Abstract
Tumor necrosis factor receptor-associated periodic syndrome (TRAPS) is a representative of autoinflammatory diseases. We conducted a nationwide survey for patients with TNFRSF1A variants in Japan. We obtained clinical and genetic features of 51 patients from 33 independent families. The most common variant was T61I (appearing in 49% of patients), and it was identified in 7 of 363 healthy controls. The common clinical features of Japanese patients were fever of >38 °C (100% of patients), arthralgia (59%), and rash (55%). The prevalence of abdominal pain (36%), myalgia (43%), and amyloidosis (0%) was significantly lower in Japanese patients than in Caucasian patients. Patients with TNFRSF1A variants are very rare in Japan, as in other countries, but there are a number of clinical and genetic differences between Japanese and Caucasian patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
11.1 Introduction
Tumor necrosis factor receptor-associated periodic syndrome (TRAPS) is a representative of autoinflammatory diseases. It is a rare disease, and has been reported mainly in Caucasians [1]. However, as reports in Japanese also increased, the Ministry of Health, Labor, and Welfare (MHLW) of Japan organized a study group for TRAPS chaired by Professor Horiuchi of Kyushu University. A nationwide survey revealed that there are at least 33 families of TRAPS in Japan [2]. In this chapter, we first describe the disease concept and pathophysiology of TRAPS. Next, the results of the nationwide survey and characteristics of TRAPS in Japan which the nationwide survey revealed are described. TRAPS has been certified as “Nanbyo” (intractable disease) on January 1, 2015.
11.2 Disease Concept
TRAPS is an autosomal dominant inherited autoinflammatory disease caused by mutations of the TNF receptor super family 1A (TNFRSF1A) gene encoding type 1 TNF receptor (TNFR1). Representative diseases of autoinflammatory diseases involve familial Mediterranean fever (FMF), mevalonate kinase deficiency (MKD), cryopyrin-associated periodic syndrome (CAPS) in addition to TRAPS, each of which is characterized by recurrent inflammatory episodes with fever and various organ involvements. The term autoinflammation was made to denote a group of diseases without the usual features of autoimmunity (high-titer autoantibodies and autoreactive T cells), which were subsequently recognized as disorders of the innate immune system [3]. TRAPS was originally reported as familial perireticular amyloidosis, familial Hibernian fever (FHF), and autosomal dominant familial periodic syndrome. In 1998, genome-wide association study revealed that both disease susceptibility loci of FHF and autosomal dominant familial periodic syndrome are located on chromosome 12p3 [4, 5]. In 1999, mutations in the TNFRSF1A gene were identified and led to the naming of TRAPS [6]. TRAPS is characterized clinically by recurrent inflammatory episodes such as fever, myalgia, joint pain, rash, periorbital edema, conjunctivitis, and serositis. Severe cases complicate amyloidosis. Although it often occurs in childhood, adult onset cases are also seen [1].
11.3 Pathophysiology
TNFR1 is a transmembrane protein consisting of 455 amino acid (Fig. 11.1). The extracellular domain of TNFR1 consists of four cysteine-rich domains (CRD1-4), each of which contains three cysteine–cysteine disulfide bonds [7]. CRD1, also known as the pre-ligand assembly domain (PLAD), mediates self-assembly in the absence of ligand [8]. The ligand binding domains are made up of CRD2 and CRD3. The intracellular region includes a death domain (DD) that can initiate signaling cascades for both inflammation and apoptosis. Soluble TNFR1, corresponding to TNFR1 extracellular domain, is shed by proteolytic cleavage. The major TNFR1 cleavage site is in the spacer region adjacent to the transmembrane domain between Asn-172 and Val-173, with a minor site between Lys-174 and Gly-175 [9]. TNFRSF1A consists of 10 exons. For example, the latter half of exon 2 and the first half of exon 3 encode CRD1. Figure 11.1 shows the location of TNFRSF1A variants. TNFRSF1A variants seen in TRAPS patients are concentrated in exon 2, 3, and 4 encoding CRD1, CRD2, and CRD3. The numbering of the amino acids for TNFRSF1A has not followed the general rule of starting with the translation initiator methionine, as most publications have started numbering after the leading sequence, i.e., leucine at residue 30. Also in this chapter numbering is done as such. The list of variants of the genes responsible for autoinflammatory diseases, including TRAPS, is maintained and updated in the Infevers database (http://fmf.igh.cnrs.fr/infevers).
Schematic representations of TNFR1 protein, TNFRSF1A gene and TNFRSF1A sequence variants. TNFR1 is a transmembrane protein consisting of 455 amino acid. The extracellular domain of TNFR1 consists of four cysteine-rich domains (CRD1–4). The intracellular region includes a death domain (DD). The TNFRSF1A gene consists of 10 exons. The locations of TNFRSF1A variants are shown. The numbering of the amino acids for TNFRSF1A has not followed the general rule of starting with the translation initiator methionine, as most publications have started numbering after the leading sequence, i.e., leucine at residue 30
Currently, the leading hypothesis of pathological mechanisms of TRAPS is the defect of intracellular trafficking of mutated TNFR1 [10, 11]. The TNFRSF1A mutation causes misfolding of the TNFR1 protein structure. The misfolding TNFR1 is not transported to the secretory pathway after the Golgi apparatus by the protein quality control mechanism, resulting in intracellular retention of mutated TNFR1 in the endoplasmic reticulum (ER). Because of autophagic abnormality, mutated TNFR1 is not degraded, and accumulates in the ER [12]. Accumulation of mutated TNFR1 enhances the production of reactive oxygen species (ROS) from mitochondria. Mitochondrial ROS activates mitogen-activated protein kinase (MAPK) through suppression of MAPK dephosphorylation [13]. Accumulation of mutated TNFR1 causes ER stress response and increases expression of ER stress-related proteins such as Spliced X-box binding protein 1 (sXBP1). sXBP1 enhances inflammatory cytokine production induced by Toll-like receptor (TLR) stimulation in ROS dependence [14]. By these mechanisms, inflammatory cytokine production such as TNF-α, IL-6, and pro-IL-1β is induced against a small amount of lipopolysaccharide (LPS) stimulation that normally does not react.
