Abstract
Spinal stenosis is the most common disorder of the lumbar spine in elderly patients (Deyo et al., Spine 18:1463–70,193). Decompressive surgery is currently the best choice in the treatment for symptomatic lumbar spinal stenosis (Weinstein et al., N Engl J Med 358:794–810, 2008). Percutaneous endoscopic decompression (PED) in progression has become a reasonable alternative to open microsurgery for lumbar spinal stenosis (Thongtrangan et al., Neurosurg Focus 16:1–10, 2004; Johnsson et al., Spine 11:107–110, 1986; Young et al., Neurosurgery 23:628–633, 1988; Sanderson et al., Bone Joint J 75:393–397, 1993; Poletti et al., Neurosurgery 37:343–347, 1995; Weiner et al., Spine 24:2268, 1999). PED has several advantages, including less paraspinal muscle injury, less postoperative back pain, and early discharge. Regarding postoperative spinal instability, however, PED surgery whether the uniportal or the biportal endoscopic technique is based on the unilateral laminectomy for bilateral decompression (so-called “over-the-top technique”). Thus the possibility of postoperative spinal instability due to extensive removal of the ipsilateral medial facet joint or the isthmus remains. A contralateral interlaminar approach is an unfamiliar method. But some microscopic tubular decompressions via a contralateral interlaminar approach for lumbar spinal stenosis or disc herniations have been reported (Niggemeyer et al., Eur Spine J 6:423–429, 1997; Ahn et al., Expert Rev Med Devices 11:605–616, 2014; Hwa Eum et al., J Neurosurg Spine 24:602–607, 2016; Komp et al., Clin Spine Surg 24:281–7, 2011; Minamide et al., J Neurosurg Spine 19:664–671, 2013; Ruetten et al., J Neurosurg Spine 10:476–485, 2009; Torudom et al., Asian Spine J 10:335–342, 2016). They emphasized that the contralateral approach procedures provided easier access to the lateral recess pathology than the ipsilateral approach, and it maintained biomechanical stability by preserving facet joints. Following the evolution of surgical instruments including development of the high-speed endoscopic drill, we can perform PED surgery via the contralateral interlaminar approach for lumbar spinal stenosis. In this chapter, we describe the technical methods of the contralateral keyhole endoscopic surgery that makes it possible to maximize preservation of facet joints and prevent segmental instability.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Spinal stenosis is the most common disorder of the lumbar spine in elderly patients [1]. Lumbar spinal stenosis is caused by degenerative changes that result in intervertebral disc degeneration, ligamentum flavum hypertrophy/calcification, osteophytes, and enlargement of facet joints. Surgical treatment is recommended after failure of nonoperatvie therapies, including nonsteroidal anti-inflammatory medication, analgesics, oral steroids, physical therapy, and epidural steroid injections. Open decompressive surgery is performed to reduce pain caused by neural compression that results from lumbar spinal stenosis and considered the gold standard for symptomatic lumbar spinal stenosis [2]. The aim of surgical treatment is to achieve adequate neural decompression while preserving bony and muscular structure and decreasing secondary spinal instability [3]. Conventional open surgery has involved wide laminectomy and medial facetectomy with foraminotomy. Although this conventional technique provides maximal operative space, there is postoperative damage of the paraspinal muscles, the interspinous ligament, the supraspinous ligament, the spinous process, and the facet joints. Hence, conventional laminectomy occasionally causes muscle weakness and postoperative spinal instability that lead to lumbar fusion surgery [4]. In 1988, unilateral laminotomy for bilateral decompression (ULBD) in patients with lumbar spine was initially described by Young et al. [5]. ULBD subsequently modified as a minimally invasive unilateral approach for bilateral decompression [6,7,8]. Weiner et al. evaluated the clinical outcome of 30 patients who underwent bilateral microdecompression via a unilateral approach, with good clinical outcomes in 87% of the patients after a mean follow-up period of 0.75 years [8]. Niggemeyer et al. reported a meta-analysis that ULBD has more favorable outcomes compared to conventional open surgery in patients with lumbar spinal stenosis [9].
