the lethal triad is very important in management. However, curative hemostasis surgery at the injured site is not simple for patients who have collapsed vital signs, and opening the abdominal and/or thoracic cavity for a long time aggravates hypothermia and the collapse of the coagulation fibrinolytic cascade associated with increased exsanguination. Furthermore, these factors can cause severe lactic acidosis, which may result in opposite effects. Two decades ago, resuscitation by a large amount of crystalloids and packed red blood cell (RBC) transfusion were widely administered to maintain tissue perfusion and sufficient oxygen delivery against traumatic hemorrhagic shock [5]. Such large volume resuscitation enabled the withdrawal of hemorrhagic shock, reduced early death due to exsanguination after severe trauma injury, and reduced the risk of acute renal failure [5, 6]. However, on the other hand, acute heart failure, pulmonary edema, and abdominal compartment syndrome (ACS) [7] due to intestinal edema (as described later) had increased following massive crystalloid resuscitation. In addition, these pathophysiological alterations increase inflammatory cytokine production, reperfusion injury, and immunity decline, which increase sepsis and late death because of multiple organ dysfunctions [8]. Based on these findings, since the mid-1980s, instead of performing curative surgery as the initial treatment of severely traumatized patients with unstable vital signs, damage control such as gauze packing to the surrounding bleeding organs to suppress the insult was introduced and has contributed to the improvement in the survival rate [5, 6, 9].
The phrase “damage control” is a naval military term [9]. Damage control in the military field refers to maintaining preliminary buoyancy and restoring power while maintaining water tightness and airtightness; especially in a ship in which fire, collision, stranding, or explosion has occurred, it refers to removing inflammable material, extinguishing a fire, and eliminating gas smoke. Moreover, by preparing emergency equipment, the spread of damage can be stopped, injured people can be treated, and failures and power supply can be restored [10, 11]. Furthermore, as for the origin of the damage control concept, it was introduced at the beginning of the Napoleonic war in the early 1800s [10]. At that time, the idea was that it was necessary to perform amputation within 24 h when the patient’s general condition was sufficiently stable to prevent death from severe extremity injury, which was difficult to treat.
Damage control surgery (DCS) is incorporated as part of the damage control strategy. This chapter details the damage control strategy of multiple injury and the influence and related issues that they have on neurocritical care.
11.2 Damage Control Strategy
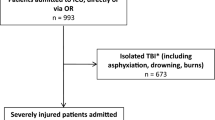
Damage control strategy consists of two fundamental actions (Fig. 11.1). The first fundamental action is DCS, the objective of which is controlling surgical bleeding. It was initially applied to abdominal trauma; the concept has spread to celiotomy, thoracotomy, orthopedics, neurosurgery, and interventional radiology (IVR) [12,13,14,15]. The second fundamental action is trauma resuscitation, the purpose of which is controlling nonsurgical bleeding. The paradigm of management is shifting from the conventional high-volume resuscitation to low-volume resuscitation (i.e., damage control resuscitation [DCR]).
11.3 Damage Control Neurosurgery and Intracranial Pressure-Related Issues
In 2004, Rosenfeld [14] emphasized that rapid intervention of neurological treatment is equivalent to damage control of neurosurgery. They reported that the management of sustained bleeding in the torso is a priority in patients with multiple traumas accompanied by traumatic brain injury (TBI); if the patient’s condition is stable, an intracranial pressure (ICP) sensor should be inserted in the emergency room or operating room in tandem with laparotomy and/or thoracotomy. The Guidelines for the Management of Severe Traumatic Brain Injury (third edition) published in 2007 recommended ICP should be monitored in TBI patients with Glasgow Coma Score (GCS) of 3–8 and either an abnormal CT scan or a normal CT if two or more of the following features were noted: age >40 years, unilateral or bilateral motor posturing, or systolic blood pressure (sBP) <90 mmHg [16]. However, the latest (fourth edition) of the guidelines published in 2017 only recommends managing severe TBI patients by using information from ICP monitoring to reduce in-hospital and 2-week postinjury mortality. There was no mention of what condition of the patients for whom ICP should be monitored; however, if the value exceeds 22 mmHg, it is desirable to treat the patient because of increased mortality [17]. Also, as soon as the fourth edition of the guidelines was published, the results of the Randomized Evaluation of Surgery with Craniectomy for Uncontrollable Elevation of Intracranial Pressure (RESCUEicp) trial were reported, which could affect the recommendation. The RESCUEicp trial is a prospective randomly assigned study of 408 patients with intracranial hypertension (i.e., ICP >25 mmHg) that compared the effect of decompressive craniectomy versus that of ongoing medical care [18]. The results revealed that decompressive craniectomy patients have lower mortality, higher rate of persistent vegetative state, and severe disability. However, moderate disability and good recovery rate were similar between two groups. This finding was not contrary to the results of the 2017 guidelines. An article in which the guidelines indicated that mortality increases above ICP 22 mmHg was based on the report by Sorrentino et al. [19]. They conducted subgroup analysis of age and sex and concluded the mortality threshold did not change; however, the threshold of favorable outcome was 18 mmHg in female patients or an age >55 years. The guideline did not support subgroup analysis results of sex and age because of the small number of cases; thus, the desirable ICP may differ, depending on sex, and age is an interesting topic for the future research.