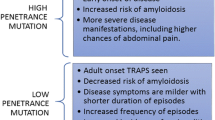
The TNFRSF1A mutations causing functional abnormalities such as intracellular trafficking defect in TNFR1 are referred to as “structural mutations” [11]. Representatives of “structural mutations” are mutations of cysteine residues that form disulfide bonds and the T50M mutation which is a mutation of threonine residue that form hydrogen bonds that are presumed to have a major influence on the structure of TNFR1. TNFRSF1A mutations such as defects in cysteine residues and the T50M mutation have not been found in patients other than TRAPS patients and asymptomatic patient relatives, whereas the R92Q and P46L variants are found in allele frequencies of about 1% in the Caucasian general population. The R92Q and P46L variants are associated with low penetrance and a mild TRAPS phenotype. A few patients with R92Q and P46L develop amyloidosis [15]. Functional abnormalities such as intracellular trafficking defect are not observed in the R92Q and P46L TNFR1. The R92Q and P46L variants are referred to as “nonstructural” [11].
It is a matter of debate whether the P46L and R92Q variants really have a pathogenic effect. In West African individuals without TRAPS-like symptoms, the allele frequency of the P46L variant is as high as 9.8% [16]. The allele frequency of the R92Q variant in children with periodic fever (2.45%) did not differ significantly from the allele frequency in healthy subjects (2.25%) in Italy [17]. It has been suggested that the R92Q variant might be a susceptibility factor in other inflammatory diseases. The frequency of the R92Q variant tended to be higher in patients with early arthritis, but this finding is a subject of controversy [18, 19]. The R92Q variant was also significantly more frequent in patients with Behçet’s disease, atherosclerosis, and idiopathic recurrent endocarditis than in healthy controls [20,21,22]. Genome-wide association studies identified the R92Q variant as a genetic risk factor for multiple sclerosis [23].
11.4 Diagnosis
TRAPS is diagnosed by genetic testing. Hull and colleagues have proposed “Diagnostic indicators of TRAPS” composed of items including symptoms and family history [1]. It should be noted that this is not a diagnostic criteria but a guideline for judging the indication of genetic testing. It is difficult to diagnose TRAPS only by clinical findings. Clinical findings such as age of onset, clinical symptoms, frequency and duration of inflammatory attack, severity of disease, and therapeutic response vary considerably among patients [24]. There is a possibility of TRAPS even in cases where symptoms such as myalgia and abdominal pain are main symptoms and fever is not observed or patients in whom disease course is continuous rather than periodic (recurrent). Atypical case was reported who was completely asymptomatic until the development of amyloidosis [25]. Additionally, the TNFRSF1A variants are often not identified in patients who are clinically consistent as TRAPS. It was reported that TNFRSF1A variants were identified in 10 families among 18 families in which multiple members had symptoms compatible with TRAPS and only 4 of 176 subjects with sporadic TRAPS-like symptoms [26]. In patients with recurrent inflammatory episodes, if etiologies such as infections, neoplasms, and other rheumatic conditions are unlikely, genetic testing of TNFRSF1A should be considered.
11.5 Treatment
If inflammatory attack is mild and infrequent, you can treat only symptomatic relief with NSAIDs alone. Colchicine and immunosuppressive agents such as methotrexate and cyclosporin are considered ineffective [1].
The most common therapeutic agents are corticosteroids. After terminating the attack using high dose corticosteroids, you should promptly taper and discontinue corticosteroids. In some cases, it is difficult to taper and discontinue corticosteroids because the required amount increases during the course or severe attacks occur frequently. Corticosteroid complications such as osteoporosis are a major problem in cases requiring high doses and long-term corticosteroid administration. For such cases the use of biological agents should be considered [27, 28].
Currently, IL-1 inhibition is a first-line biological agent. A phase-II clinical study demonstrated clear efficacy for canakinumab, leading to US Food and Drug Administration (FDA) approval of the drug for the treatment of TRAPS [29]. Also in Japan, canakinumab received approval for the treatment of TRAPS in December 2016.
Etanercept, one of TNF inhibitors, can be effective in some patients. However, the response is partial and loss of efficacy occurs in most cases [30]. The use of infliximab and adalimumab, which are TNF inhibitors, are associated with exacerbation of TRAPS and should be avoided [31,32,33]. Etanercept is a type 2 TNF receptor-Fc fusion protein, while infliximab and adalimumab are a monoclonal antibody. This structural difference may cause a difference in clinical effect.
