Abstract
Acute kidney injury (AKI) occurs frequently in children undergoing surgery for complex congenital heart disease and is associated with poor outcomes. Unfortunately, despite several decades’ worth of data delineating a strong epidemiologic signal for both high incidence and association with outcomes such as prolonged mechanical ventilation, high infection rates, and increased rates of death, very little progress has been made in reducing the reach and sequelae of the disease. In this chapter, elements of pathophysiology and epidemiology will be integrated into the perspectives of past, present, and future patient care. Existing views of the etiology and management of AKI will be challenged—ultimately shifting the AKI paradigm toward highlighting avenues of research and patient management requiring broadscale, multidisciplinary study, investment, and progress.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Acute kidney injury (AKI)
- Cardiopulmonary bypass (CPB)
- Cardiac intensive care unit (CICU)
- Fluid management
- Renal angina
- Risk stratification
- Peritoneal dialysis (PD)
- Urinary biomarkers
1 Introduction
Acute kidney injury (AKI) is a syndrome occurring frequently in critically ill patients. With remarkable consistency, AKI occurs in approximately one in four critically ill adults [1], children [2], and neonates [3]. In these recent large, multicenter population databases, the incidence of AKI and the association with poor outcomes were independent of severity of illness. In each cohort, compared to injury-free patients, patients with severe AKI suffered prolonged mechanical ventilation, longer duration of both intensive care unit (ICU) and hospital length of stay (LOS), and higher rates of mortality. A global meta-analysis of AKI data in all-age critically ill patients demonstrates a stepwise increase of poor outcome (notably mortality) in unison with increased AKI severity [4].
Nearly three decades’ worth of data indicates AKI is a significant burden in children with complex congenital heart disease undergoing cardiopulmonary bypass (CPB) [5]. In this population, AKI occurs more frequently than in the general pediatric critically ill population but is similarly associated with worse patient outcome than the absence of AKI. An extensive number of ex vivo models of CPB have delineated numerous physiologic drivers putatively placing patients at risk for, or driving, AKI. More effort expended in the past decade to reduce the severity of AKI in these patients or lessen the disease prevalence has failed to slow the overall “progression” of this disease syndrome and its downstream sequelae for children.
In this chapter, the current paradigm of AKI in children following CPB will be challenged. In place of the existing strategy of reactive diagnostics and management, a more predictive, proactive, and anticipatory diagnostic and recognition strategy will be described. Strengths, weaknesses, opportunities, and threats will be described (Fig. 19.1). The potential to move the needle and improve outcomes for children following cardiac surgery by reducing the burden of AKI is possible but requires multidisciplinary, collaborative, and sustained investment and effort.
2 Epidemiology: A Chance to Move the Needle
Acute kidney injury (AKI) is a syndrome with a significant disease burden in the critically ill patient. The recent AKI-EPI study performed in nearly 2000 adults demonstrated a high disease incidence and significant associations with increased ICU technology and death [1]. In pediatrics, the AWARE (Assessment of Worldwide Acute Kidney Injury, Renal Angina, and Biomarkers) uncovered a 26.9% AKI incidence rate in 4683 children, 11.6% severe AKI [2]. The patients with severe AKI suffered increased adjusted odds (1.77, 95% CI 1.17–2.68) for mortality and a higher death rate (11–2.5%) compared to patients without severe AKI. These findings remained consistent in the neonatal ICU as the AWAKEN (Assessment of Worldwide Acute Kidney Injury Epidemiology in Neonates) identified a 27% AKI rate in 2162 newborns [3]. In the United States, nearly a quarter of a million (240,000) adults undergo cardiac surgery requiring CPB, and 25% patients in this population experience AKI (AKI-CPB). The most recent epidemiologic reports of AKI in children following CPB report an incidence of nearly 50%, slightly higher in neonates (65%) [5,6,7]. After adjustment for covariates, AKI-CPB is independently associated with both short-term and longer-term complications. The short-term sequelae associated with AKI-CPB include longer duration of mechanical ventilation, longer ICU and hospital length of stay (LOS), higher incidence of both low cardiac output syndrome and higher vasoactive medication requirements, and high rates of mortality. Longer-term sequelae include higher incidence of, and transition to, chronic kidney disease and longer-term mortality. It is notable that these findings are consistent regardless of patient age; similar findings are consistently demonstrated in adult AKI-CPB patients. When cost-estimate models are used to isolate the financial burden of AKI in this population, even patients with small changes in serum creatinine carry increased costs (1.6-fold) compared to disease-free patients [8] with a majority of costs increased by LOS and laboratory expenditures. By any measure, the epidemiology of AKI following CPB describes an epidemic with a wide range of associated negative consequences. Taken together, there is a significant need for innovation, discovery, and outcome improvement for these patients.
