Abstract
Low-dose rate (LDR) prostate brachytherapy is a highly efficacious and cost-effective treatment with a very favorable side effect profile and has a role in the treatment paradigm of low-, intermediate-, and high-risk prostate cancers. Brachytherapy is typically an outpatient procedure where tiny radioactive “seeds” are implanted in the prostate to eradicate the cancer right where it has grown. Brachytherapy has a long and proven track record with data demonstrating it to be extremely effective when used alone in low and favorable intermediate-risk prostate cancer. Brachytherapy also shows significantly higher rates of cancer control and tumor eradication in the higher-risk setting when used in combination with external beam radiation therapy (EBRT) as compared to surgery or EBRT alone.
Despite its efficacy, brachytherapy utilization rates are declining secondary to competing treatment options, to include a shift to active surveillance. With prostate cancer diagnosis on the rise, and prospective and randomized trials showing brachytherapy’s superior efficacy over other modalities such as radical prostatectomy and EBRT, it is important to put corrective actions in place to ensure that brachytherapy is available to patients across the globe.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Low-Dose Rate Prostate Brachytherapy Efficacy Analysis and Trends
Prostate cancer accounts for approximately 8% of all newly diagnosed cancer cases worldwide and 15% of cancer diagnoses in men, with more than 1.1 million new cases being recorded in 2012 across the globe [1]. In the United States and many other countries, prostate cancer is most frequently diagnosed in older men, with the highest probability of diagnosis being between ages 65 and 74 [2]. With projections of the male population ages 55–84 showing a significant increase for the United States over the next four decades, prostate cancer diagnoses will likely simultaneously rise [2]. Screening for prostate cancer in most developed countries allows for the disease to be caught before it spreads, increasing the likelihood of providing curative treatment options to newly diagnosed men. Increasing diagnoses, however, also require careful medical research, knowledge, and availability of efficacious and cost-effective treatment regimens for these patients.
Prospective randomized comparisons of prostate cancer treatment options are largely limited by physician biases, difficulty in patient recruitment, and the long natural history of prostate cancer, making survival endpoints difficult to attain. As such, researchers are often left to interpret single-institution retrospective and single-modality prospective studies to formulate comparisons between treatment outcomes and use of biochemical control as a surrogate endpoint for study design.
With results published in 2012, the Prostate Cancer Results Study Group (PCRSG) undertook a Herculean effort with the goal of distilling studies into clinically useful comparisons and completed the first large-scale comprehensive review of the literature comparing risk-stratified patients with long-term follow-up by treatment option [3]. The literature review demonstrated that brachytherapy provides superior outcomes in patients with low-risk disease in terms of biochemical prostate-specific antigen (PSA) free progression [3]. Additionally, the combination of EBRT and brachytherapy was shown to be superior to EBRT or surgery alone for intermediate-risk disease. Combination therapies involving EBRT and brachytherapy plus or minus androgen deprivation therapy (ADT) appear superior in terms of biochemical control as compared to more localized treatments such as brachytherapy alone, surgery alone, or EBRT alone for high-risk patients [3].
In 2017, the American Brachytherapy Society (ABS) formed a committee of clinical experts in brachytherapy to update existing, but outdated, guidelines to articulate the intricacies as well as new advances for the delivery of brachytherapy as well as to highlight its efficacy in treating prostate cancer. Utilizing previously published guidelines, clinical trial results, literature, and the experience of the committee members, the results outlined patient selection criteria and delivery guidelines for patients in both the brachytherapy monotherapy and brachytherapy boost setting [4]. Evidence that was reviewed was similar to the findings of the PCRSG, demonstrating that low-risk disease can be treated with brachytherapy alone without the need for EBRT or ADT [4]. Additionally, intermediate-risk patients with favorable features can be treated with brachytherapy monotherapy in the appropriate setting, and the guidelines outline that some high-intermediate- and high-risk patients should receive EBRT with a brachytherapy boost, plus or minus ADT as needed based on specific patient risk factors [4].
