Abstract
As the climate changes, global temperatures will increase in the future, and extreme weather will occur more frequently. Epidemiological studies have shown the significant relationship between the ambient temperature and an elevated risk of mortality. With temperature increases in the future, the population mortality risk may increase. Therefore, estimating the risk of future temperature-related mortality is significant for the protection of public health and the reduction of the burden of disease. Most studies assuming relationship between temperature and mortality remain constant; the projected future temperature and future population are substituted for future temperature-related mortality. This chapter will summarize the methods used to estimate the temperature-related mortality risk globally and the progress, results, and limitations of studies in China. By reviewing these studies, we provide a direction for future studies in China that project future temperature-related mortality risk.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
8.1 Introduction
Climate change is one of the major issues of humanity. According to the fifth report of the Intergovernmental Panel on Climate Change (IPCC), the global temperature has risen 0.85 °C over the last 100 years. The report also assumed that the average global temperature would increase by 1.0 °C, 1.8 °C, 2.2 °C, and 3.7 °C in 2081–2100 under different scenarios. Many epidemiological studies have shown a significant relationship between the ambient temperature and an elevated risk of mortality and morbidity, and the effect is greater than previously documented in some sensitive populations, such as the population with cardiovascular disease and the elderly [1,2,3,4,5]. Furthermore, a meta-analysis showed that with a change in temperature condition, the risk of cardiovascular hospitalization would increase 2.8% (95% CI, 2.1–3.5%) for cold exposure, 2.2% (95% CI, 0.6–3.9%) for heat wave exposure, and 0.7% (95% CI, 0.2–1.2%) for an increase in diurnal temperature [6]. As the future temperature rises, the population health risk may increase. Therefore, the study of future projections is of great significance for the protection of public health and requires more attention.
Several studies from the 1990s have projected future temperature-related mortality risks, and the number of these studies increased obviously after 2007 for several possible reasons. One reason is that the data of both global and regional climate model simulations at the periods may be easier to obtain. Increased workstation computational power, improved epidemiological methods, and the convenience and increased speed of the Internet all might be other possible factors [7]. The majority of the locations in which studies were conducted were developed countries, including the USA, Canada, European countries, Australia, and South Korea. For example, Gasparrini et al. projected the temperature-related death risk in 451 locations of 23 countries across the world and found that the negative mortality risk of climate change under RCP 8.5 would disproportionately affect poorer and warmer regions, with the net change at the end of the century ranging from −1.2% (95% CI, −3.6–1.4%) in Australia to 12.7% (95% CI, −4.7–28.1%) in Southeast Asia and 1.5% (95% CI, −2.0–5.4%) in China [8]. These studies found that global warming is likely to cause increased heat-related, heat wave-related, and cold spell-related mortality and decreased cold-related mortality [9]. The current method of estimating future temperature-related mortality risk varies. Generally, there are three basic procedures. First, project the future daily temperature under the future scenario model proposed in the IPCC report; second, calculate the exposure-response relationship between temperature and health outcomes based on historical data; and third, combine the projected temperature and exposure-response relationship to obtain the future mortality risk under climate change.
In summary, the regions currently under study were not balanced, and the methods and results of each study were quite different. This chapter will introduce the methods of approach to the study of projecting future temperature-related mortality and will focus on the methods, results, and future research directions in China.
8.2 Method
Recent studies have been conducted to estimate future temperature-related mortality risks, including estimating the future risk of heat-related mortality cold-related mortality, heat wave-related mortality, and cold spell-related mortality [7, 10]. In this process, studies estimating future risk of temperature-related mortality are based primarily on historical data. Most studies assuming this relationship remain constant; the projected future temperature and future population are substituted for future temperature-related deaths. In the calculation of future temperature-related deaths, some studies consider future changes in the population and the population’s adaptability to temperature, which would change the exposure-response relationship. The existing research methods will be summarized from five aspects: baseline exposure response, future regional temperature projection, future population changes, future population acclimatization, and uncertainties.