11.6 Epidemiological Findings of TRAPS Before Our National Survey
From Germany, an epidemiological national survey of pediatric patients was reported in 2009 [34]. Monthly inquiries were sent to 370 children’s hospitals and pediatric rheumatological outpatient clinics and to all 23 laboratories performing genetic analyses for Hereditary periodic fever. In July 2003 to June 2006, they found 23 new patients. The incidence of TRAPS in German children was estimated to be ~5.6 per 107 person-years, and it was concluded that TRAPS is a rare disease in Caucasians. 19 (83%) of 23 cases had the R92Q variant, which is a variant of uncertain pathogenic significance. If we consider only TNFRSF1A mutations with clearly pathogenic significance, the incidence is even lower.
Case series of 158 patients was reported in 2013 from the Eurofever/ EUROTRAPS international registry, which is a web-based registry collected retrospective data on patients with TNFRSF1A sequence variants and inflammatory symptoms [24]. The median age at which symptoms began was 4.3 years but 9.1% of patients presented after 30 years of age. The most common TNFRSF1A variant was R92Q (34% of cases), followed by T50M (10%). Defect of cysteine residues were found in 27% of cases. A family history was present in 19% of patients with R92Q and 64% of those with other variants.
The first confirmed case of TRAPS in Japan was a female patient with the C70S mutation and was reported in 2003 [35]. She was also the first case in an eastern Asian population. Before our national survey, the number of Japanese patient with genetically confirmed TRAPS were 18 patients from 9 independent families [36]. A national survey for FMF was conducted twice in 2006 and 2009 and this revealed that a significant number of patients with FMF exist in Japan and Japanese FMF patients were clinically or genetically different from Mediterranean patients [37, 38]. With these backgrounds, our national survey was conducted.
11.7 Primary Survey
The MHLW study group for TRAPS conducted a national survey. In 2010, we mailed a questionnaire to all 1718 internal medicine departments and 1182 pediatric departments in hospitals with more than 200 beds, asking whether they had patients in whom TRAPS was suspected from January to December 2009. Contacting hospitals with more than 200 beds was determined to be enough to find patients with undiagnosed TRAPS, because it was presumed that patients with undiagnosed TRAPS are referred to large hospitals as patients with recurrent fever of unknown cause. The criteria for TRAPS were not set and were left up to each doctor’s judgment in order to widely screen patients in whom TRAPS was suspected. However, to assist physicians with finding TRAPS patients, we advised recruiting into the study patients who either (1) fulfilled Hull’s classification criteria for TRAPS [1] or (2) presented atypical symptoms of juvenile idiopathic arthritis (JIA) or adult-onset Still’s disease (AOSD). “Atypical disease” was defined as disease without chronic arthritis or with recurrent inflammatory attacks. It is noteworthy that a number of TRAPS patients were misdiagnosed as having atypical systemic JIA [39]. A total of 826 of 1718 internal medicine departments (48.1%) and 981 of 1182 pediatrics departments (83.0%) responded to our questionnaire (Table 11.1). There were 263 patients in whom TRAPS was clinically suspected. The number of patients in whom TRAPS was clinically suspected nationwide was estimated in units of institutions, assuming that there was a random response regardless of the number of patients. That is, we weighted by the reciprocal of the response rate and estimated the total number of patients by Stata version 11 (Stata Coop., Texas USA). As a result, it was estimated that there were 423 patients in whom TRAPS was clinically suspected nationwide.
11.8 Secondary Survey
We then asked the departments that replied that they had patients in whom TRAPS was clinically suspected to provide detailed clinical information and a blood sample for genetic testing. A total of 169 patients underwent genetic analysis in our study. Genetic testing of a total of 359 healthy controls was also conducted. All individuals were Japanese. The study was approved by the ethics committee of Kyushu University. Written informed consent was obtained from each enrolled patient. Screening for mutations of all the coding exons of the TNFRSF1A (exons 1–10), MEFV (exons 1–10), and MVK (exons 2–11) genes was performed by direct sequencing. TNFRSF1A variants were identified in 10 patients from 10 independent families. The T61I variant was found in 8 patients, while the V136M and S321I variants were found in 1 patient each. All the patients were heterozygous for the variants. Among the healthy controls, 7 of 363 individuals were heterozygous for the T61I variant. There was no significant difference in the allele frequency of the T61I variant between the patient group and the control group; however, there was a trend toward an increased frequency of the T61I variant in the patient group (p = 0.071). TNFRSF1A variants other than the T61I variant were not identified in healthy individuals. The R92Q and P46L variants, which are associated with low penetrance and a mild TRAPS phenotype and are present in about 1% of the Caucasian general population, were not observed in our patients or controls.
Although MEFV variants/polymorphisms were found in many patients and healthy individuals, mutations in exon 10, which are considered most pathogenic, were found in only 2 of the 159 patients without any TNFRSF1A variants. One patient was heterozygous for the Y688C MEFV mutation, but the patient was clinically diagnosed as having AOSD. The other was heterozygous for the M694I MEFV mutation and satisfied the Tel Hashomer criteria for FMF [40]. Therefore, this patient was diagnosed as having FMF. Heterozygous V109 L and D386N MVK variants were found in 1 patient each. One healthy individual was carrying the V109L variant. The 2 patients with these MVK variants were not carrying any TNFRSF1A variants. As MKD is an autosomal-recessive inherited disease, the MVK mutation needs to be homozygous to cause the disease. Therefore, the pathogenic role of these 2 variants is not clear.
