Abstract
Population neuroscience is an emerging field of research defined by the intersection of neuroscience with epidemiology. In this chapter, we review large-scale developmental studies conducted in clinical, longitudinal high risk, and typically developing cohorts with neuroimaging. We point out the advantages offered by developmental and neuroimaging research when conducted in epidemiological settings such as better control for confounding and the possibility to enhance generalizability. We discuss the advances in the field that we attribute to population neuroscience approach, for example, the evidence for the maturational delay in ADHD and for the early onset of autistic brain changes preceding symptoms. Current population neuroimaging studies begin to explain the role of a more complex environment such as poverty and abuse, child behavior itself, genes, and their interplay in shaping the structure and function of the human brain. We conclude that the question of how different environmental and genetic factors shape the brain and how the brain predicts child psychiatric behavior can only be addressed in large population-based studies with repeated imaging and behavior assessments using a population neuroscience approach.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
Introduction
Population Neuroscience has the potential to fundamentally change our etiological and diagnostic understanding of child psychiatric disorders like genome wide association have profoundly expanded our understanding of the biology of psychiatric disorders. Population Neuroscience is an emerging field of research defined by the intersection of neuroscience with epidemiology (Paus 2010). In this chapter, we will focus on the often-discounted advantages offered by developmental and neuroimaging research when conducted in epidemiological settings. The technical and scientific advances of brain imaging acquisition, image processing, and analyses have enabled neuroimaging studies of global and regional brain development in typically developing children and adolescents that are large and population-based. These neuroimaging studies now begin to explain the role of environment, behavior, genes, and their interplay in shaping the structure and function of the human brain. Against the background of the complexity of environmental risks and the challenges of quantifying the genetics of complex traits, the question of how environmental and genetic factors shape the brain can only be addressed in large population-based studies (White et al. 2013). Modern child psychiatric research needs population neuroscience to complement basic science.
Neurodevelopmental Studies
Researchers studying neurodevelopmental disorders have a long tradition of conducting investigations that we might wish to term Population Neuroscience now. A neurodevelopmental approach was first put forward by the Scottish psychiatrist Clouston in 1891 when describing psychosis, “in the course of the growth and development of the brain there are liable to occur certain failures in the attainment of a working standard of nervous and nutritional health” (Clouston 1891). In the more than 100 years since, many different psychiatric disorders have been conceptualized as neurodevelopmental disorders, but researchers continue to emphasize the early onset of disorders, the developmental stages, and the delayed development of central nervous functions. The current DSM defines neurodevelopmental disorders as a cluster of different co-occurring disorders including among others attention deficit hyperactivity disorder (ADHD), learning disorders, and autism spectrum disorder (ASD) (American Psychiatric Association 2013). All disorders are characterized by cognitive problems that manifest in infancy or childhood and have a less-remitting course than behavioral or emotional disorders. A male preponderance is found in all neurodevelopmental disorders, although the sex difference in prevalence of clinical and population studies varies (Thapar and Rutter 2015). Neurodevelopmental disorders are multifactorial disorders occurring across a continuum of symptom severity and impairment. Twin studies demonstrated a strong contribution of genetic risks for all neurodevelopmental disorders and indeed, a polygenetic liability threshold model best explains heritability patterns and is in line with the results of genetic studies demonstrating associations across many loci with small effect sizes. However, classification systems and most medical textbooks view neurodevelopmental disorders as a category rather than a set of quantitative dimensions which more or less characterize a disorder. While autism is often viewed as the prototypical neurodevelopmental disorder, schizophrenia and conduct problems are described only by some scientists as neurodevelopmental problems (Lewis and Levitt 2002). The developmental delay in conduct disorders is often less obvious and symptom levels tend to fluctuate more. Epidemiological researchers now commonly use the terms neurodevelopmental problems or disorders much more broadly and even include affective problems.
Many population neuroscience studies focused on prenatal and early life events prior to the imaging era investigated developmental risk factors for schizophrenia. Studies from large birth cohorts demonstrated that in-utero exposure to maternal infections and malnourishment increased the risk of schizophrenia (Bale et al. 2010). However, birth cohort studies have also identified prenatal conditions as risk factors for major depressive disorder such as influenza and famine, again supporting a link between maternal nutrition and offspring neurodevelopment (van Os et al. 1997).
A key piece of evidence underpinning the neurodevelopment hypothesis of disorders has been the delayed attainment of early motor development milestones, such as walking or standing unsupported, in cases with autism, schizophrenia, or affective disorders (Filatova et al. 2017). Various concepts have been used such as pandysmaturation (Fish 1957), fine and gross motor skills (Burton et al. 2016), and motor development milestones. However, delays in motor function and deviant language development are associated with broadly defined psychiatric problems, and in a recent study infant neuromotor development and, in particular, low muscle tone and nonoptimal senses consistently predicted internalizing problems (Serdarevic et al. 2017). More recent work showed that the genetic liability for schizophrenia or autism underlies nonoptimal motor development in early infancy (Serdarevic et al. 2018). In summary, these studies suggest that many genetic and environmental risk factors for these disorders may actually underlie these disorders and that they can manifest in the first weeks of life (Murray et al. 2017). Thus, over time the neurodevelopmental hypothesis has morphed into the Developmental Risk Factor Model and has become an integrative framework underlying Population Neuroscience (Carpenter and Strauss 2017).
Key Population Neuroscience Studies
In the 1980s scientists began to study the brains of children with autism, ADHD, dyslexia, and other developmental disorders with computerized tomography. A few years later the first cross-sectional studies followed comparing cases with neurodevelopmental disorders to controls using magnetic resonance imaging (MRI). MRI allows unprecedented access to the anatomy and physiology of the children’s brains (Giedd and Rapoport 2010). These were cross-sectional studies conducted for various disorders; the studies can be criticized for their small sample size (typically less than 50 cases) (Szucs and Ioannidis 2017), the broad age range, the referral bias leading to chronic and medicated cases, and the unsystematic selection of healthy controls. While researchers were able to demonstrate numerous unspecific brain morphological and functional correlates of disorders such as autism, ADHD, and learning disorders, they have arguably failed to advanced our knowledge of the etiology, diagnosis, or prognosis of child psychiatric disorders. Imaging in child psychiatry has not become a routine clinical utility and these early studies had little impact on clinical understanding or practice.
Population Neuroscience addresses these shortcomings employing a range of different study designs. First, follow-up studies of clinical cases are well suited to investigate prognosis, both prognosis under treatment and the natural course of a disorder. Second, follow-up studies in high risk populations such as nonaffected siblings or offspring of persons with a disorder can address the etiology and the onset of symptoms. Finally, large neuroimaging studies of typical developing children can help address selection bias inherent to clinical studies, test symptoms of the disorder along the continuum of disease and if designed longitudinally, can test both etiology and prognosis. Seminal studies utilizing these designs will be discussed to illustrate the challenges and key results. Most studies use T1 and less often T2 weighted structural imaging sequences, diffusion tensor imaging and in the last 10 years added resting state imaging sequences to the protocol. Only very large studies have introduced task-based MRI and few of these studies can be viewed epidemiological work.
