Abstract
Chinese medicine (CM) practitioners usually base clinical decisions on their own experience and judgment. Although western medicine is now much dependent on objective measurements by medical equipment, in some fields such as in psychology and psychiatry, and in taking clinical information from history and physical examination, subjective measurements are still used. However, the difference is the use of standard data collection procedure. When a CM practitioner bases their collection of clinical information on a theoretical goal, information that fits one’s mind set is of concern and that does not fit one’s aim is subconsciously screened out. With this practice, the clinical information is biased toward a set of diseases and related zhengs in mind. The standardization procedures for clinical data collection can be applied to CM to solve this problem. This chapter will present scientific methods to make standard data collection procedures such as Delphi technique in creating a standard data collection procedure and the tests of its reliability. Objective domain-based technique for questionnaire and checklist design will be discussed. The essential steps in these procedures to ensure objective measurement are the independency of theories and expert opinions and the application of scientific validation methods of the resulting data collection forms. When the results of the studies using the discussed methods confirm the traditional theories, the theoretical foundation of such the disease or zheng in CM is confirmed. When studies consistently disagree with the traditional theories, objective modification of theories makes CM moving forward and gets acceptance by western medicine.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
6.1 Introduction
For thousands of year, traditional eastern medicine (TEM), mainly used in China (Chinese Medicine, CM), Korea, Mongolia, and Tibet, has founded its theories and practices on subjective clinical information collected by observation of patients’ history, living environment, body foundation, clinical signs and symptoms of diseases, pulse palpation, and other clinical evaluation methods. China is the country that has been conducting studies in CM, so the author uses the word CM to cover the ideas and practices in TEM as a whole.
In the far past, western medicine (WM) and medical practices in other countries in Asia, such as Ayurvedic medicine in India, and traditional medicine in Southeast Asia used the same concept of clinical symptoms and signs to classify diseases as well. Diseases were believed to be caused by internal imbalance, response to the environmental change, as well as the supernatural power such as miasma, curse, and intoxication [1]. At that time, CM and Ayurvedic medicine seem to base on a firmer background of disease concept than that of the western medicine.
6.1.1 A Big Leap in Western Medicine
Around early to late nineteenth century during the time of John Snow [1, 2], Louis Pasteur [3], Robert Koch [4], and Joseph Lister [5], the discovery of germs and germ infection as the cause of infectious diseases changed the classification of the disease in western medicine to the cause of diseases rather than the classification based on presenting symptoms and signs of diseases. Such the paradigm shift in disease classification as well as the growth of material science has laid the western style of medicine very solid background for theories of diseases.
While WM practices have moved toward objective measurements, it seems like CM has been far lacking behind. CM practitioners still base their clinical decision on their own experience and judgment.
However, there are still some diseases such as psychotic disease and psychological problems that leave rooms for doctor’s judgment for diagnosis and treatment of the diseases or disorders based on patients’ symptoms and signs. In these conditions, practitioners take clinical information from history taken by patient interview, physical examination, and use subjective decision in which inconsistency in diagnosis and clinical decision varies by presentation of patients’ symptoms and signs and also by doctors’ experience.
6.1.2 The Difference Between WM and CM
However, the difference in the practice among CM and psychiatric practitioners is the use of standard data collection procedure. Various screening tests for psychiatric problems have been developed and tested for reliability and validity in systematic ways. Attitude, belief, and anything related to personal judgment fall into this phenomenon as well. Wealth and health statuses are rather subjective measurement. Health professions know this problem and have tried to develop methods to tackle this uncertainty of measurement.
One of the serious pitfalls in CM in clinical data collection is the use of its theory to guide history taking procedure, physical examination, and in collection of all other clinical information from the patients. When one uses a theoretical goal to collect clinical information, information that fits one’s mind set is of concern and that does not fit one’s aim is screened out. With this convention, the clinical information is biased toward a set of diseases and related zheng in mind. Other information that suggest the possibility of another set of diseases being intentionally excluded. The approach of western medicine nowadays is to make use of a check list of all relevant information formulated by various statistical techniques so that the goal is not set as the disease or zheng in mind. Such standardization procedures for clinical data collection in western medicine can be applied in as well.
