Abstract
Symptom development in advanced castration-resistant prostate cancer (CRPC) patients can be attributed to local invasion of the tumor, metastasis to the bone, or compression of the spinal cord. Along the course of disease progression, 50–70% of the patients will eventually develop complications. Bone metastasis and consequent skeletal complications are the most common manifestations which may increase the risk of death from prostate cancer and decrease life quality. The clinical manifestations of bone metastasis include pain, skeletal-related events, and additional medical cost. Advancements in the understanding of the disease have resulted in the development of new palliation strategies. In this chapter, we examine several interventional options for local and systemic disease manifestation, bone-targeted palliative agents, and bone-targeted agents which potentially improve survival and management strategies for spinal cord compression. These treatments include various agents, namely, bisphosphonates, human monoclonal antibodies, and alpha- and beta-emitting radiopharmaceuticals.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Symptom development in advanced castration-resistant prostate cancer (CRPC) patients can be attributed to local invasion of the tumor, metastasis to the bone, or compression of the spinal cord. Along the course of disease progression, 50–70% of the patients will eventually develop complications. Bone metastasis and consequent skeletal complications are the most common manifestations which may increase the risk of death from prostate cancer and decrease life quality. The clinical manifestations of bone metastasis include pain, skeletal-related events, and additional medical cost. Advancements in the understanding of the disease have resulted in the development of new palliation strategies. In this chapter, we examine several interventional options for local and systemic disease manifestation, bone-targeted palliative agents, and bone-targeted agents which potentially improve survival and management strategies for spinal cord compression. These treatments include various agents, namely, bisphosphonates, human monoclonal antibodies, and alpha- and beta-emitting radiopharmaceuticals.
1.1 Pain Caused by Local Manifestation
Palliation of local symptoms and maintaining a good quality of life are major goals in the treatment landscape of symptomatic metastatic castration-resistant prostate cancer (mCRPC). Early diagnosis and intervention of local manifestations related to progression of the disease are important for maximizing quality of life.
1.1.1 Bladder Outlet and Ureteric Obstruction
Prostate enlargement or local bleeding may cause bladder outlet and/or ureteric obstruction. For the treatment of lower urinary tract symptoms (LUTS), transurethral resection of the prostate (TURP) with palliative purpose is a feasible option for symptoms intractable to medication [1]. Palliative radiotherapy is an alternative treatment for symptoms caused by bladder outlet obstruction with treatment efficacy reported in up to 63% of patients [1].
Ureteric obstruction can be caused by both tumor infiltration and compression [2, 3]. For symptomatic patients, urinary diversion should be considered to relieve the obstruction. For asymptomatic patients, urinary diversion can be considered for the less dilated and better functioning kidney. A nephrostomy catheter is superior to a JJ stent; however, ureteral stenting can be considered for patients desiring an internal diversion. Palliative radiotherapy is another option to relieve the obstruction with a response rate reported in up to 62% of patients.
1.1.2 Lymphedema
Patients with metastatic lymph nodes may present with lymphedema of the lower extremities. Supportive treatments including compressive stockings or pressure pumps may improve functional deficit and alleviate pain and discomfort.
1.1.3 Ileus
Ileus can be caused by local compression and obstruction of the rectum. Surgery and rectal stenting are options to relieve the mechanical obstruction. Laxatives may improve motility and reduce pain for paralytic ileus caused by tumor involvement of the nerve plexus or secondary constipation caused by opioid analgesics.
1.1.4 Neuropathy
Nerve plexopathies can be caused by extensive skull metastasis with cranial nerve involvement, direct pelvic tumor invasion, or by extensive liver metastasis. Complete neurological evaluation should be performed, followed by pharmacological pain management including tricyclic antidepressants (amitriptyline), anticonvulsants (gabapentin, pregabalin), or corticosteroids for cranial nerve involvement. Neurolytic procedures (nerve block) can be considered for neuropathies caused by direct tumor invasion. Discontinuation of neurotoxic drugs such as docetaxel or cabazitaxel can be considered for intractable symptoms.
1.2 Pain Caused by Bone Metastasis
Bone metastasis associated with prostate cancer (PCa) is predominantly a blastic feature, reflecting a predominance of osteoblastic activity [4]. Bone metastasis is the most common etiology of chronic pain in patients diagnosed with mCRPC, while more than 20% of patients with bone metastases do not suffer from pain [2, 5]. Painful areas shown on bone scan should be evaluated with plain x-rays or computed tomography imaging to exclude osteolytic lesions or pathologic fractures. This is more important when the painful area is at weight-bearing sites. The choice and initiation of interventional therapy should depend on the metastatic site and on the patient’s performance status. Therapeutic options should be tailored for each patient, preferably those with fewest side effects being the first-line option.
