Abstract
Intravascular ultrasound (IVUS) provides anatomic information regarding the coronary artery lumen, wall, and plaques, which can help the accurate evaluation of lesion characteristics with vessel sizing. In addition, after stent implantation, underexpansion, malapposition, or edge dissections can be detected by IVUS. Thus, through further intervention based on these IVUS findings, stent optimization can be achieved, causing the improved clinical outcomes. Current guidelines recommend the use of IVUS to optimize stent implantation for select patients (Class of recommendation IIa, Level of evidence B) [1, 2]. However, recently, many evidences demonstrating the clinical usefulness of IVUS have been accumulated since the prior guidelines were released. In this chapter, clinical evidences of IVUS-guided percutaneous coronary intervention (PCI) will be discussed from observational studies, randomized studies, and meta-analysis.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Intravascular ultrasound (IVUS) provides anatomic information regarding the coronary artery lumen, wall, and plaques, which can help the accurate evaluation of lesion characteristics with vessel sizing. In addition, after stent implantation, underexpansion, malapposition, or edge dissections can be detected by IVUS. Thus, through further intervention based on these IVUS findings, stent optimization can be achieved, causing the improved clinical outcomes. Current guidelines recommend the use of IVUS to optimize stent implantation for select patients (Class of recommendation IIa, Level of evidence B) [1, 2]. However, recently, many evidences demonstrating the clinical usefulness of IVUS have been accumulated since the prior guidelines were released. In this chapter, clinical evidences of IVUS-guided percutaneous coronary intervention (PCI) will be discussed from observational studies, randomized studies, and meta-analysis.
1 Clinical Studies Evaluating Clinical Usefulness of IVUS-Guidance PCI
Several randomized clinical trials were performed to demonstrate clinical usefulness of IVUS-guidance during PCI. Recently conducted randomized controlled trials comparing IVUS-guidance vs. angiography-guidance particularly using the drug-eluting stent (DES) are summarized in Table 5.1 [3,4,5,6,7,8,9,10]. The first two trials by Jakabacin et al. and Cheiffo et al. failed to prove the clinical benefit of IVUS-guidance because of relatively small number of patients, less than 150 patients in each group were included in their studies [3, 4]. Kim et al. reported that IVUS usage for diffuse long lesions was associated with improved clinical outcomes particularly when used by operators’ decision. In the per-protocol analysis, IVUS-guidance group significantly had lower 1-year major adverse cardiovascular event (MACE) (4.0% vs. 8.1%, p = 0.048), although the strategy of routine IVUS for DES implantation did not improve the MACE rates in the intention-to-treat analysis [5]. Recent randomized trials which showed statistically significant clinical benefit were performed mainly for complex lesions, such as left main lesions [7], chronic total occlusions (CTO) [8, 9], and diffuse long lesions [10]. The CTO-IVUS (Chronic Total Occlusion InterVention with drUg-eluting Stents) study, the first randomized trial for CTO lesions, demonstrated that IVUS-guided PCI may improve 12-month MACE rates after DES implantation when compared with conventional angiography-guided CTO-PCI [8]. In the IVUS-XPL (Impact of Intravascular Ultrasound Guidance on Outcomes of Xience Prime Stents in Long Lesions) trial, IVUS-guided DES implantation compared with angiography-guided DES implantation resulted in a significantly lower rate of the composite of MACE (a composite of cardiac death, myocardial infarction [MI], or target-lesion revascularization [TLR]) at 1 year (2.9% vs. 5.8%, hazard ratio [HR] = 0.48, p = 0.007) [10]. These differences were primarily due to lower risk of TLR (2.5% vs. 5.0%, HR = 0.51, p = 0.02).
According to the ADAPT-DES (The assessment of dual antiplatelet therapy with drug-eluting stents ) study, the most recent largest observational study with all-comers (n = 8583) [11], IVUS was utilized in 3349 patients (39%), and larger-diameter devices, longer stents, and/or higher inflation pressure were used in the IVUS-guided cases. At 1 year, propensity-adjusted multivariable analysis revealed IVUS-guidance vs. angiography-guidance was associated with a reduced definite/probable stent thrombosis (0.6% vs. 1.0%, p = 0.003), MI (2.5% vs. 3.7%, p = 0.004), and composite adjudicated major cardiac events (cardiac death, MI, or stent thrombosis) (3.1% vs. 4.7%, p = 0.002). The benefits of IVUS were especially evident in patients with acute coronary syndromes and complex lesions [11]. Further recent observational studies evaluating clinical usefulness of IVUS-guided PCI are summarized in Table 5.2 [11,12,13,14,15,16,17].
