Abstract
Percutaneous endoscopic lumbar discectomy (PELD) is a minimally invasive spinal technique that has several advantages over open discectomy, including less paravertebral muscle injury, preservation of bony structure, and rapid recovery. PELD has gained popularity for removal of herniated disc (HD) material over the past few years since Kambin introduced the percutaneous posterolateral approach in 1983. Remarkable evolution of endoscopic techniques and instrumentation leads to successful outcomes comparable to conventional open surgery. PELD has been applied to various types of disc herniation and the indication has been expanded. I propose various strategies for PELD according to various types of disc herniation.
Herniated disc (HD) with migration was classified into four zones: low-grade up/down and high-grade up/down based on the extent and direction of migration. High-grade up HDs can be removed with the outside or outside-in techniques from L1-2 to L4-5. High-grade down HDs can be removed using the outside technique with additional foraminoplasty. Low-grade up/down HDs with disc space continuity can be removed using the inside-out technique. Without continuity, the outside technique or foraminoplasty may be needed. Meanwhile, at the L5-S1 level, interlaminar PELD is used to treat high-grade up/down HD with migration.
-
Foraminal/extraforaminal disc herniation
The approach angle is steeper than conventional posterolateral approach. The entry point is about 7–10 cm depending on disc location. The approach angle is about 30–50°. In case of foraminal/extraforaminal disc herniation, invading the axilla of the exiting root, the area available for cannula insertion increases due to the lateral displacement of the corresponding nerve root. It is concerned about postoperative dysesthesia with manipulation of exiting nerve root. We should use a radiofrequency probe, laser, and working cannula carefully.
Proper surgical indications and good working cannula position are important for successful PELD. PELD techniques should be specifically modified to remove the disc fragments in various types of HD.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others

Keywords
1 Migrated Disc Herniation
1.1 Introduction
Disc fragments sometimes penetrate the posterior longitudinal ligament and migrate and occupy the anterior epidural space. Removal of the migrated disc fragment requires broad bone removal, including the laminas, pars, and facet joints, leading to potential postoperative instability. In particular, clinicians are often concerned about retaining the affected disc. Percutaneous disc surgery was first introduced by Hijikata et al. [1], while Kambin introduced the contemporary endoscopic discectomy technique [2]. The concepts underlying percutaneous disc procedures have changed from central decompression to selective fragmentectomy or from indirect to direct neural decompression. Percutaneous endoscopic lumbar discectomy (PELD) has been applied to various types of disc herniations, and the indications for this procedure have been expanded [3,4,5]. High-speed endoscopic drills, reamer kits, flexible curved forceps, and probes enable the treatment of various types of disc herniation. However, percutaneous endoscopic techniques for migrated discs are technically demanding and the results depend on the surgeon’s experience [6]. Although improvements in equipment and techniques have led to successful outcomes compared to conventional open surgery, a herniated disc (HD) with migration remains a challenging condition, and it remains one of the common causes of endoscopic failure. Planning a strategy according to the classification of HD migration is important for successful PELD [7].
1.2 Classification
Migrated disc herniation was defined as herniation displaced from the endplate of the index level. Depending on direction and extent, four groups were defined: high-grade up, low-grade up, high-grade down, and low-grade down. High-grade up-migration is defined if the extent of migration is located above the half of the infrapedicle level. Low-grade up-migration is defined if the migration is located between the upper margin of the disc space and the half of the infrapedicle level. High-grade down-migration is defined if the extent of the migration is located below the suprapedicle level. Low-grade down-migration is defined if the migration is located between the lower margin of the disc space and the suprapedicle level (Fig. 13.1) [8]. Sequestration is defined as no remaining continuity of disc material between the fragment and the disc of origin.
