Abstract
Gene therapy offers a great potential for the treatment of genetic diseases as well as acquired diseases by means of delivering therapeutic nucleic acids inside the cell. To deliver nucleic acids, broadly two strategies have been employed by using viral vectors and non-viral vectors. The viral vectors exhibited high transduction efficacy both in vitro and in vivo. The non-viral vectors composed of mainly cationic polymers and lipids which provide efficient condensing capability against negatively charged nucleic acids and low cytotoxicity. Till date, >2300 clinical trials for gene therapy are going on worldwide, approximately 70% using viral vectors and remaining with non-viral vectors. The immunogenicity, non-targeting abilities are the biggest hurdles in terms of safety and efficiency for successful therapy with these vectors. These two classes of vectors have their own advantages as well as disadvantages which hinder their therapeutic endpoint in clinical trials. Now, researchers have made attempts to form virus encapsulated in chemical vectors which are called as hybrid vectors. These hybrid vectors have immense potential to evade host immune system by masking the immunogenic epitopes present on viral vectors. The molecules or scaffold which is used for encapsulating virus enhance their targeting ability and sustained release to targeted tissue. The hybrid vectors, combination of viral and chemical vectors, form a new class of gene delivery vectors which overcome the limitations of each vector and simultaneously augment desirable features such as targeting ability, low immunogenicity, cytotoxicity, higher payload, and ability to deliver more than one transgene. The hybrid vectors should retain characteristics of the each vector in order to achieve optimal tissue targeting and gene delivery with minimal toxicity. To achieve therapeutic endpoint with the hybrid vectors, development of such hybrid vectors requires extensive understanding of physicochemical properties after coating virus with chemical analogues and their optimal ratio as well. These aspects will be discussed in this chapter.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
1 Introduction
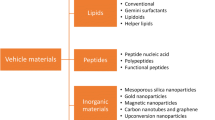
Paradigm changing recent developments in the field of nanotechnology offer the platform where Physicochemical and biological properties of metallic and nonmetallic molecules can be modulated for the wide range of applications in several areas of communications, basic sciences, engineering, medicine, robotics, etc. [1,2,3,4]. Since the introduction of the term nanotechnology, various modifications have been implemented to develop novel variants of nanoparticles with diverse properties [5, 6]. Specifically, nanoparticles are in the size range of 5–100 nm and possess high surface area to volume ratio which renders them to bind molecules with bi-specific conjugate or specific targeting peptides [7]. Based on the composition of nanoparticles, they can be categorized as polymeric (synthetic or natural polymers), Q-dots, nanoemulsions, ceramic (silica) particles, metallic (gold, silver, iron oxide), liposomes, and graphene [8]. Accordingly, nanoparticles exhibit specific optical, magnetic, chemical, and physical properties that lead to their application in various biomedical applications such as in vivo imaging, tissue-specific drug delivery, etc. [9,10,11]. The major advantage of nanoparticles containing tissue-specific moiety as a delivery vehicle is the ability to bypass side effects associated with therapeutics such as antibiotics or chemotherapeutic agents [12]. Thus, such properties make them useful for both vaccination and therapeutic strategies to circumvent an immune response or for gene delivery, respectively [13]. Delivery of a normal copy of genes inside the cells is a promising approach for the treatment of various genetic or acquired disorders and is also called as replacement gene therapy. Viruses are the potential candidates for delivering therapeutic genes inside the cells with higher efficiency; to achieve the therapeutic gene expression, various recombinant vectors have been used including adenovirus, retro-/lentivirus, and adeno-associated virus (AAV) [14]. Till date, >2300 clinical trials for gene therapy are going on worldwide out of which 70% are using viral vectors, but none of them have reached desired therapeutic endpoints [14,15,16]. The primary objective of gene therapy is to maintain stable transgene expression, but the major hurdle for gene therapy is host immunity which hinders persistent high levels of transgene expression [17]. Since the viruses are a coating of proteins, thus they are recognized as foreign bodies by host immune system and lead to their activation. The host immunity serves as a major side effect for gene therapy through viral vectors. Recently, some reports showed using the combination of nanoparticle and viral vectors to optimize therapeutic delivery, for example, viral vectors encapsulated in nanomaterials rescued gene therapy vectors from adverse immunity events [18, 19]. Taking a cue from these kinds of studies, this chapter summarizes the data available on hybrid vector-based delivery systems which consist of nanoparticle and viral vectors, the strategies to enhance the potential of the hybrid system, and their advantages.
2 Concept of Gene Therapy
The technique of delivering a therapeutic gene into host cells to ameliorate the genetic disorder or acquired disease is called gene therapy. The gene therapy can be classified into two categories as (1) somatic cell gene therapy, limited to individual, and (2) germline gene therapy – modified gene is inheritable. Due to ethical issues, insufficient knowledge, and risk to future generations, germline gene therapies are prohibited in many countries. Thus, most of the gene therapy programs have been focused on somatic gene therapy. Since its discovery in 1980, the first clinical trial was established in 1990 using retrovirus as a vector for functional adenosine deaminase [20]. Till date, >2300 clinical trials have been conducted using various viral vectors in different parts of the world [14]. As advancement in the field of viral vectors, alternative approaches have been implemented and showed promising potential by knocking down the mutated gene (suicide gene therapy) or editing faulty gene (nuclease-mediated gene editing) to reach therapeutic endpoint [21]. These delivery systems have been used in two distinct modes: (1) ex vivo, where viral vector with therapeutic gene is transduced in recipient cells (e.g., hematopoietic cells) and then transduced cells are introduced into the host body, and (2) in vivo, where the viral vectors are administered directly into host body [22]. The choice of approach is mainly based on disease and target tissue to be treated from gene delivery. An ideal vector should exhibit sustained transgene expression and tissue specificity with low immunogenicity for higher therapeutic efficacy through critical designing of viral vectors; they have been used with fair success for various genetic disorders like cystic fibrosis [23], hemophilia [24], Leber’s congenital amaurosis [25], and various severe combined immunodeficiency (SCID) [26, 27]. Currently, three kinds of viruses, i.e., adenovirus, retrovirus/lentivirus, and adeno-associated virus (AAV), have been employed as vectors for delivering therapeutic genes to the desired cells [14]. These vectors have shown promising results and success in gene therapy up to some extent. Thus, there is a scope for further advancement for improving the therapeutic efficacy.
