Abstract
-
Atrial fibrillation is the commonest arrhythmia encountered in clinical practice, the prevalence of which increases with aging.
-
AF is the leading cause of cardiovascular morbidity and mortality among geriatric population and is the most common etiology for cardiogenic thromboembolism.
-
Management strategies in AF focus on prevention of thromboembolism and management of symptoms related to tachycardia.
-
Oral anticoagulation with warfarin and more recently non-vitamin K-dependent compounds is highly effective in preventing thromboembolism related to AF.
-
Rate control and rhythm control are the two major approaches for managing atrial fibrillation.
-
Rhythm control is preferred in symptomatic paroxysmal AF especially in young patients. Catheter ablation is evolving as a promising strategy for rhythm control in this subset over antiarrhythmic therapy which is limited by efficacy and toxicity of these drugs.
-
Prevalence of atrial fibrillation increases with aging.
-
Majority of AF in developed countries are from non-valvular heart disease.
-
AF causes significant morbidity and mortality, the major complication being strokes.
-
Older people have much to gain from oral anticoagulation, which is underutilized in this age group, even though treatment has to be individualized.
-
Rate control is acceptable in more persistent and less symptomatic patients. Stricter rate control over a more lenient approach is preferred in those with symptoms and ventricular dysfunction where as both approaches yield similar long-term results in rest of the patient population.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
FormalPara Key Points-
Atrial fibrillation is the commonest arrhythmia encountered in clinical practice, the prevalence of which increases with aging.
-
AF is the leading cause of cardiovascular morbidity and mortality among geriatric population and is the most common etiology for cardiogenic thromboembolism.
-
Management strategies in AF focus on prevention of thromboembolism and management of symptoms related to tachycardia.
-
Oral anticoagulation with warfarin and more recently non-vitamin K-dependent compounds is highly effective in preventing thromboembolism related to AF.
-
Rate control and rhythm control are the two major approaches for managing atrial fibrillation.
-
Rhythm control is preferred in symptomatic paroxysmal AF especially in young patients. Catheter ablation is evolving as a promising strategy for rhythm control in this subset over antiarrhythmic therapy which is limited by efficacy and toxicity of these drugs.
-
Prevalence of atrial fibrillation increases with aging.
-
Majority of AF in developed countries are from non-valvular heart disease.
-
AF causes significant morbidity and mortality, the major complication being strokes.
-
Older people have much to gain from oral anticoagulation, which is underutilized in this age group, even though treatment has to be individualized.
-
Rate control is acceptable in more persistent and less symptomatic patients. Stricter rate control over a more lenient approach is preferred in those with symptoms and ventricular dysfunction where as both approaches yield similar long-term results in rest of the patient population.
Mr. John Smith is an 85-year-old gentleman, presenting with worsening shortness of breath and effort intolerance of 2 weeks duration. He also noticed increasing bilateral ankle swelling and weight gain of the same duration. While trying to get up and walk around with the use of a walker, he notices heart racing and feels dizzy and lightheaded. He is known to have hypertension for more than 20 years for which he takes medications. His other medical issues are diabetes, which is well controlled with medications, history of two heart attacks in the past, and diagnosed stroke which recovered completely in 48 h. He is also known to have prostatic enlargement and chronic kidney failure (creatinine 150 μmol/L), which has been stable. His wife noticed a gradual decline in his cognitive functions over the last year.
His medications included atenolol, aspirin, ramipril, metformin, tamsulosin, nitrates, and multivitamin supplements.
In the ER, he was mildly tachypneic, and saturations are 90% at room air. His pulse rate was 130 beats a minute, and blood pressure measured 180/100 mmHg. Jugular veins were distended, and mean JVP measured 12 cm from sternal angle. Cardiovascular system examination revealed cardiac enlargement with a murmur of mild-to-moderate aortic stenosis. There were fine rales over the lung bases suggestive of heart failure.
His ECG revealed rapid atrial fibrillation at a rate of 120 bpm, features of left ventricular hypertrophy, and possible old inferior wall MI. Blood biochemistry revealed marginally elevated troponins, normal electrolytes, creatinine of 200 mmol with a calculated GFR of 40, normal total and differential leucocyte counts, and normal liver function tests and TSH.