1.2.1 Single Lesion
1.2.1.1 Radiation Therapy
Palliation of focal bone pain, improvement in the quality of life, and the reduction of the risk of pain arising from sites to become symptomatic can be achieved with external beam localized radiation therapy [6]. There are various techniques, from higher doses given in less fractions to lower doses given over a longer period. The biological effect of radiotherapy depends on the total dose that is delivered, the number of treatment fractions, and the total period of the radiation. Stereotactic ablative radiation therapy is a novel radiation therapy which uses organ-limited approaches and has been reported with excellent outcomes. With radiation therapy, approximately 70% of the patients have been reported to achieve a complete relief of symptoms [7].
1.2.1.2 Orthopedic Surgery
Orthopedic surgery should be considered if more than half of the thickness of the bony cortex is involved in the metastasis [8, 9]. A sequential combination of radiofrequency and cementoplasty is a feasible option for painful osseous metastases [10].
1.2.2 Multiple Lesions
1.2.2.1 Systemic Analgesics
Nonsteroidal anti-inflammatory drugs alone can be used for chronic pain due to bone metastases. Dose escalation can be considered according to the response and side effects. Tramadol and dihydrocodeine extended-release tablets are commonly used agents. Morphine is the treatment of choice for moderate to severe degree pain. An alternative is hydromorphone; however, no clinically significant difference was shown when compared to morphine [11].
1.2.2.2 Bisphosphonates
Bisphosphonates, a class of drugs that is used to treat osteoporosis by preventing loss of bone mass, can be alternatively used as a supportive care for patients with pain caused by bone metastases. Bisphosphonates reduce bone resorption through the inhibition of osteoclastic activity and proliferation. Zoledronic acid is a potent bisphosphonate which reduces the frequency of skeleton-related events, delays the time to the first occurrence, and reduces pain compared with placebo [12, 13]. Moreover, zoledronic acid and pamidronate increase bone mineral density in men receiving long-term androgen deprivation therapy [14, 15]. Zoledronic acid is given at a dose of 4 mg intravenously every 4 weeks. Side effects include myalgia, fatigue, and anemia. Concomitant administration of oral calcium supplements and vitamin D is recommended owing to the possibility of hypocalcemia. A devastating complication of zoledronic acid is the osteonecrosis of the mandibular bone and consequent severe jaw pain. The benefit of other bisphosphonates, including etidronate, clodronate, ibandronate, and alendronate, has been studied in prospective randomized clinical trials; however, the efficacies of other bisphosphonates are inconclusive [16, 17].
1.2.2.3 Receptor Activator of Nuclear Factor-κB Ligand Inhibitors
Denosumab is a fully human monoclonal antibody against RANKL. Compared to zoledronic acid, denosumab has shown to improve the time to first skeletal-related events by 3.6 months and to prolong the time to first and subsequent skeletal-related events [18]. However, denosumab showed no benefits over other bone-targeted agents with regard to quality of life, pain management, progression-free survival, and overall survival. Toxicities of denosumab include nausea, fatigue, hypocalcemia, hypophosphatemia, and osteonecrosis of the jaw. Therefore, supplementary use of calcium and vitamin D is recommended. The recommended dose of denosumab is 120 mg administered subcutaneously every 4 weeks.
1.2.2.4 Radiopharmaceuticals
1.2.2.4.1 Beta Emitter
The beta emitters, strontium-89 (89Sr) and samarium-153 (153Sm), were historically the most commonly used radiopharmaceutical compounds [6, 19]. These agents were effective adjunctive therapies to local field radiotherapy, which improved progression-free survival and reduced the risks of future radiotherapy and analgesic support [19, 20]. With the improvement in the quality of life, 89Sr and 153Sm were both FDA approved for the palliative management of mCRPC; however, neither radiopharmaceutical demonstrated to improve overall survival.