Longitudinal Clinical Studies
Longitudinal clinical studies are ideally suited to address prognosis. In a series of seminal studies, Shaw and colleagues studied brain development in more than 220 children and adolescents with ADHD. In an early follow-up study of 2007, they calculated trajectories of cortical thickness and modeled the peak age of cortical thickness, which follows an inverted U-shaped trajectory (Shaw et al. 2007). They showed that the regional pattern of maturation was similar between cases and controls with primary sensory areas attaining peak thickness earlier than higher order association areas. However, there was a marked delay in ADHD in attaining peak cortical thickness throughout most of the cerebrum, on average about 2 years. The delay was most prominent in prefrontal regions, important for control of cognitive processes including attention and motor planning. This study provided the first neuroanatomic documentation of a maturational delay in ADHD, or any neurodevelopmental disorder, using repeated neuroimaging assessments. In a study of the same population with longer follow-up, the group was able to show that the rate of cortical thinning in the prefrontal cortex increased in parallel with the number of adult symptoms, particularly inattentive symptoms (Shaw et al. 2013). While those with persistent ADHD had a fixed, nonprogressive deficit, the trajectories of cortical thickness among persons with ADHD converged toward typical dimensions among those who remitted. This observation has implications for etiological and clinical research, in particular prognosis, as it suggests patients with ADHD may make the neurodevelopmental delay good. Clearly, these results show the importance of repeated MRI measures in longitudinal designs and of including healthy controls. Also, other longitudinal studies of ADHD have replicated the reductions in cortical volume, surface area, and gyrification particularly in frontal areas (Ambrosino et al. 2017).
Studies of children with autism have consistently identified a subset of children with enlarged head circumference. However, better designed studies with locally recruited controls less often show brain overgrowth as measured by head circumference in autism; thus, these findings may reflect generalizable norm biases rather than a disease-specific biomarker (Raznahan et al. 2013). Reviewing MRI studies, Courchesne and colleagues demonstrated that total brain enlargement is indeed present in children with ASD aged 2 to 4 years but not in older children and adolescents (Redcay and Courchesne 2005). Based on such cross-sectional MRI studies, researchers hypothesized that the brain in children with autism undergoes an abnormal growth trajectory that includes a period of early overgrowth. However, this has never been confirmed by a longitudinal study. Several longitudinal clinical studies of children with autism and controls aged 1.5–2 years at baseline have been performed. This work has demonstrated brain and precocious amygdala enlargement in young children with autism, but although the magnitude of enlargement was slightly greater at 50 months, the relative growth patterns remain unclear due to the late age of inclusion after 1.5 years (Schumann et al. 2010). Moreover, the study base (the population from which the research draws on) of these imaging studies is often not well defined, this implying that convenient control sampling can easily introduce bias.
High-Risk Studies
High-risk studies address causality and examine neurodevelopment before disorder occurrence.
First-degree relatives of persons with an ASD are at increased risk for ASD-related characteristics. This provides the opportunity to assess siblings, some of which will later develop the disorder. Prospective brain imaging studies of infants at high familial risk for ASD are better suited to identify early postnatal changes in brain characteristics occurring before the emergence of clear clinical symptoms that lead to an ASD diagnosis. In such a neuroimaging study of 106 infants at high familial risk of ASD and 42 controls, researchers showed that cortical surface area hyper-expansion between 6 and 12 months of age precedes brain volume overgrowth in those diagnosed with autism later (Hazlett et al. 2017). Similarly, the aberrant development of white matter pathways precedes the manifestation of autistic symptoms. In a prognostic study, other work has shown that that functional connectivity measured by MRI at around 6 months correctly identified which individual children would receive a research clinical best-estimate diagnosis of ASD at 24 months of age (Emerson et al. 2017). Not only do we learn from brain imaging measures using this approach; a prospective high risk study of infants later diagnosed with ASD showed a decline in eye fixation within the first 2 to 6 months of life (Jones and Klin 2013).
In ADHD and substance abuse, sibling designs have largely been used to study the effect of discordant exposure, for example, to explore the association between intra-uterine exposure to alcohol or smoking and ADHD (Donovan and Susser 2011; Obel et al. 2011). Others examined how siblings’ facilitation mediates the association between older and younger sibling alcohol use in late adolescence (Samek et al. 2015).
Studies dating back to the 1950s have yielded evidence of developmental risk factors and antecedents in offspring of patients with schizophrenia, including delayed psychomotor milestones or greater neurological soft signs (Rieder and Nichols 1979). Imaging in offspring of individuals with schizophrenia, mostly conducted cross-sectionally (Sugranyes et al. 2017), showed lower grey matter volume as biomarkers of risk for psychiatric disorders. The Edinburgh High Risk Study followed up 162 individuals at high genetic risk of schizophrenia and showed reductions in cerebral volume that were not found in control subjects (McIntosh et al. 2011). Changes in brain structure were also associated with increasing psychotic symptom severity as people developed schizophrenia.
Studies of Typically Developing Children and Adolescents
Large neuroimaging studies of typically developing children and adolescents have provided valuable information on global and regional developmental trajectories of brain development (White 2015). The initial studies excluded children with psychiatric problems, but as these imaging studies include follow-up assessments and become larger and population-based, they epitomize Population Neuroscience addressing etiology, diagnosis, and prognosis. The table below shows population neuroimaging cohorts in children and adolescents with more than 500 participants.
Cohort | Imaging sequences | N (largest wave) | Age at imaging baseline | Follow-up assessments |
Population-based cohorts | ||||
Saguenay youth study | sMRI, MRT | 1024 | 12–18 years | 1 wave |
Generation R | sMRI, DTI, rs-fMRI | 3992 | 6–12 years | 2 waves, ongoing |
Philadelphia neurodevelopmental cohort | sMRI, DTI, rs-fMRI, fMRI | 1445 | 8–21 years | No |
Norwegian Mother-Child Study (MoBa) | sMRI | 495 | 6–21 years | 2 waves |
School recruitment – convenience | ||||
IMAGEN | sMRI, fMRI | 2,223 | 13–16 years | 2 waves |
Adolescent Brain Cognitive Development (ABCD) Study | sMRI, DTI, rs-fMRI, fMRI | 11,874 | 9–10 years | 1 wave, multiple planned |
HealABCD (pilot funding assigned) | >5,000 | Fetal life forward | Multiple planned | |
Healthy volunteers | ||||
PING | sMRI, DTI, rs-fMRI | 1,493 | 3–20 | No |
NIMH intramural child cohort | sMRI, more added | 618 + 800 twins | 5–25 | Varied, some >4 |
Lifespan baby connectome project | sMRI, rs-fMRI | 500 | 0–5 years | No |
Normal development. The first large scale population imaging study on normal development was conducted at the Child Psychiatry Branch of the NIMH by Giedd and colleagues who conducted repeated MR scans of typically developing children and adolescents (Giedd and Rapoport 2010). While prior work in the field compared size differences of selected brain area, this longitudinal study examined trajectories of development over time and evaluations of neural circuitry as opposed to structures in isolation. In a series of reports, the group showed that the human brain has a spatially-distinct protracted maturation, with different neural circuits undergoing distinct dynamic changes throughout life. They demonstrated largely linearly increasing white matter volumes across adolescence and an inverted U-shaped trajectory of grey matter volumes, with peak sizes occurring at different ages in different regions. In girls the total cerebral volume peaked at age 10.5, in boys at age 14.5 (Lenroot and Giedd 2006). The repeated neuroimaging design also enabled researchers using the NIMH data to show that the neuroanatomical expression of intelligence in children is dynamic. While in early childhood there was a predominantly negative correlation between intelligence and cortical thickness, only in adolescence did they find the known positive correlation. Children with higher IQ demonstrated a particularly plastic cortex, with an initial accelerated and prolonged phase of cortical growth, followed by a more rapid cortical thinning in early adolescence (Shaw et al. 2006). While many of these observations have been replicated, the inverted U-shaped trajectories of cortical thickness may have been enhanced by poor quality (e.g., motion artifact) of the images in young children. A study with much more stringent post processing quality control found that cortical thickness across childhood from age 5 onwards was almost exclusively declining linearly, with little evidence for sex difference if corrected for total brain volume (Ducharme et al. 2016).