Percutaneous endoscopic lumbar decompression (PELD) in progression has become a reasonable alternative to open microsurgery for lumbar spinal stenosis [10,11,12,13,14,15]. PELD has several advantages, including less paraspinal muscle injury, less postoperative back pain, and early discharge. Regarding postoperative spinal instability, however, PELD by using a uniportal or biportal approach is based on the ULBD. Thus the possibility of postoperative spinal instability due to the extensive removal of the ipsilateral medial facet joint or the isthmus remains. Although a contralateral interlaminar approach is an unfamiliar method, several microscopic tubular decompressions via a contralateral interlaminar approach for lumbar spinal stenosis or disc herniations have been reported [16,17,18,19,20,21,22,23]. Alimi et al. emphasized that the contralateral approach procedures provided easier access to the lateral recess pathology than the ipsilateral approach, and it maintained biomechanical stability by preserving facet joints [21, 22]. The advent of surgical instruments such as the high-speed endoscopic drill has facilitated percutaneous endoscopic decompression via the contralateral interlaminar approach . In this chapter, we describe the technical methods of the contralateral keyhole endoscopic surgery (CKES) for lumbar spinal stenosis that makes it possible to maximize preservation of facet joints and prevent segmental instability.
2 Indications/Contraindications
CKES is the least invasive technique for epidural decompression through contralateral interlaminar approach. The contralateral interlaminar approach aims to reduce facet joint violation and minimize paraspinal muscle and posterior ligament complex injuries. Patients with enlarged facet joint who are more likely to have facet joint damage in the ipsilateral approach and patients with a wide interlaminar window are great surgical candidates for this technique. CKES is indicated in the following clinical situation: lateral recess stenosis, central canal stenosis, synovial cysts of the facet joint, ossification of the ligamentum flavum, and extruded discs or sequestered discs. CKES is contraindicated in the following clinical situation: cauda equina syndrome, severe neurologic deficits, spondylolisthesis grade II or greater, segmental Instability, and previous surgery in the same segment (Table 21.1).
3 Instruments
These surgical instruments are necessary in performing CKES: handmade working sheath having an outer diameter of 8.1 mm, serial dilators, vertebroplasty needle (Guardian®, BMKOREA, Co., Korea) (Fig. 21.1), endoscope (Vertebris lumbar, Richard Wolf, Germany), endoscopic drill (Primado 2, Nakanishi, INC., Japan), and bipolar radiofrequency (Ellman®, Elliquence, LLC, NY, USA) (Fig. 21.2) (Table 21.2).
4 Surgical Techniques
4.1 Determination of Entry Point
The point of entry is determined on the basis of the measurements of the preoperative axial T2-weighted images. The angulation to access the contralateral side depends on the spinolaminar angle for each lumbar level. The entry is to be marked at 1–2 cm away from the midline at the upper lumbar area and 2–3 cm from the lower lumbar area (Fig. 21.3).
4.2 Contralateral Interlaminar Epidural Approach
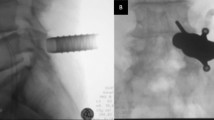
Under epidural anesthesia, the patient is placed on a prone position on a radiolucent table. The surgeon stands on the side opposite to the pathologic lesion. The level for surgery is identified by C-arm fluoroscopy. The interlaminar window should be maximized on the anterior-posterior (AP) view. At the center level of the interlaminar window, the midline and the point of entry are marked on the skin with a marking pen. A 7–8 mm skin incision is made at the entry (Fig. 21.4). A vertebroplasty needle is inserted into the entry and advanced under the C-arm fluoroscopic guidance, targeting toward the midline of the spinal canal. The cutting-type spinal needle can easily injure the thecal sac. It is recommended that a vertebroplasty needle with blunt tip for needle placement be used instead of the cutting-type spinal needle to avoid dura puncture. The tip of the needle is placed at the junction of interspinous ligament and ligamentum flavum. The needle is pushed to penetrate the ligamentum flavum and incrementally advanced towards the opposite epidural space while feeling the resistance of the ligamentum flavum. Once the tip penetrates the ligamentum flavum, a lateral fluoroscopic view is obtained to ensure that the tip rests in the dorsal epidural space. The stylette of the vertebroplasty needle is removed. A blunt guidewire is passed into the vertebroplasty needle shaft. After removal of the vertebroplasty needle shaft, serial dilators are passed over the guidewire (Fig. 21.5). The handmade working sheath is inserted in the final dilator. The beveled opening of the working sheath is initially placed toward the epidural space (bevel down) and then rotated to protect the thecal sac and the nerve root (bevel up). The final dilator is then removed, and an endoscope with an outer diameter of 6.9 mm is placed (Fig. 21.6).
