Abstract
Asthma is a heterogeneous disease, usually characterized by chronic inflammation of the airways. Fractional nitric oxide (NO) concentration in exhaled air (FeNO) is recognized as a noninvasive biomarker of eosinophilic inflammation in the lower respiratory tract. Presence of airway inflammation in addition to respiratory symptoms that are suggestive of asthma supports a diagnosis of asthma. This chapter provides recent topics pertaining to asthma including the mechanism of production of NO in the airway, methods of and interpretations in measuring FeNO, and the role of exhaled NO measurement in making diagnosis of asthma and differentiating asthma from chronic obstructive pulmonary disease (COPD).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Although asthma is a disease showing various symptoms and pathologies, chronic airway inflammation is a consistent feature of the disease and the primary target of its treatment. Airway inflammation has traditionally been assessed using sputum and/or biopsy tissue samples, but such assessments are disadvantageous due to patient invasiveness and poor rapidity of test results. Exhaled nitric oxide (NO) that allows noninvasive and real-time measurement reflects eosinophilic inflammation in the lower respiratory tract and therefore, useful for making a diagnosis of asthma and predicting steroid responsiveness [1,2,3]. Moreover, since changes in FeNO levels during anti-inflammatory treatment correlate with improvement in symptoms, airflow limitation, and airway hyperresponsiveness [4,5,6], exhaled NO is expected to play an important role in monitoring of asthma and guide for its treatment. FeNO measurement as a biomarker to assess the airway inflammation has been covered by health insurance in Japan since 2013.
2 Measurement of Exhaled Nitric Oxide: Basic Aspects
In the human body, NO is produced by NO synthase (NOS) when l-arginine is converted to l-citrulline (Fig. 9.1). Three isoforms of NO have been identified to date, and their activation mechanism, expression patterns, and intracellular localization have been characterized (Table 9.1). Neuronal NOS (nNOS) expressed in neurons and skeletal muscle cells as well as endothelial NOS (eNOS) expressed in vascular endothelial cells are constitutively expressed enzymes, which require increased Ca2+ level in the cytoplasm induced by stimulation with agonists (e.g., acetylcholine) for activation and are characterized by Ca2+-dependent action for a short time. On the other hand, inducible NOS (iNOS) whose mRNA is synthesized by stimulation with inflammatory cytokines and endotoxins does not depend on Ca2+ levels after its production and produces larger quantities of NO for longer time than constitutively expressed NOS [1, 2].
Th2 cells, ILC2 cells, and mast cells that produce inflammatory type 2 cytokines such as interleukin (IL)-4, IL-5, and IL-13 are activated in patients with asthma. IL-4 and IL-13 induce synthesis of iNOS in airway epithelial cells via transcription of STAT-6, resulting in production of a large quantities of NO [7]. Thus, higher level of NO is detected in the exhaled air from patients with asthma than that from healthy individuals [8]. In patients with asthma, FeNO correlates with the severity of eosinophilic airway inflammation determined using sputum or biopsy tissue samples. Therefore, exhaled NO measurement is regarded as “a noninvasive test to detect eosinophilic inflammation in the lower respiratory tract” [1,2,3]. Chronic obstructive pulmonary disease (COPD), an inflammatory airway disease like as asthma, however, is not associated with increased FeNO levels since NO is consumed by reactive oxygen species (ROS) locally in the airway of patients with COPD [8].
Measurement of exhaled NO requires standardization of measurement conditions since FeNO is affected by various factors including expiratory flow rate and mouth pressure. Recommendations for standardized procedures for measurement of exhaled NO were issued in 2005 by the American Thoracic Society (ATS) and European Respiratory Society (ERS) [1]. The main recommendations are as follows: (1) Since exhaled NO levels exhibit a significant dependence on expiratory flow rate, a constant expiratory flow rate of 50 mL/s should be achieved and maintained during measurement. (2) Exhalation should be started at the point of total lung capacity. (3) The mouth pressure should be 5–15 cm H2O to ensure closure of the velopharyngeal aperture and exclude contamination of the nasal NO (containing upper respiratory tract NO). (4) The exhaled NO profile versus time shows an early peak due to contamination with NO from the nasal cavity and dead space, followed by a certain NO plateau phase. This value is stable if an appropriate mouth pressure at expiration and a constant expiratory flow rate are ensured. This plateau value should be regarded as an exhaled NO from the lower respiratory tract (FeNO) (Fig. 9.2).