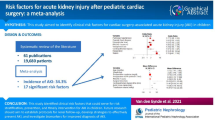
Identification of the at-risk patient for AKI-CPB has no objective methodology. The extensive data in adult and pediatric AKI-CPB has identified a long list of putative risk factors including, but not limited to, age, gender, surgical complexity, CPB time, cross-clamp time, preoperative ventilator support, diabetes mellitus, and hypertension [9]. When stratified by temporal relationship to CPB, the variables become more cleanly delineated into pre-, intra-, and post-CPB groups. The preoperative risks for AKI-CPB have expanded beyond simple demographic associations as genome-wide association studies (GWAS) and other genetic variant studies have uncovered a pattern of predisposing inherited mutations that confer added AKI risk [10]. Additionally, there is more appreciation in the preoperative period for comorbidities such as baseline chronic kidney disease, congestive heart failure, and diabetes (even in children) increasing the risk of postoperative AKI. Intraoperative variables associated with AKI-CPB have traditionally been focused exclusively on duration of bypass time and cross-clamp time. These variables have carried a direct relationship with increases in AKI rates and severity, that is, the longer the time of CPB or cross-clamp, the higher the incidence of severity of AKI. Additionally, other factors such as deep hypothermic arrest, intraoperative hypotension, and low hemoglobin have been associated with higher rates of AKI-CPB. Newer data, however, suggests an independence of AKI from CPB duration in patients controlled by age and surgical complexity. Newer, more sophisticated, and controlled data suggests the dogmatic belief in the direct relationship between AKI-CPB needs to be challenged as primary disease is more powerful in statistical modeling (controlling for confounders)—in adults following coronary artery bypass graft surgery [11], in children with a STAT (Society of Thoracic Surgeons-European Association for Cardiothoracic Surgery) score of at least three, and in homogenous neonates [12]. The postoperative variables associated with AKI-CPB have included the use of renal replacement therapy, the use of mechanical support, and volume status. Although the association of the former two with AKI is relatively intuitive, the latter is an important finding. The importance of volume status, as it relates to fluid accumulation, can be simultaneously a sign of, or a risk factor for, AKI. Early fluid accumulation is a harbinger of AKI in the pediatric CPB population [13, 14], and given the relationship with total body water, fluid accumulation may actually mask AKI recognition and diagnosis [12]. Several recent narrative documents describe phases of critical care and how each relates to net fluid balance [15]. Postoperative CPB data demonstrates a consistent association between avoidance of fluid accumulation (i.e., lower total net fluid balance) and improved patient outcomes.
Identifying the patient at risk for AKI prior to injury may ultimately improve outcome. Although no singular effective therapy has been identified to date, a prevailing sentiment in the critical care nephrology community is earlier diagnosis (or recognition) would expedite “management options” and lead to less deleterious associated effects of AKI. The parallel for this belief is the now routine assessment of cardiac angina or signs of impending and active stroke (“FAST”) for recognition of unstable acute coronary syndrome (ACS) and cerebrovascular ischemia, respectively. Simply, the recognition of risk factors paired with tangible evidence of active injury leads a practitioner to institute immediate action. In the case of ACS, the action is confirmatory testing using troponin measurements and electrocardiogram with resultant notification and activation of the cardiac catheterization team. In the case of stroke, national guidelines are in place to regulate the ideal time for management of ischemic or hemorrhagic stroke from recognition of symptoms. These paradigms do not yet exist for AKI. Driven by the examples, however, the concept of renal angina has been described in the general pediatric ICU population [16, 17]. Similar to cardiac Prinzmetal’s angina, renal angina (operationalized into the renal angina index) combines known risk factors for severe AKI with early signs of filtrative or tubular injury (small changes in creatinine or fluid accumulation) 12 h into an ICU admission for the purposes of identifying the patients at highest risk of severe AKI 3 days after admission [18]. Notably, biomarker incorporation into the model, meaning biomarkers tested in patients positive for renal angina, led to a significant improvement in the specificity of prediction [19]. Similar risk stratification tools are being tested in adult ICU patients [20].
Patients at risk of AKI after CPB can be identified earlier. Given the significant amount of data from both adults and children associating AKI-CPB with poor outcome, more attention should be given the recent literature describing the association of even early changes in creatinine and/or fluid accumulation with poor outcome. Risk factors for AKI after CPB are known. Prior to operative procedures, a patient’s risk associated with genomic variants and past medical history and comorbidities can be incorporated into a subsequent management strategy (described later). A cardiac renal angina prodrome is currently being explored. Increasing appreciation of the epidemic postoperative burden from AKI (by cardiac intensivists and cardiologists) would raise the resting index of suspicion. Taken together, if moving the needle for the epidemiology of the disease, that is, if outcomes can actually be improved, it will rely on more vigilant and objective assessments of AKI risk.