Abdominal compartment syndrome is also very important as a pathophysiological condition at a risk of elevating the ICP. The intra-abdominal pressure (IAP) is usually maintained at 0–5 mmHg, and an IAP ≥12 mmHg at rest in the supine position is defined as intra-abdominal hypertension (IAH) [20]. If the IAP rises because of abdominal trauma or intestinal edema caused by massive transfusion, the intrathoracic pressure (ITP) would also rise through the diaphragm [21]. Rising ITP decreases venous return, which increases ICP and diminishes cerebral perfusion pressure (CPP) [22]. Moreover, the worsening effect of ACS on whole body organs is substantial. The following may occur because of elevated IAP and ITP: reduced cardiac output and increased afterload in the cardiovascular system [22, 23], increased airway pressure and ventilatory failure in respiratory system [24], reduced urine volume because of hypoperfusion of the renal parenchyma and vein in the visceral organs [25], disordered mitochondrial function and energy metabolism in the liver [26], and further exacerbated edema and circulation in digestive organs [27]. Therefore, a diagnosis of ACS requires immediate intervention, and nonsurgical treatments and/or surgical management are available [20]. For primary ACS caused by abdominal trauma, decompressive laparotomy (DL) and an open abdomen are the indicated surgical treatments. For secondary ACS due to excessive volume resuscitation, nonsurgical treatment is the first-line approach [20, 28]. Nonsurgical treatment consists of five methods, as follows [20]:
-
1.
To improve abdominal wall compliance, the use of sedatives, analgesics, muscle relaxants, and management with lowering the head to ≤30° may be considered.
-
2.
To remove digestive tract contents, nasogastric tube insertion, colorectal drainage, and intestinal peristalsis should be administered.
-
3.
Percutaneous drainage should be considered to remove abdominal cavity contents.
-
4.
To control fluid balance, restricting excessive volume resuscitation and using diuretics may be considered.
-
5.
To maintain organ function, ventilation and alveolar recruitment should be optimized.
If IAP persists at ≥20 mmHg and other organ disorders appear, despite the nonsurgical management, then it is desirable to consider DL [20, 28]. In 2018, a systematic review and meta-analysis of 286 patients with ACS who received DL was published [29]. According to the article, IAP was decreased on averate by 18.2 ± 6.5 mmHg and fell within the normal range. Moreover, heart rate, central venous pressure, pulmonary capillary wedge pressure (i.e., PCWP), and peak inspiratory pressure (i.e., PIP) were decreased; the ratio of partial pressure arterial oxygen and fraction of inspired oxygen (i.e., P/F ratio) and urinary output were increased in adult patients. Nearly similar hemodynamic beneficial effects were also observed in pediatric patients, although the reported mortality rate was as high as 49.7% for adults and 60.8% for children. Based on the aforementioned findings, it was concluded that further validation is required to determine the severity and optimal timing for which DL is effective.
11.3.1 Damage Control Resuscitation
The DCR consists of the following five components [30]: (1) recovery from hypothermia, (2) correction of metabolic acidosis, (3) permissive hypotension, (4) restrictive fluid administration, (5) and hemostatic resuscitation. Each component and related issues are described below.
11.3.2 Correction of Hypothermia and Metabolic Acidosis
Hypothermia can occur for a variety of reasons such as tissue hypoperfusion, rapid infusion, transfusions, and skin exposure during surgery in patients with severe trauma. The risk of death increases to 41-fold when the core body temperature is less than 35 °C, the platelet function and all coagulation factor activities decrease when the temperature falls below 34 °C, and the mortality rate is nearly 100% when the temperature is ≤32.8 °C [31]. The supplementation of coagulation factors is ineffective, and temperature recovery is the only treatment in hypothermia-induced coagulopathy.
It is wandering away from the main subject; many discussions exist regarding the effect and complications of induced hypothermia in TBI patients. There are two methods for inducing hypothermia. Prophylactic hypothermia is administered before ICP elevation, and therapeutic hypothermia is used for treatment-resistant ICP elevation. These treatment effects have often conflicted in previous reports. In response to a report by Clifton et al. in 2011, indicating early 33 °C prophylactic hypothermia shows no difference in mortality and outcome, compared with normothermia [32]; the Brain Trauma Foundation guidelines published in 2017 do not recommend early (i.e., within 2.5 h) short-term hypothermia to improve outcomes in patients with diffuse injury [17]. Current study subjects of the therapeutic hypothermia management have shifted to duration, depth, rewarming, and which patient populations. Clinicians also need to pay attention to metabolic acidosis at trauma resuscitation. Tissue hypoperfusion due to hemorrhagic shock causes the accumulation of lactic acid and metabolic acidosis [33]. In addition, clinicians also need to pay attention because the administration of more than 2000 mL of normal saline (0.9%) at resuscitation may cause high chloride acidosis and subsequent coagulopathy [33].
