Abstract
The discovery of new therapeutic agents and targets depending upon the pathophysiology of various diseases has necessitated the delivery of therapeutic molecules to specific cellular sub-compartments. The efficiency of various treatments can be improved by carefully designing new therapeutic strategies involving modifications of nanocarriers enabling organelle-specific targeting of bioactives. In order to do that, in-depth studies to unravel the pathophysiology of diseases, internalization and intracellular trafficking pathways, as well as the time-dependent fate and release of encapsulated cargo from nanocarriers within the organelles are much needed. Despite the interdisciplinary efforts from the fields of medicine, materials science, and engineering, and the development of various nanomedicines with a precise control over their physical and chemical attributes, the subcellular targeted delivery still presents formidable challenges. Further, considering the fact that drug repurposing is now gaining interest, an intersection of nanocarriers and drug repurposing would provide key benefits like reduced time, cost, and risk in developing safer and more effective treatments for several indications. The significant opportunities and challenges in further progress toward bench-to-bedside translation of organelle-targeted nanomedicines are discussed in this chapter.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
12.1 Introduction
The concept of targeted delivery of a drug to a desired region was envisioned as early as the 1900s when Nobel laureate Paul Ehrlich proposed the “magischekugel” or “magic bullet,” which embodied a targeting agent along with the drug [1]. Later with the increase in the use of nanomaterials for biomedical applications, the research in the field of targeted drug delivery experienced an exponential surge. Targeted drug delivery involves directing a therapeutic molecule or drug specifically and preferably only to its site of action. Therapeutic index of a drug molecule depends on its effective delivery in the active form to the target site. But in most of the cases, it is associated with the lack of target site affinity toward the pathological site causing off-target side effects and toxicity issues as well as high-dose requirement for efficacy. Nanosized drug delivery systems play a vital role as carriers for the delivery of active molecules to their target sites. The main requirements of an ideal targeted drug delivery system include retention, evasion, target specificity, and release. The drug/gene should be properly loaded into an appropriate delivery vehicle and protected from degradation in vivo, and in case of intravenous administration, it should possess a longer circulation time. The chemical conjugation or physical encapsulation of the active molecules within a carrier should not inactivate the cargo and the targeting ligand employed. Further, the drug delivery vehicle should be stable in vivo and reach the desired site of action before effectively releasing the encapsulated drug at a predetermined rate of release with minimal nonspecific accumulation. The drug carrier employed should be nontoxic, nonimmunogenic, preferably biodegradable, and easily eliminated from the body. The synthesis or fabrication of the targeted nanocarriers should be reasonably simple, reproducible, cost-effective, and industrially feasible [2,3,4].
Drug targeting may be broadly classified into first, second, and third order of targeting based on the target. First-order targeting or organ-level targeting utilizes a tissue or organ as the target, e.g., lymphatics, eyes, cerebral ventricles, etc. When the target is a specific cell like a tumor cell, macrophage, or Kupffer cell, it is referred as second-order targeting or cell-level targeting. Majority of the nanocarrier systems are designed for second-order targeting against specific cells. The third-order targeting involves targeting intracellular organelles and specific intracellular molecules like DNA inside the nucleus, mitochondria, Golgi apparatus, lysosomes, etc. Each level of targeting is associated with its own advantages and complexities. For instance, if all the cells in the targeted organ require therapeutic intervention, then organ-specific delivery may be preferred, whereas to target only specific diseased cells in an organ, cell targeting may be useful [2, 5, 6].
Intracellular targeting or the third level of targeting poses tremendous research opportunities as the site of action of most of the drugs are within specific organelles. For instance, pro-apoptotic drugs are targeted to mitochondria and lysosomes, anticancer drugs interfering DNA replication need to reach the nucleus, drugs interfering protein metabolism are targeted to endoplasmic reticulum (ER), and many other active pharmaceutical agents, including large molecules like proteins, antibodies, enzymes, etc., are to be delivered subcellularly for their therapeutic effect. In addition, gene delivery against several genetic disorders also demands delivery of specific DNA sequences or protein/nonprotein drugs to specific intracellular compartments. It is postulated that efficient localization of drugs in specific organelles can enhance treatment efficiency and reduce adverse effects. Passive accumulation of drugs within cells often leads to a nonuniform distribution between organelles. However, smart drug delivery systems equipped with specific residues like nuclear localization sequences/signals (NLS), organelle-specific signal peptides, mitochondriotropic residues, etc., which can alter the intracellular trafficking, can be envisioned to deliver their cargo at specific organelles. In-depth knowledge of molecular and cell biology, cellular uptake, as well as trafficking mechanisms is of prime importance while designing subcellular targeted drug carriers [7,8,9].
Another perspective to address the urgent need for overcoming drug resistance and improved efficacy is drug repurposing, which refers to the identification and discovery of novel therapeutic uses for already clinically approved drugs by screening them against relevant disease targets. A repositioned drug goes directly to preclinical and clinical trials, thus reducing risk and costs. The structural optimization, preclinical and/or clinical trials, and clinical safety analysis of such drugs have already been completed, and the toxicological, pharmacological, and clinical safety information is already available [10, 11]. Majority of the studies investigating nanocarriers for repurposed drugs are preclinical studies for antimicrobial and anticancer applications. One such drug is disulfiram, an anti-alcoholism drug that shows anticancer properties. However, its clinical application in cancer treatment is limited due to its very short circulation half-life. Several nanocarriers have been designed to improve the pharmacokinetic properties of disulfiram and enhance its anticancer efficacy [12,13,14]. The use of targeted nanocarriers for the repurposed drugs would reduce the risks and costs related to the failures in early stages of development and warrant enhanced clinical efficacy.
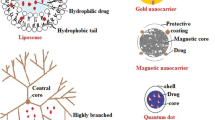
Currently, nanocarriers that have been clinically approved or under clinical trial are primarily developed to enhance pharmacokinetic and/or pharmacodynamic properties of drugs. In the majority of cases, these nanocarriers employ passive targeting, which involves nonspecific accumulation in the diseased tissue. Since 1995, about 50 nanopharmaceuticals are in clinical use after receiving the FDA approval. Table 12.1 provides few examples of the FDA-approved nanodrugs in clinical use with intracellular targets. Table 12.2 provides some of the nanomedicines undergoing clinical trials, while Table 12.3 provides examples of patents for intracellularly targeted nanocarriers.
12.2 Advantages of Targeted Drug Delivery
-
The main advantage of targeted drug delivery is that it enables preferential accumulation of the therapeutics in target cells versus normal cells, thereby minimizing the potential side effects and enhancing therapeutic efficacy as well.
-
Some of the pharmacokinetic shortcomings in terms of bioavailability, short half-life, large volume of distribution, etc. can be overcome as the pharmacokinetic behavior of the drug-loaded carriers depends on the delivery system as opposed to the encapsulated drugs.
-
Intracellular drug delivery via nanocarriers, in particular, is beneficial because the amount of drug required to exert therapeutic action is reduced significantly, which in turn reduces the side effects [26].
-
Multidrug resistance, a major hurdle in chemotherapeutic and antimicrobial drug therapy, can be to an extent overcome using intracellularly targeted nanocarriers. Since most of the transporter proteins recognize and expel drugs at the plasma membrane, internalized nanocarriers bypass this mechanism, thereby improving the efficacy of the drugs [27, 28].
-
When compared with drug conjugates, a nanocarrier system can simultaneously incorporate high density of drug and present targeting ligands at its surface. This enhances the ligand-target interaction through multivalency and subsequent internalization of the targeted carrier.
-
Targeted carriers can be designed to simultaneously deliver synergistic ligand molecules along with the encapsulated drug. This has been particularly advantageous in anticancer nanopreparations combining monoclonal antibodies with a chemotherapeutic drug, which were proven more beneficial than the drug alone or antibody alone [29,30,31].
12.3 Targeted Delivery Approaches
Active and passive targeting are the two key approaches explored for the targeted delivery of drug by nanosystems.
12.3.1 Passive Targeting Opportunities
The accumulation of drug or carrier system at the desired site of action owing to specific pathophysiological or anatomical factors is considered as passive targeting.
12.3.1.1 Pathophysiological Factors
Many diseases alter physiology and physiological functions of the diseased tissue, which can be used as a tool for intracellular targeting. Infection/inflammation leads to the release of various chemotactic mediators during tissue remodelling, which causes increased leukocyte extravasation. This pathophysiological abnormality leads to the increased vascular permeability of drug and drug carriers allowing extravasation and selective localization of the nanocarrier at the damaged tissue. This phenomenon, known as the enhanced permeation and retention (EPR) effect, is more pronouncedly used in anticancer drug targeting where solid tumors present more preferable conditions for drug accumulation [32, 33]. Angiogenesis recruits new blood vessels around the tumor to meet the demand of nutrition for the cells. But unlike the normal vasculature, this endothelium is leaky in between the adjacent cells leading to increased vascular permeability and reduced lymphatic drainage in tumors. However, a drug carrier system should have a longer circulation time to attain the EPR effect for passive targeting. Many nanosystems like liposomes, polymeric micelles, and nanoparticles target the tumor vasculature passively using EPR effect [34,35,36].
12.3.1.2 Anatomical Factors
These factors involve the delivery of the drug or drug carrier system directly into the anatomical region where the action of drug is desired. This is an indirect method of targeting the cells of a particular region like lungs, knee joints, eyes, etc. Here, the advantage of the anatomical entry of the drug has been taken into consideration in comparison with the traditional drug delivery system like tablets and capsules. This site-specific drug delivery prevents the unwanted exposure to the other tissues, which in turn avoids side effects [37, 38].