3 Viral and Non-viral Hybrid Vectors
Since the 1980s, both viral and non-viral vectors (synthetic) have been developed to overcome the limitations associated with both delivery systems for making gene therapy a viable technology in clinics (Fig. 4.1). Although viral vectors have a high transduction efficacy for DNA, they are immunogenic. On the contrary, non-viral vectors have low transfection efficacy than viral vectors, but generally, they have low immunogenicity (as they have been designed from biocompatible material). Thus, to leverage the advantages from both types of vectors, hybrid vectors were developed by the combination of both vectors to achieve higher gene delivery efficacy than individual vector alone with minimal side effects (i.e., immunogenicity). In an attempt to develop hybrid vectors, viral vectors (AAV, adenovirus, retro-/lentivirus) have been encapsulated within synthetic materials such as liposomes, dendrimers, and hydrogels (Figs. 4.3 and 4.4). Some of hybrid vectors that have shown significant efficacy in delivering genes are listed in Table 4.1. Among all the viral vectors, adenovirus showed promising potential for development of hybrid vector systems as they were able to target tumor tissues efficiently [28,29,30,31,32]. Moreover, it can function effectively with different non-viral vectors (Table 4.2) such as alginate beads [33], chitosan [34, 35], chitosan-PEG-folate conjugate [36], polyethyleneimine [37, 38], etc. To develop tissue targeting hybrid vectors, conjugation of moieties like arginine graft [39], RGD [40], and Herceptin [41] and even surface charge modification [38, 42] have shown precise targeting by vectors (Fig. 4.2 and Table 4.3). The arginine-grafted bioreducible polymers (ABP) were synthesized, and hybrid vectors were developed with adenovirus to overcome the immune response from the host with minimal cytotoxicity. In vitro results showed after electrostatic coating of ABP over adenovirus resulted in enhancement of six-fold transduction efficiency in coxsackievirus and adenovirus receptor (CAR)-negative cells as compared to naked Ad vectors [39]. These results suggested after cationic polymer coating, hybrid vectors internalize within the cell through CAR-independent pathway. Moreover, ABP-Ad vector showed 83.1% of transduction efficiency in the presence of 30% serum in A549 cells, while naked Ad vectors showed 47.49% efficiency. Further, an innate immune response was evaluated after treating RAW264.7 macrophage cells with naked Ad and ABP-Ad vectors. Pro-inflammatory cytokine IL-6 release was significantly reduced after treatment with ABP-Ad (38.57 ± 0.5 pg/mL) as compared to naked Ad (70.35 ± 0.5 pg/mL). These results strongly suggested that shielding of the viral proteins with cationic polymers can enhance circulation period for hybrid vectors and reducing innate immune response. In a similar study, a cationic biodegradable polymer, methoxy poly(ethylene glycol)-b-poly{N-[N-(2-aminoethyl)-2-aminoethyl]-L-glutamate} [PNLG], was synthesized, and hybrid vectors were developed with adenoviruses [29]. The transduction efficiency of developed PNLG-Ad vector was compared to ABP-Ad vectors in vitro and in vivo. The PNLG-Ad vectors exhibited high stability at 37 °C and pharmacokinetics due to the formation of smaller particle size (~130–140 nm), while ABP-Ad vector formed 400–1300 nm size particles. The tumor growth was reduced in various xenograft models such as 57.5% (HT1080)/47.0% (A549), whereas ABP-Ad showed reduction up to 24.8% (HT1080)/16.4% (A549). The innate immune response was also evaluated by quantifying the IL-8 and vascular endothelial growth factor (VEGF) released after treatment with ABP-Ad, PNLG-Ad, and naked Ad vectors. The results showed significant inhibition of IL-8 or VEGF secretion, 76.6% or 79.7%, respectively, on treatment with PNLG-Ad while 47.7% or 60.7% with ABP-Ad. Moreover, systemic administration of PNLG-Ad vector exhibited a 1229-fold increase in tumor to the liver ratio as compared to naked Ad. These studies revealed that biophysical property of hybrid vectors such as particle size and surface charge plays a crucial role in their therapeutic efficacy. Similarly, several reports have been published using cationic bioreducible polymers (exclusively polyethylenimine) [37, 38] and mPEG-PEI-g-Arg-S-S-Arg-gPEI-mPEG [30] for the development of hybrid vectors.
Hybrid viral nanoparticles. The combination of viral vectors and nanomaterials offers many advantages such as delivery of multiple payloads, targeting ability to specific tissue, and escape from host immune system. The schematic representation of the advantages of hybrid vectors. (a) Variations between the cationic liposomally bound viral particles and anionic liposomally bound nanoparticles. (b) Viral particles encapsulated in fibrin hydrogels. Difference between naked viral particles and hydroxyapatite (HA)-coated viral particle-loaded in fibrin hydrogels is highlighted
After successful development of hybrid vectors which can internalize inside the cell through CAR-independent pathway without triggering the immune response, researchers focused on developing hybrid vector with targeting ability. In an attempt to develop targeting hybrid vector against folate receptor (FR)-positive cancer, adenovirus was electrostatically complexed with chitosan [36]. Then, polyethylene glycol (PEG)/folic acid (FA) or PEG-FA was chemically conjugated to the surface of chitosan-Ad to develop various nanocomplex such as chitosan-Ad, chitosan-PEG-Ad, chitosan-FA, and chitosan-PEG-FA-Ad. The vectors consisting of FA on the surface (chitosan-FA-Ad, chitosan-PEG-FA-Ad) exhibited significant selectivity against folate receptor-positive cells (HeLa and KB cells) and showed cell viability up to ~45% in KB and HeLa cells while ~70–80% in FR-negative cells (U343 and A549 cells). Systemic administration of chitosan-PEG-Ad and chitosan-PEG-FA-Ad significantly increased the blood circulation time after 24 h of injection, resulting in 9.0-fold and 48.9-fold increase, respectively, as compared to naked Ad. Moreover, these hybrid vectors showed ~75% decrease in generation of adenovirus-specific neutralizing antibodies in mice when treated with chitosan-PEG-FA-Ad as compared to naked Ad. The administration of chitosan-PEG-FA-Ad exhibited 378-fold reduction in liver tissues and 285-fold increase in tumor tissue as compared to naked Ad; hence the hybrid vector was able to enhance the tumor-to-liver ratio. The targeting hybrid vector exhibited 52.8% inhibition of tumor growth as compared to naked Ad. Thus, conclusively chitosan-PEG-FA-Ad showed promising potential for further development of targeting hybrid vectors in terms of efficacy and safety. To develop targeting vectors against endothelial cells of tumor capillaries and neointimal tissues, a bioreducible cationic polymer CD was conjugated to cyclic RGD peptide (Fig. 4.2). These tissues inherently overexpresses αvβ3 and αvβ5 integrin proteins which selectively bind to RGD peptides. Two hybrid variants were synthesized with different molecular weights of PEG chains, viz., PEG500 and PEG2000 to generate CD-PEG500-RGD-Ad and CD-PEG2000-RGD-Ad [40]. The results showed RGD-tethered polymer-coated hybrid vectors were specifically killing the cancer cells having integrin protein on cell membrane, irrespective of CAR. The CD-PEG500-RGD-Ad hybrid vector was efficiently able to express shRNA against IL-8 mRNA. There was significant reduction of IL-8 expression in cancer cells was observed as compared to naked Ad, such as 79.6% decrease in HT1080 and 77.2% decrease in MCF7 cells. Further, exploiting the cell surface biomarker as a target which is overexpressed on cancer