An echocardiogram performed demonstrated left ventricular hypertrophy, mild dilatation of the ventricles, global left ventricular function of 40%, severely dilated atria, and sclerosed aortic valve with moderate transvalvular gradient. There was mild mitral regurgitation also.
How should we manage Mr. Smith and optimize his medical treatment? What should be the long-term plan for Mr. Smith?
Clinical presentation of Mr. Smith is suggestive of rapid atrial fibrillation and features of left ventricular failure.
15.1 Epidemiology of Atrial Fibrillation
Atrial fibrillation (AF) is the commonest sustained cardiac arrhythmia encountered in clinical practice. The prevalence of AF increases with age, and approximately the prevalence is 20% among those over 85 years of age [1]. After the age of 50 years, the prevalence of AF doubles every decade, and two-thirds of all the cases of AF are above the age of 75 years [2].
The global burden of AF is on the rise as a result of aging population, increasing prevalence of other cardiovascular risk factors like hypertension, coronary artery disease, heart failure, etc. In developed countries, majority of AF cases are non-valvular because of the abovementioned factors [3].
15.2 Clinical Manifestations of Atrial Fibrillation in Elderly
The most common symptoms of AF are palpitations, heart failure symptoms, chest pain, and syncope and presyncope in elderly population. Because of the declining compliance of the ventricles with aging and associated hypertension, loss of atrial contribution to ventricular filling coupled with short and irregular diastolic intervals result in increase in ventricular filling pressures and pulmonary congestion. A major complication of AF is stroke in elderly population, and this also could be the initial manifestation. Polyuria because of increased atrial natriuretic hormone release is another symptom of atrial fibrillation [4]. Prolonged periods of tachycardia can lead to heart failure secondary to tachycardiomyopathy and systolic heart failure [5]. There is an increasing prevalence of AF with worsening heart failure symptoms. The prevalence is less than 10% in NYHA class 1 and up to 50% in NYHA class 4 patients [5]. In patients with permanent AF, symptoms may be absent in up to 40% cases [6], and stroke could be the first manifestation. Asymptomatic cases are more common in males.
15.3 Prognosis of AF in Elderly
AF contributes to significant morbidity and mortality in geriatric population. It is a major reason for poor quality of life, cognitive decline, heart failure, hospitalizations, stroke, and systemic embolism. Mortality rates are also increased by 1.5–1.9 times in AF patients across a wide range of age, both in men and women [7,8,9,10,11].
AF has been implicated in cognitive decline and dementia. The proposed mechanisms involved are cerebral microvascular occlusions from recurrent microembolism mostly related to subtherapeutic anticoagulation, micro-hemorrhages, (factors directly influenced by the time in therapeutic INR range), irregular heart rate resulting in cerebral hypoperfusion, and a pro-inflammatory state induced by AF. Shared genetic factors are also implicated in predisposing AF patients for dementia [12].
Heart failure bears a complex relationship with atrial fibrillation. AF is a major risk factor for development of heart failure and can establish a vicious cycle between the two conditions. The prevalence of AF increases with increasing severity of heart failure. AF can worsen the heart failure by tachycardia, impaired ventricular filling and resultant diastolic dysfunction and pulmonary congestion, and also by inducing systolic dysfunction (tachycardiomyopathy) [5, 8, 13].
One of the most devastating and common complications of AF is thromboembolism especially to the brain. AF increases the risk of stroke up to fivefold. The stroke risk increases with age and is up to 23.5% between 80 and 89 years and 35% for the ages over 90 [13, 14].
When compared with those in sinus rhythm, there is a 50–90% increase in mortality among patients in AF irrespective of their age. The annual mortality in AF is 5–8% and half of the same is due to cardiovascular causes [11, 14].
Mortality rates are higher among women, although when adjusted for age, men had a higher mortality. Annual mortality rates are almost twice even in asymptomatic patients (9.4% vs. 4.2%) [6].
Hospitalization rates also increase with age. Among patients between 65 to 69 years, hospitalization rate was 511 per 100,000 population where as it was 1367 per 100,000 population per year among those over 85 years [15].