Etiology. The Saguenay Youth Study takes a largely etiological approach and investigates mainly early life (intrauterine exposure to smoking) and adolescence exposures (sex hormones and substance use) (Pausova et al. 2017). Higher testosterone-related volume of white matter during male adolescence was reported as well as a negative relationship between the extent of drug experimentation and the thickness of the orbitofrontal cortex. The Pediatric Imaging, Neurocognition and Genetics (PING) study advanced our understanding of how indicators of socioeconomic status cross-sectionally related to brain structure (Jernigan et al. 2016). Among children from lower income families, small differences in income were more strongly related to differences in cortical surface area than among children from higher income families (Noble et al. 2015). These relationships were most prominent in regions supporting language, reading, executive functions, and spatial skills and mediated socioeconomic differences in certain neurocognitive abilities. Importantly, analyses were adjusted for ancestral descent based on genotype data. Longitudinal studies beginning earlier in life with assessments of possible intermediates such as parenting, family stress, or nutritional markers are needed to inform public health interventions. Etiological studies were also performed in the Generation R cohort and the ABCD study. For example, the first found prospectively assessed maternal cannabis during pregnancy was related to thicker frontal cortex (El Marroun et al. 2016). Recent work in the same cohort, however, suggested this association may not be causal (El Marroun et al. 2019). Likewise, the association between screen media activity and structural correlation networks in the brain observed in the first release of the ABCD Study cannot easily be interpreted causally (Paulus et al. 2019). While such individual differences may have consequences for psychopathology and cognitive performance, the cross-sectional nature of the study precluded any etiological interpretation given the possibility of reverse causality. Other imaging studies have tested whether brain structural development mediates the relation between adverse exposures and child psychopathology. The effects of peer victimization on depression, generalized anxiety, and hyperactivity symptoms assessed at follow-up were tested in 682 participants from the longitudinal IMAGEN study (Quinlan et al. 2018). Peer victimization was indirectly associated with generalized anxiety via decreases in putamen and left caudate volume. These data suggest that the experience of chronic peer victimization during adolescence might induce psychopathology-relevant deviations from normative brain development. Other longitudinal etiological studies in Generation R suggested that a thinner cortex in childhood mediated the effect of fetal exposure to air pollution on inhibitory control (Guxens et al. 2018). Although these etiological studies might identify novel risk factors for child psychiatric disorders, their strength is to determine how environmental or genetic factors impact the brain and thus how the brain structural or functional changes may underlie the lasting effects of, for example, socio-economic status on a range of neurodevelopmental outcomes.
Diagnosis. Several imaging studies embedded in the Philadelphia Neurodevelopmental Cohort have attempted to demonstrate transdiagnostic brain-based phenotypes in individuals with increased susceptibility and symptoms of psychiatric disorders using sophisticated modeling approaches (Kaczkurkin et al. 2018). Dimensionally studied general psychopathology and psychotic experiences were cross-sectionally related to resting-state functional connectivity and white matter microstructure. Results showed shared mechanisms for psychopathology symptoms that cut across clinical diagnostic categories, but these studies are not sufficient to establish the regionally elevated perfusion in the anterior cingulate cortex or any brain morphological parameter as a diagnostic biomarker given the absence of follow-up studies and lack of comparative approaches. A similar approach was used in a white matter imaging study in Generation R (Neumann et al. 2020). The authors showed that higher levels of general psychopathology were associated with less white matter integrity but that externalizing symptoms may display the reversed associations, that is, characterized by more white matter integrity, once co-occurring general psychopathology is accounted for. This complicates research into diagnostic biomarkers as it suggests that clinical presentations of externalizing symptoms may comprise various symptoms or subdimensions each differentially related to brain characteristics which cannot easily be disentangled in an individual. One seminal diagnostic imaging study focused on depression in adults (Drysdale et al. 2017). Resting state functional magnetic resonance imaging was used in a large multisite sample to show that patients with depression can be subdivided into neurophysiological subtypes defined by distinct patterns of dysfunctional connectivity in limbic and frontostriatal networks. The patient clustering corresponded reliably to clinical profiles across data sets and predicted responsiveness to transcranial magnetic stimulation therapy. However, the distinct resting state connectivity-based subtypes of any disorder should be interpreted with caution, unless the correlations of imaging parameters and clustering of groups have been shown to be robust and reproducible (Dinga et al. 2019). However, such disorder subtypes or perhaps more likely, cross-disorder groups, may identify individuals who are most likely to benefit from specific interventions and could be a viable step towards personalized medicine in (child) psychiatry.
Prognosis. The multisite IMAGEN study, unlike other large population neuroimaging studies, also focused on functional in addition to structural imaging measures (Schumann et al. 2010). Quantitative psychological traits were related to functional correlates of reinforcement behaviors such as impulsivity, reward sensitivity, and emotional reactivity in an effort to include biological mechanisms in psychiatric classifications and predictions. Albeit exciting, rigorous diagnostic evaluation studies are lacking to formally test the claim of personalizing medicine. An elegant prognostic study was performed in IMAGEN using a machine learning approach (Whelan et al. 2014). The authors identified 30 variables from 6 domains including genetic, brain morphological, and cognitive data that predicted future binge drinking. This multivariate prediction profile highlights how brain measures, which were among the best predictors, can improve prediction independently of variables across many other domains. A sparser prediction model with imaging data may stand a chance to be used in practice.
Sensitive periods. One population neuroscience study was conducted in the form of a randomized trial of children reared in an institution in Bucharest, Romania, who were randomly selected to be removed from the center and placed into high-quality foster care during early childhood (Sheridan et al. 2012). The neurodevelopment of these children was compared with that of children who remained in the institution, and non-neglected children. Between 8 and 10 years, researchers found that children exposed to institutional rearing showed decreased cortical grey matter volumes and reduced thickness throughout the cortex. Children placed in foster care did not significantly differ from children who remained in the institution. This relatively small imaging study with about 25 children in each arm of the trial highlights how psychosocial deprivation lastingly affects the brain in the first couple of years of life. Also the observations mirror findings of suppressed growth within institutional care settings that suggest a sensitive period early in life, the adoptees’ recovery, in particular of their IQ, within adoptive families was most marked if placement occurred prior to 12 months of age (Johnson et al. 2010; Van IJzendoorn et al. 2007). This relatively small imaging study with about 25 children in each arm of the trial highlights how psychosocial deprivation lastingly affects the brain in a sensitive period in the first couple of years of life (Johnson et al. 2010; Van IJzendoorn et al. 2007).
Using data of the Generation R cohort, investigators tested if sensitive periods of brain development to prenatal maternal thyroid dysfunction could be identified (Jansen et al. 2019b). Maternal thyroid deficiency has repeatedly been associated with poor child neurodevelopmental outcomes. This study examined the association of maternal thyroid function with child brain morphology assessed at 10 years to study whether any association were dependent on the timing of thyroid assessment during pregnancy. Both low and high maternal thyroid function were associated with smaller child total grey matter and cortical volume. However, an association with a neurodevelopmental outcome is most evident when maternal thyroid function is measured early in pregnancy suggesting that embryonic brain development is particularly vulnerable to altered maternal thyroid function. Using the same data set, the association of an exposure to maternal depressive symptoms at different developmental stages from fetal life to preadolescence with child brain development was tested (Zou et al. 2019). This study included volumetric and white matter microstructure data when children were 10 years of age. Single-time-point analyses showed that maternal depressive when children were age 2 months were associated with smaller total grey matter volume and lower global fractional anisotropy, whereas maternal depressive symptoms assessed prenatally or in childhood were not. The trajectory analyses suggested in particular that children exposed to persistently high levels of maternal depressive symptoms across the perinatal period had smaller grey and white matter volumes as well as alterations in white matter microstructure. These results suggest that the postnatal period is a window of vulnerability for adverse exposures such as maternal depressive symptoms.