8.2.1 Baseline Temperature-Mortality Relationships
Thus far, many studies have explored and quantified the effect of temperature on mortality by time-series studies or case-crossover designs [11]. Studies have found that the adverse effect of temperature on mortality is a curve relationship, which significantly increases if the temperature exceeds or falls below the minimum mortality temperature (MMT). Therefore, the model of the exposure-response relationship between temperature and mortality is mainly the distributed lag nonlinear model (DLNM), which puts the lag and temperature into the generalized linear model (GLM) as a cross-basis and explores the effect of each lag day and each temperature on mortality [12, 13]. The general cold effect has a long lag time of up to 30 days, and the heat effect has a short lag time of approximately 0–7 days. In addition, the confounding factors of the exposure-response relationships include humidity, day of the week, holidays, or air pollution [14].
The relationship between temperature and mortality also largely concerned the baseline time periods and the measure of temperature. When summarizing the time span of the exposure-response relationship included in the relevant literature of this search, it was found that the time span of most of the studies is greater than 10 years to ensure that the exposure-response relationship at the baseline time period is stable enough and can be applied to the projection of future temperature-related death risk. The measure of temperature includes daily maximum temperature and daily average temperature. Most of the studies use daily average temperature, which represents the overall exposure level [15, 16]. However, it is more common to calculate the maximum temperature in the heat wave-related studies. For example, Heaviside et al. projected the future heat wave-related mortality risk in Cyprus in Europe, and the temperature index used in calculating the exposure-response relationship is the daily maximum temperature [17].
8.2.2 Future Temperature Projection
The projection of future temperature is mainly based on the use of different atmospheric cycle models under different climate change scenarios in the future and the use of downscaling to obtain the required regional future temperatures. The future climate change scenario caused by human activities has always been an important part of the work of the IPCC.
Before 2013, the world’s most widely used scenario was a set of emission scenarios (SRES) announced by the IPCC in 2007, but the SRES did not consider the impact of climate change policies on future emissions. The IPCC published a set of representative concentration path (RCP) scenarios in 2013 (Table 8.1). The purpose of these scenarios is to provide possibilities for future scenarios depending on demographic, technological, political, social, and economic developments rather than assigned probabilities [18]. Half of the current studies that projected future temperature-related mortality risks used SRES emissions before 2013, which were generally combined with A1FI (“higher emissions”), A2 (“mid-high emissions”), and B1 (“lower emissions”) [19]. Individual studies only used one of the high-emission models of A2, A1B, and A1F1 [20, 21]. A large number of studies used RCP scenarios after 2013, which were generally combined with medium- and high-emission scenario models, such as RCP 4.5 and RCP 8.5 [22]. Some studies used all four RCPs when projecting temperature, and an increasing number of studies used RCP 2.6 to explore the effect caused by policies [23, 24]. Individual studies only used RCP 8.5 when projecting temperature [16].
The global climate model, also generally known as the general circulation model (GCM), is currently the main tool for temperature projection in climatic studies. The GCM can be traced back to the basic equations used by Smagorinsky in his study in 1963 to address atmospheric circulation. After more than 50 years of development, the GCM has not only been the first simple model of “atmospheric circulation” but has also joined the coupling modes of the Earth’s hydrosphere, the cryosphere, the biosphere, and the human circle. By simulating the global and large-scale climate change process, the temperature data of the time series in the future time period are obtained. Future climate projections come from GCMs, which reflect the current understanding of the physical, dynamical, and chemical processes that control the climate system.
GCM is unique in that they contain different but reasonable methods of representing climate processes, numerical methods for solving equations, and representations of processes that occur on the spatial scale and cannot be resolved directly by climate models [25]. There is no standard for how to choose a GCM. In the current study on the projection of future temperature-related mortality risk, the number of GCMs used varies from 1 to 62. In recent years, most studies used ten or more GCMs to project future temperatures, and individual studies used only one GCM to simulate future temperatures [12, 26, 27]. Using more GCMs can reduce the uncertainty caused by the choice of GCM [7].