The economic impact of AF poses a significant challenge for healthcare systems. The annual cost of AF is about 6–26 billion dollars, mainly due to hospitalizations [16].
15.4 Management Approaches
Approaches to manage AF target on the following issues:
-
1.
Prevention of thromboembolism.
-
2.
Improvement of symptoms.
-
3.
Improvement of quality of life.
The treatment strategies include anticoagulation, rate, or rhythm control of atrial fibrillation. These goals can be achieved either by pharmacological or non-pharmacological approaches.
15.5 Prevention of Thromboembolism
The use of anticoagulants is indicated in patients who have high risk for thromboembolism [8, 9]. Warfarin therapy has been demonstrated to reduce the stroke risk by 64% [17]. In spite of this fact, oral anticoagulant therapy is significantly underused in elderly population. Risk of bleeding, which is seen in 1–13% per year in patients on anticoagulants partly, explains this underuse [14].
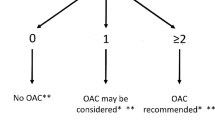
There are different scoring systems to assess the risk of stroke as well as bleeding which assist the clinician to select patients to initiate anticoagulation. Current guidelines recommend anticoagulation for patients with a CHA2DS2-VASc score of more than two unless contraindicated [9, 10]. Scoring systems are available for calculation of bleeding risk including HAS-BLED (hypertension, abnormal liver/renal functions, stroke, bleeding history or predisposition, labile INR, elderly (9 > 65 years), drugs/alcohol use concomitantly). This score is a better discriminator of bleeding risk compared to other scoring systems and if the score is >3, would indicate a higher risk of bleeding. Closer monitoring and risk/benefit analysis is recommended in such cases (Tables 15.1, 15.2, 15.3 15.4 and 15.5).
15.6 Selection of Oral Anticoagulant Medication
Vitamin K antagonists especially warfarin was the only oral anticoagulant agent available since the 1950s till recently. With the introduction of direct thrombin inhibitors and factor Xa inhibitors, the options are now open to more convenient and flexible anticoagulation regimens. The most studied non-vitamin K-dependent anticoagulants (NOACs) are dabigatran, rivaroxaban, apixaban, and edoxaban.
Warfarin has been used effectively in elderly patients for many decades. However, the major difficulties in managing warfarin in elderly patients are its interaction with food, drugs, alcohol, liver function, age-related variations, and genetic variations. Periodic monitoring of international normalized ratio (INR) and frequent dosage adjustments are required to ensure protection from thromboembolism and prevention of bleeding complications in patients treated with warfarin. The clinical benefits and risks of anticoagulation therapy with warfarin are directly related to the proportion of time that INR values are between 2 and 3, which is designated as time in therapeutic range (TTR) 21. It has been shown that TTR on warfarin is suboptimal, only 59% in ORBIT-AF study analyzing 5210 patients [18].
Another obstacle encountered in warfarin-based anticoagulation is compliance and discontinuation rates. Discontinuation of warfarin therapy has been alarmingly high 25–50% [19, 20].
The use of NOACs circumvents some of these inconveniences of warfarin. NOACs are in clinical use since 2008 and offer similar or better efficacy, safety, convenience, and freedom from frequent laboratory monitoring. There is no age-related dose adjustment for NOACs. Dose adjustments are required for patients with renal dysfunction. NOACs are not recommended for patients with end-stage renal disease on hemodialysis and in patients with mechanical heart valves [9, 10, 21, 22].
When selecting a specific anticoagulant, patient preference, renal function, and cost should be considered.
15.7 Rate and Rhythm Control
Five major prospective randomized trials (PAF2, STAF, PIAF, RACE, and AFFIRM) compared rate control strategy with that of rhythm control, and all of these trials have had similar results [25,26,27,28,27]. Most of the subjects enrolled in the trials were elderly as a reflection of the epidemiology of AF. These studies have shown no advantage of rhythm control strategy over that of rate control. A prespecified subgroup analysis of AFFIRM [27] revealed that rhythm control strategy was associated with higher mortality than rate control. There were no significant differences in functional capacity or cognitive status with either management strategies [28, 29]. Rhythm control strategy is more costly and consumed more resources compared to rate control strategy [30].
