Abstract
By providing rapid and broad surveys, radiologic imaging is an essential tool in modern medicine for the evaluation of trauma patients. Radiologic imaging may inform clinical diagnosis and the development of treatment strategies such as operation, angiointerventions, or conservative treatment.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
By providing rapid and broad surveys, radiologic imaging is an essential tool in modern medicine for the evaluation of trauma patients. Radiologic imaging may inform clinical diagnosis and the development of treatment strategies such as operation, angiointerventions, or conservative treatment.
Imaging modalities such as X-ray, ultrasonography (USG), computed tomography (CT), and magnetic resonance imaging (MRI) have unique advantages and disadvantages in the evaluation of trauma patients. Imaging strategies regarding when and which modalities are used depend on the proximity to the imaging facility, the availability of qualified imaging technicians to manage severely injured patients, and the presence of radiology experts to adjust imaging protocols according to individual cases, make interpretations, and provide reports. Generally, X-ray and USG can be used at the bedside of severely injured patients, even those with hemodynamically unstable conditions. CT offers objective findings of internal organ injury with a reasonable imaging acquisition time. MRI can be used for the evaluation of spinal cord, brain, or soft tissue injuries but is limited because of its long acquisition time and devices that can be affected by magnetic fields. Trauma clinicians should be aware of the merits and limitations of imaging modalities and provide proper imaging work-up.
This chapter discusses the general principals of radiologic imaging and the clinical application of each imaging modality based on the guidelines and recommendations.
9.1 General Principals of Imaging
-
1.
Trauma surgeons need to know the merits and limitations of each radiologic imaging modality (Table 9.1).
-
2.
Portable X-ray and USG should be available in the resuscitation room.
-
3.
Patient stay in the CT room should be as short as possible.
-
(a)
The CT room must be located near the resuscitation room.
-
(b)
The CT room must be emptied before patient arrival.
-
(c)
Trauma surgeons and imaging technicians must be trained for the patient’s safe movement to the CT table.
-
(d)
Radiologists have to manage the entire imaging process, from the individual patient-based protocol decision to the prompt interpretation.
-
(a)
9.2 Trauma Series of X-rays
X-ray is a useful tool for quick screening to assess the extent of traumatic injury. Even in unstable patients, portable X-ray can be used to exclude diseases that require immediate intervention such as tension pneumothorax, to diagnose injuries that may elicit life-threatening hemorrhage such as pelvic bone fracture, and to prevent further neurological deterioration such as C-spine dislocation. Therefore, a “trauma series of X-rays” comprising chest anteroposterior (AP), C-spine lateral, and pelvis AP is very useful for the initial evaluation of severely injured patients (Figs. 9.1, 9.2, 9.3, 9.4, 9.5, 9.6, and 9.7).
-
1.
Chest radiography
-
A.
Diseases that can be diagnosed with chest radiography
-
(i)
Pneumothorax, tension pneumothorax, hemothorax
-
(ii)
Pneumomediastinum, pneumopericardium, hemomediastinum
-
(iii)
Pulmonary contusion, aspiration pneumonitis
-
(iv)
Rib fracture, flail chest
-
(v)
Diaphragmatic rupture
-
(i)
-
B.
Check list
-
(i)
Airway of trachea and main bronchus
-
(ii)
Position and route of tubes and lines
-
(iii)
Visceral pleural line
-
(iv)
Lung parenchymal opacities
-
(v)
Mediastinal width and position
-
(vi)
Rib contiguity
-
(i)
-
A.
Chest radiography of a severely injured patient. In severely injured patients, there are many limitations to the proper interpretation of radiography, including chest radiography being performed in the anteroposterior direction in a bed-ridden state with a portable machine, with low lung volumes and increased mediastinal width. These may lead to misinterpretation of lung or mediastinal injuries. Shadows from the spine board, tubes, and electrode wires may interfere with the normal lines of lung markings, visceral pleura, and bony thorax. In this patient, pneumothorax (arrows) and multiple rib fracture (open arrows) are present but are not easy to detect because of the overlying instrument
Chest radiography of traumatic hemomediastinum and hemothorax. The chest radiography shows mediastinal widening (double-head arrow) that obscures the normal aortic knob contour and tracheal shifting to the right due to a mediastinal hematoma. The increased opacity of the left hemithorax with apical thickening (arrows) and left costophrenic angle blunting suggests hemothorax in this trauma patient
Chest radiography of tension pneumothorax. The chest radiography shows radiolucency in the left lower hemithorax with increased left hemithorax volume, resulting in widening of the intercostal space, downward shifting of the left hemidiaphragm, and mediastinal shifting to the right side. The heart is also shifted to the right side and shows a slender shape. These findings suggest tension pneumothorax requiring immediate intervention. In chest radiography performed in a supine position, free air of pneumothorax is located in the anteromedial aspect of hemithorax; therefore, the free visceral line may not be seen even though there is considerable pneumothorax
-
2.
C-spine lateral radiography
-
A.
Diseases that can be diagnosed with C-spine lateral radiography
-
(i)
C-spine fracture and/or dislocation
-
(ii)
Hematoma in prevertebral space
-
(iii)
Airway compromise of upper airway
-
(i)
-
B.