We are presenting scientific methods to make standard data collection procedures such as Delphi technique in creating a standard data collection procedure and the tests of its reliability. Objective-domain-based technique for questionnaire and checklist design will be discussed as well. The essential steps in these procedures to ensure objective measurement are the independency of theories and expert opinions and the application of scientific validation methods of the resulting data collection forms.
6.2 Standardization of Data Collection
Standardized data collection tool is an agreed instrument which enables data concerning patients, therapists, and/or healthcare settings and approaches to be collected unambiguously by a range of practitioners in a number of different clinical settings of clinical practice of services collecting and recording [6]. The standardization is the process to ensure that the data collected are reliable, precise, and reproducible. It is true that standardization of data collection cannot avoid uncertainty of the data by subjective decision. However, there are processes in minimizing uncertainty of measurement using the standard data collection methods.
In WM, standardized data collection tools may be in descriptive document where essential items are written in the medical records, data collection forms, or electronic devices. The format of data collection tools does not matter when all the essential information is collected. The important issue is how the essential information is summarized and who decide that the information is important and complete.
In CM, practitioners usually note the patient data on the medical records. CM practitioners base their decision on what to note and how to get the information on the theory of CM they are using. The problem in this practice is that there are different theories used in different text books or schools they graduated from, and the different in experiences of the CM practitioners themselves.
6.2.1 Delphi Technique
The Delphi technique is named after the Pythia prophecy, also known as the Oracle of Delphi, in the Temple of Apollo at Delphi, a place located on the slopes of Mount Parnassus in the ancient Greece. Many famous Greek leaders came to have their questions answered at Delphi.
The Delphi technique used nowadays is not the mythical one mentioned above. It mainly developed by Dalkey and Helmer at the Rand Corporation in the 1950s [7, 8], which is a widely used method for achieving convergence of opinion concerning real-world knowledge solicited from experts within certain topic areas. The Delphi technique is designed as a group communication process that aims at conducting detailed illumination and discussions of a specific issue in various fields. The technique attempts to address the question of what should be expected in case a situation occurs [9].
The Delphi technique is well suited as a means and method for building a convergent agreement using a series of questionnaire to collect data from a panel of selected informants. The process requires multiple iterations designed to develop a convergence of opinion concerning a specific topic. Theoretically, the Delphi process can be iterated until consensus is determined to have been achieved or none of the experts changes the idea. However, studies suggested that three iterations are often sufficient to collect the important information and to reach a convergence in most cases even in different topics of study [8, 10, 11].
There is a series of steps to construct a checklist that can be applied to the standard data collection form development. We suggest an approach consisted of five predefined steps [10, 12–15].
-
(1)
Literature review: A thorough literature review must be done so that a list of symptoms and signs related to the disease under study is formulated. There are different textbooks and schools of CM, those written or taught in those textbooks and schools must not be omitted.
-
(2)
Checklist design: The researchers/developers draft the initial checklist in which symptoms and signs should be systematically grouped in domains for ease of making decision by experts.
-
(3)
Scores of the items: Experts are asked to score their opinions on the items in semi-quantitative scales (see the next topic). The semi-quantitative opinions can be one of the 3, 5, or 10 Likert-type scales, or they can be in a visual analog scale.
-
(4)
Expert consensus: Now that the initial checklist is made, send the checklist to a group of no less than five experts to review and score it in at least three rounds. The developers must ask their opinions if any missing items should be added. Experts must be distributed in different schools of CM. The details of Delphi process are discussed later.
-
(5)
Finalization: After finishing Delphi process, the results must be published, disseminated, implemented, and updated at interval.
The Delphi process is a series of activities to accomplish the conclusion of the idea or a checklist of symptoms and signs of the disease of interest in CM. In drafting a checklist, one may review the literatures and textbooks and design a checklist by oneself. The problem of the action is the acceptance by experts and practitioners. Being an expert is not the exception. To avoid this problem, it is necessary to have experts and practitioners to get involved in the process. The Delphi process to ensure valid results includes the following steps.
-
(1)
Setting up a steering committee: The researchers must set up a steering committee to control the quality of whole development process and determine the contents of the checklist. The committee members must be senior researchers who have authority in CM field. It is not necessary that they are in the field of study and must not be the member of informant experts.
-
(2)
Tasks of steering committee: Their tasks are to give the direction, to help in any steps that the researchers request, and to make sure that the researchers are not misconducting. The steering committee must discuss with the researchers to approve the final list of experts and also approve the results of literature search, the initial checklist, and facilitate the contact of expert panel through their authority.