In septuagenarians, rate control when compared with rhythm control was associated with lower mortality and hospitalizations [31]. Based on the evidence, rate control is the preferred mode of management on AF in elderly. However rhythm control may be appropriate in certain circumstances such as highly symptomatic patients despite rate control, exercise intolerance, and personal preference.
15.8 Strategies Used for Rhythm Control in AF
The three major approaches for rhythm control in atrial fibrillation are antiarrhythmic drugs, cardioversion which could be chemical or electric, and catheter ablation.
Cardioversion can be safely performed without anticoagulation if the duration of AF is less than 48 h and if there is no risk of stroke. If the duration of AF is more than 48 h, anticoagulation with warfarin (to maintain INR between 2 and 3) or NOACs should be done for at least 3 weeks prior to and 4 weeks after cardioversion. Transesophageal echocardiogram (TEE) can be used to rule out the presence of left atrial/LA appendage thrombus to perform cardioversion acutely if duration of AF of more than 48 h and waiting for 3 weeks on anticoagulation is deemed inappropriate [32]. Cardioversion can be achieved by direct current shock or with the use of antiarrhythmic drugs. Among drugs, flecainide, propafenone, dofetilide, or intravenous ibutilide are considered class 1 of recommendation and amiodarone class II a recommendation for cardioversion of AF.
The decision about continuation of long-term anticoagulation depends on the stroke risk assessed by CHA2DS2-VASC score. AAD is moderately effective in maintaining sinus rhythm in long term after cardioversion; however, the long-term risk benefit of these drugs remains unclear. Among the antiarrhythmic drugs, amiodarone is found to be most effective for maintenance of sinus rhythm with less mortality risk than class 1 drugs, and the choice of AAD depends also on comorbidities of the patient and the presence of underlying structural heart disease [33]. Class 1 drugs should be used with extreme caution in patients with structural heart disease because of the risk of pro-arrhythmia. Regular monitoring of QT interval is recommended in patients on class 3 drugs like sotalol or amiodarone.
15.9 Control of Ventricular Rate
Most of the symptoms in AF is related to tachycardia, and rate control is an attractive and cost-effective strategy in improving the quality of life of AF patients. Rate control can be achieved by AV nodal blocking medications or by AV node ablation and implantation of permanent pacemaker. The common drugs used for ventricular rate control are (1) beta-adrenergic blockers, (2) non-dihydropyridine calcium channel blockers, and (3) digitalis. Both beta-blockers and calcium channel blockers are equally effective in rate control in atrial fibrillation. Digoxin is a lesser preferred drug as a first-line rate control medications except in-patient with systolic heart failure. The mechanism of action of digoxin is by enhancement of vagal tone on AV node and useful for rate control at rest. Because of the vagal withdrawal associated with exertion, digoxin is not a very useful drug for exercise related tachycardia, which is fairly common in atrial fibrillation. A narrow therapeutic window, interaction with other cardiac drugs and warfarin, and propensity for toxicity with declining renal function on elderly make digoxin a less favorable drug in management of atrial fibrillation.
Another important consideration is about the target heart rates while attempting rate control. A more lenient rate control (resting heart rate < 110 bpm) is found non-inferior to more strict rate control of resting heart rate < 80 bpm and heart rate < 110 with exercise in a randomized controlled trial of permanent AF in patients [34]. Another study compared three strategies of rate control and found no difference in clinical outcomes [35].
Guidelines recommend a stricter rate control of resting heart rate < 80 bpm in symptomatic cases (class IIa). For asymptomatic patients with preserved LV function, a more lenient rate control (<110 bpm) is reasonable (class IIb) to prevent tachycardiomyopathy.
15.10 Non-pharmacological Approaches in Management of AF
Non-pharmacological approaches in AF include catheter ablation, surgical ablation, and left atrial appendage occlusion.
15.11 Role of Catheter Ablation of AF in Elderly Population
Catheter ablation (pulmonary vein isolation) is a class 1 indication for drug refractory (to at least one class1 or class 3 antiarrhythmic drug) paroxysmal AF. Results of catheter ablation in octogenarian patients are comparable to younger patients, and complication rates were not greater [36]. Age over 65 is found to be a factor for progression of AF in spite of initial success [37]. In patients over 75 years undergoing AF ablation and those maintaining sinus rhythm, mortality and stroke rates are lower than those in AF (failed ablations or non-ablated cases) [38].