Methodological Considerations in Psychiatric Neuroimaging and Population Neuroscience
A substantial portion of the neuroimaging literature has focused on obtaining highly precise measurements of the brain and less attention has been afforded to core epidemiological concepts such as (population) sampling, generalizability, and bias (Kolossa and Kopp 2018). While gaining precision in measurements has clear benefits, the bias and lack of reproducibility are causes for concern (Shrout and Rodgers 2018). Many of the issues likely arise from relatively small sample sizes. However, irrespective of sample size, other issues are clearly at play and will be discussed below. We argue that practicing population neuroscience implies that these challenges are addressed.
Representativeness and Generalizability
Representativeness is sometimes seen as the hallmark of population neuroscience; studies should aim to recruit a subset of a population that reflects the characteristics, such as race and socio-economic status, of the larger group (Garavan et al. 2018). The goal of representativeness is to achieve generalizability of study, although that is a matter of scientific inference (Richiardi et al. 2013). Generalizability largely depends on validity of results, even if often judged just by similarities between the time, place, people, and social contexts (Leung 2015). Actually, there are good reasons for population imaging to deliberately opt for nonrepresentativeness in design: (i) to minimize bias by restricting to a particular population subgroup with less likelihood of lifestyle differences between exposed and nonexposed; and (ii) to deliberately focus on population subgroups, for example, ethnic groups, and (iii) practical considerations, for example, to restrict to living near the imaging facility. The Generation R Study, for example, was situated for practical reasons in Rotterdam. The study is not representative for the Netherlands, for example, it includes a more ethnically diverse population (Jaddoe et al. 2006). Representative studies are not necessarily more heterogeneous in exposure distribution. Nonrepresentativeness may also be “unintentional” (Richiardi et al. 2013). For example, nonrepresentativeness can be due to low baseline response rates or the recruitment of volunteers rather than a sample of a defined population (i.e., a study with a primary population base). The intramural NIMH study, for example, largely recruited from the affluent Bethesda neighborhood. The ABCD study was designed as a representative multisite study but had recruitment rates of less than 15%, similarly the Saguenay Study included less than 10% of all families (although some were not eligible). On the one hand, such baseline self-selection is likely to create a group of more motivated persons, which may result in a better response to follow-up and thus in decreased selection bias. On the other hand, it is likely that there are factors associated with selection that are also determinants of the outcome, think of family chaos or poverty that have consistently been related to neurodevelopment. Importantly, such selection bias related to baseline recruitment can occur even if the study is representative on indicators such as socio-economic status and race. Indeed, the occurrence of psychiatric problems in studies, such as Generation R or the ABCD study, is lower than in population-based studies with higher baseline response and possibly this will bias etiological associations. A descriptive study of LeWinn et al. showed how sample composition can influence age-related variation in grey matter volume and cortical thickness (LeWinn et al. 2017). The authors applied sample weights from census data to participants with structural brain imaging data from the PING study. Compared to the unweighted sample, earlier maturation of cortical and subcortical structures was found in the weighted sample. For such descriptive studies, low baseline response rates may introduce bias. However, population neuroscience should carefully weigh the advantages of representativeness against those of a well-defined but nonrepresentative population base (e.g., a population register which allows the calculation of response rates and the evaluation of selection bias) or a focus on subgroups which may better reduce bias. Representativeness is typically not needed other than in prevalence studies.
High Dimensional Data and Multiple Testing
Brain images have an immense complexity which grows exponentially with increasingly finer spatial resolution. It is then no surprise that neuroimaging presents a nontrivial dimensionality problem. Often, details of the brain are captured with various neuroimaging modalities by sampling different characteristics (e.g., structure, function). For example, with structural MRI, a grid of 3-dimensional pixels (voxels) is used and can easily surpass 65,000 data points in a single image. Depending on the neuroimaging modality (e.g., structural, functional), each voxel may also contain multiple pieces of information. One common way to simplify this dimensionality problem is to reduce the data into sub-units, often referred to as regions of interest (ROIs). In the context of motor ability, one may look preferentially to the precentral gyrus and summarize the information of all voxels in the brain which fall within this region (e.g., calculate the mean cortical thickness across the precentral gyrus). Such a strategy can reduce thousands of data points into a more manageable subset. However, common neuroanatomical atlases consist of more than 30 areas per hemisphere (Desikan et al. 2006), and state-of-the-art multimodal parcellation schemes now include hundreds of areas (Glasser et al. 2016) and thus possible ROIs. Importantly, the brain has a complex architecture with interrelated networks. Thus, for many exposures a plausible hypothesis, which justifies exploring many different ROIs, can be framed. This yields multiple tests of different ROIs, as an evidence-based a priori choice is typically not possible (like in candidate gene studies). Yet, studies using an ROI approach often do not control for multiple testing at all. Alternatively, “hypothesis free” approaches are employed, where each brain voxel is examined separately rather than aggregating information across anatomical ROIs. One playful, yet concerning, illustration of the problem is made by the famous “dead salmon study,” where postmortem functional neuroimaging of a fish showed “significant” neural activation without adjustment for multiple comparisons (Bennett et al. 2009). Though methods are able to adjust for the many thousands of statistical tests (voxels) (Bennett et al. 2009), the field has struggled to adequately control multiple testing (Eklund et al. 2016; Greve and Fischl 2018). This struggle can partly be explained by the correlated nature of the many thousands of voxels in the brain (i.e., nonindependence). Even if the number of statistical tests is accounted for properly across the thousands of brain voxels, researchers often explore several models and contrasts, and they typically do not further adjust for these tests (Alberton et al. 2019). Clearly, adequate control for multiple testing against the background of a myriad of reasonable and feasible association tests with different imaging parameters remains one of the most salient challenges in Population Neuroscience.
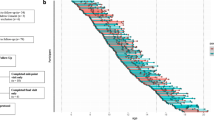
Confounding
Neurodevelopmental and neuropsychiatric imaging studies typically adjust statistical models for a basic and limited set of covariates, namely age, sex, and often total brain size. Even if suitable information on other possible confounding factors is available, many studies omit these from statistical models. Sometimes possible confounders are not ascertained or considered, sometimes matching on selected parameters is seen as sufficient, and sometimes analytical software used in imaging analyses does not allow for a complex array of covariates. In a model that includes statistical adjustments for a true confounding factor, the effect estimate of an association will typically attenuate. However, the brain architecture involved in an association is determined by the interplay of many genetic and environmental factors, that several will likely also be associated with a particular exposure or outcome such as ADHD. This has implications for neuroimaging research. The strength of the observed association between an imaging parameter and a given phenotype is often overestimated. In the context of high-dimensional analyses, studies not properly adjusting for confounding factors highlight more brain areas than are actually present. For example, Fig. 1 illustrates how attention symptoms are related to cortical surface area in the general population of 2706 children ages 8–12 years from the Generation R Study (unpublished data). Colors coded from red-to-yellow highlight how the spatial distribution of the association of surface area with attention problems varies across the brain as a function of important confounding factors. In this example, the total surface area of the association was more than 200cm2 when only adjusting for age, sex, and ethnicity and fell to 85cm2 (42% of the original size) after adjustment for several confounders such as prenatal tobacco exposure and maternal psychopathology. Poor control for confounding leads to invalid results, poor generalizability, and problems with replication of results (Ioannidis 2019). Against this background, the large meta-analyses, such as conducted by the Enigma Network, that typically adjust for few confounders only cannot easily infer causality (Hoogman et al. 2019). Consideration of confounding factors should take place before data collection begins, and population neuroscientists have to accept that more likely than not the associations tested in child psychiatry are confounded by many external factors.