11.3.3 Permissive Hypotension and Restrictive Volume Administration
Permissive hypotension is a strategy that allows the management of blood pressure lower than normal tissue perfusion pressure with the purpose of not exacerbating bleeding until surgical bleeding is controlled [34, 35]. This concept has had much focus in this decade, although it was described in 1918 by Cannon et al. [36]. They mentioned in the article for the first time the harmfulness of administering volume resuscitation before achieving hemostasis in patients with trauma injury and advocated maintaining an sBP of 70–80 mmHg until curative hemostasis is achieved. Permissive hypotension is indicated for patients with a penetrating torso injury not accompanied by severe TBI, and low-volume resuscitation, which restricts massive crystalloid administration, is used to control the sBP to 80–90 mmHg and the mean arterial blood pressure (mAP) to 50 mmHg [34]. Restrictive volume administration may provide many advantages such as mitigation of dilutional coagulopathy (i.e., RAC), suppression of “pop” a clot phenomenon, peeling off the thrombus of hemostasis by elevated blood pressure leading to rebleeding, and avoiding resuscitation injury by massive crystalloid administration, as mentioned previously [6]. However, care should be taken in sBP and infusion management in patients with severe TBI and in patients with brain injury and multiple trauma. It has long been important to avoid hypotension to reduce secondary injury and brain swelling of TBI [37], although how to manage blood pressure and volume resuscitation in patients with severe TBI and multiple injuries has not been determined. The 2005 American Heart Association’s Guidelines for Cardiovascular Care reported that administering rapid infusion with an sBP target value of ≥100 mmHg is recommended only for blunt trauma or for penetrating trauma to the brain or extremities alone [38]. The European Guideline on Management of Major Bleeding and Coagulopathy Following Trauma in 2016 states that the infusion volume should be limited with the aim of maintaining the mean arterial pressure (mAP) >80 mmHg in patients with severe TBI (GCS ≤8) and/or with spinal cord injury [34]. In the latest Brain Trauma Foundation guidelines in 2017, blood pressure management with TBI varies, based on age as follows: “maintaining sBP at ≥100 mmHg for patients 50–69 years old or at ≥110 mmHg or above for patients 15–49 or over 70 years old may be considered to decrease mortality and improve outcomes” [17]. As described previously, the reason the blood pressure management target cannot be set easily in patients with TBI is that it is difficult to evaluate and judge the cerebral blood flow (CBF). Monitoring the ICP is essential for accurate evaluation because CPP is included in the formula: mAP – ICP. However, in some environments it is difficult to initiate monitoring during the hyperacute phase, as well as establish high-quality research concerning blood pressure management in TBI, and comply with the research protocols. Moreover, CBF is theoretically preserved by autoregulation, even if blood pressure is reduced in a healthy person; however, this autoregulation may collapse in moderate to severe TBI, and CPP is not necessarily maintained only by blood pressure management. With regard to retaining CPP retention and decreasing ICP, attention should also be paid to the infusion fluid type for trauma patients. The use of mannitol or hypertonic saline at the time of increasing ICP is recommended [17], although hypertonic saline is recommended in DCR [39]. At present, it seems that there is no problem in choosing to administer hypertonic saline in patients with multiple trauma and TBI with the expectation that the ICP will decrease. The European guidelines in 2016 recommend avoiding hypotonic solutions such as Ringer’s lactate in patients with severe head trauma to minimize fluid shift to damaged brain tissue [34]. Furthermore, caution is required for the administration of a colloid solution. Investigators in the Saline versus Albumin Fluid Evaluation (SAFE) study, which investigated in 460 patients with TBI, reported that the administration of albumin (4%) increases the mortality rate (RR, 1.62), compared with the administration of normal saline [40]. The SAFE-TBI study post hoc analysis revealed that the increase in mortality due to albumin administration in patients with severe TBI was associated with increased ICP [41]. The 2016 European Guideline on Management of Major Bleeding and Coagulopathy Following Trauma advocates “use of colloids be restricted because of the adverse effects on hemostasis” [34].
11.3.4 Resuscitative Endovascular Balloon Occlusion of the Aorta
Even if volume resuscitation is administered during the initial trauma management, it is possible for a crisis situation to occur in which the sBP cannot be maintained. If the uncontrolled hemorrhagic region is peripheral to the abdomen, an option is to maintain blood pressure through thoracic or abdominal aortic cross-clamping. The purpose of the procedure is to preserve blood flow and pressure in the heart and the central nervous system (CNS) by disrupting or reducing blood flow below the clamp. Even if the method of aortic cross-clamping directly by thoracotomy or laparotomy is complete, blood flow below the clamping region is completely disrupted, and the insult caused by the procedure itself may worsen a patient’s condition [42]. Resuscitative endovascular balloon occlusion of the aorta (REBOA), a method of blocking blood flow by inflating a balloon inserted in the aorta, is minimally invasive and can even be administered by a physician who is not learned in surgical procedures. Animal experiments of the REBOA procedure have data indicating that the mortality rate and lactic acid level increase when the blocking time exceeds 60 min [43]; therefore, a continuous cutoff time of 45 min or less is recommended. In direct cross-clamping, blood flow below a clamp is completely blocked, whereas REBOA can control the blood flow below the blocking region to some extent by the amount of normal saline injected into the balloon; this procedure is called partial REBOA [44]. Resuscitation is possible when the sBP is controlled to a 80–90 mmHg target as a permissive hypotension by partial REBOA in trauma patients without brain injury and is controlled to a 100 mmHg target in patients with multiple trauma and TBI. However, in actual practice, whether REBOA is beneficial or harmful for patients with TBI is inconclusive. It has been hypothesized that increased carotid artery blood flow by REBOA leads to deterioration by cerebral edema, elevation of ICP, and exacerbation of intracranial hemorrhage [45]. Some investigators report that the mortality of patients with multiple injuries and TBI requiring REBOA is as high as 50% [46, 47]. By contrast, there are animal experiments that such a supraphysiological response does not lead to hemorrhage exacerbation of brain CT. Johnson et al. [48] created hemorrhagic shock using a standardized brain trauma swine model and measured the mAP, carotid artery blood flow, and ICP and obtained brain CT imaging in the REBOA group, the partial aortic clamp group, and the control group. The mAP and carotid artery blood flow in the REBOA group was significantly high; however, the ICP was largest at the time of resuscitation due to the rapid transfusion in control group, which was contrary to expectation. There was no significant difference between the three groups in the proportion of hemorrhage exacerbations on the brain CT, and REBOA was not a factor that worsened TBI. Further study will be required for the effects and adverse effects of REBOA in patients with TBI and multiple injuries.