Surgical MAZE procedure is recommended for patients undergoing cardiac surgery for other reasons (class IIa), and results are comparable in elderly patients [39].
Left atrial appendage occlusion or excision is a non-pharmacologic therapy for stroke prevention in non-valvular AF patients who are at high risk for bleeding with anticoagulation. It is a class IIb indication in patients undergoing cardiac surgery [40]. Percutaneous LAA closure devices are also used in this patient subgroup. Percutaneous LAA occlusion using Watchman™ device has been approved for patients who are at high risk for stroke and bleeding.
A meta-analysis of two randomized trials of LAA occlusion has shown improved rates of hemorrhagic stroke, cardiovascular/unexplained death, and bleeding compared to warfarin [41].
Currently the US clinical guidelines for management of AF does not include recommendations for the use of LAA closure devices for stroke prevention because only one device (Watchman™ from Boston Scientific) has been approved by the USFDA. Currently Watchman™ is the only device, which has undergone testing against warfarin therapy, which is considered as the gold standard for anticoagulation. The focused update by the European Society of Cardiology (ESC) in 2012 for the management of AF provides a relatively weak recommendation for LAA closure/occlusion/excision with percutaneous technologies. The procedure is recommended in patients at high risk for stroke unable to take long-term anticoagulation (class IIb recommendation, level of evidence B) [9] (Fig. 15.1).
Algorithm for stroke prevention in atrial fibrillation. LAA left atrial appendage, NOAC non-vitamin K antagonist oral anticoagulant, OAC oral anticoagulant (adapted from Ref. 42)
Conclusions
Atrial fibrillation is the commonest sustained arrhythmia in clinical practice, and the incidence and prevalence increases with age. AF is associated with significant morbidity and mortality and has huge impact on healthcare system. Management of AF should include stroke prevention by the use of anticoagulation and control of ventricular rates either by rate control or rhythm control strategies to improve symptoms and quality of life. The decision of rate or rhythm control should be individualized as there are no significant differences in hard clinical outcomes between these approaches. Advent of NOACS, improvement is catheter-based technologies for ablative treatments, and strategies for LAA occlusion/exclusion for stroke prevention are some of the advances made in the field of management of atrial fibrillation. Ongoing research and randomized trials will help in refining the pharmacotherapy as well as interventional management of atrial fibrillation.
Case Continued
Mr. Smith’s case provides an opportunity to review the management options in a case of AF and heart failure. Being hemodynamically unstable, he needs cardioversion, which is best achieved by DC shock. Since the duration of AF is not clear and the stroke risk being very high, ideal strategy is to perform a TEE and cardioversion after exclusion of an LAA thrombus. Long-term anticoagulation is required, and choice of medication is either warfarin or apixaban in view of lower GFR. Mr. Smith’s LV function is 40%, which could be primary cardiomyopathy or tachycardiomyopathy. A repeat echocardiogram after restoration of sinus rhythm would aid in making the distinction. Both rate control and rhythm control can be attempted in this case to prevent tachycardiomyopathy. In view of LVH and LV dysfunction, the only useful antiarrhythmic drug is amiodarone in this case. Amiodarone intolerance and recurrence of symptomatic AF are indication of non-pharmacologic approaches for rate or rhythm control by catheter ablation. AV node ablation and pacemaker implantation or pulmonary vein /LA ablation for rhythm control are strategies for rate control and rhythm control, respectively. A decision for long-term management should be made based on a consensus between the patient and the physician.
Mr. Smith underwent a TEE, which was followed by electrical cardioversion. He was loaded with amiodarone with a dose of 10 g over 3 weeks and a maintenance dose of 200 mg. Anticoagulation was initiated with apixaban 2.5 mg BID. In view of his LV dysfunction, beta blockade with bisoprolol and ACE inhibition with small dose of ramipril were started with continued monitoring of renal functions. A long-term plan for AV nodal ablation with permanent pacemaker implantation was discussed in case if he becomes drug refractory or develops side effects from medications. Six monthly liver function and thyroid function assessments, yearly chest X rays, and ophthalmic examinations were planned as a part of his follow-up as he is on amiodarone.