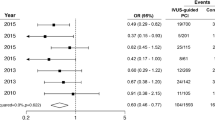
Lastly, meta-analyses comparing the IVUS-guidance and angiography-guidance are presented in Table 5.3 [18,19,20,21,22]. Shin et al. reported the results of meta-analysis with individual patient-level data from 2345 randomized patients. IVUS-guided new-generation DES implantation vs. angiography-guided DES implantation was associated with a favorable outcome, particularly the occurrence of hard clinical endpoint (the composite of cardiac death, MI, or stent thrombosis) for complex lesions [22]. Of note, the primary endpoint of this meta-analysis did not include TLR. Therefore, different from the IVUS-XPL trial showing the benefit of IVUS due primarily to the less frequent TLR events [10], MACEs, even excluding the TLR events in this meta-analysis, were less frequent with IVUS-guidance than angiography-guidance [22].
2 Left Main Lesion
Procedural complication or failure of left main lesion of PCI is critical. Thus, IVUS-guidance PCI for left main lesion is currently recommended as a class IIa or class IIb recommendation [1, 2]. In addition to the stent optimization, particularly for left main lesions, functionally significant lesion can be relatively accurately predicted by IVUS examination for intermediate lesions because of the limited variability of left main coronary artery length, diameter, and the amount of supplied myocardium. Minimal lumen area (MLA) less than 4.5 mm2 predicted the fractional flow reserve (FFR) less than 0.80 with sensitivity of 77% and specificity of 82% [23]. Other studies also reported the optimal cut-off value of MLA by IVUS for predicting functionally significant left main lesions (FFR less than 0.75) were 5.9 mm2 and 4.8 mm2, respectively [24, 25]. IVUS is also essential for the optimization to reduce the restenosis. A previous study showed that the cut-off values of post-stenting MLA that best predicted in-stent restenosis were 5.0 mm2 in ostial left circumflex, 6.3 mm2 in ostial left anterior descending, 7.2 mm2 in polygon of confluence, and 8.2 mm2 in left main [26].
Recently, a randomized trial for unprotected left main lesions revealed that IVUS-guided group had a lower composite of death, non-fatal MI, or TLR (13.1% vs. 29.3%, p = 0.031), although small number of patients were studied in this study [7]. Also, a recent pooled analysis from 4 Spanish registries demonstrated that IVUS-guided DES implantation for unprotected left main showed a lower 3-year composite rate of cardiac death, MI, and TLR compared with the angiography-guided DES implantation (11.3% vs 16.4%, p = 0.04), and a more prominent in the subgroup with distal left main lesions (10.0% vs 19.3%, p = 0.03) [17].
3 Bifurcation Lesion
There were no randomized studies performed particularly for the bifurcation lesions . According to the observational studies, Kim et al. demonstrated that the 3-year cumulative incidence of death or MI was significantly lower in the IVUS-guided PCI group than the angiography-guided PCI group (3.8% vs 7.8%, p = 0.03) [15]. Another observational study with bifurcation lesions, the rate of TLR was significantly lower in the IVUS-guided PCI group (6% vs 21%, p = 0.001) [27]. In the first study, two-stent technique and final kissing balloon were more frequently used in the IVUS-guidance group [15], whereas in the second study, the number of implanted stents was significantly lower in the IVUS-guidance group [27]. In this regard, although further studies are needed to determine the optimal stent strategies including the stent number particularly for bifurcation lesions, the role of IVUS for the decision of stent strategies may be important to improve clinical outcomes for the complex bifurcation lesions. A previous study evaluated the IVUS parameters predicting the IVUS ≥4 mm2 at 9-month follow-up IVUS for both main vessel and side branch after bifurcation T-stenting with first-generation DES [28]. Inadequate post-procedural minimal stent area (MSA) with increased neointimal hyperplasia may cause the side branch ostium to be the most frequent restenotic site after bifurcation PCI and the optimal cut-off value of post-procedural MSA was 4.83 mm2 [28].