cells, various potential ligands have been investigated. Her2/neu is widely known as human epidermal growth factor 2 receptor and overexpressed in 20–30% of breast cancer patients. This receptor plays an important role as an oncogene in cancer cells. Drugs which target these receptors like trastuzumab and lapatinib are in clinical use; trastuzumab (Herceptin), a monoclonal antibody specific for Her2/neu, is also being used widely for treatment of both early and metastatic breast cancer [43, 44]. To develop Her2/neu targeting hybrid vector, adenovirus (Ad) was chemically conjugated with bioreducible PEG chain, and Herceptin was tethered terminally, HER-PEG-Ad [41]. Specificity and CAR-independent cellular uptake of these Herceptin-conjugated hybrid vectors were evaluated in vitro using Her2-positive (MDA-MB435, SK-OV3, and MDA-MB231) and Her2-negative (SK-Her1 and HeLa) cells. Further, innate response and stability of the HER-PEG-Ad were evaluated after systemic administration in BALB/c mice. The results showed after administration, IL-6 secretion level was found to be 77 pg/mL, 14 pg/mL, 411 pg/mL, and 46 pg/mL for HER-PEG-Ad, PEG-Ad, naked Ad, and PBS, respectively. After 1 h of administration, HER-PEG-Ad and PEG-Ad were six-fold higher than naked Ad in blood circulation. The ligand-modified hybrid vector showed significant higher targeting ability for tumor in xenograft model, and HER-PEG-Ad showed 1010-fold increase in tumor-to-liver ratio with minimal hepatic toxicity. These reports suggest that the development of hybrid systems from nanomaterial-coated viral vector using nonpathogenic viruses like AAV serves as excellent candidates for higher efficacy with minimal side effects.
4 Dendrimer-Coated Virus Particles
In a recent study, the hybrid vector (as shown in Fig. 4.3) was developed for gene transfer in liver cancer xenograft model from adenovirus coated with poly(amidoamine) dendrimer generation 5 (PAMAM-G5) [45]. The transduction efficacy and tissue tropism of coated adenovirus particles (Ad5-CMV/NIS) which consist of hNIS transgene (sodium-iodide symporter) were tested by radioactive iodine isotope (123I) scintigraphy. The in vitro results have shown a significant decrease in antibody-mediated neutralization and increase in the CAR-negative cell (extent in adenovirus infection). Further, when this hybrid vector was administered in mice, it showed sustained transgene expression and reduction in tumor size as well. The study showed such delivery systems using adenovirus hybrid vectors indicate high therapeutic potential. Moreover, to incorporate targeting ability to the dendrimer-based hybrid vectors, dendrimer was conjugated to the peptide as a ligand specific for epidermal growth factor receptor (EGFR), PAMAM-GE11 [46]. In this study, PAMAM-G2 and PAMAM-G5 were used, but PAMAM-G2-GE11 showed better efficiency due to improved covering of adenoviral surface epitopes by smaller diameter of dendrimers. This hybrid vector also showed CAR-independent cellular uptake with low hepatic accumulation as well as an increase in transduction efficiency over tumor cells in the xenograft model.
5 Virus Particles Encapsulated Liposomes
Viral gene therapy holds great potential in treating cancer using oncolytic replication-selective viruses (OVs) as they selectively replicate within cancer cells and causes apoptosis [47]. The use of OV-based gene therapy showed significant alleviation of cancer in human clinical trials even with advanced stages of cancer [48]. However, their efficacy has been limited by rapid clearance through reticuloendothelial (RE) system in liver and neutralization by antibodies which affect their distribution into the tumor cells [49]. To overcome the issue of neutralization of OV by antibodies, Yotnda P. et al. have encapsulated adenovirus vectors in bilamellar cationic liposomes consists of DOTAP (1,2-dioleoyloxypropyl)-N,N,N-trimethylammonium chloride) and cholesterol [50] (Fig. 4.4a). This hybrid vector was able to efficiently transfect the cells which either lacks adenoviral receptors or in the presence of receptor, as compared to naked adenovirus. However, their clinical application was hindered due to systemic toxicity, low targeting efficacy, and poor serum stability. To address these issues, adenoviral vectors (adenovirus 5, Ad5) were encapsulated in anionic bilamellar liposomes composed of phosphatidylcholine, phosphatidylethanolamine, inositol phosphatides, cholesterol, PEG-2000, and nontoxic lecithin (Fig. 4.4a) [51]. These anionic liposome-encapsulated adenoviral-based hybrid vectors have shown superior transfection efficacy in cancer cells than naked Ad5 and were able to administer repeatedly without any immunogenic response in vivo. Moreover, the anionic liposomal virus particles have shown stability for 32 h as a monodisperse solution, while cationic liposomal virus particle got aggregated within a couple of hours (Fig. 4.4A). The anionic liposomal-based encapsulated viral particles have shown promising results for further use in clinical application [51].
6 Virus Vector-Laden Hydrogels
In a study to develop a better transduction profile with lentiviruses, lentiviruses were encapsulated in hydrogels composed of collagen and hydroxyapatite [52]. The effect of material used for hydrogel formation and their degradation kinetics for transgene expression was evaluated both in vitro and in vivo. The encapsulated lentivirus showed ~80% of transfection efficiency in invasive C6 glioma cells. Further, the virion release and cell migration from the surrounding tissue was depending on the composition of collagen hydrogel (0.05%, 0.15%, 0.3%). While the efficacy of lentivirus loaded in hydroxyapatite containing collagen-gels was marginal (~33% increase in luciferase gene expression) as compare to only collagen-containing gels in an animal model (CD-1 male mice). Similarly, another study was carried out using fibrin and hydroxyapatite hydrogel encapsulated lentiviruses for localized vector transduction in CD-1 mice (Fig. 4.4b), but this strategy did not affect the virus infectivity or their cellular infiltration [53]. To develop high-performance delivery systems, researchers have used AAV vectors combined with elastin-like polypeptides (ELP) and evaluated for their infectivity on human neural stem cells (NSCs) and murine fibroblasts (NIH3T3) [54]. This study was carried out using AAV variant r3.45 which showed a significant increase in transduction efficacy when conjugated to ELP as compared to control groups. The results showed potential use of these hybrid vectors in NSCs for the treatment of various neurodegenerative disorders. To maximize the AAV contact with tissue for efficient and sustained gene transfer, AAVs were encapsulated in a nanofiber scaffold composed of ELP and poly(ε-caprolactone) (PCL) through electrospinning [18]. The super paramagnetic iron oxide nanoparticles (SPION) were coated with heparin and combined with AAV variant r3.45 which showed enhanced gene delivery in different types of cell lines, e.g., HEK293T and PC12 cell lines [55]. Even a short incubation period of <180 min was sufficient in transducing the target cells with the same efficiency achieved with conventional 24-hour incubation of naked virus. Moreover, the magnetically driven AAV transduction improved some of the critical phenotypes such as the neurite extension and expression for nerve growth factor in PC12 cells. These reports suggest that the hybrid vectors have several advantages over the convention delivery vectors, but its development requires exhaustive understanding related to host immune response, tissue specificity, and kinetics of nanoparticle-vector hybrid delivery under in vivo settings.