-
(3)
Roles of expert panel: The expert panel must clearly know the aims of the study and agree to complete all rounds of the discussion. They must know that they themselves are also the subjects of the study.
-
(4)
Rounds of Delphi process: In traditional Delphi process, it is advised that the process should begin with open-ended questions [16]. In this chapter where we are going to make a structural checklist, it is necessary to start with a structured initial one. The researchers are responsible to draft an initial checklist and distribute to experts who are approved by the steering committee. The researchers are also collect their opinions and summarize the results of the first round and send the feedback to them and ask for the second round of their opinions. In summarization of the results of the first round, researchers must set the threshold of the response before hand. Any items that get an average score below the threshold would be cut from the second round of the checklist. Such process and threshold must be known by the expert panel at the invitation to join the study. Repeat the process in the third round. As mentioned earlier that three iterations are usually enough to get a high intra-rater agreement even the inter-rater agreement is not high [10], the results of the second and third rounds are usually similar and the fourth round is not necessary.
-
(5)
Summary reports: Researchers must report back the results of the study to all members of the expert panel and the steering committee. Together with the report, a letter of thanks arid appreciation of their help should be sent.
For clinical use, it is easier to use when the checklist consists of items with answers yes or no, present or absent. However, there are some cases that the answers should be graded where the knowledge of constructing a semi-quantitative answer described below is required. Thus, the final checklist for clinical use is not the one that the expert panels see but is a practical checklist that is easy to use by practitioners.
In summary, the Delphi technique is time and effort consuming procedure. However, it is necessary if one needs a checklist of symptoms and signs in CM that is accepted by the majority of the CM practitioner, irrespective of textbooks they are using or the school from which they were graduated.
6.3 Construction of a Semi-quantitative Measurement
Some variables are in nominal scale and mutually exclusive. In this case, a semi-quantitative measurement is not appropriate. For example, a patient can be male or female but not in between the two. For allergy, a series of questions to explore which allergen the patient exposed in the last few days, such as whether the patient recently ate seafood, can be answered as yes or no. The amount of exposure is not important in finding the potential allergen. In this situation, a binomial measurement is suitable.
However, there are a lot more clinical symptoms and signs that the extent of the phenomenon, i.e., the exposure to external environment and the manifestation of a disease, can be graded with a quantitative measurement obtained from a medical equipment such as body temperature and blood sugar level. However, there are a number of gradable clinical manifestations that need interpretation by doctor’s observation. In this case, a semi-quantitative measurement is needed.
A semi-quantitative measurement is the procedure to transform qualitative measurement in detecting the presence or absence of a subjective observation to provide a numeric representation of the amount of the observed phenomenon. A binomial measurement of the presence or absence of a phenomenon of interest is graded into a range of score for the observed event. The benefit of this method is to make room for observers to state an uncertainty they observe between the presence and absence of the occurrence of that symptom or sign. In fact, in many cases observers are sure that the event is absent or present. In situation that they are not certain to state the extremes, they have an opportunity to say that the fact is likely to be somewhere between the two ends.
On the other hand, the semi-quantitative assessment is also used in interpretation of the results in scientific measurement in percentage or continuous scales that are hard to interpret into a few categories, i.e., low, medium, and high. In this case, uncertainty occurs around the cutpoints as well. This phenomenon is not important to CM since it also occurs in results from medical equipment and statistical analysis in WM.
Even one cannot avoid uncertainty of the semi-quantitative measurement, it is better to state the intermediate or indeterminate decision rather than to force the evidence to be on an extreme side of binomial determination. Some may prefer Likert-type scales of 1 to 3, 5, 10, or 100 in measuring different phenomena. Some may use a visual analog scale (VAS) where observers of patients can mark their decision on the symptom or sign on a straight line where 0 and 10 or 100 are on the two opposite ends. In measurement of severity of pain, doctors in WM usually use a VAS score and 0 means no pain at all and 10 or 100 means the severity of pain that the patient cannot tolerate.
The use of semi-quantitative measurement is clear when a doctor wants to follow a clinical presentation in a long period of time. It is easy to follow the change in ordinal or continuous scales than in a binomial scale. CM practitioners can adopt such a concept to evaluate the presence of a phenomenon to an ordinal or continuous scale of its severity and use the score in statistical analysis.
