Abstract
Retrograde transneuronal injury refers to damage from superior neurons to their inferior neurons across synapse retrogradely in the course of the nerve conduction pathway. In the visual pathway, common pathological changes are those lesions in the lateral geniculate body (LGB), mainly including the vascular lesions, tumor, infections, and trauma on the occipital or temporal lobes, which may lead to damage to the retinal ganglion cells (RGCs) and their axons (nerve fibers). In this section, we will describe two cases and tentatively explore the mechanism.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Retrograde transneuronal injury refers to damage from superior neurons to their inferior neurons across synapse retrogradely in the course of the nerve conduction pathway. Common pathological changes are those lesions in the lateral geniculate body (LGB), mainly including the vascular lesions, tumor, infections, and trauma on the occipital or temporal lobes, which may lead to damage to the retinal ganglion cells (RGCs) and their axons (nerve fibers). In this section, we will describe two cases and tentatively explore the mechanism.
1 Case 1
1.1 Case Presentation
A 32-year-old female patient complained of blurred vision in both eyes for 6 months after the temporal lobe meningioma excision. She had neither accompanying symptoms including visual distortion, red eye, and sore eye nor discomforts such as headache, nausea, and vomiting. Three months before, the patient had been found with left hemianopia in both eyes during the visual field test. She had been given neurotrophic drugs for improving microcirculation. The history of trauma, other ocular diseases, and systemic diseases was denied.
The uncorrected visual acuity (UCVA) was 20/20 OU. The intraocular pressure (IOP) was normal OU. Slit-lamp examination of her anterior segments was unremarkable in both eyes, with sensitive direct light reflexes of both pupils. Fundus examination revealed that the optic disc was pale in color with clear margin in both eyes, and many vascular branches were distributed above the right optic disc, while macula fovea reflection was present in both eyes (Fig. 58.1).
Standardized automated perimetry demonstrated left homonymous hemianopia that partially extended across the vertical midlines, more severe in the left eye (3 months after the onset, Fig. 58.2).
Optical coherence tomography (OCT) scan of the ganglion cell layer (GCL) thickness at the macula showed that, bounded by a vertical midline through the macular fovea, GCL thickness of the temporal retina at the right macula and GCL thickness of the nasal retina at the left macula decreased significantly (Fig. 58.3).
OCT scan of the macula thickness showed that, with a vertical midline through the macular fovea as the boundary, the GCL thickness decreased significantly at its temporal side in the right eye and at its nasal side in the left eye (Fig. 58.4).
Pattern visual evoked potential (P-VEP) showed decreased amplitudes of P100 with normal latency in both eyes (Fig. 58.5).
Magnetic resonance imaging (MRI) in axial view of the head revealed multiple patch-like hypointense signals on T1-weighed image (T1WI) and hyperintense T2WI in the right temporal lobe, basal ganglion, and thalamus, suggesting multiple softening lesions (Fig. 58.6).
1.2 Final Diagnosis
The final diagnosis was postoperative complications of temporal lobe meningioma resection.
1.3 Case Review
The visual field damages of the patient in this case are left homonymous hemianopia, mainly due to the damage on the right LGB and the visual pathway behind it caused by the meningioma in the right temporal lobe, basal ganglia, and thalamus. In addition to left hemianopia, the bilateral visual field damages partially crossed over the vertical midline. The reason may be the damage on the anterior visual pathway from transient intracranial hypertension or ischemia during the preoperative or perioperative period. It is noteworthy that, with a vertical midline through the fovea as the boundary, the RGCs and the thickness of macula decreased significantly on the nasal side in the right eye and temporal side in the left eye. Especially in the layer of RGCs, such manifestations were more prominent. In this case, there were no abnormalities in either eye in the past, and the visual field defects and retinal changes both occurred secondary to the meningioma. Therefore, we speculated that retrograde transneuronal injury was the theoretical basis for the damage to the RGCs in both his eyes.
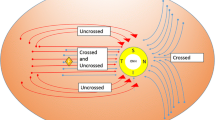
In the visual pathway, nerve fibers originated from RGCs converge and form optic nerves, which perform neurotransmissions in the LGB. The fibers from the LGB form the optic radiation and project to the visual center of the occipital lobe. In this case, the damage on the LGB and the visual pathway behind it crossed synapses retrogradely and run backward to cause damage to its inferior neurons, RGCs. Clinically, we have also observed optic nerve damages, mainly manifested as thinning of peripapillary retinal nerve fiber layers. However, the distribution of the thinning regions was more complicated. The anatomical correspondence between such changes and the lesion locations of the posterior visual pathway were not as consistent as that observed between the distribution of the thinning of the GCL and the lesion locations. Therefore, no in-depth analysis of the optic nerve damage is made here.