References
Heeringa J, van der Kuip DA, Hofman A, Kors JA, VanHerpen G, Stricker BHC, Stijnen T, Lip GYH, Witteman JCM. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur Heart J. 2006;27:e949–53.
Donoghue OA, Jansen S, Dooley C, De Rooij S, Van DerVelde N, Kenny RA. Atrial fibrillation is associated with impaired mobility in community-dwelling older adults. J Am Med Dir Assoc. 2014;15(12):929–33.
Kirchhoff P, Ammenorp B, Darius H, et al. Management of atrial fibrillation in seven European countries after the publication of 2010 ESC guidelines for atrial fibrillation. Primary results of the PREvention of thromboembolic events—European registry in Atrial Fibrillation (PREFER in AF). Europace. 2014;16(1):6–14.
Zallo MA. Atrial regulation of intravascular volume: observations on the tachycardia-Polyureasyndrome. Am Heart J. 1991;122(1 pt 1):188–94.
Maisel WH, Stevenson LW. Atrial fibrillation in heart failure: epidemiology, pathophysiology and rationale for therapy. Am J Cardiol. 2003;91(6A):2D–8D.
Boriani G, Laroche C, Diemberger I, et al. Asymptomatic atrial fibrillation: clinical correlates, management and outcomes in the EORP-AF pilot general registry. AM J Med. 2015;128(5):509–18.e2.
Benjamin EJ, Wolf PA, D’Agostino RB, et al. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation. 1998;98(10):946–52.
European Heart Rhythm Association; European Association for Cardio-Thoracic Surgery, Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S, Van Gelder IC, Al-Attar N, Hindricks G, Prendergast B, Heidbuchel H, Alfieri O, Angelini A, Atar D, Colonna P, De Caterina R, De Sutter J, Goette A, Gorenek B, Heldal M, Hohloser SH, Kolh P, LeHeuzey JY, Ponikowski P, Rutten FH. Guidelines for the management of atrial fibrillation: The Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J. 2010;31(19):2369–429.
Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the Euro Heart Survey on atrial fibrillation. Chest. 2010;137(2):263–72.
January CT, Wann LS, Alpert JS, Calkins H, Cleveland JC Jr, Cigarroa JE, Conti JB, Ellinor PT, Ezekowitz MD, Field ME, Murray KT, Sacco RL, Stevenson WG, Tchou PJ, Tracy CM, Yancy CW. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64(21):e1–76.
Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138(5):1093–100. doi:10.1378/chest.10-0134.
Jacobs V, Cutler MJ, Day JD, Bunch TJ. Atrial fibrillation and dementia. Trends Cardiovasc Med. 2015;25(1):44–51.
Kazemian P, Oudit G, Jugdutt BI. Atrial fibrillation and heart failure in the elderly. Heart Fail Rev. 2012;17(4–5):597–613.
Hanon O, Assayag P, Belmin J, Collet JP, Emeriau JP, Fauchier L, Forette F, Friocourt P, Gentric A, Leclercq C, Komajda M, Le Heuzey JY, French Society of Geriatrics and Gerantology; French Society of Cardiology. Expert consensus of the French Society of Geriatrics and Gerontology and the French Society of Cardiology on the management of atrial fibrillation inelderly people. Arch Cardiovasc Dis. 2013;106(5):303–23.
Naderi S, Wang Y, Miller AL, Rodriguez F, Chung MK, Radford MJ, Foody JM. The impact of age on the epidemiology of atrial fibrillation hospitalizations. Am J Med. 2014;127(2):158.e1–7.
Kim MH, Johnston SS, Chu BC, Dalal MR, Schulman KL. Estimation of total incremental health care costs in patients with atrial fibrillation in the United States. Circ Cardiovasc Qual Outcomes. 2011;4:313–20.
Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007;146:857–67.