3 Pathophysiology: Biology to Drive Diagnostics
The pathophysiology of AKI-CPB is multifactorial. Traditional thinking identifies, broadly, the categories of oxygen delivery, inflammation, and direct free radical or oxidative toxicity as drivers for reducing renal function for patients on and after CPB support. Renal blood flow can be impaired during CPB, particularly during aortic cross-clamp, leading to regional ischemia in the renal circulation. Concordant with ischemia is impairment in oxygen delivery to a system already under precise homeostatic control of regional oxygen tone. Study of animal models of AKI-CPB is limited to larger animals (as opposed to murine models) given technical complexity, but available data suggest homology in both perturbations in regional oxygen delivery and renal blood flow during CPB [21]. Clinical studies consistently demonstrate an association with noninvasive tissue oximetry and measurement of oxygen metabolism with the initiation, continuation, and discontinuation of CPB (changes occur in response to blood flow). Inflammation during and after CPB is secondary to liberation of humoral cytokines as blood interacts with an artificial surface such as a catheter or bypass surface. Numerous ex vivo and in vitro studies describe a pro-inflammatory cascade during this interaction (blood and surface), theoretically leading to an increase in systemic inflammation during and after CPB ultimately affecting the renal parenchyma and cellular integrity [22,23,24]. Central to the pro-inflammatory cascade is the transcription factor NF-kB [25], an intracellular mediator of upregulation of adhesins, selectins, and multiple immunoglobulins. Interestingly, evidence demonstrating a persistent regional upregulation of NF-kB-related gene products with downstream mediators of dysregulation in inflammation in the renal circulation or parenchyma is scant. The direct nephrotoxicity of CPB is felt to be associated with the liberation and transmigration of oxygen radicals and free oxygen moieties (again when red blood cells come in contact with and shear on the surface of artificial polymers) [26]. Renal tubular epithelial cell integrity can be compromised in the presence of high levels of superoxide and can undergo epithelial-mesenchymal transition to a more pro-fibrotic milieu in the presence of high circulating transforming growth factor-β, upregulated by oxidative conditions [24, 27]. The clinical parallel to these laboratory findings is difficult to isolate as existing diagnostic tools cannot differentiate between types of incipient or ongoing injury in the kidney.
Existing diagnostic criteria create an imprecise definition of AKI after CPB. The available markers of renal dysfunction are either increases in serum creatinine (SCr) or changes in urine output (UOP) as direct indices and changes in filtration, electrolyte imbalance, aberrant drug clearance, and loss of urinary concentrating ability or proteinuria. The markers are themselves flawed. Widespread data and innumerable reports discuss the limitations of SCr for the prediction or diagnosis of AKI, but the most problematic aspects in children are the dependency on muscle mass, the discrepancies between local laboratory standards and “steady state,” and the effect of dilutional volume. The latter is a phenomenon initially described in a post hoc analysis of the Fluid and Catheter Treatment Trial for acute respiratory distress syndrome in adults [28]. Data from children suggests that correcting SCr for net fluid balance uncovers a refined creatinine-based diagnosis of AKI and associated sequelae [12]. Urine output is not reliably checked in the pediatric population without the presence of a Foley catheter. Initiatives to reduce the rate of catheter-associated urinary infections have made a priority of removing “unnecessary” Foley catheters; however, recent adult and pediatric data suggests following urine output closely in the initial days of ICU admission is vital to the accurate identification of AKI [2, 29, 30]. Outside of SCr and UOP, historic data lists serum and urine metrics for AKI diagnosis that have been relatively abandoned since the adoption of international AKI census criteria (RIFLE, AKIN, KDIGO) [31]. Unfortunately, the existing markers and the consensus diagnostic guidelines do little to advance the understanding of AKI or refine diagnosis. Creatinine and UOP still lead to imprecise nomenclature for AKI such as “prerenal” or “intrinsic renal/acute tubular necrosis.” The former is flawed in the sense that patients diagnosed as prerenal may have injury occurring in the kidney, injury may be severe, injury may not be transient, and injury may not be responsive to volume (all of these are implied by the name). An apt example of an imprecise “prerenal” diagnosis is congestive heart failure. Concurrently, patients labeled as ATN often have no histologic evidence of tubular necrosis [32, 33], and more data suggests how inappropriate this terminology is from a pathophysiologic standpoint.