7 Challenges
The cellular uptake of nanoparticles in a large quantity inside the host cells generates concentration gradient across vascular endothelium which leads to inhibition of further uptake [56]. Moreover, this phenomenon stimulates the residential monocytic-phagocytic system and results in an aberrant distribution of nanoparticles (Fig. 4.5). However, there are various properties of hybrid nanoparticles such as size, surface charge, stability, and route of delivery which decide the efficiency of these vectors inside the cell [57, 58]. Under in vivo condition, the interaction of natural multivalent biomolecules in blood circulation and viral vectors generates the immune response and has been described below [59,60,61]. Many reports are suggesting that the generation of immune response associated with administering vaccines and drug delivery vehicles [10]. The extent of innate response mainly depends on targeted tissue (e.g., skin, lungs, gut), as each of tissue having a different number of residential immune cells [61, 62]. After cellular uptake, hybrid vectors got fragmented and stimulate either innate or adaptive immune response through a cascade of events initiating from antigen generation by antigen-presenting cells (APCs) to exocytosis or leading to cellular apoptosis [63]. The invasive property of hybrid vectors which causes endothelial cell injury and malfunction acts as the first sign for toxic effects on vascular system (Fig. 4.5) [64]. The immune response associated from various nanoparticle has been summarized in Table 4.4, but the overlap between the response generated is also frequently observed. In Fig. 4.6, detailed schematic representation of a possible number of events which lead to adaptive immunity in the presence of nanoparticles has been described. The nanoparticle antigens are captured by immature dendritic cells from closest lymph nodes which lead to the activation of T-cell differentiation and stimulating B cell as well [65]. Several inflammatory cytokines (TNF-α and IL-1β) and co-stimulatory receptor ligands CD80 (B7-1) and CD86 (B7-2) are responsible for activation and functionalization of DCs with antigen [66]. These activated DCs perform a cascade of signals along with MHC class I and II molecules to naive T cells having T-cell antigen receptor (TCR) [67]. Co-stimulatory signals CD80/86 which are generated from APCs interact with CD28 (T-cell receptor), and simultaneously secretion of cytokines (IL-12, IL-14, IL-16, TGF-β) also takes place which stimulates naive T cells to differentiate into Th1, Th2, or Th17 cells. The antigen functionalization involves MHC class II loading pathway [68] which leads to the generation of a limited number of CD8+ T cells, and thus antigens can only be presented to only specific groups of DCs in the spleen or lymph nodes [69]. These pathways are suggesting the possibility to modify strategies against induction of immunological tolerance associated with hybrid vectors. In a study using modified PEI/DNA complex, nanoparticles have suppressed the antigen-specific T-cell responses and lead to regulatory T-cell activation via IFN-αβ-mediated DC activation [70]. However, experimental variations by using different animal strains (C57BL/6 and BALB/c) were also affecting clearance of nanoparticles in mice strains [71]. These reports suggest that further extensive studies are needed to determine the fate of nanoparticles during in vivo administration of vectors. Moreover, the targeting ability of hybrid vectors needs further improvement for efficient gene delivery. The major drawback of viral vectors is their ability to induce oncogenicity and lack of gene transfer specificity [72, 73]. Among other viral vectors, lentiviral vectors can integrate the foreign gene into the host genome and activates proto-oncogenes [74]. Thus, there is a need for further systematic studies for hybrid vectors (viral vector and nanomaterial) to overcome the barriers of individual vectors which hinder their use in the clinical applications.
Innate immune response against nanoparticles. The entry of nanoparticles through endothelial cells is a primary event that triggers a cascade of signals toward nanoparticles or their fragments [75]. Innate immune response toward them differs substantially as it depends on the physical characteristics of nanoparticle such as size, shape, charge, and associated ligand/peptide molecules as well as route of entry [76,77,78]. The invasion of nanoparticle through endothelial cells leads to disruption of endothelial membrane and eventually activates vascular system along the nanoparticle concentration gradient. Events 1–5 show five different nanoparticles, i.e., silica, silver, gold, liposome, and carbon nanotubes, and the innate response observed against them. Macrophage-mediated phagocytosis of nanoparticle/ fragment involves multiple events including macrophage migration and differentiation in response to cytokines/chemokines that activates Th1Mϕ /Th2Mϕ cells [79,80,81]
This schematic representation depicts the adaptive immunity observed against the nanoparticles. (1) Dendritic cells act as a link between innate and adaptive immune system and regulate their cross activation through several signals (MHCI/II-peptide complex, CD80-CD80L, etc.) [66,67,68,69]. Movement of DCs bearing the peptide/MHC complex toward lymph nodes [82] is a critical factor that determines the magnitude of this activation. (2) In response to MHCI/II complex, cytokines (IL-4, IL-6, IL-12, TGF-β) and chemokines are released by naïve T cells that further activate downstream effectors such as the residential macrophages/monocytes which capture and destroy nanoparticle containing host cells. (3) Nanoparticle interaction with adaptive immune cells/molecules that leads to activation of host dendritic and cytotoxic T-cell population [83]. Some reports suggested that the nanoparticle coated with peptide ligand can also activate B cell and generate antibodies. (4) Nanoparticle-mediated response through T cell or B cell has been bypassed through activation of T-regulatory cells and suppression of pro-inflammatory molecules (IL-2, IL-6, TNF-α, etc.). (5) Macrophage activation and differentiation by dendritic cells and nanoparticle phagocytosis leads to the expulsion of nanoparticle from the host cells [84, 85]
8 Conclusions
Till now, viral and non-viral vectors have been extensively used to deliver a gene of interest to multiple target tissues. Combining both the vectors, hybrid vectors offers immense potential to deliver more than one transgene with tissue specificity. These vectors impart shielding of viral epitope surface to evade host immune response and provide a platform for conjugation of receptor-specific ligands on the surface to enhance targeting ability. However, the development of hybrid vector systems needs exhaustive knowledge of virus structure and the effect of nanomaterial coating on physicochemical properties of vectors. Further, most of the synthetic nanomaterials are also immunogenic in nature which cannot be overlooked. Thus, to generate hybrid system and for other biomedical applications, it is necessary to alleviate the immunogenicity of the synthetic nanomaterial. It is essential to select an appropriate non-immunogenic nanomaterial to develop hybrid vector systems and achieve higher efficacy with minimal side effects.