1.3 Endoscopic Technique
1.3.1 Inside-Out Technique
The PELD procedure was performed under local anesthesia in the prone position. The patients communicated with the surgeon during the entire procedure. The skin entry point was generally 10–14 cm from the midline. After infiltration of the entry point with local anesthetics, an 18-gauge spinal needle was introduced under fluoroscopic guidance. The needle tip was positioned at one point of the medial pedicle line on the anteroposterior fluoroscopic projection and at the posterior vertebral line on the lateral projection. Then, the following steps were performed: a guide wire was inserted through the spinal needle, a tapered cannulated obturator was inserted along the guide wire, and last a bevel-ended, oval-shaped, working cannula was inserted into the disc along the obturator. Next, an endoscope (YESS system; Richard Wolf, Knittlingen, Germany) was inserted through the cannula. The disc material was removed using endoscopic forceps by moving from the central portion to the lateral portion of the disc space on the anteroposterior image (Fig. 13.2a, b). The inflamed nucleus was observed to be anchored to the annular fissure. The HD and fibrotic scar tissues were released and removed using endoscopic forceps rotating the working bevel toward the migrated disc fragment. If the disc fragment remained in the epidural space, the working cannula was retrieved to the epidural space to locate the remnant disc using a flexible curved probe and forceps after cutting the posterior longitudinal ligament (Fig. 13.2c). After the herniated fragment was completely removed, the endoscope was removed.
(a) Inside-out technique for performing the intradiscal working tunnel and cavity. After releasing the annular fissure, the herniated disc is grasped by forceps. (b) Schematic illustration of the inside-out technique: (1) working cannula is located in the disc. (2) Pulling out the cannula in the epidural space and shifting upward or downward. (c) Radiography of the inside-out technique showing that flexible curved forceps catches the down-migrated disc
1.3.2 Outside or Outside-in Technique
The working cannula was placed in the epidural space without penetrating the annulus (Fig. 13.3a, b) [9]. By shifting the cannula upward (Fig. 13.3c), the exiting nerve root (ENR) was exposed. After the identification of the ENR or the axilla of the ENR, the ruptured disc covered by the ligament was located. After removing part of the ligament with bleeding control, the fragment below the ENR was removed with forceps. If protrusions or loose intradiscal fragments in the disc space were found, the disc material was subsequently removed (outside-in).
(a) Outside technique without penetrating the disc space. The herniated disc in the epidural space is accessed directly. (b) Sequential procedure of the outside or outside-in techniques. (1) The working cannula is located in the epidural space. (2) Shifting the cannula upward. (3) Penetrating the disc space or removing intradiscal tissue. (c) Radiography of the outside technique showing that the working cannula is adjusted in the caudo-cranial direction for up-migrated disc herniation
1.3.3 Foraminoplasty Technique
1.3.3.1 Foraminoplasty Using a Bone Reamer
With a craniocaudal inclinatory 20–30° angle, the needle was placed superior to the pedicle of the lower vertebra (Fig. 13.4a). A serial guide rod was docked between the lower vertebral body and the ventral surface of the superior facet. A reamer kit (TESSYS, Joimax GmbH, Karlsruhe, Germany; Fig. 13.4b) was advanced to the medial pedicle line serially, using large diameter reamers. After removing the superior facet and widening the intervertebral foramen, the working cannula was placed below the disc fragment.
(a) Intraoperative radiography shows initial targeting and foraminoplasty using serial reamers . (b) Serial dilators and reamers are shown. (c) Intraoperative radiography shows removals of a superior articular process (SAP) and upper pedicle using an endoscopic drill. (d) Endoscopic view shows removal of the upper pedicle (★), SAP (◆), and disc space (▲)
1.3.3.2 Foraminoplasty Using an Endoscopic Drill
A tapered cannulated obturator was inserted along the guide wire. The cannula was placed outside the foramen and the lateral border of the facet joint. An endoscopic drill (Primado 2, Nakanishi Inc., Japan) was used to remove the part of the superior articular process and the pedicle (Fig. 13.4c, d). From the outside to the inside of the foramen, the facet joint and foraminal ligament were partially removed using a drill, cutting forceps, and an endoscopic Kerrison punch, while engaging the working cannula in the medial foraminal zone to undercut the superior facet.
The ligament was removed and the traversing nerve root was exposed. Generally, the fragment is hidden under the traversing nerve root. Under the endoscopic view, the disc fragment was pulled out with a curved probe and curved forceps. After removal of the fragment, the traversing nerve root was movable. If disc protrusion was found in the disc space, the subannular disc was removed using the conventional method.