Check list
-
(i)
C-spine alignment and bony integrity
-
(ii)
Width of retropharyngeal soft tissue
-
(iii)
Airway of larynx and upper trachea
-
(i)
-
A.
Hangman’s fracture of C2. There is a complete fracture of the pars interarticularis of C2 (arrow), with mild anterior dislocation of the C2 body. The imaginary spinolaminal line is disrupted (curved line), and the interspinous distance (double-head arrow) is increased. There is also widening of the retropharyngeal soft tissue shadow (asterisk) at the C2/C3 level due to a fracture-related hematoma
-
3.
Pelvis AP radiography
-
A.
Disease that can be diagnosed with pelvis AP radiography
-
(i)
Pelvic bone fracture
-
(ii)
Prediction of bladder or urethral injury
-
(i)
-
B.
Check list
-
(i)
Bony integrity of sacrum and bilateral pelvic bones and femur
-
(ii)
Pelvic ring contiguity
-
(iii)
Hip joint and sacroiliac joint alignment
-
(i)
-
A.
9.3 Ultrasonography
Severely injured patients can be evaluated at the bedside by USG, so-called focused assessment with sonography in trauma (FAST), during the initial resuscitation in the emergency room owing to the improved portability and image quality of USG. Bedside USG can be easily performed anywhere and at any time and can provide critical real-time information about injured patients. In trauma situations, the role of FAST was initially confined to the detection of intraperitoneal (e.g., hemoperitoneum) and pericardial fluid, but its role has recently been extended to the evaluation of airway and thorax injuries (e.g., pneumothorax, hemothorax, etc.). Figure 9.7 illustrates the location of the standard FAST view. Originally, the standard view included four locations (the “four Ps”), namely, the pericardial, perihepatic (right upper quadrant), perisplenic (left upper quadrant), and pelvic areas (Fig. 9.8). These views allow the evaluation of sites where free fluid is more easily collected, identifying as little as 250 mL of free intraperitoneal fluid. USG can also be used to detect pneumothorax or hemothorax, referred to as extended FAST (E-FAST), by adding additional bilateral views of both hemithoraces (Fig. 9.9).
-
General Principles
-
FAST must be available 24 h a day in the resuscitation room.
-
Trauma surgeons, emergency medicine physicians, and radiologists must be trained to perform FAST appropriately.
-
-
Merits
-
Accessibility: bedside examination with portable USG
-
Real-time imaging with high temporal resolution
-
Non-radiation, noninvasive examination
-
Serial imaging for patient monitoring
-
-
Pitfalls
-
Dependent on operator skill and patient habitus.
-
Limited for solid organ and gastrointestinal tract, retroperitoneal, and diaphragm injuries.
-
Negative FAST results do not exclude the presence of intra-abdominal injury.
-
-
Interference due to intraperitoneal air.
-
False-positive results from nonhemorrhagic intraperitoneal fluid such as ascites secondary to other medical conditions (e.g., liver cirrhosis, renal failure, etc.) or urine due to urinary bladder rupture.
-
Four standard focused assessment with sonography in trauma (FAST) views. (a) Pericardial view can be obtained by placing a transducer at the subxiphoid position pointing toward the left shoulder. Anechoic pericardial fluid (*) is observed in the periphery of the left ventricle (LV) wall. (b) Prehepatic view at the right mid- to posterior axillary line of the intercostal space between the 11th and 12th ribs showing a small amount of anechoic fluid (arrows) in the Morrison’s pouch between the liver and right kidney. This location is the most common location of free fluid. (c) Perisplenic view at the left posterior axillary line of the intercostal space between the 10th and 11th ribs showing a large amount of free fluid (asterisk) around the spleen. (d) Pelvic view can be obtained by placing a transducer just superior to the symphysis pubis. This view allows the identification of the free fluid in the rectovesical (asterisk) and retrouterine spaces, the second most common locations of free fluid
Bilateral thoracic view for extended FAST (E-FAST). The thoracic view is usually obtained by placing a higher-frequency transducer in the 3rd or 4th intercostal space. In the normal thorax, “pleural sliding” and “comet-tail artifact” can be identified. “Pleural sliding” is the sliding motion of the visceral pleura (open arrows) against the inner margin of the thoracic wall (parietal pleura). A “comet-tail artifact” (arrows) is a hyperechogenic narrow-based reverberation artifact. If these findings are absent, pneumothorax should be considered
9.4 CT and MRI Work-Up in Trauma Patients
Trauma surgeons and emergency medicine physicians should determine the severity of trauma on the basis of initial imaging (X-ray, FAST), physical examination, and trauma mechanisms. According to this severity, selective CT, limiting the extent of CT exposure in the suspected anatomical region, or whole-body CT (WBCT) is performed selectively in trauma patients. However, the use of selective CT requires attention because of the limited reliability of physical examination in patients with low levels of consciousness or other significant injuries. There is also a risk of unnoticed injuries, particularly in seriously injured elderly patients with traumatic brain injury or visible vascular damage. Therefore, trauma clinicians should be aware of the indication and limitation of CT and MRI to avoid missing critical trauma and unnecessary testing that may delay appropriate treatment in trauma patients.