4 Chronic Total Occlusion
The roles of IVUS for CTO intervention could be classified into 3 different uses: (1) wire-crossing for the stumpless CTO lesions, (2) pre-stenting use, and (3) post-stent use. For the stumpless CTO lesions, IVUS-guidance has been reported to lead a higher success rate and to be useful in revealing the entry point of occlusion and in repositioning a guidewire in the event of inadvertent sub-intimal passage [29]. Pre-stenting IVUS could provide the accurate information regarding vessel size and lesion length and cause resultant appropriate stent size and length for stent optimization. CTO vessel often increases in size following the successful CTO PCI. An IVUS follow-up study at 6 month after CTO PCI revealed that distal lumen diameter was increased in two thirds of patients by 0.4 mm (p < 0.001) [30]. Post-stent IVUS may detect PCI complications or suboptimal stent expansion and could lead to stent optimization and finally can decide the need for additional stenting or ballooning. However, there had been a lack of evidence regarding the beneficial role of IVUS-guided CTO intervention using current-generation DES for the improved clinical outcomes after stent implantation. Two randomized trials were performed particularly for CTO lesions [8, 9]. In the CTO-IVUS trial, 402 patients with CTOs were randomized to the IVUS-guided group (n = 201) or the angiography-guided group (n = 201) after successful guidewire crossing [8]. Although IVUS-guided CTO intervention did not significantly reduce cardiac mortality, IVUS-guided CTO intervention improved 12-month MACE rate after new-generation DES implantation when compared with conventional angiography-guided CTO intervention. In this study, IVUS-guidance group had a higher proportion of high-pressure post-stent dilation (51% vs. 41%, p = 0.045) with a higher maximum post-stent balloon pressure (14.6 vs. 13.8 atm, p = 0.040). Consequently, the post-procedural minimal lumen diameter was significantly larger in the IVUS-guidance vs. angiography-guidance (2.64 vs. 2.56 mm, p = 0.025).
In the second randomized trial, Tian et al. reported stent late lumen loss at 1 year between IVUS- vs. angiography-guidance [9]. Late lumen loss was significantly lower in the IVUS-guided group compared with the angiography-guided group (0.28 vs 0.46 mm, p = 0.025), although these angiographic findings were not translated into the improvement of clinical outcomes.
5 Diffuse Long Lesion
A long lesion inevitably increases the length of implanted stent, and long stent increases the incidence of stent underexpansion. In the IVUS-XPL enrolling 1400 patients requiring ≥28 mm everolimus-eluting stents, adjunct post-stent balloon dilation was more frequently performed in the IVUS-guided stent group (76%) than in the angiography-guided stent group (76% vs 57%, p < 0.001) [10]. The mean final balloon size was larger in the IVUS-guided group than in the angiography-guided group. On post-procedural quantitative angiography analysis, minimum lumen diameter was greater and diameter stenosis was smaller in the IVUS-guided stent group than in the angiography-guided stent group [10]. In addition, in the post hoc analysis in that study among the patients within the IVUS-guided stent group, the patients who did not meet the IVUS criteria (n = 315, 46%) had a significantly higher incidence of the primary endpoint compared with those meeting the IVUS criteria for stent optimization (n = 363, 54%) (4.6% vs 1.5%, p = 0.02), when IVUS criteria for stent optimization after PCI was defined as an MLA greater than the lumen cross-sectional area at the distal reference segments [10].
6 In-Stent Restenosis
The use of IVUS to guide PCI for the treatment of restenosis is a class IIa recommendation in the current PCI guidelines [1, 2]. IVUS can differentiate whether restenosis is related to intimal hyperplasia or mechanical complications, such as stent fracture or underexpansion. According to the recent IVUS study comparing the mechanisms and patterns of in-stent restenosis among bare metal stents and DES, restenotic first- and second-generation DES were characterized by less neointimal hyperplasia, smaller stent areas, longer stent lengths, and more stent fractures [31].
7 Patients with Chronic Kidney Disease
Patients with chronic kidney disease (CKD) comprise a challenging subset of patients because of the increased incidence of contrast-induced acute kidney injury following angiography and PCI. Considerable efforts have been made to reduce contrast volume particularly in patients with CKD. Although most randomized clinical trials measured clinical or angiographic outcomes, the MOZART (Minimizing cOntrast utiliZation With IVUS Guidance in coRonary angioplasty) trials measured the total volume contrast agent used during PCI as the primary endpoint [6]. In this trial, a total of 83 patients with a high risk of contrast-induced acute kidney injury or volume overload were randomized to IVUS-guided PCI or angiography-guided PCI, and IVUS group had a lower total volume of contrast (20 ml vs. 65 ml, p < 0.001). Also, recent another study with a total of 31 patients with advanced CKD (creatinine = 4.2 mg/dL) revealed that PCI without contrast using IVUS and physiologic guidance may be performed safely with high procedural success and without complications [32].