1.3.4 Interlaminar Technique
The skin entry angle and the direction of the cannula were quite different depending on up- or down-migration. With up-migration of the L5–S1, the caudo-cranial direction and shoulder approach of the S1 nerve root can facilitate the access to the up-migrated fragment below the axilla of the L5 nerve root or the lateral margin of the thecal sac parallel to the upper lamina. With down-migration of the L5–S1, the craniocaudal direction and axilla approach can provide direct vision above the mid S1 pedicle level. Far-down migration requires partial removal of the upper S1 lamina. After opening the ligament flavum, the margin of the nerve root was exposed. Upon advancing the working cannula to the target, the ruptured fragment was exposed. The HD was removed using forceps. Depending on the condition, loose disc fragments or protruded discs were removed from the disc space.
1.4 Endoscopic Strategy
-
Low-grade up-/down-migration with disc space continuity: inside-out technique
Via the conventional posterolateral endoscopic approach, the entire migrated fragment can be extracted with the inside-out technique by grasping the root of the HD interposing the annular fissure. Depending on the situation, cutting the posterior longitudinal ligament (PLL) and adjusting the bevel opening of the working cannula facilitate the extraction of the migrated fragment.
-
Low-grade up/down sequestration : outside technique or outside technique with foraminoplasty
This situation is not common. Penetration of the annulus by the working cannula is not required. The cannula should be placed in the epidural space. To extract the migrated disc, the nerve root should be exposed and inspected under or on the PLL.
-
High-grade down-migration : outside technique with foraminoplasty
A rigid endoscope cannot be used to visualize the whole fragment of a high-grade down-migrated disc via the conventional technique. An inclinatory approach, which means approaching from the craniocaudal direction, and foraminal widening would be necessary to visualize the anterior epidural space (Fig. 13.5). A curved probe and forceps facilitate extraction and grasping of the disc fragment. Choi et al. used an endoscopic diamond drill to undercut the superior facet [3]. Schubert and Hoogland used a bone reamer under fluoroscopic guidance [9]. However, they could not completely visualize the fragment below the mid-pedicle of the low vertebra. If the migrated disc is in one piece, this technique can provide a guarantee of complete removal of the disc material. If the disc fragments are in multiple pieces, there is a possibility of remnant disc fragments below the pedicle [6].
-
High-grade up-migration: outside or outside-in technique
A 34-year-old woman with right leg radiating pain (L5 dermatome). A parasagittal magnetic resonance (MR) image (a) shows a high-grade down-migrated disc herniation at L4–5. After partial removal of SAP and the superior pedicle using an endoscopic drill (b), A postoperative MR parasagittal image (c) shows a widened intervertebral foramen MR image (d) showing the complete removal of the herniated disc
In general, upward-migrated disc fragments compress the axilla of the exiting nerve or dorsal root ganglion. The working cannula should not penetrate the disc space if possible and should be adjustable (Fig. 13.6). Upper lumbar levels with sufficient foraminal dimensions are necessary for the outside or outside-in techniques [10]. At the lower lumbar level, foraminal widening is sometimes required. The outside-in technique enables the removal of the protruded disc from the disc space as well as to remove the foraminal or upward-migrated discs.
-
High-grade up/down at the L5–S1—interlaminar technique
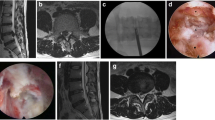
A 55-year-old woman suffered from severe left anterior thigh pain and inguinal pain. Magnetic resonance (MR) images (a and b) showing high-grade up-migration at the L2–3 level. After discography (c) with slight oblique trajectory, the obturator (d) and working cannula were inserted serially. With caudo-cranial direction, free fragments in the epidural space were found with a curved probe (e). Postoperative MR images (f and g) showing complete removal of the up-migrated disc
The transforaminal route, including a posterolateral approach, has a narrow window at the L5–S1 level. The iliac crest hinders posterolateral access and a narrow intervertebral foramen restricts free manipulation of the working cannula at the L5–S1 [11]. For the L5–S1 high-grade up-/down-migrated discs and low-grade up-/down-migrated discs with a high iliac crest, an interlaminar PELD can directly access and remove the ventral lesion (Fig. 13.7). Ruetten et al. suggested that migration over the maximal half of the vertebral body should be excluded [12]. However, Choi et al. reported an 8 mm maximal migration in the craniocaudal direction over half of the adjacent vertebral body [13]. The accessibility of the migrated disc would depend on the vertical diameter of the interlaminar window. If the interlaminar window is not large enough, endoscopic bone work is necessary using an endoscopic drill.