Exhaled nitric oxide concentration and mouth pressure versus time for the single exhalation. This figure shows an early peak due to contamination with NO from the nasal cavity and dead space, followed by a certain NO plateau phase (red line). This plateau value should be regarded as an exhaled NO from the lower respiratory tract
As of January 2018, three maintenance-free online devices for exhaled NO measurement have been approved for use under health insurance medical services in Japan: NIOX MINO® and NIOX VERO® from CHEST MI, Inc. and NObreath® from HARADA corporation.
3 Role of FeNO Measurement in the Diagnosis of Asthma
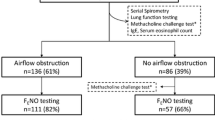
Diagnosis of asthma is based not only characteristic symptoms including paroxysmal wheezing that is likely to occur at night and in the early morning, dyspnea, and recurrent cough but also such physiological signs as reversible airflow limitation and increased airway hyperresponsiveness. An atopic predisposition and presence of airway inflammation (i.e., sputum eosinophilia and increased FeNO) usually support the diagnosis of asthma3.
Clinical application of FeNO measurement requires establishment of specific normal ranges or cutoff values. A study to establish a normal range in Japanese revealed the mean FeNO level in healthy adults of 15 ppb and the statistically estimated upper limit of normal of 37 ppb [9]. In adults, such factors as gender, height, and body mass index (BMI) had no statistically significant effects on FeNO levels [9]. In another study, FeNO levels were compared between healthy adults with normal lung function and without respiratory symptoms and steroid-naive asthmatic patients with respiratory symptoms suggesting asthma who showed significant bronchodilator reversibility and/or increased airway hyperresponsiveness to determine a FeNO cutoff value for diagnosis of asthma [10]. FeNO levels were significantly higher in patients with asthma than in healthy volunteers, and a cutoff value to distinguish these two populations was calculated to be 22 ppb with a sensitivity of 91% and a specificity of 84% [10]. The area under the curve (AUC) from a receiver operating characteristic (ROC) analysis was 0.90, indicating that an FeNO level of ≥22 ppb in addition to presence of respiratory symptoms is associated with a high likelihood of asthma [10]. On the other hand, the sensitivity and specificity for diagnosis of asthma of a cutoff value of 37 ppb, the upper limit of normal [9], were 52% and 99%, respectively. Therefore, the use of this value should be associated with a low false-positive rate and is good for catching actual cases of asthma (high specificity). It should be noted, however, that the use of this cutoff value is associated with a high risk of missing cases of asthma (low sensitivity) (Fig. 9.3).
Reference values of FeNO to support the diagnosis of asthma. Scatter plot of the FeNO levels in control subjects (n = 224) and asthmatic patients (n = 142). The horizontal red bars indicated the mean value for each group. The dotted lines indicated the cutoff value for asthma diagnosis (22 ppb) and the normal upper limit of Japanese healthy subjects (37 ppb), respectively
Additionally, multivariate analysis in the above two populations identified current smoking and allergic rhinitis as individual factors significantly affecting FeNO levels. Irrespective of asthma, individuals with rhinitis had significantly higher EeNO levels, and current smokers had significantly lower FeNO levels [10]. When the study subjects were divided into four subgroups according to current smoking status and concurrent rhinitis, subgroup analyses revealed cutoff values for diagnosis of asthma of 22 ppb in non-smokers without rhinitis, 28 ppb in non-smokers with rhinitis, 18 ppb in current smokers without rhinitis, and 22 ppb in current smokers with rhinitis. Although the cutoff value of FeNO varied depending on host factors, their sensitivity and specificity were high in all of the four subgroups, and the AUC was not lower than 0.85 in any subgroup, indicating that FeNO provides an adequately reliable complementary tool to support the diagnosis of asthma [10].