The National Cancer Database, representing an estimated 60–70% of newly diagnosed cancers in the United States, has shown over the past 15 years a trend in the increased utilization of prostatectomy, largely motivated by robotic-assisted radical prostatectomy, which was FDA approved for use in 2000 in the United States [5]. This has come at the cost of a decline in brachytherapy despite its proven clinical efficacy, as well as EBRT [5]. With a greater number of surgeries being performed, the use of ADT has also declined as it is not utilized with initial surgical removal of the prostate but used in combination with radiation techniques in the treatment of select higher-intermediate- and most high-risk and metastatic cancers [5].
Factors negatively impacting brachytherapy are multifactorial, some of which can be attributed to changes in screening, monitoring, and financial incentives for physicians [6]. The United States has seen a decrease in PSA screening which has resulted in a decrease in prostate cancer diagnosis due to the US Preventive Services Task Force discouraging the use of the service beginning in 2012 up until a change in 2017 [6]. Beginning in 2017, it is now recommended that PSA screening be offered based on individual circumstance [6]. This, with a simultaneous increase in patients electing active surveillance, has decreased treatment rates in recent years [6]. Additionally, an increase in the number of robotic prostatectomy as mentioned and the increased technical sophistication of EBRT technologies such as intensity-modulated radiation therapy (IMRT), stereotactic body radiation therapy, and proton beam therapies have resulted in a decrease in patients being referred for brachytherapy [6].
Radiation oncology practices in the United States have demonstrated a significant reduction in the use of brachytherapy from 2004 to 2012 [7]. Considering the superior results demonstrated for brachytherapy from multiple trials [3, 8], the future of brachytherapy’s role in treating prostate cancer needs to be considered carefully or a proven technology will be in jeopardy, and patients may not be granted access to a highly effective treatment which has minimal side effects [7]. Suboptimal volume of brachytherapy procedures has resulted in less training opportunities, leaving a question as to whether future physicians can be trained in this procedure [7]. Lack of knowledge of brachytherapy’s efficacy also remains widespread across the globe despite the ABS and other radiation therapy organizations offering schools and other opportunities for physicians to learn brachytherapy delivery techniques [7]. Simulation-based trainings at academic society organization’s annual meetings, creation of centers of excellence for training of residents and attending physicians, as well as worldwide collaboration in providing educational opportunities in the future could remedy the downward trend of brachytherapy’s utilization.
2 Brachytherapy in Low-Risk Prostate Cancer
Results of phase II/III clinical trials and large observational studies demonstrate brachytherapy is a highly efficacious and cost-effective treatment of low-risk prostate cancer. Studies have shown that brachytherapy as monotherapy is appropriate in low-risk prostate cancer, without the need for it to be combined with EBRT or ADT [3].
The American College of Surgeons Oncology Group’s phase III Surgical Prostatectomy Versus Interstitial Radiation Intervention Trial (SPIRIT) studied men with low-risk prostate cancer who attended a multidisciplinary education session through the University of Toronto Health Network and either elected to be randomized to radical prostatectomy or brachytherapy (n = 34 randomized) or chose to elect either radical prostatectomy (n = 62) or brachytherapy (n = 94) and assessed quality of life following treatment with a median follow-up of 5.2 years [8]. Although the trial closed secondary to poor accrual, men treated with brachytherapy scored better on health-related quality of life surveys for urinary (91.8 vs 88.1; P = 0.02) and sexual (52.5 vs 39.2; P = 0.001) areas as well as in overall patient satisfaction (93.6 vs 76.9; P < 0.001) as compared to patients who received radical prostatectomy [8].
In a similar study comparing brachytherapy for organ-confined disease to historical data of prostatectomy and EBRT, researchers on RTOG 98-05 study found that brachytherapy resulted in only 3 of 98 patients (3%) having maximum late toxicities of grade 3, all of which were genitourinary (GU), with no grade 4 or 5 toxicities [9]. The 8-year overall survival (OS) rate was 88%, with no patients having died of prostate cancer or toxicities related to care [9].