The precision of AKI diagnostics can be improved. A new analysis of creatinine suggests that static measures of creatinine are less indicative of glomerular filtration, instead supporting the case for a kinetic GFR based on change in creatinine over time [34]. In parallel fashion, urine output should be tracked and should likely be tracked in a dynamic state, flow rate change as a function of time. The critical care nephrology community has already issued statements to use more precise terminology such as “functional” or “damage-associated” AKI and to denote AKI phenotypes [35]. AKI biomarkers from the urine are able to delineate a more discrete location of AKI—glomerular, tubular, and mesenchymal—than the generic index reported by changes in creatinine or urine output. Although few novel biomarkers are broadly available for use at the current time, the development and introduction of these markers into clinical practice will facilitate a more precise understanding of the location and severity of AKI. Additionally, as has been well reported, many of these markers are more sensitive to injury, responding in a more temporally proximal nature to incipient or ongoing injury. The most widely reported data focuses on neutrophil gelatinase-associated lipocalin (NGAL), kidney injury molecule-1 (KIM-1), and tissue inhibitor of metalloproteinase-2/insulin-like growth factor-binding protein 7 (TIMP-2/IGFBP7). The pediatric CPB population has served as the ideal cohort of patients for discovery, isolation, derivation, and validation of these markers for prediction of AKI and diagnosis of AKI severity. Respectively, they confer information about tubular viability, mesenchymal or parenchymal damage, and molecular cell-cycle arrest at the level of the glomerulus. Taken together, these markers may render AKI phenotypes that are quite distinct, even though all may demonstrate similar “increases” of SCr from baseline. Literally what this means is testing of biomarkers in combination is likely the next step in biomarker adjudication [29]. Preliminary data indicates that a simple combination of a tubular injury marker and a glomerular filtration marker identifies distinct cohorts of patients—functional AKI or severe AKI [36]. Additionally, tracking biomarkers as they change over time may deliver information with regard to real-time fluid handling and also predict subsequent changes in creatinine, thereby filtration [37]. In addition to markers of kidney injury, testing the functional capacity of the kidney is possible. Applying standardized, objective criteria to urine production after a dose of furosemide, adult data identifies the value of the “furosemide stress test” (FST) for the prediction of severe AKI, AKI progression, and ultimately renal replacement therapy (RRT) utilization [38, 39]. By comparison, the FST is superior to biomarker prediction of AKI [40, 41]. Pediatric data supporting the predictive performance of the FST is beginning to emerge [42]. For the pediatric patient following CPB, the FST is particularly important. Precise control over fluid is emphasized in the perioperative period, and recent data suggests a benefit of early implementation of peritoneal dialysis over the use of furosemide (or continued use) [43]. The ability to use initial response to furosemide to predict AKI progression would potentially be a piece of actionable clinical decision support to the CICU provider making decisions with regard to fluid removal in the patient immediately postoperative from CPB.
Refined epidemiologic data may refine risk factors associated with AKI-CPB. Data controlled for age and surgical complexity now suggests AKI-CPB carries no association with CPB time or patient age [12, 14, 44]. Additionally, modeling suggests a lack of persistent inflammatory mediators in the nephron after 6 h following CPB (initial rise at 2 h with exponential decay)—suggesting a constant pro-inflammatory environment is potentially not contributing to progressive AKI.
Expedited diagnostics may lead to improved outcomes. A host of more contemporary diagnostics for AKI-CPB is available or soon will be (Fig. 19.2). Management bundles for AKI can be derived from the KDIGO AKI practice guideline. In adult patients following CPB, stratification by TIMP-2/IGFBP7 levels post-op into receipt of AKI bundled care resulted in less AKI, less severe AKI, and improved patient outcomes (for those receiving the bundle) [45]. In total, diagnostic improvement for AKI following CPB is imminent. A combination of markers and functional tests, when used in the appropriate context of risk, should identify the patients at highest risk for AKI and certainly delineate levels of risk. The varying degrees of risk, or even incipient and ongoing injury, should naturally suggest more personalized and precise management plans.
Diagnostic advances in AKI. The past, present, and future for the field of AKI diagnostics are depicted. The past and current paradigm is limited by essentially one diagnostic tool—expected to serve as a “do-all” and “be-all” marker. This is inappropriate. The future will offer the opportunity to refine the diagnosis of AKI, improving the precision of diagnosis and hopefully making a more tailored management approach to the disease possible
4 Management: Defense to Offense
The paradigm of management for AKI has been centered on supportive care. Prior to the adoption of census criteria, a universally “accepted” approach lacking stratification included maintenance of mean perfusion pressure, adjustment of medications for renal clearance, avoidance of contrast or other iatrogenic sources of nephrotoxicity, and control of glycemia. The KDIGO guidelines created a tiered approach to management based on degree of AKI risk or severity. Although implementation of the guidelines has been slow, data has emerged demonstrating benefit to the incorporation of these steps in the management of patients with recognized AKI. In the patient with AKI-CPB, no published guidelines exist for management. Most clinicians would recognize the importance of the above stipulated tenets of care but would also incorporate fluid management and special care during the period of postoperative care when low cardiac output syndrome occurs at greatest frequency. The importance of control over fluid balance cannot be overemphasized. Repeated data from pediatric patients demonstrates the negative association of fluid accumulation in the post-CPB period with outcomes, even independent of AKI [46]. Notably, both small changes in SCr and small increases in fluid overload increase the odds for poor patient outcome [47]. Phases of fluid balance in the critically ill patient may be slightly different in the post-CPB patient, especially considering the widespread utilization of modified ultrafiltration during separation from bypass. As mentioned earlier, however, recognition of AKI by SCr can be masked by fluid accumulation, particularly in the small neonate following cardiac surgery. Correction of SCr for net fluid balance has been described in limited data sets and at the very least merits consideration for integration into routine practice (as infants are 75–80% total body water). Outside of these supportive care measures, however, there are few routine actions taken which prevent AKI or reduce AKI progression or severity. In total, the paradigm of AKI management, particularly in CPB, is reactive.