4.3 Making Keyhole
To avoid neural compression injury, the hand-down technique is used consistently during the operation. Bipolar radiofrequency and forceps are used to remove any residual muscular and soft tissues overlying the lamina and interlaminar area. At this point in time, it is important to identify the endoscopic surgical anatomy, including the lamina, ligamentum flavum , and thecal sac underneath the flavum. An endoscopic high-speed drill is used to partially remove the inferior margin of the upper lamina, the superior margin of the lower lamina, and the base of the spinous process in a round form. Then, the midline portion of the ligament flavum and a small part of the interspinous ligament are removed using a punch, rongeurs, and forceps (we call this part of the operation “making keyhole”). The keyhole with widened dorsal midline epidural space contributes to more free manipulation of the endoscope (Fig. 21.7).
4.4 Contralateral Sublaminoplasty and Flavectomy
Care is taken to undercut the inner cortex of the cranial lamina and drill the upper edge of the caudal lamina. Pay particular attention to the caudal laminar drilling above the exiting nerve root. And then the ligamentum flavum can be detached from the lamina. The ligamentum flavum is left as a protective barrier for the dura and epidural veins. However, the ligamentum flavum is removed usually before reaching the lateral recess because the thickened ligamentum flavum itself can compress the neural structure (Fig. 21.8a–c). While the endoscope reaches the lateral recess, the working sheath usually is replaced with 0.5–1.5 mm longer length tongue (Fig. 21.8d–f). Sublaminoplasty and flavectomy should be performed until the traversing and exiting nerve roots are exposed. The thecal sac and the nerve root can be directly visualized by endoscope for confirmation of decompression (Fig. 21.9, Video 21.1).
(a) Initially, soft tissues and muscles are removed using forceps and bipolar radiofrequency. (b) Sublaminoplasty is performed with a high-speed drill. Note that the ligamentum flavum is kept intact to protect the underlying dura. (c) Ligamentum flavum is removed before reaching the lateral recess. (d–f) The working sheath is replaced with 0.5–1.5 mm longer length tongue for neural protection
5 Discussion
In ipsilateral approach for lumbar decompression, extensive resection of the facet joint might be necessary for complete decompression of lateral recess stenosis or foraminal stenosis. This may lead to spinal instability and cause postoperative back pain. Numerous studies reported that morbidity related to detaching the paraspinal muscles and resection of the facet joint could result in postoperative instability or fusion surgery [24,25,26].
In 2008, Yeom et al. reported a study in which two patients had undertaken microdiscectomy with a tubular retractor via a contralateral approach for L5-S1 intraforaminal disc herniations [17]. They mentioned that intraforaminal herniations at L5-S1 cannot be approached easily using ipsilateral lateral approaches because the iliac crest limits medial angulation of the operative corridor. They could easily remove the intraforaminal disc material through a contralateral tubular approach with minimal resection of osseous and ligamentous structures. Berra et al. described a modified surgical procedure for approaching the neural foramen from the contralateral side, minimizing muscle retraction and bone/ligament resection [23]. They obtained successful results in nine patients with intraforaminal or intra/extraforaminal lumbar disc herniation.