A classic example is delivery to the brain, which is limited due to the tight barrier of the blood-brain barrier (BBB) making the permeation of drug molecules difficult. Although various selective transport mechanisms like diffusion amd receptor-mediated or fluid-phase endocytosis play important roles in the absorption and transport of drugs via the BBB, the systemic administration and subsequent transport of therapeutic agents to the brain are still challenging. Efflux mechanisms are mainly responsible for preventing the drug delivery systems from reaching the target site. To overcome these challenges in brain drug delivery, microinjection technique or nose-to-brain drug delivery has been researched as alternatives. Microinjection technique involves the direct injection of the drug solution or nanocarrier system into the cerebrospinal fluid, which takes the drug to the brain. Nose-to-brain delivery utilizes the nasal pathway for the drug delivery to the brain. This leads to higher drug concentrations in the brain owing to bypassing of the BBB [39,40,41]. As an example, R Jain et al. developed and characterized micellar nanosystems of sumatriptan for intranasal delivery and further evaluated the biodistribution in rats. The nanomicellar carriers were found to be homogenous and spherical in shape. In vivo biodistribution and radiography studies revealed significantly higher sumatriptan brain uptake from the micelles as compared to sumatriptan drug solution given by nasal route. This investigation thus indicated the potential to target nanocarriers for brain drug delivery via nasal pathway [42].
12.3.1.3 Physicochemical Factors
Various physiological factors like size, surface charge, and hydrophilicity, which play an important role in the biodistribution and clearance of the nanocarriers, can be manipulated for passive targeting of the drug. Reticuloendothelial system (RES) clears 90% of the nanosystems out of the systemic circulation when injected intravenously from liver and spleen. This inherent tendency of nanosystems having size less than 100 nm to accumulate in the liver and spleen presents excellent opportunities for passive targeting to these organs. This has been utilized for the intracellular passive targeting of antiviral and antimicrobial agents. Although this approach is more promising for targeting to highly perfused organs, it holds the drawback of rapid clearance of the drug from the circulation. Many approaches have been researched and optimized to escape the RES uptake, improve the circulation of the nanosystems, and exhibit the action of the drug molecule at the desired site of action [43,44,45].
12.3.2 Active Targeting Opportunities
Passive targeting presents limited scope in drug delivery, and hence immense efforts have been directed toward active targeting of the drug or nanocarrier via modification with active ligands having selective affinity toward specific receptors or proteins on the cell membrane or lipid components of the cell compartments. A wide number of studies were carried on by direct coupling of a ligand to nanosystems like polymeric nanoparticles, liposomes, dendrimers, micellar systems, etc. to enhance the efficacy and minimize the off-target side effects of the drug. In many cases, the active-targeted nanosystems act as carriers to deliver the cargo to the inner compartments of the cell where they lack the entry phenomenon. In many diseased states, some receptors or surface antigens/proteins are expressed uniquely, or there is a structural or molecular change in the cellular membrane structure as compared to normal cells. Taking benefit of these changes, active agents like ligands, antibodies, or antigens have been extensively employed for active targeting. Various drugs are delivered by the active targeting approach at different receptors like folic acid receptors, LDL receptors, peptide receptors, G-protein-coupled receptors, etc. The following agents can be used as targeting moieties: antibodies and their fragments; lipoproteins; hormones; lectins; mono-, oligo-, and polysaccharides; and low molecular weight ligands like folate. Recently, monoclonal antibodies are the most commonly used vector molecules against characteristic tissue components.
The major targets involve different body compartments and pathologies like components of cardiovascular system, RES, lymphatic system, tumors, infarcts, inflammations, infections, transplants, etc. Currently, coupling a drug directly to the targeting ligand seems the easiest method for active targeting, for example, the development of direct drug-antibody conjugates has been explored for treatment of malignant diseases, such as cancer [46].
12.4 Design Considerations for Carrier-Mediated Intracellular Drug Targeting
Carrier-mediated passive targeting for intracellular delivery can be possible by utilizing pharmacological and physicochemical factors. Pathophysiological conditions such as leaky vasculature and change in pH of cancerous cells pave the way for passive targeting, specifically by modulating size, shape, surface charge, or composition of carrier.
12.4.1 Shape and Size
Particle size plays a vital role in pharmacokinetics of the drug-loaded carrier. Particle size affects the attachment, adhesion, cellular uptake, circulation half-life, and accumulation of the carrier [47]. Modulation of particle size can also help in avoiding or encouraging cellular uptake by endocytosis [48, 49]. Small nanoparticles having size 10–20 nm exhibit extensive accumulation in several organs by crossing the tight endothelial junctions and show rapid hepatic as well as renal clearance. Thus, having carrier particle size greater than 20 nm can ensure avoidance of clearance by filtration through the kidneys [50, 51]. Polymeric particles and liposomes with higher particle size (200 nm–few μm) generally exhibit phagocytic uptake. So nanocarriers of size between 10 and 100 nm are ideal [52]. Particle size not only affects the mode of cellular uptake but can also mediate the essential molecular processes for regulating cellular functions [53]. The smaller molecules easily diffuse, while EPR effect dominates in the case of larger and long-circulating nanocarriers (> 100 nm) due to lack of effective lymphatic system [54].
Apart from size, particle shape is also a strong determinant of cellular uptake of the carrier. Although traditionally, spherical nanocarriers such as polymeric nanoparticles, liposomes, and micelles dominated the targeted delivery research, lately it has been observed that non-spherical shapes have great potential as drug delivery vectors. Non-spherical carriers of ellipsoid, rod, and worm shapes offer several advantages in terms of improved drug delivery efficiency owing to high drug loading efficiency, long circulation time, enhanced attachment and binding affinity to target cells, and better cellular uptake [55, 56]. Sharma et al. showed that nanoparticles with at least one extended axis, like prolate ellipsoids, are promising long-circulating drug carriers. Non-spherical particles bypassed phagocytosis because of incomplete actin structure formation [57]. Particle shape was also found to influence attachment and internalization during phagocytosis [58]. Yoo et al. compared non-spherical geometry of elliptical disks with spherical geometry and showed that the former exhibits slow uptake kinetics with equilibrium distribution of particles in cells [59].
12.4.2 Composition
The composition of subcellular targeted nanocarriers designed to deliver drug intracellularly through either passive or active means has also shown to influence their trafficking. Inclusion of negatively charged phospholipids such as phosphatidylserine and phosphatidyl glycerol in multilamellar vesicles containing phosphatidylcholine greatly favored the binding and phagocytosis by macrophages as compared to neutral phospholipids [60]. However, nanocarriers internalized via the endocytic pathway get entrapped in the endosome and lysosome and eventually get degraded by the action of the lysosomal enzymes. Therefore, several strategies have been attempted to achieve delivery of nanocarriers like liposomes, micelles, etc. into the cell cytoplasm, circumventing the endocytic pathway.
Torchilin et al. showed that incorporation of different polymers into liposomes can result in enhanced circulation time as a function of concentration. In addition, the use of pH-sensitive carriers, which destabilize endosomal membrane at low pH and liberate the loaded cargo into the cytoplasm, is a promising approach to avoid lysosomal degradation. [61, 62] Micelles, including polymeric micelles, are also widely studied pharmaceutical carriers owing to their smaller size, in vivo stability, feasibility to load water insoluble anticancer drugs, and prolonged circulation times [63]. Passive targeting of micelle is possible due to the small micellar size and the EPR effect. Modification of composition of amphiphilic polymer micelles with phosphatidyl ethanolamine and lipid moieties as hydrophobic blocks that cap hydrophilic polymer chains endows additional advantages like particle stability and enhanced accumulation [64]. Further modification of these micelles with cationic lipids may improve the internalization of drug-loaded micelles within cells and facilitate the escape from endosomes to enter the cytoplasm [65].
12.4.3 Surface Characteristics
Surface charge of nanoparticles shows significant impact on the circulation, biodistribution, internalization, and trafficking. It also effects the opsonization by macrophages, which further affects their biodistribution [47]. Anionic cell membrane shows better interaction with positively charged nanocarriers leading to higher phagocytic uptake and less circulation time than negatively charged nanocarriers [66, 67]. Conversely, it has also been demonstrated that neutral and cationic nanoparticles exhibit limited internalization of particles by RES and are cleared less rapidly than the anionic ones [68]. Xiao et al. studied both cationic and anionic nanocarriers for their in vivo fate. This study demonstrated that nanocarriers with high positive or negative surface charge get internalized nonspecifically by macrophages in vitro and in vivo, resulting in high liver uptake after systematic administration [69]. Further, upon investigating the uptake of both cationic and anionic nanocarriers in phagocytic and non-phagocytic cells, it was observed that a slightly negative surface charge of nanocarriers was optimal for use as drug delivery carriers in cancer therapy [68].
Apart from charge, surface hydrophobicity can also affect the opsonization, phagocytosis, blood circulation, and biodistribution of nanocarriers [47]. As hydrophobic nanocarriers are preferentially coated and scavenged by RES, increasing the surface hydrophilicity is seen as a promising strategy to evade RES. PEGylation of nanocarriers such as dendrimers, polymeric nanoparticles, liposomes, etc. is one of the most explored strategies to prolong circulation half-life and improve the accumulation of nanocarriers in tumor cells [70]. PEGylated proteins, micelles, and low molecular weight drugs showed improved therapeutic efficacy by passive targeting in a novel way [71].
12.4.4 Target Specificity
Active targeting is preferred for the subcellular targeted delivery of macromolecular drugs such as DNA, siRNA, and proteins. However, nanocarriers upon endocytosis may undergo degradation, which may not be desirable for nucleic acid or macromolecules delivery. Such drugs must be thus delivered to specific cellular organelles like nuclei, lysosomes, mitochondria, etc. to exert their therapeutic action. For example, to overcome the enzymatic degradation as well as poor cellular uptake and endosomal escape of nucleic acid therapeutics like antisense oligonucleotides, small interfering RNA, etc., viral vectors have been employed. Viral vectors such as adenoviruses, herpesviruses, hepadnaviruses, influenza viruses, etc. have been investigated for gene therapy, but these showed several drawbacks such as toxicity, immunogenicity, and limitation in the size of the plasmid to be inserted. Polyelectrolytes diffuse passively into the nucleus and tend to be retained due to cationic histone and anionic nucleic acids [72]. Complexes with cationic polymers like chitosan, poly-L-lysine and poly(ethyleneimine), and lipoplexes (complexes with cationic lipids) have also been employed for nucleus targeting [73].