Figure depicts what happens to significant associations between ADHD and surface area with additional adjustment of estimates for confounding effects. M1 = Model 1 and includes age, sex, and ethnicity. M2 = Model 2 and represents Model 1 + parental educational level. M3 = Model 3 and represents Model 2 + family income. M4 = Model 4 and represents M3 + prenatal exposure to tobacco. M5 = Model 5 and represents M4 + maternal psychiatric problems. Red color represents minimally/basic adjusted models and yellow indicates more complete/fully adjusted models.
Reverse Causality and Bidirectionality in Brain-Behavior Studies
Though often implicit, nearly all studies utilizing brain imaging to study psychopathology operate under the assumption that neuroimaging features associated with psychopathology precede the symptomatology, omitting the possibility of downstream effects, or “behaviors shaping the brain.” Imagine a child with anxiety symptoms, who likely lacks certain social interactions, spends more time in bed sleeping and is more withdrawn than his or her peers; these behavioral and emotional problems very likely alter the course of brain development, though any neuroimaging correlates will misleadingly be interpreted as antecedents of the symptoms. In a study of 480 children participating in a repeated imaging study, it was shown that higher levels of internalizing and externalizing problems measured at age 6 were predictive of reduced (slower) changes in subcortical grey matter and white matter microstructure from ages 6-to-12 years of age (Muetzel et al. 2018). However, imaging metrics assessed at age 6 were not predictive of changes in externalizing and internalizing problems over time. As of yet, it is unclear how much and at what age behavior impacts the brain most. Nevertheless, this population neuroscience finding has profound implications for the interpretation of cross-sectional studies, the typical inferences, and that emotional or behavioral symptoms are always a consequence of brain alterations. It implies that we need longitudinal studies to demonstrate the associations of brain and behavior, otherwise studies will likely be biased, inconsistent and cannot be accurately interpreted.
Imaging Genetic Studies
The advent of genome wide association studies (GWAS) and modern molecular genetics is of particular relevance for Population Neuroscience, although imaging genetics is in its infancy. First, genetic studies of imaging parameters are conducted that may help better understand brain development. The function and structure of the human brain is strongly shaped by genetic influences. Yet only in the past years have several large consortia studies shed some light on the genetic variants related to imaging parameters, though typically in adults (Hirschhorn and Gajdos 2011). A GWA study of intracranial volume showed a high genetic correlation between adult intracranial volume and child head circumference (Adams et al. 2016). As with most other large genetic imaging studies of various brain structures, some genetic variants identified were related to childhood cognitive functioning. Another large seminal GWA study investigated seven subcortical structures (Hibar et al. 2015). Interestingly, genetic variants related to the putamen were located on genes (e.g., DCC) most highly expressed in the first two trimesters of prenatal development suggesting that this variant may influence brain volumes early in neurodevelopment. More recently, imaging genetic studies in the UK Biobank showed that iron transport and storage genes were related to magnetic susceptibility of subcortical brain tissue, whereas extracellular matrix and epidermal growth factor genes with white matter microstructure and lesions (Elliott et al. 2018). These results may provide some insights into the molecular mechanisms underlying brain development, but the hope that this approach will yield novel candidate genes for neurodevelopmental disorders has not materialized. As the genetic loci discovered in imaging studies are rarely related to psychiatric traits, these MRI parameters cannot be viewed as intermediate endophenotypes helping to unravel the genetic architecture of child psychiatric disorders.
Second, genetic correlation studies are used to better understand the link between psychiatric traits and neurodevelopment. Likewise, polygenic risk scores (aggregates of risk based on genetic information) derived from GWA studies of psychiatric traits have been related to neuroimaging and other neurodevelopmental parameters and vice versa. These studies clearly show widespread pleiotropy between cognitive, mental health traits, and brain parameters although they cannot demonstrate if this reflects mediated or biological pleiotropy, or simply correlated genetic loci (Salinas et al. 2018). Several studies tested whether the polygenic susceptibility for disorders such as schizophrenia, autism spectrum disorders, or ADHD is associated with brain morphological characteristics in children. Indeed, a higher genetic susceptibility for ADHD, for example, was associated with smaller caudate volume and this explained part of the association with attention problems in boys (Alemany et al. 2019). However, polygenic risk scores of education or intelligence generally showed a stronger signal with child brain morphology, which probably reflects the large statistical power in the GWAs of cognitive traits. In contrast, the genetic loci found in adult neuroimaging studies are not or only very weakly associated with child psychiatric phenotypes. A recent study found no genetic correlation of white matter characteristics and neurodevelopmental disorders, only a positive correlation of white matter characteristics (here fractional anisotropy) with cognition and negatively with depression (Zhao et al. 2019). Similarly, no evidence of shared genetic influences between subcortical brain volumes and schizophrenia was found although improved statistical modeling recently suggests some genetic overlap (Franke et al. 2016; Smeland et al. 2018). Most genetic correlation or polygenetic studies in the neurodevelopmental field are cross-disorder studies which will not be discussed in detail. Consistently, these genetic studies provide evidence for shared genetic effects on different neurodevelopmental disorders (Smoller et al. 2019). For example, SNPs identified the ADHD GWAS strongly predict autism and many other traits (Jansen et al. 2019a). The poorly explained positive genetic correlation between autism and intelligence is arguably one of the most exciting leads for future genetically informed neuroimaging studies (Savage et al. 2018).
Thirdly, modern genetic research offers a perspective of how epidemiological rigor can advance a scientific field. Like imaging studies, early genetic studies were limited by logistical considerations, nominally significant results were interpreted as definitive, and the this was exacerbated by technical artifacts (Hirschhorn and Gajdos 2011). However, stringent control for multiple testing, replication protocols, large scale studies has provided the ability to detect small effects validly. In addition, genetic studies helped advance causal inference. However, methodological advances such as Mendelian randomization have hardly been introduced in Population Neuroscience (Van 't Ent et al. 2017).
In summary, the clinical utility of genetic risk prediction at present is still low; the effect sizes of these aggregate measures remain too small. Imaging genetics studies of neurodevelopmental traits are still in their early stages, also due of the scarce use of multivariate strategies in data analysis. Moreover, the selection effects, observed in particular in the imaging studies, provide an underestimated challenge for risk prediction modeling. Yet, as the ancestral diversity and sample sizes of genome-wide association studies increase, there is real promise for clinical practice.
Clinical and Public Health Relevance of Population Neuroscience
The advance in Population Neurosciences like in most scientific disciplines is incremental and the clinical applications arise less quickly than expected. Landmark neuroimaging studies have provided insights in the development of ADHD and autism. A maturational lag across multiple neural circuits has been demonstrated in ADHD, but studies also show that this often disappears with age. Sibling studies in children with autism provide evidence that in severe cases autism can also be conceptualized as a syndrome of degeneration, as these children have experienced regression and degeneration probably underlying the loss of neurological function (Constantino 2018; Kern et al. 2013). These highlights illustrate the advance in the understanding of brain development in children with psychiatric disorders, but what insights for etiological, diagnostic, and prognostic understanding can we expect from Population Neuroscience? Epidemiological studies provide evidence for the substantial comorbidity of child psychiatric traits, and population neuroscience confirmed the likely etiological overlap. Imaging markers can serve as a sensitive biomarker of brain developmental effects. Large longitudinal imaging studies could also show that certain brain alterations mediated environmental, intra-uterine, or social exposures; however, we must not turn to Population Neuroscience to discover new risk factors. Arguably, the field most likely to be advanced by population neuroscience is research on diagnostic classifications. While behavioral and molecular genetic studies have cast doubt on the validity of several diagnostic entities, imaging studies may be useful to define more robust subgroups. In particular resting state fMRI is a hopeful approach; the work of the Liston group discussed above suggests that this modality has the sensitivity to reflect change over time and probably environmental effects. The depression subgroups identified by resting-state fMRI profiles predicted outcome well, although much more work is needed to define robust diagnostic categories including neuroimaging data. Other approaches using one or different imaging modalities have shown to predict the onset of substance abuse or recurring delinquency and such applications will increase with more carefully conducted longitudinal studies. Arguably, the lack of clinical utility of neuroimaging for child and adolescent psychiatry does not reflect the limited potential of imaging in this field, but the lack of epidemiological designs, that is, the lack of population neuroscience.