References
Liu Y, Chen C (2016) Role of nanotechnology in HIV/AIDS vaccine development. Adv Drug Deliv Rev 103:76–89
Padovani GC, Feitosa VP, Sauro S, Tay FR, Duran G, Paula AJ, Duran N (2015) Advances in dental materials through nanotechnology: facts, perspectives and toxicological aspects. Trends Biotechnol 33(11):621–636
Fukuda T, Nakajima M, Kojima M (2010) Micro-Nano robotics and automation system. IFAC Proceedings Volumes 43(8):20–25
Segev-Bar M, Haick H (2013) Flexible sensors based on nanoparticles. ACS Nano 7(10):8366–8378
Amoozgar Z, Yeo Y (2012) Recent advances in stealth coating of nanoparticle drug delivery systems. Wiley Interdiscip Rev Nanomed Nanobiotechnol 4(2):219–233
Petrov A, Audette GF (2012) Peptide and protein-based nanotubes for nanobiotechnology. Wiley Interdiscip Rev Nanomed Nanobiotechnol 4(5):575–585
Jin S, Ye K (2007) Nanoparticle-mediated drug delivery and gene therapy. Biotechnol Prog 23(1):32–41
Ilinskaya AN, Dobrovolskaia MA (2013) Nanoparticles and the blood coagulation system. Part I: benefits of nanotechnology. Nanomedicine 8(5):773–784
Issa B, Obaidat IM, Albiss BA, Haik Y (2013) Magnetic nanoparticles: surface effects and properties related to biomedicine applications. Int J Mol Sci 14(11):21266–21305
Silva JM, Videira M, Gaspar R, Preat V, Florindo HF (2013) Immune system targeting by biodegradable nanoparticles for cancer vaccines. J Control Release 168(2):179–199
Barua S, Yoo JW, Kolhar P, Wakankar A, Gokarn YR, Mitragotri S (2013) Particle shape enhances specificity of antibody-displaying nanoparticles. Proc Natl Acad Sci USA 110(9):3270–3275
Fortina P, Kricka LJ, Surrey S, Grodzinski P (2005) Nanobiotechnology: the promise and reality of new approaches to molecular recognition. Trends Biotechnol 23(4):168–173
Rawat M, Singh D, Saraf S (2006) Nanocarriers: promising vehicle for bioactive drugs. Biol Pharm Bull 29(9):1790–1798
Manno CS, Pierce GF (2006) Successful transduction of liver in hemophilia by AAV-Factor IX and limitations imposed by the host immune response. Nat Med 12(3):342–347
Bowles DE, McPhee SW, Li C, Gray SJ, Samulski JJ, Camp AS, Li J, Wang B, Monahan PE, Rabinowitz JE, Grieger JC, Govindasamy L, Agbandje-McKenna M, Xiao X, Samulski RJ (2012) Phase 1 gene therapy for Duchenne muscular dystrophy using a translational optimized AAV vector. Mol Ther 20(2):443–455
Dobrovolskaia MA, Aggarwal P, Hall JB, McNeil SE (2008) Preclinical studies to understand nanoparticle interaction with the immune system and its potential effects on nanoparticle biodistribution. Mol Pharm 5(4):487–495
Lee PY, Wong KK (2011) Nanomedicine: a new frontier in cancer therapeutics. Curr Drug Deliv 8(3):245–253
Reetz J, Herchenroder O, Putzer BM (2014) Peptide-based technologies to alter adenoviral vector tropism: ways and means for systemic treatment of cancer. Viruses 6(4):1540–1563
Anderson WF (2000) Gene therapy. The best of times, the worst of times. Science 288(5466):627–629
Setlow JK (2003) Genetic engineering: principles and methods. Springer, New York
Hackett NR, Crystal RG (2004) Gene and cell therapy: therapeutic mechanisms and strategies, 2nd edn (ed: Templeton NS). Merkel Dekker, Inc, Texas
Flotte T, Carter B, Conrad C, Guggino W, Reynolds T, Rosenstein B, Taylor G, Walden S, Wetzel R (1996) A phase I study of an adeno-associated virus-CFTR gene vector in adult CF patients with mild lung disease. Hum Gene Ther 7(9):1145–1159
Nathwani AC, Tuddenham EG, Rangarajan S et al (2011) Adenovirus-associated virus vector-mediated gene transfer in hemophilia B. N Engl J Med 365(25):2357–2365
Hauswirth WW, Aleman TS, Kaushal S, Cideciyan AV, Schwartz SB, Wang L, Conlon TJ, Boye SL, Flotte TR, Byrne BJ, Jacobson SG (2008) Treatment of leber congenital amaurosis due to RPE65 mutations by ocular subretinal injection of adeno-associated virus gene vector: short-term results of a phase I trial. Hum Gene Ther 19(10):979–990
Buckley RH (2004) Molecular defects in human severe combined immunodeficiency and approaches to immune reconstitution. Annu Rev Immunol 22:625–655
D’Costa J, Mansfield SG, Humeau LM (2009) Lentiviral vectors in clinical trials: current status. Curr Opin Mol Ther 11(5):554–564
Kim J, Kim PH, Kim SW, Yun CO (2012) Enhancing the therapeutic efficacy of adenovirus in combination with biomaterials. Biomaterials 33(6):1838–1850
Kim J, Li Y, Kim SW, Lee DS, Yun CO (2013) Therapeutic efficacy of a systemically delivered oncolytic adenovirus–biodegradable polymer complex. Biomaterials 34(19):4622–4631
Jung SJ, Kasala D, Choi JW, Lee SH, Hwang JK, Kim SW, Yun CO (2015) Safety profiles and antitumor efficacy of oncolytic adenovirus coated with bioreducible polymer in the treatment of a CAR negative tumor model. Biomacromolecules 16(1):87–96
Kim PH, Kim J, Kim TI, Nam HY, Yockman JW, Kim M, Kim SW, Yun CO (2011) Bioreducible polymer-conjugated oncolytic adenovirus for hepatoma-specific therapy via systemic administration. Biomaterials 32(35):9328–9342
Kim J, Kim PH, Nam HY, Lee JS, Yun CO, Kim SW (2012) Linearized oncolytic adenoviral plasmid DNA delivered by bioreducible polymers. J Control Release 158(3):451–460
Park H, Kim PH, Hwang T, Kim J, Kim TI, Nam HY, Yockman JW, Kim M, Kim SW, Yun CO (2012) Fabrication of cross-linked alginate beads using electrospraying for adenovirus delivery. Int J Pharm 427(2):417–425