In this study, we found 10 patients with TNFRSF1A variants, from 10 independent families. In addition, we collected information on 17 patients from 13 independent families with TNFRSF1A variants and symptoms of inflammation who had not been described in the literature. A total of 27 patients from 23 families were shown in Table 11.2. The C15Y, V125 M, V136 M, and S321I variants were novel variants found in this study. A literature search revealed that 24 additional cases from 11 families with TNFRSF1A variants and symptoms of inflammation had been reported from Japan [35, 39, 41,42,43,44,45,46,47,48]. In total, clinical and genetic features of 51 patients from 33 independent families were obtained (Table 11.3
).
11.9 Genetic Features of Patients with TNFRSF1A Variant in Japan
Defects in cysteine residues and the T50M variant referred to as “structural mutations” were found in 33% of the 51 patients with TNFRSF1A variant. T61I was the most common variant, found in 19 families, followed by the C30Y and T50M variants in two families each. The sporadic cases included 14 patients with the T61I variant and 1 patient each with the C15Y, N101K, V136M, and S321I variants. Among the sporadic cases, the parents of five patients with the T61I variant and the parents of 1 patient each with the C15Y and S321I variants underwent genetic analysis. Both parents of 1 patient with the T61I variant was found to carry the variant, and 1 parent each of the other 6 patients carried the variant. De novo mutations were not found. The C15Y, N25D, T61I, C70S, N101K, V125M, V136M, and S321I variants were reported exclusively in Japan.
11.10 Clinical Features of Patients with TNFRSF1A Variant in Japan
The main clinical findings in Japanese patients with TNFRSF1A variants are a fever of 38 °C (100% of patients), abdominal pain (36%), myalgia (43%), skin rash (55%), conjunctivitis (18%), periorbital edema (9%), chest pain (14%), arthralgia (59%), and headache (23%). No patient had amyloidosis. None of the Japanese patients underwent any abdominal operation because of misdiagnosis. When we classified the C15Y, T50M, and C70S variants as “structural mutations,” N25D, T61I, N101K, V125M, V136M, and S321I variants as other mutations, there was no significant difference in clinical manifestations between patients carrying “structural mutations” and others, except for family history and age at onset. A positive family history of recurrent inflammatory episodes of unknown cause and a disease onset at age <20 years were significantly more frequent in patients carrying “structural mutations” than others (94.1% vs. 29.2% and 87.5% vs. 58.1%, each).
We compared clinical characteristics between patients in Japan and those registered in the Eurofever/EUROTRAPS international registry, the largest cohort of patients carrying TNFRSF1A, with patients from six European countries participating [24]. All of the patients in Japan showed a fever of 38 °C, which was significantly more prevalent than the case in Europe (100% vs. 84%). In contrast, a number of clinical symptoms were significantly less frequent in Japanese patients, including abdominal pain (36% vs. 70%), myalgia (43% vs. 70%), and amyloidosis (0% vs. 10%). Clinical symptoms may be milder in Japanese patients than in Caucasian patients. Interestingly, a national survey of FMF in Japan revealed that Japanese FMF patients had a lower prevalence of abdominal pain and amyloidosis than Mediterranean FMF patients [38]. The low prevalence of abdominal pain and amyloidosis in autoinflammatory diseases may be an ethnic characteristic of Japanese.
11.11 The Pathogenic Significance of the TNFRSF1A Variants in Japan
Although the most prominent genetic characteristic in Japanese patients with TNFRSF1A variants is the presence of the T61I variant, the most common variant in Japanese patients, the pathogenic significance of this variant remains unclear. In our 16 patients carrying the T61I variant, two patients had the M694I mutations of MEFV. Their inflammatory symptoms were explained with the M694I mutations of MEFV. We considered the possibility that patients carrying the T61I variant had other autoinflammatory disease-related gene mutations. We conducted genetic analysis of NLRP3, NOD2, PSTPIP1, PLCG2, NLRP12, IL1RN, NLRC4, and PSMB8 in addition to TNFRSF1A, MEFV, and MVK. These additional eight genes are supposed to cover almost all of the genes responsible for autoinflammatory diseases [49,50,51,52,53]. In our 16 patients carrying the T61I variant (patients 4–19 in Table 11.2), we identified some additional variants. All variants except 1 were supposed to be common variants according to the Exome Aggregation Consortium database (http://exac.broadinstitute.org). Only patient 11 was carrying a rare NLRC4 variant, L70F. Although NLRC4 mutations that have been reported to cause autoinflammation are located in the nucleotide-binding oligomerization domain coding region, L70F is located in the caspase recruitment domain coding region [50,51,52]. Therefore, the pathogenic role of L70F is not clear. In our 16 patients carrying the T61I variant, except for two patients having the M694I mutations of MEFV, we identified no other pathogenic variants in a total of 11 autoinflammatory disease-related genes, which might support a possible pathogenic role of the T61I variant.
Two-thirds of the patients carrying the T61I variant had sporadic illness. There was no significant difference in the allele frequency of the T61I variant between patients and controls; however, there was a trend toward an increased frequency of the T61I variant in patients (p = 0.071). Considering that the sister of patient 6 was homozygous for the T61I variant but was asymptomatic (Table 11.2), it may be certain that the T61I variant does not have a potent pathogenic effect seen with “structural mutations.” It is interesting that two patients having a combination of heterozygous T61I and heterozygous M694I mutations of MEFV had inflammatory episodes for up to 14 days, which is long compared to the typical FMF course, which terminates within 3 days. It is possible that the T61I variant influences the phenotype of the M694I mutation.