Lysosomal targeting strategies mainly revolve around two main objectives: (i) to directly target lysosomes through receptor-mediated endocytosis and (ii) to protect the cargo molecule from lysosomal degradation and make it available in the cytoplasm for further action [74]. Similarly, the distinct mitochondrial features including high membrane potential across the inner mitochondrial membrane, the organelle’s protein import machinery, and the mitochondrial fusion process have been exploited for developing a targeting strategy to the mitochondria within living mammalian cells [75]. Lipophilic cations owing to their cationic charge and hydrophobic surface area possess low activation energy for their movement across the membrane and, hence, can easily transverse across the plasma membrane and the mitochondrial membranes. Triphenylphosphonium (TPP) cation was originally used to assess the mitochondrial membrane potential, and its uptake into mitochondria is well recognized. It can be easily incorporated into a compound late in the chemical synthesis scheme, typically by displacing a leaving group [76]. Mitochondrial targeting signal (MTS) peptide can be used to deliver proteins to the mitochondrial matrix. The MTS sequence leads the cargo protein to the mitochondria and is then cleaved enabling localization and function of the fused protein [77].
The various opportunities for subcellular targeting to the different organelles have been discussed in detail in the following sections.
12.5 Opportunities in Intracellular Drug Delivery
Recent advances in molecular biological techniques have led to the detailed understanding of the pathophysiology of diseases. This lead to the identification of newer cellular and molecular targets for drug discovery and imaging purposes. Further, the integration of the computer-aided drug designing along with molecular biology has opened paths for the target-specific drug molecules or drug delivery carriers. However, the molecular complexity and inaccessible drug targets lead to the evolvement of novel nanodrug carrier systems as the most desirable option. Several nanodrug delivery systems were designed to target intracellular organelles. Treatment strategies against a host of diseases have been explored by targeting the cellular organelles like mitochondria (cancer, diabetes mellitus, cardiomyopathy), Golgi apparatus (Alzheimer’s disease, CDG syndrome), ER (cystic fibrosis), lysosomes (Tay-Sachs diseases, autoimmune diseases), plasma membrane (familial hypercholesterolemia, infectious diseases), as well as the nuclear envelope (progeria, muscular dystrophy) (Fig. 12.1).
12.5.1 Nuclear Targeting
Nucleus is the eukaryotic cell controller responsible for the regulation of gene expression, transcription, and translocation of proteins from nucleus to cytoplasm for various cellular processes. The human nuclear genome database contains two copies each of 3.2 billion base pairs, of which only 2% codes for 30,000 diverse proteins. Several disorders like cancer, heart dysfunction, and neurodegenerative and other brain diseases are manifestations of mutations in the promoter/enhancer regions of these genes and their splice sites. Various drugs used in the treatments of cancer act at the DNA to prevent the transcription of genes. However, only some of the total drug administered translocate into the nucleus from the cytoplasm to exert its action, which ultimately warrants a higher dose of the drug to be administered. In addition, proliferating cells develop genetic changes, which may lead to resistance to a particular drug. This may also result in the generation of new drug-resistant daughter cells, which have the properties of the parent cells. This necessitates the need for nanoparticle-based delivery systems for direct and effective nuclear delivery of drugs or plasmids to avoid the adverse drug reactions [78,79,80,81,82].
The main barriers for nuclear-targeted carriers are in the form of cell membrane, entrapment and degradation in endo-/lysosomes, cytoplasmic trafficking, and nuclear membrane. The smaller nanoparticles (< 25 nm) have been found to enter the cells passively, while the larger nanocarriers are taken up by endocytosis and traverse the endolysosomal pathway or get trafficked to other organelles or exocytosed. Nanocarriers modified with ligands targeting LDL receptors, transferrin receptors, epidermal growth factor receptors, etc. undergo clathrin-mediated endocytosis and ultimately get degraded in the lysosomes. Ligands like folic acid, albumin, cholesterol, etc. have been found to assist in caveolae-mediated and lipid raft endocytosis that allow bypassing of endosomal pathway, cytoplasmic trafficking, and delivery to non-lysosomal compartments by activating signal transduction cascade [83]. Nuclear pore complex (NPC), a central perforated channel of 9 nm, plays a vital role in all the passive and active transport of the molecules measuring less than 50 kDa across the nuclear envelope. Molecules larger than 50 kDa need assistance from NLS and NPC. NLS specifically interacts with the NLS receptor in an energy-dependent recognition successively docking the cargo by an energy-dependent translocation and subsequent release into the nucleus [84]. Several viral-mediated gene delivery strategies have been developed following the advances in the field of viral infection mechanisms. Adenovirus type 2 and type 5, the most commonly studied virus for gene delivery, get endocytosed by the epithelial cells, enter the cytosol in an integrin-dependent manner, and are translocated to a microtubule organizing complex and then nucleus [85]. Simian virus has also been investigated to facilitate caveolae-mediated endocytosis, and simian virus NLS have been employed to assist nanocarriers in nuclear localization [86]. Viral-mediated nuclear delivery offers an advantage of high translocation efficiency, but their use in drug delivery is limited owing to the considerable toxicity associated with the viral components. Various non-viral vectors (liposomes, nanoparticles) have also been surface modified with the identified NLS sequences for nuclear-targeted gene delivery. The NLS-modified carriers bind and interact with the NLS binding domain of a cytoplasmic transporter, importin-α, and the resultant complex then binds to importin-β. The final complex then interacts with nucleoporins and docks into the NPC effecting nuclear entry [87].
Liposomes, with their phospholipid bilayer nature, are unique because of their ability to fuse with cell membrane. Upon entering the cell by fusion, the liposomes avoid endosomal entrapment and deliver their cargo to the cytoplasm. However, liposomes also get endocytosed, fuse with the endosomal membrane, and release their cargo in the cytoplasm after endosomal escape [88, 89]. The chances of nuclear delivery have been found to increase if the nanocarrier is modified to avoid the endolysosomal pathway. Cell-penetrating peptides and various small viral peptides, like KKKRKV from SV40 large T antigen, fusogenic peptides like HA2 peptide from influenza virus hemagglutinin, etc., have also shown effective nuclear localization and, hence, are used for nuclear delivery [84, 90]. Certain cationic lipids and polymers complexed with DNA, known as lipoplexes and polyplexes, respectively, have also been developed to deliver DNA into the nucleus and are in the clinical trials for the treatment of melanoma [91, 92]. Another study showed that a complex of plasmid DNA and low molecular weight protamine efficiently translocated into the cell and then entered the nucleus due to the structural similarity of protamine with HIV-TAT peptide [93]. Few examples of nuclear-targeted nanocarriers are given in Table 12.4.
12.5.2 Mitochondrial Targeting
Mitochondria, known as the powerhouse of the cell, provide adenosine triphosphate, ATP, to the cell by oxidative phosphorylation. They are also associated with other metabolic pathways, like the citrate cycle, fatty acids oxidation, and the synthesis of hormones and gluconeogenesis. Mitochondrial dysfunction and somatic mutations contribute to various human disorders, like obesity, diabetes, cardiomyopathy, Parkinson’s, kidney and liver diseases, and stroke to name a few. Mitochondria have a vital role in apoptosis, and the mutations in apoptosis-related genes, viz., p53, PTEN, and Bcl-2, and their homologues cause chemoresistance in most cancers. They also regulate the concentration of intracellular calcium ion and reduce the oxidative stress by oxidative phosphorylation via the mitochondrial respiratory chain. The multiple functionality of mitochondria thus makes them a major target in pharmacological interventions. Reduction in oxidative damage and calcium overload could prevent mitochondrial damage. Several strategies for targeting the mitochondria and nullifying the effect of mutant genes have been employed for treating mitochondrial gene mutations [100,101,102,103,104].
Several clinically used drugs, such as paclitaxel, etoposide, lonidamine, ceramide, etc., act on mitochondria directly and cause apoptosis. One of the attempts to target the mitochondria is through transmembrane electrochemical gradient, contributed from both negative membrane potential and pH difference (acidic outside). Owing to the negative membrane potential, cationic molecules get attracted by the mitochondria. Vitamin E covalently coupled to a mitochondrotropic molecule, TPP cation, was driven across the mitochondrial inner membrane due to a large membrane potential ranging from –150 to –180 mV. This leads to higher accumulation of vitamin E in mitochondrial matrix as compared to its native form. TPP cation has also been explored to realize mitochondrial delivery of antioxidants like coenzyme Q, ubiquinone, nitroxides, peptide nucleic acids, cyclosporin A, etc. [105, 106]. Another strategy for mitochondrial targeting involves MTS, i.e., mitochondrial targeting sequence. MTS are nonspecific and have similar physiochemical properties of the mature protein of which they are a part of. There are several studies attempting gene therapy involving restriction enzymes that are targeted to the mitochondria using MTS. An example of such an attempt involves targeted delivery of the restriction endonuclease Sma1 to mitochondria and consequent removal of mutant mitochondrial DNA [107].