CM practitioners may feel uncomfortable to classify zheng as a probability with uncertainty as shown above. However, in clinical practice of CM, one can see variability of signs, symptoms, and zheng in a patient. With this method, it is easy in describing the change in these things over time. And it also allows CM practitioners to communicate the zheng diagnosis in the way that a patient has got moderate degree of this zheng and some degree of another or others at the same time.
6.4 Statistical Methods for Grouping of Signs and Symptoms
The presence of a group of signs and symptoms of patients, and probably with history of past exposure to climate or diet, leads to zheng classification of a disease and diagnosis of a disease. It is possible that the classification of zhengs and diseases is different from one to another school of CM, and it may change when systematic analysis of signs and symptoms is evaluated by systematic methods using statistics of grouping.
There are a series of statistical methods to solve grouping problems of clinical manifestations of a disease to identify underlying zheng classification. Usually, we use statistical models in the group of latent class analysis and cluster analysis. Other appropriate models can be applied whenever they can group sets of variable with reasonable statistical presumptions and constrains.
6.4.1 Latent Class Analysis
Latent class analysis (LCA) is a statistical method for identifying unmeasured class membership among subjects in a dataset using categorical and/or continuous observed variables. LCA procedure defines latent classes by the criterion of ‘conditional independence.’ This means that each variable is statistically independent of every other variable within each latent class. For example, within a latent class corresponding to a distinct syndrome, the presence/absence of one symptom is viewed as unrelated to presence/absence of all others. Alternative models were described by Lindsay et al. [17].
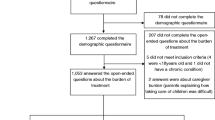
The study of Yang et al. [18] was an example of the use of LCA on dichotomous outcomes. Zheng classification of psoriasis was evaluated using this method on a standardized clinical checklist developed by the Delphi technique [10]. Three zhengs were identified and the difference from those documented in the textbooks was discussed. In Yang’s study, dichotomous nature of signs and symptoms was used. For grade characteristics such as tongue coating, they transformed the grades into a series of binomial variables, i.e., thing and thick tongue coating to the presence of thin tongue coating—yes or no, thick tongue coating—yes or no.
Further derivation of LCA is the latent tree model (LTM) described in detail by Zhang et al. [19, 20]. In-depth explanation of the statistical methods of both LCA and LTM is skipped since the aim of this chapter is on standardization of data collection not on statistical analysis.
6.4.2 Cluster Analysis
Cluster analysis is a multivariate method which aims to classify a sample of subjects (or objects) on the basis of a set of measured variables into a number of groups in which similar subjects are placed [21]. It is used in various fields in sciences. An example where the method is used in the field of psychiatry is to characterize patients on the basis of clusters of symptoms. In public health, it is used to identify disease outbreaks. It can also be applied to identify clusters of signs and symptoms which relate to zhengs in a disease [22]. Cluster analysis is also used in classification of Chinese herbs and network of herbs used in some diseases [23, 24].
References
Tognotti E. The dawn of medical microbiology: germ hunters and the discovery of the cause of cholera. J Med Microbial. 2011:60(Pt 4):555–8. doi:10.1099/jmn.0.025700-0.
Lippi D, Gotuzzo E. The greatest steps towards the discovery of Vibrio cholerae. Clin Microbiol Infect. 2014;20(3):191–5. doi:10.1111/1469-0691.12390.
Toledo-Pereyra LH. Louis Pasteur surgical revolution. J Invest Slug. 2009;22(2):82–7. doi:10.1080/08941930902794729.
Blevins SM, Bronze MS. Robert Koch and the ‘golden age’ of bacteriology. Int J Infect Dis. 2010;14(9):e744–51. doi:10.1016/j.ijid.2009.12.003.
Toledo-Pereyra LH. Joseph Lister’s surgical revolution. J Invest Surg. 2010;23(5):241–3. doi:10.3109/08941939.2010.520574.
Moore AP, Bryant EC, Olivier GWJ. Development and use of standardised data collection tools to support and inform musculoskeletal practice. Man Ther. 2012;17(6):489–96. doi:10.1016/j.math.2012.07.008.
Dalkey NC, Helmer O. An experimental application of the Delphi method to the use of experts. Manag Sci. 1963;9(3):458–67.
Hsu C-C, Sandford BA. The Delphi technique: making sense of consensus. Pract Assess Res Eval. 2007;12(10):1–7.