James et al. reported on 16 patients with a median follow-up period of 18 months who were treated for lumbar juxtafacet cyst by facet-sparing contralateral minimally invasive surgery [20]. Out of the 16 patients, 14 patients had excellent and good outcomes. In this particular series, they concluded that a contralateral approach using a tubular retractor system provides excellent visualization of the facet cyst wall allowing safe cyst resection and nerve root decompression without compromising the facet joint. Alimi et al. reported a retrospective cohort study of 32 patients with unilateral radiculopathy undergoing the contralateral approach via a tubular retractor technique [21]. In this study, the functional outcome was excellent and good in 95.2%. As mentioned above, they emphasized that the contralateral approach provided easier access to the lateral recess pathology than the ipsilateral approach. They indicated that, theoretically, the endoscopic approach is the least invasive, but the movement of the instruments is limited. We previously described the technical details of CKES in 14 patients with unilateral radiculopathy [27]. To solve the limitation of endoscopic movement in the interlaminar window, especially the upper lumbar spine, we have created a “keyhole” in which the endoscope can move freely. Thereby, we could achieve sufficient neural decompression of the nerve root and thecal sac with minimal muscle damage and facet joint violation.
Kim et al. reported a literature review about the scientific basis of minimally invasive spine surgery as it relates to posterior lumbar surgery [19]. He mentioned that the goals of minimally invasive surgery are to decrease muscle crush injuries during retraction, avoid disruption of the osseotendinous complex of the paraspinal muscles, and ultimately maintain the dynamic stability of the spine. In this study, he briefly introduced a case of the bilateral paramedian approach for the treatment of L4-5 spinal stenosis. This contralateral paramedian decompression was performed bilaterally to spare the tendinous attachment of the multifidus muscle at the spinous and allowed minimal facet resection during decompression of the lateral recess. Subsequently, Shin et al. performed bilateral decompression via microscopic tubular crossing laminotomy for 17 patients with lumbar spinal stenosis and followed them for 17.5 months (Fig. 21.10) [18]. The median value of operation time was 89.11 min. They reported good clinical results at 6-months and 12-months postoperative evaluation and demonstrated well-preserved bilateral facet joints postoperatively with sufficient spinal canal enlargement. There was no postoperative instability in radiological findings. We also have experienced bilateral decompression via CKES for nine patients with lumbar spinal stenosis till now (Fig. 21.14). Mean operation time was 115 min (unpublished data). Although it is obvious that this percutaneous endoscopic approach is less invasive than tubular retractor surgery, the longer operation time is still a challenge to overcome.
The contralateral approach is unfamiliar and CKES has a steep learning curve. This technique may be difficult to apply to all types of lumbar spinal stenosis such as severe spinal stenosis with grade II spondylolisthesis. However, CKES to carefully selected patients is a safe and reliable technique that protects the paraspinal muscles and posterior ligament complex and minimizes facet joint damage.
6 Case Illustrations
6.1 Case 1
A 53-year-old woman has been experiencing low back pain and right sciatic pain. The symptoms developed 1 year prior to consultation and got worse 3 months ago. MRI revealed the right lateral recess stenosis at L4-5 level. The patient’s symptoms did not improve after 2 months of conservative treatment. We performed the contralateral keyhole endoscopic surgery for the right lateral recess stenosis . Postoperatively the patient’s radicular pain was gone and the postoperative MRI showed sufficient decompression of the lateral recess stenosis (Fig. 21.11).
6.2 Case 2
A 61-year-old woman presented with a 6-month history of progressively worsening back pain, right buttock pain, and right leg radiation pain. MRI revealed the facet cyst with spinal stenosis at L4-5 level. A nerve block provided only a few days of relief. Postoperative MRI showed complete epidural decompression after selective removal of the facet cyst (Fig. 21.12).
Preoperative T2-weighted images of a 61-year-old woman show a facet cyst at the L4-5 level (a, b). Postoperative T2-weighted images demonstrate complete removal of the facet cyst (d, e). Intraoperative endoscopic image shows the excellent visualization of the facet cyst wall (c). The tip of the endoscopic instrument reaches the lateral recess (f)
6.3 Case 3
A 73-year-old woman presented with 5 years of low back pain and 3 months of right lower extremity radicular pain in an L4 dermatome. Preoperative MRI demonstrated a right ossified ligamentum flavum with the lateral recess stenosis at L3-4 level. The patient’s symptoms completely subsided immediately after the contralateral keyhole endoscopic surgery. Postoperative MRI revealed total removal of the ossified ligamentum flavum (Fig. 21.13).