Research into the late effects of brachytherapy as monotherapy shows that results in terms of biochemical failure and toxicity compare very favorably to other treatment modalities [10]. The rates of biochemical relapse-free survival (bRFS), distant metastasis-free survival (DMFS), OS, and prostate cancer-specific mortality (PCSM) were studied in a cohort of 1989 low-, intermediate-, and high-risk patients treated from 1996 to 2007 by Kittel et al. [10]. The overall 10-year rates for bRFS, DMFS, OS, and PCSM were recorded as 81.5%, 91.5%, 76.1%, and 2.5%, respectively [10]. The overall rates of late grade ≥ 3 GU and gastrointestinal (GI) toxicity were 7.6% and 0.8%, respectively, which are comparable to results of other studies on brachytherapy as monotherapy in the United States [10]. Additionally, a study looking at biochemical relapse in brachytherapy published in 2015 showed that at a median follow-up of 5 years, 108 of 2223 patients (4.8%) treated with brachytherapy had developed either local or distant recurrence, proving lower rates of recurrence than most studies reviewed that reported on rates of distant recurrence following prostatectomy [11].
Long-term toxicities impacting quality of life are rare when brachytherapy is performed as monotherapy for patients with low-risk disease. Randomized evidence [8] suggests a favorable side effect profile, subsequent patient satisfaction, and durable urinary and sexual quality of life with brachytherapy as compared to other treatment modalities as well as good long-term survival outcomes.
3 Brachytherapy in Intermediate-Risk Prostate Cancer
Intermediate-risk patients can be candidates for brachytherapy monotherapy when their specific risk factors are considered by their physician. However, most often these patients are treated with brachytherapy in combination with EBRT and/or ADT [3]. Recent phase II/III evidence demonstrates brachytherapy provides excellent biochemical control for selected patients with intermediate-risk prostate cancer when utilized in combination with EBRT.
As with many treatment techniques, the quality of a brachytherapy implant and patient-specific disease characteristics are highly linked to rates of cancer control. Eleven American institutions combined data on 2693 patients diagnosed with low- and intermediate-risk disease that were treated with brachytherapy monotherapy between 1988 and 1998 [12]. With a median follow-up of 63 months, it was found that outcomes after brachytherapy relate to tumor stage, Gleason score (GS), pretreatment PSA, year of brachytherapy implant, and post-brachytherapy dosimetric quality, highlighting the importance of patient-specific risk factors when determining treatment recommendations for low-intermediate- and high-intermediate-risk prostate cancers [12]. PSA nadir ≤0.5 ng/mL was particularly associated with durable long-term PDFS [12].
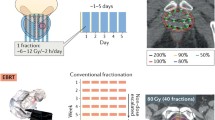
RTOG 0232 compared EBRT followed by brachytherapy boost and brachytherapy alone in patients with intermediate-risk disease at 68 participating centers throughout the United States and Canada from 2003 to 2012 (Prestidge, 13). Patients GS 2–6 and PSA ≥10 but <20 or GS 7 and PSA <10 received either EBRT 45 Gy/25 + brachytherapy or brachytherapy monotherapy (I125; Pd103) [13]. Freedom from progression (FFP) was studied, and it was found that the addition of EBRT to brachytherapy in men with intermediate-risk disease, stratified by GS, PSA, and ADT utilization, did not statistically improve outcomes [13]. At the fifth interim analysis, of the required 443 patients with 5 years of follow-up, 5-year PFS (95% CI) was 85% (80, 89) for the EBRT plus brachytherapy arm and 86% (81, 90) for the brachytherapy arm (HR Z 1.02, futility P Z 0.0006) [13].
An estimate of toxicities following EBRT (45 Gy in 25 fractions), followed 2–6 weeks later by brachytherapy to a delivered dose of 108 Gy, was published by Lee et al. in 2006 [14]. Patients were analyzable for acute and late toxicities [14]. Acute grade 3 toxicity was documented in 10 of 131 patients (7.6%), and no grade 4 or 5 acute toxicities were observed [14]. The estimate of late grade 3 GU and GI toxicity at 18 months was 3.3%, and no late grade 4 or 5 toxicities were observed [14].