-
General Principles
-
CT scans should be performed only in hemodynamically stable patients. Trauma patients should be stabilized prior to radiographic studies, and clinicians should pay attention to potential spinal cord injuries and prevent further injuries during patient positioning and transfer for radiographic studies. Clinicians familiar with trauma care should accompany the patient to the CT room, as the patient may deteriorate rapidly.
-
CT scans of trauma patients should be completed at once, avoiding additional transfer and CT scans.
-
CT should be performed without performing X-rays if the X-rays might delay CT scans or operation in trauma patients.
-
The application of MRI to the investigation of trauma patients is limited because of the long image acquisition time and the difficulty in removing ferromagnetic material (i.e., foreign bodies and the use of life support devices) prior to testing.
-
9.4.1 Whole-Body CT for Severe Trauma Patients
9.4.1.1 Patient Selection Criteria for WBCT
Patient section criteria that requires WBCT in severe trauma patients [1] |
|---|
1. High-risk injury mechanism |
Traffic accidents |
Pedestrian/cyclist/motorcyclist hit by a vehicle |
Prolonged patient extrication (>15 min) |
Death of another passenger |
Ejection from the vehicle |
High-speed automobile collision |
Motorcycle accident |
Fall from >3 m, unknown height, stairs |
2. Evidence of anatomical injuries |
Visible injuries in two anatomical regions (head/neck/thorax/abdomen/pelvis/long bones) |
Sign of vascular damage (expansive hematoma, deep wound in arterial trajectory) |
Signs of spinal cord damage |
Unstable pelvic fracture |
Fractures of more than one long bone |
3. Vital signs |
Glasgow score < 12, intubated |
Systolic blood pressure < 100 mmHg |
Respiratory frequency: <10 or >30 rpm |
Pulse >120 bpm |
SatO2 < 90% |
Age > 65 years |
Anticoagulation |
-
General Principles
-
The British Royal College of Radiologists (RCR) has restricted the use of WBCT in severe trauma patients with an Injury Severity Score (ISS) > 15 [2]
-
WBCT quickly identifies life-threatening trauma lesions, including the presence of active bleeding and unexpected injuries, and can be used to assess the overall injuries of the trauma patient simultaneously.
-
WBCT is useful in severely injured patients with changes in mental status.
-
In comparison to conventional imaging in severe trauma patients, WBCT takes about one-quarter of the time to scan and reduces about half of the patient transfer [3].
-
WBCT results in more radiation exposure compared to that of selective CT, limiting the extent of radiation exposure in the suspected anatomical region in mild trauma patients, which can be an important consideration, especially in younger patients.
-
In the case of WBCT, one report indicated that traumatic injury was not identified in 30% of cases [4]; therefore, appropriate selection of trauma patients who require WBCT is needed.
-
9.4.1.2 Controversy Regarding the Application of WBCT
There is still some debate about the usefulness of WBCT. WBCT has the advantage of reducing the duration of intensive care unit (ICU) admission, reducing the duration of ventilation, decreasing the percentage of organ failure [5], inducing rapid discharge [6], and minimizing unrecognized damage at the beginning [7]. Some researchers claim that WBCT is useful in severely injured patients with changes in mental status. A retrospective database analysis of 5208 patients in Japan with Glasgow Coma Scale (GCS) scores ranging from 3 to 12 noted decreased mortality in patients who received WBCT scans [8]. However, an international, multicenter trial reported that in-hospital mortality did not differ between WBCT and conventional imaging work-up or between patients with polytrauma and those with traumatic brain injury [9]. Therefore, additional studies on the usefulness and cost-effectiveness of WBCT are needed.
9.4.2 Selective CT for Trauma Patients
9.4.2.1 Head Trauma
1. GCS < 15 two hours post injury |
2. Suspected open skull fracture |
3. Sign of skull base fracture Hemotympanum Raccoon eyes (intraorbital bruising) Battle sign (retroauricular bruising) Cerebrospinal fluid leak, oto- or rhinorrhea |
4. Vomiting more than twice |
5. Age ≥ 60 years |
6. Amnesia post event >30 min |
7. Dangerous mechanism of injury Pedestrian struck by motor vehicle Occupant ejected from motor vehicle Fall from >3 feet or 5 stairs |
8. Neurological deficit |
9. Seizure |
10. Blood thinner (oral anticoagulant use or bleeding diathesis) |
11. Return visit for reassessment of a head injury |
The clinical criteria were based on clinical criteria validated in three prospective studies: the Canadian CT head rule (CCHR) [10], the New Orleans Criteria (NOC) [11], and the National Emergency X-Radiography Utilization Study II (NEXUS II) [12]. These three clinical criteria have high sensitivity for patients with clinically significant CT findings and have the effect of reducing the number of CT examinations performed.
The sensitivities of the three clinical criteria for the identification of brain damage requiring neurological intervention were 100% (NOC), 100% (CCHR), and 95% (NEXUS II). The sensitivities of these clinical criteria for the identification of clinically significant brain injury without neurological intervention were 92%, 79%, and 89%, respectively. The sensitivity to clinical outcomes was highest in the NOC. However, the specificity of these criteria was very low, at less than 50%, and lowest in the NOC (<25%) [13].