Park Y, Kang E, Kwon OJ, Hwang T, Park H, Lee JM, Kim JH, CO Y (2010) Ionically crosslinked Ad/chitosan nanocomplexes processed by electrospinning for targeted cancer gene therapy. J Control Release 148(1):75–82
Park Y, Kang E, Kwon OJ, Park HK, Kim JH, Yun CO (2010) Tumor targeted adenovirus nanocomplex ionically crosslinked by chitosan. J Control Release 148(1):e124
Kwon OJ, Kang E, Choi JW, Kim SW, Yun CO (2013) Therapeutic targeting of chitosan-PEG-folate-complexed oncolytic adenovirus for active and systemic cancer gene therapy. J Control Release 169(3):257–265
Lee CH, Kasala D, Na Y, Lee MS, Kim SW, Jeong JH, Yun CO (2014) Enhanced therapeutic efficacy of an adenovirus-PEI-bile-acid complex in tumors with low coxsackie and adenovirus receptor expression. Biomaterials 35(21):5505–5516
Choi JW, Nam JP, Nam K, Lee YS, Yun CO, Kim SW (2015) Oncolytic adenovirus coated with multidegradable bioreducible core-cross-linked polyethylenimine for cancer gene therapy. Biomacromolecules 16(7):2132–2143
Kim PH, Kim TI, Yockman JW, Kim SW, CO Y (2010) The effect of surface modification of adenovirus with an arginine-grafted bioreducible polymer on transduction efficiency and immunogenicity in cancer gene therapy. Biomaterials 31(7):1865–1874
Kim J, Nam HY, Kim TI, Kim PH, Jihoon R, Yun CO, Kim SW (2011) Active targeting of RGD-conjugated bioreducible polymer for delivery of oncolytic adenovirus expressing shRNA against IL-8 mRNA. Biomaterials 32(22):5158–5166
Kim PH, Sohn JH, Choi JW, Jung Y, Kim SW, Haam S, Yun CO (2011) Active targeting and safety profile of PEG-modified adenovirus conjugated with herceptin. Biomaterials 32(9):2314–2326
Choi JW, Kim J, Bui QN, Li Y, Chae-Ok Yun CO, Lee DS, Kim SW (2015) Tuning surface charge and PEGylation of biocompatible polymers for efficient delivery of nucleic acid or adenoviral vector. Bioconjug Chem 26(8):1818–1829
Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL (1987) Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 235(4785):177–182
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, Fleming T, Eiermann W, Wolter J, Pegram M, Baselga J, Norton L (2001) Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med 344(11):783–792
Grunwald GK, Vetter A, Klutz K, Kathrin K, Willhauck MJ, Schwenk N, Senekowitsch-Schmidtke R, Schwaiger M, Zach C, Wagner E, Göke B, Holm PS, Ogris M, Spitzweg C (2013) Systemic image-guided liver cancer radiovirotherapy using dendrimer-coated adenovirus encoding the sodium iodide symporter as theranostic gene. J Nucl Med 54(8):1450–1457
Grunwald GK, Vetter A, Klutz K, Willhauck MJ, Schwenk N, Senekowitsch- Schmidtke R, Schwaiger M, Zach C, Wagner E, Goke B, Holm PS, Ogris M, Spitzweg C (2013) EGFR-targeted adenovirus dendrimer coating for improved systemic delivery of the theranostic NIS gene. Mol Ther Nucleic Acids 2(11):e131. https://doi.org/10.1038/mtna.2013.58
Heise CC, Williams AM, Xue S, Propst M, Kirn DH (1999) Intravenous administration of ONYX-015, a selectively replicating adenovirus, induces antitumoral efficacy. Cancer Res 59(11):2623–2628
Liu TC, Galanis E, Kirn D (2007) Clinical trial results with oncolytic virotherapy: a century of promise, a decade of progress. Nat Clin Pract Oncol 4(2):101–117
Yamamoto M, Curiel DT (2010) Current issues and future directions of oncolytic adenoviruses. Mol Ther 18(2):243–250
Yotnda P, Chen DH, Chiu W, Piedra PA, Davis A, Templeton NS, Brenner MK (2002) Bilamellar cationic liposomes protect adenovectors from preexisting humoral immune responses. Mol Ther 5(3):233–241
Mendez N, Herrera V, Zhang L, Hedjran F, Feuer R, Blair SL, Trogler WC, Reid TR, Kummel AC (2014) Encapsulation of adenovirus serotype 5 in anionic lecithin liposomes using a bead-based immunoprecipitation technique enhances transfection efficiency. Biomaterials 35(35):9554–9561
Shin S, Shea LD (2010) Lentivirus immobilization to nanoparticles for enhanced and localized delivery from hydrogels. Mol Ther 18(4):700–706
Kidd ME, Shin S, Shea LD (2013) Fibrin hydrogels for lentiviral gene delivery in vitro and in vivo. J Control Release 157(1):80–85
Kim JS, Chu HS, Park KI, Won JI, Jang JH (2012) Elastin-like polypeptide matrices for enhancing adeno-associated virus mediated gene delivery to human neural stem cells. Gene Ther 19(3):329–337
Hwang JH, Lee S, Kim E, Kim JS, Lee CH, Ahn IS, Jang JH (2011) Heparin-coated superparamagnetic nanoparticle-mediated adeno-associated virus delivery for enhancing cellular transduction. Int J Pharm 421(2):397–404
Chrastina A, Massey KA, Schnitzer JE (2013) Overcoming in vivo barriers to targeted nanodelivery. Wiley Interdiscip Rev Nanomed Nanobiotechnol 3(4):421–437
Kunugi S, Yamaoka T, Akagi T, Baba M, Akashi M (2012) Biodegradable nanoparticles as vaccine adjuvants and delivery systems: regulation of immune responses by nanoparticle-based vaccine. In: Polymers in Nanomedicine. Springer, Berlin/Heidelberg, pp 31–64
Torchilin VP (2006) Multifunctional nanocarriers. Adv Drug Deliv Rev 58(14):1532–1555
Lee LA, Wang Q (2006) Adaptations of nanoscale viruses and other protein cages for medical applications. Nanomedicine 2(3):137–149
Champion JA, Mitragotri S (2006) Role of target geometry in phagocytosis. Proc Natl Acad Sci USA 103(13):4930–4934
Cubas R, Zhang S, Kwon S, Sevick-Muraca EM, Li M, Chen C, Yao Q (2009) Virus-like particle (VLP) lymphatic trafficking and immune response generation after immunization by different routes. J Immunother 32(2):118–128