A small number of patients and none of healthy controls had the C15Y, N25D, N101K, V125M, V136M, and S321I variants. Therefore, their pathogenic significance could not be deduced from the penetrance level. We thought that it would be useful to examine the cell surface and intracellular expression of variant TNFRI proteins to assess their contribution to disease. We examined the effect on TNFRI trafficking of variants by using the same experimental procedures as those described previously [10]. We transfected expression vectors encoding wild-type or variant TNFRI into human embryonic 293T cells. We assessed the cell surface expression of receptors by using FACS analysis. Consistent with a previous observation, cells transfected with C33Y or T50M TNFRI showed less cell surface expression than cells transfected with wild-type or R92Q TNFRI. Cells transfected with the C15Y variant showed decreased cell surface expression, in the same manner as the C33Y and T50M variants. In contrast, cells transfected with N25D, T61I, N101K, V125M, V136M, and S321I receptors showed cell surface expression at levels as high as those in cells with the wild-type or R92Q receptor. This result suggests that the C15Y variant has the same pathogenic significance as the other “structural mutations.” In contrast, the N25D, T61I, N101K, V125M, V136M, and S321I variants should be distinguished from “structural mutations.”
11.12 Diagnostic Indicators of Japanese TRAPS
Because the rate of mutation detection is low (<20%) among patients having symptoms consistent with autoinflammatory diseases, A diagnostic score to predict the probability of a positive genetic test result for any of the TNFRSF1A, MEFV, and MVK genes has been proposed by Gattorno et al. [54]. Most of the patients in that study were children age < 18 years and of Italian origin, which is a different population from that of our patients. In addition, abdominal pain, which was less frequent in Japanese patients with TNFRSF1A variants, was included in the calculation as an important predicting factor. We therefore considered that this scoring system was not applicable to our patients.
In order to identify sensitive and specific markers for detecting TNFRSF1A mutations in our Japanese patients, the clinical features of the patients carrying TNFRSF1A “structural mutations” (n = 17) and those without any TNFRSF1A mutations/variants (n = 146) were compared to elucidate variables for obtaining positive results by genetic analysis of TNFRSF1A. Using univariate analyses, we identified a positive family history of recurrent inflammatory episodes of unknown cause and a disease onset at age <20 years as clinical parameters predicting positive results of genetic analysis. Multivariate logistic regression analysis showed that only a positive family history of recurrent inflammatory episodes was strongly associated with the possibility of obtaining a positive result for “structural mutation” of the TNFRSF1A gene. There were no significant differences in symptoms such as fever, abdominal pain, myalgia, and skin rash. In our Japanese cohort, when the patient had a family history of recurrent inflammatory episodes, the sensitivity was 94.1% and the specificity was 89.7% for the probability of carrying TNFRSF1A “structural mutations.” Further validation of this finding is needed with another patient cohort.
On the basis of these results, TRAPS diagnostic criteria, which are conditions for certification of designated intractable diseases “Nanbyo” and chronic specific diseases for children, were created. By satisfying this, patients can receive public medical expense subsidies. Repeated symptoms of inflammation more than 6 months are essential conditions and genetic testing is recommended when satisfying supplementary items such as family history. The final diagnosis is by genetic testing. Interpretation of genetic test results requires consultation with experts.
Conclusion
We conducted a nationwide survey for TRAPS for the first time in Japan or Asia overall. The incidence of patients with TNFRSF1A variants in Japan was rare, as in other European countries, but a number of clinical and genetic features of Japanese patients were different from those of Caucasian patients.
Many of the TNFRSF1A variants identified in Japan, including the T61I variant, have an uncertain pathogenic significance. It is considered essential for the understanding of Japanese TRAPS to clarify the pathogenic significance of these variants.
References
Hull KM, Drewe E, Aksentijevich I, Singh HK, Wong K, Mcdermott EM, et al. The TNF receptor-associated periodic syndrome (TRAPS). Medicine. 2002;81:349–68. https://doi.org/10.1097/00005792-200209000-00002.
Ueda N, Ida H, Washio M, Miyahara H, Tokunaga S, Tanaka F, et al. Clinical and genetic features of patients with TNFRSF1A variants in Japan: findings of a Nationwide survey. Arthritis & Rheumatology. 2016;68:2760–71. https://doi.org/10.1002/art.39793.
Masters SL, Simon A, Aksentijevich I, Kastner DL. Horror Autoinflammaticus: the molecular pathophysiology of autoinflammatory disease. Annu Rev Immunol. 2009;27:621–68. https://doi.org/10.1146/annurev.immunol.25.022106.141627.
Mulley J, Saar K, Hewitt G, Rüschendorf F, Phillips H, Colley A, et al. Gene localization for an autosomal dominant familial periodic fever to 12p13. Am J Hum Genet. 1998;62:884–9. https://doi.org/10.1086/301793.
Mcdermott MF, Ogunkolade BW, Mcdermott EM, Jones LC, Wan Y, Quane KA, et al. Linkage of familial Hibernian fever to chromosome 12p13. Am J Hum Genet. 1998;62:1446–51. https://doi.org/10.1086/301886.
Mcdermott MF, Aksentijevich I, Galon J, Mcdermott EM, Ogunkolade B, Centola M, et al. Germline mutations in the extracellular domains of the 55 kDa TNF receptor, TNFR1, define a family of dominantly inherited autoinflammatory syndromes. Cell. 1999;97:133–44. https://doi.org/10.1016/s0092-8674(00)80721-7.