9.4.2.2 Blunt Cerebrovascular Injury (BCVI)
Patient section criteria that requires CTA for screening BCVI [14,15,16] |
|---|
1. Unexplained neurological sign and symptom |
Arterial hemorrhage from the neck, mouth, nose, or ear Cervical hematoma Cervical bruit in a patient younger (<50 years) Focal or lateralizing neurological deficit |
2. Injury mechanism (severe cervical hyperextension/rotation or hyperflexion) |
3. Severe facial trauma (bilateral facial fractures, complex midface, subcondylar fractures) |
4. Basilar skull fracture involving carotid canal |
5.Cervical vertebral body fracture, transverse foramen fracture, subluxation, or ligamentous injury at any level or any fracture at the level of C1–C3 |
6. Diffuse axonal brain injury (closed head injury with GCS < 6) |
7. Near-hanging resulting in cerebral anoxia |
8. Clothesline-type injury or seat belt abrasion with significant cervical pain, swelling, or altered mental status |
These criteria have clinical signs, symptoms, or risk factors that suggest BCVI. The risk factors listed above are based on the Eastern and Western Trauma Associations of the United States, which are used to screen for patients with no symptoms [14,15,16]. Computed tomographic angiography (CTA) is the screening test of choice in patients with suspected BCVI in an emergency. The sensitivity and specificity of CTA vary depending on the CT equipment. A study using four- and eight-slice scanners showed 83–92% sensitivity and 88–92% specificity for blunt carotid injuries and 50–60% sensitivity and 90–97% specificity for blunt vertebral injury [17]. A 16-slice scanner study showed lesion detection equivalent to that of digital subtraction angiography [18]. A recent study showed that WBCT with a single dose of contrast agent may be as accurate as CTA for the diagnosis of BCVI [19].
-
General Principles
-
Patients with BCVI initially have no symptoms but develop stroke symptoms about one day later [20].
-
BCVI occurs in 30–37% of patients with multiple trauma who do not meet the BCVI screening criteria [21]. Therefore, it is necessary to carefully evaluate WBCT images in severe trauma patients, always considering the possibility of BCVI, even if it is not the case for these indications.
-
Bilateral cerebrovascular injuries are common, occurring in 18–25% of patients [22].
-
Carotid injuries occur more frequently than vertebral injuries [23].
-
BCVI may occur in the contralateral vessel as well as in the ipsilateral vessel in the injured area of the head and neck due to vessel sharing injuries, requiring caution in image analysis [23]. Therefore, in patients with BCVI or blunt neck trauma, it is necessary to carefully evaluate both vessels of the neck (Figs. 9.10 and 9.11).
-
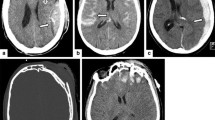
BCVI (blunt cerebrovascular injury) in a major trauma patient. (a) Cervical spinal CT shows a fracture of the cervical spine across the left transverse foramen. (b) CT angiography shows a left vertebral artery occlusion. (c) Diffusion-weighted images show acute infarct in the left cerebellar hemisphere
9.4.2.3 Cervical Spine Injury
Patient section criteria that requires cervical spinal CT [24, 25] |
|---|
1. Dangerous mechanism of injury (high-speed motor vehicle collision, fall from height including diving, rollover motor accident, bicycle collision) |
2. Death at scene of motor vehicle crash |
3. Significant closed head injury or intracranial hemorrhage seen on CT |
4. Neurologic symptoms or sign referred to the cervical spine |
5. Pelvic or multiple extremity fractures |
6. Multi-region trauma |
7. Technically inadequate plain X-ray |
8. Suspicious or definitely abnormal plain X-ray |
9. Age ≥ 60 years |
-
General Principles
-
Cervical spinal CT should be performed in patients with severe trauma, those at high risk, or those with changes in mental status.
-
There is insufficient evidence to replace plain radiography with CT as the initial screening method in lower-risk patients.
-
It may be necessary to perform cervical spinal CT if it is difficult to obtain a technically appropriate image by plain radiography. A retrospective study of blunt trauma patients showed that 72% of plain radiography images were inadequate to view the entire cervical spine [26]. In addition, insufficient images are often obtained in severe trauma patients due to blunt trauma, and misdiagnosis of cervical spinal fractures are reported in up to 16% of cases [27].
-
It may be preferable to perform cervical spinal CT in elderly patients because the interpretation of plain radiography may be difficult in elder trauma patients [28].
-
9.4.2.4 Thoracic, Lumbar, and Sacral (TLS) Spinal Injury
Patient section criteria that requires TLS spinal CT [29,30,31,32] |
|---|
1. Suspicious or definitely abnormal plain X-ray |
2. Signs of injury or neurological deficit in the thoracic or lumbosacral regions |
3. New another spine injury, particularly a known cervical fracture |
4. High-energy mechanism (fall ≥3 m, ejection from a vehicle, motor vehicle rack, forceful direct blow) |
5. Patient (age ≥ 60 years) with sign/symptom or mechanism causing TLS spine injury |
6. Depressed metal status (GCS < 15 or signs of intoxication) with sign/symptom or mechanism causing TLS spine injury |
-
General Principles
-
According to the Eastern Association for the Surgery of Trauma practice guidelines, there is no need to perform an imaging test on the TLS spine in blunt trauma patients with normal mental status and no risks [31].