8 IVUS Predictors for the Better Clinical Outcomes: Stent Optimization
The IVUS predictors of stent failure after DES implantation are underexpansion, dissections, and significant plaque burden (Table 5.4) [33,34,35]. When a total of 804 patients who underwent both post-intervention IVUS examination after long everolimus-eluting stent (≥28 mm in length) implantation were analyzed from two randomized trials (RESET trial and IVUS-XPL trial), the predictors of MACE were the post-intervention MLA at the target lesion and the ratio of MLA/distal reference segment lumen area [33]. The MLA and MLA-to-distal reference segment lumen area ratio that best predicted patients with MACE from those without it were 5.0 mm2 and 1.0, respectively. Patients with an MLA < 5.0 mm2 or a distal reference segment lumen area had a higher risk of MACE than those without MACE (HR = 6.2, p = 0.003). Similarly, Song et al. reported that the optimal MSA to predict angiographic restenosis at 9 months were 5.3 mm2 for zotarolimus-eluting stents and 5.4 mm2 for everolimus-eluting stents [34]. Therefore, the confirmation of sufficient MLA by IVUS is important after DES implantation. Figure 5.1 represents the stent underexpansion detected by IVUS examination despite of angiographically acceptable diameter stenosis, suggesting the need of post-stent adjuvant ballooning. Figure 5.2 represents the achievement of sufficient MLA after post-stent adjuvant ballooning.
Representative case showing the stent underexpansion by IVUS despite of angiographically acceptable diameter stenosis. After implantation of everolimus-eluting stent (Xience prime 2.75 × 38 mm, Abbott Vascular) for diffuse stenosis of right coronary artery, the residual stenosis by angiography at proximal portion of the stent was 8.1%, which was angiographically acceptable. However, on IVUS evaluation, the MLA was measured 4.95 mm2 (c), which was smaller than the distal reference lumen area of 5.19 mm2 (a) and less than 5 mm2, suggesting the need of post-stent adjuvant ballooning
Representative case showing the achievement of sufficient minimal lumen area measured by IVUS after post-stent adjuvant ballooning . After post-stent adjuvant ballooning with 3.0 mm-sized non-compliant balloon catheter based on the findings of IVUS, the minimal lumen was increased from 4.95 mm2 to 5.75 mm2. Same patients presented in Fig. 5.1
Kang et al. evaluated IVUS predictors for angiographic edge restenosis after newer generation DES [35]. The predictive cut-off of the reference plaque burden was 56.3% for Endeavor zotarolimus-eluting stents, 57.3% for Resolute zotarolimus-eluting stents, and 54.2% for everolimus-eluting stents. Figure 5.3 presents the representative case showing the need of additional stenting at proximal segment of stent because of edge dissection and residual plaque more than 60%, even though angiographic findings were acceptable.
Representative case showing the need of additional stenting at proximal segment of stent because of edge dissection and residual plaque . Although angiographic findings were acceptable, another stent was additionally implanted at the proximal segment based on the IVUS finding, (c) the dissection at the proximal edge of the stent with (d) residual plaque more than 60%
Although IVUS studies have reported that the late stent malapposition is a predictor of late or very late stent thrombosis, there is no data linking isolated acute stent malapposition without stent underexpansion to early stent thrombosis or restenosis [36].
From the bare-metal stent era, the need for a standard to examine the stent optimization led to the formation of IVUS defined criteria. IVUS criteria for stent optimization used in the recent randomized clinical trials were summarized in Table 5.5 [3, 8,9,10]. Despite the need for a consensus, several different criteria have been employed in different clinical studies. However, according to the previous studies and the criteria used in recent trials, the achievement of sufficient lumen area by IVUS may be imperative.
References
Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention. A report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines and the society for cardiovascular angiography and interventions. J Am Coll Cardiol. 2011;58:e44–122.
Windecker S, Kolh P, Alfonso F, et al. 2014 ESC/EACTS guidelines on myocardial revascularization: the task force on myocardial revascularization of the European society of cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35:2541–619.
Jakabcin J, Spacek R, Bystron M, et al. Long-term health outcome and mortality evaluation after invasive coronary treatment using drug eluting stents with or without the ivus guidance. Randomized control trial. HOME DES IVUS. Catheter Cardiovasc Interv. 2010;75:578–83.