Another approach involves a molecule or nanocarrier that possesses specific mitochondrial affinity. Dequalinium chloride (DQA), a single-chain bola mitochondriotropic amphiphile having two delocalized positive charge centers, has been found to specifically accumulate in the mitochondria of cancer cells. Weissig et al., in 1998, first proposed DQA-based liposome-like vesicles (DQAsomes) as a mitochondrial-specific drug delivery system. These bola-like amphiphiles (bolasomes) form cationic vesicles with diameters between 70 and 700 nm entrapping various drugs and DNA and transport them to mitochondrion. Later, it was demonstrated that DQAsomes conjugate with DNA and release it in mitochondria after entering the cells [108,109,110,111,112]. It was also attempted to target liposomes to mitochondria by modifying with a mitochondrial membrane fraction. The incorporation of stearyl triphenylphosphonium (STPP) in liposomes enabled the stearyl residue of STPP to act as an anchor for the TPP residue that would result in a liposomal formulation having an inherent predisposition for mitochondria [113]. In another study, the octaarginine residues used to modify liposomes enabled cell entry via macropinocytosis, while the lipid composition of the liposomes facilitated preferential fusion with the mitochondrial membrane and release of the encapsulated cargo in mitochondria [114, 115]. TPP modified N-(2-hydroxylpropyl) methacrylamide nanoparticles and inorganic nanoparticles like amorphous silica nanocages were also explored for mitochondria-specific delivery although the exact mechanism of mitochondrial accumulation of silica nanocages was not clear [116, 117].
12.5.3 Lysosomal Targeting
Lysosomes are single membrane-bound, subcellular organelles with acidic pH and approximately 60 hydrolases that can degrade various biological molecules. They also play a role in the recycling of cell surface molecules and receptors. Macromolecules reach the lysosome exogenously via phagosomes or endosomes and endogenously via autophagy. Certain inherited diseases like Tay-Sachs disease, Gaucher’s disease, Fabry disease, Niemann-Pick disease, etc. are manifestations of the deficiency of some lysosomal enzymes (lysosomal storage diseases) and can be treated only by administering exogenous enzymes. Several glucosidases, glucocerebrosidase, phenylalanine ammonia lyase, and other enzymes are used for treating lysosomal storage diseases. For many disease conditions, the treatment with purified exogenous enzymes shows very encouraging results than with native enzymes. Treatment with native enzymes gives short-term relief only because of short biological half-life and relatively inefficient lysosomal transport [118,119,120]. Liposomes were researched as carriers for replacement enzymes that could avoid inactivation of enzymes and improve their intracellular delivery and lysosomal transport. G Gregoriadis studied the biodistribution of β-fructofuranosidase entrapped in liposomes composed of phosphatidylcholine, phosphatidic acid, and cholesterol. It was shown that after 6 h and 48 h, 45% and 25% of the administered enzyme activity, respectively, was shown to be accumulated in the liver. It is of prime importance that about 50% of the intracellular enzyme activity is localized within the lysosomal fraction. Similar kind of study attempted the intravenous administration of α-mannosidase and neuraminidase encapsulated in liposomes [121, 122]. Recently, several targeting ligands like folate, RGD, rhodamine, transferrin, etc. were also employed to functionalize liposomes and enhance their lysosomal delivery [123, 124].
A transmembrane glycoprotein called intercellular adhesion molecule-1 (ICAM-1) has been widely explored to facilitate lysosomal delivery of nanocarriers. Anti-ICAM-1 antibody-functionalized polymeric nanoparticles, solid-lipid nanoparticles, polyelectrolyte complexes, etc. were developed against Pompe disease, Gaucher’s disease, and Fabry disease [125,126,127,128]. Lysosomotropic agents like octadecyl rhodamine B, anti-LAMP1 antibodies, Gly-Leu-Phe-Gly peptide, etc. induce permeability of lysosomal membrane and release of hydrolytic enzymes and reactive oxygen species resulting in apoptosis of cells. Such agents have been used to functionalize nanocarriers and enable their preferential accumulation in lysosomes and release of their cargo, eventually leading to cell death [129,130,131]. Lysosomal targeting has also been explored to direct nanocarriers like single-wall carbon nanotubes, polybutylcyanoacrylate nanoparticles, gold nanoparticles, etc. and induce autophagy in neurodegenerative diseases, infectious diseases, as well as autoimmune disorders [132,133,134]. For several therapies, it is required that the drug/nanoencapsulated cargo need to escape from the endo-/lysosome and get released to the cytoplasm. In such cases, “pH buffering” or “proton sponge” effect caused by polyethylene imine, polyamidoamines, lipopolyamines, etc. is employed to cause endo-/lysosomal escape. Membrane disruptive agents like poly(acrylic acid), polyethylacrylic acid, pyridyldisulfide acrylate, etc. can also be employed to achieve the same [135,136,137].
12.5.4 Golgi/ER Targeting
Golgi apparatus is one of the key organelles of the cell secretory pathway and has functions similar to ER. It is mainly involved in the posttranslational modification of newly synthesized proteins and synthesis of carbohydrate and proteoglycans structures like glycosaminoglycans and polysaccharides. Certain alterations in the Golgi apparatus caused by pharmacological agents, pathological changes, and overexpression of associated proteins result in various neurodegenerative disorders including Alzheimer’s, Parkinson’s, Niemann-Pick disease, etc. Further, the Golgi apparatus and the ER are also involved in development of targeted anticancer therapy against androgen-dependent and androgen-independent prostate cancer [138,139,140].
The ER, a system of folded membrane tubules and sacs extending from the nuclear membrane, is responsible for the folding of secretory and membrane proteins, calcium storage, calcium signalling, and apoptosis regulation. The absence or misfolding of a protein or the presence of a mutant protein can lead to ER storage diseases like familial hypoparathyroidism, familial central diabetes insipidus, chronic pancreatitis, etc. [141, 142]. Targeting mammalian target of rapamycin (mTOR), the central regulator of cell growth and proliferation (e.g., by rapamycin), is an example of targeting Golgi body or ER as an anticancer therapy [143, 144]. Some polymeric nanocarriers like polycaprolactone and PLGA nanoparticles were found to accumulate in the Golgi-associated vesicles of late endosomes and hence can be used for Golgi/ER targeting [145, 146].
12.6 Challenges in Intracellular Drug Delivery
The key problem in targeted delivery of different pharmaceutical active molecules is the intracellular transport, especially to the subcellular organelles. Successful drug targeting requires not just performance at the target site and drug receptor interactions but also (a) high drug loading, (b) drug retention in active form within the carrier until it reaches the target site, and (c) the pharmacodynamically appropriate drug release upon reaching the desired site of action. The drug loss from the carrier due to release or degradation, uptake into nontarget sites, or reduction in drug activity due to protein sequestration may result in failure of the drug delivery system to deliver its cargo in sufficient quantities at the site of action or suboptimal drug release rate limiting therapeutic effects. Further, limited knowledge about the physical, biophysical, or biological nature of the target sites and the therapeutic drug levels required at the individual organ or cell level may result in failure of in vivo experiments. Although it is necessary that the drug remains encapsulated during circulation, conversely, it may bind so tightly that it is not released at the target site. The recirculation of drug carriers further increases opportunities to interact with the target but also sustains the duration of the carrier in the circulation, increasing the risk of drug leakage. In addition, there is untimely drug loss in the case of time-dependent drug release, rather than triggered by some mechanisms (pH change or enzymatic reaction) [147]. Further, if it is difficult for free drug molecules in accessing tissues, the same problem may exist for the drug within a carrier, even if it is taken in considerable quantities to the core of the target and then released. Even after safe delivery of drugs into the cytoplasm, it is still challenging to reach the specific organelles like nuclei, lysosomes, mitochondria, etc., where they are expected to exert their therapeutic effect [148]. This is the main hurdle in the case of gene delivery where the prime requirement is to release the cargo inside the nucleus. In both non-viral and viral vector-mediated gene delivery, uptake and movement toward the nucleus are decisive. Some early initial trials with different vectors were encouraging; however, the latest results have posed certain concerns. In many instances, aggregation of nanocarriers in circulation may happen, resulting in the change of the desired particle size critical to reach targets or interact with receptors. Studies on the oral delivery and uptake of nanoparticles have clearly shown the limited size-dependent internalization of particles below 100 nm by endothelial enterocytes and the M cells in Peyer’s patches in the order of 5% of the administered dose. There is little success to increase the uptake and bioavailability in turn by using absorption enhancers or efflux inhibitors [149]. The probability of an individual nanoparticle recognizing and attaching to a receptor is also low, especially in dynamic blood circulation interactions. To counteract this, a large numbers of particles may be administered, and a specific number of particles need to be engaged to bring about a therapeutic effect [150]. Further, adhesion of the nanocarrier to the target does not necessarily lead to cellular uptake. Even if it does, the carrier may not release the cargo within the cytoplasm or may be thrown out of the cell. Therefore, the probabilities of adhesion, uptake, diffusion, and escape from the cell into the adjacent ones should be taken into consideration [151, 152]. Another factor to be considered while designing the targeted carrier is the fact that targets can also change; tumors grow and are heterogeneous depending on their susceptibility to chemotherapy [153]. The properties of nanosystems also undergo continuous phase changes when they are administered. For example, the stability of an aqueous formulation is altered when injected into the blood. The differences in the viscosity of bimodal dispersions from that of monodisperse and polydisperse colloidal suspensions have also been established [154, 155]. Further, the particle flow profile is also dependent on the pressure during flow in circulation, the particle size and distribution, the flocculation tendency, and the tube diameter. Several studies of particle flow have been conducted to analyze the interaction of nanoparticles with surface receptors without considering biological applications in mind. In concentrated Brownian suspensions, an initially uniform suspension can become less concentrated near the walls and more concentrated near the axis of the channel. On the other hand, the circulating particles drift toward the vessel walls in the microcirculation due to margination [156, 157]. Unlike cellular uptake, which may be a size-dependent process, the diffusion in the cytoplasm is dependent on various factors like concentration gradients, particle diameter, physical obstruction effects, and the gel-like nature of some regions [53]. The NPC with its 8-nm-diameter limit for passage of particles presents the final barrier for gene delivery. Thus, multistage drug delivery involving the use of micro- and nanosystems nested together may help in successful delivery and targeting by overcoming some of the barriers. While the inclusion of nanosystems within microsystems may protect the former while in circulation, the downstream events may be affected by other variables [158, 159].