4 Exhaled NO Concentrations in Asthma and COPD
COPD, a disease characterized by persistent airflow limitation caused by pulmonary or respiratory tract injury mainly due to inhaled harmful particles such as tobacco, is of importance both in differentiation of asthma and as a complication of asthma [11]. Although both asthma and COPD are inflammatory airway disease, different types of inflammation are involved in them; asthma is characterized by eosinophilic and/or CD4+ lymphocyte-mediated inflammation, while neutrophils and/or CT8+ lymphocytes mainly contribute to inflammation in COPD [11, 12]. Assessment of airway inflammation is helpful for differentiation of asthma and COPD in patients for whom differential diagnosis is difficult only based on symptoms and physiological examination. In a study comparing age- and airflow limitation-matched patients with asthma and those with COPD, the FeNO level in patients with asthma was significantly higher than that in patients with COPD, and the sensitivity and specificity of the reported cutoff FeNO value for differential diagnosis (35 ppb) were 91% and 77%, respectively [12].
Some patients with asthma mainly complain of exertional dyspnea and show persistent airflow limitation that will not be normalized even after the inhalation of bronchodilator. On the other hand, some patients with COPD show bronchodilator reversibility even though their FEV1 (forced expiratory volume in one second)/FVC (forced vital capacity) cannot be normalized with bronchodilators. Such patients that have both several features usually associated with asthma and several features usually associated with COPD and show persistent airflow limitation are currently called patients with asthma-COPD overlap (ACO) [11]. In Japanese guidelines [3], it is recommended that concurrent asthma should be considered and reflected in the treatment strategy for patients with COPD in whom at least one of the following is observed after excluding alternative diagnoses such as heart failure and lung cancer: paroxysmal dyspnea or wheezing, reversible airflow limitation, increased airway hyperresponsiveness, atopic predisposition, and any sign of airway inflammation such as sputum eosinophilia and increased FeNO level. Some patients with a clinical diagnosis of COPD show the type 2 molecular signatures (e.g., IL-4, IL-5, and IL-13) assessed by several biomarkers, such as immunoglobulin E, eosinophils in the blood or sputum, serum periostin, and FeNO [13,14,15]. Interestingly, presence of type 2 inflammation in COPD is strongly associated with responsiveness to steroid therapy [16, 17]. The mean FeNO level in patients with COPD was approximately 20 ppb, with a considerable highly variation [15]. It has been reported that approximately 16% of patients with COPD demonstrated high FeNO levels of at least 35 ppb which strongly suggested concurrent asthma from the viewpoint of inflammatory profile of the airway [15].
5 Conclusion
Measurement of exhaled NO may be affected not only by measurement conditions such as expiratory flow rate and mouth pressure but also by various host factors. Many recent studies, however, have shown that increased level of FeNO measured by standardized method is an important type 2 signature that supports the diagnosis of asthma. Assessment of airway inflammation using exhaled NO in addition to traditional assessments of symptoms and lung function is expected to allow further improvement of efficiency in management of chronic inflammatory airway diseases including asthma and COPD.
Abbreviations
- ACO:
-
Asthma-COPD overlap
- COPD:
-
Chronic obstructive pulmonary disease
- eNOS:
-
Endothelial nitric oxide synthase
- FeNO:
-
Fractional nitric oxide concentration in exhaled air
- FEV1:
-
Forced expiratory volume in one second
- FVC:
-
Forced vital capacity
- iNOS:
-
Inducible nitric oxide synthase
- NO:
-
Nitric oxide
- nNOS:
-
Neuronal nitric oxide synthase
- ROS:
-
Reactive oxygen species
References
American Thoracic Society; European Respiratory Society. ATS/ERS recommendations for standardized procedures for the online and offline measurement of exhaled lower respiratory nitric oxide and nasal nitric oxide. Am J Respir Crit Care Med. 2005;171:912–30.
Dweik RA, Boggs PB, Erzurum SC, Irvin CG, Leigh MW, Lundberg JO, Olin AC, Plummer AL, Taylor DR, American Thoracic Society Committee on Interpretation of Exhaled Nitric Oxide Levels (FENO) for Clinical Applications. An official ATS clinical practice guideline: interpretation of exhaled nitric oxide levels (FeNO) for clinical applications. Am J Respir Crit Care Med. 2011;184:602–15.