11.3.5 Hemostatic Resuscitation
As with other injuries, TBI was traditionally managed to maintain a high hemoglobin (Hb) level to prevent secondary brain damage due to reduced oxygen delivery [5, 49]. However, this concept has also changed in recent years. Robertson et al. [50] reported that neurological prognosis after 6 months did not change in a study of TBI patients when comparing the Hb transfusion thresholds of 7 and 10 g/dL. In a retrospective review of 1150 TBI patients, Salim et al. [49] concluded that blood transfusion is associated with high mortality (adjusted odds ratio [OR], 2.19) and high complication rate (OR, 3.67) in patients with or without anemia. Thus, it may be that maintaining a Hb level higher than necessary is rather harmful; however, it is also a fact that there are circumstances in which massive transfusion must be administered rapidly in patients with multiple traumas. Hemostatic resuscitation in patients with multiple traumas is a strategy to minimize acute coagulopathy of trauma and shock (ACoTS) and RAC by the transfusion protocol and drug administration for massive hemorrhage [4]. Details of coagulopathy due to trauma and coagulopathy associated with massive fluid resuscitation such as ACoTS and RAC are discussed in Chap. 9 (“Coagulopathy and Brain Injury”). In this chapter, we describe the main treatment strategies for patients with multiple injuries.
11.3.5.1 Massive Transfusion Protocol
For the initial treatment of patients with severe multiple injuries and unstable vital signs, many trauma centers have adopted the massive transfusion protocol (MTP), which involves promptly administrating erythrocyte concentrate, fresh frozen plasma (FFP), and platelet concentrate (PLT) at an appropriate ratio without waiting for blood test results [4, 51]. In addition, massive transfusion is defined as the administration of more than 10 units of RBCs per 24 h, ≥150 mL/h, or 100% blood in less in 24 h; however, this definition is not evidence-based [52]. Many traumatic deaths due to exsanguination occur within 2–3 h of injury [53]. Therefore, in discussing massive transfusion in severe trauma, defining it as a transfusion volume per 24 h may not have a significant meaning [54]. Over the last decade, there have been discussions regarding whether the transfusion ratio of plasma to platelet to RBC is favorable at 1:1:1 in the MTP. Some investigators report that the survival rate increases when the proportion of plasma is increased [56,57,57], whereas other investigators indicate this finding is because of survival bias [58, 59]. Therefore, the appropriate ratio is of interest to researchers. Recent studies may have settled this discussion [53, 60]. The Prospective, Observational, Multicenter, Major Trauma Transfusion (PROMMTT) study published by Holcomb et al. [60] in 2013 was a prospective cohort study that observed 905 trauma patients who had required at least 3 units of transfusion within 24 h of admission [60]. They elucidated a significant decrease in 6-h mortality because of the early high rate resuscitation of plasma and PLT (plasma:PLT:RBC = 1:1:1), compared with patients with a ratio less than 1:2. Furthermore, a transfusion ratio less than 1:2 was associated with a three- to fourfold mortality rate. The Pragmatic, Randomized Optimal Platelets and Plasma Ratios (PROPPR) study published in 2015 was a multicenter prospective randomized control trial in which the plasma:PLT:RBC ratios of 1:1:1 and 1:1:2 were compared in 680 patients with severe trauma [53]. The 1:1:1 transfusion group had more hemostasis (86% vs. 78%) and less exsanguination (9% vs. 15%) in the first 24 h, but the 24-h mortality and 30-day mortality were comparable. The authors suggested that the reason the mortality was not significant was that most deaths due to exsanguination often do not occur after 24 h of injury, but within 2–3 h of injury. In addition, the 1:1:2 group eventually underwent many transfusions after the intervention and frequently used cryoprecipitate (described later) with a high hemostatic effect (22% vs. 29%). This appeared an attempt to achieve the 1:1:1 strategy. Some current guidelines recommend a 1:1:1 strategy because of the aforementioned results and similarity of complication rate associated with transfusion [61, 62]. The subject of the PROMMTT and PROPPR studies was severe trauma in general; however, neither study differentiated TBIs. In 2011, a study that differentiated TBIs was reported by Brasel et al. [54]. They retrospectively examined patients who were divided into (1) TBI+ patients with an abbreviated injury scale of ≥3 and (2) TBI− patients with an abbreviated injury scale <3. To prevent survival bias, patients were excluded who died within 60 min. They found that a high PLT:RBC ratio improved 30-day survival in the TBI+ group and a high plasma:RBC ratio was associated with an improvement in the 30-day survival in the TBI− group. The reason the authors proposed for the favorable outcome of high ratio of PLT administration in the TBI+ group is that PLT may activate oligodendrocyte precursor cells, which differentiate into oligodendrocytes in the damaged CNS and restore demyelinated areas; they also cited an experiment of blood-brain barrier damage in a rodent model [63]. For the platelet count, it is recommended to maintain the number of platelets ongoing bleeding with TBI at 100 × 109/L or more, based on the European guidelines 2016 [34]. At present, it appears that there is no problem in using the 1:1:1 protocol in patients with multiple traumas and brain injury. However, rapid transfusion may increase ICP, based on the animal experiment of REBOA cited earlier [48]. Further research is necessary to obtain conclusions.
11.3.5.2 Fibrinogen Concentrate and Cryoprecipitate
Fibrinogen is the final component of the coagulation cascade and an essential element for stable thrombus formation [64]. It is cleaved by thrombin into fibrin, which polymerizes to form a strong thrombus resistant to fibrinolysis [64]. In a prospective study of 517 trauma patients, Rourke et al. [65] reported that a low fibrinogen level was a predictor of 24-h mortality and 28-day mortality. The importance of fibrinogen is widely recognized in the treatment of multiple trauma. However, cryoprecipitate is purified by concentrating the coagulation factors contained in plasma and contains factor VIII, factor XIII, von Willebrand factor (vWF), and fibrinogen, which have a high hemostatic effect [66]. The European guidelines in 2007 recommended supplementation at a fibrinogen level of 1 g/L or less in patients with trauma [67]. However, the 2016 guidelines recommend supplementation of fibrinogen concentrate or cryoprecipitate at 1.5–2.0 g/L or less. The initial desirable fibrinogen administration is 3–4 g, which is approximately 15–20 units for cryoprecipitate or approximately 20–25 units for FFP [34].