The electronic health record (EHR) can be incorporated into AKI management. Recent reports demonstrate the power of AKI sniffers and alert systems embedded within the EHR—expediting both recognitions for intensive care management teams but also triggering nephrology involvement [48]. The electronic record has several advantages—notably round-the-clock surveillance, objectified assessment, ability to instantaneously and simultaneously alert multiple providers, and the possibility of moving between institutions. As with other systems, EHR recognition systems are limited to some degree by the input variables requiring human. Interestingly, programming to algorithmically follow changes in urine output, or urine flow rate, can increase the rate of AKI prediction [49]. The use of these systems facilitates automatic incorporation or activation of AKI care bundles. Early reports of these systems are promising—demonstrating a reduction in AKI incidence, severity, and progression. As the ability to identify risk factors increases, the preoperative phase may be the time when the EHR serves the greatest utility. A mechanism to create an AKI-CPB risk score prior to CPB—and ultimately adjust intraoperative variables in proportion to the degree of risk or to specific aspects of risk—is how precision medicine will be oriented. Given the amount of pre-, intra-, and postoperative data available on pediatric CPB patients, the population seems ideal to derive and validate automated models of preventative AKI care.
Fluid control in the AKI-CPB patient can be proactive. Novel biomarkers may predict tubular dysfunction and the patients at risk for fluid retention. Early data suggests that the dynamic change of sequential tubular biomarkers can even predict who will be responsive to diuresis [37]. Additionally, retrospective data indicates early and persistent elevation in tubular markers—even in the absence of creatinine elevation, can predict fluid accumulation and the eventual initiation of renal replacement therapy [50]. Next-generation fluid removal machines can ultrafiltrate serum through peripheral catheters, eliminating the need for peritoneal dialysis drains or large central intravenous access in small patients [51]. The incorporation of these next steps will allow providers to be more “in control” of the fluid balance of their patients.
The care of children following cardiopulmonary bypass can move from reactive to proactive. The traditional mindset has followed a defensive, reactive paradigm—limitation of nephrotoxicity, supportive care of vital organs, fluid removal, and frequent assessment of filtration function by creatinine. A more offensive-minded approach is possible with current tools. Stratification of patients both preoperatively and immediately postoperatively into risk strata, linking risk to management bundles from the preoperative phase, early initiation of volume management to prevent fluid accumulation, and use of the electronic medical record to identify patients at risk or experiencing AKI is possible. AKI in the CPB patient is associated with long-term chronic kidney disease, parallel to the rise in chronic renal insufficiency in both adult survivors of AKI and survivors of critical illness in the general pediatric population. A more preventative approach is warranted.
5 Call to Action: Moving the Needle
The understanding and management of acute kidney injury following cardiopulmonary bypass in the pediatric patient is flawed. A combination of the poor understanding of the pathophysiology of disease and outdated and imprecise diagnostics leads to both a likely underestimate of disease incidence and underappreciation of associated sequelae. Problematically, all of these inadequacies synergistically handcuff management—creating a relatively ignorant and defensive approach. The needle can be moved and outcomes can be improved.
In this chapter, the path forward to improved patient outcomes in the pediatric AKI-CPB population has been outlined (Fig. 19.3). This cohort of patients should be risk stratified—and is an ideal population to understand from a genomic and pathophysiologic standpoint—how much risk exists at baseline. This means moving beyond a binary appreciation of risk—but moving to a quantified, objective calculation of risk. A cardiac renal angina score is a first step. Integration of urinary biomarkers for the purpose of assessment of baseline glomerular, tubular, and mesenchymal integrity would be valuable given the recent data describing the importance of sequential biomarker measurements. This should not come as a surprise as almost all of the meaningful metrics of critical illness are, in fact, more illustrative when tracked in dynamic fashion—over time (e.g., lactate, pH). The electronic health record must be integrated into the next generation of management strategies—leveraging the power of instantaneous alerts, data, and objective assessments. A patient-specific bundle of preventative measures can be instituted upon assessment of risk, and combinations of biomarkers can be used to not only help guide postoperative fluid management but also target cohorts of patients potentially responsive to “AKI therapies.” Novel therapeutics were not discussed in this text but include a list of renal vasoactive medications, anti-inflammatory or apoptotic agents, stem cell therapy, and monoclonal therapeutics. Additionally, previous trials for AKI therapeutics including agents such as diuretics, steroids, sodium bicarbonate, and other commonly used medications may actually demonstrate a functional response in the appropriate, stratified groups of patients. Together, all of these approaches offer the potential to increase the recognition and awareness of the problem of AKI-CPB and associated patient outcome. To actually improve outcome, a multidisciplinary approach is required: intensivists, pediatricians, surgeons, cardiologists, nephrologists, pharmacists, and more are required to engage in collaborative prospective study—investing time, resources, and bandwidth to turn the tide against an epidemic.