1.2.2.4.2 Alpha Emitter
The alpha-emitting radiopharmaceutical, radium-223 (Ra-223), is a new concept radiopharmaceutical which delivers intense and highly localized radiation to the bone [21]. Alpha particles are approximately 7000 times heavier than beta particles, and one or two hits can induce cell death, in comparison with hundreds or thousands of hits required with beta particles. Moreover, alpha particles have a very short path length (<100 μm), by which surrounding the healthy bone can be maximally spared [22].
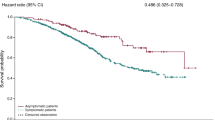
The ALSYMPCA trial was a randomized, double-blind, placebo-controlled phase III trial which compared Ra-223 versus placebo in men diagnosed with mCRPC without visceral or lymph node metastases [23]. Ra-223 was administered at a dose of 50 kBq/kg (intravenous) every 4 weeks for a total of six doses. Overall survival was improved by Ra-223 compared to placebo which resulted with a median survival improvement of 3.6 months. Moreover, Ra-223 showed benefit for secondary endpoints including time to first symptomatic skeletal event and quality of life. Based on the results of this trial, Ra-223 gained FDA approval for its use in patients with symptomatic bone metastatic CRPC.
1.3 Spinal Cord Compression
The collapse of a vertebral body or pressure exerted from a metastatic tumor within the spinal canal may cause spinal cord compression. The overall incidence of spinal cord compression in patients with prostate cancer is less than 10%, and the most common site is the thoracic cord. Early identification and intervention of spinal metastasis are important to preserve ambulatory ability and bladder and bowel function and to prevent and delay the onset of pain [24].
High-dose intravenous glucocorticoids should be the first therapeutic intervention in patients with suspected or documented spinal cord compression. The most commonly used agent is dexamethasone at daily doses from 16 to 100 mg. A loading dose of 10 mg followed by 4–10 mg every 6 h is administered. On improvement of symptoms, dose tapering may be performed throughout a 2–3-week period.
Definitive surgical intervention using spinal stabilization with anterior decompression or radiotherapy can be considered. Although radiotherapy is the mainstay of spinal cord compression, primary decompressive surgery could be considered for patients with compression at a single site, paraplegia of less than a 48-h period, tumors that are not radiosensitive, and patients’ survival that is predicted to be longer than 3 months [25]. This is evident from a report suggesting that decompressive surgery after radiotherapy could result with better surgical outcome compared to performing radiotherapy alone [26]. Treatment selection should depend on the overall prognosis of the patient and status of the underlying comorbidities.
2 Summary
-
1.
Early diagnosis and intervention of local symptoms in symptomatic mCRPC patients are essential in maintaining a good quality of life.
-
2.
The choice of treatment for bone metastasis should depend on the site and number of the pathology and on the patient’s physical condition. Therapeutic options include systemic analgesics, external beam radiation therapy, surgery, bisphosphonates, RANKL inhibitors, and radiopharmaceuticals, which should be tailored for each patient.
-
3.
Initial treatment for spinal cord compression symptom should include high-dose intravenous glucocorticoid injection. Definitive treatment with surgery or radiotherapy should then be considered.

Modified from EAU Guidelines on Pain Management & Palliative Care, 2014
References
Cameron MG, Kersten C, Guren MG, Fosså SD, Vistad I. Palliative pelvic radiotherapy of symptomatic incurable prostate cancer—a systematic review. Radiother Oncol. 2014;110(1):55–60.
Banning A, Sjogren P, Henriksen H. Pain causes in 200 patients referred to a multidisciplinary cancer pain clinic. Pain. 1991;45(1):45–8.
Nielsen OS, Munro AJ, Tannock IF. Bone metastases: pathophysiology and management policy. J Clin Oncol. 1991;9(3):509–24.
Roodman GD. Mechanisms of bone metastasis. N Engl J Med. 2004;350(16):1655–64.
Wagner G. Frequency of pain in patients with cancer. Recent Results Cancer Res. 1984;89:64–71.
Porter AT, McEwan AJ, Powe JE, Reid R, McGowan DG, Lukka H, et al. Results of a randomized phase-III trial to evaluate the efficacy of strontium-89 adjuvant to local field external beam irradiation in the management of endocrine resistant metastatic prostate cancer. Int J Radiat Oncol Biol Phys. 1993;25(5):805–13.
Tiedje LB, Kingry MJ, Stommel M. Patient attitudes concerning health behaviors during pregnancy: initial development of a questionnaire. Health Educ Q. 1992;19(4):481–93.
Pathological fractures due to bone metastases. Br Med J (Clin Res Ed). 1981;283(6294):748.