Preoperative axial (a) and sagittal (e) T2-weighted images and computed tomography image (b) disclose the ossified ligamentum flavum with thecal sac compression in a 73-year-old man with unilateral radiculopathy. Postoperative axial (c) and sagittal (f) T2-weighted images and computed tomography image (d) show complete removal of the ossified ligamentum flavum
6.4 Case 4
A 65-year-old woman presented with low back pain and limitation in mobility as being able to walk 30 meters for 6 months due to both leg pain. MRI showed a lumbar spinal stenosis with the left facet hypertrophy at L4-5 level. The patient’s symptoms did not improve after 1 month of conservative treatment. We performed the bilateral contralateral keyhole endoscopic surgery for the L4-5 lumbar spinal stenosis . After lumbar decompressive surgery, the patient recovered with both leg pain. Postoperative MRI revealed a free spinal canal with the removal of the hypertrophic facet (Fig. 21.14).
Preoperative axial T2-weighted image (a) of a 65-year-old woman shows marked compression of the thecal sac with facet hypertrophy in the left fact join. Postoperative axial T2-weighted image (b) shows adequate decompression of the spinal canal with bilateral minimal facet resection. Intraoperative photograph (c) demonstrates bilateral contralateral interlaminar access. The tip of the vertebroplasty needle comes into contact with the working sheath over the thecal sac (d)
6.5 Case 5
A 42-year-old woman presented with a 3-week history of persistent right leg radiating pain. She had developed progressive back pain with right buttock pain. Radiographs revealed sequestered disc herniation at the right L5-S1 level. The contralateral interlaminar approach for the high-grade cranially migrated disc herniation was performed. Postoperatively, her symptoms have improved immediately (Fig. 21.15).
(a) Contralateral keyhole endoscopic decompression can be performed in patients with sequestered disc herniations . (b, d) Preoperative T2-weighted images of a 42-year-old woman show sequestered disc herniations at the L5-S1 level. (c, e) Postoperative T2-weighted images demonstrate complete removal of the disc material
References
Deyo RA, Ciol MA, Cherkin DC, Loeser JD, Bigos SJ. Lumbar spinal fusion: a cohort study of complications, reoperations, and resource use in the Medicare population. Spine. 1993;18(11):1463–70.
Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Blood E, Hanscom B, et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med. 2008;358(8):794–810.
Thongtrangan I, Le H, Park J, Kim DH. Minimally invasive spinal surgery: a historical perspective. Neurosurg Focus. 2004;16(1):1–10.
K-e J, Willner S, Johnsson K. Postoperative instability after decompression for lumbar spinal stenosis. Spine. 1986;11(2):107–10.
Young S, Veerapen R, O’laoire SA. Relief of lumbar canal stenosis using multilevel subarticular fenestrations as an alternative to wide laminectomy: preliminary report. Neurosurgery. 1988;23(5):628–33.
Sanderson P, Wood P. Surgery for lumbar spinal stenosis in old people. Bone Joint J. 1993;75(3):393–7.
Poletti CE. Central lumbar stenosis caused by ligamentum flavum: unilateral laminotomy for bilateral ligamentectomy. Neurosurgery. 1995;37(2):343–7.
Weiner BK, Walker M, Brower RS, McCulloch JA. Microdecompression for lumbar spinal canal stenosis. Spine. 1999;24(21):2268.
Niggemeyer O, Strauss J, Schulitz K. Comparison of surgical procedures for degenerative lumbar spinal stenosis: a meta-analysis of the literature from 1975 to 1995. Eur Spine J. 1997;6(6):423–9.
Ahn Y. Percutaneous endoscopic decompression for lumbar spinal stenosis. Expert Rev Med Devices. 2014;11(6):605–16.
Hwa Eum J, Hwa Heo D, Son SK, Park CK. Percutaneous biportal endoscopic decompression for lumbar spinal stenosis: a technical note and preliminary clinical results. J Neurosurg Spine. 2016;24(4):602–7.
Komp M, Hahn P, Merk H, Godolias G, Ruetten S. Bilateral operation of lumbar degenerative central spinal stenosis in full-endoscopic interlaminar technique with unilateral approach: prospective 2-year results of 74 patients. Clin Spine Surg. 2011;24(5):281–7.