Miller LE. Determining what could/should be: The Delphi technique and its application. Paper presented at the meeting of the 2006 annual meeting of the Mid-Western Educational Research Association, Columbus, Ohio. 2006.
Yang X, Chongsuvivatwong V. McNeil E, Ye J, Ouyang X, Yang E, Srip lung H. Developing a diagnostic checklist of traditional Chinese medicine symptoms and signs for psoriasis: a Delphi study. Chin Med. 2013;8(1):10. doi:10.1186/1749-8546-8-10.
Witt CM, Aickin M, Cherkin D, Che CT, Elder C, Flower A, et al. Effectiveness guidance document (EGD) for Chinese medicine trials: a consensus document. Trials. 2014;15:169. doi:10.1186/1745-6215-15-169.
Schmutz J, Eppich WJ, Hoffmann F, Heimberg E, Manser T. Five steps to develop checklists for evaluating clinical performance: an integrative approach. Acad Med. 2014;89(7):996–1005. doi:10.1097/ACM.0000000000000289.
Mullen PM. Delphi: myths and reality. J Health Organ Manag. 2003;17(1):37–52.
Pietersma S, de Vries M, van den Akker-van Made ME. Domains of quality of life: results of a three-stage Delphi consensus procedure among patients, family of patients, clinicians, scientists and the general public. Qual Life Res. 2014;23(5):1543–56. doi:10.1007/s11136-013-0578-3.
Shi N, Zhong LL, Han X, Ziea IC, Ng B, Bian Z, Lu A. Enhanced evidence-based Chinese medicine clinical practice guidelines in Hong Kong: a study protocol for three common diseases. Evid Based Complement Altern Med. 2015;2015:482706. doi:10.1155/2015/482706.
Custer RL, Scarcella JA, Stewart BR. The modified Delphi technique: a rotational modification. J Vocat Tee Educ. 1999;15(2):1–10.
Lindsay B, Clogs CC, Grego J. Semiparametric estimation in the Rasch model and related exponential response models, including a simple latent class model for item analysis. J Am Stat Assoc. 1991;86(413):96–107.
Yang X, Chongsuvivatwong V. Lerkiatbundit S, Ye J, Ouyang X, Yang E, Sriplung H. Identifying the Zheng in psoriatic patients based on latent class analysis of raditional Chinese medicine symptoms and signs. Chin Med. 2014;9(1):1. doi:10.1186/1749-8546-9-1.
Zhang NL, Yuan S, Chen T, Wang Y. Latent tree models and diagnosis in traditional Chinese medicine. Artif Intell Med. 2008;42(3):229–45.
Zhang NL, Yuan S, Chen T, Wang Y. Statistical validation of traditional chinese medicine theories. J Ahem Complement Med. 2008;14(5):583–7. doi:10.1089/acm.2007.7019.
Everitt BS. Cluster analysis. Chichester, West Sussex, U.K.: Wiley; 2011.
Tao F, Lu H, Oppert JM, Basdevant A. MENG may contribute to obesity phenotypes based on body composition: a pilot study on the traditional Chinese medicine approach. Evid Based Complement Altemat Med. 2014;2014:580803. doi:10.1155/2014/580803.
Pang J, Yang M, Fu J, Zhao X, van Wijk E, Wang M, Liu Y, Zhou X, Fan H, Han J. Classification of Chinese herbs based on the cluster analysis of delayed luminescence. Luminescence. 2015. doi:10.1155/2014/580803.
Chen HY, Lin YH, Hu S, Yang SH, Chen JL, Chen YC. Identifying Chinese herbal medicine network for eczema: implications from a nationwide prescription database. Evid Based Complement Altemat Med. 2015;2015:347164. doi:10.1155/2015/347164.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media Singapore
About this chapter
Cite this chapter
Sriplung, H., Yang, X. (2016). A Need for Standard Data Collection Procedure in Studies on Traditional Chinese Medicine. In: Leung, Sw., Hu, H. (eds) Evidence-based Research Methods for Chinese Medicine. Springer, Singapore. https://doi.org/10.1007/978-981-10-2290-6_6
Download citation
DOI: https://doi.org/10.1007/978-981-10-2290-6_6
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-2289-0
Online ISBN: 978-981-10-2290-6
eBook Packages: MedicineMedicine (R0)