Banner DW, D'Arcy A, Janes W, Gentz R, Schoenfeld HJ, Broger C, et al. Crystal structure of the soluble human 55 kd TNF receptor-human TNF beta complex: implications for TNF receptor activation. Cell. 1993;73:431–45. https://doi.org/10.2210/pdb1tnr/pdb.
Chan FK, Chun HJ, Zheng L, Siegel RM, Bui KL, Lenardo MJ. A domain in TNF receptors that mediates ligand-independent receptor assembly and signaling. Science. 2000;288:2351–4. https://doi.org/10.1126/science.288.5475.2351.
Hawari FI, Rouhani FN, Cui X, Yu Z-X, Buckley C, Kaler M, et al. Release of full-length 55-kDa TNF receptor 1 in exosome-like vesicles: a mechanism for generation of soluble cytokine receptors. Proc Natl Acad Sci. 2004;101:1297–302. https://doi.org/10.1073/pnas.0307981100.
Lobito AA, Kimberley FC, Muppidi JR, Komarow H, Jackson AJ, Hull KM, et al. Abnormal disulfide-linked oligomerization results in ER retention and altered signaling by TNFR1 mutants in TNFR1-associated periodic fever syndrome (TRAPS). Blood. 2006;108:1320–7. https://doi.org/10.1182/blood-2005-11-006783.
Simon A, Park H, Maddipati R, Lobito AA, Bulua AC, Jackson AJ, et al. Concerted action of wild-type and mutant TNF receptors enhances inflammation in TNF receptor 1-associated periodic fever syndrome. Proc Natl Acad Sci. 2010;107:9801–6. https://doi.org/10.1073/pnas.0914118107.
Bachetti T, Chiesa S, Castagnola P, Bani D, Zanni ED, Omenetti A, et al. Autophagy contributes to inflammation in patients with TNFR-associated periodic syndrome (TRAPS). Ann Rheum Dis. 2012;72:1044–52. https://doi.org/10.1136/annrheumdis-2012-201952.
Bulua AC, Simon A, Maddipati R, Pelletier M, Park H, Kim KY, et al. Mitochondrial reactive oxygen species promote production of proinflammatory cytokines and are elevated in TNFR1-associated periodic syndrome (TRAPS). J Exp Med. 2011;208:519–33. https://doi.org/10.1084/jem.20102049.
Dickie LJ, Aziz AM, Savic S, Lucherini OM, Cantarini L, Geiler J, et al. Involvement of X-box binding protein 1 and reactive oxygen species pathways in the pathogenesis of tumour necrosis factor receptor-associated periodic syndrome. Ann Rheum Dis. 2012;71:2035–43. https://doi.org/10.1136/annrheumdis-2011-201197.
Ravet N, Rouaghe S, Dode C, Bienvenu J, Stirnemann J, Levy P, et al. Clinical significance of P46L and R92Q substitutions in the tumour necrosis factor superfamily 1A gene. Ann Rheum Dis. 2006;65:1158–62. https://doi.org/10.1136/ard.2005.048611.
Tchernitchko D, Chiminqgi M, Galactéros F, Préhu C, Segbena Y, Coulibaly H, et al. Unexpected high frequency of P46L TNFRSF1A allele in sub-Saharan west African populations. Eur J Hum Genet. 2004;13:513–5. https://doi.org/10.1038/sj.ejhg.5201344.
Dosualdo A, Ferlito F, Prigione I, Obici L, Meini A, Zulian F, et al. Neutrophils from patients withTNFRSF1A mutations display resistance to tumor necrosis factor–induced apoptosis: Pathogenetic and clinical implications. Arthritis Rheum. 2006;54:998–1008. https://doi.org/10.1002/art.21657.
Aksentijevich I, Galon J, Soares M, Mansfield E, Hull K, Oh HH, et al. The tumor-necrosis-factor receptor-associated periodic syndrome: new mutations in TNFRSF1A, ancestral origins, genotype-phenotype studies, and evidence for further genetic heterogeneity of periodic fevers. Am J Hum Genet. 2001;69:301–14. https://doi.org/10.1086/321976.
Dieude P, Goossens M, Cornelis F, Michou L, Bardin T, Tchernitchko DO. The TNFRSF1A R92Q mutation is frequent in rheumatoid arthritis but shows no evidence for association or linkage with the disease. Ann Rheum Dis. 2007;66:1113–5. https://doi.org/10.1136/ard.2006.060764.
Amoura Z, Dodé C, Hue S, Caillat-Zucman S, Bahram S, Delpech M, et al. Association of the R92QTNFRSF1Amutation and extracranial deep vein thrombosis in patients with Behçets disease. Arthritis Rheum. 2005;52:608–11. https://doi.org/10.1002/art.20873.
Poirier O, Nicaud V, Gariépy J, Courbon D, Elbaz A, Morrison C, et al. Polymorphism R92Q of the tumour necrosis factor receptor 1 gene is associated with myocardial infarction and carotid intima-media thickness – the ECTIM, AXA, EVA and GENIC studies. Eur J Hum Genet. 2003;12:213–9. https://doi.org/10.1038/sj.ejhg.5201143.
Cantarini L, Lucherini OM, Brucato A, Barone L, Cumetti D, Iacoponi F, et al. Clues to detect tumor necrosis factor receptor-associated periodic syndrome (TRAPS) among patients with idiopathic recurrent acute pericarditis: results of a multicentre study. Clin Res Cardiol. 2012;101:525–31. https://doi.org/10.1007/s00392-012-0422-8.