12.7 Toxicological Considerations in Intracellular Nanoparticulate Delivery
The nanotechnology-based drugs are either aimed to improve release or uptake of agents into target cells or to reduce toxicity associated with the agents. Although a nanoparticle delivers the drug into or at the vicinity of target organs, recently several findings have reported unexpected toxicities owing to nanoparticles, leading to the origin of the field of nanotoxicology. However, the fundamental cause-effect relationships are not very well defined or explored in detail. Hence, there is an urgent need of studies to demonstrate and identify different structural elements causing cyto- and organ toxicity. Nanomaterial first interacts with proteins or cellular components of cells and causes deleterious toxic effects. Several in vitro and in vivo experimental studies have reported the potentially harmful effects of nanoparticles and identified key physicochemical properties like particle size, composition, charge, surface area, agglomeration, and dispensability influencing nanoparticle toxicity [160, 161]. Particle size is one of the significant factors influencing nanoparticle toxicity, and it varies in different dispersion mediums such as deionized water and cell culture media. The nanoparticles having size less than 100 nm are postulated to possess suitable mechanical, electrical, and chemical properties that are essential for drug delivery. These smaller particles can pass through the BBB and also trigger immune reactions as well as damage cell membranes. For example, in vitro cytotoxicity study with 1.4 nm and 15 nm gold nanoparticles in connective tissue fibroblasts, epithelial cells, macrophages, and melanoma cells showed that particles of 15 nm size are nontoxic, but 1.4 nm gold particles efficiently inhibited the growth at the same concentration [162]. Owing to their small size, the nanoparticles offer higher surface area for the interaction with biological membranes and tissues making them more susceptible to toxicity. The surface properties such as composition, charge, and porosity are important factors affecting nanoparticle-associated toxicity [163]. Nanoparticle composition and surface charge, generally indicated by zeta potential, can affect tissue accumulation and toxicity. Zeta potential reflects the electrical potential of the nanosystems imparting physical stability to the system as well as the tissue affinity in the circulation. For example, cationic liposomes can result in dose-dependent toxicity and pulmonary inflammation in in vivo models. DOTAP, a monovalent cationic lipid and lipofectamine, a multivalent cationic liposome, accumulate in the vasculature and can be preferentially internalized by the liver and the spleen. Stearylamine, the first-generation monoalkyl cationic lipid, causes hemagglutination and hemolysis of human erythrocytes. Hence, their use in humans is not recommended for drug delivery [164, 165]. Nanoparticles tend to agglomerate via Brownian motion and van der Waals forces due to the increased surface area to volume ratio. Prevention of agglomeration is a key factor during clinical use of nanoparticles since this may alter the physicochemical properties such as size distribution, surface to volume ratio, surface activity, as well as concentration of nanoparticles. This in turn affects the potential toxicity of nanoparticles due to vascular or lymphatic blockage. Several preventive measures like sonication, detergents, lung surfactants, PEG, and serum can prevent agglomeration to decrease toxicity or deleterious side effects [166, 167].
Considering the risk associated with nanoparticles, detailed characterization of nanoparticles and validated procedures are necessary for the assessment of nanoparticles. Nanoparticle possesses special characteristics, which impose a higher challenge in assessing toxicity using classical assays. Furthermore, lack of standardized guidelines for nanoparticle toxicological characterization could impede movement of these agents to the clinic [168]. Characterization of physicochemical properties, cellular and noncellular in vitro toxicity assays, and animal-based toxicological assessment are the key elements needed to evaluate the potential toxicity. Chemical composition, particle size and distribution, agglomeration, density, shape, and surface properties such as area as well as charge are the physicochemical properties that may influence the toxic effects of nanomaterials [169, 170]. In addition, various in vitro assessments should be done for the safety and efficacy of nanoparticles like biocompatibility assays, hemolysis and platelet aggregation assay, immune system activation assay, reactive oxygen species and oxidative stress measurements, genotoxicity assay, mutagenicity assay, etc. [171].
12.8 Conclusion
Novel and improved therapeutic strategies evolve with the discovery of molecular basis of diseases, new intracellular targets, and the mechanisms to specifically target them. Though significant strides have been made in the direction of organelle-targeted drug delivery in the recent past, this field of research demands more competence. There have been few partially successful, yet promising, attempts at directing therapeutics to the cytoplasm or individual organelles. Most of them provide qualitative analysis of intracellular sequestration of drugs based on the cell line or in vitro experiments. Sensible selection of materials and physical attributes of drug carriers, real-time molecular and functional study of the various uptake mechanisms, and the interaction of these carriers with cellular components are of paramount importance while designing organelle-targeted nanocarriers. Another important factor to be considered is the intracellular fate and subsequent disposition of these carriers warranting detailed nanotoxicological evaluations of the developed drug delivery systems. Although the goal of organelle-targeting seems challenging now, utilizing innovative nanomaterial and molecular biology advancements can help in the success of this new paradigm in nanomedicine to achieve a realistic clinical outcome. Further, innovative strategies like drug repurposing in combination with nanotechnology advancements can help in overcoming the high attrition rates, high costs, and slow pace of new drug discovery.
References
Strebhardt K, Ullrich A (2008) Paul Ehrlich’s magic bullet concept: 100 years of progress. Nat Rev Cancer 8:473–480
Torchilin VP (2000) Drug targeting. Front Biopharm 11:S81–S91
Singh R, Lillard JW (2009) Nanoparticle-based targeted drug delivery. Spec Issue Struct Biol 86(3):215–223
Bae YH, Park K (2011) Targeted drug delivery to tumors: myths, reality and possibility. J Control Release Off J Control Release Soc 153(3):198–205
Kleinstreuer C, Feng Y, Childress E (2014) Drug-targeting methodologies with applications: a review. World J Clin Cases 2(12):742–756
Syjk N (2014) Novel drug delivery systems and regulatory affairs. S Chand & Company Limited
Himri I, Guaadaoui A (2018) Chapter 1 – cell and organ drug targeting: types of drug delivery systems and advanced targeting strategies. In: Grumezescu AM (ed) Nanostructures for the engineering of cells, tissues and organs. William Andrew Publishing, Oxford, pp 1–66
Prokop A, Davidson JM (2008) Nanovehicular intracellular delivery systems. J Pharm Sci 97(9):3518–3590
Sakhrani NM, Padh H (2013) Organelle targeting: third level of drug targeting. Drug Des Devel Ther 17(7):585–599
Li YY, Jones SJ (2012) Drug repositioning for personalized medicine. Genome Med 4(3):27–40
Padhy B, Gupta Y (2011) Drug repositioning: re-investigating existing drugs for new therapeutic indications. J Postgrad Med 57(2):153–160
Triscott J, Rose Pambid M, Dunn SE (2015) Concise review: bullseye: targeting cancer stem cells to improve the treatment of Gliomas by repurposing disulfiram. Stem Cells 33(4):1042–1046
Wang Z, Tan J, McConville C, Kannappan V, Tawari PE, Brown J et al (2017) Poly lactic-co-glycolic acid controlled delivery of disulfiram to target liver cancer stem-like cells. Nanomed Nanotechnol Biol Med 13(2):641–657
Pushpakom S, Iorio F, Eyers PA, Escott KJ, Hopper S, Wells A et al (2018) Drug repurposing: progress, challenges and recommendations. Nat Rev Drug Discov 18:41–58
Ventola CL (2017) Progress in nanomedicine: approved and investigational nanodrugs. P T Peer-Rev J Formul Manag 42(12):742–755
V Torchilin, R Rammohan, T Levchenko, N Volodina (2005) – Intracellular delivery of therapeutic agents. US Patent App. 10/503,776
Benenato K, Kumarasinghe E, Cornebise M (2017) Compounds and compositions for intracellular delivery of therapeutic agents. US patent US20170210697 A1
Zalipsky S, Allen T, Huang S (2002) Liposome composition for improved intracellular delivery of a therapeutic agent. US Patent US20020192275A1
Galindo SM, Muzykantov VR, Schuchman EH (2006) Targeted protein replacement for the treatment of lysosomal storage disorders. WO2006007560