-
In addition to physical examination, it is necessary to consider the traumatic mechanism when selecting patients who require CT examination because there are limitations in the physical examinations. In one large prospective study, TLS spine injuries requiring surgical treatment were found in more than 20% of patients with normal physical examinations [32].
-
TLS spinal CT may still be required despite an unremarkable physical examination.
-
However, reformatted thoracic and abdominal CT images in severe trauma patients may be sufficient to assess most TLS spine injuries and do not require additional TL spine administration [33].
-
9.4.2.5 Thoracic Injury
Patient section criteria that requires thoracic CT |
|---|
1. Severe trauma patients |
2. Mild trauma patient with following risk factors Abnormal plain chest radiograph despite the absence of obvious clinical signs of injury |
Concerning clinical findings (e.g., severe pain or marked chest tenderness, hypoxia, dyspnea, tachypnea) with normal chest radiography |
High-energy mechanism |
Generally, chest CT is unnecessary in trauma patients with low-energy mechanisms of injury, minimal injury on physical examination, and normal chest radiography findings [34]. However, observational studies have shown clinically significant chest trauma on chest CT in trauma patients with normal chest radiography, although these studies included only a small number of patients [35]. Conversely, abnormal findings in simple chest radiography suggest clinically significant chest trauma [36].
There is conflicting evidence regarding the need for chest CT in trauma patients with high-energy mechanisms of injury; however, chest CT is generally preferred. In one prospective study, although there was no external sign of thoracic injury in 592 hemodynamically stable patients with a significant injury mechanism, clinically significant findings were found in 19.6% of chest CTs [37]. In a prospective study of 609 blunt trauma patients, clinically significant findings were found in 11% of chest CT cases in which emergency physicians determined that CT was unnecessary [38].
The NEXUS is a prospectively validated decision instrument to determine the need for chest CT in trauma patients [39, 40].
Types | Criteria factors | Accuracy |
|---|---|---|
NEXUS decision instrument (earlier iteration) [39] | Age > 60 years Chest pain Intoxication Abnormal alertness or mental status Chest wall tenderness Distracting painful injury Rapid deceleration mechanism | Sensitivity (98.8%) and specificity (13.3%) percent for any thoracic injury seen on chest imaging (If all criteria are absent, the patient has a very low risk for intrathoracic injury and chest imaging is not indicated) |
NEXUS decision instrument (Chest CT-All) [40] | Chest wall tenderness Distracting painful injury Rapid deceleration mechanism Abnormal plain chest radiograph Sternal tenderness Thoracic spine tenderness Scapular tenderness | Sensitivity (99.2%), specificity (20.8%), and negative predictive value (NPV) (99.8%) for major injury Sensitivity (95.4%), specificity (25.5%), and a NPV (93.9%) for either major or minor injury |
NEXUS decision instrument (chest CT-majora) [40] | Chest wall tenderness Distracting painful injury Abnormal plain chest radiograph Sternal tenderness Thoracic spine tenderness Scapular tenderness | Sensitivity (99.2%), specificity (31.7%), and a NPV (99.9%) for major injury |
The application of these criteria would reduce unnecessary chest CT. However, when applying the NEXUS criteria to trauma patients, it is important to note the presence of any one criteria factor represents a low rate of major clinical injury, so clinicians should discuss the potential risks and benefit of chest CT in these cases. However, in the patient with an abnormal chest X-ray, the risks of major clinical injury and minor injury are considerably higher than with the other criteria [36].
-
General Principales
-
Chest CT should be performed in cases of abnormal chest radiography findings in mild trauma patients and clinically suspicious cases with normal chest radiography findings.
-
Chest CT should be performed if the clinician suspects chest injury regardless of the criteria. The clinician should lower the threshold for performing an imaging test for a chest injury.
-
9.4.2.6 Abdominal Injury
Patient section criteria that requires abdominal CT [41, 42] |
|---|
1. Physical examination findings |
Seat belt sign |
Rebound tenderness |
Hypotension |
Abdominal distension |
Abdominal guarding |
Severe distracting injury (e.g., femur fracture) |
2. The presence of an altered sensorium or painful extra-abdominal injuries, even in the absence of suggestive symptoms or signs |
3. Abnormal chest radiograph suggesting intra-abdominal injury (lower rib fractures, diaphragmatic hernia, free air under the diaphragm) |
4. Fracture involving the pelvic ring |
5. History features |
Fatality at the scene |
Vehicle type and velocity |
Whether the vehicle rolled over |
Patient’s location within the vehicle |
Extent of intrusion into the passenger compartment |
Extent of damage to the vehicle; steering wheel deformity |
Whether seat belts were used and what type (unrestrained victims are at higher risk of injury); whether air bags deployed |
6. Age > 60 |
Emergency and trauma clinicians managing blunt trauma should maintain a high clinical suspicion of intra-abdominal injuries, especially in patients with suggestive trauma mechanisms, signs of external trauma, and altered sensorium due to head injury and intoxication. Up to 10% of isolated head injury patients may have an intra-abdominal injury [43]. According to one prospective observational study, approximately 7% of blunt trauma patients with distracting extra-abdominal injuries have intra-abdominal injuries despite the absence of signs or symptoms suggestive of abdominal injuries [44]. Patients with fractures of the pelvic ring should also be suspected of intra-abdominal injury. Abdominal injuries are observed in up to 16.5% of patients with pelvic bone fractures [45]. Both visceral organs (i.e., liver and spleen) and the bowels can be involved in the damage [42, 45].