Due to the limitation of the calculation conditions, the resolution adopted by the GCM is generally low (currently between 125 and 400 km). If the climate change scenario is to be estimated at regional and local scales on a smaller scale, statistical or dynamic downscaling is required. The statistical downscaling method obtains downscaling results by establishing a link between large-scale model results and observational data, such as circulation and ground variables. Although the statistical downscaling method lacks the physical mechanism and is affected by the observational data of the training model, it is easy to calculate and can integrate multiple GCMs, and it has been used more in recent years [7]. Of the studies retrieved for this review that project future temperature-related mortality risks, many used statistical downscaling to obtain future temperatures in the study area [10]. Dynamic downscaling is simulated using global high-resolution climate models at global or regional scales. The dynamic downscaling method has the advantages of clear physical meaning, unaffected by observational data, and all points facing the coverage area. However, it has a large number of calculations, is inconvenient to simulate, and cannot integrate multiple GCMs. Few studies used dynamic downscaling methods to obtain future regional temperatures [28, 29].
8.2.3 Future Demographic Changes
Several studies have shown that the risk of temperature on people will be different in different age groups and older people are more susceptible to the effects of temperature [1, 5]. The world’s population will increase to 5.5–14.0 billion by 2100, and the structure of the population in different age groups will also change [30, 31]. Changes in the composition of the future population will affect the projection of temperature-related death risks. In the event of future temperature-related mortality risks, if the aging of the population is not considered, the risk of future temperature-to-population deaths will be underestimated. For example, when Hajat et al. projected the future heat-related mortality risk in the UK, it was found that considering an aging population would increase the mortality risk by 206% [32].
Few of the previous studies projecting future temperature-related mortality risk have considered the impact of future demographic changes. The methods of studies obtaining future local population estimates varied. Many studies projected the risk of future temperature-related deaths using the local Bureau of Statistics projected population [17, 33]. Few studies projected the future temperature-related mortality risk utilizing the population projected by the United Nations for high, medium, and low fertility rates [34]. In addition, some studies projected the future temperature-related mortality risk and used the future population projected by the five population scenarios’ shared socioeconomic pathways (SSPs) 1–5 provided by the IPCC5 [15]. Individual studies projected the future temperature-related mortality risk with future populations by a statistical model [29]. These methods of projecting future populations can be applied to the study of projecting temperature-related mortality risks, and the current study prefers to use the predicted population under the SSP scenario with the refinement of the IPCC report.
8.2.4 Future Population Acclimatization
The use of air conditioning in the future and the intervention of early warning systems will affect the population’s adaptability to temperature, and different regions may differ in air-conditioning usage due to different socioeconomic conditions [35]. Whether or not the population’s adaptability to temperature is taken into account in projecting the temperature-related mortality risk has an impact on the relationship between future temperature and mortality.
A small number of studies have considered the population’s adaptability to temperature. The population will have increased adaptability to heat and heat waves due to physiological mechanisms. Jenkins et al. measured the risk of future heat-related deaths in London, UK, and found that considering the population’s adaptability to heat, the risk of temperature-related mortality can be reduced by 69% [35].
Some studies hypothesized that the future relationship between heat and mortality will change as people’s ability to adapt to temperature changes or that the MMT will change as people’s ability to adapt to temperature changes [36, 37]. Some studies have assumed that the relationship between the future temperature and the mortality of the population of the study location was consistent with the exposure-response relationship at a previous stage in other similar cities [38]. Gosling et al. summarized six different adaptive model methods for estimating future heat-related death risk (absolute threshold temperature changes; relative threshold temperature changes; exposure-reaction relationship slope changes; absolute threshold temperature changes combined with changes in exposure-response relationships; and relative threshold temperature changes combined with changes in exposure-response relationships, using exposure-response relationships in similar cities) and found that different adaptive methods have a greater impact on projected results [26]. Gosling et al. suggested that we could combine the change of threshold temperature and the slope of the exposure response in the projection of future temperature-related mortality risk [26].