Memorial Sloan Kettering Cancer Center studied the toxicities and outcomes of patients being treated with 45 Gy EBRT to the prostate and seminal vesicles, followed by brachytherapy boost with I125 (100 Gy) or Pd103 (90 Gy) [15]. At a median follow-up of 73 months, late GI and GU toxicity grade 2 and 3 occurred in 20% and 3% of patients, respectively [15]. The OS at 72 months was 96.1% [15].
4 Brachytherapy in High-Risk Prostate Cancer
The standard recommendation for patients with high-risk disease is EBRT and ADT as “multimodality” therapy. Recent studies have shown that the addition of brachytherapy to EBRT, however, improves biochemical control long-term, and therefore, patients with high-intermediate- or high-risk disease receiving EBRT +/− ADT should also be offered brachytherapy as a dose escalation or “trimodality” technique.
The Canadian Androgen Suppression Combined with Elective Nodal and Dose Escalated Radiation Therapy (ASCENDE-RT) trial studied patients with intermediate- or high-risk prostate cancer who had negative metastatic work-up with GS 8–10 or initial PSA (iPSA) 20–40 ng/mL [15]. Patients who had iPSA >40, cT-Stage ≥T3b, prior TUPR, and TRUS prostate volume > 75 cm3 or were unfit for general or spinal anesthesia were excluded per protocol [16]. The randomized study assigned men to either traditional dose-escalated EBRT in combination with ADT or EBRT plus a brachytherapy boost [16]. The study followed these patients in follow-up for a median of 6.5 years, and results demonstrated men who received a brachytherapy boost were nearly twice as likely to be free of biochemical failure [16].
A phase II study of men with high-risk prostate cancer found that a trimodality approach involving 2 years of ADT, EBRT, and brachytherapy and the addition of upfront docetaxel is well tolerated in patients and results in limited side effects while producing good long-term control results [17]. Eligibility for this study included PSA >20 ng/mL or GS 7 and a PSA >10 ng/mL, any GS 8–10, or stage T2b–T3 regardless of GS or PSA [17]. Patients received 45 Gy EBRT to the pelvis, followed 1 month later by brachytherapy with either I125 or Pd103 [17]. One month after brachytherapy, patients received three cycles of docetaxel and completed 2 years of ADT [17]. The median follow-up was 5.6 years [16]. Grade 2 and 3 acute GU and GI toxicities were 50.0% and 14.2%, respectively, with no grade 4 toxicities [17]. The 5- and 7-year actuarial rates of late grade 2 GI/GU toxicity, with no grade 3–5 toxicities reported, were 7.7% [17]. The 5- and 7-year FFBF rates were 89.6% and 86.5%, and corresponding rates for disease-free survival were 76.2% and 70.4% with 5- and 7-year OS rates being 83.3% and 80.1% [17].
5 The Future of Prostate Brachytherapy
It is recommended by both the American Association of Physicists in Medicine (AAPM) and ABS that a robust quality assurance program is key to ensure successful patient care [18]. Quality assurance is key in brachytherapy as factors such as inadequate training of physicians, physicist, dosimetrists, and therapists can lead to incorrect seed placement, program structure deficiencies, inadequate procedures, and poor management oversight of program and contractors [18]. The lack of a peer review process or lack of a culture of safety can lead to underutilization or improper utilization of brachytherapy to treat prostate cancer. As discussed, the development of centers of excellence, taking advantage of organizational training opportunities across the globe, and the consultation of organizations such as AAPM and ABS are critical in the creation and maintenance of a high-quality brachytherapy program [6].
Adoption of programs such as the design and implementation of a training program utilizing phantom-based simulators to teach the process of brachytherapy at The University of Texas MD Anderson Cancer Center will advance brachytherapy techniques worldwide [19]. The MD Anderson program focuses on teaching practicing oncologists, fellows, and resident physicians to focus on quality assurance through hands-on education for the simulation, treatment planning, implant technique, treatment evaluation, and outcome assessment of brachytherapy procedures [19]. Analysis of the program’s participants for brachytherapy implants showed a high degree of consistency between trainees as compared to implants in clinical practice, highlighting the potential opportunities to train brachytherapists in the skills necessary to safely perform and ensure quality assurance across the globe in the future [19].