Conclusion
Most developmental neuroimaging studies cannot easily be generalized, with many arguably biased due to poor control for confounding and selection effects. Often the temporal direction of the associations reported remains unclear, for example, is the child behavior such as anxiety a cause or a consequence of the brain morphological differences detected in the basal ganglia? Population neuroscience is an attempt to address these challenges with larger sample sizes, a clear study design and sampling frame, longitudinal data including repeated brain imaging assessments, and a more careful control for multiple testing. Importantly, population neuroscience attempts to integrate different imaging modalities, environmental factors, and genetic data with behavioral phenotypes. It remains to be seen if population neuroscience will result in clinically meaningful diagnostic and prognostic parameters for child psychiatry or even better treatment allocation, but presents us with a clear opportunity and the most sensible way forward.
References
Adams HH, Hibar DP, Chouraki V, Stein JL, Nyquist PA, Renteria ME, … Thompson PM (2016) Novel genetic loci underlying human intracranial volume identified through genome-wide association. Nat Neurosci 19(12):1569–1582. https://doi.org/10.1038/nn.4398
Alberton BAV, Nichols TE, Gamba HR, Winkler AM (2019) Multiple testing correction over contrasts for brain imaging. bioRxiv:775106
Alemany S, Jansen P, Muetzel R, Marques N, El Marroun H, Jaddoe V, … White T (2019) Common polygenic variations for psychiatric disorders and cognition in relation to brain morphology in the general pediatric population. J Am Acad Child Adolesc Psychiatry 58:600–607
Ambrosino S, De Zeeuw P, Wierenga LM, van Dijk S, Durston S (2017) What can cortical development in attention-deficit/hyperactivity disorder teach us about the early developmental mechanisms involved? Cereb Cortex 27(9):4624–4634
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. APA, Arlington
Bale TL, Baram TZ, Brown AS, Goldstein JM, Insel TR, McCarthy MM, … Nestler EJ (2010) Early life programming and neurodevelopmental disorders. Biol Psychiatry 68(4):314–319. https://doi.org/10.1016/j.biopsych.2010.05.028
Bennett CM, Wolford GL, Miller MB (2009) The principled control of false positives in neuroimaging. Soc Cogn Affect Neurosci 4(4):417–422
Burton BK, Hjorthøj C, Jepsen JR, Thorup A, Nordentoft M, Plessen KJ (2016) Research review: do motor deficits during development represent an endophenotype for schizophrenia? A meta-analysis. J Child Psychol Psychiatry 57(4):446–456
Carpenter WT, Strauss JS (2017) Developmental interactive framework for psychotic disorders. Oxford University Press, Oxford
Clouston TS (1891) The neurosis of development. Oliver & Boyd, Edinburgh
Constantino JN (2018) Deconstructing autism: from unitary syndrome to contributory developmental endophenotypes. Int Rev Psychiatry 30(1):18–24. https://doi.org/10.1080/09540261.2018.1433133
Desikan RS, Ségonne F, Fischl B, Quinn BT, Dickerson BC, Blacker D, … Hyman BT (2006) An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage 31(3):968–980
Dinga R, Schmaal L, Penninx B, van Tol MJ, Veltman DJ, van Velzen L, … Marquand AF (2019) Evaluating the evidence for biotypes of depression: methodological replication and extension of. Neuroimage Clin 22:101796. https://doi.org/10.1016/j.nicl.2019.101796
Donovan SJ, Susser E (2011) Commentary: advent of sibling designs. Int J Epidemiol 40(2):345–349. https://doi.org/10.1093/ije/dyr057
Drysdale AT, Grosenick L, Downar J, Dunlop K, Mansouri F, Meng Y, … Liston C (2017) Resting-state connectivity biomarkers define neurophysiological subtypes of depression. Nat Med 23(1):28–38. https://doi.org/10.1038/nm.4246
Ducharme S, Albaugh MD, Nguyen TV, Hudziak JJ, Mateos-Perez JM, Labbe A, … Brain Development Cooperative Group (2016) Trajectories of cortical thickness maturation in normal brain development – the importance of quality control procedures. Neuroimage 125:267–279. https://doi.org/10.1016/j.neuroimage.2015.10.010
Eklund A, Nichols TE, Knutsson H (2016) Cluster failure: why fMRI inferences for spatial extent have inflated false-positive rates. Proc Natl Acad Sci 113(28):7900–7905
El Marroun H, Tiemeier H, Franken IH, Jaddoe VW, van der Lugt A, Verhulst FC, … White T (2016) Prenatal cannabis and tobacco exposure in relation to brain morphology: a prospective neuroimaging study in young children. Biol Psychiatry 79(12):971–979
El Marroun H, Bolhuis K, Franken IH, Jaddoe VW, Hillegers MH, Lahey BB, Tiemeier H (2019) Preconception and prenatal cannabis use and the risk of behavioural and emotional problems in the offspring; a multi-informant prospective longitudinal study. Int J Epidemiol 48(1):287–296
Elliott LT, Sharp K, Alfaro-Almagro F, Shi S, Miller KL, Douaud G, … Smith SM (2018) Genome-wide association studies of brain imaging phenotypes in UK Biobank. Nature 562(7726):210–216. https://doi.org/10.1038/s41586-018-0571-7
Emerson RW, Adams C, Nishino T, Hazlett HC, Wolff JJ, Zwaigenbaum L, … Elison JT (2017) Functional neuroimaging of high-risk 6-month-old infants predicts a diagnosis of autism at 24 months of age. Sci Transl Med 9(393):eaag2882
Filatova S, Koivumaa-Honkanen H, Hirvonen N, Freeman A, Ivandic I, Hurtig T, … Miettunen J (2017) Early motor developmental milestones and schizophrenia: a systematic review and meta-analysis. Schizophr Res 188:13–20
Fish B (1957) The detection of schizophrenia in infancy. J Nerv Ment Dis 125:1–24
Franke B, Stein JL, Ripke S, Anttila V, Hibar DP, van Hulzen KJE, … Sullivan PF (2016) Genetic influences on schizophrenia and subcortical brain volumes: large-scale proof of concept. Nat Neurosci 19(3):420–431. https://doi.org/10.1038/nn.4228
Garavan H, Bartsch H, Conway K, Decastro A, Goldstein RZ, Heeringa S, … Zahs D (2018) Recruiting the ABCD sample: design considerations and procedures. Dev Cogn Neurosci 32:16–22. https://doi.org/10.1016/j.dcn.2018.04.004
Giedd JN, Rapoport JL (2010) Structural MRI of pediatric brain development: what have we learned and where are we going? Neuron 67(5):728–734
Glasser MF, Coalson TS, Robinson EC, Hacker CD, Harwell J, Yacoub E, … Jenkinson M (2016) A multi-modal parcellation of human cerebral cortex. Nature 536(7615):171–178
Greve D, Fischl B (2018) False positive rates in surface-based anatomical analysis. NeuroImage 171:6–14
Guxens M, Lubczyńska MJ, Muetzel RL, Dalmau-Bueno A, Jaddoe VW, Hoek G, … Brunekreef B (2018) Air pollution exposure during fetal life, brain morphology, and cognitive function in school-age children. Biol Psychiatry 84(4):295–303