Changing the paradigm. The needle for outcomes of children suffering AKI-CPB can be moved from an antiquated, defensive reactive paradigm to a more proactive and “offensive” approach. In this paradigm, patients are risk stratified prior to CPB and then recalibrated intra-and postoperatively. Patients are stratified by risk to receive proactive and preventative care, incorporating profiling and phenotyping of illness and ultimately targeted therapeutics
References
Hoste EA, Bagshaw SM, Bellomo R, Cely CM, Colman R, Cruz DN, et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. 2015;41(8):1411–23.
Kaddourah A, Basu RK, Bagshaw SM, Goldstein SL, Investigators A. Epidemiology of acute kidney injury in critically ill children and young adults. N Engl J Med. 2017;376(1):11–20.
Jetton JG, Boohaker LJ, Sethi SK, Wazir S, Rohatgi S, Soranno DE, et al. Incidence and outcomes of neonatal acute kidney injury (AWAKEN): a multicentre, multinational, observational cohort study. Lancet Child Adolesc Health. 2017;1(3):184–94.
Susantitaphong P, Cruz DN, Cerda J, Abulfaraj M, Alqahtani F, Koulouridis I, et al. World incidence of AKI: a meta-analysis. Clin J Am Soc Nephrol. 2013;8(9):1482–93.
Li S, Krawczeski CD, Zappitelli M, Devarajan P, Thiessen-Philbrook H, Coca SG, et al. Incidence, risk factors, and outcomes of acute kidney injury after pediatric cardiac surgery: a prospective multicenter study. Crit Care Med. 2011;39(6):1493–9.
Sethi SK, Kumar M, Sharma R, Bazaz S, Kher V. Acute kidney injury in children after cardiopulmonary bypass: risk factors and outcome. Indian Pediatr. 2015;52(3):223–6.
Sethi SK, Goyal D, Yadav DK, Shukla U, Kajala PL, Gupta VK, et al. Predictors of acute kidney injury post-cardiopulmonary bypass in children. Clin Exp Nephrol. 2011;15(4):529–34.
Dasta JF, Kane-Gill SL, Durtschi AJ, Pathak DS, Kellum JA. Costs and outcomes of acute kidney injury (AKI) following cardiac surgery. Nephrol Dial Transplant. 2008;23(6):1970–4.
Jefferies JL, Devarajan P. Early detection of acute kidney injury after pediatric cardiac surgery. Prog Pediatr Cardiol. 2016;41:9–16.
Stafford-Smith M, Li YJ, Mathew JP, Li YW, Ji Y, Phillips-Bute BG, et al. Genome-wide association study of acute kidney injury after coronary bypass graft surgery identifies susceptibility loci. Kidney Int. 2015;88(4):823–32.
Schopka S, Diez C, Camboni D, Floerchinger B, Schmid C, Hilker M. Impact of cardiopulmonary bypass on acute kidney injury following coronary artery bypass grafting: a matched pair analysis. J Cardiothorac Surg. 2014;9:20.
Basu RK, Andrews A, Krawczeski C, Manning P, Wheeler DS, Goldstein SL. Acute kidney injury based on corrected serum creatinine is associated with increased morbidity in children following the arterial switch operation. Pediatr Crit Care Med. 2013;14(5):e218–24.
Hassinger AB, Wainwright MS, Lane JC, Haymond S, Backer CL, Wald E. Elevated preoperative serum asymmetrical dimethylarginine (ADMA) is associated with poor outcomes after pediatric cardiac surgery. Intensive Care Med. 2012;38(10):1697–704.
Hassinger AB, Backer CL, Lane JC, Haymond S, Wang D, Wald EL. Predictive power of serum cystatin C to detect acute kidney injury and pediatric-modified RIFLE class in children undergoing cardiac surgery. Pediatr Crit Care Med. 2012;13(4):435–40.