Hubbell JA, Thomas SN, Swartz MA (2009) Materials engineering for immunomodulation. Nature 462(7272):449–460
Ravichandran P, Baluchamy S, Gopikrishnan R, Biradar S, Ramesh V, Goornavar V, Thomas R, Wilson BL, Jeffers R, Hall JC, Ramesh GT (2011) Pulmonary biocompatibility assessment of inhaled single-wall and multiwall carbon nanotubes in BALB/c mice. J Biol Chem 286(34):29725–29733
Shi J, Sun X, Lin Y, Zou X, Li Z, Liao Y, Du M, Zhang H (2014) Endothelial cell injury and dysfunction induced by silver nanoparticles through oxidative stress via IKK/NF-kappaB pathways. Biomaterials 35(24):6657–6666
Klippstein R, Pozo D (2010) Nanotechnology-based manipulation of dendritic cells for enhanced immunotherapy strategies. Nanomed Nanotechnol Biol Med 6(4):523–529
Reis e Sousa C (2006) Dendritic cells in a mature age. Nat Rev Immunol 6(6):476–483
Grewal IS, Flavell RA (1998) CD40 and CD154 in cell-mediated immunity. Annu Rev Immunol 16:111–135
Nair-Gupta P, Blander JM (2013) An updated view of the intracellular mechanisms regulating cross-presentation. Front Immunol 4:401
Kurts C, Robinson BW, Knolle PA (2010) Cross-priming in health and disease. Nat Rev Immunol 10(6):403–414
Huang L, Lemos HP, Li L, Li M, Chandler PR, Baban B, McGaha TL, Ravishankar B, Lee JR, Munn DH, Mellor AL (2012) Engineering DNA nanoparticles as immunomodulatory reagents that activate regulatory T cells. J Immunol 188(10):4913–4920
Jones SW, Roberts RA, Robbins GR, Perry JL, Kai MP, Chen K, Bo T, Napier ME, Ting JP, Desimone JM, Bear JE (2013) Nanoparticle clearance is governed by Th1/Th2 immunity and strain background. J Clin Invest 123(7):3061–3073
Howe SJ, Mansour MR, Schwarzwaelder K et al (2008) Insertional mutagenesis combined with acquired somatic mutations causes leukemogenesis following gene therapy of SCID-X1 patients. J Clin Invest 118(9):3143–3150
Frecha C, Szecsi J, Cosset FL, Verhoeyen E (2008) Strategies for targeting lentiviral vectors. Curr Gene Ther 8(6):449–460
Knight S, Collins M, Takeuchi Y (2013) Insertional mutagenesis by retroviral vectors: current concepts and methods of analysis. Curr Gene Ther 13(3):211–227
Chrastina A, Massey KA, Schnitzer JE (2011) Overcoming in vivo barriers to targeted nanodelivery. Wiley Interdiscip Rev Nanomed Nanobiotechnol 3(4):421–437
Gupta AS, Huang G, Lestini BJ, Sagnella S, Kottke-Marchant K, Marchant RE (2005) RGD-modified liposomes targeted to activated platelets as a potential vascular drug delivery system. Thromb Haemost 93(1):106–114
Huang G, Zhou Z, Srinivasan R, Penn MS, Kottke-Marchant K, Marchant RE, Gupta AS (2008) Affinity manipulation of surface-conjugated RGD peptide to modulate binding of liposomes to activated platelets. Biomaterials 29(11):1676–1685
Srinivasan R, Marchant RE, Gupta AS (2009) In vitro and in vivo platelet targeting by cyclic RGD-modified liposomes. J Biomed Mater Res A 93(3):1004–1015
Dabbas S, Kaushik RR, Dandamudi S, Kuesters GM, Campbell RB (2008) Importance of the liposomal cationic lipid content and type in tumor vascular targeting: physicochemical characterization and in vitro studies using human primary and transformed endothelial cells. Endothelium 15(4):189–201
Juliano RL, Hsu MJ, Peterson D, Regen SL, Singh A (1983) Interactions of conventional or photopolymerized liposomes with platelets in vitro. Exp Cell Res 146(2):422–427
Constantinescu I, Levin E, Gyongyossy-Issa M (2003) Liposomes and blood cells: a flow cytometric study. Artif Cells Blood Substit Immobil Biotechnol 31(4):395–424
Kwon YJ, Standley SM, Goh SL, Frechet JM (2005) Enhanced antigen presentation and immunostimulation of dendritic cells using acid-degradable cationic nanoparticles. J Control Release 105(3):199–212
Nordly P, Rose F, Christensen D, Nielsen HM, Andersen P, Agger EM, Foged C (2010) Immunity by formulation design: induction of high CD8+ T-cell responses by poly(I:C) incorporated into the CAF01 adjuvant via a double emulsion method. J Control Release 150(3):307–317
Lewis JS, Zaveri TD, Crooks CP, Keselowsky BG (2012) Microparticle surface modifications targeting dendritic cells for non-activating applications. Biomaterials 33(29):7221–7232
Hirota K, Hasegawa T, Nakajima T, Makino K, Terada H (2011) Phagostimulatory effect of uptake of PLGA microspheres loaded with rifampicin on alveolar macrophages. Colloids Surf B Biointerfaces 87(2):293–298
Liu Y, Fang Y, Zhou Y, Zandi E, Lee CL, Joo KI, Wang P (2013) Site-specific modification of adeno-associated viruses via a genetically engineered aldehyde tag. Small 9(3):421–429
Lee S, Kim JS, Chu HS, Kim GW, Won JI, Jang JH (2011) Electrospun nanofibrous scaffolds for controlled release of adeno-associated viral vectors. Acta Biomater 7(11):3868–3876
Lee WK, Park JY, Jung S, Ballester-Antxordoki L, Perez-Temprano N, Rojas E, Sanz D, Iglesias-Gaspar M, Moya S, Gonzalez-Fernandez A, Rey M (2005) Preparation and characterization of biodegradable nanoparticles entrapping immunodominant peptide conjugated with PEG for oral tolerance induction. J Control Release 105(1–2):77–88
Deb S, Patra HK, Lahiri P, Dasgupta AK, Chakrabarti K, Chaudhuri U (2011) Multistability in platelets and their response to gold nanoparticles. Nanomedicine 7(4):376–384
Lozano-Fernandez T, Ballester-Antxordoki L, Perez-Temprano N, Ballester-Antxordoki L, Perez-Temprano N, Rojas E, Sanz D, Iglesias-Gaspar M, Moya S, Gonzalez-Fernandez A, Rey M (2014) Potential impact of metal oxide nanoparticles on the immune system: the role of integrins, L-selectin and the chemokine receptor CXCR4. Nanomedicine 10(6):1301–1310