The adaptability to cold and cold waves was unclear [39]. A few studies assumed that climate change will reduce cold adaptation and that the cold-related mortality risk will increase with considerable acclimatization [40]. However, studies have shown that seasonality may affect the results of such adaptation [39].
8.2.5 Uncertainties
Uncertainty in estimating temperature-related mortality risk is mainly due to temperature projection (selection of GCM, selection of emission models), temperature-mortality relationship, changes in the number and composition of future populations, changes in adaption to heat and cold, socioeconomic changes in the future, and improvement of medical conditions [41]. Uncertainty in projecting temperature-related mortality risk is unavoidable, but researchers should minimize uncertainty and make projections more scientific. At present, the methods to reduce the uncertainty of the estimated temperature-related death risk mainly include selecting more GCMs and as many greenhouse gas scenarios as possible when projecting future temperature, choosing a better adaptive approach, and considering future demographic scenarios.
There have been studies that have begun to quantitatively estimate the uncertainty associated with temperature-related risks. Some studies estimated temperature-related mortality risk using ANOVA-type (Analysis of Variance) estimation of variance components to calculate uncertainty due to RCPs, GCM, and different demographic scenarios [34]. Individual methods used Monte Carlo simulations in the calculation of confidence intervals to represent the uncertainty by temperature-mortality relationship [8]. Gosling et al. quantified the uncertainties associated with six adaptive models, five GCMs, and two RCPs when estimating temperature-related mortality risk and found that the uncertainty caused by adaptability is greater than the uncertainty caused by GCM and RCP [26].
8.3 Review of Studies in China
Previous studies have shown that the risk of heat-related mortality increased with the future warming of the climate, and the results of developing countries were more pronounced. China recently conducted some studies to project the risk of temperature-related mortality (Table 8.2).
8.3.1 Research Progress
Of the studies in China, four project the future risk of heat-related mortality [15, 34, 37, 42]. The three studies simultaneously project the risk of future heat- and cold-related mortality [40, 43, 44]. There were seven single-center studies conducted in Beijing, Tianjin, and Jiangsu, four of which were conducted in Beijing. Only one relevant multicenter study was conducted in Beijing, Shanghai, and Guangzhou, to compare the results among different cities [44].
All studies project the future temperature-related mortality risk of different periods representing the short-term and long-term effects of climate change to allow for different strategies to be used in different periods. In the process of projecting future temperature, in addition to individual study-specified future temperatures, most of the research is based on different GCMs and different RCPs to obtain the future temperature.
Since the studies were all conducted after 2013, when the IPCC5 was published, they all used RCPs and mostly tend to use RCP 4.5 and RCP 8.5 for 2018. However, two studies also applied RCP 2.6, which assumed that emissions might be controlled by policies [40, 45]. By far, an increasing number of GCMs were used in the studies, which can reduce the uncertainty caused by GCM selection and make the projection results more scientific. Current studies used statistical downscaling methods to obtain the future temperatures of the region, which may be related to the greater number of GCMs and the fact that statistical downscaling is more convenient and feasible. In the calculation of the exposure-response relationship between temperature and mortality, the time span of most studies is very short (below 5 years), and individual studies range from 5 to 10 years. Most of the studies used DLNM, which is recognized worldwide; the daily average temperature is a more common temperature indicator. Finally, when projecting temperature-related mortality risk in the future, half of the studies projected the risk of future temperature-related deaths utilizing the population projected by the United Nations for high, medium, and low fertility rates and the future population projected by the five population scenarios’ SSPs 1–5 provided by the IPCC5. Only two studies considered the population’s adaptability to future temperatures, using methods that reduce the slope of exposure-response relationship and change the threshold temperature [34, 40]. In the process of projecting future temperature-related mortality, only two studies quantified the uncertainty and used the method of ANOVA-type estimation of variance components (VC) [34, 37].