Minamide A, Yoshida M, Yamada H, Nakagawa Y, Kawai M, Maio K, et al. Endoscope-assisted spinal decompression surgery for lumbar spinal stenosis. J Neurosurg Spine. 2013;19(6):664–71.
Ruetten S, Komp M, Merk H, Godolias G. Surgical treatment for lumbar lateral recess stenosis with the full-endoscopic interlaminar approach versus conventional microsurgical technique: a prospective, randomized, controlled study. J Neurosurg Spine. 2009;10(5):476–85.
Torudom Y, Dilokhuttakarn T. Two portal percutaneous endoscopic decompression for lumbar spinal stenosis: preliminary study. Asian Spine J. 2016;10(2):335–42.
Wiltse L, Spencer C. New uses and refinements of the paraspinal approach to the lumbar spine. Spine. 1988;13(6):696–706.
Yeom JS, Kim KH, Hong SW, Park K-W, Chang B-S, Lee C-K, et al. A minimally invasive technique for L5–S1 intraforaminal disc herniations: microdiscectomy with a tubular retractor via a contralateral approach. J Neurosurg Spine. 2008;8(2):193–8.
Shin M-H, KiM J-S, Ryu K-S, HuR J-W. Bilateral decompression via microscopic tubular crossing laminotomy (MTCL) for lumbar spinal stenosis: technique and early surgical result. Neurol Med Chir. 2015;55(7):570–7.
Kim CW. Scientific basis of minimally invasive spine surgery: prevention of multifidus muscle injury during posterior lumbar surgery. Spine. 2010;35(26S):S281–S6.
James A, Laufer I, Parikh K, Nagineni VV, Saleh TO, Härtl R. Lumbar juxtafacet cyst resection: the facet sparing contralateral minimally invasive surgical approach. Clinical Spine Surgery. 2012;25(2):E13–E7.
Alimi M, Njoku I Jr, Cong G-T, Pyo SY, Hofstetter CP, Grunert P, et al. Minimally invasive foraminotomy through tubular retractors via a contralateral approach in patients with unilateral radiculopathy. Oper Neurosurg. 2014;10(3):436–47.
Alimi M, Hofstetter CP, Pyo SY, Paulo D, Härtl R. Minimally invasive laminectomy for lumbar spinal stenosis in patients with and without preoperative spondylolisthesis: clinical outcome and reoperation rates. J Neurosurg Spine. 2015;22(4):339–52.
Berra LV, Foti D, Ampollini A, Faraca G, Zullo N, Musso C. Contralateral approach for far lateral lumbar disc herniations: a modified technique and outcome analysis of nine patients. Spine. 2010;35(6):709–13.
Schöller K, Steingrüber T, Stein M, Vogt N, Müller T, Pons-Kühnemann J, et al. Microsurgical unilateral laminotomy for decompression of lumbar spinal stenosis: long-term results and predictive factors. Acta Neurochir. 2016;158(6):1103–13.
Müslüman AM, Cansever T, Yılmaz A, Çavuşoğlu H, Yüce İ, Aydın Y. Midterm outcome after a microsurgical unilateral approach for bilateral decompression of lumbar degenerative spondylolisthesis. J Neurosurg Spine. 2012;16(1):68–76.
Caputy AJ, Luessenhop AJ. Long-term evaluation of decompressive surgery for degenerative lumbar stenosis. J Neurosurg. 1992;77(5):669–76.
Hwang JH, Park WM, Park CW. Contralateral interlaminar keyhole percutaneous endoscopic lumbar surgery in patients with unilateral radiculopathy. World Neurosurg. 2017;101:33–41.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
1 Electronic Supplementary Material
The video presentation of contralateral keyhole endoscopic surgery for facet cyst (WMV 702159 kb)
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Hwang, J.H., Park, C.W. (2020). Contralateral “Keyhole” Endoscopic Surgery. In: Kim, JS., Lee, J., Ahn, Y. (eds) Endoscopic Procedures on the Spine. Springer, Singapore. https://doi.org/10.1007/978-981-10-3905-8_21
Download citation
DOI: https://doi.org/10.1007/978-981-10-3905-8_21
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-3904-1
Online ISBN: 978-981-10-3905-8
eBook Packages: MedicineMedicine (R0)