A 54-year-old woman presented with right posterolateral leg pain. Magnetic resonance (MR) images (a and b) showing a sequestrated disc fragment far from the L5–S1 disc space. Intraoperative radiography (c) showing that the forceps grasped the disc fragment below the L5 pedicle. Endoscopic view (d) via interlaminar percutaneous endoscopic lumbar discectomy showing the herniated disc fragment (★) below the L5 nerve root (◆). Postoperative MR images (e and f) showing complete removal of the disc fragment
Lee et al. proposed a conventional inside-out PELD technique, called the half-and-half technique , for removing near-migrated discs [14]. They also suggested the epiduroscopic technique for far-migrated discs. Their outcomes with far-migrated discs were inferior to those with near-migrated discs. In our series, there was no difference in outcomes for direction and degree of migration [7]. In high-grade HD with migration, the outside technique, foraminoplasty, and interlaminar PELD techniques facilitate complete removal of the disc fragments. However, we could not visualize the disc fragment above the mid-pedicle of the upper vertebra and below the mid-pedicle of the lower vertebra despite the oblique trajectory of the working cannula and the bone work performed for foraminal widening. If the migrated fragment is located above or below the mid-pedicle level, a flexible curved probe and forceps would assist in the location of the obscured fragment. In these situations, a combination of the transforaminal and interlaminar approach techniques (Fig. 13.8) and the translaminar or transpedicular approaches (Fig. 13.9) could also provide guarantee for complete removal of the disc [15].
A 39-year-old male suffered from low back pain and severe right leg radiating pain as L5 and S1 dermatome. T2-weighted sagittal MR image (a) showing that a large disc herniation (arrows) of the L4-5 level extends to the S1 pedicle level. Intraoperative radiography (b) showing that the working cannula is located between the spinous process and right medial pedicle line via the contralateral (left) approach. Endoscopic forceps (c) accesses the ventral epidural space below the L5 pedicle via the L5-S1 interlaminar approach . Postoperative T2-weighted sagittal MR image (d) showing complete removal of the herniated disc
A 38-year-old male presented with left leg radiating pain as L4 dermatome and decreased strength of ankle dorsiflexion. MR sagittal image (a) showing a disc herniation of the L3-4 level extends to the L4 lower endplate level. Via transpedicular route, an endoscopic forceps grasped disc fragment (b). Postoperative MR image (c) showing complete removal of the disc fragment. Postoperative computed tomography (d) showing a trace of transpedicular PELD
2 Foraminal/Extraforaminal Disc Herniation
2.1 Introduction
The incidence of foraminal/extraforaminal disc herniation (FEDH) constitutes approximately 7–12% of all lumbar disc herniations [16]. The foraminal zone is regarded from the medial border of the pedicle to the lateral border of the pedicle. The extraforaminal zone is defined beyond the lateral border of the pedicle. Lateral disc herniation is regarded as FEDH. FEDH is usually found in older patients and presents with severe radicular symptoms. The pain is aggravated by extension and lateral bending. Axial and parasagittal magnetic resonance (MR) images are considered to be the gold standard for detecting FEDH. Nevertheless, FEDH can be underdiagnosed by omitting lateral parasagittal images and by being confused with the dorsal root ganglion. High-resolution computed tomography (CT) and coronal MR images may assist in the detection of FEDH.