8.3.2 Results
Although most of the studies were conducted in different cities, the results of China’s studies showed a consistent direction. The studies projecting future heat-related mortality have all shown that it would increase and the risk of a longer projection period is greater [15, 34, 37, 40, 43, 44]. Under the RCP 8.5 scenario, the number of heat-related deaths among aging individuals is projected to increase by a median of 39.1% (95% CI, 11.1–83.3%) in the 2020s and 264.9% (95% CI, 117.5–427.3%) in the 2080s, compared with the number of deaths in the 1980s in Beijing [34]. The studies simultaneously projecting future heat-related mortality and cold-related mortality have shown that the heat effects would increase and the cold effects would decrease. Zhang et al. indicated that with the temperature decreased 1 °C in the 2080–2099 period, Beijing, Shanghai, and Guangzhou would experience a decrease of 3.1, 2.2, and 4.8 deaths, respectively, per 100,000 people. In addition, the decreased cold-related mortality did not offset the effects of increased heat-related mortality [44]. The future temperature-related mortality risk will vary by different outcomes, populations, and adaption abilities.
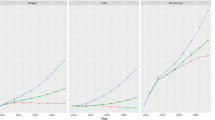
The projection of the causes of mortality is also an important issue under the changing climate. The current studies tended to project the future effects of temperature on cardiovascular disease [40, 42, 43]. The number of cold-related cardiovascular deaths of the 2070s would decrease by 694 under RCP 8.5 in Beijing, but it did not offset the increased heat-related cardiovascular mortality, which was 1013 deaths, under RCP 8.5 [40]. Compared to the corresponding risks of the baseline period, the future heat-related cardiovascular mortality risks in Beijing will increase by an average percentage of 18.4%, 47.8%, and 69.0% in the 2020s, 2050s, and 2080s, respectively, under RCP 4.5, and by 16.6%, 73.8%, and 134% in the 2020s, 2050s, and 2080s, respectively, under RCP 8.5 [42]. Recent studies have begun to project the future temperature effect of stroke and acute ischemic heart disease. Figure 8.1 showed that with the population held constant at the 2010 level, the annual number of net and heat-related acute deaths in Beijing from the 1980s to the 2080s under both RCP 4.5 and RCP 8.5 was highest for acute ischemic heart disease, followed by ischemic stroke and hemorrhagic stroke, and the annual number of cold-related acute deaths was highest for acute ischemic heart disease, followed by hemorrhagic stroke and ischemic stroke [37] (Fig. 8.1). In addition, this study also projected the percentage variation in the change of the monthly median number temperature-related deaths from the 1980s to the 2080s under RCP 4.5 and RCP 8.5. And this calculation showed that the percentage increases for the monthly death projections ischemic heart disease and stroke in the 2080s were greatest in the summer months, obviously occurring in August [37].
Distribution of temperature-related annual acute deaths for ischemic stroke, hemorrhagic stroke, and acute ischemic hearth disease in the 1980s, 2020s, 2050s, and 2080s using 31 climate models and the RCP 4.5 and RCP 8.5 scenarios (Reproduced with permission from Li et al. [43])
Understanding the future health risk of vulnerable populations under changing climates is crucial for policy making. So far, most studies only project the risk of future temperature-related deaths in the total population, and only one study regarded the elderly as a vulnerable population. Li et al. projected the heat-related mortality risk among the aging population in Beijing and found that under RCP 8.5 and a medium-sized scenario of population by the 2080s, the future number of deaths showed a 264.9% increase compared with the number of deaths in the 1980s [34] (Fig. 8.2). More research is needed to project the future temperature-related mortality risk of more vulnerable populations in China.