Ichinose M, Sugiura H, Nagase H, Yamaguchi M, Inoue H, Sagara H, Tamaoki J, Tohda Y, Munakata M, Yamauchi K, Ohta K, Japanese Society of Allergy. Japanese guidelines for adult asthma. Allergol Int. 2017;66:163–89.
Ichinose M, Takahashi T, Sugiura H, Endoh N, Miura M, Mashito Y, Shirato K. Baseline airway hyperresponsiveness and its reversible component: role of airway inflammation and airway caliber. Eur Respir J. 2000;15:248–53.
Matsunaga K, Kawabata H, Hirano T, Sugiura H, Minakata Y, Ichnose M. Difference in time-course of improvement in asthma control measures between budesonide and budesonide/formoterol. Pulm Pharmacol Ther. 2013;26:189–94.
Matsunaga K, Hirano T, Akamatsu K, Minakata Y. Predictors for identifying the efficacy of systemic steroids on sustained exhaled nitric oxide elevation in severe asthma. Allergol Int. 2013;62:359–65.
Alving K, Malinovschi A. Basic aspects of exhaled nitric oxide. Eur Respir Mon. 2010;49:1–31.
Ichinose M, Sugiura H, Yamagata S, Koarai A, Shirato K. Increase in reactive nitrogen species production in chronic obstructive pulmonary disease airways. Am J Respir Crit Care Med. 2000;162:701–6.
Matsunaga K, Hirano T, Kawayama T, Tsuburai T, Nagase H, Aizawa H, Akiyama K, Ohta K, Ichinose M. Reference ranges for exhaled nitric oxide fraction in healthy Japanese adult population. Allergol Int. 2010;59:363–7.
Matsunaga K, Hirano T, Akamatsu K, Koarai A, Sugiura H, Minakata Y, Ichinose M. Exhaled nitric oxide cutoff values for asthma diagnosis according to rhinitis and smoking status in Japanese subjects. Allergol Int. 2011;60:331–7.
Global Initiative for Chronic Obstructive Lung Disease: Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease, NHLBI/WHO workshop report 2017.
Fabbri LM, Romagnoli M, Corbetta L, Casoni G, Busljetic K, Turato G, Ligabue G, Ciaccia A, Saetta M, Papi A. Differences in airway inflammation in patients with fixed airflow obstruction due to asthma or chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2003;167:418–24.
McDonald VM, Higgins I, Wood LG, Gibson PG. Multidimensional assessment and tailored interventions for COPD: respiratory utopia or common sense? Thorax. 2013;68:691–4.
Konstantelou E, Papaioannou AI, Loukides S, Bartziokas K, Papaporfyriou A, Papatheodorou G, Bakakos P, Papiris S, Koulouris N, Kostikas K. Serum periostin in patients hospitalized for COPD exacerbations. Cytokine. 2017;93:51–6.
Tamada T, Sugiura H, Takahashi T, Matsunaga K, Kimura K, Katsumata U, Takekoshi D, Kikuchi T, Ohta K, Ichinose M. Biomarker-based detection of asthma-COPD overlap syndrome in COPD populations. Int J Chron Obstruct Pulmon Dis. 2015;10:2169–76.
Akamatsu K, Matsunaga K, Sugiura H, Koarai A, Hirano T, Minakata Y, Ichinose M. Improvement of airflow limitation by fluticasone propionate/salmeterol in chronic obstructive pulmonary disease: what is the specific marker? Front Pharmacol. 2011;2:36. https://doi.org/10.3389/fphar.2011.00036.
Christenson SA, Steiling K, van den Berge M, Hijazi K, Hiemstra PS, Postma DS, Lenburg ME, Spira A, Woodruff PG. Asthma-COPD overlap. Clinical relevance of genomic signatures of type 2 inflammation in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2015;191:758–66.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Matsunaga, K. (2019). Diagnostic Value of Fractional Exhaled Nitric Oxide (FeNO). In: Yokoyama, A. (eds) Advances in Asthma. Respiratory Disease Series: Diagnostic Tools and Disease Managements. Springer, Singapore. https://doi.org/10.1007/978-981-13-2790-2_9
Download citation
DOI: https://doi.org/10.1007/978-981-13-2790-2_9
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-2789-6
Online ISBN: 978-981-13-2790-2
eBook Packages: MedicineMedicine (R0)