FEDH can be treated surgically with the intertransverse approach via a midline incision and the transmuscular approach via a paramedian incision. The midline approach provides easy anatomic orientation but requires a long incision and large muscle dissection. Microdecompression through the lateral intermuscular approach was introduced by Reulen et al. [17] and Wiltse and Spencer [18]. This technique has the advantages of minimizing facet joint removal as well as providing access from the medial facet joint to the distal ala. However, it is associated with surgical morbidity and recurrent back pain by iatrogenic instability.
The percutaneous endoscopic posterolateral approaches are effective for lumbar disc herniation. The percutaneous endoscopic technique preserves spinal stability, avoids iatrogenic muscle injury, and reduces epidural fibrosis. As a minimally invasive procedure, the posterolateral endoscopic approach for FEDH is also effective and safe [19,20,21,22].
2.2 Surgical Technique
The approach angle is steeper than the conventional posterolateral approach for intracanal disc herniation (Fig. 13.10). The entry point is about 7–10 cm from midline, depending on disc location. The approach angle is about 30–50°. The final target point of the spinal needle was the middle pedicle line on the anteroposterior view and the posterior vertebral line on the lateral view (Fig. 13.11). After insertion of the needle to the disc space, discography was performed using a mixture of telebrix and indigo carmine for the staining of the disc fragment. Then, the following steps were performed: a guide wire was inserted through the spinal needle, a tapered cannulated obturator was inserted along the guide wire, and last a bevel-ended, oval-shaped, working cannula was inserted into the disc along the obturator. Next, an endoscope was inserted through the cannula. Depending on the condition, internal debulking was performed in the disc with pituitary forceps. The working cannula was removed from disc space to the foramen. The ENR is usually cranially and laterally displaced by the HD fragment. Fat tissue was cleared with a flexible bipolar radiofrequency probe (Elliquence, Baldwin, NY, USA). After the identification of the ENR or the axilla of the ENR, the ruptured disc covered by the ligament or adhesive tissue was found (Fig. 13.12a and Video 13.1). Grasping the fragment with endoscopic forceps and gently pulling it can remove the disc fragment (Fig. 13.12b). By moving and rotating the working cannula, other fragments or obscured fragments can be visualized. Last, adequate decompression of the ENR can be achieved by inspecting the course of the ENR (Fig. 13.12c). Finally, the working cannula is withdrawn.
For paramedian disc herniation, the target point (white arrow) of the spinal needle is the medial pedicle line (white line) in the anteroposterior (AP) view (a) and the posterior vertebral line (white line) in the lateral view (b). For central disc herniation, the spinal needle targets a point between the medial pedicle line (white line) and midline (dotted line) in the AP view (c) and the posterior vertebral line in the lateral view (b). For foraminal/extraforaminal disc herniation, the spinal needle targets the mid-pedicle line (dashed dotted line) in the AP view (d) and the posterior vertebral line (white line) in the lateral view (b)
A 68-year-old woman suffered from right severe radiating leg pain from buttock to knee. The knee jerk on the right side decreased. She could not extend her back. Magnetic resonance (MR) images (a and b) showing foraminal disc herniation at the L4–5. Endoscopic view (c) showing a ruptured disc covered by ligament (◆). After cutting the yellowish tissue, the ruptured disc (★) was visualized under the exiting nerve root (ENR) (d). The ENR (▲) could be found by removal of the disc fragment (e). Postoperative MR images (f and g) showing complete removal of the disc fragment in the foraminal zone
2.3 Outcomes and Technical Consideration
An 82–92% success rate has been reported for the results of the endoscopic posterolateral approach for FEDH [19,20,21, 23], while the surgical success rate ranged from 71% to 88% with the paraspinal muscle-splitting microsurgical technique [16, 24]. The incidence of postoperative dysesthesia is relatively higher in FEDH than in intracanal disc herniation. The incidence of dysesthesia with open microsurgery was 7–25%, and the incidence of reflex sympathetic dystrophy was 1–2%. With the endoscopic approach, the incidence of dysesthesia was 6–17%. These complications usually resolve with conservative treatment within several weeks. However, postoperative dysesthesia is one of the significant sequelae and negatively affects the patient’s daily life. The target of the needle should not exit the safe zone. The nerve root in the foraminal zone courses in a vertical direction, crossing the disc space between the middle and lateral borders of the pedicle. The distance between the ENR and the disc space from the medial border of the pedicle to the lateral border decreases. At the lateral border of the pedicle, the nerve root passes through the disc space [25]. The course of the nerve root limits the safe insertion of the cannula between the middle and the medial borders of the pedicle. In cases where FEDH is invading the axilla of the exiting root, the area available for cannula insertion increases due to the lateral displacement of the corresponding nerve root. Some authors recommend that: (1) the skin entry point is kept more medial, (2) the needle angle is relatively steeper, and (3) the needle target point is identified as the mid-pedicle line near the superior endplate of the caudal vertebra to prevent ENR injury. The bevel-type working cannula facilitates the visualization and the protection of the ENR during the discectomy, by rotating the bevel. The radiofrequency probe, l aser, and working cannula should be used with care. Combined with foraminal/extraforaminal stenosis, especially in the L5–S1 level, it is too difficult to directly access the disc fragment without bone removal such as of the ilium, thick L5 transverse process, and sacral ala. In this situation, disc removal should be preceded by adequate bone decompression using an endoscopic drill or reamers.