Distribution of annual heat-related deaths for 31 GCMs and RCP 4.5 and RCP 8.5 scenarios in the 1980s, 2020s, 2050s, and 2080s, with constant population (Reproduced from Li et al. [34])
There are very few studies that consider adaptation when projecting the health risks under climate change. Only two studies considered the population’s adaptability to future temperatures, using methods that reduce the slope of the exposure-response relationship and change the threshold temperature [34, 40]. Future heat-related mortality risk will decrease when this adaptation is considered. In the 2080s, with the adaptation rates assumed at 30 and 50% in Beijing, the increase in the number of heat-related deaths in the aging population is approximately 7.4 times and 1.3 times larger, respectively, than the corresponding number of deaths in the 1980s under a scenario of high-sized population and RCP 8.5 [34] (Fig. 8.3). The number of cold-related deaths may increase due to worse adaptation to colder temperatures. Zhang et al. indicated that under RCP 8.5, the number of cold-related deaths during the 2050s increased by 548 under 100% adaptation, compared with that under 0% adaptation [40].
Increases in the number of heat-related deaths from the 1980s (median of 31 models) in the 2020s, 2050s, and 2080s under RCP 4.5 and RCP 8.5 scenarios and different population-variant scenarios with different adaptation levels (Reproduced from Li et al. [34])
8.4 Limitations and Perspectives in China
In summary, the first study to project the temperature-related mortality risk in China was conducted in 2014, and there have been few studies in China until recently. Some limitations and perspectives are provided below.
First, current studies mostly concentrate on Chinese metropolitan areas (e.g., Beijing, Shanghai, Tianjin, Jiangsu, Guangzhou), ignoring the emerging health risk in other cities with higher future temperatures. Therefore, more multiple-city and multiple-county studies should be required to project the risk of future temperature-related mortality.
Second, future climate warming will not only increase the risk of heat-related mortality but also lead to a lower risk of cold-related mortality. Considering that current studies mostly focus on the risk of future heat-related mortality, more studies should also focus on the risk of future net temperature-related mortality.
Third, because the effect of temperature on different diseases is different, the outcome of future studies should focus not only on non-accidental mortality risk but should also continue to project the risk of mortality from sensitive diseases, such as myocardial infarction.
Fourth, the longer the historical data is, the more stable the exposure-relationship between the temperature and mortality. Now, in the calculation of the exposure-response relationship, the periods of historical data were too short (generally 3–5 years), and studies should extend the periods of historical data.
Fifth, it is best to obtain the time series of the daily values by multiple GCMs and multiple RCPs. When projecting future temperatures, some studies have specified the temperatures; because the specified temperature is published by the IPCC at the global level, it cannot accurately represent the temperature change in the study area, so this method cannot accurately project the time series of future daily deaths. In addition, some studies use fewer GCMs and RCPs, which would increase the uncertainty in projecting future temperatures.
Sixth, changes in the structure of the future population and adaptability to future temperatures will affect the projection of future temperature-related death risks; thus, demographic changes should be considered upon the assessment of future temperature-related mortality risk. In addition, future studies are required to address the changing acclimatization of the population to future temperatures.
References
Hopstock LA, Fors AS, Bønaa KH, et al. The effect of daily weather conditions on myocardial infarction incidence in a subarctic population: the Tromsø study 1974-2004. J Epidemiol Community Health. 2012;66:815–20.
Oudin Åström D, Schifano P, Asta F, et al. The effect of heat waves on mortality in susceptible groups: a cohort study of a Mediterranean and a northern European City. Environ Health. 2015;14:30.
Sen T, Astarcioglu MA, Asarcikli LD, et al. The effects of air pollution and weather conditions on the incidence of acute myocardial infarction. Am J Emerg Med. 2016;34:449–54.
Smith S, Elliot AJ, Hajat S, et al. The impact of heatwaves on community morbidity and healthcare usage: a retrospective observational study using real-time syndromic surveillance. Int J Environ Res Public Health. 2016;13(1):E132.
Wichmann J, Ketzel M, Ellermann T, Loft S. Apparent temperature and acute myocardial infarction hospital admissions in Copenhagen, Denmark: a case-crossover study. Environ Health. 2012;11:19.