Pokorney SD, Simon DN, Thomas L, Fonarow GC, Kowey PR, Chang P, Singer DE, Ansell J, Blanco RG, Gersh B, Mahaffey KW, Hylek EM, Go AS, Piccini JP, Peterson ED, Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF) Investigators. Patients’ time in therapeutic range on warfarin among US patients with atrial fibrillation: results from ORBIT-AF registry. Am Heart J. 2015;170(1):141–148., 148.e1, Epub 1 Apr 2015. doi:10.1016/j.ahj.2015.03.017.
Spivey CA, Qiao Y, Liu X, Mardekian J, Parker RB, Phatak H, Claflin AB, Kachroo S, Abdulsattar Y, Chakrabarti A, Wang J. Discontinuation/interruption of warfarin therapy in patients with nonvalvular atrial fibrillation. J Manag Care Spec Pharm. 2015;21(7):596–606.
Fang MC, Go AS, Chang Y, Borowsky LH, Pomernacki NK, Udaltsova N, Singer DE. Warfarin discontinuation after starting warfarin for atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2010;3(6):624–31.
da Silva RM. Novel oral anticoagulants in non-valvular atrial fibrillation. Cardiovasc Hematol Agents Med Chem. 2014;12(1):3–8.
Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz MD, Camm AJ, Weitz JI, Lewis BS, Parkhomenko A, Yamashita T, Antman EM. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955–62.
Brignole M, Menozzi C, Gasparini M, Bongiorni MG, Botto GL, Ometto R, Alboni P, Bruna C, Vincenti A, Verlato R, PAF 2 Study Investigators. An evaluation of the strategy of maintenance of sinus rhythm by antiarrhythmic drug therapy after ablation and pacing therapy in patients with paroxysmal atrial fibrillation. Eur Heart J. 2002;23:892–900.
Carlsson J, Miketic S, Windler J, et al. Randomized trial of rate-control versus rhythm-control in persistent atrial fibrillations: (STAF) strategies of treatment of atrial fibrillation study. J Am Coll Cardiol. 2003;41:1690–6.
Hohnloser SH, Kuck KH, Lilienthal J. Rhythm or rate control in atrial fibrillation—pharmacological intervention in atrial fibrillation (PIAF): a randomised trial. Lancet. 2000;356:1789–94.
Van Gelder IC, Hagens VE, Bosker HA, et al. Rate control versus electrical cardioversion for persistent atrial fibrillation (RACE) study group. N Engl J Med. 2002;347:1834–40.
Wyse DG, Waldo AL, DiMarco JP, et al. The atrial fibrillation follow-up investigation of rhythm management (AFFIRM) investigators. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002;347:1825–33.
Jenkins LS, for the NHLBI AFFIRM Quality of Life Substudy Investigators. Quality of life in patients with atrial fibrillation and risk factors for stroke and death: an AFFIRM substudy. PACE 2002. Presented at annual scientific sessions of the north American Society of Pacing and Electrophysiology as a late-breaking clinical trial; May 11, 2002, San Diego, CA.
Gronefeld GC, Lilienthal J, Kuck KH, Hohnloser SH, for the Pharmacological Intervention in Atrial Fibrillation (PIAF) Study Group. Impact of rate versus rhythm control on quality of life in patients with persistent atrial fibrillation. Results from a prospective randomized trial. Eur Heart J. 2003;24:1430–6.
Marshall AD, Levy AR, Vidaillet H, et al. Cost-effectivenessof rhythm versus rate control for treatment of atrial fibrillation: results from the AFFIRM study. Ann Intern Med. 2004;141:653–61.
Shariff N, Desai RV, Patel K, Ahmed MI, Fonarow GC, Rich MW, Aban IB, Banach M, Love TE, White M, Aronow WS, Epstein AE, Ahmed A. Rate-control versus rhythm-control strategies and outcomes in septuagenarians with atrial fibrillation. Am J Med. 2013;126(10):887–93.
Klein AL, Grimm RA, Murray RD, Apperson-Hansen C, Asinger RW, Black IW, Davidoff R, Erbel R, Halperin JL, Orsinelli DA, Porter TR, Stoddard MF. Use of transesophageal echocardiography to guide cardioversion in patients with atrial fibrillation. N Engl J Med. 2001;344:1411–20.