Corbalan JJ, Medina C, Jacoby A, Malinski T, Radomski MW (2011) Amorphous silica nanoparticles trigger nitric oxide/peroxynitrite imbalance in human endothelial cells: inflammatory and cytotoxic effects. Int J Nanomedicine 6:2821–2835
Liu X, Sun J (2010) Endothelial cells dysfunction induced by silica nanoparticles through oxidative stress via JNK/P53 and NF-kappaB pathways. Biomaterials 31(32):8198–8209
Pondman KM, Sobik M, Nayak A, Tsolaki AG, Jakel A, Flahaut E, Hampel S, Ten Haken B, Sim RB (2014) Kishore U complement activation by carbon nanotubes and its influence on the phagocytosis and cytokine response by macrophages. Nanomedicine 10(6):1287–1299
Walker VG, Li Z, Hulderman T, Schwegler-Berry D, Kashon ML, Simeonova PP (2009) Potential in vitro effects of carbon nanotubes on human aortic endothelial cells. Toxicol Appl Pharmacol 236(3):319–328
Radomski A, Jurasz P, Alonso-Escolano D, Drews M, Morandi M, Malinski T, Radomski MW (2005) Nanoparticle-induced platelet aggregation and vascular thrombosis. Br J Pharmacol 146(6):882–893
Barregard L, Sallsten G, Andersson L, Almstrand AC, Gustafson P, Andersson M, Olin AC (2008) Experimental exposure to wood smoke: effects on airway inflammation and oxidative stress. Occup Environ Med 65(5):319–324
Nemmar A, Hoet PH, Dinsdale D, Vermylen J, Hoylaerts MF, Nemery B (2003) Diesel exhaust particles in lung acutely enhance experimental peripheral thrombosis. Circulation 107(8):1202–1208
Dobrovolskaia MA, Patri AK, Potter TM, Rodriguez JC, Hall JB, McNeil SE (2011) Dendrimer-induced leukocyte procoagulant activity depends on particle size and surface charge. Nanomedicine 7(2):245–256
Li C, Hirsch M, DiPrimio N, Asokan A, Goudy K, Tisch R, Samulski RJ (2009) Cytotoxic-T-lymphocyte-mediated elimination of target cells transduced with engineered adeno-associated virus type 2 vector in vivo. J Virol 83(13):6817–6824
Pourazar J, Mudway IS, Samet JM, Helleday R, Blomberg A, Wilson SJ, Frew AJ, Kelly FJ, Sandstrom T (2005) Diesel exhaust activates redox-sensitive transcription factors and kinases in human airways. Am J Physiol Lung Cell Mol Physiol 289(5):L724–L730
Salvi S, Blomberg A, Rudell B, Kelly F, Sandstrom T, Holgate ST, Frew A. Acute inflammatory responses in the airways and peripheral blood after short-term exposure to diesel exhaust in healthy human volunteers. Am J Respir Crit Care Med 1999;159(3):702–709
Baulig A, Garlatti M, Bonvallot V, Marchand A, Barouki R, Marano F, Baeza-Squiban A (2003) Involvement of reactive oxygen species in the metabolic pathways triggered by diesel exhaust particles in human airway epithelial cells. Am J Physiol Lung Cell Mol Physiol 285(3):L671–L679
Alfaro-Moreno E, Nawrot TS, Nemmar A, Nemery B (2007) Particulate matter in the environment: pulmonary and cardiovascular effects. Curr Opin Pulm Med 13(2):98–106
Erdely A, Hulderman T, Salmen R, Liston A, Zeidler-Erdely PC, Schwegler-Berry D, Castranova V, Koyama S, Kim YA, Endo M, Simeonova PP (2009) Cross-talk between lung and systemic circulation during carbon nanotube respiratory exposure. Potential biomarkers. Nano Lett 9(1):36–43
Stasko NA, Johnson CB, Schoenfisch MH, Johnson TA, Holmuhamedov EL (2007) Cytotoxicity of polypropylenimine dendrimer conjugates on cultured endothelial cells. Biomacromolecules 8(12):3853–3859
Jones CF, Campbell RA, Franks Z, Gibson CC, Thiagarajan G, Vieira-de-Abreu A et al (2012) Cationic PAMAM dendrimers disrupt key platelet functions. Mol Pharm 9(6):1599–1611
Bartneck M, Peters FM, Warzecha KT, Warzecha KT, Bienert M, van Bloois L, Trautwein C, Lammers T, Tacke F (2013) Liposomal encapsulation of dexamethasone modulates cytotoxicity, inflammatory cytokine response, and migratory properties of primary human macrophages. Nanomedicine 10(6):1209–1220
Lonez C, Bessodes M, Scherman D, Vandenbranden M, Escriou V, Ruysschaert JM (2014) Cationic lipid nanocarriers activate toll-like receptor 2 and NLRP3 inflammasome pathways. Nanomedicine 10(4):775–782
Mayer A, Vadon M, Rinner B, Novak A, Wintersteiger R, Frohlich E (2009) The role of nanoparticle size in hemocompatibility. Toxicology 258(2–3):139–147
Dube A, Reynolds JL, Law WC, Maponga CC, Prasad PN, Morse GD (2014) Multimodal nanoparticles that provide immunomodulation and intracellular drug delivery for infectious diseases. Nanomedicine 10(4):831–838
Lowe KC, Akande SL, Bonnett R, White RD, Berenbaum MC (1992) Protective effects of a novel perfluorochemical emulsion in photodynamic therapy. Biomater Artif Cell Immobil Biotechnol 20(2–4):925–927
Vercellotti GM, Hammerschmidt DE, Craddock PR, Jacob HS (1982) Activation of plasma complement by perfluorocarbon artificial blood: probable mechanism of adverse pulmonary reactions in treated patients and rationale for corticosteroids prophylaxis. Blood 59(6):1299–1304
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Mahato, M., Jayandharan, G.R., Vemula, P.K. (2018). Viral- and Non-viral-Based Hybrid Vectors for Gene Therapy. In: Jayandharan, G. (eds) Gene and Cell Therapy: Biology and Applications. Springer, Singapore. https://doi.org/10.1007/978-981-13-0481-1_4
Download citation
DOI: https://doi.org/10.1007/978-981-13-0481-1_4
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-0480-4
Online ISBN: 978-981-13-0481-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)