Hazlett HC, Gu H, Munsell BC, Kim SH, Styner M, Wolff JJ, … Statistical Analysis (2017) Early brain development in infants at high risk for autism spectrum disorder. Nature 542(7641):348–351. https://doi.org/10.1038/nature21369
Hibar DP, Stein JL, Renteria ME, Arias-Vasquez A, Desrivieres S, Jahanshad N, … Medland SE (2015) Common genetic variants influence human subcortical brain structures. Nature 520(7546), 224–229. https://doi.org/10.1038/nature14101
Hirschhorn JN, Gajdos ZK (2011) Genome-wide association studies: results from the first few years and potential implications for clinical medicine. Annu Rev Med 62:11–24. https://doi.org/10.1146/annurev.med.091708.162036
Hoogman M, Muetzel R, Guimaraes JP, Shumskaya E, Mennes M, Zwiers MP, … Franke B (2019) Brain imaging of the cortex in ADHD: a coordinated analysis of large-scale clinical and population-based samples. Am J Psychiatry 176(7):531–542. https://doi.org/10.1176/appi.ajp.2019.18091033
Ioannidis JPA (2019) What have we (not) learnt from millions of scientific papers with P values? Am Stat 73(sup1):20–25. https://doi.org/10.1080/00031305.2018.1447512
Jaddoe VW, Mackenbach JP, Moll HA., Steegers EA, Tiemeier H, Verhulst FC, … Hofman A (2006) The Generation R Study: design and cohort profile. Eur J Epidemiol 21(6):475
Jansen AG, Dieleman GC, Jansen PR, Verhulst FC, Posthuma D, Polderman TJC (2019a) Psychiatric polygenic risk scores as predictor for attention deficit/hyperactivity disorder and autism spectrum disorder in a clinical child and adolescent sample. Behav Genet. https://doi.org/10.1007/s10519-019-09965-8
Jansen TA, Korevaar TI, Mulder TA, White T, Muetzel RL, Peeters RP, Tiemeier H (2019b) Maternal thyroid function during pregnancy and child brain morphology: a time window-specific analysis of a prospective cohort. Lancet Diabetes Endocrinol 7(8):629–637
Jernigan TL, Brown TT, Hagler DJ, Jr, Akshoomoff N, Bartsch H, Newman E, … Genetics S (2016) The Pediatric Imaging, Neurocognition, and Genetics (PING) data repository. Neuroimage 124(Pt B):1149–1154. https://doi.org/10.1016/j.neuroimage.2015.04.057
Johnson D, Guthrie D, Smyke A, Koga S, Fox N, Zeanah C, Nelson C (2010) Growth and associations between auxology, caregiving environment, and cognition in socially deprived Romanian children randomized to foster vs ongoing institutional care. Arch Pediatr Adolesc Med 164(6):507–516
Jones W, Klin A (2013) Attention to eyes is present but in decline in 2-6-month-old infants later diagnosed with autism. Nature 504(7480):427–431. https://doi.org/10.1038/nature12715
Kaczkurkin AN, Moore TM, Calkins ME, Ciric R, Detre JA, Elliott MA, … Satterthwaite TD (2018) Common and dissociable regional cerebral blood flow differences associate with dimensions of psychopathology across categorical diagnoses. Mol Psychiatry 23(10):1981–1989. https://doi.org/10.1038/mp.2017.174
Kern J, Geier D, Sykes L, Geier MR (2013) Evidence of neurodegeneration in autism spectrum disorder 2. Transl Neurodegen 2:17
Kolossa A, Kopp B (2018) Data quality over data quantity in computational cognitive neuroscience. NeuroImage 172:775–785
Lenroot RK, Giedd JN (2006) Brain development in children and adolescents: insights from anatomical magnetic resonance imaging. Neurosci Biobehav Rev 30(6):718–729
Leung L (2015) Validity, reliability, and generalizability in qualitative research. J Family Med Primary Care 4(3):324
LeWinn KZ, Sheridan MA, Keyes KM, Hamilton A, McLaughlin KA (2017) Sample composition alters associations between age and brain structure. Nat Commun 8(1):1–14
Lewis DA, Levitt P (2002) Schizophrenia as a disorder of neurodevelopment. Annu Rev Neurosci 25(1):409–32
McIntosh AM, Owens DC, Moorhead WJ, Whalley HC, Stanfield AC, Hall J, … Lawrie SM (2011) Longitudinal volume reductions in people at high genetic risk of schizophrenia as they develop psychosis. Biol Psychiatry 69(10):953–958. https://doi.org/10.1016/j.biopsych.2010.11.003
Muetzel RL, Blanken LME, van der Ende J, El Marroun H, Shaw P, Sudre G, … White T (2018) Tracking brain development and dimensional psychiatric symptoms in children: a longitudinal population-based neuroimaging study. Am J Psychiatry 175(1):54–62. https://doi.org/10.1176/appi.ajp.2017.16070813
Murray RM, Bhavsar V, Tripoli G, Howes O (2017) 30 years on: how the neurodevelopmental hypothesis of schizophrenia morphed into the developmental risk factor model of psychosis. Schizophr Bull 43(6):1190–1196. https://doi.org/10.1093/schbul/sbx121
Neumann A, Muetzel RL, Lahey BB, Bakermans-Kranenburg MJ, van IJzendoorn MH, Jaddoe VW, Hillegers MH, White T, Tiemeier H (2020) White matter microstructure and the general psychopathology factor in children. J Am Acad Child Adolesc Psychiatry
Noble KG, Houston SM, Brito NH, Bartsch H, Kan E, Kuperman JM, … Sowell ER (2015) Family income, parental education and brain structure in children and adolescents. Nat Neurosci 18(5):773–778. https://doi.org/10.1038/nn.3983
Obel C, Olsen J, Henriksen TB, Rodriguez A, Järvelin MR, Moilanen I, … Ebeling H (2011) Is maternal smoking during pregnancy a risk factor for hyperkinetic disorder?—Findings from a sibling design. Int J Epidemiol 40(2):338–345
Paulus MP, Squeglia LM, Bagot K, Jacobus J, Kuplicki R, Breslin FJ, … Tapert SF (2019) Screen media activity and brain structure in youth: Evidence for diverse structural correlation networks from the ABCD study. Neuroimage 185:140–153. https://doi.org/10.1016/j.neuroimage.2018.10.040
Paus T (2010) Population neuroscience: why and how. Hum Brain Mapp 31:891–903
Pausova Z, Paus T, Abrahamowicz M, Bernard M, Gaudet D, Leonard G, … Veillette S (2017) Cohort profile: the Saguenay Youth Study (SYS). Int J Epidemiol 46(2):e19. https://doi.org/10.1093/ije/dyw023
Quinlan EB, Barker ED, Luo Q, Banaschewski T, Bokde ALW, Bromberg U, … IMAGEN Consortium (2018) Peer victimization and its impact on adolescent brain development and psychopathology. Mol Psychiatry. https://doi.org/10.1038/s41380-018-0297-9
Raznahan A, Wallace GL, Antezana L, Greenstein D, Lenroot R, Thurm A, … Giedd JN (2013) Compared to what? Early brain overgrowth in autism and the perils of population norms. Biol Psychiatry 74(8):563–575. https://doi.org/10.1016/j.biopsych.2013.03.022
Redcay E, Courchesne E (2005) When is the brain enlarged in autism? A meta-analysis of all brain size reports. Biol Psychiatry 58(1):1–9
Richiardi L, Pizzi C, Pearce N (2013) Commentary: representativeness is usually not necessary and often should be avoided. Int J Epidemiol 42(4):1018–1022. https://doi.org/10.1093/ije/dyt103
Rieder RO, Nichols PL (1979) Offspring of schizophrenics III: hyperactivity and neurological soft signs. Arch Gen Psychiatry 36(6):665–674