Chieffo A, Latib A, Caussin C, et al. A prospective, randomized trial of intravascular-ultrasound guided compared to angiography guided stent implantation in complex coronary lesions: the AVIO trial. Am Heart J. 2013;165:65–72.
Kim JS, Kang TS, Mintz GS, et al. Randomized comparison of clinical outcomes between intravascular ultrasound and angiography-guided drug-eluting stent implantation for long coronary artery stenoses. JACC Cardiovasc Interv. 2013;6:369–76.
Mariani J Jr, Guedes C, Soares P, et al. Intravascular ultrasound guidance to minimize the use of iodine contrast in percutaneous coronary intervention: the MOZART (minimizing contrast utilization with ivus guidance in coronary angioplasty) randomized controlled trial. JACC Cardiovasc Interv. 2014;7:1287–93.
Tan Q, Wang Q, Liu D, et al. Intravascular ultrasound-guided unprotected left main coronary artery stenting in the elderly. Saudi Med J. 2015;36:549–53.
Kim BK, Shin DH, Hong MK, et al. Clinical impact of intravascular ultrasound-guided chronic total occlusion intervention with zotarolimus-eluting versus biolimus-eluting stent implantation: randomized study. Circ Cardiovasc Interv. 2015;8:e002592.
Tian NL, Gami SK, Ye F, et al. Angiographic and clinical comparisons of intravascular ultrasound- versus angiography-guided drug-eluting stent implantation for patients with chronic total occlusion lesions: two-year results from a randomised AIR-CTO study. EuroIntervention. 2015;10:1409–17.
Hong SJ, Kim BK, Shin DH, et al. Effect of intravascular ultrasound-guided vs angiography-guided everolimus-eluting stent implantation: the ivus-xpl randomized clinical trial. JAMA. 2015;314:2155–63.
Witzenbichler B, Maehara A, Weisz G, et al. Relationship between intravascular ultrasound guidance and clinical outcomes after drug-eluting stents: the assessment of dual antiplatelet therapy with drug-eluting stents (ADAPT-DES) study. Circulation. 2014;129:463–70.
Roy P, Steinberg DH, Sushinsky SJ, et al. The potential clinical utility of intravascular ultrasound guidance in patients undergoing percutaneous coronary intervention with drug-eluting stents. Eur Heart J. 2008;29:1851–7.
Park KW, Kang SH, Yang HM, et al. Impact of intravascular ultrasound guidance in routine percutaneous coronary intervention for conventional lesions: data from the EXCELLENT trial. Int J Cardiol. 2013;167:721–6.
Youn YJ, Yoon J, Lee JW, et al. Intravascular ultrasound-guided primary percutaneous coronary intervention with drug-eluting stent implantation in patients with ST-segment elevation myocardial infarction. Clin Cardiol. 2011;34:706–13.
Kim JS, Hong MK, Ko YG, Choi D, Yoon JH, Choi SH, Hahn JY, Gwon HC, Jeong MH, Kim HS, Seong IW, Yang JY, Rha SW, Tahk SJ, Seung KB, Park SJ, Jang Y. Impact of intravascular ultrasound guidance on long-term clinical outcomes in patients treated with drug-eluting stent for bifurcation lesions: data from a korean multicenter bifurcation registry. Am Heart J. 2011;161:180–7.
Hong SJ, Kim BK, Shin DH, et al. Usefulness of intravascular ultrasound guidance in percutaneous coronary intervention with second-generation drug-eluting stents for chronic total occlusions (from the multicenter Korean-chronic total occlusion registry). Am J Cardiol. 2014;114:534–40.
de la Torre Hernandez JM, Baz Alonso JA, Gomez Hospital JA, et al. Clinical impact of intravascular ultrasound guidance in drug-eluting stent implantation for unprotected left main coronary disease: pooled analysis at the patient-level of 4 registries. JACC Cardiovasc Interv. 2014;7:244–54.
Jang JS, Song YJ, Kang W, et al. Intravascular ultrasound-guided implantation of drug-eluting stents to improve outcome: a meta-analysis. JACC Cardiovasc Interv. 2014;7:233–43.
Ahn JM, Kang SJ, Yoon SH, et al. Meta-analysis of outcomes after intravascular ultrasound-guided versus angiography-guided drug-eluting stent implantation in 26,503 patients enrolled in three randomized trials and 14 observational studies. Am J Cardiol. 2014;113:1338–47.