Dattagupta N, Das AR, Sridhar CN, Patel JR (1998) Method for the intracellular delivery of biomolecules using liposomes containing cationic lipids and vitamin D. US Patent US5711964A
Felgner PL, Kumar R, Basava C, Border RC, Hwang-Felgner J-Y (1995) Cationic lipids for intracellular delivery of biologically active molecules. US Patent US5459127A
Berry D, Anderson D, Lynn D, Sasisekharan R, Langer R (2006) Methods and products related to the intracellular delivery of polysaccharides. US Patent US20060083711A1
Gieseler R, Marquitan G, Scolaro M, Schwarz A (2007) Carbohydrate-derivatized liposomes for targeting cellular carbohydrate recognition domains of Ctl/Ctld lectins, and intracellular delivery of therapeutically active compounds. US Patent US20070292494A1
Lakkaraju A, Dubinsky J, Low W, Rahman Y-E (2003) Anionic liposomes for delivery of bioactive agents. US Patent US20030026831A1
Akita H, Fujiwara T, Harashima H (2009) Liposome for targeting golgi apparatus. Japanese Patent JP2009286709A
Fahmy TM, Fong PM, Goyal A, Saltzman WM (2005) Targeted for drug delivery. Mater Today 8(8, Supplement):18–26
Schinkel AH, Jonker JW (2003) Mammalian drug efflux transporters of the ATP binding cassette (ABC) family: an overview. Drug Efflux Transp Implic Drug Deliv Dispos Response 55(1):3–29
Huwyler J, Cerletti A, Fricker G, Eberle AN, Drewe J (2002) By-passing of P-glycoprotein using immunoliposomes. J Drug Target 10(1):73–79
Nowak AK, Robinson BWS, Lake RA (2003) Synergy between chemotherapy and immunotherapy in the treatment of established murine solid tumors. Cancer Res 63(15):4490–4496
Pegram M, Hsu S, Lewis G, Pietras R, Beryt M, Sliwkowski M et al (1999) Inhibitory effects of combinations of HER-2/neu antibody and chemotherapeutic agents used for treatment of human breast cancers. Oncogene 18:2241–2251
Czuczman MS, Grillo-López AJ, White CA, Saleh M, Gordon L, LoBuglio AF et al (1999) Treatment of patients with low-grade B-cell lymphoma with the combination of chimeric anti-CD20 monoclonal antibody and chop chemotherapy. J Clin Oncol 17(1):268–276
Edens HA, Levi BP, Jaye DL, Walsh S, Reaves TA, Turner JR et al (2002) Neutrophil transepithelial migration: evidence for sequential, contact-dependent signaling events and enhanced paracellular permeability independent of transjunctional migration. J Immunol 169(1):476–486
Schiffelers RM, Storm G, Bakker-Woudenberg IAJM (2001) Host factors influencing the preferential localization of sterically stabilized liposomes in klebsiella pneumoniae-infected rat lung tissue. Pharm Res 18(6):780–787
Matsumura Y, Maeda H (1986) A new concept for macromolecular therapeutics in cancer chemotherapy: mechanism of tumoritropic accumulation of proteins and the antitumor agent smancs. Cancer Res 46(12 Part 1):6387–6392
Maeda H, Wu J, Sawa T, Matsumura Y, Hori K (2000) Tumor vascular permeability and the EPR effect in macromolecular therapeutics: a review. J Control Release 65(1):271–284
Toyokazu U, Hiroaki S, Kohtaro A, Yasuharu M, Tsuyoshi H, Keiji O et al (2003) Application of nanoparticle technology for the prevention of restenosis after balloon injury in rats. Circ Res 92(7):e62–e69
Guzman Luis A, Vinod L, Cunxian S, Yangsoo J, Michael LA, Robert L et al (1996) Local intraluminal infusion of biodegradable polymeric nanoparticles. Circulation 94(6):1441–1448
Pardridge WM (1999) Vector-mediated drug delivery to the brain. Blood-Brain Barrier Dyn Interface Drug Deliv Brain 36(2):299–321
Abbott NJ, Romero IA (1996) Transporting therapeutics across the blood-brain barrier. Mol Med Today 2(3):106–113
Egleton RD, Davis TP (1997) Bioavailability and transport of peptides and peptide drugs into the brain. Peptides 18(9):1431–1439
Francis J, Bastia E, Matthews C, Parks D, Schwarzschild M, Brown R et al (2004) Tetanus toxin fragment C as a vector to enhance delivery of proteins to the CNS. Brain Res 1011(1):7–13
Jain SA, Chauk DS, Mahajan HS, Tekade AR, Gattani SG (2009) Formulation and evaluation of nasal mucoadhesive microspheres of Sumatriptan succinate. J Microencapsul 26(8):711–721
Stolnik S, Illum L, Davis SS (1995) Long circulating microparticulate drug carriers. Long-Circ Drug Deliv Syst 16(2):195–214
Juliano RL (1988) Factors affecting the clearance kinetics and tissue distribution of liposomes, microspheres and emulsions. Mononucl Phagocyte Syst 2(1):31–54
Rodrigues JM, Fessi H, Bories C, Puisieux F, Devissaguet J-P (1995) Primaquine-loaded poly(lactide) nanoparticles: physicochemical study and acute tolerance in mice. Int J Pharm 126(1):253–260
Ding L, Samuel J, MacLean GD, Noujaim AA, Diener E, Longenecker BM (1990) Effective drug-antibody targeting using a novel monoclonal antibody against the proliferative compartment of mammalian squamous carcinomas. Cancer Immunol Immunother 32(2):105–109
Duan X, Li Y (2013) Physicochemical characteristics of nanoparticles affect circulation, biodistribution, cellular internalization, and trafficking. Small 9(9–10):1521–1532
Champion JA, Walker A, Mitragotri S (2008) Role of particle size in phagocytosis of polymeric microspheres. Pharm Res 25(8):1815–1821
Gratton SEA, Ropp PA, Pohlhaus PD, Luft JC, Madden VJ, Napier ME et al (2008) The effect of particle design on cellular internalization pathways. Proc Natl Acad Sci 105(33):11613–11618
Longmire M, Choyke PL, Kobayashi H (2008) Clearance properties of nano-sized particles and molecules as imaging agents: considerations and caveats. Nanomedicine 3(5):703–717
Venturoli D, Rippe B (2005) Ficoll and dextran vs. globular proteins as probes for testing glomerular permselectivity: effects of molecular size, shape, charge, and deformability. Am J Physiol-Ren Physiol 288(4):F605–F613
Danhier F, Feron O, Préat V (2010) To exploit the tumor microenvironment: passive and active tumor targeting of nanocarriers for anti-cancer drug delivery. J Control Release 148(2):135–146
Jiang W, Kim BYS, Rutka JT, Chan WCW (2008) Nanoparticle-mediated cellular response is size-dependent. Nat Nanotechnol 3(3):145–150
Pirollo KF, Chang EH (2008) Does a targeting ligand influence nanoparticle tumor localization or uptake? Trends Biotechnol 26(10):552–558
Chen J, Clay N, Kong H (2015) Non-spherical particles for targeted drug delivery. Chem Eng Sci 125:20–24
Truong NP, Whittaker MR, Mak CW, Davis TP (2015) The importance of nanoparticle shape in cancer drug delivery. Expert Opin Drug Deliv 12(1):129–142
Devarajan PV (2014) Targeted drug delivery: concepts and design. Springer, New York
Sharma G, Valenta DT, Altman Y, Harvey S, Xie H, Mitragotri S et al (2010) Polymer particle shape independently influences binding and internalization by macrophages. J Control Release Off J Control Release Soc 147(3):408–412
Yoo J-W, Doshi N, Mitragotri S (2010) Endocytosis and intracellular distribution of PLGA particles in endothelial cells: effect of particle geometry. Macromol Rapid Commun 31(2):142–148
Ahsan F (2002) Targeting to macrophages: role of physicochemical properties of particulate carriers—liposomes and microspheres—on the phagocytosis by macrophages. J Control Release 79(1–3):29–40
Torchilin VP (2005) Recent advances with liposomes as pharmaceutical carriers. Nat Rev Drug Discov 4(2):145–160
Ducat E, Deprez J, Gillet A, Noël A, Evrard B, Peulen O et al (2011) Nuclear delivery of a therapeutic peptide by long circulating pH-sensitive liposomes: benefits over classical vesicles. Int J Pharm 420(2):319–332
Jafarzadeh-Holagh S, Hashemi-Najafabadi S, Shaki H, Vasheghani-Farahani E (2018) Self-assembled and pH-sensitive mixed micelles as an intracellular doxorubicin delivery system. J Colloid Interface Sci 523:179–190
Lukyanov AN, Hartner WC, Torchilin VP (2004) Increased accumulation of PEG-PE micelles in the area of experimental myocardial infarction in rabbits. J Control Release Off J Control Release Soc 94(1):187–193
Wang J, Mongayt D, Torchilin VP (2005) Polymeric micelles for delivery of poorly soluble drugs: preparation and anticancer activity in vitro of paclitaxel incorporated into mixed micelles based on poly(ethylene glycol)-lipid conjugate and positively charged lipids. J Drug Target 13(1):73–80
Roser M, Fischer D, Kissel T (1998) Surface-modified biodegradable albumin nano- and microspheres. II: effect of surface charges on in vitro phagocytosis and biodistribution in rats. Eur J Pharm Biopharm Off J Arbeitsgemeinschaft Pharm Verfahrenstechnik EV 46(3):255–263
Blau S, Jubeh TT, Haupt SM, Rubinstein A (2000) Drug targeting by surface cationization. Crit Rev Ther Drug Carrier Syst 17(5):425–465
Fröhlich E (2012) The role of surface charge in cellular uptake and cytotoxicity of medical nanoparticles. Int J Nanomedicine 7:5577–5591
Xiao K, Li Y, Luo J, Lee JS, Xiao W, Gonik AM et al (2011) The effect of surface charge on in vivo biodistribution of PEG-oligocholic acid based micellar nanoparticles. Biomaterials 32(13):3435–3446
Jain NK, Nahar M (2010) PEGylated nanocarriers for systemic delivery. Methods Mol Biol Clifton NJ 624:221–234