Hoste EA, Maitland K, Brudney CS, Mehta R, Vincent JL, Yates D, et al. Four phases of intravenous fluid therapy: a conceptual model. Br J Anaesth. 2014;113(5):740–7.
Basu RK, Zappitelli M, Brunner L, Wang Y, Wong HR, Chawla LS, et al. Derivation and validation of the renal angina index to improve the prediction of acute kidney injury in critically ill children. Kidney Int. 2014;85(3):659–67.
Basu RK, Chawla LS, Wheeler DS, Goldstein SL. Renal angina: an emerging paradigm to identify children at risk for acute kidney injury. Pediatr Nephrol. 2012;27(7):1067–78.
Basu RK, Wang Y, Wong HR, Chawla LS, Wheeler DS, Goldstein SL. Incorporation of biomarkers with the renal angina index for prediction of severe AKI in critically ill children. Clin J Am Soc Nephrol. 2014;9(4):654–62.
Menon S, Goldstein SL, Mottes T, Fei L, Kaddourah A, Terrell T, et al. Urinary biomarker incorporation into the renal angina index early in intensive care unit admission optimizes acute kidney injury prediction in critically ill children: a prospective cohort study. Nephrol Dial Transplant. 2016;31(4):586–94.
Cruz DN, Ferrer-Nadal A, Piccinni P, Goldstein SL, Chawla LS, Alessandri E, et al. Utilization of small changes in serum creatinine with clinical risk factors to assess the risk of AKI in critically ill adults. Clin J Am Soc Nephrol. 2014;9(4):663–72.
Murphy GJ, Lin H, Coward RJ, Toth T, Holmes R, Hall D, et al. An initial evaluation of post-cardiopulmonary bypass acute kidney injury in swine. Eur J Cardiothorac Surg. 2009;36(5):849–55.
Sellke FW, DiMaio JM, Caplan LR, Ferguson TB, Gardner TJ, Hiratzka LF, et al. Comparing on-pump and off-pump coronary artery bypass grafting: numerous studies but few conclusions: a scientific statement from the American Heart Association council on cardiovascular surgery and anesthesia in collaboration with the interdisciplinary working group on quality of care and outcomes research. Circulation. 2005;111(21):2858–64.
Okusa MD. The inflammatory cascade in acute ischemic renal failure. Nephron. 2002;90(2):133–8.
Haase M, Bellomo R, Haase-Fielitz A. Novel biomarkers, oxidative stress, and the role of labile iron toxicity in cardiopulmonary bypass-associated acute kidney injury. J Am Coll Cardiol. 2010;55(19):2024–33.
Paparella D, Yau TM, Young E. Cardiopulmonary bypass induced inflammation: pathophysiology and treatment. An update. Eur J Cardiothorac Surg. 2002;21(2):232–44.
Westhuyzen J, McGiffin DC, McCarthy J, Fleming SJ. Tubular nephrotoxicity after cardiac surgery utilising cardiopulmonary bypass. Clin Chim Acta. 1994;228(2):123–32.
Yap SC, Lee HT. Acute kidney injury and extrarenal organ dysfunction: new concepts and experimental evidence. Anesthesiology. 2012;116(5):1139–48.
Macedo E, Bouchard J, Soroko SH, Chertow GM, Himmelfarb J, Ikizler TA, et al. Fluid accumulation, recognition and staging of acute kidney injury in critically-ill patients. Crit Care. 2010;14(3):R82.
McCullough PA, Shaw AD, Haase M, Bouchard J, Waikar SS, Siew ED, et al. Diagnosis of acute kidney injury using functional and injury biomarkers: workgroup statements from the tenth acute dialysis quality initiative consensus conference. Contrib Nephrol. 2013;182:13–29.
Kellum JA, Sileanu FE, Murugan R, Lucko N, Shaw AD, Clermont G. Classifying AKI by urine output versus serum creatinine level. J Am Soc Nephrol. 2015;26(9):2231–8.
Sampaio MC, Maximo CA, Montenegro CM, Mota DM, Fernandes TR, Bianco AC, et al. Comparison of diagnostic criteria for acute kidney injury in cardiac surgery. Arq Bras Cardiol. 2013;101(1):18–25.
Langenberg C, Gobe G, Hood S, May CN, Bellomo R. Renal histopathology during experimental septic acute kidney injury and recovery. Crit Care Med. 2014;42(1):e58–67.
Langenberg C, Bagshaw SM, May CN, Bellomo R. The histopathology of septic acute kidney injury: a systematic review. Crit Care. 2008;12(2):R38.
Chen S. Retooling the creatinine clearance equation to estimate kinetic GFR when the plasma creatinine is changing acutely. J Am Soc Nephrol. 2013;24(6):877–88.
Murray PT, Mehta RL, Shaw A, Ronco C, Endre Z, Kellum JA, et al. Potential use of biomarkers in acute kidney injury: report and summary of recommendations from the 10th acute dialysis quality initiative consensus conference. Kidney Int. 2014;85(3):513–21.