Elgendy IY, Mahmoud AN, Elgendy AY, et al. Outcomes with intravascular ultrasound-guided stent implantation: a meta-analysis of randomized trials in the era of drug-eluting stents. Circ Cardiovas Interv. 2016;9:e003700.
Steinvil A, Zhang YJ, Lee SY, et al. Intravascular ultrasound-guided drug-eluting stent implantation: an updated meta-analysis of randomized control trials and observational studies. Int J Cardiol. 2016;216:133–9.
Shin DH, Hong SJ, Mintz GS, et al. Effects of intravascular ultrasound-guided versus angiography-guided new-generation drug-eluting stent implantation: meta-analysis with individual patient-level data from 2,345 randomized patients. JACC Cardiovasc Interv. 2016;9:2232.
Park SJ, Ahn JM, Kang SJ, et al. Intravascular ultrasound-derived minimal lumen area criteria for functionally significant left main coronary artery stenosis. JACC Cardiovasc Interv. 2014;7:868–74.
Jasti V, Ivan E, Yalamanchili V, et al. Correlations between fractional flow reserve and intravascular ultrasound in patients with an ambiguous left main coronary artery stenosis. Circulation. 2004;110:2831–6.
Kang SJ, Lee JY, Ahn JM, et al. Intravascular ultrasound-derived predictors for fractional flow reserve in intermediate left main disease. JACC Cardiovasc Interv. 2011;4:1168–74.
Kang SJ, Ahn JM, Song H, et al. Comprehensive intravascular ultrasound assessment of stent area and its impact on restenosis and adverse cardiac events in 403 patients with unprotected left main disease. Circ Cardiovasc Interv. 2011;4:562–9.
Patel Y, Depta JP, Novak E, et al. Long-term outcomes with use of intravascular ultrasound for the treatment of coronary bifurcation lesions. Am J Cardiol. 2012;109:960–5.
Hahn JY, Song YB, Lee SY, et al. Serial intravascular ultrasound analysis of the main and side branches in bifurcation lesions treated with the t-stenting technique. J Am Coll Cardiol. 2009;54:110–7.
Park Y, Park HS, Jang GL, et al. Intravascular ultrasound guided recanalization of stumpless chronic total occlusion. Int J Cardiol. 2011;148:174–8.
Park JJ, Chae IH, Cho YS, et al. The recanalization of chronic total occlusion leads to lumen area increase in distal reference segments in selected patients: an intravascular ultrasound study. JACC Cardiovasc Interv. 2012;5:827–36.
Goto K, Zhao Z, Matsumura M, et al. Mechanisms and patterns of intravascular ultrasound in-stent restenosis among bare metal stents and first- and second-generation drug-eluting stents. Am J Cardiol. 2015;116:1351–7.
Ali ZA, Karimi Galougahi K, Nazif T, et al. Imaging- and physiology-guided percutaneous coronary intervention without contrast administration in advanced renal failure: a feasibility, safety, and outcome study. Eur Heart J. 2016;37:3090–5.
Lee SY, Shin DH, Kim JS, et al. Intravascular ultrasound predictors of major adverse cardiovascular events after implantation of everolimus-eluting stents for long coronary lesions. Rev Esp Cardiol. 2017;70:88.
Song HG, Kang SJ, Ahn JM, et al. Intravascular ultrasound assessment of optimal stent area to prevent in-stent restenosis after zotarolimus-, everolimus-, and sirolimus-eluting stent implantation. Catheter Cardiovasc Interv. 2014;83:873–8.
Kang SJ, Cho YR, Park GM, et al. Intravascular ultrasound predictors for edge restenosis after newer generation drug-eluting stent implantation. Am J Cardiol. 2013;111:1408–14.
Hassan AK, Bergheanu SC, Stijnen T, et al. Late stent malapposition risk is higher after drug-eluting stent compared with bare-metal stent implantation and associates with late stent thrombosis. Eur Heart J. 2010;31:1172–80.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Hong, SJ., Jang, Y., Kim, BK. (2018). Clinical Evidence of Intravascular Ultrasound-Guided Percutaneous Coronary Intervention. In: Hong, MK. (eds) Coronary Imaging and Physiology. Springer, Singapore. https://doi.org/10.1007/978-981-10-2787-1_5
Download citation
DOI: https://doi.org/10.1007/978-981-10-2787-1_5
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-2786-4
Online ISBN: 978-981-10-2787-1
eBook Packages: MedicineMedicine (R0)