Despite brachytherapy’s low rate of toxicity to organs at risk, toxicities overall remain a concern to radiation oncologists when prescribing radiation dose delivery. Although rectal injury is uncommon with advanced imaging, technologies developed to assist in the protection of organs at risk such as hydrogel spacers have been shown to greatly reduce toxicities such as grade 1–2 proctitis, which is reported in between 1 and 21% of prostate cancer patients and can potentially prevent severe rectal complications such as grade 3 ulcers and grade 4 fistulas. A key motivation in the utilization of rectal spacers is the higher risk of grade 3 rectal toxicity on EBRT + brachytherapy arm of the ASCENDE-RT trial [16].
By placing a hydrogel spacer between the Denonvilliers’ fascia and the rectal wall, space is created to protect the rectal wall from radiation delivered with both EBRT and brachytherapy. A randomized controlled trial recently looked at the dosimetry and clinical effects of perirectal hydrogel spacer application for patients undergoing EBRT and found that late rectal toxicity was 2.0% (all grade 1) in the spacer and 7.0% (up to grade 3) in the control group [20]. A long-term follow-up study completed by Hamstra et al. showed grade 1+ rectal toxicity at 3 years decreased by 75% in the spacer arm (control 9% vs spacer 2% p < 0.03), and no grade 2+ rectal toxicity was observed in patients who received a perirectal hydrogel spacer (p < 0.015) [21]. American institutions are beginning to incorporate rectal spacers into brachytherapy workflows as well, placing the spacer in the operating room immediately following radioactive seed implantation. Utilization of these advanced technologies, which are currently in the process of becoming widely available across the globe, can spare normal tissues from being negatively affected by radiation delivered to eradicate nearby tumors.
Another advancement for brachytherapy in the future is the integration of magnetic resonance imaging (MRI) technologies into treatment delivery. MRI is the standard imaging tool for staging of prostate cancer in much of the world, and the next step in the integration process for MRI technologies is its utilization in the planning and delivery of brachytherapy, which has grown in investigational and clinical use over the past decade [22]. Several advantages to MRI integration into brachytherapy treatment delivery include soft tissue resolution, localization of the disease within the prostate, visualization of the prostate’s apex, as well as localization of the bladder, rectum, and neurovascular bundles in relation to the prostate [22].
Lack of widespread utilization of MRI technologies can be attributed to access to these technologies, economic considerations and reimbursement, the learning curve associated with utilization of this technology in the operating room, reproducibility issues between treatment planning and delivery, as well as the favorable results of brachytherapy utilizing the current standard of CT-based planning and TRUS-based treatment delivery [22]. Investigational research in the United States has focused on the advancement of MRI in brachytherapy treatment planning and delivery, and it is believed that once operational costing and training opportunities are remedied, these technologies will be more utilized globally as MRI-based treatment planning and delivery has the potential to allow physicians to better define the prostate and the disease within, decreasing side effects for patients and increasing clinical outcomes.
Significant research has gone into costing analysis to define the value of brachytherapy as a treatment modality both with standard utilization of CT planning and TRUS-based treatment delivery as well as with the utilization of MRI in the workflow. Time-driven activity-based costing analysis demonstrated low resource utilization for brachytherapy overall, with 41% and 10% of costs occurring in the operating room and with the MRI scan, respectively, with no large increase in the cost of providing brachytherapy with utilization of an MRI as compared to the standard treatment regime of CT and TRUS-based care [23].
Conclusion
Research shows that brachytherapy is a cost-effective treatment modality with outcomes as good, if not superior, to other modalities. Regardless, data shows varying degrees of utilization across economic and geographic landscapes, and the application of this technique has seen a decline at academic centers, comprehensive community centers, and community cancer centers alike [6]. Given the increasing pressures facing radiation therapy centers across the globe, consideration needs to be given to the utilization of brachytherapy as a form of conformal therapy because of its ability to safely deliver high doses of radiation for disease control and cost-effectiveness both for implementation and long-term program sustainability [24].
References
Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. GLOBOCAN 2012 v1.1, Cancer incidence and mortality worldwide: IARC CancerBase no. 11 [internet]. Lyon, France: International Agency for Research on Cancer; 2014.
Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2014, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2014/, based on November 2016 SEER data submission, posted to the SEER web site, April 2017.
Grimm P, Billiet I, Bostwick D, et al. Comparative analysis of prostate-specific antigen free survival outcomes for patients with low, intermediate and high risk prostate cancer treatment by radical therapy. Results from the prostate Cancer results study group. BJU Int. 2012;109(Suppl 1):22–9.
Bittner NH, Orio PF, Merrick GS, Prestidge BR, Hartford AC, Rosenthal SA. The American College of Radiology and the American Brachytherapy Society practice parameter for transperineal permanent brachytherapy of prostate cancer. Brachytherapy. 2017;16(1):59–67.
Martin JM, Handorf EA, Kutikov A, Uzzo RG, Bekelman JE, Horwitz EM, Smaldone MC. The rise and fall of prostate brachytherapy: use of brachytherapy for the treatment of localized prostate Cancer in the National Cancer Data Base. Cancer. 2014;120:2114–21.
Orio PF, Nguyen PL, Buzurovic I, Cail DW, Chen YW. Prostate brachytherapy case volumes by academic and non-academic practices: implications for future residency training. Int J Radiat Oncol Biol Phys. 2016;96(3):624–8.
Orio PF, Nguyen PL, Buzurovic I, Cail DW, Chen YW. The decreased use of brachytherapy boost for intermediate and high-risk prostate cancer despite evidence supporting its effectiveness. Brachytherapy. 2016;15(6):701–6.
Crook JM, Gomez-Iturriaga A, Wallace K, Ma C, Fung S, Alibhai S, Jewett M, Fleshner N. Comparison of health-related quality of life 5 years after SPIRIT: surgical prostatectomy versus interstitial radiation intervention trial. J Clin Oncol. 2011;29(4):362–8.
Lawton CA, Hunt D, Lee WR, Gomella L, Grignon D, Gillin M, Morton G, Pisansky TM, Sandler H. Long-term results of a phase II trial of ultrasound-guided radioactive implantation of the prostate for definitive management of localized adenocarcinoma of the prostate (RTOG 98-05). Int J Radiat Oncol Biol Phys. 2011;81(1):1–7.
Kittel JA, Reddy CA, Smith KL, Stephans KL, Tendulkar RD, Ulchaker J, Angermeier K, Campbell S, Stephenson A, Klein EA, Wilkinson DA, Ciezki JP. Long-term efficacy and toxicity of low-dose-rate 125I prostate brachytherapy as monotherapy in low-, intermediate-, and high-risk prostate Cancer. Int J Radiat Oncol Biol Phys. 2015;92(4):884–93.
Lo AC, Morris WJ, Pickles T, Keyes M, McKenzie M, Tyldesley S. Patterns of recurrence after low-dose-rate prostate brachytherapy: a population-based study of 2223 consecutive low- and intermediate-risk patients. Int J Radiat Oncol Biol Phys. 2015 Mar 15;91(4):745–51.
Zelefsky MJ, Kuban DA, Levy LB, Potters L, Beyer DC, Blasko JC, Moran BJ, Ciezki JP, Zietman AL, Pisansky TM, Elshaikh M, Horwitz EM. Multi-institutional analysis of long-term outcome for stages T1-T2 prostate cancer treated with permanent seed implantation. Int J Radiat Oncol Biol Phys. 2007 Feb 1;67(2):327–33.
Prestidge BR, Winter K, Sanda MG, Amin M, Bice WS, Michalski J, Ibbott GS, Crook JM, Catton CN, Gay HA, Donavanik V, Beyer DC, Frank SJ, Papagikos MA, Rosenthal SA, Barthold HJ, Sandler HM RM. Initial report of NRG oncology/RTOG 0232: a phase III study comparing combined external beam radiation and transperineal interstitial permanent brachytherapy with brachytherapy alone for selected patients with intermediate risk prostatic carcinoma. Int J Radiat Oncol Biol Phys. 2016;96(2):S4.