-
General Principles
-
Abdominal pain and tenderness increase the likelihood of intra-abdominal injuries; however, the negative likelihood ratio for each is low, and the absence of these findings cannot exclude abdominal injuries.
-
Clinicians should maintain a high index of suspicion for intra-abdominal injuries especially in those patients older than 60 years of age since the signs and symptoms of abdominal injuries often appear to be weakened.
-
Altered sensorium or painful extra-abdominal injuries increase the likelihood of intra-abdominal injuries even in the absence of symptoms or signs suggestive of abdominal injuries.
-
9.4.3 MRI Work-Up for Trauma Patients
9.4.3.1 MRI for Head Trauma
MRI is not a first-line imaging study in the initial examination of patients with head trauma. It is difficult to perform MRI in emergency situations. Long scan times and multiple devices are limiting factors in performing MRI. MRI is more sensitive than CT for the detection of parenchymal, subdural, and epidural hemorrhages, as well as contusion, brainstem injury including posterior fossa, and diffusion axonal injury [46, 47]. In acute mild traumatic brain injury patients, abnormal MRI findings are reported in 30% of normal CT patients [46, 47]. Most of these findings were axonal injuries but also included small contusions and subarachnoid hemorrhage. Both brain contusion and hemorrhagic axonal injury are associated with poor 3-month outcomes [47]. In head trauma patients, selective MRI is useful in patients with unexplained neurological deficits or in patients who do not recover as expected.
-
General Principle
-
If the trauma patient has a severe neurologic abnormality with normal CT findings at the initial examination, the patient is judged to have an axonal or brainstem injury, and MRI should be performed after emergency operation and treatment.
-
9.4.3.2 MRI for Spinal Column Injury
MRI is more useful than CT for the evaluation of spinal cord integrity, intervertebral discs, soft tissues, and ligamentous structures around the vertebra and is more sensitive to the detection of epidural hematoma than CT [48]. Traumatic spinal cord injury (TSCI) is found in MRI scans in 5.8% of cases with negative CT scans [49]. However, it is difficult to perform MRI in the initial examination of trauma patients because of metallic foreign bodies and lift-supporting equipment as well as cardiac pacemakers in trauma patients. In addition, it may be difficult to monitor patient vital signs during MRI.
-
General Principles
-
MRI should be performed when the clinical condition of the patient is suitable for performing MRI, if spinal cord injury is suspected or occult spinal injury is suspected in patients with normal CT findings.
-
The high incidence of multiple vertebral injuries means that whole-spine MRI scans should be performed [50].
-
9.5 Summary
-
1.
Trauma clinicians should aware of the merits, limitations, and indications for imaging.
-
2.
Portable X-ray and USG should be available in the resuscitation room.
-
3.
A “trauma series of X-rays” comprising chest AP (anteroposterior), C-spine lateral, and pelvis AP views is very useful for the initial evaluation of severely injured patients.
-
4.
Trauma clinicians can skip X-rays if it might delay the CT scan or operation in trauma patients.
-
5.
CT scans should be performed only in hemodynamically stable patients.
-
6.
CT scans of trauma patients should be completed all at once to avoid additional transfer and CT scans.
-
7.
WBCT quickly identifies life-threatening trauma lesions in severe trauma patient all at once.
-
8.
The application of MRI for the initial evaluation of trauma patients is limited because of the long image acquisition time and the difficulty of removing ferromagnetic material.
-
9.
Discrepancies between the neurologic abnormalities and head CT findings in trauma patients suggest axonal injury and follow-up MRI of the brain should be performed after emergency operation.
-
10.
The high incidence of multiple vertebral injuries means that whole-spine scans should be performed.
References
Artigas Martin JM, Marti de Gracia M, Claraco Vega LM, Parrilla Herranz P. Radiology and imaging techniques in severe trauma. Med Intensiva. 2015;39(1):49–59.
RCR. Standards of practice and guidance for trauma radiology in severely injured patient. London: Royal College of Radiologist; 2011.
Saltzherr TP, Bakker FC, Beenen LF, Dijkgraaf MG, Reitsma JB, Goslings JC. Randomized clinical trial comparing the effect of computed tomography in the trauma room versus the radiology department on injury outcomes. Br J Surg. 2012;99(Suppl 1):105–13.
Harvey JJ, West AT. The right scan, for the right patient, at the right time: the reorganization of major trauma service provision in England and its implications for radiologists. Clin Radiol. 2013;68(9):871–86.
Weninger P, Mauritz W, Fridrich P, et al. Emergency room management of patients with blunt major trauma: evaluation of the multislice computed tomography protocol exemplified by an urban trauma center. J Trauma. 2007;62(3):584–91.
Livingston DH, Lavery RF, Passannante MR, et al. Admission or observation is not necessary after a negative abdominal computed tomographic scan in patients with suspected blunt abdominal trauma: results of a prospective, multi-institutional trial. J Trauma. 1998;44(2):273–80; discussion 80–2.