2 Case 2
2.1 Case Presentation
A 47-year-old male patient had suffered from a shadow over half of the visual field in both eyes for 1 year. He had felt blurred vision during driving 1 year before. There had been no accompanying ocular symptoms such as visual distortion, red eye, or sore eye and no systemic discomforts such as dizziness, headache, nausea, vomiting, and tinnitus. The patient had visited a local hospital and was treated with drugs, but the details were not clear. However, his visual acuities in both eyes decreased progressively accompanied by left limb weakness. Visual field test showed left homonymous hemianopia. The brain MRI image showed infarction in the right occipital lobe, temporal lobe, and thalamus. Then the patient was diagnosed with cerebral infarction and was treated with drugs for improving circulation and neurotrophy. After that, the symptoms of left limb weakness improved, but the shadow in visual fields of both eyes had no significant relief. The patient had suffered from hyperlipidemia and fatty liver for 5 years and denied the history of trauma, other ocular diseases, or familial diseases.
The uncorrected visual acuity (UCVA) was 20/25 OD and 20/50 OS, and the best corrected visual acuity (BCVA) was 1.0 OU. The intraocular pressure (IOP) was normal OU. Slit-lamp examination of his anterior segments in both eyes was unremarkable, except for slightly increased density of both lenses. Fundus examination revealed pink optic disc with clear margin and normal retinal vessels in both eyes (Fig. 58.7).
Standardized automated perimetry demonstrated left homonymous hemianopia in both eyes (Fig. 58.8).
OCT scan of GCL thickness at the macula showed that the color representing the thickness of RGCs temporal to the right macula and nasal to the left macula significantly faded (arrow) in the pseudo-color thickness maps, suggesting local GCL thickness is decreasing. The measurements of sector thickness showed that the GCL thickness in the temporal sector of the right macula and the GCL thickness in the nasal sector of the left macula became thinner than those of the contralateral sectors (Fig. 58.9).
GCL thickness analysis printout in OCT. The color representing the region temporal to the right macula and the region nasal to the left macula (arrow) significantly faded, suggesting that decreased GCL thickness is there; the GCL in the temporal sector of the right macula and in the nasal sector of the left macula became thinner than those of the contralateral sectors
Pseudo-color images in OCT scan of macular thickness showed no significant changes in either eye, but the topographic maps showed that the macular thickness in the temporal region of the right macula and in the nasal region of the left macula were slightly smaller than those in the corresponding contralateral regions (Fig. 58.10).
Macular thickness analysis printout in OCT. Pseudo-color images in OCT scan of macular thickness showed no significant changes in either eye, but the topographic maps showed that the macular thickness in the temporal region of the right macula and in the nasal region of the left macula were slightly smaller than those in the corresponding contralateral regions (thickness value in green areas is smaller than that in the faint yellow and pink areas)
P-VEP revealed the amplitude values of the P100 wave decreased with normal latencies in both eyes (Fig. 58.11).
Head MRI demonstrated an extensive softening lesion involving the right occipital lobe, temporal lobe, and thalamus (Fig. 58.12).
2.2 Final Diagnosis
The final diagnosis was infarction in the right occipital lobe, temporal lobe, and thalamus.
2.3 Case Review
The visual field of this patient was also manifested as left hemianopia, which was mainly due to the damage on the visual pathway behind the LGB and the occipital center, which was caused by the infarction involving the right occipital lobe, basal ganglia, and thalamus. OCT results showed that, with a vertical midline through the fovea as the boundary, GCL thickness decreased significantly on its temporal side in the right eye and its nasal side in the left eye, as compared with those on the contralateral sides. In this case, there were no abnormalities in either eye in the past, and visual field defects and GCL thickness changes both occurred secondary to cerebral infarction. Therefore, we speculated that the loss of RGCs in both eyes was due to the damage retrograding from the occipital lobe or the posterior visual pathway behind the LGB to the retina after the cerebral infarction, i.e., retrograding across one level of neurons or two levels of neurons, respectively.
Compared with case 1, the loss of RGCs in case 2 occurred later and less severely. The reason may be that the lesion of case 1 was located more anteriorly in the visual pathway and more severe, which lead to the damage on RGCs from retrograding across one level of neurons. In case 2, the lesion was located closer to the posterior visual pathway, and the damage on RGCs resulted from retrograding across two levels of neurons; furthermore, there might be collateral synapse connections, so the damage to RGCs was less severe. In addition, in OCT printout, it can be seen that RGCs in case 2 showed a significant loss, but the change in retinal thickness was still not obvious. Therefore, the observation of GCL thickness is more sensitive than that of macular thickness for the detection of a retrograde transneuronal injury.