Lee WR, DeSilvio M, Lawton C, Gillin M, Morton G, Firat S, Baikadi M, Kuettel M, Greven K, Sandler H. A phase II study of external beam radiotherapy combined with permanent source brachytherapy for intermediate-risk, clinically localized adenocarcinoma of the prostate: preliminary results of RTOG P-0019. Int J Radiat Oncol Biol Phys. 2006 Mar 1;64(3):804–9.
Hurwitz MD, Halabi S, Archer L, McGinnis LS, Kuettel MR, DiBiase SJ, Small EJ. Combination external beam radiation and brachytherapy boost with androgen deprivation for treatment of intermediate-risk prostate Cancer. Cancer. 2011;117(24):5579–88.
Morris WJ, Tyldesley S, Roda S, Halperon R, Pai H, McKenzie M, Duncan G, Morton G, Hamm J, Murray N. Androgen suppression combined with elective nodal and dose escalated radiation therapy (the ASCENDE-RT Trial): an analysis of survival endpoints for a randomized trial comparing a low-dose-rate brachytherapy boost to a dose-escalated external beam boost for high- and intermediate-risk prostate cancer. Int J Radiation Oncol Biol Phys. 98:275–85.
Dibiase SJ, Hussain A, Kataria R, Amin P, Bassi S, Dawson N, Kwok Y. Long-term results of a prospective, phase II study of long-term androgen ablation, pelvic radiotherapy, brachytherapy boost, and adjuvant docetaxel in patients with high-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2011 Nov 1;81(3):732–6.
Pfeiffer D, Sutlief S, Feng W, Pierce HM, Kofler J. AAPM task group 128: quality assurance tests for prostate brachytherapy ultrasound systems. Med Phys. 2008 Dec;35(12):5471–89.
Thaker NG, Kudchadker RJ, Swanson DA, Albert JM, Mahmood U, Pugh TJ, Boehling NS, Bruno TL, Prestidge BR, Crook JM, Cox BW, Potters L, Moran BJ, Keyes M, Kuban DA, SJ F. Establishing high-quality prostate brachytherapy using a phantom simulator training program. Int J Radiat Oncol Biol Phys. 2014 Nov 1;90(3):579–86.
Mariados NM, Sylverseter J, Shah D, et al. Hydrogel spacer prospective multicenter randomized controlled pivotal trial: dosimetric and clinical effects of perirectal spacer application in men undergoing prostate image guided intensity modulated radiation therapy. Int J Radiation Oncol Biol Phys. 2014;92(5):971–7.
Hamstra DA, et al. Continued benefit to rectal separation for prostate radiation therapy: final results of a phase III trial. Int J Radiation Oncol Biol Phys. 2017;97(5):976–85.
Pugh TJ, Pokharel SS. Magnetic resonance imaging in prostate brachytherapy: evidence, clinical end points to data, and direction forward. Brachytherapy. 2017;16:659–64.
Thaker NG, Pugh TJ, Mahmood U, Choi S, Spinks TE, Martin NE, Sio TT, Kudchadker RJ, Kaplan RS, Kuban DA, Swanson DA, Orio PF, Zelefsky MJ, Cox BW, Potters L, Buchholz TA, Feeley TW, Frank SJ. Defining the value framework for prostate brachytherapy using patient-centered outcome metrics and time-driven activity-based costing. Brachytherapy. 2016 May-Jun;15(3):274–82.
Orio PF, Durkee B, Lanni T, Lievens Y, Petereit D. Is brachytherapy cost effective? In: William Y, Tanderup K, Pieters B, editors. Emerging Technologies in Brachytherapy. Boca Raton: CRC Press; 2017.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Orio, P.F., Crouse, K.A., Nguyen, P.L., King, M.T. (2019). Prostate Brachytherapy: Clinical Efficacy and Future Trends. In: Yoshioka, Y., Itami, J., Oguchi, M., Nakano, T. (eds) Brachytherapy. Springer, Singapore. https://doi.org/10.1007/978-981-13-0490-3_10
Download citation
DOI: https://doi.org/10.1007/978-981-13-0490-3_10
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-0489-7
Online ISBN: 978-981-13-0490-3
eBook Packages: MedicineMedicine (R0)