Mishra P, Nayak B, Dey RK (2016) PEGylation in anti-cancer therapy: an overview. Asian J Pharm Sci 11(3):337–348
Pouton C, Wagstaff K, Roth D, Moseley G, Jans D (2007) Targeted delivery to the nucleus. Adv Drug Deliv Rev 59(8):698–717
Barratt G (2011) Delivery to intracellular targets by nanosized particles. In: Intracellular delivery: fundamentals and applications, Fundamental biomedical technologies. Springer, Dordrecht/New York, pp 73–96
Sharma A, Vaghasiya K, Ray E, Verma RK (2018) Lysosomal targeting strategies for design and delivery of bioactive for therapeutic interventions. J Drug Target 26(3):208–221
Agrawal U, Sharma R, Vyas S (2014) Chp 7 targeted drug delivery to the mitochondria. In: Targeted drug delivery: concepts and design. Springer, New York, pp 241–270
Smith RAJ, Murphy MP (2011) Mitochondria-targeted antioxidants as therapies. Discov Med 11(57):106–114
Zhang C, Sriratana A, Minamikawa T, Nagley P (1998) Photosensitisation properties of mitochondrially localised green fluorescent protein. Biochem Biophys Res Commun 242(2):390–395
Pollard H, Remy J-S, Loussouarn G, Demolombe S, Behr J-P, Escande D (1998) Polyethylenimine but not cationic lipids promotes transgene delivery to the nucleus in mammalian cells. J Biol Chem 273(13):7507–7511
International Human Genome Sequencing Consortium, Lander ES, Linton LM, Birren B, Nusbaum C, Zody MC et al (2001) Initial sequencing and analysis of the human genome. Nature 409:860–921
Mouse Genome Sequencing Consortium, Chinwalla AT, Cook LL, Delehaunty KD, Fewell GA, Fulton LA et al (2002) Initial sequencing and comparative analysis of the mouse genome. Nature 420(6915):520–562
Venter JC, Adams MD, Myers EW, Li PW, Mural RJ, Sutton GG et al (2001) The sequence of the human genome. Science 291(5507):1304–1351
Peters MF, Nucifora FC, Kushi J, Seaman HC, Cooper JK, Herring WJ et al (1999) Nuclear targeting of mutant huntingtin increases toxicity. Mol Cell Neurosci 14(2):121–128
Bareford LM, Swaan PW (2007) Endocytic mechanisms for targeted drug delivery. Organelle-Specif Target Drug Deliv Des 59(8):748–758
Yasuhara N, Takeda E, Inoue H, Kotera I, Yoneda Y (2004) Importin α/β-mediated nuclear protein import is regulated in a cell cycle-dependent manner. Exp Cell Res 297(1):285–293
Strunze S, Trotman LC, Boucke K, Greber UF (2005) Nuclear targeting of adenovirus type 2 requires CRM1-mediated nuclear export. Mol Biol Cell 16(6):2999–3009
Tammam SN, Azzazy HM, Breitinger HG, Lamprecht A (2015) Chitosan nanoparticles for nuclear targeting: the effect of nanoparticle size and nuclear localization sequence density. Mol Pharm 12(12):4277–4289
Sun Y, Xian L, Xing H, Yu J, Yang Z, Yang T et al (2016) Factors influencing the nuclear targeting ability of nuclear localization signals. J Drug Target 24(10):927–933
Chan C-K, Jans DA (2002) Using nuclear targeting signals to enhance non-viral gene transfer. Immunol Cell Biol 80(2):119–130
Smyth TN (2002) Cationic liposome-mediated gene delivery in vivo. Biosci Rep 22(2):283–295
Patel LN, Zaro JL, Shen W-C (2007) Cell penetrating peptides: intracellular pathways and pharmaceutical perspectives. Pharm Res 24(11):1977–1992
Li S, Huang L (2000) Nonviral gene therapy: promises and challenges. Gene Ther 7:31–34
Nabel GJ, Nabel EG, Yang ZY, Fox BA, Plautz GE, Gao X et al (1993) Direct gene transfer with DNA-liposome complexes in melanoma: expression, biologic activity, and lack of toxicity in humans. Proc Natl Acad Sci U S A 90(23):11307–11311
Park YJ, Liang JF, Ko KS, Kim SW, Yang VC (2003) Low molecular weight protamine as an efficient and nontoxic gene carrier: in vitro study. J Gene Med 5(8):700–711
Ye S, Tian M, Wang T, Ren L, Wang D, Shen L et al (2012) Synergistic effects of cell-penetrating peptide Tat and fusogenic peptide HA2-enhanced cellular internalization and gene transduction of organosilica nanoparticles. Nanomed Nanotechnol Biol Med 8(6):833–841
Jeon O, Lim H-W, Lee M, Song SJ, Kim B-S (2007) Poly(l-lactide-co-glycolide) nanospheres conjugated with a nuclear localization signal for delivery of plasmid DNA. J Drug Target 15(3):190–198
Huo S, Jin S, Ma X, Xue X, Yang K, Kumar A et al (2014) Ultrasmall gold nanoparticles as carriers for nucleus-based gene therapy due to size-dependent nuclear entry. ACS Nano 8(6):5852–5862
Grandinetti G, Smith AE, Reineke TM (2012) Membrane and nuclear permeabilization by polymeric pDNA vehicles: efficient method for gene delivery or mechanism of cytotoxicity? Mol Pharm 9(3):523–538
Austin LA, Kang B, Yen C-W, El-Sayed MA (2011) Nuclear targeted silver nanospheres perturb the cancer cell cycle differently than those of nanogold. Bioconjug Chem 22(11):2324–2331
Fan W, Shen B, Bu W, Zheng X, He Q, Cui Z et al (2015) Design of an intelligent sub-50 nm nuclear-targeting nanotheranostic system for imaging guided intranuclear radiosensitization. Chem Sci 6(3):1747–1753
Kim J, Dang CV (2006) Cancer’s molecular sweet tooth and the Warburg effect. Cancer Res 66(18):8927–8930
Warburg O (1956) On the origin of cancer cells. Science 123(3191):309–314
Costantini P, Jacotot E, Decaudin D, Kroemer G (2000) Mitochondrion as a novel target of anticancer chemotherapy. JNCI J Natl Cancer Inst 92(13):1042–1053
Duchen MR (2004) Roles of mitochondria in health and disease. Diabetes 53(suppl 1):S96–S102
Murphy MP, Smith RA (2000) Drug delivery to mitochondria: the key to mitochondrial medicine. Recent Adv Cell Subcell Mol Target 41(2):235–250
Ross MF, Kelso GF, Blaikie FH, James AM, Cochemé HM, Filipovska A et al (2005) Lipophilic triphenylphosphonium cations as tools in mitochondrial bioenergetics and free radical biology. Biochem Mosc 70(2):222–230
Muratovska A, Lightowlers RN, Taylor RW, Turnbull DM, Smith RA, Wilce JA et al (2001) Targeting peptide nucleic acid (PNA) oligomers to mitochondria within cells by conjugation to lipophilic cations: implications for mitochondrial DNA replication, expression and disease. Nucleic Acids Res 29(9):1852–1863
Tanaka M, Borgeld H-J, Zhang J, Muramatsu S, Gong J-S, Yoneda M et al (2002) Gene therapy for mitochondrial disease by delivering restriction endonuclease SmaI into mitochondria. J Biomed Sci 9(6):534–541
Weissig V, D’Souza GG, Torchilin V (2001) DQAsome/DNA complexes release DNA upon contact with isolated mouse liver mitochondria. J Control Release 75(3):401–408
Chen Z-P, Li M, Zhang L-J, He J-Y, Wu L, Xiao Y-Y et al (2016) Mitochondria-targeted drug delivery system for cancer treatment. J Drug Target 24(6):492–502
Kang HC (2004) Roles of Mitochondria in Health and Disease. Diabetes 53(suppl 1):S96
D’Souza GGM, Boddapati SV, Weissig V (2005) Mitochondrial leader sequence-plasmid DNA conjugates delivered into mammalian cells by DQAsomes co-localize with mitochondria. Mitochondrion 5(5):352–358
D’Souza GG, Cheng S-M, Boddapati SV, Horobin RW, Weissig V (2008) Nanocarrier-assisted sub-cellular targeting to the site of mitochondria improves the pro-apoptotic activity of paclitaxel. J Drug Target 16(7–8):578–585
Boddapati SV, Tongcharoensirikul P, Hanson RN, D’Souza GGM, Torchilin VP, Weissig V (2005) Mitochondriotropic Liposomes. J Liposome Res 15(1–2):49–58
Yamada Y, Akita H, Kamiya H, Kogure K, Yamamoto T, Shinohara Y et al (2008) MITO-porter: a liposome-based carrier system for delivery of macromolecules into mitochondria via membrane fusion. Biochim Biophys Acta Biomembr 1778(2):423–432
Yasuzaki Y, Yamada Y, Harashima H (2010) Mitochondrial matrix delivery using MITO-Porter, a liposome-based carrier that specifies fusion with mitochondrial membranes. Biochem Biophys Res Commun 397(2):181–186
Callahan J, Kopecek J (2006) Semitelechelic HPMA copolymers functionalized with triphenylphosphonium as drug carriers for membrane transduction and mitochondrial localization. Biomacromolecules 7(8):2347–2356
Zhou L, Liu J-H, Ma F, Wei S-H, Feng Y-Y, Zhou J-H et al (2010) Mitochondria-targeting photosensitizer-encapsulated amorphous nanocage as a bimodal reagent for drug delivery and biodiagnose in vitro. Biomed Microdevices 12(4):655–663
Lübke T, Lobel P, Sleat DE (2009) Proteomics of the lysosome. Lysosomes 1793(4):625–635
Bagshaw RD, Mahuran DJ, Callahan JW (2005) A proteomic analysis of lysosomal integral membrane proteins reveals the diverse composition of the organelle. Mol Amp Cell Proteomics 4(2):133–143
Parkinson-Lawrence EJ, Shandala T, Prodoehl M, Plew R, Borlace GN, Brooks DA (2010) Lysosomal storage disease: revealing lysosomal function and physiology. Physiology 25(2):102–115
Gregoriadis G, Ryman BE (1972) Lysosomal localization of -fructofuranosidase-containing liposomes injected into rats. Biochem J 129(1):123–133
PATEL HM, RYMAN BE (1974) α-Mannosidase in zinc-deficient rats: possibility of liposomal therapy in mannosidosis. Biochem Soc Trans 2(5):1014–1017
Cabrera I, Abasolo I, Corchero JL, Elizondo E, Gil PR, Moreno E et al (2016) α-Galactosidase-a loaded-nanoliposomes with enhanced enzymatic activity and intracellular penetration. Adv Healthc Mater 5(7):829–840