Jager PLD, Jia X, Wang J, Bakker PIWD, Ottoboni L, Aggarwal NT, et al. Meta-analysis of genome scans and replication identify CD6, IRF8 and TNFRSF1A as new multiple sclerosis susceptibility loci. Nat Genet. 2009;41:776–82. https://doi.org/10.1038/ng.401.
Lachmann HJ, Papa R, Gerhold K, Obici L, Touitou I, Cantarini L, et al. The phenotype of TNF receptor-associated autoinflammatory syndrome (TRAPS) at presentation: a series of 158 cases from the Eurofever/EUROTRAPS international registry. Ann Rheum Dis. 2013;73:2160–7. https://doi.org/10.1136/annrheumdis-2013-204184.
Kallinich T. "periodic fever" without fever: two cases of non-febrile TRAPS with mutations in the TNFRSF1A gene presenting with episodes of inflammation or monosymptomatic amyloidosis. Ann Rheum Dis. 2005;65:958–60. https://doi.org/10.1136/ard.2005.043570.
Aganna E, Hammond L, Hawkins PN, Aldea A, McKee SA, van Amstel HK, et al. Heterogeneity among patients with tumor necrosis factor receptor-associated periodic syndrome phenotypes. Arthritis Rheum. 2003;48:2632–44. https://doi.org/10.1002/art.11215.
Kusuhara K, Hoshina T, Saito M, Ishimura M, Inoue H, Horiuchi T, et al. Successful treatment of a patient with tumor necrosis factor receptor-associated periodic syndrome using a half-dose of etanercept. Pediatr Int. 2012;54:552–5. https://doi.org/10.1111/j.1442-200x.2011.03525.x.
ter Haar NM, Oswald M, Jeyaratnam J, Anton J, Barron KS, Brogan PA, et al. Recommendations for the management of autoinflammatory diseases. Ann Rheum Dis. 2015;74:1636–44. https://doi.org/10.1136/annrheumdis-2015-207546.
Gattorno M, Obici L, Cattalini M, Tormey V, Abrams K, Davis N, et al. Canakinumab treatment for patients with active recurrent or chronic TNF receptor-associated periodic syndrome (TRAPS): an open-label, phase II study. Ann Rheum Dis. 2016;76:173–8. https://doi.org/10.1136/annrheumdis-2015-209031.
Bulua AC, Mogul DB, Aksentijevich I, Singh H, He DY, Muenz LR, et al. Efficacy of etanercept in the tumor necrosis factor receptor-associated periodic syndrome: a prospective, open-label, dose-escalation study. Arthritis Rheum. 2012;64:908–13. https://doi.org/10.1002/art.33416.
Jacobelli S, Andre M, Alexandra J-F, Dode C, Papo T. Failure of anti-TNF therapy in TNF receptor 1-associated periodic syndrome (TRAPS). Rheumatology. 2007;46:1211–2. https://doi.org/10.1093/rheumatology/kel298.
Drewe E, Powell R, Mcdermott E. Comment on: failure of anti-TNF therapy in TNF receptor 1-associated periodic syndrome (TRAPS). Rheumatology. 2007;46:1865–6. https://doi.org/10.1093/rheumatology/kem231.
Siebert S, Amos N, Lawson TM. Comment on: failure of anti-TNF therapy in TNF receptor 1-associated periodic syndrome (TRAPS). Rheumatology. 2007;47:228–9. https://doi.org/10.1093/rheumatology/kem243.
Lainka E, Neudorf U, Lohse P, Timmann C, Stojanov S, Huss K, et al. Incidence of TNFRSF1A mutations in German children: epidemiological, clinical and genetic characteristics. Rheumatology. 2009;48:987–91. https://doi.org/10.1093/rheumatology/kep140.
Kusuhara K, Nomura A, Nakao F, Hara T. Tumour necrosis factor receptor-associated periodic syndrome with a novel mutation in the TNFRSF1A gene in a Japanese family. Eur J Pediatr. 2004;163:30–2. https://doi.org/10.1007/s00431-003-1338-0.
Washio M, Nakano T, Kawaguchi Y, Takagi K, Kiyohara C, Tsukamoto H, et al. Tumor necrosis factor receptor-associated periodic syndrome (TRAPS) in Japan: a review of the literature. Mod Rheumatol. 2013;23:210–7. https://doi.org/10.3109/s10165-012-0737-3.
Tsuchiya-Suzuki A, Yazaki M, Nakamura A, Yamazaki K, Agematsu K, Matsuda M, et al. Clinical and genetic features of familial Mediterranean fever in Japan. J Rheumatol. 2009;36:1671–6. https://doi.org/10.3899/jrheum.081278.
Migita K, Uehara R, Nakamura Y, Yasunami M, Tsuchiya-Suzuki A, Yazaki M, et al. Familial Mediterranean fever in Japan. Medicine (Baltimore). 2012;91:337–43. https://doi.org/10.1097/MD.0b013e318277cf75.
Manki A, Nishikomori R, Nakata-Hizume M, Kunitomi T, Takei S, Urakami T, et al. Tumor necrosis factor receptor-associated periodic syndrome mimicking systemic juvenile idiopathic arthritis. Allergol Int. 2006;55:337–41. https://doi.org/10.2332/allergolint.55.337.