In 2017, Innerhofer et al. [68] announced early cancelation of the Reversal of Trauma Induced Coagulopathy Using Coagulation Factor Concentrates or Fresh Frozen Plasma (RETIC) trial because of futility and safety reasons, which was verifying the effects of FFP or coagulation factor concentrates (CFCs) for patients with severe trauma and coagulopathy (including TBI patients). The CFCs administered in this trial consisted of fibrinogen and/or prothrombin complex concentrate and/or factor XIII. The reason for the trial cancelation was that more rescue therapy is required in the FFP group (OR, 25.3) and the necessity for massive transfusion was increased (OR, 3.0). Based on these results, they concluded that first-line CFCs outperformed FFP administration, and they emphasized the importance of early effective fibrinogen supplementation for clotting failure with severe trauma. Prospective studies are being conducted to determine whether supplementation of urgent cryoprecipitate will improve the outcome. In 2015, the CRYOSTAT pilot study [69] examined cryoprecipitate supplementation within 90 min of arrival, and, in 2018, the Early-Fibrinogen in Trauma (E-FIT 1) pilot trial [70] aimed to administer cryoprecipitate within 45 min of arrival for patients undergoing MTP for hemorrhagic shock. A prudent interpretation of E-FIT 1 trial is required because administering cryoprecipitate supplementation within 45 min is difficult. However, the early supplementation group had no significant difference in all-cause mortality at 28 days, compared with the normal administration group in either trial. It is not reasonable to administer cryoprecipitate immediately after admission. However, the accumulation of further research results is required because the efficacy for TBI is unknown.
11.3.5.3 Antifibrinolytic Agents
Tranexamic acid (TXA) has a leading role in antifibrinolytic therapy. The Clinical Randomization of an Antifibrinolytic in Significant Hemorrhage 2 (CRASH-2) trial is a randomized controlled trial involving 20,111 injured patients with massive exsanguination, which includes TBI, within 8 h, or hypotension and/or tachycardia [71]. The TXA group, which received loading 1 g of TXA over 10 min, followed by 1 g infusion of TXA over 8 h, was compared with the placebo group (0.9% saline). The all-cause mortality (relative risk [RR], 0.91) and the risk of death from hemorrhage (RR, 0.85) decreased because of TXA administration. There were no significant differences in vascular occlusion complications and amount of transfusion. Furthermore, in an additional report in 2011, the risk of hemorrhage was significantly decreased when TXA was administered within 1 h (RR, 0.68) or 1–3 h postinjury (RR, 0.79) [72]. By contrast, the risk of hemorrhagic death was increased by administering TXA 3 h postinjury (RR, 1.44). Based on the results of the CRASH-2 trial, the 2016 European guidelines recommended TXA administration within 3 h, based on the method used in the trial [34]. In addition, the CRASH-3 trial is in progress [73]. The CRASH-3 trial is an international, multicenter, pragmatic randomized, double-blind, placebo-controlled trial for patients with intracranial hemorrhage on CT or with a GCS ≤12 among adults with single brain injuries within 8 h of injury and uncertainty as to whether TXA should be administered. The method of administration of TXA is similar to that in the CRASH-2 trial. The research results are pending regarding the extent an effect can be obtained for patients with single brain trauma.
11.3.5.4 Ionized Calcium (iCa)
Ionized calcium (iCa) is indispensable for the formation and stabilization of fibrin polymerization; a reduction in cytosolic iCa concentration decreases all platelet activity [74]. Giancarelli et al. [75] reported that, among 156 trauma patients who underwent massive transfusion in 2009–2013, 97% had hypocalcemia and 71% had severe hypocalcemia (iCa <0.9 mmol/L). The mortality was significantly higher among the severe hypocalcemia group than among the hypocalcemia group (49% vs. 24%), when compared with normal limit. The 2016 European guidelines recommend that iCa levels be monitored and maintained within the normal range during massive transfusion [34].
11.3.5.5 Factor VIIa
Boffard et al. [76] in their prospective study reported on the effect of factor VIIa in reducing the transfusion amount in patients with blunt trauma, even though it did not decrease mortality. Since that report, recombinant factor VIIa (rFVIIa) administration has been included in the MTP in many trauma centers [77]. The CONTROL trial in 2010 was a randomized, assignment, prospective study to verify the efficacy of rFVIIa in patients with torso or femoral trauma and refractory hemorrhage [78]. This study unfortunately resulted in less than one-half of the anticipated mortality reduction, and enrollment was censored. In 2018, Lombard et al. reported a propensity score analysis of rFVIIa administration in TBI, although it is a level III evidence [79]. This investigation covered 4284 TBI patients with GCS ≤13 who were diagnosed with brain CT and treated at 11 level 1 trauma centers. Of 129 patients were administered rFVIIa which is not involved in the risk reduction of mortality or morbidity as a result of comparison with the non-administered group. The results of prospective studies will be required to determine the effect of FVIIa administration.
11.4 Summary
As mentioned previously, some treatment strategies for patients with multiple traumas have undergone major transformations in recent decades. However, some treatment strategies also include revival of treatments that had been conducted in the past. In multiple trauma, including brain injury, there are many parts so that management is different for the torso and/or extremity injury and many factors that remain unknown. With cutting-edge treatment technology and development, we hope that the knowledge and experiences abandoned in the past will be integrated and renovate conventional trauma management, and thus many patients will be saved.
References
Barry WE. The deadly triad. Aerosp Med. 1974;45:931–2.
Cosgriff N, Moore EE, Sauaia A, Kenny-Moynihan M, Burch JM, Galloway B. Predicting life-threating coagulopathy in the massively transfused trauma patient. J Trauma. 1997;42:857–61.
Hess JR, Brohi K, Dutton RP, Hauser CJ, Holcomb JB, Kluger Y, et al. The coagulopathy of trauma: a review of mechanisms. J Trauma. 2008;65:748–54.