3 Discussion
Transneuronal injury refers to the damage from a level of neurons to its upper or lower level of neurons via crossing the synapses along the nerve conduction pathway. Such injury is also known as transsynaptic degeneration. In other words, the loss of extraneous projecting nerve fibers will lead to neurons’ atrophy and death. There are two types of transneuronal injuries. If the optic nerve is damaged in one eye, the neurons in the LGB will undergo atrophy and then disappear, which is called ascending transneuronal degeneration. Otherwise, the degeneration and apoptosis of RGCs occurring after the onset of occipital lobe lesions are called retrograde or descending transneuronal damage. The ones discussed in this section belong to the latter.
Clinically, visual field damages of homonymous hemianopia are caused by the damage to the visual pathway behind the optic chiasm especially the posterior visual pathway behind LGB. The retrograde transneuronal damage on the optic nerve from the lesions in the occipital visual center or the posterior visual pathway behind the LGB has already been confirmed by autopsy and animal studies but is still in controversy in clinical practice. Therefore, this theory had not been confirmed until the introduction of OCT, which can be used to objectively and dynamically observe the change in the thickness of the retinal nerve fiber layers [1]. At the same time, it also suggests that the synapses not only transmit visual signals via neurotransmitters but also help superior neurons to exert neurotrophic and supportive effects on inferior neurons.
The first common reason of the damages on the posterior visual pathway behind the LGB is vascular lesions in the temporal lobe and the occipital lobe, such as cerebral hemorrhage and infarction. A common clinical manifestation is a sudden occurrence of contralateral homonymous hemianopia, often accompanied by the symptoms of limbs ipsilateral to the lesion. The second reason is space-occupying lesions, such as meningioma, neuroglioma, hemangioma, and acoustic neuroma in the temporal or occipital lobes. These lesions also clinically manifest homonymous hemianopia with chronic onset and gradual severity, often accompanied by the intracranial hypertension manifestations such as headache. In addition, traumatic injury to the temporal or occipital lobe is more easily diagnosed as there is usually a definite history of trauma. Homonymous hemianopia is also a characteristic visual field change of them.
We also found that the loss of RGCs and their fibers was not always detectable in patients with homonymous hemianopia, which is also one of the main reasons why this theory is controversial. This may be related to the patient’s age of disease onset, the severity of intracranial lesions, the lesion location in the visual pathway, and the time from disease onset. Studies have shown that the loss of RGCs and their fibers caused by occipital lobe damage can be detected as early as 3.6 months after onset, and the most significant loss is within 2 years after onset, and the loss will continue in the progression of disease, with the loss rate of peripapillary RNFL being about 9.08 μm reduction in thickness every 10 years [2].
There are also some authors who do not believe in retrograde transneuronal injury. They believe that even there is such a phenomenon, RGCs damage is secondary to the damage on the white matter of the visual pathway or due to the influence of the blood supply in the visual pathway, including the LGB. However, animal experiments confirmed that, after the cortex receiving the macular projecting in the occipital lobe was removed, RGCs in macula experienced significant loss or degeneration [3]. Obviously, the removal of partial occipital cortex will not affect the LGB or the posterior visual pathway; therefore, only the theory of retrograde transneuronal damage can explain the loss of RGCs under this condition.
The visualization of the optic nerve and the high resolution of OCT not only enable the confirmation of the existence of retrograde transneuronal damage but also provide a platform for further studies [1]. However, due to the great individual differences in the optic nerves and retina, retrograde transneuronal damages are greatly influenced by gender, age, ocular axis, refractive status, and optic disc dysplasia. With regard to the study of retrograde transneuronal damages using OCT, longitudinal studies with large sample sizes and control groups are more convincing.
In addition, it is also worth investigating whether the visual field changes caused by retrograde transneuronal damages will aggravate the visual field damages caused by the original disease and how to judge the retrograde transneuronal damage by perimetry.
References
Jindahra P, Petrie A, Plant GT. Retrograde trans-synaptic retinal ganglion cell loss identified by optical coherence tomography. Brain. 2009;132(Pt 3):628–34.
Jindahra P, Petrie A, Plant GT. The time course of retrograde trans-synaptic degeneration following occipital lobe damage in humans. Brain. 2012;135(Pt 2):534–41.
Johnson H, Cowey A. Transneuronal retrograde degeneration of retinal ganglion cells following restricted lesions of striate cortex in the monkey. Exp Brain Res. 2000;132(2):269–75.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd. & People's Medical Publishing House, PR of China
About this chapter
Cite this chapter
Xie, X., Fan, N., Wang, N. (2019). Retrograde Transneuronal Injury: From the Posterior Optic Pathway to Retinal Ganglion Cells. In: Wang, N., Liu, X., Fan, N. (eds) Optic Disorders and Visual Field. Advances in Visual Science and Eye Diseases, vol 2. Springer, Singapore. https://doi.org/10.1007/978-981-13-2502-1_58
Download citation
DOI: https://doi.org/10.1007/978-981-13-2502-1_58
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-2501-4
Online ISBN: 978-981-13-2502-1
eBook Packages: MedicineMedicine (R0)