Phung D, Thai PK, Guo Y, et al. Ambient temperature and risk of cardiovascular hospitalization: an updated systematic review and meta-analysis. Sci Total Environ. 2016;550:1084–102.
Sanderson M, Arbuthnott K, Kovats S, et al. The use of climate information to estimate future mortality from high ambient temperature: a systematic literature review. PLoS One. 2017;12:e0180369.
Gasparrini A, Guo Y, Sera F, et al. Projections of temperature-related excess mortality under climate change scenarios. Lancet Planet Health. 2017;1(9):e360–7.
Woodward A. Heat, cold and climate change. J Epidemiol Community Health. 2014;68(7):595–6.
Wang Y, Shi L, Zanobetti A, Schwartz JD. Estimating and projecting the effect of cold waves on mortality in 209 US cities. Environ Int. 2016;94:141–9.
Bhaskaran K, Gasparrini A, Hajat S, et al. Time series regression studies in environmental epidemiology. Int J Epidemiol. 2013;42:1187–95.
Lee JY, Lee SH, Hong S-C, Kim H. Projecting future summer mortality due to ambient ozone concentration and temperature changes. Atmos Environ. 2017;156:88–94.
Guo Y, Li S, Liu DL, et al. Projecting future temperature-related mortality in three largest Australian cities. Environ Pollut. 2016;208:66–73.
Bunker A, Wildenhain J, Vandenbergh A, et al. Effects of air temperature on climate-sensitive mortality and morbidity outcomes in the elderly; a systematic review and meta-analysis of epidemiological evidence. EBioMedicine. 2016;6:258–68.
Chen K, Horton RM, Bader DA, et al. Impact of climate change on heat-related mortality in Jiangsu Province, China. Environ Pollut. 2017;224:317–25.
Martinez GS, Baccini M, De Ridder K, et al. Projected heat-related mortality under climate change in the metropolitan area of Skopje. BMC Public Health. 2016;16:407.
Heaviside C, Tsangari H, Paschalidou A, et al. Heat-related mortality in Cyprus for current and future climate scenarios. Sci Total Environ. 2016;569–570:627–33.
Huang C, Barnett AG, Wang X, et al. Projecting future heat-related mortality under climate change scenarios: a systematic review. Environ Health Perspect. 2011;119:1681–90.
Sheridan SC, Allen MJ, Lee CC, Kalkstein LS. Future heat vulnerability in California, part II: projecting future heat-related mortality. Clim Change. 2012;115:311–26.
Barreca AI. Climate change, humidity, and mortality in the United States. J Environ Econ Manage. 2012;63(1):19–34.
Ostro B, Barrera-Gómez J, Ballester J, et al. The impact of future summer temperature on public health in Barcelona and Catalonia, Spain. Int J Biometeorol. 2012;56:1135–44.
Kingsley SL, Eliot MN, Gold J, et al. Current and projected heat-related morbidity and mortality in Rhode Island. Environ Health Perspect. 2016;124(4):460–7.
Lee JY, Kim H. Projection of future temperature-related mortality due to climate and demographic changes. Environ Int. 2016;94:489–94. https://doi.org/10.1016/j.envint.2016.06.007.
Wang Y, Nordio F, Nairn J, et al. Accounting for adaptation and intensity in projecting heat wave-related mortality. Environ Res. 2018;161:464–71.
Sexton DMH, Murphy JM, Collins M, et al. Multivariate probabilistic projections using imperfect climate models part I: outline of methodology. Climate Dynam. 2012;38(11–12):2513–42.
Gosling SN, Hondula DM, Bunker A, et al. Adaptation to climate change: a comparative analysis of modeling methods for heat-related mortality. Environ Health Perspect. 2017;125(8):087008.
Mills D, Schwartz J, Lee M, et al. Climate change impacts on extreme temperature mortality in select metropolitan areas in the United States. Clim Change. 2015;131:83–95.