Lafuente-Lafuente C, Mouly S, Longás-Tejero M, Mahé I, Bergmann J. Antiarrhythmic drugs for maintaining sinus rhythm after cardioversion of atrial fibrillation: a systematic review of randomized controlled trials. Arch Intern Med. 2006;166(7):719–28.
Van Gelder IC, Groenveld HF, Crijns HJ, Tuininga YS, Tijssen JG, Alings AM, Hillege HL, Bergsma-Kadijk JA, Cornel JH, Kamp O, Tukkie R, Bosker HA, Van Veldhuisen DJ, Van den Berg MP, RACE II Investigators. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010;362(15):1363–73.
Groenveld HF, Tijssen JG, Crijns HJ, Van den Berg MP, Hillege HL, Alings M, Van Veldhuisen DJ, Van Gelder IC, RACE II Investigators. Rate control efficacy in permanent atrialfibrillation: successful and failed strict rate control against a background of lenient rate control: data from RACE II (rate control efficacy in permanent atrial fibrillation). J Am Coll Cardiol. 2013;61(7):741–8.
Bunch TJ, Weiss JP, Crandall BG, May HT, Bair TL, Osborn JS, Anderson JL, Lappe DL, Muhlestein JB, Nelson J, Day JD. Long-term clinical efficacy and risk of catheter ablation for atrial fibrillation in octogenarians. Pacing Clin Electrophysiol. 2010;33(2):146–52.
Takigawa M, Takahashi A, Kuwahara T, Okubo K, Takahashi Y, Watari Y, Takagi K, Fujino T, Kimura S, Hikita H, Tomita M, Hirao K, Isobe M. Long-term follow-up after catheter ablation of paroxysmal atrial fibrillation: the incidence of recurrence and progression of atrial fibrillation. Circ Arrhythm Electrophysiol. 2014;7(2):267–73.
Nademanee K, Amnueypol M, Lee F, Drew CM, Suwannasri W, Schwab MC, Veerakul G. Benefits and risks of catheter ablation in elderly patients with atrial fibrillation. Heart Rhythm. 2015;12(1):44–51.
Nakamura T, Izutani H, Sawa Y. Mid-term outcomes of the modified Cox-maze procedure for elderly patients: a risk analysisfor failure. Interact Cardiovasc Thorac Surg. 2011;12(6):924–8.
Van Wagoner DR, Piccini JP, Albert CM, Anderson ME, Benjamin EJ, Brundel B, Califf RM, Calkins H, Chen PS, Chiamvimonvat N, Darbar D, Eckhardt LL, Ellinor PT, Exner DV, Fogel RI, Gillis AM, Healey J, Hohnloser SH, Kamel H, Lathrop DA, Lip GY, Mehra R, Narayan SM, Olgin J, Packer D, Peters NS, Roden DM, Ross HM, Sheldon R, Wehrens XH. Progress toward the prevention and treatment of atrial fibrillation: a summary of the Heart Rhythm Society Research Forum on the Treatment and Prevention of Atrial Fibrillation, Washington, DC, December 9–10, 2013. Heart Rhythm. 2015;12(1):e5–e29.
Holmes DR Jr, Doshi SK, Kar S, Price MJ, Sanchez JM, Sievert H, Valderrabano M, Reddy VY. Left atrial appendage closure as an alternative to warfarin for stroke prevention in atrial fibrillation: a patient-level meta-analysis. J Am Coll Cardiol. 2015;65(24):2614–23. doi:10.1016/j.Jacc.2015.04.025.
Meier B, Blaauw Y, Khattab AA, Lewalter T, Sievert H, Tondo C, Glikson M. EHRA/EAPCI expert consensus statement on catheter-based left atrial appendage occlusion. EuroIntervention. 2015;10(9):1109–25.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 The Editor(s)
About this chapter
Cite this chapter
Divakara Menon, S.M. (2018). Special Problems in Management of Atrial Fibrillation in the Elderly. In: Nair, B. (eds) Geriatric Medicine. Springer, Singapore. https://doi.org/10.1007/978-981-10-3253-0_15
Download citation
DOI: https://doi.org/10.1007/978-981-10-3253-0_15
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-3252-3
Online ISBN: 978-981-10-3253-0
eBook Packages: MedicineMedicine (R0)