Salinas YD, Wang Z, DeWan AT (2018) Statistical analysis of multiple phenotypes in genetic epidemiologic studies: from cross-phenotype associations to pleiotropy. Am J Epidemiol 187(4):855–863. https://doi.org/10.1093/aje/kwx296
Samek DR, McGue M, Keyes M, Iacono WG (2015) Sibling facilitation mediates the association between older and younger sibling alcohol use in late adolescence. J Res Adolesc 25(4):638–651. https://doi.org/10.1111/jora.12154
Savage JE, Jansen PR, Stringer S, Watanabe K, Bryois J, de Leeuw CA, … Posthuma D (2018) Genome-wide association meta-analysis in 269, 867 individuals identifies new genetic and functional links to intelligence. Nat Genet 50(7):912–919. https://doi.org/10.1038/s41588-018-0152-6
Schumann CM, Bloss CS, Barnes CC, Wideman GM, Carper RA, Akshoomoff N, … Courchesne E (2010) Longitudinal magnetic resonance imaging study of cortical development through early childhood in autism. J Neurosci 30(12):4419–4427. https://doi.org/10.1523/JNEUROSCI.5714-09.2010
Serdarevic F, Ghassabian A, van Batenburg-Eddes T, Tahirovic E, White T, Jaddoe VW, … Tiemeier H (2017) Infant neuromotor development and childhood problem behavior. Pediatrics 140(6):e20170884
Serdarevic F, Jansen PR, Ghassabian A, White T, Jaddoe VW, Posthuma D, Tiemeier H (2018) Association of genetic risk for schizophrenia and bipolar disorder with infant neuromotor development. JAMA Psychiat 75(1):96–98
Shaw P, Greenstein D, Lerch J, Clasen L, Lenroot R, Gogtay N, … Giedd J (2006) Intellectual ability and cortical development in children and adolescents. Nature 440(7084):676–679. https://doi.org/10.1038/nature04513
Shaw P, Eckstrand K, Sharp W, Blumenthal J, Lerch JP, Greenstein D, … Rapoport JL (2007) Attention-deficit/hyperactivity disorder is characterized by a delay in cortical maturation. Proc Natl Acad Sci USA 104(49):19649–19654. https://doi.org/10.1073/pnas.0707741104
Shaw P, Malek M, Watson B, Greenstein D, De Rossi P, Sharp W (2013) Trajectories of cerebral cortical development in childhood and adolescence and adult attention-deficit/hyperactivity disorder. Biol Psychiatry 74(8):599–606
Sheridan MA, Fox NA, Zeanah CH, McLaughlin KA, Nelson CA (2012) Variation in neural development as a result of exposure to institutionalization early in childhood. Proc Natl Acad Sci 109(32):12927–12932
Shrout P, Rodgers J (2018) Psychology, science, and knowledge construction: broadening perspectives from the replication crisis. Ann Rev Psychol 69:487–510
Smeland OB, Wang Y, Frei O, Li W, Hibar DP, Franke B, … Andreassen OA (2018) Genetic overlap between schizophrenia and volumes of hippocampus, putamen, and intracranial volume indicates shared molecular genetic mechanisms. Schizophr Bull 44(4), 854–864. https://doi.org/10.1093/schbul/sbx148
Smoller J, Andreassen O, Edenberg H, Faraone S, Glatt S, Kendler K (2019) Psychiatric genetics and the structure of psychopathology. Mol Psychiatry 24(3):409–420
Sugranyes G, de la Serna E, Borras R, Sanchez-Gistau V, Pariente JC, Romero S, … Castro-Fornieles J (2017) Clinical, cognitive, and neuroimaging evidence of a neurodevelopmental continuum in offspring of probands with schizophrenia and bipolar disorder. Schizophr Bull 43(6):1208–1219. https://doi.org/10.1093/schbul/sbx002
Szucs D, Ioannidis JP (2017) Empirical assessment of published effect sizes and power in the recent cognitive neuroscience and psychology literature. PLoS Biol 15(3):e2000797. https://doi.org/10.1371/journal.pbio.2000797
Thapar A, Rutter M (2015) Neurodevelopmental disorders. In: ThaparA, Pine DS, Leckman JF, Scott S, Snowling MJ, Taylor E (eds) Rutter’s child and adolescent psychiatry, 6th edn. Wiley, Chichester, pp 31–40
Van IJzendoorn M, Bakermans-Kranenburg M, Juffer F (2007) Plasticity of growth in height, weight, and head circumference: meta-analytic evidence of massive catch-up after international adoption. J Dev Behav Pediatr 28(4):334–343
van Os J, Jones P, Lewis G, Wadsworth M, Murray R (1997) Developmental precursors of affective illness in a general population birth cohort. Arch Gen Psychiatry 54(7):625–631
Van 't Ent D, den Braber A, Baselmans BML, Brouwer RM, Dolan CV, Hulshoff Pol HE, … Bartels M (2017) Associations between subjective well-being and subcortical brain volumes. Sci Rep 7(1):6957. https://doi.org/10.1038/s41598-017-07120-z
Westerhausen R, Friesen CM, Rohani DA, Krogsrud SK, Tamnes CK, Skranes JS, … Walhovd KB (2018) The corpus callosum as anatomical marker of intelligence? A critical examination in a large-scale developmental study. Brain Struct Funct 223(1):285–296. https://doi.org/10.1007/s00429-017-1493-0
Whelan R, Watts R, Orr CA, Althoff RR, Artiges E, Banaschewski T, … IMAGEN Consortium (2014) Neuropsychosocial profiles of current and future adolescent alcohol misusers. Nature 512(7513):185–189. https://doi.org/10.1038/nature13402
White T (2015) Subclinical psychiatric symptoms and the brain: what can developmental population neuroimaging bring to the table? J Am Acad Child Adolesc Psychiatry 54(10):797–798. https://doi.org/10.1016/j.jaac.2015.07.011
White T, El Marroun H, Nijs I, Schmidt M, van der Lugt A, Wielopolki PA, … Verhulst FC (2013) Pediatric population-based neuroimaging and the Generation R Study: the intersection of developmental neuroscience and epidemiology. Eur J Epidemiol 28(1):99–111. https://doi.org/10.1007/s10654-013-9768-0
Zhao B, Zhang J, Ibrahim JG, Luo T, Santelli RC, Li Y, … Zhu H (2019) Large-scale GWAS reveals genetic architecture of brain white matter microstructure and genetic overlap with cognitive and mental health traits (n = 17,706). Mol Psychiatry. https://doi.org/10.1038/s41380-019-0569-z
Zou R, Tiemeier H, Van Der Ende J, Verhulst FC, Muetzel RL, White T, … El Marroun H (2019) Exposure to maternal depressive symptoms in fetal life or childhood and offspring brain development: a population-based imaging study. Am J Psychiatry 176(9):702–710
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Section Editor information
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this entry
Cite this entry
Tiemeier, H., Muetzel, R. (2020). Population Neuroscience. In: Taylor, E., Verhulst, F., Wong, J., Yoshida, K. (eds) Mental Health and Illness of Children and Adolescents. Mental Health and Illness Worldwide. Springer, Singapore. https://doi.org/10.1007/978-981-10-2348-4_12
Download citation
DOI: https://doi.org/10.1007/978-981-10-2348-4_12
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-2346-0
Online ISBN: 978-981-10-2348-4
eBook Packages: Behavioral Science and PsychologyReference Module Humanities and Social SciencesReference Module Business, Economics and Social Sciences