Noel P, Cashen S, Patel B. Trauma-induced coagulopathy: from biology to therapy. Semin Hematol. 2013;50:259–69.
Cohen MJ. Towards hemostatic resuscitation: the challenging concept understanding of acute traumatic biology, massive bleeding, and damage-control resuscitation. Surg Clin N Am. 2012;92:877–91.
Alam HB, Velmohas GC. New trends in resuscitation. Curr Probl Surg. 2011;48:531–64.
Balogh Z, McKinley BA, Cocanour CS, Kozar RA, Valdivia A, Sailors RM, et al. Supranormal trauma resuscitation causes more cases of abdominal compartment syndrome. Arch Surg. 2003;138:637–42.
Cotton BA, Guy JS, Morris JA Jr, Abumrad NN. The cellular, metabolic, and systemic consequences of aggressive fluid resuscitation strategies. Shock. 2006;26:115–21.
Rotondo MF, Schwab CW, McGonigal MD, Phillips GR 3rd, Fruchterman TM, Kauder DR, et al. ‘Damage control’: an approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma. 1993;35:375–82.
Helling TS, McNabney WK. The role of amputation in the management of battlefield casualties: a history of two millennia. J Trauma. 2000;49:930–9.
Brewer LA III. The contributions of the Second Auxiliary Surgical Group to military surgery during World War II with special reference to thoracic surgery. Ann Surg. 1983;197:318–26.
Hildebrand F, Giannoudis P, Kretteck C, Pape HC. Damage control: extremities. Injury. 2004;35:678–89.
Giannoudis PV, Pape HC. Damage control orthopaedics in unstable pelvic ring injuries. Injury. 2004;35:671–7.
Rosenfeld JV. Damage control neurosurgery. Injury. 2004;35:655–60.
Reilly PM, Rotondo MF, Carpenter JP, Sherr SA, Schwab CW, et al. Temporary vascular continuity during damage control: intraluminal shunting for proximal superior mesenteric artery injury. J Trauma. 1995;39:757–60.
American Association of Neurological Surgeons; Congress of Neurological Surgeons. Guidelines for the management of severe traumatic brain injury. J Neurotrauma. 2007;24(Suppl 1):S1–106.
Carney N, Totten AM, O’Reilly C, Ullman JS, Hawryluk GW, Bell MJ, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017;80:6–15.
Peter JH, Angelos GK, Ivan ST, Elizabeth AC, Marek C, Jake T, et al. Trial of decompressive craniectomy for traumatic intracranial hypertension. N Engl J Med. 2016;375:1119–30.
Sorrentino E, Diedler J, Kasprowicz M, Budohoski KP, Haubrich C, Smielewski P, et al. Critical thresholds for cerebrovascular reactivity after traumatic brain injury. Neurocrit Care. 2012;16:258–66.
Kirkpatrick AW, Roberts DJ, De Waele J, Jaeschke R, Malbrain ML, De Keulenaer B, et al. Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the World Society of the Abdominal Compartment Syndrome. Intensive Care Med. 2013;39:1190–206.
Malbrain ML, Wilmer A. The polycompartment syndrome: towards an understanding of the interactions between different compartments! Intensive Care Med. 2007;33:1869–72.
Bloomfield GL, Ridings PC, Blocher CR, Marmarou A, Sugerman HJ. Effects of increased intra-abdominal pressure upon intracranial and cerebral perfusion pressure before and after volume expansion. J Trauma. 1996;40:936–41.
Oda J, Ueyama M, Yamashita K, Inoue T, Harunari N, Ode Y, et al. Effects of escharotomy as abdominal decompression on cardiopulmonary function and visceral perfusion in abdominal compartment syndrome with burn patients. J Trauma. 2005;59:369–74.
Obeid F, Saba A, Fath J, Guslits B, Chung R, Sorensen V, et al. Increases in intra-abdominal pressure affect pulmonary compliance. Arch Surg. 1995;130:544–7, discussion 547–8.
Doty JM, Saggi BH, Blocher CR, Fakhry I, Gehr T, Sica D, et al. Effects of increased renal parenchymal pressure on renal function. J Trauma. 2000;48:874–7.
Nakatani T, Sakamoto Y, Kaneko I, Ando H, Kobayashi K. Effects of intra-abdominal hypertension on hepatic energy metabolism in a rabbit model. J Trauma. 1998;44:446–53.
Diebel LN, Dulchavsky SA, Wilson RF. Effect of increased intra-abdominal pressure on mesenteric arterial and intestinal mucosal blood flow. J Trauma. 1992;33:45–8, discussion 48–9.
Coccolini F, Roberts D, Ansaloni L, Ivatury R, Gamberini E, Kluger Y, et al. The open abdomen in trauma and non-trauma patients: WSES guidelines. World J Emerg Surg. 2018;13:7. https://doi.org/10.1186/s13017-018-0167-4.
Van Damme L, De Waele JJ. Effect of decompressive laparotomy on organ function in patients with abdominal compartment syndrome: a systematic review and meta-analysis. Crit Care. 2018;22:179. https://doi.org/10.1186/s13054-018-2103-0.
Kaafarani HMA, Velmahos GC. Damage control resuscitation in trauma. Scand J Surg. 2014;103:81–8.
Duchesne JC, McSwain NE Jr, Cotton BA, Hunt JP, Dellavolpe J, Lafaro K, et al. Damage control resuscitation: the new face of damage control. J Trauma. 2010;69:976–90.
Clifton GL, Allen S, Barrodale P, Plenger P, Berry J, Koch S, et al. A phase II study of moderate hypothermia in severe brain injury. J Neurotrauma. 1993;10:263–71.