2.4 Conclusion
For successful PELD, the disc’s location should be considered in selecting the appropriate endoscopic approach and strategy.
References
Hijikata S, Yamagishi M, Nakayama T, Oomori K. Percutaneous discectomy: a new treatment method for lumbar disc herniation. J Toden Hosp. 1975;5(5):39–44.
Kambin P, Sampson S. Posterolateral percutaneous suction-excision of herniated lumbar intervertebral discs. Report of interim results. Clin Orthop Relat Res. 1986;(207):37–43.
Choi G, Lee SH, Lokhande P, Kong BJ, Shim CS, Jung B, Kim JS. Percutaneous endoscopic approach for highly migrated intracanal disc herniations by foraminoplastic technique using rigid working channel endoscope. Spine. 2008;33(15):E508–15. https://doi.org/10.1097/BRS.0b013e31817bfa1a.
Lee SH, Choi KC, Baek OK, Kim HJ, Yoo SH. Percutaneous endoscopic intra-annular subligamentous herniotomy for large central disc herniation: a technical case report. Spine. 2014;39(7):E473–9. https://doi.org/10.1097/BRS.0000000000000239.
Osman SG, Sherlekar S, Malik A, Winters C, Grewal PK, Narayanan M, Gemechu N. Endoscopic trans-iliac approach to L5-S1 disc and foramen - a report on clinical experience. Int J Spine Surg. 2014;8. https://doi.org/10.14444/1020.
Choi KC, Lee JH, Kim JS, Sabal LA, Lee S, Kim H, Lee SH. Unsuccessful percutaneous endoscopic lumbar discectomy: a single-center experience of 10,228 cases. Neurosurgery. 2015;76(4):372–80. discussion 380-371; quiz 381. https://doi.org/10.1227/NEU.0000000000000628.
Choi KC, Lee DC, Shim HK, Shin SH, Park CK. A strategy of percutaneous endoscopic lumbar discectomy for migrated disc herniation. World Neurosurg. 2017;99:259–66. https://doi.org/10.1016/j.wneu.2016.12.052.
Fardon DF, Milette PC, Combined Task Forces of the North American Spine Society ASoSR, American Society of Neuroradiology. Nomenclature and classification of lumbar disc pathology. Recommendations of the Combined task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine. 2001;26(5):E93–E113.
Schubert M, Hoogland T. Endoscopic transforaminal nucleotomy with foraminoplasty for lumbar disk herniation. Oper Orthop Traumatol. 2005;17(6):641–61. https://doi.org/10.1007/s00064-005-1156-9.
Min JH, Kang SH, Lee JB, Cho TH, Suh JK, Rhyu IJ. Morphometric analysis of the working zone for endoscopic lumbar discectomy. J Spinal Disord Tech. 2005;18(2):132–5.
Choi KC, Park CK. Percutaneous endoscopic lumbar discectomy for L5-S1 disc herniation: consideration of the relation between the iliac crest and L5-S1 disc. Pain Physician. 2016;19(2):E301–8.