Baaghideh N, Intergovernmental Panel on Climate Change, editors. Special report on emissions scenarios: a special report of Working Group III of the Intergovernmental Panel on Climate Change. Cambridge, New York: Cambridge University Press; 2000.
Petkova EP, Vink JK, Horton RM, et al. Towards more comprehensive projections of urban heat-related mortality: estimates for new York City under multiple population, adaptation, and climate scenarios. Environ Health Perspect. 2017;125(1):47–55.
Gerland P, et al. World population stabilization unlikely this century. Science. 2014;346:234–7.
Lutz W, Samir KC. Dimensions of global population projections: what do we know about future population trends and structures? Philos Trans R Soc Lond A. 2010;365(1554):2779–91.
Hajat S, Vardoulakis S, Heaviside C, Eggen B. Climate change effects on human health: projections of temperature-related mortality for the UK during the 2020s, 2050s and 2080s. J Epidemiol Community Health. 2014;68:641–8.
Kim D-W, Deo RC, Chung J-H, Lee J-S. Projection of heat wave mortality related to climate change in Korea. Nat Hazards. 2016;80(1):623–37.
Li T, Horton RM, Bader DA, et al. Aging will amplify the heat-related mortality risk under a changing climate: projection for the elderly in Beijing, China. Sci Rep. 2016;6:28161.
Jenkins K, Hall J, Glenis V, et al. Probabilistic spatial risk assessment of heat impacts and adaptations for London. Clim Change. 2014;124:105–17.
Ballester J, Robine J-M, Herrmann FR, Rodó X. Long-term projections and acclimatization scenarios of temperature-related mortality in Europe. Nat Commun. 2011;2:358.
Li T, Horton RM, Bader DA, et al. Long-term projections of temperature-related mortality risks for ischemic stroke, hemorrhagic stroke, and acute ischemic heart disease under changing climate in Beijing, China. Environ Int. 2018b;112:1–9.
Knowlton K, Lynn B, Goldberg RA, et al. Projecting heat-related mortality impacts under a changing climate in the new York City region. Am J Public Health. 2007;97:2028–34.
Kinney PL, Schwartz J, Pascal M, Petkova E, Tertre AL, Medina S, Vautard R. Winter season mortality: will climate warming bring benefits? Environ Res Lett. 2015;10(6):064016.
Zhang B, Li G, Ma Y, Pan X. Projection of temperature-related mortality due to cardiovascular disease in Beijing under different climate change, population, and adaptation scenarios. Environ Res. 2018;162:152–9.
Kinney PL, O’Neill MS, Bell ML, Schwartz J. Approaches for estimating effects of climate change on heat-related deaths: challenges and opportunities. Environ Sci Policy. 2008;11:87–96.
Li T, Ban J, Horton RM, et al. Heat-related mortality projections for cardiovascular and respiratory disease under the changing climate in Beijing, China. Sci Rep. 2015;5:11441. https://doi.org/10.1038/srep11441.
Li Y, Li G, Zeng Q, et al. Projecting temperature-related years of life lost under different climate change scenarios in one temperate megacity, China. Environ Pollut. 2018;233:1068–75.
Zhang J, Li T, Tan JG, et al. Impact of temperature on mortality in three major Chinese cities. Biomed Environ Sci. 2014;27:485–94.
Li G, Guo Q, Liu Y, et al. Projected temperature-related years of life lost from stroke due to global warming in a temperate climate City, Asia: disease burden caused by future climate change. Stroke. 2018a;49:828–34.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Li, T., Sun, Z., Zhang, Y., Chen, C., Ban, J. (2019). Future Temperature-Related Mortality Risk Under Climate Change Scenarios. In: Lin, H., Ma, W., Liu, Q. (eds) Ambient Temperature and Health in China. Springer, Singapore. https://doi.org/10.1007/978-981-13-2583-0_8
Download citation
DOI: https://doi.org/10.1007/978-981-13-2583-0_8
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-2582-3
Online ISBN: 978-981-13-2583-0
eBook Packages: MedicineMedicine (R0)