Healey MA, Davis RE, Liu FC, Loomis WH, Hoyt DB, et al. Lactated ringer’s is superior to normal saline in a model of massive hemorrhage and resuscitation. J Trauma. 1998;45:894–9.
Rossaint R, Bouillon B, Cerny V, Coats TJ, Duranteau J, Fernández-Mondéjar E, et al. The European guideline on management of major bleeding and coagulopathy following trauma: fourth edition. Crit Care. 2016;20:100.
Duchesne JC, Kimonis K, Marr AB, Rennie KV, Wahi G, Wells JE, et al. Damage control resuscitation in combination with damage control laparotomy: a survival advantage. J Trauma. 2010;69:46–52.
Cannon WB, Fraser J, Cowell EM. The preventive treatment of wound shock. J Am Med Assoc. 1918;70:618–20.
Klauber MR, Marshall LF, Luerssen TG, Frankowski R, Tabaddor K, Eisenberg HM. Determinants of head injury mortality: importance of the low risk patient. Neurosurgery. 1989;24:31–6.
Maegele M, Lefering R, Yucel N. American Heart Association guidelines for cardiovascular care. Part 10.7: Cardiac arrest associated with trauma. Circulation. 2005;112:146–9.
Palmer L, Martin L. Traumatic coagulopathy. Part 2: Resuscitative strategies. J Vet Emerg Crit Care. 2014;24:75–92.
SAFE Study Investigators, Australian and New Zealand Intensive Care Society Clinical Trials Group, Australian Red Cross Blood Service, et al. Saline or albumin for fluid resuscitation in patients with traumatic brain injury. N Engl J Med. 2007;357:874–84.
Cooper DJ, Myburgh J, Heritier S. Albumin resuscitation for traumatic brain injury: is intracranial hypertension the cause of increased mortality? J Neurotrauma. 2013;30:512–8.
Seamon JM, Haut ER, Van Arendonk K, Barbosa RR, Chiu WC, Dente CJ, et al. An evidence-based approach to patient selection for emergency department thoracotomy: a practice management guideline from the eastern association for the surgery of trauma. J Trauma Acute Care Surg. 2015;79:159–73.
Avaro JP, Mardelle V, Roch A, Gil C, de Biasi C, Oliver M, et al. Forty-minute endovascular aortic occlusion increases survival in an experimental model of uncontrolled hemorrhagic shock caused by abdominal trauma. J Trauma. 2011;71:720–5.
Hammer M, Jovin T, Wahr JA, Heiss WD. Partial occlusion of the descending aorta increases cerebral blood flow in a nonstroke porcine model. Cerebrovasc Dis. 2009;28:406–10.
Russo RM, Neff LP, Johnson MA, Williams TK. Emerging endovascular therapies for non-compressible torso hemorrhage. Shock. 2016;46:12–9.
Norii T, Crandall C, Terasaka Y. Survival of severe blunt trauma patients treated with resuscitative endovascular balloon occlusion of the aorta compared with propensity score-adjusted untreated patients. J Trauma Acute Care Surg. 2015;78:721–8.
Uchino H, Tamura N, Echigoya R, Ikegami T, Fukuoka T. “REBOA”—is it really safe? A case with massive intracranial hemorrhage possibly due to endovascular balloon occlusion of the aorta (REBOA). Am J Case Rep. 2016;17:810–3.
Johnson MA, Williams TK, Ferencz SE, Davidson AJ, Russo RM, O’Brien WT, et al. The effect of resuscitative endovascular balloon occlusion of the aorta, partial aortic occlusion and aggressive blood transfusion on traumatic brain injury in a swine multiple injuries model. J Trauma Acute Care Surg. 2017;83:61–70.
Salim A, Hadjizacharia P, DuBose J, Brown C, Inaba K, Chan L, et al. Role of anemia in traumatic brain injury. J Am Coll Surg. 2008;207:398–406.
Robertson CS, Hannay HJ, Yamal JM, Gopinath S, Goodman JC, Tilley BC, et al. Effect of erythropoietin and transfusion threshold on neurological recovery after traumatic brain injury: a randomized clinical trial. JAMA. 2014;312:36–47.
Duan K, Yu W, Li N. The pathophysiology and management of acute traumatic coagulopathy. Clin Appl Thromb Hemost. 2015;21:645–52.
Davenport R, Khan S. Management of major trauma hemorrhage: treatment priorities and controversies. Br J Haematol. 2011;155:537–48.
Holcomb JB, Tilley BC, Baraniuk S, Fox EE, Wade CE, Podbielski JM, et al.; PROPPR Study Group. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma; the PROPPR randomized clinical trial. JAMA. 2015;313:471–82.
Brasel KJ, Vercruysse G, Spinella PC, Wade CE, Blackbourne LH, Borgman MA, et al. The association of blood component use ratios with the survival of massively transfused trauma patients with and without brain injury. J Trauma. 2011;71:S343–52.
Johansson PI, Hansen MB, Sorensen H. Transfusion practice in massively bleeding patients: time for a change? Vox Sang. 2005;89:92–6.
Borgman MA, Spinella PC, Perkins JG, Grathwohl KW, Repine T, Beekley AC, et al. The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. J Trauma. 2007;63:805–13.
Maegele M, Lefering R, Paffrath T, Tjardes T, Simanski C, Bouillon B, Working Group on Polytrauma of the German Society of Trauma Surgery (DGU). Red-blood-cell to plasma ratios transfused during massive transfusion are associated with mortality in severe multiple injury: a retrospective analysis from the Trauma Registry of the Deutsche Gesellschaft für Unfallchirurgie. Vox Sang. 2008;95:112–9.
Brown JB, Cohen MJ, Minei JP, Majer RV, West MA, Billiar TR, et al. Debunking the survival bias myth; characterization of mortality during the initial 24 h for patients requiring massive transfusion. J Trauma Acute Care Surg. 2012;73:358–64.