Hamill KM, Wexselblatt E, Tong W, Esko JD, Tor Y (2017) Delivery of cargo to lysosomes using GNeosomes. In: Öllinger K, Appelqvist H (eds) Lysosomes: methods and protocols. Springer New York, New York, pp 151–163
Barrias CC, Lamghari M, Granja PL, Sá Miranda MC, Barbosa MA (2005) Biological evaluation of calcium alginate microspheres as a vehicle for the localized delivery of a therapeutic enzyme. J Biomed Mater Res A 74A(4):545–552
Ghaffarian R, Roki N, Abouzeid A, Vreeland W, Muro S (2016) Intra- and trans-cellular delivery of enzymes by direct conjugation with non-multivalent anti-ICAM molecules. J Control Release 238:221–230
Giannotti MI, Esteban O, Oliva M, García-Parajo MF, Sanz F (2011) pH-Responsive polysaccharide-based polyelectrolyte complexes as nanocarriers for lysosomal delivery of therapeutic proteins. Biomacromolecules 12(7):2524–2533
Giannotti MI, Abasolo I, Oliva M, Andrade F, García-Aranda N, Melgarejo M et al (2016) Highly versatile polyelectrolyte complexes for improving the enzyme replacement therapy of lysosomal storage disorders. ACS Appl Mater Interfaces 8(39):25741–25752
Thekkedath R, Koshkaryev A, Torchilin VP (2013) Lysosome-targeted octadecyl-rhodamine B-liposomes enhance lysosomal accumulation of glucocerebrosidase in Gaucher’s cells in vitro. Nanomedicine 8(7):1055–1065
Gao W, Cao W, Zhang H, Li P, Xu K, Tang B (2014) Targeting lysosomal membrane permeabilization to induce and image apoptosis in cancer cells by multifunctional Au–ZnO hybrid nanoparticles. Chem Commun 50(60):8117–8120
Domenech M, Marrero-Berrios I, Torres-Lugo M, Rinaldi C (2013) Lysosomal membrane permeabilization by targeted magnetic nanoparticles in alternating magnetic fields. ACS Nano 7(6):5091–5101
Xue X, Wang L-R, Sato Y, Jiang Y, Berg M, Yang D-S et al (2014) Single-walled carbon nanotubes alleviate autophagic/lysosomal defects in primary glia from a mouse model of alzheimer’s disease. Nano Lett 14(9):5110–5117
Härtig W, Kacza J, Paulke B-R, Grosche J, Bauer U, Hoffmann A et al (2009) In vivo labelling of hippocampal β-amyloid in triple-transgenic mice with a fluorescent acetylcholinesterase inhibitor released from nanoparticles. Eur J Neurosci 31(1):99–109
Yang Z, Zhang Y, Yang Y, Sun L, Han D, Li H et al (2010) Pharmacological and toxicological target organelles and safe use of single-walled carbon nanotubes as drug carriers in treating Alzheimer disease. Nanomed Nanotechnol Biol Med 6(3):427–441
Singh B, Maharjan S, Park T-E, Jiang T, Kang S-K, Choi Y-J et al (2015) Tuning the buffering capacity of polyethylenimine with glycerol molecules for efficient gene delivery: staying in or out of the endosomes. Macromol Biosci 15(5):622–635
Kelley VA, Schorey JS (2003) Mycobacterium’s arrest of phagosome maturation in macrophages requires Rab5 activity and accessibility to iron. Mol Biol Cell 14(8):3366–3377
Dowdy SF (2017) Overcoming cellular barriers for RNA therapeutics. Nat Biotechnol 35:222–229
Mazzarello P, Bentivoglio M (1998) The centenarian Golgi apparatus. Nature 392:543–544
Aridor M, Hannan LA (2008) Traffic jam: a compendium of human diseases that affect intracellular transport processes. Traffic 1(11):836–851
Wlodkowic D, Skommer J, McGuinness D, Hillier C, Darzynkiewicz Z (2009) ER–Golgi network—a future target for anti-cancer therapy. Leuk Res 33(11):1440–1447
Boelens J, Lust S, Offner F, Bracke ME, Vanhoecke BW (2007) The endoplasmic reticulum: a target for new anticancer drugs. In Vivo 21(2):215–226
Paschen W, Frandsen A (2008) Endoplasmic reticulum dysfunction – a common denominator for cell injury in acute and degenerative diseases of the brain? J Neurochem 79(4):719–725
Pópulo H, Lopes JM, Soares P (2012) The mTOR signalling pathway in human cancer. Int J Mol Sci 13(2):1886–1918
Drenan RM, Liu X, Bertram PG, Zheng XFS (2004) FKBP12-Rapamycin-associated protein or mammalian target of Rapamycin (FRAP/mTOR) localization in the endoplasmic reticulum and the golgi apparatus. J Biol Chem 279(1):772–778
Chernenko T, Matthäus C, Milane L, Quintero L, Amiji M, Diem M (2009) Label-free raman spectral imaging of intracellular delivery and degradation of polymeric nanoparticle systems. ACS Nano 3(11):3552–3559
Cartiera MS, Johnson KM, Rajendran V, Caplan MJ, Saltzman WM (2009) The uptake and intracellular fate of PLGA nanoparticles in epithelial cells. Biomaterials 30(14):2790–2798
Price P, Griffiths J (1994) Tumour pharmacokinetics?—we do need to know. Lancet 343(8907):1174–1175
Siepmann J, Siepmann F, Florence AT (2006) Local controlled drug delivery to the brain: mathematical modeling of the underlying mass transport mechanisms. Local Control Drug Deliv Brain 314(2):101–119
Florence AT (1997) The oral absorption of micro- and nanoparticulates: neither exceptional nor unusual. Pharm Res 14(3):259–266
Willmott N, Cummings J, Stuart JFB, Florence AT (1985) Adriamycin-loaded albumin microspheres: preparation, in vivo distribution and release in the rat. Biopharm Drug Dispos 6(1):91–104
Decuzzi P, Ferrari M (2007) The role of specific and non-specific interactions in receptor-mediated endocytosis of nanoparticles. Biomaterials 28(18):2915–2922
Decuzzi P, Ferrari M (2008) Design maps for nanoparticles targeting the diseased microvasculature. Biomaterials 29(3):377–384
Cristini V, Sinek J, Frieboes H (2005) Two-dimensional chemotherapy simulations demonstrate fundamental transport and tumor response limitations involving nanoparticles. Cancer Res 65(9 Supplement):1196
Farris RJ (1968) Prediction of the viscosity of multimodal suspensions from unimodal viscosity data. Trans Soc Rheol 12(2):281–301
Lionberger RA (2002) Viscosity of bimodal and polydisperse colloidal suspensions. Phys Rev E 65(6):061408–061418
Semwogerere D, Morris JF, Weeks ER (2007) Development of particle migration in pressure-driven flow of a brownian suspension. J Fluid Mech 581:437–451
Frank M, Anderson D, Weeks ER, Morris JF (2003) Particle migration in pressure-driven flow of a brownian suspension. J Fluid Mech 493:363–378
Sakamoto J, Annapragada A, Decuzzi P, Ferrari M (2007) Antibiological barrier nanovector technology for cancer applications. Expert Opin Drug Deliv 4(4):359–369
Verberg R, Alexeev A, Balazs AC (2006) Modeling the release of nanoparticles from mobile microcapsules. J Chem Phys 125(22):224712
De Jong WH, Borm PJA (2008) Drug delivery and nanoparticles: applications and hazards. Int J Nanomedicine 3(2):133–149
Oberdörster G (2009) Safety assessment for nanotechnology and nanomedicine: concepts of nanotoxicology. J Intern Med 267(1):89–105
Sharma A, Madhunapantula SV, Robertson GP (2012) Toxicological considerations when creating nanoparticle-based drugs and drug delivery systems. Expert Opin Drug Metab Toxicol 8(1):47–69
Murdock RC, Braydich-Stolle L, Schrand AM, Schlager JJ, Hussain SM (2008) Characterization of nanomaterial dispersion in solution prior to in vitro exposure using dynamic light scattering technique. Toxicol Sci 101(2):239–253
Farhood H, Gao X, Son K, Lazo JS, Huang L, Barsoum J et al (1994) Cationic liposomes for direct gene transfer in therapy of cancer and other diseases. Ann N Y Acad Sci 716(1):23–35
Felgner PL, Gadek TR, Holm M, Roman R, Chan HW, Wenz M et al (1987) Lipofection: a highly efficient, lipid-mediated DNA-transfection procedure. Proc Natl Acad Sci U S A 84(21):7413–7417
Borm P, Klaessig FC, Landry TD, Moudgil B, Pauluhn J, Thomas K et al (2006) Research strategies for safety evaluation of nanomaterials, part v: role of dissolution in biological fate and effects of nanoscale particles. Toxicol Sci 90(1):23–32
Hall JB, Dobrovolskaia MA, Patri AK, McNeil SE (2007) Characterization of nanoparticles for therapeutics. Nanomedicine 2(6):789–803
Medina C, Santos-Martinez MJ, Radomski A, Corrigan OI, Radomski MW (2007) Nanoparticles: pharmacological and toxicological significance. Br J Pharmacol 150(5):552–558
Dhawan A, Sharma V (2010) Toxicity assessment of nanomaterials: methods and challenges. Anal Bioanal Chem 398(2):589–605
Oberdörster G, Maynard A, Donaldson K, Castranova V, Fitzpatrick J, Ausman K et al (2005) Principles for characterizing the potential human health effects from exposure to nanomaterials: elements of a screening strategy. Part Fibre Toxicol 2(1):8–42
Stone V, Johnston H, Schins RPF (2009) Development of in vitro systems for nanotoxicology: methodological considerations. Crit Rev Toxicol 39(7):613–626
Acknowledgments
We would like to acknowledge UGC for providing D.S. Kothari Postdoctoral Fellowship to Sreeranjini Pulakkat.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Dhoble, S., Dhage, S., Pulakkat, S., Patravale, V.B. (2019). Opportunities and Challenges in Targeted Carrier-Based Intracellular Drug Delivery: Increased Efficacy and Reduced Toxicity. In: Misra, A., Shahiwala, A. (eds) Novel Drug Delivery Technologies. Springer, Singapore. https://doi.org/10.1007/978-981-13-3642-3_12
Download citation
DOI: https://doi.org/10.1007/978-981-13-3642-3_12
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-3641-6
Online ISBN: 978-981-13-3642-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)