Livneh A, Langevitz P, Zemer D, Zaks N, Kees S, Lidar T, et al. Criteria for the diagnosis of familial mediterranean fever. Arthritis Rheum. 1997;40:1879–85. https://doi.org/10.1002/art.1780401023.
Ida H. A novel mutation (T61I) in the gene encoding tumour necrosis factor receptor superfamily 1A (TNFRSF1A) in a Japanese patient with tumour necrosis factor receptor-associated periodic syndrome (TRAPS) associated with systemic lupus erythematosus. Rheumatology. 2004;43:1292–9. https://doi.org/10.1093/rheumatology/keh320.
Horiuchi T, Tsukamoto H, Mitoma H, Miyagawa H, Tamimoto Y, Yoshizawa S, et al. Novel mutations in TNFRSF1A in patients with typical tumor necrosis factor receptor-associated periodic syndrome and with systemic lupus erythematosus in Japanese. Int J Mol Med. 2004. https://doi.org/10.3892/ijmm.14.5.813.
Ohmori S, Hino R, Nakamura M, Tokura Y. Heparin serves as a natural stimulant of the inflammasome and exacerbates the symptoms of tumor necrosis factor receptor-associated periodic syndrome (TRAPS). J Dermatol Sci. 2012;66:82–4. https://doi.org/10.1016/j.jdermsci.2011.11.006.
Ohmori S, Hino R, Nakamura M. Inflammatory response to heparinoid and heparin in a patient with tumor necrosis factor receptor-associated periodic syndrome: the second case with a T61I mutation in theTNFRSF1Agene. J Dermatol. 2014;41:1112–3. https://doi.org/10.1111/1346-8138.12689.
Takagi K, Kawaguchi Y, Fujikawa S, Otani T, Sugiura T, Hara M. Tumor necrosis factor receptor-associated periodic syndrome with a C30R mutation in a Japanese family. Mod Rheumatol. 2007;17:265–6. https://doi.org/10.1007/s10165-007-0580-0.
Kai M, Tamaki S, Nishikomori R, Takaoka Y, Ohara O, Oshima K. A case of TNF receptor-associated periodic syndrome. Ryumachika (Rheumatology). 2011;45:456–460. In Japanese.
Nakamura M. Tokura Y. A novel missense mutation in tumour necrosis factor receptor superfamily 1A (TNFRSF1A) gene found in tumour necrosis factor receptor-associated periodic syndrome (TRAPS) with high serum interleukin (IL)-22. Eur J Dermatol. 2010;20:508–9. https://doi.org/10.1684/ejd.2010.0951.
Nakamura M, Kobayashi M, Tokura Y. A novel missense mutation in tumour necrosis factor receptor superfamily 1A (TNFRSF1A) gene found in tumour necrosis factor receptor-associated periodic syndrome (TRAPS) manifesting adult-onset still disease-like skin eruptions: report of a case and review of the Japanese patients. Br J Dermatol. 2009;161:968–70. https://doi.org/10.1111/j.1365-2133.2009.09409.x.
Zhou Q, Lee GS, Brady J, Datta S, Katan M, Sheikh A, et al. A hypermorphic missense mutation in PLCG2, encoding phospholipase Cγ2, causes a dominantly inherited autoinflammatory disease with immunodeficiency. Am J Hum Genet. 2012;91:713–20. https://doi.org/10.1016/j.ajhg.2012.08.006.
Romberg N, Moussawi KA, Nelson-Williams C, Stiegler AL, Loring E, Choi M, et al. Mutation of NLRC4 causes a syndrome of enterocolitis and autoinflammation. Nat Genet. 2014;46:1135–9. https://doi.org/10.1038/ng.3066.
Canna SW, Jesus AAD, Gouni S, Brooks SR, Marrero B, Liu Y, et al. An activating NLRC4 inflammasome mutation causes autoinflammation with recurrent macrophage activation syndrome. Nat Genet. 2014;46:1140–6. https://doi.org/10.1038/ng.3089.
Kitamura A, Sasaki Y, Abe T, Kano H, Yasutomo K. An inherited mutation inNLRC4causes autoinflammation in human and mice. J Exp Med. 2014;211:2385–96. https://doi.org/10.1084/jem.20141091.
Arima K, Kinoshita A, Mishima H, Kanazawa N, Kaneko T, Mizushima T, et al. Proteasome assembly defect due to a proteasome subunit beta type 8 (PSMB8) mutation causes the autoinflammatory disorder, Nakajo-Nishimura syndrome. Proc Natl Acad Sci. 2011;108:14914–9. https://doi.org/10.1073/pnas.1106015108.
Gattorno M, Sormani MP, Dosualdo A, Pelagatti MA, Caroli F, Federici S, et al. A diagnostic score for molecular analysis of hereditary autoinflammatory syndromes with periodic fever in children. Arthritis Rheum. 2008;58:1823–32. https://doi.org/10.1002/art.23474.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Ueda, N., Horiuchi, T. (2019). Epidemiological Studies of Specified Rare and Intractable Disease. In: Washio, M., Kobashi, G. (eds) Epidemiological Studies of Specified Rare and Intractable Disease. Current Topics in Environmental Health and Preventive Medicine. Springer, Singapore. https://doi.org/10.1007/978-981-13-1096-6_11
Download citation
DOI: https://doi.org/10.1007/978-981-13-1096-6_11
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-1095-9
Online ISBN: 978-981-13-1096-6
eBook Packages: MedicineMedicine (R0)