Snyder CW, Weinberg JA, McGwin G Jr, Melton SM, George RL, Reiff DA, et al. The relationship of blood product ratio to mortality: survival benefit or survival bias? J Trauma. 2009;66:358–62.
Holcomb JB, del Junco DJ, Fox EE, Wade CE, Cohen MJ, Schreiber MA, et al.; PROMMTT Study Group. The prospective, observational, multicenter, major trauma transfusion (PROMMTT) study: comparative effectiveness of a time-varying treatment with competing risks. JAMA Surg. 2013;148:127–36.
Glen J, Constanti M, Brohi K. Assessment and initial management of major trauma: summary of NICE guideline. BMJ. 2016;353:i3051.
Klein AA, Arnold P, Bingham RM, Brohi K, Clark R, Collis R, et al. AAGBI guidelines: the use of blood components and their alternatives 2016. Anesthesia. 2016;71:829–42.
Rhodes KE, Raivich G, Fawcett JW. The injury response of oligodendrocyte precursor cells is induced by platelets, macrophages and inflammation-associated cytokines. Neuroscience. 2006;140:87–100.
Levy JH, Welsby I, Goodnough LT. Fibrinogen as a therapeutic target for bleeding: a review of critical levels and replacement therapy. Transfusion. 2014;54:1389–405.
Rourke C, Curry N, Khan S, Taylor R, Raza I, Davenport R, et al. Fibrinogen levels during trauma hemorrhage, response to replacement therapy, and association with patient outcomes. J Thromb Haemost. 2012;10:1342–51.
Jensen NH, Stensballe J, Afshari A. Comparing efficacy and safety of fibrinogen concentration to cryoprecipitate in bleeding patients: a systematic review. Acta Anaesthesiol Scand. 2016;60:1033–42.
Spahn DR, Cerny V, Coats TJ, Duranteau J, Fernández-Mondéjar E, Gordini G, et al. Management of bleeding following major trauma: a European guideline. Crit Care. 2007;11:R17.
Innerhofer P, Fries D, Mittermayr M, Innerhofer N, von Langen D, Hell T, et al. Reversal of trauma-induced coagulopathy using first-line coagulation factor concentrates or fresh frozen plasma (RETIC): a single-centre, parallel-group, open-label, randomised trial. Lancet Haematol. 2017;4:e258–71.
Curry N, Rourke C, Davenport R, Beer S, Pankhurst L, Deary A, et al. Early cryoprecipitate for major haemorrhage in trauma: a randomized controlled feasibility trial. Br J Anaesth. 2015;115:76–83.
Curry N, Foley C, Wong H, Mora A, Curnow E, Zarankaite A, et al. Early fibrinogen concentrate therapy for major haemorrhage in trauma (E-FIT 1): results from a UK multi-centre, randomized, double blind, placebo-controlled pilot trial. Crit Care. 2018;22:164. https://doi.org/10.1186/s13054-018-2086-x.
CRASH-2 trial collaborators, Shakur H, Roberts I, Bautista R, Caballero J, Coats T, Dewan Y, et al. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomized, placebo-controlled trial. Lancet. 2010;376:23–32.
CRASH-2 trial collaborators, Roberts I, Shakur H, Afolabi A, Brohi K, Coats T, Dewan Y, et al. The importance of early treatment with tranexamic acid in bleeding trauma patients: an exploratory analysis of the CRASH-2 randomised controlled trial. Lancet. 2011;377:1096–101.
CRASH-3 collaborators, Dewan Y, Komolafe EO, Mejía-Mantilla JH, Perel P, Roberts I, Shalur H. CRASH-3 – tranexamic acid for the treatment of significant traumatic brain injury: study protocol for an international randomized, double-blind, placebo-controlled trial. Trials. 2012;13:87. https://doi.org/10.1186/1745-6215-13-87.
Perkins JG, Cap AP, Weiss BM, Reid TJ, Bolan CD. Massive transfusion and nonsurgical hemostatic agents. Crit Care Med. 2008;36(7 Suppl):S325–39.
Giancarelli A, Birrer KL, Alban RF, Hobbs BP, Liu-DeRyke X, et al. Hypocalcemia in trauma patients receiving massive transfusion. J Surg Res. 2016;202:182–7.
Boffard KD, Riou B, Warren B, Choong PI, Rizoli S, Rossaint R, et al.; NovoSeven Trauma Study Group. Recombinant factor VIIa as adjunctive therapy for bleeding control in severely injured trauma patients: two parallel randomized, placebo-controlled, double-blind clinical trials. J Trauma. 2005;59:8–15, discussion 15–8.
Horton JD, DeZee KJ, Wagner M. Use of rFVIIa in the trauma setting—practice patterns in United States trauma centers. Am Surg. 2008;74:413–7.
Hauser CJ, Boffard K, Dutton R, Bernard GR, Croce MA, Holcomb JB, et al.; CONTROL Study Group. Results of the CONTROL trial: efficacy and safety of recombinant activated Factor VII in the management of refractory traumatic hemorrhage. J Trauma. 2010;69:489–500.
Lombardo S, Millar D, Jurkovich GH, Coimbra R, Nirula R. Factor VIIa administration in traumatic brain injury: an AAST-MITC propensity score analysis. Trauma Surg Acute Care Open. 2018;3(1):e000134. https://doi.org/10.1136/tsaco-2017-000134.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Ebihara, T. (2019). Multiple Injury. In: Kinoshita, K. (eds) Neurocritical Care . Springer, Singapore. https://doi.org/10.1007/978-981-13-7272-8_11
Download citation
DOI: https://doi.org/10.1007/978-981-13-7272-8_11
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-7271-1
Online ISBN: 978-981-13-7272-8
eBook Packages: MedicineMedicine (R0)