Geyer LL, Korner M, Linsenmaier U, et al. Incidence of delayed and missed diagnoses in whole-body multidetector CT in patients with multiple injuries after trauma. Acta Radiol. 2013;54(5):592–8.
Kimura A, Tanaka N. Whole-body computed tomography is associated with decreased mortality in blunt trauma patients with moderate-to-severe consciousness disturbance: a multicenter, retrospective study. J Trauma Acute Care Surg. 2013;75(2):202–6.
Sierink JC, Treskes K, Edwards MJ, et al. Immediate total-body CT scanning versus conventional imaging and selective CT scanning in patients with severe trauma (REACT-2): a randomised controlled trial. Lancet. 2016;388(10045):673–83.
Stiell IG, Wells GA, Vandemheen K, et al. The Canadian CT head rule for patients with minor head injury. Lancet. 2001;357(9266):1391–6.
Haydel MJ, Preston CA, Mills TJ, Luber S, Blaudeau E, DeBlieux PM. Indications for computed tomography in patients with minor head injury. N Engl J Med. 2000;343(2):100–5.
Mower WR, Hoffman JR, Herbert M, Wolfson AB, Pollack CV Jr, Zucker MI. Developing a decision instrument to guide computed tomographic imaging of blunt head injury patients. J Trauma. 2005;59(4):954–9.
Ro YS, Shin SD, Holmes JF, et al. Comparison of clinical performance of cranial computed tomography rules in patients with minor head injury: a multicenter prospective study. Acad Emerg Med. 2011;18(6):597–604.
Biffl WL, Cothren CC, Moore EE, et al. Western Trauma Association critical decisions in trauma: screening for and treatment of blunt cerebrovascular injuries. J Trauma. 2009;67(6):1150–3.
Bromberg WJ, Collier BC, Diebel LN, et al. Blunt cerebrovascular injury practice management guidelines: the eastern Association for the Surgery of trauma. J Trauma. 2010;68(2):471–7.
Mundinger GS, Dorafshar AH, Gilson MM, Mithani SK, Manson PN, Rodriguez ED. Blunt-mechanism facial fracture patterns associated with internal carotid artery injuries: recommendations for additional screening criteria based on analysis of 4,398 patients. J Oral Maxillofacial Surg. 2013;71(12):2092–100.
Bub LD, Hollingworth W, Jarvik JG, Hallam DK. Screening for blunt cerebrovascular injury: evaluating the accuracy of multidetector computed tomographic angiography. J Trauma. 2005;59(3):691–7.
Berne JD, Reuland KS, Villarreal DH, McGovern TM, Rowe SA, Norwood SH. Sixteen-slice multidetector computed tomographic angiography improves the accuracy of screening for blunt cerebrovascular injury. J Trauma. 2006;60(6):1204–9; discussion 1209–10.
Sliker CW, Shanmuganathan K, Mirvis SE. Diagnosis of blunt cerebrovascular injuries with 16-MDCT: accuracy of whole-body MDCT compared with neck MDCT angiography. AJR Am J Roentgenol. 2008;190(3):790–9.
Cothren CC, Moore EE, Ray CE, et al. Screening for blunt cerebrovascular injuries is cost-effective. Am J Surg. 2005;190(6):849–54.
Jacobson LE, Ziemba-Davis M, Herrera AJ. The limitations of using risk factors to screen for blunt cerebrovascular injuries: the harder you look, the more you find. World J Emerg Surg. 2015;10:46.
Edwards NM, Fabian TC, Claridge JA, Timmons SD, Fischer PE, Croce MA. Antithrombotic therapy and endovascular stents are effective treatment for blunt carotid injuries: results from long-term follow-up. J Am Coll Surg. 2007;204(5):1007–13.
Biffl WL, Ray CE Jr, Moore EE, et al. Treatment-related outcomes from blunt cerebrovascular injuries: importance of routine follow-up arteriography. Ann Surg. 2002;235(5):699.
Hanson JA, Blackmore CC, Mann FA, Wilson AJ. Cervical spine injury: a clinical decision rule to identify high-risk patients for helical CT screening. AJR Am J Roentgenol. 2000;174(3):713–7.
Amy Kaji RSH. Evaluation and acute management of cervical spinal column injuries in adults. UpToDate; 2017.
Gale SC, Gracias VH, Reilly PM, Schwab CW. The inefficiency of plain radiography to evaluate the cervical spine after blunt trauma. J Trauma Acute Care Surg. 2005;59(5):1121–5.
Widder S, Doig C, Burrowes P, Larsen G, Hurlbert RJ, Kortbeek JB. Prospective evaluation of computed tomographic scanning for the spinal clearance of obtunded trauma patients: preliminary results. J Trauma Acute Care Surg. 2004;56(6):1179–84.
Greenbaum J, Walters N, Levy PD. An evidenced-based approach to radiographic assessment of cervical spine injuries in the emergency department. J Emerg Med. 2009;36(1):64–71.
Hsu JM, Joseph T, Ellis AM. Thoracolumbar fracture in blunt trauma patients: guidelines for diagnosis and imaging. Injury. 2003;34(6):426–33.