Galasko CS. The management of skeletal metastases. J R Coll Surg Edinb. 1980;25(3):144–61.
Lane MD, Le HB, Lee S, Young C, Heran MK, Badii M, et al. Combination radiofrequency ablation and cementoplasty for palliative treatment of painful neoplastic bone metastasis: experience with 53 treated lesions in 36 patients. Skelet Radiol. 2011;40(1):25–32.
Miles CL, Fellowes D, Goodman ML, Wilkinson S. Laxatives for the management of constipation in palliative care patients. Cochrane Database Syst Rev. 2006;18(4):CD003448.
Smith MR. Zoledronic acid to prevent skeletal complications in cancer: corroborating the evidence. Cancer Treat Rev. 2005;31(Suppl 3):19–25.
Saad F, Gleason DM, Murray R, Tchekmedyian S, Venner P, Lacombe L. Long-term efficacy of zoledronic acid for the prevention of skeletal complications in patients with metastatic hormone-refractory prostate cancer. J Natl Cancer Inst. 2004;96(11):879–82.
Smith MR, McGovern FJ, Zietman AL, Fallon MA, Hayden DL, Schoenfeld DA, et al. Pamidronate to prevent bone loss during androgen-deprivation therapy for prostate cancer. N Engl J Med. 2001;345(13):948–55.
Smith MR, Eastham J, Gleason DM, Shasha D, Tchekmedyian S, Zinner N. Randomized controlled trial of zoledronic acid to prevent bone loss in men receiving androgen deprivation therapy for nonmetastatic prostate cancer. J Urol. 2003;169(6):2008–12.
Berry S, Waldron T, Winquist E, Lukka H. The use of bisphosphonates in men with hormone-refractory prostate cancer: a systematic review of randomized trials. Can J Urol. 2006;13(4):3180–8.
Van den Wyngaert T, Huizing MT, Fossion E, Vermorken JB. Bisphosphonates in oncology: rising stars or fallen heroes. Oncologist. 2009;14(2):181–91.
Fizazi K, Carducci M, Smith M, Damião R, Brown J, Karsh L, et al. Denosumab versus zoledronic acid for treatment of bone metastases in men with castration-resistant prostate cancer: a randomised, double-blind study. Lancet. 2011;377(9768):813–22.
Sartor O, Reid RH, Hoskin PJ, Quick DP, Ell PJ, Coleman RE, et al. Samarium-153-Lexidronam complex for treatment of painful bone metastases in hormone-refractory prostate cancer. Urology. 2004;63(5):940–5.
Roqué I, Figuls M, Martinez-Zapata MJ, Scott-Brown M, Alonso-Coello P. Radioisotopes for metastatic bone pain. Cochrane Database Syst Rev. 2011;(7):CD003347.
Tu SM, Millikan RE, Mengistu B, Delpassand ES, Amato RJ, Pagliaro LC, et al. Bone-targeted therapy for advanced androgen-independent carcinoma of the prostate: a randomised phase II trial. Lancet. 2001;357(9253):336–41.
Henriksen G, Fisher DR, Roeske JC, Bruland ØS, Larsen RH. Targeting of osseous sites with alpha-emitting 223Ra: comparison with the beta-emitter 89Sr in mice. J Nucl Med. 2003;44(2):252–9.
Parker C, Nilsson S, Heinrich D, Helle SI, O’Sullivan JM, Fosså SD, et al. Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med. 2013;369(3):213–23.
Grossman SA, Lossignol D. Diagnosis and treatment of epidural metastases. Oncology (Williston Park). 1990;4(4):47–54; discussion 55,58.
George R, Jeba J, Ramkumar G, Chacko AG, Leng M, Tharyan P. Interventions for the treatment of metastatic extradural spinal cord compression in adults. Cochrane Database Syst Rev. 2015;9:CD006716.
Patchell RA, Tibbs PA, Regine WF, Payne R, Saris S, Kryscio RJ, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet. 2005;366(9486):643–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Koo, K.C. (2018). Palliative Care for Metastatic Symptomatic CRPC. In: Kim, C. (eds) Management of Advanced Prostate Cancer. Springer, Singapore. https://doi.org/10.1007/978-981-10-6943-7_25
Download citation
DOI: https://doi.org/10.1007/978-981-10-6943-7_25
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-6942-0
Online ISBN: 978-981-10-6943-7
eBook Packages: MedicineMedicine (R0)