Ruetten S, Komp M, Godolias G. A New full-endoscopic technique for the interlaminar operation of lumbar disc herniations using 6-mm endoscopes: prospective 2-year results of 331 patients. Minim Invasive Neurosurg. 2006;49(2):80–7. https://doi.org/10.1055/s-2006-932172.
Choi KC, Kim JS, Ryu KS, Kang BU, Ahn Y, Lee SH. Percutaneous endoscopic lumbar discectomy for L5-S1 disc herniation: transforaminal versus interlaminar approach. Pain Physician. 2013;16(6):547–56.
Lee S, Kim SK, Lee SH, Kim WJ, Choi WC, Choi G, Shin SW. Percutaneous endoscopic lumbar discectomy for migrated disc herniation: classification of disc migration and surgical approaches. Eur Spine J. 2007;16(3):431–7. https://doi.org/10.1007/s00586-006-0219-4.
Choi KC, Lee JH, Kim JS, Lee DC, Park CK. Combination of transforaminal and interlaminar percutaneous endoscopic lumbar diskectomy for extensive down-migrated disk herniation. J Neurol Surg A Cent Eur Neurosurg. 2018;79(1):60–5. https://doi.org/10.1055/s-0037-1601875.
Epstein NE. Evaluation of varied surgical approaches used in the management of 170 far-lateral lumbar disc herniations: indications and results. J Neurosurg. 1995;83(4):648–56. https://doi.org/10.3171/jns.1995.83.4.0648.
Reulen HJ, Muller A, Ebeling U. Microsurgical anatomy of the lateral approach to extraforaminal lumbar disc herniations. Neurosurgery. 1996;39(2):345–50. discussion 350-341.
Wiltse LL, Spencer CW. New uses and refinements of the paraspinal approach to the lumbar spine. Spine. 1988;13(6):696–706.
Choi G, Lee SH, Bhanot A, Raiturker PP, Chae YS. Percutaneous endoscopic discectomy for extraforaminal lumbar disc herniations: extraforaminal targeted fragmentectomy technique using working channel endoscope. Spine. 2007;32(2):E93–9. https://doi.org/10.1097/01.brs.0000252093.31632.54.
Jang JS, An SH, Lee SH. Transforaminal percutaneous endoscopic discectomy in the treatment of foraminal and extraforaminal lumbar disc herniations. J Spinal Disord Tech. 2006;19(5):338–43. https://doi.org/10.1097/01.bsd.0000204500.14719.2e.
Lew SM, Mehalic TF, Fagone KL. Transforaminal percutaneous endoscopic discectomy in the treatment of far-lateral and foraminal lumbar disc herniations. J Neurosurg. 2001;94(2 Suppl):216–20.
Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: Surgical technique, outcome, and complications in 307 consecutive cases. Spine. 2002;27(7):722–31.
Kambin P, O'Brien E, Zhou L, Schaffer JL. Arthroscopic microdiscectomy and selective fragmentectomy. Clin Orthop Relat Res. 1998;347:150–67.
Epstein NE. Different surgical approaches to far lateral lumbar disc herniations. J Spinal Disord. 1995;8(5):383–94.
Hurday Y, Xu B, Guo L, Cao Y, Wan Y, Jiang H, Liu Y, Yang Q, Ma X. Radiographic measurement for transforaminal percutaneous endoscopic approach (PELD). Eur Spine J. 2017;26(3):635–45. https://doi.org/10.1007/s00586-016-4454-z.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
1 Electronic Supplementary Material
(MPG 101688 kb)
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Choi, KC., Lee, D.C., Park, CK. (2020). Modified Endoscopic Access for Migrated and Foraminal/Extraforaminal Disc Herniation. In: Kim, JS., Lee, J., Ahn, Y. (eds) Endoscopic Procedures on the Spine. Springer, Singapore. https://doi.org/10.1007/978-981-10-3905-8_13
Download citation
DOI: https://doi.org/10.1007/978-981-10-3905-8_13
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-3904-1
Online ISBN: 978-981-10-3905-8
eBook Packages: MedicineMedicine (R0)