O’Connor E, Walsham J. Review article: indications for thoracolumbar imaging in blunt trauma patients: a review of current literature. Emerg Med Australas. 2009;21(2):94–101.
Sixta S, Moore FO, Ditillo MF, et al. Screening for thoracolumbar spinal injuries in blunt trauma: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012;73(5 Suppl 4):S326–32.
Inaba K, Nosanov L, Menaker J, et al. Prospective derivation of a clinical decision rule for thoracolumbar spine evaluation after blunt trauma: an American Association for the Surgery of Trauma Multi-Institutional Trials Group Study. J Trauma Acute Care Surg. 2015;78(3):459–65; discussion 65–7.
Kim S, Yoon CS, Ryu JA, et al. A comparison of the diagnostic performances of visceral organ-targeted versus spine-targeted protocols for the evaluation of spinal fractures using sixteen-channel multidetector row computed tomography: is additional spine-targeted computed tomography necessary to evaluate thoracolumbar spinal fractures in blunt trauma victims? J Trauma. 2010;69(2):437–46.
Kea B, Gamarallage R, Vairamuthu H, et al. What is the clinical significance of chest CT when the chest x-ray result is normal in patients with blunt trauma? Am J Emerg Med. 2013;31(8):1268–73.
Brink M, Deunk J, Dekker HM, et al. Added value of routine chest MDCT after blunt trauma: evaluation of additional findings and impact on patient management. AJR Am J Roentgenol. 2008;190(6):1591–8.
Raja AS, Mower WR, Nishijima DK, et al. Prevalence and diagnostic performance of isolated and combined NEXUS chest CT decision criteria. Acad Emerg Med. 2016;23(8):863–9.
Salim A, Sangthong B, Martin M, Brown C, Plurad D, Demetriades D. Whole body imaging in blunt multisystem trauma patients without obvious signs of injury: results of a prospective study. Arch Surg. 2006;141(5):468–75.
Gupta M, Schriger DL, Hiatt JR, et al. Selective use of computed tomography compared with routine whole body imaging in patients with blunt trauma. Ann Emerg Med. 2011;58(5):407–16.e15.
Rodriguez RM, Anglin D, Langdorf MI, et al. NEXUS chest: validation of a decision instrument for selective chest imaging in blunt trauma. JAMA Surg. 2013;148(10):940–6.
Rodriguez RM, Langdorf MI, Nishijima D, et al. Derivation and validation of two decision instruments for selective chest CT in blunt trauma: a multicenter prospective observational study (NEXUS Chest CT). PLoS Med. 2015;12(10):e1001883.
Nishijima DK, Simel DL, Wisner DH, Holmes JF. Does this adult patient have a blunt intra-abdominal injury? JAMA. 2012;307(14):1517–27.
Cannada LK, Taylor RM, Reddix R, Mullis B, Moghadamian E, Erickson M. The Jones-Powell classification of open pelvic fractures: a multicenter study evaluating mortality rates. J Trauma Acute Care Surg. 2013;74(3):901–6.
Schurink G, Bode P, Van Luijt P, Van Vugt A. The value of physical examination in the diagnosis of patients with blunt abdominal trauma: a retrospective study. Injury. 1997;28(4):261–5.
Ferrera PC, Verdile VP, Bartfield JM, Snyder HS, Salluzzo RF. Injuries distracting from intraabdominal injuries after blunt trauma. Am J Emerg Med. 1998;16(2):145–9.
Demetriades D, Karaiskakis M, Toutouzas K, Alo K, Velmahos G, Chan L. Pelvic fractures: epidemiology and predictors of associated abdominal injuries and outcomes. J Am Coll Surg. 2002;195(1):1–10.
Hughes DG, Jackson A, Mason DL, Berry E, Hollis S, Yates DW. Abnormalities on magnetic resonance imaging seen acutely following mild traumatic brain injury: correlation with neuropsychological tests and delayed recovery. Neuroradiology. 2004;46(7):550–8.
Yuh EL, Mukherjee P, Lingsma HF, et al. Magnetic resonance imaging improves 3-month outcome prediction in mild traumatic brain injury. Ann Neurol. 2013;73(2):224–35.
Goldberg AL, Kershah SM. Advances in imaging of vertebral and spinal cord injury. J Spinal Cord Med. 2010;33(2):105–16.
Schoenfeld AJ, Bono CM, McGuire KJ, Warholic N, Harris MB. Computed tomography alone versus computed tomography and magnetic resonance imaging in the identification of occult injuries to the cervical spine: a meta-analysis. J Trauma Acute Care Surg. 2010;68(1):109–14.
Barron D. (ii) Polytrauma imaging–the role of integrated imaging. Orthop Trauma. 2011;25(2):83–90.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Hong, GS., Lee, C.W. (2019). The Role of Radiology in Trauma Patients. In: Hong, SK., Kim, D., Jeon, S. (eds) Primary Management of Polytrauma . Springer, Singapore. https://doi.org/10.1007/978-981-10-5529-4_9
Download citation
DOI: https://doi.org/10.1007/978-981-10-5529-4_9
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-5528-7
Online ISBN: 978-981-10-5529-4
eBook Packages: MedicineMedicine (R0)