Basu RK, Wong HR, Krawczeski CD, Wheeler DS, Manning PB, Chawla LS, et al. Combining functional and tubular damage biomarkers improves diagnostic precision for acute kidney injury after cardiac surgery. J Am Coll Cardiol. 2014;64(25):2753–62.
Varnell CD Jr, Goldstein SL, Devarajan P, Basu RK. Impact of near real-time urine neutrophil gelatinase-associated lipocalin assessment on clinical practice. Kidney Int Rep. 2017;2(6):1243–9.
Chawla LS, Davison DL, Brasha-Mitchell E, Koyner JL, Arthur JM, Shaw AD, et al. Development and standardization of a furosemide stress test to predict the severity of acute kidney injury. Crit Care. 2013;17(5):R207.
Chawla LS. The furosemide stress test to predict renal function after continuous renal replacement therapy. Authors’ response. Crit Care. 2014;18(3):429.
Koyner JL, Davison DL, Brasha-Mitchell E, Chalikonda DM, Arthur JM, Shaw AD, et al. Furosemide stress test and biomarkers for the prediction of AKI severity. J Am Soc Nephrol. 2015;26(8):2023–31.
Koyner JL, Chawla LS. Use of stress tests in evaluating kidney disease. Curr Opin Nephrol Hypertens. 2017;26(1):31–5.
Borasino S, Wall KM, Crawford JH, Hock KM, Cleveland DC, Rahman F, et al. Furosemide response predicts acute kidney injury after cardiac surgery in infants and neonates. Pediatr Crit Care Med. 2018;19(4):310–7.
Kwiatkowski DM, Goldstein SL, Cooper DS, Nelson DP, Morales DL, Krawczeski CD. Peritoneal dialysis vs furosemide for prevention of fluid overload in infants after cardiac surgery: a randomized clinical trial. JAMA Pediatr. 2017;171(4):357–64.
Gist KM, Goldstein SL, Wrona J, Alten JA, Basu RK, Cooper DS, et al. Kinetics of the cell cycle arrest biomarkers (TIMP-2*IGFBP-7) for prediction of acute kidney injury in infants after cardiac surgery. Pediatr Nephrol. 2017;32(9):1611–9.
Meersch M, Schmidt C, Hoffmeier A, Van Aken H, Wempe C, Gerss J, et al. Prevention of cardiac surgery-associated AKI by implementing the KDIGO guidelines in high risk patients identified by biomarkers: the PrevAKI randomized controlled trial. Intensive Care Med. 2017;43(11):1551–61.
Alobaidi R, Morgan C, Basu RK, Stenson E, Featherstone R, Majumdar SR, et al. Association between fluid balance and outcomes in critically ill children: a systematic review and meta-analysis. JAMA Pediatr. 2018;172(3):257–68.
Hassinger AB, Wald EL, Goodman DM. Early postoperative fluid overload precedes acute kidney injury and is associated with higher morbidity in pediatric cardiac surgery patients. Pediatr Crit Care Med. 2014;15(2):131–8.
James MT, Hobson CE, Darmon M, Mohan S, Hudson D, Goldstein SL, et al. Applications for detection of acute kidney injury using electronic medical records and clinical information systems: workgroup statements from the 15(th) ADQI consensus conference. Can J Kidney Health Dis. 2016;3:9.
Song Y, Kim DW, Kwak YL, Kim BS, Joo HM, Ju JW, et al. Urine output during cardiopulmonary bypass predicts acute kidney injury after cardiac surgery: a single-center retrospective analysis. Medicine (Baltimore). 2016;95(22):e3757.
Klein SJ, Brandtner AK, Lehner GF, Ulmer H, Bagshaw SM, Wiedermann CJ, et al. Biomarkers for prediction of renal replacement therapy in acute kidney injury: a systematic review and meta-analysis. Intensive Care Med. 2018;44(3):323–36.
Askenazi D, Ingram D, White S, Cramer M, Borasino S, Coghill C, et al. Smaller circuits for smaller patients: improving renal support therapy with Aquadex. Pediatr Nephrol. 2016;31(5):853–60.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Basu, R.K. (2019). Acute Kidney Injury in Children Following Cardiopulmonary Bypass: A Call for Action. In: Sethi, S., Raina, R., McCulloch, M., Bunchman, T. (eds) Critical Care Pediatric Nephrology and Dialysis: A Practical Handbook. Springer, Singapore. https://doi.org/10.1007/978-981-13-2276-1_19
Download citation
DOI: https://doi.org/10.1007/978-981-13-2276-1_19
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-2275-4
Online ISBN: 978-981-13-2276-1
eBook Packages: MedicineMedicine (R0)